Abstract
Objectives
As the primary public health strategy for controlling the 2022 Mpox outbreak, it is critical to evaluate the impact of Mpox vaccination campaigns for transgender people and gay, bisexual and other men who have sex with men (T/GBM). We measured vaccine uptake and associated factors among T/GBM clients of an urban STI clinic in British Columbia (BC).
Methods
We conducted a cross-sectional online survey between August 8–22, 2022 of clients who had attended the STI clinic, 5–7 weeks following the first-dose Mpox vaccination campaign in BC. We drew on a systematic review of factors associated with vaccine uptake to develop survey questions, and measured vaccine uptake among vaccine-eligible T/GBM.
Results
Overall, 51% of T/GBM had received the first dose of the vaccine. The sample (331 participants) was majority White and university educated, identified as a man and gay, 10% had trans experience, and 68% met eligibility criteria for vaccination. Among vaccine-eligible participants identifying as T/GBM, 66% had been vaccinated; being unvaccinated was more common among participants identifying as bisexual or heteroflexible/mostly straight, and who spent less time with other T/GBM. Eligible yet unvaccinated participants had lower perceived susceptibility, and reported fewer cues to action (e.g., fewer saw information promoting the vaccine), and increased constraints to vaccine access; vaccine barriers related to accessing clinics and privacy were common. The majority (85%) of those eligible and unvaccinated at time of survey were willing to receive the vaccine.
Conclusion
In this sample of STI clinic clients, vaccine uptake among eligible T/GBM was high in the initial weeks following a Mpox vaccination campaign. However, uptake was patterned on social gradients with lower uptake among T/GBM who may be less effectively engaged by available promotion channels. We recommend early, intentional and diverse engagement of T/GBM populations in Mpox and other targeted vaccination programs.
Keywords: Mpox, Monkeypox, Transgender, Gay, Men who have sex with men, Vaccine, Uptake
1. Introduction
Mpox (formerly known as monkeypox) is a zoonotic infection which has primarily occurred in several countries in Central and West Africa, and reported over the last four decades. In May 2022, an outbreak of Mpox was identified in multiple countries where the disease has not to date been endemic, mainly involving populations of Two-Spirit, transgender, gay, bisexual and other men who have sex with men (2STGBM) with primary transmission through sexual contact.[1] At the time of writing (November 29, 2022), 110 countries have reported 81,107 confirmed Mpox cases and 55 deaths.[2] In Canada, 1,456 cases have been reported, with an epidemic peak occurring in July-August 2022.[3] In response, Health Canada supplied provinces with the live-attenuated, non-replicating Smallpox and Mpox Vaccine Modified Vaccinia Ankara-Bavarian Nordic® (Imvamune ®; hereafter referred to as Mpox vaccine), and was initially used for post-exposure prophylaxis of contacts during public health follow-up of cases.[4] The Mpox vaccine was then supplied for pre-exposure prophylaxis for individuals at higher risk of Mpox infection with provinces rolling out vaccination campaigns targeting 2STGBM in June-July 2022.
Given that vaccination has been a primary public health strategy for controlling the Mpox outbreak, it is critical to evaluate the impact of Mpox vaccination campaigns for 2STGBM. While the effectiveness of the current Mpox vaccine (Imvamune) in relation to the currently circulating strain is an area of ongoing study, understanding the vaccine uptake among 2STGBM populations in relation to ongoing transmission is also important in determining whether population vaccination levels may be high enough to prevent local transmission and control or eliminate Mpox in a geographic region (i.e., as herd immunity is a function of both vaccine coverage and vaccine effectiveness).[5] Furthermore, assessing factors that may affect differential uptake by groups of 2STGBM including vaccine acceptability, knowledge and beliefs can help identify the extent to which - and where - further vaccine promotion and delivery may be needed to improve social equity of the public health response. Studies to date among 2SGBTM have demonstrated high overall acceptability of the Mpox vaccine, which may be patterned along social gradients.[6], [7], [8] However, acceptability may not predict actual uptake of vaccine and to our knowledge few studies of Mpox vaccine uptake among 2SGBTM have been reported.
This study took place in the initial months of the Mpox outbreak in British Columbia (BC) with an overall goal of informing ongoing vaccination programming, which initially focused on transgender people and gay, bisexual and other men who have sex with men (T/GBM; used in this manuscript when specifically referring to our study findings instead of the more broadly inclusive 2STGBM). The objective of our study was to assess the acceptability and uptake of Mpox vaccine among T/GBM clients of an STI clinic in Vancouver, BC, and identify factors associated with uptake. Considering that vaccines continued to be delivered to this population at the time of our survey, we hypothesized that uptake of vaccine would be<66% (based on self-reported uptake of meningococcal C vaccine in a community survey of gay, bisexual and other men who have sex with men following an outbreak in BC in 2006).[9] We hypothesized that acceptability among unvaccinated clients in our sample would be high (>63%, the average estimate of vaccine acceptability in a systematic review of vaccine outcomes among GBM drawing on studies of vaccines commonly offered to this population).[10].
