Abstract
The relative contribution of the respiratory route to transmission of mpox (formerly known as monkeypox) is unclear. We review the evidence for respiratory transmission of monkeypox virus (MPXV), examining key works from animal models, human outbreaks and case reports, and environmental studies. Laboratory experiments have initiated MPXV infection in animals via respiratory routes. Some animal-to-animal respiratory transmission has been shown in controlled studies, and environmental sampling studies have detected airborne MPXV. Reports from real-life outbreaks demonstrate that transmission is associated with close contact, and although it is difficult to infer the route of MPXV acquisition in individual case reports, so far respiratory transmission has not been specifically implicated. Based on the available evidence, the likelihood of human-to-human MPXV respiratory transmission appears to be low; however, studies should continue to assess this possibility.
Introduction
In 2022, human-to-human clade II monkeypox virus (MPXV) transmission occurred at an accelerated rate, resulting in tens of thousands of cases worldwide in non-endemic countries. Several factors probably contributed to the outbreak, including the virus's initial entry into a global network of sexually active men who have sex with men,1 the waning of herd and individual immunity conferred by smallpox vaccination,2 and increased recognition of and testing for the virus.
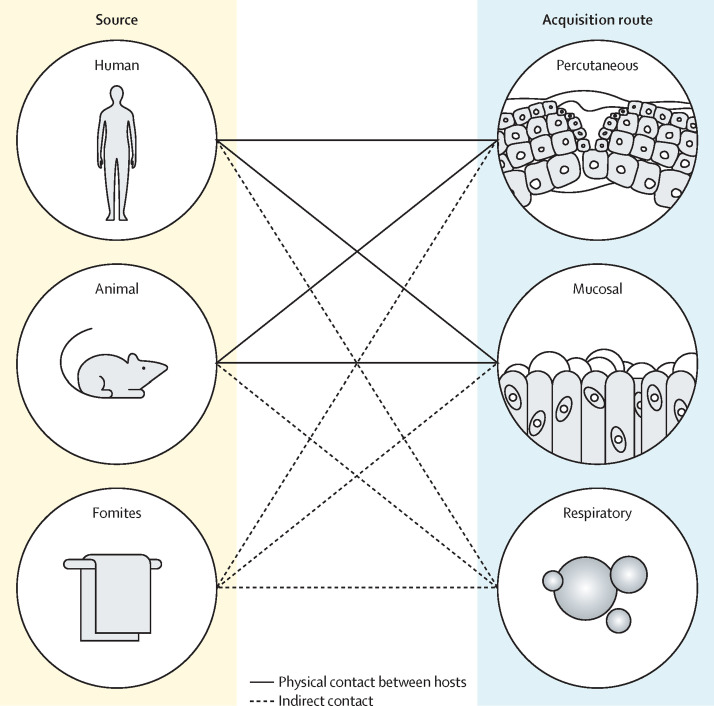
MPXV transmission can arise from many combinations of routes and sources of infection (figure ). Based on its similarities to variola virus (smallpox), historical observations of MPXV, and a small amount of experimental evidence, routes of MPXV acquisition are widely thought to include percutaneous exposure, such as through direct exposure of skin, especially broken skin; direct exposure of mucous membranes, such as those found in the mouth, vagina, and rectum; and inhalation of infectious particles into the respiratory tract.3, 4 Sources of infection include infected humans or animals, or alternatively, contaminated fomites (objects or materials that harbour infectious matter).5 In the ongoing outbreak that began in 2022, sexual contact among cases and the prevalence of anogenital lesions at diagnosis suggest that direct sexual contact is the primary route of acquisition;1 however, the role of inhalation of infectious viral particles in disease transmission remains uncertain and has substantial implications for public health recommendations.
Figure.
Main sources and potential acquisition routes of MPXV that have been documented historically
Infection with MPXV is believed to arise from several combinations of routes of acquisition (percutaneous, mucosal, and respiratory) and sources (humans, animals, and fomites). MPXV=monkeypox virus.
In contrast to respiratory viruses such as SARS-CoV-2 and influenza that preferentially bind specific receptors found in human respiratory tract cells, orthopoxviruses such as MPXV do not bind to one specific receptor type for viral–cell surface attachment (although glycosaminoglycans have been implicated with vaccinia virus strains).6 Instead, for cell entry, orthopoxviruses are engulfed (at the plasma membrane or through macropinocytosis) and subsequently spread from cell to cell via actin tails.6
Respiratory transmission of infectious diseases has often been dichotomised into droplet and airborne transmission. Droplet transmission refers to the spread of pathogens through large particles (ie, droplets) produced during sneezing, coughing, or talking, and deposited onto the mucous membranes of a susceptible host. These large particles typically travel only short distances (ie, <2 m) before settling onto the ground or other surfaces. Airborne transmission refers to the spread of pathogens in very small particles (ie, aerosols) that can also be produced via sneezing, coughing, and talking, and remain suspended in the air for extended periods of time, thus not requiring close contact (<2 m) with an infected individual. Both types of particles can be infectious when they are inhaled or contact a person's mucous membranes. In reality, these types of transmission exist along a continuum, with particles of varying sizes being continually exuded, resulting in the potential for both long-range and short-range transmission for many infections. In the mpox (formerly known as monkeypox) context, lesion-derived particulate matter (eg, pulverised scab material) from non-oral lesions can also be inhaled when suspended in the air. Here, we collectively refer to transmission through the air (whether through droplet sprays or inhalation of aerosols or lesion-derived particulates) as respiratory transmission. Notably, we did not consider infection resulting from direct contact with upper respiratory tract mucosa (eg, during kissing or oral sex) to be respiratory transmission.
