Abstract
Background
The involvement of pharmacists and pharmacy clinical assistants (CAs) in hospital clinics has demonstrated benefits for improving medication safety and care delivery. Internationally, pharmacy staff played a crucial role in the safe storage, provision and administration of vaccines, as well as reinforcement of pharmacovigilance efforts during the COVID-19 pandemic. In Australia, healthcare providers collaborated to rapidly facilitate a phased COVID-19 vaccination program. The perspectives of the pharmacy team, including pharmacy students, involved in implementing novel health services are underexplored in the literature.
Objective
To describe the key learnings in how a team of pharmacists, CAs and pharmacy students contributed to the COVID-19 vaccine service, and to explore their preparedness and experiences working at a vaccination clinic within a quaternary hospital.
Method
This study involved semi-structured interviews with pharmacy students, CAs and pharmacists. All pharmacy staff who worked in the clinic were invited to participate in the study and a snowball strategy was used to maximise recruitment. The interviews were audio-recorded, transcribed, and analysed using inductive thematic techniques to identify major themes.
Results
A total of 11 participants were interviewed including: four pharmacists, four CAs and three undergraduate students. Using thematic analysis, five main themes were identified: (1) Potential for student value and experiential learning; (2) Adaptive procedures and work practices in a rapidly changing environment; (3) Clear leadership, with role clarity, role expansion and interchangeability; (4) Supportive learning environment and (5) Stakeholder drivers for service delivery and to optimise societal benefit. These five themes often interacted with each other, highlighting the complexities of implementing and operating the service.
Conclusions
The vaccine clinic service provided a novel and valuable opportunity for students, CAs, and pharmacists to work collaboratively, extending their scope of practice to contribute to better national health outcomes. Participants expressed their support for future initiatives involving pharmacy students and healthcare staff collaborating in hospital settings.
Keywords: Pharmacy, Pharmacist, Vaccine, Vaccination, Student, COVID-19
Highlights
-
•
This study included insights from three perspectives in the pharmacy workforce: clinical assistants, students, & pharmacists.
-
•
Key learnings included: adaptive procedures, clear leadership, team preparedness, supportive environments, & shared purpose.
-
•
A student-centred model is described, exemplifying experiential learning that simultaneously optimises service delivery.
-
•
The findings are a foundation for the implementation of other multidisciplinary healthcare initiatives.
1. Introduction
Pharmacy staff can play a crucial role in the safe acquisition, storage, and administration of vaccines.1 After the onset of the Coronavirus 2019 (COVID-19) pandemic, the Therapeutic Goods Administration (TGA) in Australia initially approved the use of the COVID-19 mRNA (Comirnaty®) vaccine and the ChAdOx1-S [recombinant] (Vaxzeria®) vaccine for administration to the public. During the initial critical period (February 2021 to August 2021), healthcare professionals (i.e., nurses, pharmacists, doctors) collaborated to rapidly facilitate phased COVID-19 vaccination. In Australia, phased COVID-19 vaccination meant at-risk staff (e.g., frontline healthcare workers) and vulnerable patient groups received priority vaccination as part of a national roll-out strategy, which was ultimately expanded to the wider population.1 Unlike traditional influenza vaccines, that are usually prefilled syringes in Australia, there were challenges with the COVID-19 vaccines. Both vaccines required aseptic preparation using multi-dose vials and the Comirnaty® vaccine required storage at minus 700C and reconstitution.2 Given the novel handling requirements of these vaccines, healthcare professionals needed thorough training and an accredited competency to ensure safe, efficient, and effective vaccination.3 Vaccine training and competency frameworks are mandatory in Australia, and health professionals who elect to become COVID-19 vaccination providers are required to complete compulsory online training.3 This training covers vaccine handling, storage, documentation, administration, and monitoring for individuals in clinical roles3; and all providers must additionally meet immunisation training requirements for their profession and State or Territory of practice.3 This is in keeping with international standards, whereby health professionals in the United States need to register and undertake training in order to become a COVID-19 vaccination provider.4 A provider refers to someone who is licenced to administer vaccinations and who is required to adhere to best practices pertaining to the storage, handling and administration of vaccines.4 Additionally, providers are required to complete vaccination-related reporting (e.g. number of vaccinations administered, adverse event information).4