2. Materials and methods
2.1. Study design, population, and setting:
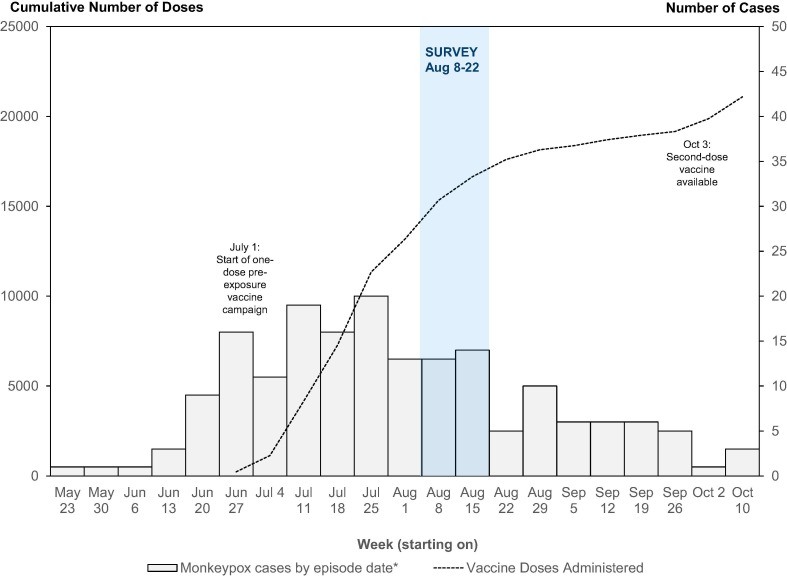
We conducted a cross-sectional online survey among clients of a low-barrier sexually transmitted infection (STI) clinic in Vancouver, Canada operated by the BC Centre for Disease Control (BCCDC) which typically sees > 10,000 clients per year. This online survey was conducted from August 8 to 22, 2022, starting nine weeks following the detection of the first Mpox case in BC and five weeks following the implementation of a single-dose pre-expo sure prophylaxis vaccination campaign with Mpox vaccine on July 1 (Fig. 1 ; the campaign was expanded to a two-dose vaccination campaign in October 2022). Transgender people and people who self-identified as belonging to the gay, bisexual and other men who have sex with men community (18 years or older) and who self-identified as meeting any of the following eligibility criteria were eligible to receive the vaccine: 1) having a bacterial STI diagnosis (i.e., chlamydia, gonorrhea, syphilis) in the past two months; 2) having had two or more sexual partners in the past 21 days; 3) having attended venues or other locations for sexual contact within the past 21 days (e.g., bath houses, sex clubs, park play) or may be planning to; 4) having anonymous/casual sex in the past 21 days (e.g., using apps, online sites formal/informal gatherings) or may be planning to; 5) engaged in sex work or may be planning to, either as a worker or a client. In recognition that societal stigma may lead to hiding of identities and behaviours among sexual and gender minorities, and anticipation of privacy concerns among the T/GBM population who would benefit from vaccination, in BC a low-barrier approach was used in Mpox vaccination clinics. Individuals presenting for vaccination were not required to show identification, and were shown information about eligibility criteria and asked whether they are met (i.e., without requiring individuals to disclose how they meet eligibility requirements). For further information about the measures taken in the BC context in response to the outbreak that may influence vaccination outcomes, please see Supplementary Data 1.
Fig. 1.
Monkeypox cases and doses of vaccine administered, British Columbia, May to September 2022.
2.2. Survey instrument
We drew on a broad, social-ecological framework of vaccine acceptability, uptake and completion in GBM based on a systematic review and meta-analysis of literature to identify factors potentially affecting vaccination outcomes.[10] In this framework, vaccine outcomes are situated within an interrelated system comprising multiple levels. At the individual level, we also drew on behavioural and psychological theories associated with vaccine acceptability, hesitancy, and uptake including: i) the Health Belief Model, for identifying individual-level factors motiving an individual to receive a vaccine (drawing on its six concepts of perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, and self-efficacy);[11] and psychological antecedents of vaccination (5Cs: confidence, complacency, constraints, calculation, and collective responsibility).[12] Questions based on these frameworks were adapted to the local context of the Mpox outbreak and public health response in British Columbia. In total, the survey domains covered socio-demographics, sexual history, Mpox knowledge, beliefs, psychological antecedents of vaccination and cues to action. The survey was piloted (and subsequently revised) with nine members of our research team’s Community Advisory Board and research staff, the majority of whom self-identify as or have experience working with T/GBM. Please see Supplementary Data 2 for a copy of the survey instrument used in our study.
2.3. Recruitment and data collection:
We used established recruitment methods to invite STI clinic clients who had previously consented to be contacted for research to participate in this survey (∼20% of all clinic clients).[13], [14] A generic e-mail invitation to the survey was sent to all consenting clients who visited the clinic between June 1, 2019 and May 31, 2022, with a link to the online survey landing page which outlined the additional eligibility criteria (age 16 years and older and able to complete a survey in English) and provided the information needed for informed consent. Proceeding to start the survey was considered provision of informed consent, and all participants starting the survey were offered the opportunity to enter a prize draw for a $200 VISA gift card. The initial recruitment email was sent on 8 August 2022, with three follow-up reminders before survey closure on August 22, 2022. Survey data were collected and managed using REDCap electronic data capture tools hosted at the BC Children’s Hospital Research Institute.[15] Ethics approval for this study was obtained from the UBC Behavioural Research Ethics Board.
2.4. Statistical analysis:
Data from all submitted questionnaires were imported into R version 3.5.2 (2018–12-20)[16] for analysis. We restricted this analysis to all participants who self-identified as T/GBM at the time of the survey (based on answering “Yes” to the question: “In BC, the Mpox vaccine is available to transgender people or people who self-identify as belonging to the gay, bisexual or other men who have sex with men community. Based on this description, would you qualify for the vaccine?”). Our main outcomes of interest were vaccine uptake, defined as receipt of the first dose of the Mpox vaccine (“Have you received a dose of the Mpox vaccine?” coded as “yes” vs “no/not sure”) and vaccine acceptability among participants, defined as either receipt of vaccine, or, if not vaccinated, willingness to receive the Mpox vaccine (“How unwilling or willing are you to receive the Mpox vaccine?” coded as “very willing/willing” vs. “neither unwilling nor willing/unwilling/very unwilling”). Due to limited data on which to estimate vaccine uptake shortly after the start of a vaccination campaign, we based our sample size calculation on vaccine acceptability. Based on an expected average vaccine acceptability among T/GBM of 63%[10] with a 95% confidence interval, 5% margin of error, an underlying population estimate of 37,900 GBM in the geographic region serviced by the clinic (unpublished data), our desired sample size was 347 T/GBM completing the survey. For the five psychological antecedents of vaccination constructs a validated short scale was used, with scores assigned from 1 (low) to 7 (high), with reverse coding for the construct related to collective responsibility.[12].
We used descriptive analysis to describe vaccine outcomes for the total analytic sample, and stratified by self-reported eligibility for vaccine (binary variable based on reporting meeting at least one of the five eligibility criteria listed above since the start of the vaccination campaign), and characteristics of participants within each stratum. Restricting the sample further to those eligible, we then used bivariate analyses to assess the relationship between explanatory variables and vaccine uptake using Pearson’s chi-square, Fisher’s exact test, or t-test as appropriate. Participants with missing data for each variable analysed were excluded, which had a greater impact for questions asked later in the survey (including socio-demographics questions). Due to multiple comparisons, we set our level of significance at p-value < 0.01.