In this Personal View, we describe evidence for and against MPXV respiratory transmission available from key works published from 1961 to 2022, including controlled experiments with animal models, human case reports and outbreaks, and environmental studies for both clade I and the currently circulating clade II MPXV.7, 8
Animal models and MPXV respiratory transmission
Studies of clade I and clade II MPXV in prairie dogs and non-human primates have helped shape the current understanding of MPXV transmission. Prairie dogs are a useful animal model in laboratory experiments because they are susceptible to MPXV infection, exhibit a long incubation period, can transmit MPXV, and are the only small animal model that develops the characteristic skin rash seen in human mpox.9 Non-human primates are another valuable animal model because of their genetic proximity to humans, similar disease presentation (ie, characteristic skin rash), and susceptibility to infection with MPXV in the wild.10
Studies in prairie dogs have shown that inoculation via the upper respiratory tract results in experimentally infected animals with the ability to produce infectious secretions (and therefore potentially transmit virus without direct contact) with the recovery of viable virus from oropharyngeal secretions and oral and nasal swabs.3 Additionally, both the upper and lower respiratory tract can be involved in naturally occurring MPXV infection in animals: in a sooty mangabey (Cercocebus atys) infected in the wild in Côte d'Ivoire in 2012, viable clade II MPXV virus was isolated from a throat swab and lung tissue.10
Respiratory transmission was demonstrated with clade I MPXV (but not clade II MPXV) in a prairie dog experimental model in a 2013 study.11 Eight prairie dogs (four challenged with intranasal MPXV and four naive) were housed separately in metal cages that were maintained 4 inches (roughly 10 cm) apart with multiple ventilation holes (1 inch [roughly 2·5 cm] in diameter) cut into walls that faced each other, with directional airflow from the challenged to the naive animals. The animals were unable to touch. When challenged with clade II MPXV, three of four animals developed disease; however, no transmission occurred to the naive animals. When the authors repeated the experiment with clade I MPXV, all four challenged animals developed disease, and transmission occurred to one of four naive prairie dogs.11
Experiments with non-human primates in the 1970s also suggested possible respiratory transmission, leading scientists at the time to believe that this could be an important MPXV transmission pathway. In a 1971 laboratory study, several yellow baboons (Papio cynocephalus) were housed in separate cages in the same room with shared airflow.12 Two animals were inoculated intramuscularly with a high dose of MPXV of West African origin (clade II) and developed clinical illness consistent with mpox. Of six sentinel animals housed (in separate cages) in the same room, two (33%) became ill. The authors postulated that the two infected animals became sick during the third week of exposure. An important limitation of this study is that the distance between cages and the type of barrier between cages are not specified, leaving open the possibility of mucosal or percutaneous transmission (ie, if the animals were able to touch).
Although these studies used small numbers of animal subjects, experimental models with prairie dogs and non-human primates suggest that MPXV respiratory transmission is possible, at least for clade I MPXV. Importantly, however, the artificial approach to inoculation and simulated exposures might not replicate the conditions of human-to-human contact.
Human case reports and outbreaks
Respiratory manifestations of mpox in humans
The involvement of the respiratory tract in human mpox infections is important to consider when examining the possibilities for respiratory transmission. Although the presence of respiratory symptoms does not predict the route of acquisition, respiratory symptoms are likely to enhance the production of infectious respiratory secretions, which could, in turn, promote respiratory transmission.
Historically, case reports of human mpox have included upper or lower respiratory tract symptoms, but these can also be absent. Severe respiratory distress or bronchopneumonia have been noted late in the course of illness with clade I MPXV.13 Oral lesions, in addition to other oropharyngeal signs and symptoms (eg, tonsillar lesions, pharyngitis, odynophagia, and epiglottitis) have been reported both historically13 and during the 2022 clade II outbreak.14, 15 Sore throat was reported in 17–37% of patients in 2022.14, 15, 16, 17 Prior to 2022, cough was documented in approximately half of patients with both clade I and clade II MPXV,18 but in reports from the 2022 outbreak, this symptom, along with dyspnoea and nasal congestion, has been far less common,14, 15, 16, 17 with cough occurring in just 7% of patients in one cross-sectional study.14
Both historical and recent reports also document isolation of MPXV from oral or respiratory anatomical locations. Pharyngeal swabs (n=37) and saliva (n=2) have yielded detectable MPXV via PCR in patients who have concurrent skin lesions.14 Adler and colleagues identified upper respiratory tract MPXV clade II DNA in seven patients described in a case series from the UK (2018–21) in the absence of respiratory symptoms and even after skin lesion resolution. In three patients, upper respiratory tract shedding occurred for longer than 3 weeks.19 Viral DNA was also detected during one patient's relapse of disease that occurred 6 weeks after hospital discharge and 10 weeks after initial symptom onset.19 The association between viral DNA presence and shedding of viable infectious virus from the respiratory tract leading to infection is unknown, since many of these studies did not include cell culture. However, in one study,20 infectious virus was cultivated from some oropharyngeal swabs and measured by a plaque assay.