Undergraduate pharmacy students are well positioned to assist with the preparation of vaccines, including the COVID-19 vaccination, and their contribution could help improve the efficiency of vaccine programmes. However, pharmacy students do not receive aseptic compounding training during their undergraduate degree. As part of the Bachelor of Pharmacy undergraduate degree, Queensland pharmacy students undertake basic training in extemporaneous compounding (i.e., creams, lotions, ointments) and vaccine administration, in accordance with Standard 5.3 of the National Pharmacy Competency Framework.5 In countries such as Canada, pharmacy students have a wide scope of practice, with studies showing their positive impact on influenza vaccine administration and the provision of vaccine education.6 Student participation in Canadian vaccination programs found that vaccination rates increased from 18.5% to 68%.5 Incorporating pharmacy students into COVID-19 vaccination services could also introduce them to an interdisciplinary team environment in the hospital setting, which is an infrequent experience during the Bachelor of Pharmacy undergraduate program.6 This means that student COVID-19 vaccination clinics may have benefits for student learning, as well as the potential to improve service delivery. Other members of the pharmacy team, such as clinical assistants (CAs; i.e., otherwise known as pharmacy technicians or assistants) and pharmacists, are essential to facilitate student supervision, training, and vaccine preparation, particularly those that specialise in aseptic compounding. Studies have demonstrated how CAs have contributed to aseptic compounding and vaccine preparation, which can improve immunisation rates and service workflow.7, 8, 9
The value of a diverse pharmacy team working in multidisciplinary outpatient clinics has been demonstrated by several local studies,10, 11, 12 including benefits in medication management and patient safety. When incorporated in the clinic setting, pharmacists' knowledge, adaptability, and communication were viewed as highly valuable for the delivery of safe and effective care.11 Similar benefits have been observed with CAs working collaboratively with pharmacists in hospitals and outpatient clinics.13 Given these benefits, the experiences and learnings from implementing service models with a diverse pharmacy team, incorporating pharmacists, CAs, and students, should be explored. In this study, the pharmacy department from the Princess Alexandra Hospital (PAH), partnered with three local universities to employ third- and fourth-year pharmacy students to assist with COVID-19 vaccine preparation. This resulted in the assembly of a novel, multidisciplinary COVID-19 vaccination clinic which incorporated all members of the pharmacy team and was initiated in response to the unprecedented situation of the pandemic. The vaccination clinic involved the acquisition, storage, reconstitution, allocation, and administration of the COVID-19 vaccines. Additionally, there were logistical responsibilities such as staffing, training, procedure/policy development, and ensuring appropriate physical space to safely deliver the service. The aim of this study was to describe the key learnings in how the pharmacy team contributed to the provision of the COVID-19 vaccination clinic and to explore team preparedness and experiences in service implementation at the PAH, a quaternary hospital (i.e., provides high level of specialised care, (e.g., neurosurgery, cardiothoracic surgery)) in Brisbane, Australia.
2. Method
This study involved semi-structured interviews with undergraduate students enrolled in a Bachelor of Pharmacy program, CAs and pharmacists to elicit an in-depth understanding and individual perspectives about the clinic from three different groups in the pharmacy team. Ethics approval for this research was granted by the Metro South Human Research Ethics committee (HREC/2021/QMS/76690) and ratified by The University of Queensland Research Ethics and Integrity committee (2021/HE002045). All participants provided written informed consent. The consolidated criteria for reporting qualitative studies (COREQ) was adhered to throughout data collection and analysis.14
2.1. Setting and participants
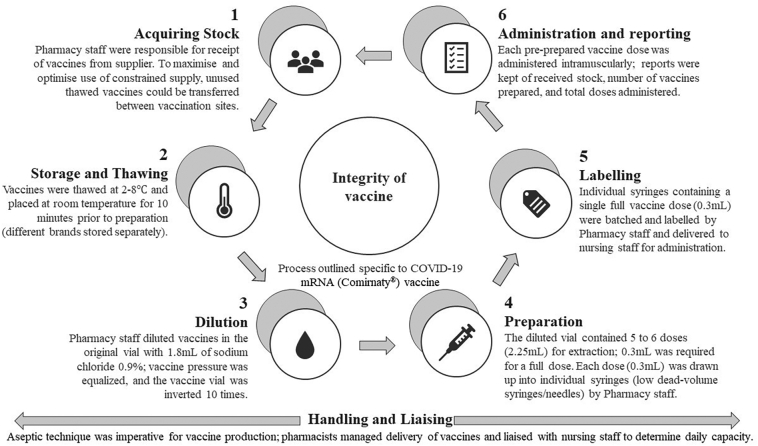
