Abstract
Objective
To investigate the effectiveness of tele-counseling for the mental health of staff working in hospitals and reference clinics during the COVID-19 outbreak.
Methods
In the first stage of the study, using a convenience sampling strategy, 313 staff members working at Iran’s hospitals and COVID-19 clinics answered a Hospital Anxiety and Depression Scale and the Short Health Anxiety Inventory online. In a second stage, 95 staff members who were willing to participate in the intervention were randomly assigned to the intervention (n = 51) or control (n = 44) groups. The intervention consisted of seven intensive tele-counseling sessions.
Results
In the first stage, the percentages of anxiety and depression related to coronavirus were 79.2% and 82.1% and the mean health anxiety score was 17.42. In the intervention phase, anxiety related to coronavirus and to perceived risk of illness (likelihood of illness) were significantly lower in the intervention group in comparison with the control group (p = 0.001). Depression related to coronavirus and anxiety related to the negative consequences of infection were non-significantly reduced in the intervention group compared to the control group (p = 0.08 and 0.12; respectively).
Conclusion
Continuous monitoring of the negative psychological impacts on medical staff of outbreaks as well as implementation of appropriate interventions to respond to them should be emphasized in order to improve staff mental health.
Clinical trial registration: Iranian Registry of Clinical Trials, IRCT20170611034452N11.
Keywords: Coronavirus, tele-counseling, staff, hospitals, clinics, anxiety, depression, health anxiety
Introduction
Scientific background and explanation of rationale
Occupational health and mental health have significant impacts on each other. During epidemics, health care providers are continually exposed to the factors associated with the risk of developing mental disorders such as stress, anxiety, and depression. Being infected or fear of infection have been significantly associated with absenteeism, leaving the workplace, negative attitudes, and decreased efficiency and performance of medical staff.1 Infections and occupational injuries can lead to more severe forms of distress response in epidemic conditions.2,3
In pandemics, especially in the case of newly emerging epidemics in which treatment and safety protocols are yet to be properly investigated, a large number of patients are hospitalized and the medical team is subjected to a heavy burden imposed by workload, anxiety, and fear related to the concern of being infected.4 Unknown infections with unknown transmission routes, rapid global prevalence, and relatively high mortality can affect health care staff more than members of other organizations. These conditions may have a potentially deleterious impact on physical and mental health, ability to manage crises, and performance in patient care delivery.5 In this scenario, mood disorders, insomnia, perceived negative emotions, and post-traumatic stress disorder are among the problems that can affect the quality of life of staff.6
The novel beta-coronavirus, associated with a series of respiratory system symptoms and later named SARS-CoV-2, emerged in Wuhan, China, in December 2019 and spread rapidly to other countries and, in spite of interventions, this virus continues to infect populations all over the world.7,8 The increased number of confirmed or suspected cases, heavy workload, lack of personal protective equipment, excessive media coverage, lack of specific medications, and feelings of insufficient support all increase the psychological burden on medical staff.9 Moreover, feelings of vulnerability, loss of control, concerns about personal health and transmitting the virus to family members and others, occupational change and fear of isolation, rapid human-to-human transmission of the virus, and the high mortality rate of the infection all increase staff’s awareness of the risk they are taking.10 Furthermore, factors such as age, gender, marital status, and the type of hospital and service department are associated with the severity of fear, anxiety, sadness, anger, and sleep disorder symptoms in hospital staff.11
Lack of social support, awareness, adaptability, and calming strategies increases the emergence of negative psychological outcomes.12 The feeling of occupational pressure and stress in the coronavirus crisis necessitates intervention to improve mental health by teaching management and coping strategies.13 Advising this group to maintain safe interactions and providing social support will help reduce the psychological burden of occupational exposure.14
To address the psychological needs of medical professions, an intervention program involving identification of stressors and promotion of emotion regulation and problem solving skills can reduce anxiety.15 For instance, mindfulness-based interventions try to improve mental health by reducing the overall stress a person experiences.16 Furthermore, these interventions increase awareness, enhance coping strategies, alleviate the negative effects of epidemics,17 and moderate perceived stress and depression.18 Psychological methods for monitoring thoughts in the face of critical situations can relieve symptoms of mood disorders, by creating new beliefs to curb cognition errors and behavioral mistakes.19 During the coronavirus epidemic, when social distancing is unavoidable, online systems for providing mental health care services are extremely important.20
Burdened by heavy workloads and exhaustion as well as anxiety and depression, the medical staff in Iran suffer from high rates of infection, mortality, and morbidity from COVID-19 infection.21 To date, health care providers in many countries have not received any training to maintain their mental health in optimum condition.22 So far, no studies have been published on providing staff with tele-counseling for coping with the distress and tension of the COVID-19 pandemic in order to reduce its negative consequences.
Specific objectives
The aim of this study was to investigate the effectiveness of tele-counseling for improving the mental health of staff in hospitals and COVID-19 clinics in Iran.
Methods
Trial design
This study is a randomized controlled trial with one intervention group and one control group, conducted from March 10 to March 30, 2020. All health care providers in private and state hospitals and COVID-19 clinics in the southern half of Iran were invited to participate in this study using a convenience sampling method.
The invitation to participate was distributed in several ways. Firstly, a letter was sent from the vice president of Kerman University of Medical Sciences to the vice chancellors of health and curative affairs. Requesting them to encourage their staff to fill out the online questionnaires. Secondly, an invitation letter containing the link was shared with the research team’s professional and social networks and personal connections and snowball sampling was employed to invite health care providers as well.
In the second phase, medical staff who indicated their willingness to participate in the intervention on the questionnaire in the previous stage were contacted and invited to participate. Then they were randomly allocated by the study’s statistics consultant using a random number table (allocation ratio: 1/1) to the intervention group (n = 51) or the control group (n = 44). Those assessing outcomes were blinded to the study.