3. Results
Overall, 3,930 clients consenting to be contacted for research were sent an email invitation to the survey, of which 3,539 (90.0%) had valid email addresses; 26.7% (946/3,539) consented and began the survey. Sixty-seven participants were excluded for not answering the T/GBM identity question (40) and not living in BC at the time of the survey (27). Of the remaining 879 participants, 331 (37.7%) self-identified as T/GBM and represent our final analytic sample. The median age of participants was 34 years, and the majority of participants were White (178/298, 59.7%), identified as a man (227/298, 76.2%) and gay (206/298, 69.1%), and were university educated (194/298, 65.1%). Ten percent (9.8%, 29/296) identified as transgender, 7.1% (21/296) as living with HIV, and 14.4% (43/298) reported an annual income of less than CDN $20,000 (see Table 1 for a full description of sample characteristics). No participant reported having tested positive for Mpox infection in the past three months.
Table 1.
Key sociodemographic characteristics of the transgender people and gay, bisexual and other men who have sex with men included in the final analytic sample (N = 331).
| Variable |
Total Sample (N=331)* n/N (%) |
|---|---|
| Age (median (IQR)) | 34 years (28-41) |
| Race/Ethnicity (check all that apply) | |
| Indigenous (First Nations, Inuk/Inuit, Métis) | 13/298 (4.4%) |
| Black | 3/298 (1.0%) |
| East Asian | 39/298 (13.1%) |
| Latin American | 38/298 (12.8%) |
| Hispanic | 14/298 (4.7%) |
| Middle Eastern | 5/298 (1.7%) |
| South Asian | 14/298 (4.7%) |
| Southeast Asian | 23/298 (7.7%) |
| White | 178/298 (59.7%) |
| Another race category | 10/298 (3.4%) |
| Prefer not to say | 3/298 (1.0%) |
| Two-Spirit (among Indigenous respondents) | 7/298 (2.3%) |
| Gender identity (check all that apply) | |
| Agender | 4/298 (1.3%) |
| Genderfluid | 10/298 (3.4%) |
| Genderqueer | 20/298 (6.7%) |
| Man | 227/298 (76.2%) |
| Non-Binary | 25/298 (8.4%) |
| Woman | 30/298 (10.1%) |
| Unsure/questioning | 4/298 (1.3%) |
| Other term | 2/298 (0.7%) |
| Prefer not to say | 4/298 (1.3%) |
| Gender identity: | |
| Transgender | 29/296 (9.8%) |
| Cisgender | 249/296 (8.4%) |
| Other / Prefer not to say | 18/296 (6.1%) |
| Sexual identity (check all that apply) | |
| Asexual | 4/298 (1.3%) |
| Bi (bisexual) | 52/298 (17.4%) |
| Gay | 206/298 (69.1%) |
| Heteroflexible (mostly straight) | 20/298 (6.7%) |
| Lesbian | 7/298 (2.3%) |
| Pansexual | 34/298 (11.4%) |
| Queer | 55/298 (18.5%) |
| Straight (heterosexual) | 6/298 (2.0%) |
| Other term | 7/298 (2.3%) |
| Prefer not to say | 5/298 (1.7%) |
| Education | |
| High school or equivalent (or less) | 35/298 (11.7%) |
| Post-secondary school (e.g., certificate, diploma) | 67/298 (22.5%) |
| Bachelor’s degree | 132/298 (44.3%) |
| Graduate degree (Master’s, PhD, MD, etc.) | 62/298 (20.8%) |
| Prefer not to say | 2/298 (0.7%) |
| Annual income | |
| Less than $20,000 | 43/298 (14.4%) |
| $20,000-$39,000 | 66/298 (22.1%) |
| $40,000-$59,000 | 61/298 (20.5%) |
| $60,000-$79,000 | 44/298 (14.8%) |
| $80,000 or more | 72/298 (24.2%) |
| Prefer not to say | 12/298 (4.0%) |
| Employment (check all that apply) | |
| Employed full-time (30+ hours/week) | 181/298 (60.7%) |
| Employed part-time (less than 30 hours/week) | 39/298 (13.3%) |
| Self-employed (e.g., professional, contractor, business owner) | 48/298 (16.1%) |
| On government assistance (e.g., on disability, E.I.) | 12/298 (4.0%) |
| Student | 35/298 (11.7%) |
| Retired | 13/298 (4.4%) |
| Unemployed | 11/298 (3.7%) |
| Unable to work | 6/298 (2.0%) |
| Prefer not to say | 1/298 (0.3%) |
| Unstable Housing | |
| Homeless in the past year (e.g., live in shelter, street, parks, makeshift shelter, vehicle, abandoned building) | 5/298 (1.7%) |
| Temporarily live with someone else in past year because had nowhere else to live | 22/298 (7.4%) |
| Ever diagnosed with HIV | 21/296 (7.1%) |
*Note: 298 participants in our sample completed the socio-demographic section of the questionnaire.
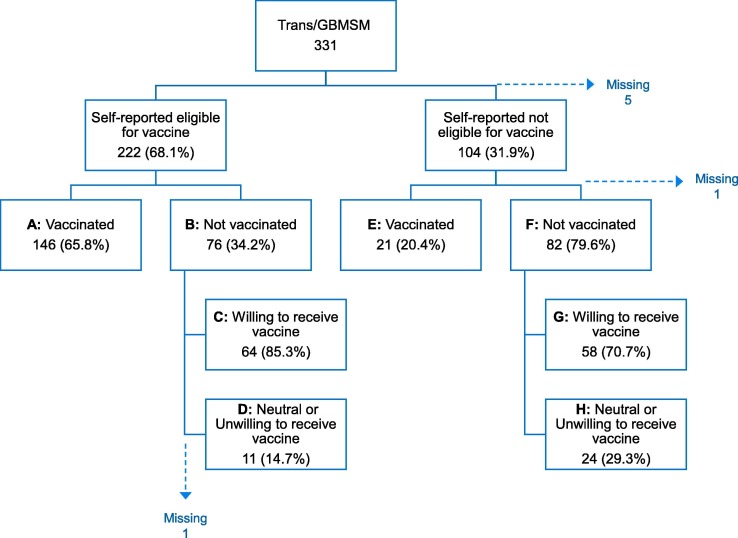
Among all T/GBM participants in our survey vaccine acceptability was 89.2% (289/324) and vaccine uptake was 51.4% (167/325; Fig. 2 ). Two-thirds of T/GBM participants (222/326, 68.1%) reported being eligible for vaccination, with a vaccine uptake of 65.8% in this group (146/222). Among the 76 eligible participants who had not been vaccinated, vaccine acceptability was 85.3% (64/75). Of the 104 participants reporting not being eligible for vaccination, 20.4% (21/103) had received the vaccine (i.e., in our sample, of the participants who received the vaccine 87.4% (146/167) self-identified as being eligible for vaccination). Of participants who reported receiving one dose of the vaccine, 92.1% (152/165) strongly agreed/agreed they would get a second dose of the vaccine if recommended.