Although respiratory symptoms seem to be an uncommon manifestation of MPXV in the 2022 outbreak, the presence of viral DNA in the respiratory tract has been documented even in individuals without respiratory symptoms.14 Whether respiratory manifestations of MPXV infection or isolation of MPXV from oral or respiratory secretions in humans have any correlation with the potential for respiratory transmission remains unclear.
Outbreaks in humans
Most of the mpox transmission studies in humans before 2022 were done in African households.5, 21, 22, 23, 24, 25 Close contact primarily within households has been implicated in extended transmission chains ranging from four to eight generations.19, 21, 22, 23, 24, 25 The nature of close contact in household settings might entail various combinations of acquisition routes, with confounding exposures such as caregiving, children's play, bed-sharing, shared eating utensils, and sexual contact.
The 2003 US human outbreak of the clade II strain arising from infected prairie dogs provides another illustration of confounding exposures but also offers examples of activities that did not result in infection. All 47 individuals who developed symptomatic MPXV infections had contact with prairie dogs or fomites contaminated by infected animals (eg, cleaning animal cages or touching animal bedding).26, 27 Although excluding the possibility of animal-to-human respiratory transmission during this outbreak is difficult, simply being near an infected animal (defined by the investigators as within 6 feet [roughly 1·8 m] for >3 h) was not associated with infection.28 Furthermore, no health-care personnel in proximity to the affected patients (<6 feet [roughly 1·8 m]) were infected, even though 81% (46/57) reported not consistently wearing an N95 respirator and 75% (43/57) reported not consistently wearing a surgical mask.29
Data on the re-emergence of clade II MPXV in Nigeria in 2017, using viral genomic analyses, demonstrated instances of human-to-human transmission occurring among four people incarcerated in a prison and in a health-care worker.30, 31 Three of the four incarcerated people who were infected had known contact with at least one other infected person (contact included sharing a prison cell and other unspecified contact). For the remaining individual, no link was disclosed. Without the details of the type of contact between people in the prison and the types of personal protective equipment worn or types of contact by health-care personnel, drawing conclusions about possible routes of exposure during this outbreak remains challenging.
Investigations of MPXV transmission associated with air travel also can provide insights about the risk of respiratory transmission. So far, there have been no cases of transmission on international or domestic flights. Between 2018 and 2021, eight individuals were diagnosed with clade II MPXV after travelling from Nigeria to the UK,19, 32, 33 Singapore,34 Israel,35 and the USA.36, 37 Among these eight cases, four were symptomatic during international flights, and contact investigations were performed for all four (table 1 ). No additional cases were identified in any investigated contacts for ten different trips (flights, and car or train journeys), four of which were flights longer than 8 h in duration. Importantly, masks were worn during the 2021 flights because of requirements related to the COVID-19 pandemic and might have protected against respiratory transmission.37
Table 1.
Transportation routes and duration of travel for symptomatic mpox patients, 2018–21, ordered by origin and date of arrival at destination
| Destination | Transportation type | Estimated trip duration | Estimated contacts investigated | Reference | |
|---|---|---|---|---|---|
| Case 1 (Sept 2, 2018) | |||||
| Abuja, Nigeria | London, UK | Flight | 8 h 55 m | ∼41* | Vaughan et al (2018)32 |
| London, UK | Cornwall, UK | Train | 5 h 20 m | NR | .. |
| Case 2 (Sept 4, 2018) | |||||
| Lagos, Nigeria | Paris, France | Flight | 8 h 20 m | ∼41* | Vaughan et al (2018)32 |
| Paris, France | Manchester, UK (assumed)† | Flight | 1 hr 15m | ∼41* | .. |
| Case 3 (July 8–9, 2021) | |||||
| Lagos, Nigeria | Atlanta, GA, USA | Flight‡ | 13 h 2 m | 144§ | Rao et al (2022)37 |
| Atlanta, GA, USA | Dallas, TX, USA | Flight‡ | 2 h 14 m | 5 | .. |
| Dallas, TX, USA | Dallas, TX, USA | Car | NR | 1 | .. |
| Dallas, TX, USA | Dallas, TX, USA | Car | NR | 1 | .. |
| Case 4 (November, 2021) | |||||
| Lagos, Nigeria | Maryland, USA | Flight‡ | 13 h 55 m | 9 | (Kreuze M, Centers for Disease Control and Prevention, personal communication) |
| Maryland, USA | Maryland, USA | Car | NR | 8 | .. |
No transmission was identified in any of the contact investigations. NR=not reported.
Assumptions: each row has two sets of three seats; people sitting on both sides of the aisle were contacted.
Based on the location of Blackpool Teaching Hospital.
Masks worn on flights.
Those investigated included flight crew, close exposures, and far exposures who could have used the toilets.