Eligibility criteria for participants and settings and locations
No limitations on age, specialty, place of work, or years of work experience were used to restrict participation in this study. All of the staff working in hospitals and COVID-19 clinics were eligible to participate in the first and second stages. The exclusion criteria were as follows: (a) history of severe physical and psychiatric disorder preventing the participant from active participation in the sessions, (b) participation in other psychological interventions that could influence anxiety, depression, and health anxiety, and (c) absence from more than two sessions.
Outcome measurements
The primary outcome of this study was the frequency of anxiety and depression related to coronavirus and health anxiety (anxiety in two domains caused by the perceived risk of illness as well as associated negative consequences of infection). The secondary outcome was the effect of tele-counseling on the levels of depression and anxiety related to the coronavirus pandemic as well as two domains of heath anxiety.
Ethical considerations
The study was approved by the medical ethics committee at Kerman University of Medical Sciences (IR.KMU.REC.1398.737) and registered with the Iranian Registry of Clinical Trials (IRCT20170611034452N11). The study was also conducted in accordance with the Declaration of Helsinki. Participants were told that they were able to withdraw from participation at any point of time, no reason required. All data were recorded in a manner that protected the anonymity of the participants. The online questionnaire began with a general description of the study and the questionnaire included a button with which the participant could indicate that they provided their informed consent. The investigator’s contact information was given at the end of the online questionnaire, in case participants had any questions about the study. In addition, staff who were willing to take part in the second stage informed the researcher. Control group members could request to participate in similar sessions to those provided to the intervention group after the index intervention had been completed.
Measurements
Demographics
The information on the sociodemographic data collection form was selected based on the relevant literature as well as the researchers’ experience. The findings are presented in Table 1.
Table 1. Demographic and clinical characteristics of subjects in the two study groups.
| Variable | Intervention | Control | p-value |
|---|---|---|---|
| Age | |||
| < 30 | 37 (72.5.9) | 28 (63.6) | 0.239 |
| ≥ 30 | 14 (27.5) | 16 (36.4) | |
| Gender | |||
| Male | 44 (86.3) | 36 (81.8) | 0.553 |
| Female | 7 (13.7) | 8 (18.2) | |
| Working in coronavirus patients’ wards | |||
| No | 34 (66.7) | 35 (79.5) | 0.160 |
| Yes | 17 (33.3) | 9 (20.5) | |
| Being in contact with coronavirus patients | |||
| No | 37 (72.5) | 31 (70.5) | 0.821 |
| Yes | 14 (27.5) | 13 (29.5) | |
| Being in contact with patients suspected of having coronavirus | |||
| No | 19 (37.3) | 16 (36.4) | 0.928 |
| Yes | 32 (62.7) | 28 (63.6) | |
| Having any symptom of coronavirus at present | |||
| No | 47 (92.2) | 35 (79.5) | 0.075 |
| Yes | 4 (7.8) | 9 (20.5) | |
| Living with an elderly person (> 65 y) | |||
| No | 43 (84.3) | 38 (86.4) | 0.779 |
| Yes | 8 (15.7) | 6 (13.6) | |
| Suffering from a chronic disease | |||
| No | 51 (100) | 42 (95.5) | 0.124 |
| Yes | 0 (0.0) | 2 (4.5) | |
| Suffering from a documented psychiatric disorder | |||
| No | 45 (88.2) | 40 (90.9) | 0.672 |
| Yes | 6 (11.8) | 4 (9.1) |
Data presented as n (%).
The Hospital Anxiety and Depression Scale (HADS)
The HADS was developed by Zigmond and Snaith in 1983 and is a self-report tool used to measure both anxiety and depression. The tool comprises 14 items on two subscales, seven related to anxiety (HADS-A) and seven related to depression (HADS-D).22 Each item is answered on a 4-point Likert scale (scores ranging from 0-3) and the total score of each subscale ranges from 0 to 21. The cutoff score for both anxiety and depression is 7.23 The tool has been validated in different languages and cultures. The Persian version of HADS, translated by Montazeri et al., was used in this study. Montazeri et al. reported that the HADS scale significantly discriminated between anxiety and depression. The results for convergent validity showed a significant negative correlation between the Cancer Quality of Life Questionnaire (EORTC QLQ-C30) and the HADS. HADS has been validated in different fields such as in cancer,23 infertility,24 and epilepsy25 in the Iranian population. It is sensitive to mood changes during the course of therapy in response to psychotherapeutic and psychopharmacological intervention.26 The health care staff were requested to answer all the questions specifically in relation to “the effects of coronavirus”, in order to assess anxiety and depression specific to this epidemic.
Short Health Anxiety Inventory (SHAI)
The SHAI is an 18-item self-report tool developed by Salkovskis et al., in 2002 to assess health anxiety along a four-point Likert scale (0 to 3). Total scores range from 0 to 54; with higher scores indicating greater symptomology. The first 14 items are related to mental concern and frequent encounters with health issues (likelihood of illness domain). The remaining 4 items (the negative consequences domain) deal with people’s attitudes towards how awful it would be if they developed a serious illness.27 Nargesi et al. assessed the validity of the Persian version of the SHAI in a sample of university students, reporting a Cronbach’s alpha of 75%.28
Sample size calculation
In the first stage of the study, the sample size calculation formula for cross-sectional studies was used to calculate the minimum sample size necessary for measuring the prevalence of anxiety, depression, and health anxiety among the staff of hospitals and COVID-19 clinics. Considering α = 0.05; d = 0.06 and P = 0.5029; the sample size was calculated at 267 people. Accounting for a 15% probability of drop-outs and incomplete questionnaires, the final sample size was calculated as 308 people.
In the second stage, to calculate the minimum sample size for the intervention group (those taking part in tele-counseling sessions), the two-point comparison formula was used based on a similar study conducted in China in 2019.30 The sample size calculated for each group was 8 people. In order to increase the study’s power, accounting for possible drop-outs during the intervention by performing parametric probability distribution tests, at least 30 samples were required for each group.