The study took place at the PAH, a large 900-bed adult, metropolitan, quaternary hospital in Brisbane, Queensland, Australia. The staff at the PAH were responsible for the planning and implementation of one of the first major COVID-19 vaccination hubs in the State. The service commenced in February 2021 and ceased operation in August 2021, once community vaccination hubs became self-sufficient and the majority of hospital staff were vaccinated. A total of 65,784 vaccinations were prepared by pharmacy staff during the service timeframe. The aseptic vaccine management process, which highlights the daily workflow, is shown in Fig. 1. As part of the service, the hospital auditorium was repurposed into a vaccination centre with sterile rooms set up for aseptic preparation of vaccines. Nursing, medical and administration staff assisted with administration of vaccines and logistics (e.g., clinic bookings, opening/closing the clinic). Pharmacy staff were wholly responsible for the procurement, storage, aseptic preparation and distribution of vaccines as part of the wider COVID-19 vaccine service initiative. In accordance with best practice standards for vaccine preparation, individual aliquots of vaccines were aseptically prepared in batches, labelled and delivered to nursing staff for safe administration (Fig. 1). To alleviate workload pressure for busy hospital staff and to create a sustainable service, pharmacy students were invited to participate in the clinic by helping to reconstitute and aseptically prepare vaccines.
Fig. 1.
The daily workflow and aseptic vaccine management process undertaken by pharmacy staff working in the COVID-19 vaccination clinic.
All members of pharmacy staff (five pharmacists, seven CAs, and fourteen students) involved in the vaccine service were invited to participate in the interview study via email between August to December 2021. It was important to gather data within six months after the cessation of the clinic to maximise participants recollection of the service and reduce recall bias. A snowball strategy15, 16, 17. was also utilised to optimise recruitment where participants would verbally invite their colleagues who were involved in the vaccine service to participate. This ensured that participants were invited by multiple means which was an important strategy for pharmacy students who had returned to university at the time of the interviews. Participation was voluntary and no compensation or incentives were provided to participants. Recruitment was finalised once data saturation was achieved and there was representation from all three groups (pharmacy students, CAs and pharmacists).
2.2. Data collection
All participants were required to complete and sign a written consent form and demographic information questionnaire prior to their interview. Interviews were conducted either face-to-face or via videoconference, depending on what was feasible and preferred by the participant. Interviews were conducted in a private setting to ensure that participants felt that they were able to disclose their experiences without the risk of being overheard by colleagues. Scheduling of the interview was governed by the availability of the participant, and they were given the opportunity to reschedule if required. Interviews were conducted by NF and CP, both of whom are pharmacist researchers with a background in hospital pharmacy. Whilst both interviewers had conceptual understanding of the roles and responsibilities of pharmacists and pharmacy staff, both were independent from the implementation and operation of the COVID-19 vaccine service. To ensure consistency between interviewers, an interview guide (Supplementary file 1) was developed by the research team and adhered to for each interview. The interview guide, which consisted of semi-structured questions with prompts, was piloted by both NF and CP prior to the first interview with two senior pharmacists independent of the research team, and then subsequently, with the members of the research team. Afterwards, the research team discussed and reviewed the questions to reach consensus for the final interview guide. Field notes were completed by the interviewers after each interview. The interviews were audio-recorded (by NF and CP) and transcribed verbatim by one researcher (CP). Transcripts were de-identified prior to analysis.
2.3. Data analysis
Transcripts were manually coded by one researcher (KD) and the codes were used to generate themes and subthemes following an inductive thematic analysis approach.15 This was completed using the six-step approach to thematic analysis described by Braun and Clarke15: familiarisation, generating initial codes, searching for themes, reviewing the themes, defining and naming themes, and producing the report. Microsoft Excel® software was used to organise the transcripts so that the initial coding process could be completed by one researcher (KD). A random sample of two transcripts (18%) were independently coded by NF to test the reliability of coding. Peer debriefing meetings were held between KD, NF and CP to verify the codes and reach consensus. Initial patterns and codes were identified (Supplementary file 2), and then organised into subthemes. This led to the generation of overarching themes and subthemes, which were then compared to the documented field notes to ensure themes encapsulated the data. Each researcher (KD, NF and CP) then independently selected exemplars from the data to represent each theme and these were discussed until a consensus was reached.