Finally, reports from health-care and congregate settings for the 2022 outbreak are becoming available and provide useful case studies for examining the possibility of respiratory transmission in the absence of sexual or close, intimate contact. In endemic areas, health-care personnel are known to be at higher risk for MPXV infection relative to the general population;38 however, in a 2022 investigation in Colorado, USA, none of 313 health-care personnel exposed to patients with mpox became infected, including seven reported to be exposed during aerosol-generating procedures (four of whom did not wear an N95 respirator).39 Additionally, transmission without close, intimate contact has not yet been documented in congregate settings such as shelters, correctional facilities, and schools. After a symptomatic resident with mpox spent 7 days in congregate housing in a prison in Chicago, IL, USA, sharing a dormitory with 57 individuals, no additional cases were identified among a subset of those exposed who were actively monitored for symptoms or consented to serological testing.40 Of ten distinct instances in which a child or adolescent with mpox attended a childcare facility or school while symptomatic, none resulted in secondary cases.41
Clinical and outbreak data show that transmission has primarily occurred during close, prolonged contact. So far, no outbreaks that clearly implicate human-to-human respiratory transmission have been reported in other congregate or residential group settings.
MPXV in the environment
Orthopoxviruses, including MPXV, are stable in the environment, and several studies have assessed the ability of the virus to persist in the air, as well as the role of fomites as a vehicle for transmission. For example, MPXV viral particles were recently found in three of four air samples taken during a bedding change in a health-care setting, including replication-competent virus (Ct value range: 32·7–36·2).42 Air samples from which MPXV was identified were located more than 15 m away and at a height of up to 2 m and were collected over the course of 10 min. In the same study, a high degree of surface contamination of viral DNA was found in a patient room and bathroom, including surfaces unlikely to have been directly touched (eg, the air vent above the door), which could indicate non-contact contamination through droplets or aerosolised viral particles, although viral culture was not attempted for these samples (Ct value range: 25·9–33·6).42 Another investigation conducted continuous air sampling for viral DNA for 4-h sessions in a clinic suite housing patients suspected of having mpox.43 MPXV DNA was detected in six of six sampling sessions (Ct value range: 32·0–38·0) that occurred with confirmed patients with mpox in the room; culture was not attempted. Notably, attending health-care personnel were protected with N95 respirators and patients wore surgical masks, and transmission within the facility did not occur. A laboratory study of suspension of viral particles in the air also demonstrated the persistence of replication-competent viral particles for at least 90 h in a small (10·7 L) rotating chamber.44
Evidence also suggests that MPXV can remain viable on surfaces for long periods, although respiratory transmission under these circumstances has not been definitively proven. A 2021 US environmental sampling study detected culturable virus on household surfaces 15 days after the infected person had left,45 which could pose a potential risk for respiratory transmission through inhalation of viral material resuspended in the air (eg, during handling of contaminated linens). A case report from the UK in 2018 described a health-care worker who was infected while handling the used bedding and clothing of a patient with mpox, despite wearing a disposable apron and gloves.46 No face mask or respirator was worn. Although respiratory exposure (eg, inhalation or direct mucosal inoculation of lesion-derived particulate matter) from a fomite source has been hypothesised, the exact nature of exposure to the bedding was unknown and any of the three acquisition routes (percutaneous, mucosal, or respiratory) was possible.
Key findings and public health implications
In this Personal View, we summarise different types of key evidence to evaluate the contribution of respiratory transmission to the spread of MPXV. The available types of evidence regarding respiratory transmission of MPXV are summarised in table 2 . Laboratory experiments in prairie dogs and non-human primates attempt to isolate the respiratory route of acquisition (by eliminating other possibilities) but are challenging to extrapolate to real-life settings. Respiratory symptoms and the presence of virus in the upper respiratory tract suggest transmission potential by the respiratory route, but these data cannot definitively demonstrate respiratory transmission, nor do they allow assessment of the relative importance of the respiratory route compared with other routes. Environmental sampling studies can show the presence of replication-competent virus in the air or on surfaces, but the presence of virus does not equate to infectivity or person-to-person transmission. Outbreak reports offer insight into the likelihood of transmission under realistic conditions, but often do not have detailed exposure histories.
Table 2.
Summary of possible evidence for respiratory transmission of mpox and study limitations, 1961–2022
| Examples in the scientific literature | Study limitations | |
|---|---|---|
| Animal models | ||
| Experiments showing transmission between separately housed animals with shared airflow | Animals might be infected following laboratory challenge methods that differ from exposures in natural settings; small numbers of animals | |
| Respiratory inoculation with monkeypox virus | Animals might be infected with relatively large viral doses (eg, ∼1 × 104–3·53 × 107 plaque-forming units) not likely to be observed in natural settings; respiratory droplet size produced by nebuliser systems in some studies might not mimic natural systems; small numbers of animals | |
| Identification of virus from saliva or upper respiratory tract, evidence of oral lesions, inflammation of the lungs | Identification of virus on mucosal surfaces does not necessarily indicate that infective respiratory secretions could be expelled; small numbers of animals | |
| Human case reports | ||
| Identification of replication-competent virus from saliva, upper respiratory tract, or evidence of oral lesions | Identification of virus on mucosal surfaces does not necessarily indicate that infective respiratory secretions could be expelled | |
| Human outbreaks | ||
| Observed transmission between people with shared airspace, no direct contact, and no mucosal or percutaneous transmission via fomites (eg, adjacent hospital beds or prison cells) | No evidence to date | Settings where this is possible are often confounded by the possibility of transmission via fomites, which itself could result in mucosal, percutaneous, or inhalational inoculation |
| Environmental studies | ||
| Aerosolisation of contaminated droplets, detection of monkeypox virus on surfaces unlikely to have been touched (eg, air vents on ceilings) | Viability and infectivity of respiratory particles in uncontrolled settings is probably more variable | |
Equally important is what the outbreak data do not show. If respiratory transmission of MPXV between humans were commonplace, we would expect to see many more infections of uncertain origin, in which there is no physical contact with cases. Case investigations involving air travel and congregate settings would be expected to yield secondary cases with greater frequency. Furthermore, we would expect a higher secondary attack rate in households—for MPXV clade I, the secondary attack rate is estimated to be between 0% and 11%.56 These figures contrast with those of other viruses (eg, SARS-CoV-2 and respiratory syncytial virus) for which respiratory transmission is the dominant route of spread: for these viruses, household secondary attack rates range from 19% to 70%.57 From these observations, we conclude that although respiratory transmission of MPXV is possible, it is not the primary mode of spread and is unlikely to be a substantial contributor to person-to-person transmission of the virus in the current mpox outbreak.