Psychological intervention
Aim of counseling
To manage anxiety and depression related to the COVID-19 outbreak and the resulting health anxiety of medical workers, the intervention implemented in this study was designed to provide information regarding workers’ safety; to be supportive and mindfulness-based; to clarify workers’ cognitive errors regarding the epidemic; to facilitate behavioral modification; and to improve workers’ mental health level.
Intervention design
The psychological intervention implemented in this study is in line with recommendations made by Zhang et al. for responding to the COVID-19 epidemic.31 The content of the seven sessions was chosen according to standard cognitive-behavioral and mindfulness-based techniques.
Counseling method
Medical workers who were allocated to the intervention group were divided into 21 WhatsApp groups. Counseling was implemented through voice or video calls, text chats, and video clips shared on WhatsApp, in seven sessions on seven consecutive days Depending on the number of questions and participants’ experience, the duration of audio and video exchange in each session varied from a minimum of 45 minutes up to 90 minutes. Control group members were able to request to participate in similar sessions after the index intervention had been completed.
Counselors
The intervention was delivered by 21 trained counselors who were “Counseling in Midwifery” master’s students trained by the lead researcher, who is an associate professor in guidance and counseling, based on the study protocol.
Study protocol
Session 1: Information regarding safety of medical staff and implementation of a healthy lifestyle in the recent outbreak via a psychoeducational approach; dysfunctional beliefs related to coronavirus-induced stress; relaxation techniques; introduction to mindfulness; “conscious eating” technique; and homework.
Session 2: Defining mindfulness and its benefits in the recent outbreak; mindful breathing techniques and meditation; personal borders and boundaries; systematic desensitization for anxiety starting from this session and continued in all subsequent sessions; and homework.
Session 3: Information regarding consequences of stress and anxiety via psychoeducational approach; cognitive errors of medical staff in the recent outbreak; overcoming occupational fatigue during epidemic workload; aerobic exercises to increase breathing capacity (helpful if infected in the future); and homework.
Session 4: Defining the automatic mind pilot and coping skills; meditation; mindful breathing; and homework.
Session 5: Re-discussing cognitive errors about worries and fears in epidemics; improving mindful intimacy and love; meditation; and homework.
Session 6: Discussion about accepting conditions and commitment in the recent outbreak; organizational mindfulness; body scan; and homework
Session 7: Talking about (pleasant and unpleasant) life events; related emotions and point of view toward them; self-care; describing how life is like the game of snakes and ladders; mountain meditation; reviewing and summarizing.
Statistical analysis
Descriptive statistics were reported as frequency, percentage, and mean ± SD. The chi-square test was used to compare demographic variables between intervention group and control group, in view of their homogeneity. The paired t-test was used to compare anxiety and depression scores for each group measured in the initial screening phase with the same parameters at the end of the study. The independent t-test was used to compare the anxiety and depression changes (before-after) between the intervention and control groups. Data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 22; and the significance level adopted was 0.05.
Results
This study is a randomized controlled trial with one intervention group and one control group conducted from March 10 to March 30, 2020. In the first stage, 313 staff members filled out the questionnaires in an online survey. Following Montazeri et al.,23 a score of 7 was adopted as the cutoff score for both anxiety and depression. The percentages of anxiety and depression related to coronavirus among 313 staff in the first stage were 79.2% and 82.1%; respectively. The mean health anxiety score was 17.42 and mean scores for the two subscales, anxiety of likelihood of illness and its negative consequences, were 13.7 and 3.45, respectively.
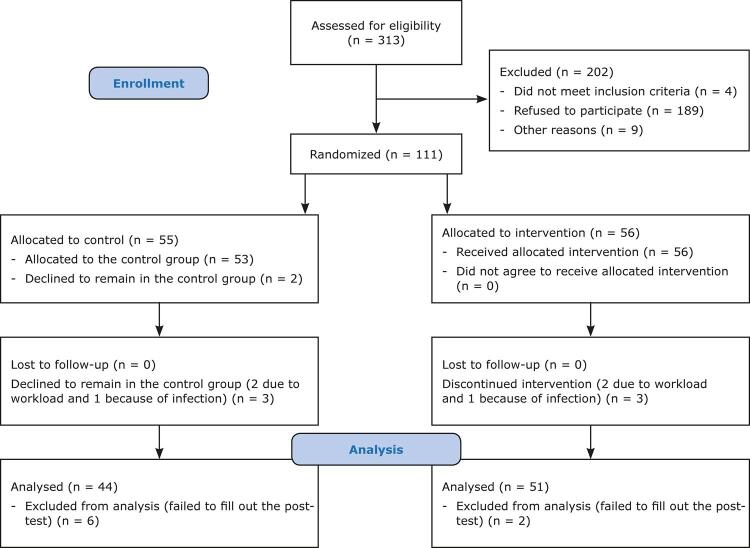
For the second stage, 202 phase one participants were excluded because they did not meet eligibility criteria for inclusion (n = 4) or refused to participate in the intervention (n = 189), or for other reasons (n = 9). 111 staff were randomly divided into the intervention (n = 51) and control (n = 44) groups (Figure 1). Table 1 shows demographic data, which were homogenous at baseline in two groups. Table 2 shows the results for comparisons of depression and anxiety related to coronavirus, anxiety of likelihood of illness, and anxiety of its negative consequences within and between the control and intervention groups.
Figure 1. Flow diagram illustrating sample selection.