2.4. Demonstrating rigor of method
An essential component of reporting qualitative research is to describe the credibility, transferability, dependability and confirmability of the chosen method.14,18, 19, 20 Credibility in this study was maintained by having researchers who had a conceptual understanding of core pharmacy business (e.g., dispensing, aseptic production) as well as the roles and responsibilities of pharmacy staff. Members of the research team (MB and KW) were also involved in overseeing the implementation of the vaccine service and had in-depth understanding of the operation of the clinic. These researchers did not have access to interview transcripts until after they had been de-identified and the data had been themed. Transferability in this study was achieved through ensuring perspectives from all members of pharmacy staff (CAs, students, and pharmacists) were sought to reduce limiting the results to the viewpoint of a single group. The documentation of field notes by both interviewers throughout this study, as well as regular peer debriefing meetings to discuss progress and research management, ensured that dependability was established.19, 20, 21, 22 Any methodological changes to the research were documented and discussed with the research team. Two minor changes were undertaken during the research process which included: 1) the decision to keep reflexive journals after the first two interviews and 2) the addition of another research team member (KD - external to the vaccine service) to help conduct the analysis, participate in peer debriefing meetings, and contribute to project write-up. Confirmability was ensured using two methods19,20; first through having a researcher independently code a random sample of transcripts (n = 2) to ensure that there was consistency and authenticity in coding. Second, by having meetings between researchers to verify codes, subthemes, and main themes. Further details on how trustworthiness was enhanced have been provided (Supplementary file 3).
2.5. Reflexivity
Reflexivity allows researchers to reflect on how their own inherent preconceived ideas, experiences and knowledge impact on the construction, communication and development of qualitative research in order to minimise potential bias.22, 23., 24. The risk of bias was reduced as KD, NF and CP were independent from the implementation and operation of the COVID-19 vaccine clinic and had minimal preconceived ideas about the service. However, as all are hospital pharmacists, they acknowledge that their opinions and beliefs about the unique skills and services pharmacy staff can offer may have influenced their interpretation of the data. The potential for unequal relationships during interviews with pharmacy students and staff was minimised as both interviewers (NF and CP) were not part of the senior management team at both the PAH or university. Members of the research team who may have been perceived by students and staff as figures of authority (MB, KW and AC) did not have access to identifiable information and this was explained to participants prior to the interview. This was done to reduce the risk of influencing participant responses about their perceptions of the clinic. As the interviewers (NF and CP) are both pharmacists, there were some participants that were known to them. Where possible, recruitment and the interview were undertaken by the interviewer that was not known to the participant to reduce the risk of the interviewee feeling pressured to participate in the research. Information disclosed during the interview remained confidential for all participants and was not discussed outside of the interview.
3. Results
The participant's demographics are presented in Table 1. Eleven participants were interviewed: four pharmacists, four CAs and three students. The CAs had the most previous experience with aseptic dispensing. Pharmacists had an average (standard deviation [SD]) of 9.8 (6.9) years' experience as a pharmacist and an average of 8.8 (7.7) years hospital experience. CAs had an average of 12.3 (6.7) years' experience as a CA with an average of 7.6 (5.3) years hospital experience. All students were in their fourth and final year of the Bachelor of Pharmacy undergraduate program. The duration of the interviews ranged from 17 to 71 min (average [SD] = 35 [17] minutes).
Table 1.
Participant demographic characteristics (N = 11).
| Characteristic | |||
|---|---|---|---|
| Sex | N (%) | ||
| Male | 5 (45) | ||
| Female | 6 (55) | ||
| Clinic Role | N (%) | ||
| Pharmacist | 4 (36) | ||
| Clinical Assistant | 4 (36) | ||
| Student | 3 (27) | ||
| Yes | No | ||
| Previous aseptic dispensing experience | N (%) | N (%) | |
| Pharmacist | 1 (17) | 3 (60) | |
| Clinical Assistant | 4 (67) | 0 (0) | |
| Student | 1 (17) | 2 (40) | |
| Mean (SD) | |||
| Years of experience in role as pharmacist or clinical assistant (non-applicable to students) | Pharmacist | 9.8 (6.9) | |
| Clinical Assistant | 12.3 (6.7) | ||
| Years of experience working in a hospital setting (non-applicable to students) | Pharmacist | 8.8 (7.7) | |
| Clinical Assistant | 7.6 (5.3) | ||
SD is standard deviation.