Moving forward, outbreak investigations that include detailed documentation of exposure histories could help to elucidate whether respiratory, percutaneous, or mucosal exposures occurred, and whether or not fomites were involved in transmission. Additional data from contact investigations from air travel exposures and congregate settings would also be informative, including documentation of exposures that did not result in secondary cases.
Experimental approaches with animal models could further address questions about the frequency of different acquisition routes, and even help elucidate the probability of airborne spread versus large respiratory droplet spread by repeating experiments at various distances. Studies in prairie dogs examining respiratory transmission were done only at very short distances (eg, 4 inches [roughly 10 cm]),11 and could be repeated at further distances using impermeable barriers (to exclude close contact while also allowing for airflow). The efficiency of fomites as vehicles for various inoculation routes, including the respiratory pathway, could also be addressed. MPXV clade II should be evaluated for both aerosol and surface stability.58
Historically, MPXV has been presumed to be less transmissible than its most famous congener, variola virus (smallpox), which was thought to transmit efficiently between hosts via the respiratory route.4 In recent years, although both clade I and clade II MPXV have proven to be more transmissible than was previously believed,59, 60 accumulating data continue to support a minimal role of respiratory transmission. However, this possibility should continue to be thoroughly and repeatedly examined as phenotypic changes due to viral evolution are a constant threat. While DNA viruses such as MPXV mutate with less frequency than RNA viruses (such as coronaviruses and influenza), a high number and frequency of mutations have been noted in the two dominant strains causing the 2022 outbreak. The phenotypic implications of such mutations are so far unknown.55, 61 Another notable discovery from the current outbreak is the effect of a human enzyme (APOBEC3) that appears to cause mutations in the MPXV genome.61 Poxviruses were not previously thought to be subject to APOBEC3 editing, but recent findings suggest APOBEC3 activity has been important in clade II MPXV evolution.61 The potential emergence of more highly transmissible MPXV variants through this or other mechanisms deserves careful vigilance and will require additional study.
In the absence of more definitive data, public health authorities have recommended broad respiratory transmission reduction strategies, including both source control (containing infectious particles that a person breathes, coughs, or sneezes out) and respiratory protection (filtering out infectious particles in inhaled air), as an adjunct to other protective measures focused on reducing transmission through close contact. Specifically, the UK Health Security Agency and the US Centers for Disease Control and Prevention recommend that people with mpox wear a well-fitting medical mask if close contact with others cannot be avoided, and that contacts of an individual with mpox wear a respirator or well-fitting medical mask when in proximity with infected people for longer than a brief encounter.62, 63 Furthermore, it is also recommended that health-care personnel wear a respirator with N95 or higher-level filters, in addition to a gown, gloves, and eye protection, when entering the rooms or care areas of patients with suspected or confirmed mpox.63, 64
Despite an increase in human-to-human transmission of mpox during the past 40 years, Dr Zdenek Jezek's remarks about a 1988 Democratic Republic of the Congo outbreak could still hold true today: “The absence of illness among neighbours who had no direct face-to-face contact with a [mpox] patient suggests that there is no (or only minimal) risk of airborne transmission.”4 Only time (and meticulous epidemiological investigation) will tell whether or not this observation prevails.
Declaration of interests
We declare no competing interests.
Acknowledgments
Acknowledgments
We thank the current and past members of the Centers for Disease Control and Prevention (CDC) Poxvirus and Rabies Branch and the CDC Multi-national Mpox Response. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
Contributors
AB, AS, and SAJG contributed to conceptualisation, project administration, writing the original draft, and review and editing of the manuscript. CLH, FW, KMA, FSM, and CM contributed to writing the original draft, and review and editing of the manuscript. KC contributed to data curation, and review and editing of the manuscript. MGR and AMM contributed to conceptualisation, and review and editing of the manuscript.