Table 2. Comparisons within and between control and intervention groups of depression and anxiety related to coronavirus, anxiety of likelihood of illness, and anxiety of negative consequences.
| Variable | Before Mean ± SD | After Mean ± SD | p* (effect size; mean difference; 95%CI) | p†(effect size; mean difference; 95%CI) | Difference (before – after) Mean ± SD | p‡(effect size; mean difference; 95%CI) |
|---|---|---|---|---|---|---|
| Anxiety related to coronavirus | ||||||
| Intervention | 10.17±2.29 | 8.58±1.99 | 0.06 (1.89; 0.91; -0.04-1.84) | < 0.001 (5.06; 1.58; 0.95-2.21) | 1.58±2.23 | 0.001 (3.41; 1.52; 0.63-2.4) |
| Control | 9.27± 2.33 | 9.2±2.22 | 0.82 (0.21; 0.06; -0.56-0.69) | 0.06±2.07 | ||
| Depression related to coronavirus | ||||||
| Intervention | 10.27±2.08 | 9.05±2.07 | 0.36 (0.92; 0.41; -0.47-1.29) | 0.002 (3.24; 1.21; 0.46-1.96) | 1.21±2.67 | 0.08 (1.76; 0.87; -0.11-1.87) |
| Control | 9.86±2.24 | 9.52±2.33 | 0.27 (1.1; 0.34; -0.28-0.96) | 0.34±2.05 | ||
| Anxiety of likelihood of illness | ||||||
| Intervention | 15.27±5.325.32 | 10.66±5.39 | 0.41 (0.82; 0.98; -1.37-3.33) | < 0.001 (5.35; 4.67; 2.87-6.33) | 4.60±6.10 | 0.001 (3.43; 3.60; 1.52-5.69) |
| Control | 14.29±6.21 | 13.29±6.55 | 0.068 (1.87; 1; -0.07-2.07) | 1.00±3.54 | ||
| Anxiety of negative consequences | ||||||
| Intervention | 4.09±2.6 | 2.62±3.21 | 0.09 (1.67; 0.93; -0.18-2.06) | 0.01 (2.55; 1.47; 0.31-2.62) | 1.47±4.11 | 0.12 (1.56; 1.06; -0.28-2.41) |
| Control | 3.15±2.86 | 2.75±2.76 | 0.18 (1.36; 0.41; -0.19-1.01) | 0.40±1.99 | ||
95%CI = 95% confidence interval.
* p-value for comparison between the control and intervention groups at baseline.
† p-value for comparison between values before and after intervention, within each group separately;
‡ p-value for comparison of mean difference (before – after) between the control and intervention groups;
Before the counseling sessions, there were no significant differences in mean scores between two groups for anxiety (p = 0.82) or depression related to coronavirus (p = 0.27), anxiety of likelihood of illness (p = 0.06), or anxiety of negative consequences (p = 0.18). However, after the counseling sessions, mean scores for all the abovementioned variables had significantly decreased in the intervention group (p < 0.01); After the intervention, anxiety related to coronavirus and likelihood of illness were significantly lower in the intervention group than they were in the control group (p = 0.001 and p = 0.001, respectively). Depression related to coronavirus and anxiety of negative consequences decreased non-significantly after the counseling sessions in the intervention group in comparison with the control group (p = 0.08 and p = 0.12, respectively).
Discussion
For the first stage of the study, in the first months of the COVID-19 pandemic, a web-based cross-sectional survey of Iranian medical staff who work in high-risk situations was conducted with the modified HADS and SHAI.32 The results indicated a very high prevalence of anxiety and depression related to coronavirus. The COVID-19 pandemic compromised the psychological health and emotional state of medical staff who have direct contact with infected patients.33 This is similar to previous pandemic outbreaks, in that a high incidence of psychopathological responses was detected among medical staff.13,34-36 Taking care of infected patients makes them afraid of being infected themselves and of transmitting the disease to their family, friends, and colleagues.37,38
Using SHAI to measure cognitive factors associated with hypochondriasis,39 this study revealed that the mean values of the total health anxiety score and its two domain scores (the anxiety of likelihood of illness and anxiety of negative consequences) were higher than they were in some other non-clinical samples.39-42 It seems this high level of health anxiety was related to the vulnerability of the members of the sample, who worked in close contact with a new emerging and very highly contagious disease with high mortality and morbidity rates. Individuals in different jobs may experience different levels of health anxiety, but those who are at the core of the crisis are affected more.13,21,43
Fatal virus pandemics weaken health systems and disrupt plans for protecting the mental health of medical workers and patients.44 How to best respond to such challenges during outbreaks is unknown.45 Unfortunately, most of the time, the mental health of the staff is ignored in these situations.9,46 The lower the level of mindfulness is, the worse staff wellbeing will be.47,48
Improving health care staff’s ability to regulate emotions and enhancing effective coping strategies increase the chances of winning the battle against the pandemic.11,49 In view of the recommendations on social distancing as well as the crowded and compressed working shifts of medical personnel during the COVID-19 epidemic, attending face-to-face counseling sessions is very inconvenient for medical staff. Therefore, tele-counseling is a better option in this situation20,33 and was planned and delivered for the participants in the second stage of this study.
After the counseling sessions, both the level of anxiety related to coronavirus and the level of anxiety related to likelihood of illness were significantly decreased. The psychological intervention delivered in this study was in the line with the recommendations made by Zhang et al. for responding to the COVID-19 epidemic.31 The core components of counseling content in this study were cognitive-behavioral and mindfulness-based techniques as well as emotional support that aimed to produce better mental states and coping styles.50 Cognitive-behavioral therapy is the most researched and widely recommended treatment for alleviating health anxiety.51,52
Overall, there is evidence for the efficacy of specifically designed psychological interventions in conditions of crisis.51,53 Even a brief mind-body skill training course was associated with improvements of depression and anxiety.52 Mindfulness may serve as a protective factor that alleviates or eliminates the negative effects of perceived stress.16 Symptoms of high levels of depression and anxiety of negative consequences were not significantly decreased in this study. This can be attributed to some factors. Firstly, tele-counseling seems to be less effective than face-to-face sessions.54 Secondly, the goal of holding intensive sessions in this study was to implement an urgent intervention to control the high incidence of depression and anxiety among staff, to maintain their mental health and clinical performance. However, they did not have enough time to do their homework, which was related to the pressure of high workloads.