3.1. Overall themes and subthemes
Five themes described the key learnings in how the pharmacy team contributed to the vaccine service (Table 2). Within each of these themes, the experience and preparedness of the pharmacy team working in the COVID-19 vaccine clinic were identified and discussed. The five themes were: (1) Potential for student value and experiential learning (2) Adaptive procedures and work practices in a rapidly changing environment, (3) Clear leadership with role clarity, role expansion, and interchangeability, (4) Supportive learning environment, and (5) Stakeholder drivers for service delivery and to support societal benefit. Within each of the five main themes, further subthemes were identified. For theme (1), the subthemes were: the need for experiential learning during university and innovative student service models in clinical settings. For theme (2), these were: team response to dynamic situation, consideration of clinic feasibility and set-up and the need for a well-integrated service. For theme (3), the subthemes were: clear leadership and clinic management, and expanding roles and responsibilities. For theme (4), the subthemes were: establishing supportive relationships, learning from experienced colleagues and building team skills and experiences. For theme (5), the subthemes were: humanitarian motivation for clinic involvement, and media and government influenced stakeholder decisions.
Table 2.
Description of main themes and subthemes.
| Main themes | Description | Subtheme identified within each theme | Description |
|---|---|---|---|
|
There is significant potential for students to provide value to clinical service teams, simultaneously providing them with opportunities for learning | Need for experiential learning during university | Students can benefit from working in clinical environments by gaining practical and real-world experiences within multidisciplinary teams |
| Innovative student service models in clinical settings | Innovative service models can enable students to positively contribute to clinical environments by providing value and assistance to others | ||
|
An adaptive team with adaptive processes was needed to effectively operate the COVID-19 vaccination clinic in a rapidly changing environment | Team response to dynamic situation | Ability for the team to be flexible and adaptive in order to respond to the changing clinic service demands |
| Consideration of clinic feasibility and set-up | Considerations for vaccine resources, human resources, and physical space were all important for clinic set-up and operation | ||
| The need for a well-integrated service | Clinic processes need to be streamlined and well-integrated with the entire pharmacy service (often regular pharmacy operations/duties were disrupted) | ||
|
Clear leadership and role clarity was important for the pharmacy team, whilst also enabling expansion and interchangeability of roles and responsibilities | Pharmacists managed logistical processes | Pharmacists managed and led clinic teams, providing oversight for logistical processes, clinic workflows, day-to-day processes, and rosters |
| Expanding roles and responsibilities | There was a need to expand roles and responsibilities, where appropriate, to efficiently run the clinic | ||
|
A supportive learning environment, and supportive teaching, was important for the pharmacy team | Establishing supportive relationships | Pharmacists and CAs led and supported students |
| Learning from experienced colleagues | Clinic staff, particularly students, were guided by experienced team members | ||
| Building team skills and experiences | Training and preparation were integral to clinic operation in conjunction with real-time learnings from practical clinic experience | ||
|
Stakeholder sentiment and decisions in the vaccine clinics were impacted by COVID-19 and aimed at optimising societal benefit | Humanitarian motivation for clinic involvement | Clinic staff had humanitarian reasons for clinic involvement, wanting to help their community and take part in a role that is bigger than themselves |
| Media and government influenced stakeholder decisions | The clinic service was heavily impacted by executive decisions, government mandates, political policies and the media's influence in response to COVID-19 |
3.2. Theme 1: potential for student value and experiential learning
The COVID-19 vaccine service initiative has shown how students can provide value in hospital settings, whilst simultaneously attaining real-world learning experiences. Student involvement in the clinic was viewed positively by all members of the team, with pharmacists and CAs appearing to enjoy teaching and playing an active role in student development. Similarly, students enjoyed working with other pharmacy staff and increasing their confidence throughout the duration of the service. The pharmacy team frequently expressed how they appreciated working in the clinic environment and emphasised the ‘need for experiential learning during university.’ Students described their practical experiences within the clinic and how this could benefit their future work prospects, in both clinical and non-clinical roles:
“This is one of the best things that happened before I actually graduate and then get into the real-world job. Especially, that it was long-term and seeing different types of people… talking and chatting with people who had more than 10 years' experience, that was so good.” (Student3).