References
- 1.Vivancos R, Anderson C, Blomquist P, et al. Community transmission of monkeypox in the United Kingdom, April to May 2022. Euro Surveill. 2022;27 doi: 10.2807/1560-7917.ES.2022.27.22.2200422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rimoin AW, Mulembakani PM, Johnston SC, et al. Major increase in human monkeypox incidence 30 years after smallpox vaccination campaigns cease in the Democratic Republic of Congo. Proc Natl Acad Sci USA. 2010;107:16262–16267. doi: 10.1073/pnas.1005769107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hutson CL, Olson VA, Carroll DS, et al. A prairie dog animal model of systemic orthopoxvirus disease using West African and Congo Basin strains of monkeypox virus. J Gen Virol. 2009;90:323–333. doi: 10.1099/vir.0.005108-0. [DOI] [PubMed] [Google Scholar]
- 4.Jezek Z, Grab B, Szczeniowski MV, Paluku KM, Mutombo M. Human monkeypox: secondary attack rates. Bull World Health Organ. 1988;66:465–470. [PMC free article] [PubMed] [Google Scholar]
- 5.Learned LA, Reynolds MG, Wassa DW, et al. Extended interhuman transmission of monkeypox in a hospital community in the Republic of the Congo, 2003. Am J Trop Med Hyg. 2005;73:428–434. [PubMed] [Google Scholar]
- 6.Cudmore S, Cossart P, Griffiths G, et al. Actin-based motility of vaccinia virus. Nature. 1995;378:636–638. doi: 10.1038/378636a0. [DOI] [PubMed] [Google Scholar]
- 7.Likos AM, Sammons SA, Olson VA, et al. A tale of two clades: monkeypox viruses. J Gen Virol. 2005;86:2661–2672. doi: 10.1099/vir.0.81215-0. [DOI] [PubMed] [Google Scholar]
- 8.Chen N, Li G, Liszewski MK, et al. Virulence differences between monkeypox virus isolates from West Africa and the Congo basin. Virology. 2005;340:46–63. doi: 10.1016/j.virol.2005.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hutson CL, Carroll DS, Gallardo-Romero N, et al. Monkeypox disease transmission in an experimental setting: prairie dog animal model. PLoS One. 2011;6 doi: 10.1371/journal.pone.0028295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Radonic A, Metzger S, Dabrowski PW, et al. Fatal monkeypox in wild-living sooty mangabey, Côte d'Ivoire, 2012. Emerg Infect Dis. 2014;20:1009–1011. doi: 10.3201/eid2006.131329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hutson CL, Gallardo-Romero N, Carroll DS, et al. Transmissibility of the monkeypox virus clades via respiratory transmission: investigation using the prairie dog-monkeypox virus challenge system. PLoS One. 2013;8 doi: 10.1371/journal.pone.0055488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heberling RL, Kalter SS. Induction, course, and transmissibility of monkeypox in the baboon (Papio cynocephalus) J Infect Dis. 1971;124:33–38. doi: 10.1093/infdis/124.1.33. [DOI] [PubMed] [Google Scholar]
- 13.McCollum AM, Damon IK. Human monkeypox. Clin Infect Dis. 2014;58:260–267. doi: 10.1093/cid/cit703. [DOI] [PubMed] [Google Scholar]
- 14.Angelo KM, Smith T, Camprubi-Ferrer D, et al. Epidemiological and clinical characteristics of patients with monkeypox in the GeoSentinel Network: a cross-sectional study. Lancet Infect Dis. 2022;23:196–206. doi: 10.1016/S1473-3099(22)00651-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thornhill JP, Barkati S, Walmsley S, et al. Monkeypox virus infection in humans across 16 countries - April-June 2022. N Engl J Med. 2022;387:679–691. doi: 10.1056/NEJMoa2207323. [DOI] [PubMed] [Google Scholar]
- 16.Patel A, Bilinska J, Tam JCH, et al. Clinical features and novel presentations of human monkeypox in a central London centre during the 2022 outbreak: descriptive case series. BMJ. 2022;378 doi: 10.1136/bmj-2022-072410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tarin-Vicente EJ, Alemany A, Agud-Dios M, et al. Clinical presentation and virological assessment of confirmed human monkeypox virus cases in Spain: a prospective observational cohort study. Lancet. 2022;400:661–669. doi: 10.1016/S0140-6736(22)01436-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Benites-Zapata VA, Ulloque-Badaracco JR, Alarcon-Braga EA, et al. Clinical features, hospitalisation and deaths associated with monkeypox: a systematic review and meta-analysis. Ann Clin Microbiol Antimicrob. 2022;21:36. doi: 10.1186/s12941-022-00527-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adler H, Gould S, Hine P, et al. Clinical features and management of human monkeypox: a retrospective observational study in the UK. Lancet Infect Dis. 2022;22:1153–1162. doi: 10.1016/S1473-3099(22)00228-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Paran N, Yahalom-Ronen Y, Shifman O, et al. Monkeypox DNA levels correlate with virus infectivity in clinical samples, Israel, 2022. Euro Surveill. 2022;27 doi: 10.2807/1560-7917.ES.2022.27.35.2200636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Breman JG, Kalisa R, Steniowski MV, Zanotto E, Gromyko AI, Arita I. Human monkeypox, 1970-79. Bull World Health Organ. 1980;58:165–182. [PMC free article] [PubMed] [Google Scholar]