Limitations: The use of online systems for data collection and intervention may have caused bias in the randomization. Conducting the study with staff who participated voluntarily may reduce the generalizability of the results.
Conclusion
It is suggested that hospital managers focus on psychological support for their staff by providing training and counseling services to enhance their coping strategies. Governments should provide psychiatric services for addressing stress and other negative psychological effects of pandemics. Continuous surveillance and monitoring of the psychological status of medical staff both before and during outbreaks should be emphasized.
Acknowledgements
This research was supported in part by the Deputy of Research, Kerman University of Medical Sciences (grant No. 98001242).
We would like to thank the following masters candidates from the Counseling in Midwifery major for helping us finalize the project: Alieh Zarbaf, Elahe Bahador, Fatemeh Hassanshahi, Omolbanin Heydari, Maryam Dehghanipour, Zahra Ramazanian Bafghi, Laleh Tajadiny, Sanaz Atef, Mohadese Yazdani, Fahimeh Baghbani, Fatemeh Esmaeili, Hediye Barkhordari, Zahra Teimouri, Zahra Pakdel, Zahra kashfi, Rezvan Khaleghi, Omolbanin Lotfi, Masoumeh Nasrollahi, Maryam Gholami, Setareh Yousefi, and Zeinab Moslemi Zadeh.
References
- 1.1. Tran TT, Nguyen NB, Luong MA, Bui TH, Phan TD, Ngo TH, et al. Stress, anxiety and depression in clinical nurses in Vietnam: a cross-sectional survey and cluster analysis. Int J Ment Health Syst. 2019;13:3. [DOI] [PMC free article] [PubMed]; Tran TT, Nguyen NB, Luong MA, Bui TH, Phan TD, Ngo TH, et al. Stress, anxiety and depression in clinical nurses in Vietnam: a cross-sectional survey and cluster analysis. 3Int J Ment Health Syst. 2019;13 doi: 10.1186/s13033-018-0257-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.2. Stone PW, Clarke SP, Cimiotti J, Correa-de-Araujo R. Nurses’ working conditions: implications for infectious disease. Emerg Infect Dis. 2004;10:1984-9. [DOI] [PMC free article] [PubMed]; Stone PW, Clarke SP, Cimiotti J, Correa-de-Araujo R. Nurses’ working conditions: implications for infectious disease. Emerg Infect Dis. 2004;10:1984–1989. doi: 10.3201/eid1011.040253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.3. De Boer JC, Lok A, van’t Verlaat E, Duivenvoorden HJ, Bakker AB, Smit BJ. Work-related critical incidents in hospital-based health care providers and the risk of post-traumatic stress symptoms, anxiety, and depression: a meta-analysis. Soc Sci Med. 2011;73:316-26. [DOI] [PMC free article] [PubMed]; De Boer JC, Lok A, van’t Verlaat E, Duivenvoorden HJ, Bakker AB, Smit BJ. Work-related critical incidents in hospital-based health care providers and the risk of post-traumatic stress symptoms, anxiety, and depression: a meta-analysis. Soc Sci Med. 2011;73:316–326. doi: 10.1016/j.socscimed.2011.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.4. Chen R, Chou KR, Huang YJ, Wang TS, Liu SY, Ho LY. Effects of a SARS prevention programme in Taiwan on nursing staff’s anxiety, depression and sleep quality: A longitudinal survey. Int J Nurs Stud Adv. 2006;43:215-25. [DOI] [PMC free article] [PubMed]; Chen R, Chou KR, Huang YJ, Wang TS, Liu SY, Ho LY. Effects of a SARS prevention programme in Taiwan on nursing staff’s anxiety, depression and sleep quality: A longitudinal survey. Int J Nurs Stud Adv. 2006;43:215–225. doi: 10.1016/j.ijnurstu.2005.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.5. Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B, Evans S, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12:1924-32. [DOI] [PMC free article] [PubMed]; Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B, Evans S, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12:1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.6. Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54:302-11. [DOI] [PMC free article] [PubMed]; Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54:302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.7. Singhal T. A review of corona virus disease-2019 (COVID-19). Indian J Pediatr. 2020;87:281-6. [DOI] [PMC free article] [PubMed]; Singhal T. A review of corona virus disease-2019 (COVID-19) Indian J Pediatr. 2020;87:281–286. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.8. Lupia T, Scabini S, Pinna SM, Di Perri G, De Rosa FG, Corcione S. 2019-novel coronavirus outbreak: A new challenge. J Glob Antimicrob Resist. 2020;21:22-7. [DOI] [PMC free article] [PubMed]; Lupia T, Scabini S, Pinna SM, Di Perri G, De Rosa FG, Corcione S. 2019-novel coronavirus outbreak: A new challenge. J Glob Antimicrob Resist. 2020;21:22–27. doi: 10.1016/j.jgar.2020.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.9. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. [DOI] [PMC free article] [PubMed]; Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.10. Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7:300-2. [DOI] [PMC free article] [PubMed]; Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7:300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.11. Huang L, Xu F, Liu H. Emotional responses and coping strategies of nurses and nursing college students during COVID-19 outbreak. medRxiv. 2020;15:e0237303. [Epub ahead of print]. doi: 10.1101/2020.03.05.20031898. [DOI] [PMC free article] [PubMed]; Huang L, Xu F, Liu H. Emotional responses and coping strategies of nurses and nursing college students during COVID-19 outbreak. medRxiv. 2020;15:e0237303. doi: 10.1101/2020.03.05.20031898. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.12. Naushad VA, Bierens JJ, Nishan KP, Firjeeth CP, Mohammad OH, Maliyakkal AM, et al. A systematic review of the impact of disaster on the mental health of medical responders. Prehosp Disaster Med. 2019;34:632-43. [DOI] [PubMed]; Naushad VA, Bierens JJ, Nishan KP, Firjeeth CP, Mohammad OH, Maliyakkal AM, et al. A systematic review of the impact of disaster on the mental health of medical responders. Prehosp Disaster Med. 2019;34:632–643. doi: 10.1017/S1049023X19004874. [DOI] [PubMed] [Google Scholar]
- 13.13. Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. [Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19]. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38:192-5. [DOI] [PubMed]; Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38:192–195. doi: 10.3760/cma.j.cn121094-20200219-00063. [DOI] [PubMed] [Google Scholar]
- 14.14. World Health Organization (WHO). Mental health and psychosocial considerations during the COVID-19 outbreak [Internet]. 2020 Mar 18 [cited 2021 Mar 12]. www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf; World Health Organization. WHO [cited 2021 Mar 12];Mental health and psychosocial considerations during the COVID-19 outbreak. 2020 Mar 18; www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf Internet.