“It was just a once in a lifetime kind of opportunity. You don't really have the opportunity to do something like that, so it's helping, with a worldwide kind of deal, and especially also helping the community as well, because you are helping to create vaccines for everyone. It was kind of a win-win because it was a cool opportunity and you're helping quite a lot of people.” (Student2).
This further helped create a conducive learning environment in the clinic as students were able to connect with, be supported by, and learn from experienced pharmacists in their profession:
“Well, we could also ask them about their experiences as a pharmacist as well and advice about working in that field.” (Student2).
The team spoke about how the limited hospital and aseptic compounding experience led to challenges in clinic. For many pharmacy staff, this was their first encounter with aseptic techniques, and whilst staff felt well prepared, many were apprehensive prior to their first shift in the clinic. Reflecting on this, some of the team members highlighted how aseptic teaching could be incorporated into university courses:
“I guess the undergraduate compounding courses and units could be changed slightly to incorporate more sterile productions or aseptic compounding so students can become familiar with how to use syringes and needles and vials versus you know spatulas and pipettes, so instead of a more experimental role in the lab to doing more of a clinical role in the lab.” (Pharmacist1).
This demonstrated how participants felt that vaccine clinics and advanced scope roles would likely become embedded into future pharmacy practice. Although students had limited hospital and aseptic experience, pharmacists described how students were keen to learn and readily took on feedback:
“I think both parties benefit from it, It's a great help to us and it's also really good I feel for undergraduates to see what they need to grow into, what sort of role… and they are very keen to learn.” (Pharmacist2).
All members of the pharmacy team spoke about how the students contributed positively to the COVID-19 vaccine service initiative, demonstrating the effectiveness of ‘innovative student service models in clinical settings.’ Participants provided different ideas where students could be involved in other hospital service models. Students may be able to conduct other clinical tasks under the supervision of pharmacists which may include medication history taking, medication dispensing or supply, and medication reconciliation:
“I guess certain areas where we can get students to do some medication history taking. If there's a possibility of doing medication reconciliation. Those kind of basic things where we can get information from the patients. I guess that is a good initiative to have because, like basically students can take this opportunity to communicate to the patients and also practice getting those kind of soft skills.” (Student1).
Overall, pharmacists and CAs discussed the successes of utilising students in the vaccine clinic. They further emphasised that students were a valuable resource, could assist where appropriate, and were important team members:
“But I think that they were an excellent cohort. And yeah, a great utilisation of resources because they … [helped with] … at least administration, and things like that.” (Pharmacist3).
3.3. Theme 2: adaptive procedures and work practices in a rapidly changing environment
Participants discussed how adaptive procedures and work practices were integral to implementing and operating the COVID-19 vaccine clinic. All participants described how there was a continuous need to adapt to the changing clinic environment which required a ‘team response to the dynamic situation.’ The unpredictability of the timing and extent of the service provision, and the increasing demands of the clinic, were often challenging for the team:
“I think what I've learned in this role is that plans change every day. One day, we're doing this, and this is what our hours are going to be and how we're working. Then, the next day, there's an outbreak and we have to be open much longer.” (Pharmacist4).
This meant that participants felt they had to be flexible within their roles, cover each other where required, and strive to continually improve their team approach:
“So, common things like using emails and group chats. And just regularly touching base as well, so you know when we start morning shifts, … daily catch ups and daily plans – so, what was the plan for today or what's the plan for the week? Who's working on what days and what are the expected patient numbers? And if there's going to be any changes.” (Pharmacist1).
Participants described how they continually refined and adapted clinic operational processes to ensure a streamlined service. This often involved a ‘consideration of clinic feasibility and set-up’ which included discussion about the physical environment, processes for vaccine preparation, and clinic workflow. One of the barriers identified was the difficulty in having a physical space that was not designed specifically for a vaccine service:
“It's one of those things where it was just very ad hoc. The hospital is not designed to be holding a public vaccination clinic, so it was really something when we turned an auditorium into a vaccine clinic.” (Pharmacist1).