Fig. 2.
Distribution of monkeypox vaccine outcomes among the final analytic sample of transgender people and gay, bisexual and other men who have sex with men (T/GBM).Note: Vaccine uptake overall was 51.4% [167/325=(A + E)/(A + B + E + F)]. Vaccine acceptability overall was 89.2% [289/324=(A + C + E + G)/(A + C + D + E + G + H)] and among eligible participants was 95.0% [210/221=(A + C)/(A + C + D)]. Percentages calculated from previous step excluding missing results.
On comparing sociodemographic characteristics of eligible participants by vaccination status, we found statistically significant differences by gender identity and sexual identity (Table 2 ). Greater proportions of unvaccinated eligible participants identified as a woman (11.4% vs 1.4%, p = 0.003), or as bisexual (31.4% vs. 9.4%, p < 0.001) or heteroflexible/mostly straight (12.9% vs. 1.4%, p = 0.001). Fewer unvaccinated participants identified as gay (51.4% vs. 85.5%, p < 0.001). We also observed a trend towards a greater proportion of unvaccinated participants having an annual income of <$20,000 (20.0% vs 8.7%, p = 0.035). We also found a significant difference in the time spent with other T/GBM (p < 0.001), whereby the majority (48.6%) of unvaccinated participants spent “little to 25%” and 58.7% of vaccinated spent “75% to most” of their time with other T/GBM. In terms of sexual behaviour and history, lower proportions of unvaccinated eligible participants met vaccine eligibility criteria for having two or more sexual partners (67.1% vs. 84.1%, p < 0.006), or attending venues/locations for sexual contact (28.9% vs 48.6%, p = 0.008). No other statistically significant differences were identified.
Table 2.
Comparison of characteristics of participants identifying as eligible for Mpox vaccine by vaccination status.
| Variable |
Total Eligible (N=222) n/N (%) |
Vaccinated (N=146) n/N (%) |
Not Vaccinated (N=76) n/N (%) |
p-value |
|---|---|---|---|---|
| SOCIO-DEMOGRAPHICS | ||||
| Age (median (IQR)) | 34 (28-41) | 34 (29-41) | 34 (27-42) | 0.928 |
| Race/Ethnicity (collapsed) | 0.679 | |||
| Indigenous | 11/206 (5.3%) |
6/136 (4.4%) |
5/70 (7.1%) |
|
| Other Racialized Minority | 87/206 (42.2%) |
59/136 (43.4%) |
28/70 (40.0%) |
|
| White | 108/206 (52.4%) |
71/136 (52.2%) |
37/70 (52.9%) |
|
| Gender identity (check all that apply) | ||||
| Genderqueer | 14/208 (6.7%) |
10/138 (7.2%) |
4/70 (5.7%) |
0.777 |
| Man | 173/208 (83.2%) |
121/138 (87.7%) |
52/70 (74.3%) |
0.025 |
| Non-Binary | 19/208 (9.1%) |
12/138 (8.7%) |
7/70 (10.0%) |
0.957 |
| Woman | 10/208 (4.8%) |
2/138 (1.4%) |
8/70 (11.4%) |
0.003 |
| Other term/Prefer not to say | 13/208 (6.3%) |
6/138 (4.3%) |
7/70 (10.0%) |
0.188 |
| Gender identity | 0.212 | |||
| Transgender | 19/206 (9.2%) |
10/137 (7.3%) |
9/69 (13.0%) |
|
| Cisgender | 174/206 (84.5%) |
120/137 (87.6%) |
54/69 (78.3%) |
|
| Other/Prefer not to say | 13/206 (6.3%) | 7/137 (5.1%) | 6/69 (8.7%) | |
| Sexual identity (check all that apply) | ||||
| Bi (bisexual) | 35/208 (16.8%) |
13/138 (9.4%) |
22/70 (31.4%) |
<0.001 |
| Gay | 154/208 (74.0%) |
118/138 (85.5%) | 36/70 (51.4%) | <0.001 |
| Heteroflexible (mostly straight) | 11/208 (5.3%) | 2/138 (1.4%) | 9/70 (12.9%) | 0.001 |
| Pansexual | 25/208 (12.0%) | 12/138 (8.7%) | 13/70 (18.6%) | 0.065 |
| Queer | 40/208 (19.2%) |
26/138 (18.8%) |
14/70 (20.0%) |
0.989 |
| Straight (heterosexual) | 1/208 (0.05%) |
1/208 (0.05%) |
0/208 (0.0%) |
--- |
| Other term/prefer not to say | 13/208 (6.3%) |
6/138 (4.3%) |
7/70 (10.0%) |
0.198 |
| Education (University vs. lower) | 137/208 (65.9%) |
96/138 (69.6%) |
41/70 (58.6%) |
0.154 |
| Annual income (< $20,000 vs. higher) | 26/208 (12.5%) |
12/138 (8.7%) |
14/70 (20.0%) |
0.035 |
| Employment (Full-time 30+ hours/week vs. other) | 130/208 (62.5%) |
89/138 (64.5%) |
41/70 (58.6%) |
0.495 |
| Unstable Housing (Homeless or temporarily live with someone else, past year vs. not) | 20/208 (9.6%) |
14/138 (10.1%) |
6/70 (8.6%) |
0.909 |
| Ever diagnosed with HIV (vs. not) | 16/206 (7.8%) |
13/137 (9.5%) |
3/69 (4.3%) |
0.272 |
| Time spent hanging out with Transgender people or gbMSM | <0.001 | |||
| Little to 25% | 64/208 (30.8%) |
30/138 (21.7%) |
34/70 (48.6%) |
|
| 50% | 37/208 (17.8%) |
27/138 (19.6%) |
10/70 (14.3%) |
|
| 75% to most | 107/208 (51.4%) |
81/138 (58.7%) |
26/70 (37.1%) |
|