- 15.15. Brunero S, Cowan D, Fairbrother G. Reducing emotional distress in nurses using cognitive behavioral therapy: a preliminary program evaluation. Jpn J Nurs Sci. 2008;5:109-15.; Brunero S, Cowan D, Fairbrother G. Reducing emotional distress in nurses using cognitive behavioral therapy: a preliminary program evaluation. Jpn J Nurs Sci. 2008;5:109–115. [Google Scholar]
- 16.16. Lu F, Xu Y, Yu Y, Li P, Wu T, Wang T, et al. Moderating effect of mindfulness on the relationships between perceived stress and mental health outcomes among Chinese intensive care nurses. Front Psychiatry. 2019;10:260. [DOI] [PMC free article] [PubMed]; Lu F, Xu Y, Yu Y, Li P, Wu T, Wang T, et al. Moderating effect of mindfulness on the relationships between perceived stress and mental health outcomes among Chinese intensive care nurses. 260Front Psychiatry. 2019;10 doi: 10.3389/fpsyt.2019.00260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.17. Mackenzie CS, Poulin PA, Seidman-Carlson R. A brief mindfulness-based stress reduction intervention for nurses and nurse aides. Appl Nurs Res. 2006;19:105-9. [DOI] [PubMed]; Mackenzie CS, Poulin PA, Seidman-Carlson R. A brief mindfulness-based stress reduction intervention for nurses and nurse aides. Appl Nurs Res. 2006;19:105–109. doi: 10.1016/j.apnr.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 18.18. Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822-48. [DOI] [PubMed]; Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 19.19. Sampson M, Melnyk BM, Hoying J. Intervention effects of the MINDBODYSTRONG cognitive behavioral skills building program on newly licensed registered nurses’ mental health, healthy lifestyle behaviors, and job satisfaction. J Nurs Adm. 2019;49:487-95. [DOI] [PubMed]; Sampson M, Melnyk BM, Hoying J. Intervention effects of the MINDBODYSTRONG cognitive behavioral skills building program on newly licensed registered nurses’ mental health, healthy lifestyle behaviors, and job satisfaction. J Nurs Adm. 2019;49:487–495. doi: 10.1097/NNA.0000000000000792. [DOI] [PubMed] [Google Scholar]
- 20.20. Liu S, Yang L, Zhang C, Xiang YT, Liu Z, Hu S, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:17-8. [DOI] [PMC free article] [PubMed]; Liu S, Yang L, Zhang C, Xiang YT, Liu Z, Hu S, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:17–18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.21. Nemati M, Ebrahimi B, Nemati F. Assessment of Iranian nurses’ knowledge and anxiety toward COVID-19 during the current outbreak in Iran. Arch Clin Infect Dis. 2020;15:e102848.; Nemati M, Ebrahimi B, Nemati F. Assessment of Iranian nurses’ knowledge and anxiety toward COVID-19 during the current outbreak in Iran. Arch Clin Infect Dis. 2020;15:e102848 [Google Scholar]
- 22.22. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361-70. [DOI] [PubMed]; Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 23.23. Montazeri A, Vahdaninia M, Ebrahimi M, Jarvandi S. The Hospital Anxiety and Depression Scale (HADS): translation and validation study of the Iranian version. Health Qual Life Outcomes. 2003;1:14. [DOI] [PMC free article] [PubMed]; Montazeri A, Vahdaninia M, Ebrahimi M, Jarvandi S. The Hospital Anxiety and Depression Scale (HADS): translation and validation study of the Iranian version. 14Health Qual Life Outcomes. 2003;1 doi: 10.1186/1477-7525-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.24. Amini P, Maroufizadeh S, Samani RO. Evaluating the factor structure, item analyses, and internal consistency of hospital anxiety and depression scale in Iranian infertile patients. Int J Reprod Biomed. 2017;15:287-96. [PMC free article] [PubMed]; Amini P, Maroufizadeh S, Samani RO. Evaluating the factor structure, item analyses, and internal consistency of hospital anxiety and depression scale in Iranian infertile patients. Int J Reprod Biomed. 2017;15:287–296. [PMC free article] [PubMed] [Google Scholar]
- 25.25. Evans SJ, Bassis CM, Hein R, Assari S, Flowers SA, Kelly MB, et al. The gut microbiome composition associates with bipolar disorder and illness severity. Psychiatry Res. 2017;87:23-9. [DOI] [PMC free article] [PubMed]; Evans SJ, Bassis CM, Hein R, Assari S, Flowers SA, Kelly MB, et al. The gut microbiome composition associates with bipolar disorder and illness severity. Psychiatry Res. 2017;87:23–29. doi: 10.1016/j.jpsychires.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.26. Herrmann C. International experiences with the Hospital Anxiety and Depression Scale-a review of validation data and clinical results. Psychiatry Res. 1997;42:17-41. [DOI] [PubMed]; Herrmann C. International experiences with the Hospital Anxiety and Depression Scale-a review of validation data and clinical results. Psychiatry Res. 1997;42:17–41. doi: 10.1016/s0022-3999(96)00216-4. [DOI] [PubMed] [Google Scholar]
- 27.27. Bati AH, Mandiracioglu A, Govsa F, Çam O. Health anxiety and cyberchondria among Ege University health science students. Nurse Educ Today. 2018;71:169-73. [DOI] [PubMed]; Bati AH, Mandiracioglu A, Govsa F, Çam O. Health anxiety and cyberchondria among Ege University health science students. Nurse Educ Today. 2018;71:169–173. doi: 10.1016/j.nedt.2018.09.029. [DOI] [PubMed] [Google Scholar]