Nevertheless, participants spoke about how they developed local protocols and step-by-step guidelines, as driven by the pharmacy department, to help with the preparation and compounding of COVID-19 vaccines. These protocols were collaboratively developed using the team's expertise pertaining to aseptic procedures, infectious diseases and the legalities and requirements around stock handling and pharmaceutical care delivery. Team members spoke about adapting pre-existing guidelines, such as the protocol for aseptic dispensing in the oncology setting, as well as creating new COVID-19 specific procedures:
“They actually … created procedure cards, to make sure that we are able to follow them, step-by-step, if we were unclear or unfamiliar with our procedures.” (Student1).
Within the vaccine preparation process, participants further discussed the challenges with compounding different vaccine brands (which require different storage and preparation) and the need for careful handling of valuable vaccine resources (i.e., drawing up all possible Comirnaty® vaccine doses from the diluted vial), particularly in light of constantly changing vaccine stock issues:
“When we started there, we were only told to do…at least five doses… It's because the stock that we had before wasn't a low [dead space] needle, which if you were asked to do six doses, you really had to fight for it…sometimes I couldn't make the last dose of it, because there wasn't enough [without the low dead space needle].”(CA2).
“The issue is just that, when we were doing both Pfizer and AstraZeneca, because they have different steps, there may be the confusion of us diluting the AstraZeneca instead of the Pfizer...” (Student3).
The pharmacist clinic role within the team was continually evolving. Senior pharmacists were responsible for clinic oversight, which included completion of staff rosters, management of cold chain, organisation of vaccine stock orders and delivery, and development of procedures. Given the unpredictability of service needs, the team highlighted how achieving adequate staffing numbers across the clinic service and the core hospital pharmacy service was often challenging, explaining the importance of considering both separate services as a cohesive whole:
“And then obviously, your Main Department still needs to be running. So, it was a bit of a juggling act. But, yes, we made it work in the end ….” (CA3).
Participants reported that the clinic needs sometimes disrupted pharmacy processes, highlighting ‘the need for a well-integrated service’. This is so that the clinic can operate efficiently whilst simultaneously providing a full-capacity hospital pharmacy service.
3.4. Theme 3: clear leadership with role clarity, role expansion and interchangeability
The successful implementation of the service was dependent upon each pharmacy team member having a designated role and being able to adapt to the dynamic demands of the clinic. As part of the wider healthcare team, participants reported that ‘clear leadership and pharmacist management’ helped to effectively manage workflow in the clinic:
“On a day-to-day basis, running the preparation of the vaccines, and making sure there is good workflow for the nurses to be able to administer the vaccines.” (Pharmacist2).
Pharmacists often had managerial roles, which required them to coordinate the clinic staff, oversee vaccine ordering and administration, and undertake reporting and documentation. This was in addition to the roles pharmacists adopted to help supervise pharmacy students. For most pharmacists, this deviated from their usual clinical and patient facing role in the hospital pharmacy department, and they appreciated the ability to develop an underutilised skillset:
“My role was more management of the clinic in terms of doing the roster for the students and the pharmacists, maintenance of cold chain and the order and delivery of the stock, [and] development of procedures and those types of things.” (Pharmacist4).
Many participants also expressed that there was clear leadership from the pharmacy department director and senior staff, highlighting that the pharmacy team had the necessary expertise, diverse skill mix and appropriate resourcing in order to perform their roles effectively:
“The job was very clear, and also, you had good support from the top. Yeah, and good experienced team leaders.” (CA1).
“There was a vast array of expertise in there, and in the end, we had our leaders who were our HP5s [senior pharmacists] who had a lot of experience in aseptic compounding as well and sterile production, so they gave us all the right resources.” (Pharmacist1).
In response to the changing environment, participants often reported that they had to “jump in” and perform various tasks (e.g., rostering, aseptic preparation, liaison with nursing staff) where required, highlighting the importance of ‘expanding roles and responsibilities.’ Some participants, especially CAs, discussed how they were keen to expand their traditional, dispensing orientated role, which was supported by pharmacists and viewed as an opportunity to maximise the productivity of the pharmacy team:
“Expanding your skill set, and preparing you for this other health professional role, that was awesome.” (CA1).
“The division between pharmacists and CAs I think is … a bit silly…. We should be promoting everyone up and should advance our scope to be able to do more, because in the end it's going to be beneficial for everyone.” (Pharmacist1).