- 22.Doshi RH, Guagliardo SAJ, Doty JB, et al. Epidemiologic and ecologic investigations of monkeypox, Likouala Department, Republic of the Congo, 2017. Emerg Infect Dis. 2019;25:281–289. doi: 10.3201/eid2502.181222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hutin YJ, Williams RJ, Malfait P, et al. Outbreak of human monkeypox, Democratic Republic of Congo, 1996 to 1997. Emerg Infect Dis. 2001;7:434–438. doi: 10.3201/eid0703.010311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jezek Z, Arita I, Mutombo M, Dunn C, Nakano JH, Szczeniowski M. Four generations of probable person-to-person transmission of human monkeypox. Am J Epidemiol. 1986;123:1004–1012. doi: 10.1093/oxfordjournals.aje.a114328. [DOI] [PubMed] [Google Scholar]
- 25.Mukinda VB, Mwema G, Kilundu M, Heymann DL, Khan AS, Esposito JJ. Re-emergence of human monkeypox in Zaire in 1996. Monkeypox Epidemiologic Working Group. Lancet. 1997;349:1449–1450. doi: 10.1016/S0140-6736(05)63725-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention Update: multistate outbreak of monkeypox–Illinois, Indiana, Kansas, Missouri, Ohio, and Wisconsin, 2003. MMWR Morb Mortal Wkly Rep. 2003;52:642–646. [PubMed] [Google Scholar]
- 27.Sejvar JJ, Chowdary Y, Schomogyi M, et al. Human monkeypox infection: a family cluster in the midwestern United States. J Infect Dis. 2004;190:1833–1840. doi: 10.1086/425039. [DOI] [PubMed] [Google Scholar]
- 28.Reynolds MG, Davidson WB, Curns AT, et al. Spectrum of infection and risk factors for human monkeypox, United States, 2003. Emerg Infect Dis. 2007;13:1332–1339. doi: 10.3201/eid1309.070175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fleischauer AT, Kile JC, Davidson M, et al. Evaluation of human-to-human transmission of monkeypox from infected patients to health care workers. Clin Infect Dis. 2005;40:689–694. doi: 10.1086/427805. [DOI] [PubMed] [Google Scholar]
- 30.Ogoina D, Izibewule JH, Ogunleye A, et al. The 2017 human monkeypox outbreak in Nigeria–report of outbreak experience and response in the Niger Delta University Teaching Hospital, Bayelsa State, Nigeria. PLoS One. 2019;14 doi: 10.1371/journal.pone.0214229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yinka-Ogunleye A, Aruna O, Dalhat M, et al. Outbreak of human monkeypox in Nigeria in 2017–18: a clinical and epidemiological report. Lancet Infect Dis. 2019;19:872–879. doi: 10.1016/S1473-3099(19)30294-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vaughan A, Aarons E, Astbury J, et al. Two cases of monkeypox imported to the United Kingdom, September 2018. Euro Surveill. 2018;23 doi: 10.2807/1560-7917.ES.2018.23.38.1800509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hobson G, Adamson J, Adler H, et al. Family cluster of three cases of monkeypox imported from Nigeria to the United Kingdom, May 2021. Euro Surveill. 2021;26 doi: 10.2807/1560-7917.ES.2021.26.32.2100745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ng OT, Lee V, Marimuthu K, et al. A case of imported monkeypox in Singapore. Lancet Infect Dis. 2019;19 doi: 10.1016/S1473-3099(19)30537-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Erez N, Achdout H, Milrot E, et al. Diagnosis of imported monkeypox, Israel, 2018. Emerg Infect Dis. 2019;25:980–983. doi: 10.3201/eid2505.190076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Minhaj FS, Rao AK, McCollum AM. Imported monkeypox from international traveler, Maryland, USA, 2021. Emerg Infect Dis. 2022;28 doi: 10.3201/eid2808.220726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rao AK, Schulte J, Chen TH, et al. Monkeypox in a traveler returning from Nigeria – Dallas, Texas, July 2021. MMWR Morb Mortal Wkly Rep. 2022;71:509–516. doi: 10.15585/mmwr.mm7114a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Petersen BW, Kabamba J, McCollum AM, et al. Vaccinating against monkeypox in the Democratic Republic of the Congo. Antiviral Res. 2019;162:171–177. doi: 10.1016/j.antiviral.2018.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marshall KE, Barton M, Nichols J, et al. Health care personnel exposures to subsequently laboratory-confirmed monkeypox patients – Colorado, 2022. MMWR Morb Mortal Wkly Rep. 2022;71:1216–1219. doi: 10.15585/mmwr.mm7138e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hagan LM, Beeson A, Hughes S, et al. Monkeypox case investigation – Cook County Jail, Chicago, Illinois, July–August 2022. MMWR Morb Mortal Wkly Rep. 2022;71:1271–1277. doi: 10.15585/mmwr.mm7140e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hennessee I, Shelus V, McArdle CE, et al. Epidemiologic and clinical features of children and adolescents aged <18 years with monkeypox — United States, May 17–September 24, 2022. MMWR Morb Mortal Wkly Rep. 2022;71:1407–1411. doi: 10.15585/mmwr.mm7144a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gould S, Atkinson B, Onianwa O, et al. Air and surface sampling for monkeypox virus in a UK hospital: an observational study. Lancet Microbe. 2022;3:e904–e911. doi: 10.1016/S2666-5247(22)00257-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mellon G, Rubenstein E, Antoine M, et al. Air detection of monkeypox virus in a dedicated outpatient clinic room for monkeypox infection diagnosis. J Infect. 