- 28.28. Nargesi F, Izadi F, Kariminejad K, Rezaii SA.The investigation of the reliability and validity of Persian version of Health anxiety questionnaire in students of Lorestan University of Medical Sciences. J Educ Meas. 2017;7:147-60.; Nargesi F, Izadi F, Kariminejad K, Rezaii SA. The investigation of the reliability and validity of Persian version of Health anxiety questionnaire in students of Lorestan University of Medical Sciences. J Educ Meas. 2017;7:147–160. [Google Scholar]
- 29.29. Lwanga SK, Lemeshow S, Hosmer DW. Adequacy of sample size in health studies: Chichester: Wiley; 1990.; Lwanga SK, Lemeshow S, Hosmer DW. Adequacy of sample size in health studies. Chichester: Wiley; 1990. [Google Scholar]
- 30.30. Hwang WJ, Jo HH. Evaluation of the effectiveness of mobile app-based stress-management program: a randomized controlled trial. Int J Environ Res Public Health. 2019;16:4270. [DOI] [PMC free article] [PubMed]; Hwang WJ, Jo HH. Evaluation of the effectiveness of mobile app-based stress-management program: a randomized controlled trial. 4270Int J Environ Res Public Health. 2019;16 doi: 10.3390/ijerph16214270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.31. Zhang J, Wu W, Zhao X, Zhang W. Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: a model of West China Hospital. Precis Clin Med. 2020 Feb 18: pbaa006. Published online 2020 Feb 18. doi: 10.1093/pcmedi/pbaa006. [DOI] [PMC free article] [PubMed]; Zhang J, Wu W, Zhao X, Zhang W. Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: a model of West China Hospital. Precis Clin Med. 2020 Feb 18; doi: 10.1093/pcmedi/pbaa006.. pbaa006. Published online 2020 Feb 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.32. Bocéréan C, Dupret E. A validation study of the Hospital Anxiety and Depression Scale (HADS) in a large sample of French employees. BMC Psychiatry. 2014;14:354. [DOI] [PMC free article] [PubMed]; Bocéréan C, Dupret E. A validation study of the Hospital Anxiety and Depression Scale (HADS) in a large sample of French employees. 354BMC Psychiatry. 2014;14 doi: 10.1186/s12888-014-0354-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.33. Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:15-6. [DOI] [PMC free article] [PubMed]; Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:15–16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.34. de Medeiros Carvalho PM, Moreira MM, de Oliveira MN, Landim JM, Rolim Neto ML. The psychiatric impact of the novel coronavirus outbreak. Psychiatry Res. 2020;286:112902. [DOI] [PMC free article] [PubMed]; de Medeiros Carvalho PM, Moreira MM, de Oliveira MN, Landim JM, Rolim ML., Neto The psychiatric impact of the novel coronavirus outbreak. 112902Psychiatry Res. 2020;286 doi: 10.1016/j.psychres.2020.112902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.35. Rolim Neto ML, Almeida HG, Esmeraldo JD, Nobre CB, Pinheiro WR, de Oliveira CR, et al. When health professionals look death in the eye: the mental health of professionals who deal daily with the 2019 coronavirus outbreak. Psychiatry Res. 2020;288:112972. [DOI] [PMC free article] [PubMed]; Rolim ML, Neto, Almeida HG, Esmeraldo JD, Nobre CB, Pinheiro WR, de Oliveira CR, et al. When health professionals look death in the eye: the mental health of professionals who deal daily with the 2019 coronavirus outbreak. 112972Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.36. Joob B, Wiwanitkit V. Medical personnel, COVID-19 and emotional impact. Psychiatry Res. 2020;288:112952. [DOI] [PMC free article] [PubMed]; Joob B, Wiwanitkit V. Medical personnel, COVID-19 and emotional impact. 112952Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.37. Maunder R, Hunter J, Vincent L, Bennett J, Peladeau N, Leszcz M, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ.2003;168:1245-51. [PMC free article] [PubMed]; Maunder R, Hunter J, Vincent L, Bennett J, Peladeau N, Leszcz M, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168:1245–1251. [PMC free article] [PubMed] [Google Scholar]
- 38.38. Musarezaie N, Samouei R, Shahrzadi L, Ashrafi-Rizi H. Prediction of health information-seeking behavior components based on health anxiety among users of public libraries. J Educ Health Promot. 2019;8:227. [DOI] [PMC free article] [PubMed]; Musarezaie N, Samouei R, Shahrzadi L, Ashrafi-Rizi H. Prediction of health information-seeking behavior components based on health anxiety among users of public libraries. 227J Educ Health Promot. 2019;8 doi: 10.4103/jehp.jehp_262_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.39. Abramowitz JS, Deacon BJ, Valentiner DP. The short health anxiety inventory: psychometric properties and construct validity in a non-clinical sample. Cognit Ther Res. 2007;31:871-83. [DOI] [PMC free article] [PubMed]; Abramowitz JS, Deacon BJ, Valentiner DP. The short health anxiety inventory: psychometric properties and construct validity in a non-clinical sample. Cognit Ther Res. 2007;31:871–883. doi: 10.1007/s10608-006-9058-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.40. Kocjan J. Short Health Anxiety Inventory (SHAI)-Polish version: evaluation of psychometric properties and factor structure. Arch Gen Psychiatry. 2016;3:68-78.; Kocjan J. Short Health Anxiety Inventory (SHAI)-Polish version: evaluation of psychometric properties and factor structure. Arch Gen Psychiatry. 2016;3:68–78. [Google Scholar]