| SEXUAL BEHAVIOUR | ||||
| Eligibility criteria met for vaccine: (yes vs. no/prefer not to say) | ||||
| Two or more sexual partners | 173/221 (78.3%) |
122/145 (84.1%) |
51/76 (67.1%) |
0.006 |
| Diagnosis of bacterial STI | 48/219 (21.9%) |
31/144 (21.5%) |
17/75 (22.7%) |
0.983 |
| Attended venues/locations for sexual contact | 92/220 (41.8%) |
70/144 (48.6%) |
22/76 (28.9%) |
0.008 |
| Anonymous or casual sex | 182/221 (82.4%) |
123/146 (84.2%) |
59/75 (78.7%) |
0.399 |
| Engage in sex work or planning to as worker or client | 15/220 (6.8%) |
12/145 (8.3%) |
3/75 (4.0%) |
0.363 |
| Types of sex (past 6 mos; check all that apply) | ||||
| Threesomes | 99/204 (48.5%) |
72/135 (53.3%) |
27/69 (39.1%) | 0.076 |
| Group sex (sex between 4 or more people) | 38/204 (18.6%) |
30/135 (22.2%) |
8/69 (11.6%) |
0.098 |
| There is an outbreak of monkeypox in BC (yes vs. no) | 206/222 (92.8%) |
138/146 (94.5%) |
68/76 (89.5%) |
0.269 |
| Most cases of monkeypox have been in men who have sex with men (yes vs. no) | 206/221 (93.2%) |
141/145 (97.2%) |
65/76 (85.5%) |
0.003 |
| Symptoms include blisters or lesions (yes vs. no) | 204/221 (92.3%) |
140/145 (96.6%) |
64/76 (84.2%) |
0.003 |
| Main route of transmission is through close physical contact during sex (yes vs. no) | 199/220 (90.5%) |
131/144 (91.0%) |
68/76 (89.5%) |
0.906 |
| There is a vaccine which provides protection (yes vs. no) | - | - | 67/76 (88.2%) |
- |
| BELIEFS | ||||
| Perceived Susceptibility (I believe I am at risk of monkeypox; strongly agree/agree vs. other responses) | 166/218 (76.1%) |
120/145 (82.8%) |
46/73 (63.0%) |
0.002 |
| Perceived Severity (If I got monkeypox the consequences would be severe; strongly agree/agree vs. other responses) | 116/216 (53.7%) |
76/144 (52.8%) |
40/72 (55.6%) |
0.809 |
| Perceived Benefits (I believe the vaccine is effective; strongly agree/agree vs. other responses) | 179/218 (82.1%) |
122/145 (84.1%) |
57/73 (78.1%) |
0.361 |
| Perceived Safety (I believe the vaccine is safe; strongly agree/agree vs. other responses | 188/216 (87.0%) |
129/144 (89.6%) |
59/72 (81.9%) |
0.174 |
| PSYCHOLOGICAL ANTECEDENTS OF VACCINATION1 |
Mean score (SD) |
Mean score (SD) |
Mean score (SD) |
|
| Confidence (I am completely confident that vaccines are safe) | 6.35 (1.00) | 6.38 (0.91) | 6.29 (1.16) | 0.572 |
| Complacency (Vaccination is unnecessary because vaccine-preventable diseases are not common anymore) | 1.52 (1.24) | 1.52 (1.29) | 1.51 (1.14) | 0.935 |
| Constraints (Everyday stress prevents me from getting vaccinated) | 2.06 (1.66) | 1.82 (1.53) | 2.51 (1.81) | 0.006 |
| Calculation (When I think about getting vaccinated, I weigh benefits and risks to make the best decision possible). | 5.18 (1.85) | 5.18 (1.91) | 5.18 (1.73) | 0.996 |
| Collective Responsibility (When everyone is vaccinated, I don’t have to get vaccinated too). | 6.55 (0.98) | 6.52 (1.00) | 6.61 (0.93) | 0.515 |
| CUES TO ACTION | ||||
| Knows someone who tested positive for MPox (Yes vs. No/Not Sure) | 28/221 (12.7%) |
22/146 (15.1%) |
6/75 (8.0%) |
0.200 |
| Knows someone who has received the vaccine (Yes vs. No/Not Sure) | 172/218 (78.9%) |
139/145 (95.9%) |
33/73 (45.2%) |
<0.001 |
| Saw information promoting the vaccine (past 3 months; Yes vs. No/Not Sure) | 158/218 (72.5%) |
117/145 (80.7%) |
41/73 (56.2%) |
<0.001 |
|
Vaccine recommended by: (past 3 months; Yes vs. No/Not Sure) |
||||
| Friends | 143/212 (67.5%) |
114/141 (80.9%) |
29/71 (40.8%) |
<0.001 |
| Family Members or Relatives | 24/209 (11.5%) |
21/138 (15.2%) |
3/71 (4.2%) |
0.021 |
| Partner or Sexual Partner(s) | 110/211 (52.1%) |
91/140 (65.0%) |
19/71 (26.8%) |
<0.001 |
| Doctor or Nurse | 99/210 (47.1%) |
85/139 (61.2%) |
14/71 (19.7%) |
<0.001 |
| Staff member of a community organization | 67/211 (31.8%) |
56/140 (40.0%) |
11/71 (15.5%) |
<0.001 |
| Someone else | 44/207 (21.3%) |
33/136 (24.3%) |
11/71 (15.5%) |
0.199 |
| PREVIOUS RECEIPT OF VACCINES | ||||
| COVID Vaccine (any) | 206/210 (98.1%) |
138/139 (99.3%) |
68/71 (95.8%) |
0.113 |
| COVID Vaccine (at least one booster) | 194/210 (92.4%) |
131/139 (94.2%) |
63/70 (88.7%) |
0.250 |
| Hepatitis A Vaccine | 173/210 (82.4%) |
115/139 (82.7%) |
58/70 (81.7%) |
1.00 |
For each item, based on score from 1 (lowest; strongly disagree) to 7 (highest; strongly agree); collective responsibility is reverse scored).