2022 doi: 10.1016/j.jinf.2022.12.025. published online Dec 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Verreault D, Killeen SZ, Redmann RK, Roy CJ. Susceptibility of monkeypox virus aerosol suspensions in a rotating chamber. J Virol Methods. 2013;187:333–337. doi: 10.1016/j.jviromet.2012.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Morgan CN, Whitehill F, Doty JB, et al. Environmental persistence of monkeypox virus on surfaces in household of person with travel-associated infection, Dallas, Texas, USA, 2021. Emerg Infect Dis. 2022;28:1982–1989. doi: 10.3201/eid2810.221047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vaughan A, Aarons E, Astbury J, et al. Human-to-human transmission of monkeypox virus, United Kingdom, October 2018. Emerg Infect Dis. 2020;26:782–785. doi: 10.3201/eid2604.191164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Saijo M, Ami Y, Suzaki Y, et al. Virulence and pathophysiology of the Congo basin and West African strains of monkeypox virus in non-human primates. J Gen Virol. 2009;90:2266–2271. doi: 10.1099/vir.0.010207-0. [DOI] [PubMed] [Google Scholar]
- 48.Stittelaar KJ, Neyts J, Naesens L, et al. Antiviral treatment is more effective than smallpox vaccination upon lethal monkeypox virus infection. Nature. 2006;439:745–748. doi: 10.1038/nature04295. [DOI] [PubMed] [Google Scholar]
- 49.Stittelaar KJ, van Amerongen G, Kondova I, et al. Modified vaccinia virus Ankara protects macaques against respiratory challenge with monkeypox virus. J Virol. 2005;79:7845–7851. doi: 10.1128/JVI.79.12.7845-7851.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Estep RD, Messaoudi I, O'Connor MA, et al. Deletion of the monkeypox virus inhibitor of complement enzymes locus impacts the adaptive immune response to monkeypox virus in a nonhuman primate model of infection. J Virol. 2011;85:9527–9542. doi: 10.1128/JVI.00199-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Goff AJ, Chapman J, Foster C, et al. A novel respiratory model of infection with monkeypox virus in cynomolgus macaques. J Virol. 2011;85:4898–4909. doi: 10.1128/JVI.02525-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dyall J, Johnson RF, Chen DY, et al. Evaluation of monkeypox disease progression by molecular imaging. J Infect Dis. 2011;204:1902–1911. doi: 10.1093/infdis/jir663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hahon N, McGavran MH. Air-borne infectivity of the variola-vaccinia group of poxviruses for the cynomolgus monkey, Macaca irus. J Infect Dis. 1961;109:294–298. doi: 10.1093/infdis/109.3.294. [DOI] [PubMed] [Google Scholar]
- 54.Nalca A, Livingston VA, Garza NL, et al. Experimental infection of cynomolgus macaques (Macaca fascicularis) with aerosolized monkeypox virus. PLoS One. 2010;5 doi: 10.1371/journal.pone.0012880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Isidro J, Borges V, Pinto M, et al. Phylogenomic characterization and signs of microevolution in the 2022 multi-country outbreak of monkeypox virus. Nat Med. 2022;28:1569–1572. doi: 10.1038/s41591-022-01907-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Beer EM, Rao VB. A systematic review of the epidemiology of human monkeypox outbreaks and implications for outbreak strategy. PLoS Negl Trop Dis. 2019;13 doi: 10.1371/journal.pntd.0007791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Leung NHL. Transmissibility and transmission of respiratory viruses. Nat Rev Microbiol. 2021;19:528–545. doi: 10.1038/s41579-021-00535-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Charniga K, McCollum AM, Hughes CM, et al. American Society of Tropical Medicine and Hygiene; Oct 30–Nov 3, 2022. Updating reproduction number estimates for monkeypox in the Democratic Republic of Congo using surveillance data. (abstr 1810). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Centers for Disease Control and Prevention Technical report 3: multi-national mpox outbreak, United States, 2022. Jan 6, 2023. https://www.cdc.gov/poxvirus/monkeypox/cases-data/technical-report/report-3.html
- 61.Gigante CM, Korber B, Seabolt MH, et al. Multiple lineages of monkeypox virus detected in the United States, 2021–2022. Science. 2022;378:560–565. doi: 10.1126/science.add4153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Centers for Disease Control and Prevention Hand hygiene, source control, and personal protective equipment. Aug 11, 2022. https://www.cdc.gov/poxvirus/monkeypox/clinicians/infection-control-home.html#hand-hygiene
- 63.UK Health Security Agency Principles for monkeypox control in the UK: 4 nations consensus statement. Nov 3, 2022. https://www.gov.uk/government/publications/principles-for-monkeypox-control-in-the-uk-4-nations-consensus-statement/principles-for-monkeypox-control-in-the-uk-4-nations-consensus-statement
- 64.Centers for Disease Control and Prevention Infection prevention and control of monkeypox in healthcare settings. Oct 31, 2022. https://www.cdc.gov/poxvirus/monkeypox/clinicians/infection-control-healthcare.html