- 41.41. Jungmann SM, Witthöft M. Health anxiety, cyberchondria, and coping in the current COVID-19 pandemic: which factors are related to coronavirus anxiety? J Anxiety Disord. 2020;73:102239. [DOI] [PMC free article] [PubMed]; Jungmann SM, Witthöft M. Health anxiety, cyberchondria, and coping in the current COVID-19 pandemic: which factors are related to coronavirus anxiety? 102239J Anxiety Disord. 2020;73 doi: 10.1016/j.janxdis.2020.102239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.42. Bajcar B, Babiak J. Self-esteem and cyberchondria: the mediation effects of health anxiety and obsessive–compulsive symptoms in a community sample. Curr Psychol. 2019; [Epub ahead of print]. doi.org/10.1007/s12144-019-00216-x; Bajcar B, Babiak J. Self-esteem and cyberchondria: the mediation effects of health anxiety and obsessive–compulsive symptoms in a community sample. Curr Psychol. 2019 doi: 10.1007/s12144-019-00216-x. Epub ahead of print. [DOI] [Google Scholar]
- 43.43. Zarghami M. Psychiatric aspects of coronavirus (2019-nCoV) infection. Iran J Psychiatry Behav Sci. 2020;14:e102957.; Zarghami M. Psychiatric aspects of coronavirus (2019-nCoV) infection. Iran J Psychiatry Behav Sci. 2020;14:e102957 [Google Scholar]
- 44.44. Kamara S, Walder A, Duncan J, Kabbedijk A, Hughes P, Muana A. Mental health care during the Ebola virus disease outbreak in Sierra Leone. Bull World Health Organ. 2017;95:842-7. [DOI] [PMC free article] [PubMed]; Kamara S, Walder A, Duncan J, Kabbedijk A, Hughes P, Muana A. Mental health care during the Ebola virus disease outbreak in Sierra Leone. Bull World Health Organ. 2017;95:842–847. doi: 10.2471/BLT.16.190470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.45. Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228-9. [DOI] [PMC free article] [PubMed]; Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.46. Adams JG, Walls RM. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020;323:1439-40. [DOI] [PubMed]; Adams JG, Walls RM. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020;323:1439–1440. doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 47.47. Kexian L, Tingting Y, Qu S. Relationships between sleep quality, mindfulness and work-family conflict in Chinese nurses: a cross-sectional study. Appl Nurs Res. 2020;55:151250. [DOI] [PubMed]; Kexian L, Tingting Y, Qu S. Relationships between sleep quality, mindfulness and work-family conflict in Chinese nurses: a cross-sectional study. 151250Appl Nurs Res. 2020;55 doi: 10.1016/j.apnr.2020.151250. [DOI] [PubMed] [Google Scholar]
- 48.48. Dearholt S. Improving nurse well-being through a mindfulness-based education strategy [dissertation]. Minneapolis: Walden University; 2019.; Dearholt S. Improving nurse well-being through a mindfulness-based education strategy. Minneapolis: Walden University; 2019. dissertation. [Google Scholar]
- 49.49. Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288:112936. [DOI] [PMC free article] [PubMed]; Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. 112936Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.50. Shen X, Zhu X, Wu Y, Zhou Y, Yang L, Wang Y, et al. Effects of a psychological intervention programme on mental stress, coping style and immune function in percutaneous coronary intervention patients. PloS One. 2018;13:e0187745. [DOI] [PMC free article] [PubMed]; Shen X, Zhu X, Wu Y, Zhou Y, Yang L, Wang Y, et al. Effects of a psychological intervention programme on mental stress, coping style and immune function in percutaneous coronary intervention patients. PloS One. 2018;13:e0187745. doi: 10.1371/journal.pone.0187745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.51. Jiang X, Deng L, Zhu Y, Ji H, Tao L, Liu L, et al. Psychological crisis intervention during the outbreak period of new coronavirus pneumonia from experience in Shanghai. Psychiatry Res. 2020;286:112903. [DOI] [PMC free article] [PubMed]; Jiang X, Deng L, Zhu Y, Ji H, Tao L, Liu L, et al. Psychological crisis intervention during the outbreak period of new coronavirus pneumonia from experience in Shanghai. 112903Psychiatry Res. 2020;286 doi: 10.1016/j.psychres.2020.112903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.52. Nguyen MC, Gabbe SG, Kemper KJ, Mahan JD, Cheavens JS, Moffatt-Bruce SD. Training on mind-body skills: Feasibility and effects on physician mindfulness, compassion, and associated effects on stress, burnout, and clinical outcomes. Posit Psychol. 2020;15:194-207.; Nguyen MC, Gabbe SG, Kemper KJ, Mahan JD, Cheavens JS, Moffatt-Bruce SD. Training on mind-body skills: Feasibility and effects on physician mindfulness, compassion, and associated effects on stress, burnout, and clinical outcomes. Posit Psychol. 2020;15:194–207. [Google Scholar]
- 53.53. Saravanan C, Kingston R. A randomized control study of psychological intervention to reduce anxiety, amotivation and psychological distress among medical students. J Res Med Sci. 2014;19:391. [PMC free article] [PubMed]; Saravanan C, Kingston R. A randomized control study of psychological intervention to reduce anxiety, amotivation and psychological distress among medical students. 391J Res Med Sci. 2014;19 [PMC free article] [PubMed] [Google Scholar]
- 54.54. Wong KP, Bonn G, Tam CL, Wong CP. Preferences for online and/or face-to-face counseling among university students in Malaysia. Front Psychol. 2018;9:64. [DOI] [PMC free article] [PubMed]; Wong KP, Bonn G, Tam CL, Wong CP. Preferences for online and/or face-to-face counseling among university students in Malaysia. 64Front Psychol. 2018;9 doi: 10.3389/fpsyg.2018.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]