While Mpox knowledge was high in both groups, a lower proportion of non-vaccinated eligible participants knew that most cases of Mpox were among MSM (85.5% vs. 97.2%;) and that symptoms of Mpox included blisters or lesions (84.2% vs. 96.6%; p = 0.003). We found few differences between groups related to beliefs about the vaccine. Perceived susceptibility was significantly lower among non-vaccinated eligible participants (63.0% vs 82.8%, p = 0.002). Overall perceived vaccine benefits and safety were high among all eligible participants (82.1% and 87.0% respectively) and did not differ by vaccination status. Similarly, there were few differences in psychological antecedents of vaccination. Although scored lower in relation to other constructs, a greater proportion of non-vaccinated participants had higher scores for constraints (mean score 2.51 (out of 7) vs 1.82, p = 0.006). Mean scores for all eligible participants were highest for the positive antecedents of collective responsibility (6.55), confidence (6.35) and calculation (5.18) with no differences by vaccination status. We did however, find several differences between non-vaccinated and vaccinated eligible participants related to cues to action (i.e., to get vaccinated). Significantly lower proportions of non-vaccinated participants reported knowing someone who has received the vaccine (45.2% vs. 95.9%), seeing information promoting the vaccine (56.2% vs. 80.7%), or being recommended the vaccine by others (by friends (40.8% vs. 80.9%), by partner or sexual partner(s) (26.8% vs 65.0%), by a doctor or nurse (19.7% vs 61.2%) or by a staff member of a community organization (15.5% vs. 40.0%); all p < 0.001).
Finally, of the 76 eligible participants who were not vaccinated, 75.3% (55/73) reported high perceived self-efficacy to get the vaccine. When presented with a list of potential challenges in accessing the vaccine, 38.9% (28/72) reported no challenge, 39.9% (28/72) reported a challenge related to physically accessing vaccination clinics (e.g., distance, convenience, not able to access during work hours), and 22% (16/72) reported challenges related to privacy or stigma (e.g., having vaccine on health record; having to disclose gender, sexual identity or behaviours to access vaccine; embarrassment; concern about being judged).
4. Discussion
We found high acceptability and uptake of the Mpox vaccine among eligible T/GBM clients of an STI clinic five to seven weeks after launching the one first-dose vaccination campaign in BC (with two-thirds of eligible T/GBM participants reporting receiving the first-dose of the vaccine). We found high levels of factors known to be positively associated with vaccination outcomes among gay, bisexual, and other men who have sex with men, including Mpox knowledge, vaccine beliefs (perceived benefits and safety), and psychological antecedents of vaccination (confidence, collective responsibility, and low complacency).[10] Overall, among T/GBM eligible participants there were high levels of reported confidence in the vaccine, perceived benefits of vaccination, and safety, which are important indicators for public health messaging. Our findings of increased constraints reported among eligible and unvaccinated participants indicate that efforts to increase ease of access (i.e., clinic availability) may increase uptake among those eligible for vaccination.
Our findings also confirm the appropriateness of using a low-barrier approach to offering vaccination, as a large majority of vaccinated participants reported meeting eligibility criteria, and a subset of eligible but unvaccinated participants reported privacy and stigma-related challenges accessing the Mpox vaccine (a known barrier to vaccination among 2STGBM).[17], [18] However, when comparing the characteristics of vaccinated and unvaccinated eligible participants we found that vaccine uptake in our sample was patterned along social gradients, consistent with reports of similar patterning for Mpox vaccine acceptability. [6], [7], [8] Specifically, we found lower uptake by eligibile participants who may be more on the margins of the 2STGBM population in the Greater Vancouver area, including eligible participants identifying as a sexual identity other than gay, or who spend less time with other 2STGBM people. These findings reflect challenges in targeting health interventions to 2STGBM, as available venues and promotion channels may preferentially reach gay-identifying men with greater community and social connections. Continuing and expanding efforts to engage diverse groups of 2STGBM in Mpox vaccination is important, using strategies such as outreach in non-traditional settings (e.g., in cruising locations), engaging a wide range of community stakeholders, and diversity in promotional materials for different audiences to increase cues to action across the 2STGBM population. Healthcare providers recommending vaccination to 2STGBM patients during purposeful or opportunistic healthcare encounters is also an important strategy for improving vaccine uptake.
We also found lower perceived susceptibility to Mpox among participants eligible for vaccine but not vaccinated, which may reflect a lower risk profile in this population (i.e., significantly fewer reporting two or more partners, or attending venues/locations for sexual contact). Providers in Mpox vaccination clinics and public health staff following up with new Mpox cases also suggested that for some 2STGBM messaging about who is eligible for vaccine may have unintentionally led some people meeting fewer eligibility criteria to conclude that they were not at sufficient risk to get vaccinated (personal communication, Meena Dawar). As a result, Mpox vaccine eligibility criteria in BC have been revised to focus on criteria that are more widely applicable (e.g., having two or more partners or a partner who does, casual sex / cruising).[19].
We found vaccine acceptability to be high in our sample (89.5% overall) which is consistent with other surveys of T/GBM in Europe prior to widespread use of the Mpox vaccine for pre-exposure prophylaxis. In a United Kingdom cross-sectional survey from June 15–27, 2022 on LGBTQI community social media channels and Grindr, 86% of participants said they would accept the Mpox vaccine, if offered.[6] Acceptability was 82% in a similar European survey on Grindr/Hornet from July 31-August 12, 2022.[7] A lower estimate, 70%, was found among participants surveyed from an existing cohort of MSM and an online app in the Netherlands in July 2022.[8] However, there are fewer reported estimates of vaccine uptake with which to compare our findings, and such comparisons are challenging due to multiple factors including: regional differences in outbreak epidemiology; timing, availability and delivery of vaccine for pre-exposure prophylaxis; eligibility criteria for vaccination. At the time of writing, to our knowledge only one other study has examined vaccine uptake. A United States internet survey of cisgender men reporting sex with another man in the past year during the same time period as our study found 18.6% of participants had received ≥ 1 dose of Mpox vaccine. [20] The higher uptake in our sample of 51.4% among all participants may reflect the BC context (Supplementary Data 1), particularly having a supply of Mpox vaccine sufficient to meet demand among 2STGBM in this urban setting in BC. This U.S. study also found vaccine uptake patterned along sociodemographic gradients, with higher uptake in urban areas and differences by race/ethnicity (higher among Hispanic and lower among Black men),[20] also affirming the importance of equity-focused vaccination programming for 2STGBM populations.
We also do not yet know what thresholds for Mpox vaccine coverage need to be achieved in order to control or eliminate ongoing transmission or decrease the potential for a resurgence of Mpox among 2STGBM. Mathematical models looking at optimal allocation of vaccine suggest prioritizing larger transmission networks, with more initial infections, or a greater reproductive number (i.e., as may be found in larger cities) although the impact may depend on the degree of inter-city mixing.[21] Models have suggested that vaccination programs will be most beneficial when targeted to gay, bisexual and other men who have sex with men with higher sexual activity,[22] including a Belgian cohort model that estimated vaccinating 50% of high-risk men would result in a 95% reduction in the number of Mpox cases.[23] The critical threshold to vaccinate also depends on vaccine effectiveness, the extent of population behaviour change, and extent of other public health measures such as testing and contact tracing. In a US model in a scenario with modest public health response (20% of community cases detected and 25% of cases traced), the critical threshold ranged from 5% to 43% (assuming 100% vaccine efficacy).[24] Our study’s estimate of vaccine uptake may inform further mathematical modeling to understand outbreak dynamics and effect of vaccines in more depth.
We were able to rapidly mobilize an existing cohort of STI clinic clients to gain timely data and evidence to inform ongoing public health efforts, and answer our research questions. Other strengths of our study were being able to assess uptake against eligibility criteria for the vaccine. Furthermore, our survey questions were grounded in health behaviour theory, and drew on an evidence-informed conceptual framework to examine factors associated with vaccine acceptability and uptake.[10] We also recognize several important limitations to our study. First, as a healthcare-receiving sample of STI clinic clients, participants were more likely to be accepting of vaccines/biomedical prevention tools and have higher uptake, as suggested by previous vaccination studies among 2STGBM.[10], [20], [7] Other challenges to generalizability include our sample being largely urban, and having a lower than expected prevalence of participants living with HIV likely due to people with HIV being tested for STI as part of HIV-related care, and therefore not attending STI clinics (7.1% in our sample vs. 14–24% in other estimates among gay, bisexual and other men who have sex with men in Metro Vancouver).[25], [26] Second, participants in our survey were majority White, university educated and with access to healthcare, and as such we may not have detected important group differences in vaccine uptake - a common limitation of vaccine studies among GBM.[10] Third, we recognize our estimates of vaccine uptake and acceptability may be biased by overrepresentation of STI clinic clients who are more concerned about Mpox, or social desirability bias leading to overreporting vaccine uptake and acceptability. Fourth, our survey question about eligibility was based on the specific wording of the vaccine eligibility criteria first used in BC which may have lacked specificity to the populations where Mpox infections were occurring and have been challenging to interpret by individuals. This likely carried through to our data; for example, of the 10 women self-identifying as eligible for vaccine in our survey, all reported sexual minority identities but only four would be classified as transgender women based on their survey responses. The vaccine program’s eligibility criteria were later revised to be more specific, defining the population to whom vaccine was available as Two-Spirit and transgender people and cisgender males who self-identify as belonging to the gay, bisexual and other men who have sex with men community. Fifth, we acknowledge that the need to provide consent to be invited to the survey and low participation rate may have introduced selection bias into our findings; in a previous study in this same clinic, we found that clients consenting to be contacted for research included more homosexual or bisexual-identified persons.[13] Finally, we recognize that our survey was anchored to a specific point in time and as vaccine doses continued to be administered following the survey, we may have underestimated the vaccine uptake subsequently reached in our sample during the fall of 2022. Continuing to monitor vaccine acceptability and uptake in an dynamic outbreak will be important for continuing to inform public health protection and control efforts.
5. Conclusions
In conclusion, we found high vaccine acceptability and uptake among T/GBM clients of an STI clinic in Vancouver, BC following a first-dose Mpox vaccination campaign. As vaccine uptake was patterned on social gradients, our study speaks to the importance of early, intentional, and continued efforts to engage a diverse range of members of 2STGBM communities when delivering targeted vaccination programs, as well as considering barriers related to stigma, privacy and clinie access. This is an area of active effort currently among public health and community partners in BC, particularly with the implementation of a second-dose vaccine campaign starting on October 1, 2022 in order to meet our provincial goal of eliminating local transmission of Mpox. Given the limits on generalizability of our sample, we also welcome further research on Mpox vaccine outcomes outside of urban centres, in more diverse populations, and over time.[27] Finally, while our study has shed important information on vaccine equity in relation to the 2022 outbreak in BC, we recognize that significant global vaccine equity gaps persist for countries where Mpox has long been endemic.[28] Effective prevention and control of Mpox globally requires these gaps to be addressed.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements:
The authors would like to acknowledge the efforts of community and public health organizations and service providers in rapidly mobilizing to deploy Mpox vaccine in BC, and to the BCCDC STI clinic clients who took the time to complete this survey.
Funding:
Funding for this study was provided by the Canadian Institutes of Health Research (Funding reference number VS1-175518), who otherwise had no role in the in the study design, data collection, analysis and interpretation, writing of the article and the and decision to submit the article for publication.
Patient consent
Informed consent was obtained from all participants. The e-mail invitation to the survey contained all the information required for informed consent, with proceeding to the survey considered provision of informed consent.
Contributors
MG led all aspects of this study. TG, AA, HC, TG, TS, MAI, MN, GO contributed to the design of the study, with AA and HC leading data acquisition and analysis. All authors contributed to the review and interpretation of findings, and all authors contributed to drafting the manuscript and have provided approval for this manuscript to be published.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2023.02.075.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
Data availability
The data that has been used is confidential.
REFERENCES
- 1.Monkeypox Outbreak. 2022 https://www.who.int/emergencies/situations/monkeypox-oubreak-2022 [Google Scholar]
- 2.World Health Organization. 2022 Monkeypox Outbreak: Global Trends. https://worldhealthorg.shinyapps.io/mpx_global/.
- 3.Public Health Agency of Canada & Government of Canada. Monkeypox epidemiology update. https://health-infobase.canada.ca/monkeypox/.
- 4.NACI Rapid Response - Interim guidance on the use of Imvamune in the context of monkeypox outbreaks in Canada.
- 5.Garnett G.P. Role of herd immunity in determining the effect of vaccines against sexually transmitted disease. J Infect Dis. 2005;191 doi: 10.1086/425271. [DOI] [PubMed] [Google Scholar]
- 6.Paparini, S. et al. Public understanding, awareness, and response to monkeypox virus outbreak: A cross-sectional survey of the most affected communities in the United Kingdom during the 2022 public health emergency. medRxiv 2022.08.25.22279207 (2022). [DOI] [PubMed]
- 7.Reyes-urueña J., et al. High monkeypox vaccine acceptance among male users of smartphone-based online gay-dating apps in Europe, 30 July to 12 August 2022. Eurosurveillance. 2022;27:1–9. doi: 10.2807/1560-7917.ES.2022.27.42.2200757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang, H., d’Abreu de Paulo, K. J. I., Gültzow, T., Zimmermann, H. M. L. & Jonas, Kai. J. Monkeypox self-diagnosis abilities, determinants of vaccination and self-isolation intention after diagnosis among MSM, the Netherlands, July 2022. Eurosurveillance27, (2022). [DOI] [PMC free article] [PubMed]
- 9.Brodkin E., Gilbert M., Gustafson R., Daly P. ‘If you toke get poked’: A social marketing campaign in response to an outbreak of meningococcal C disease in men who have sex with men in BC. Abstracts: 7th Canadian Immunization Conferece. 2006;December 3 to 6 Canadian Jounal of Infectious Diseases and Medical Microbiology, 2006. [Google Scholar]
- 10.Nadarzynski T., et al. Vaccine acceptability, uptake and completion amongst men who have sex with men: A systematic review, meta-analysis and theoretical framework. Vaccine. 2021;39:3565–3581. doi: 10.1016/j.vaccine.2021.05.013. [DOI] [PubMed] [Google Scholar]
- 11.Rosenstock I.M., Strecher V.J., Becker M.H. Social Learning Theory and the Health Belief Model. Health Educ Behav. 1988;15:175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 12.Betsch C., et al. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One. 2018;13 doi: 10.1371/journal.pone.0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gilbert M., et al. Differences in experiences of barriers to STI testing between clients of the internet-based diagnostic testing service GetCheckedOnline.com and an STI clinic in Vancouver, Canada. Sex Transm Infect. 2019;95:151–156. doi: 10.1136/sextrans-2017-053325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gilbert M., et al. Accessing needed sexual health services during the COVID-19 pandemic in British Columbia, Canada: a survey of sexual health service clients. Sex Transm Infect. 2022;98:360–365. doi: 10.1136/sextrans-2021-055013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harris P.A., et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95 doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.R Core Team. R: A language and environment for statistical computing.
- 17.Rhodes S.D., Hergenrather K.C. Using an integrated approach to understand vaccination behavior among young men who have sex with men: Stages of change, the health belief model, and self-efficacy. J Community Health. 2003;28:347–362. doi: 10.1023/a:1025444629753. [DOI] [PubMed] [Google Scholar]
- 18.Newman P.A., Logie C.H., Doukas N., Asakura K. HPV vaccine acceptability among men: A systematic review and meta-Analysis. Sex Transm Infect. 2013;89:568–574. doi: 10.1136/sextrans-2012-050980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.British Columbia Centre for Disease Control. Interim guidance: Public Health Management of Cases and Contacts Associated with Monkeypox in the Community Setting. (2022).
- 20.Delaney K.P., et al. Strategies Adopted by Gay, Bisexual, and Other Men Who Have Sex with Men to Prevent Monkeypox virus Transmission — United States, August 2022. MMWR Morb Mortal Wkly Rep. 2022;71:1126–1130. doi: 10.15585/mmwr.mm7135e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Knight, J., Tan, D. H. S. & Mishra, S. Maximizing the impact of limited vaccine supply under different epidemic conditions: a two-city monkeypox modelling analysis. medRxiv 2022.08.18.22278949 (2022). [DOI] [PMC free article] [PubMed]
- 22.Brand, A. S. P. C., Cavallaro, M., Hilton, J., Guzman-rincon, L. M. & House, T. The role of vaccination and public awareness in medium-term forecasts of monkeypox incidence in the United Kingdom. (2022). [DOI] [PMC free article] [PubMed]
- 23.Van Dijck C., Hens N., Kenyon C., Tsoumanis A. The roles of unrecognized monkeypox cases, contact isolation and vaccination in determining epidemic size in Belgium. A modelling study medRxiv. 2022;2022.07.28.22278048 doi: 10.1101/2022.07.28.22278048. [DOI] [PubMed] [Google Scholar]
- 24.Chitwood M.H., et al. Testing, Tracing, and Vaccination Targets for Containment of the US Monkeypox Outbreak: A Modeling Study. medRxiv. 2022;2022.08.01.22278199 doi: 10.1101/2022.08.01.22278199. [DOI] [Google Scholar]
- 25.Rich A.J., et al. Estimating the Size of the MSM Population in Metro Vancouver, Canada, Using Multiple Methods and Diverse Data Sources. J Urban Health. 2018;95:188–195. doi: 10.1007/s11524-017-0176-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gustafson P., et al. Impact of statistical adjustment for frequency of venue attendance in a venue-based survey of men who have sex with men. Am J Epidemiol. 2013;177:1157–1164. doi: 10.1093/aje/kws358. [DOI] [PubMed] [Google Scholar]
- 27.Paparini S., et al. Case study research for better evaluations of complex interventions: rationale and challenges. BMC Med. 2020;18:1–6. doi: 10.1186/s12916-020-01777-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nolen S. Treatments and Tests are Unavailable in Much of the World; The New York Times: 2022. Monkeypox Shots. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that has been used is confidential.