Within the expansion of roles and responsibilities, pharmacists also discussed how important it was to delegate tasks to different members of the team in order to ensure that the clinic ran smoothly and efficiently:
“I was able to essentially take [a] step back delegate my work to other people and just make sure the whole day was running smoothly and as planned, I can make sure as well that I also check on staff, one on one, to make sure everyone's happy and make sure everyone has no problems.” (Pharmacist1).
3.5. Theme 4: supportive learning environment
One of the most positive aspects of the COVID-19 vaccine initiative discussed by the pharmacy team was the supportive learning environment. The team frequently described how they were ‘establishing supportive relationships.’ Students expressed that they felt supported by pharmacists, which helped them feel more comfortable in their role:
“All the students and the pharmacist were just really supportive, like because I know I stuffed up…one of the vials, and they were really supportive and made sure that I take it slow, and really get the basics down. And yeah, it was a good environment.” (Student2).
In addition, the pharmacy team described how they were ‘learning from experienced colleagues’ which further created a supportive environment. Students spoke about how they valued working with pharmacists as they were able to get a sense of their role in hospital, which enabled them to reflect upon their own future practice. Many staff members had diverse professional backgrounds, including working across Australia and in a range of different healthcare settings (e.g., research, industry, community, hospital, oncology). This enabled staff and students to share experiences, expand their horizons and consider alternative avenues for career progression in different aspects of pharmacy service delivery:
“So, working with pharmacists, who are working in hospital, it was so enjoyable for me seeing how helpful they are to other staff, to the patient, and how hard they're working, ...because before I was always scared to work, in pharmacy or maybe hospital.” (Student3).
Some students expressed how there was limited interactions with other health professionals, such as nurses. Pharmacists mentioned how they benefited from the varied skill mix within the team, learning from CAs and other more experienced pharmacists. CA's positively reflected on their ability to support other members of both the pharmacy and multidisciplinary team:
“So that's why I think it's really good that I mean, one of the other pharmacists I work with, [name], has amazing experience. And they are amazing at seeing the bigger picture … that was really useful.” (Pharmacist3).
“Okay, I'm a technician, but I also have this skillset that I can still teach the pharmacist, the doctors or the nurse. So, it's actually pretty cool.” (CA4).
In addition to establishing relationships and learning from experienced colleagues, the pharmacy team described how ‘building team skills and experiences’ helped create a supportive learning environment. Participants highlighted the diversity of the team and emphasised how they utilised their varied skills and experiences. Most CAs had prior aseptic compounding experience which was valued by other team members:
“We were really lucky here at the PAH, in the fact that we've got our sterile production centre. So, we utilised their skills ... So, we have a few CAs that have many years [of] aseptic experience.” (Pharmacist4).
Participants further spoke about how the pharmacy team members were a good fit and how a mix of staff including pharmacists, CAs and students were necessary. The absence of aseptic compounding experience, particularly for students and pharmacists, was often described as a challenge. However, initial, and practical training for vaccine preparation and aseptic compounding was thought to adequately prepare them for their role:
“We had a training sort of session where they explained to us how to draw up the vials and I think it was pretty good, like if it was just the online modules it probably wouldn't have been sufficient, but then, when we actually got the hands-on training session it definitely helped going into that first shift because I had already done it a couple times before.” (Student2).
3.6. Theme 5: stakeholder drivers for service delivery and to optimise societal benefit
The implementation of the vaccine service initiative amidst the global pandemic influenced staff and stakeholder motivators and sentiment. All participants emphasised that a key driver for participation in the clinic was a ‘humanitarian motivation for clinic involvement’ and conveyed how they valued the significance of their role in helping the wider community for societal benefit:
“I thought [it] was a good opportunity, just to be involved in something that's world changing really and being part of an integral part of the community to help combat the situation.” (Pharmacist1).
“It was just like, we're going to come here and do this, so that I can help the community out to get everyone vaccinated.” (CA1).
Participants believed that the clinic was a novel service, and members of the team expressed enthusiasm towards the role. They highlighted how the role provided an important opportunity to gain new experiences and be part of something bigger than themselves:
“I just wanted to do something for the community and people that have lost like, we've lost a lot of loved ones, especially back in my home country, and so I thought that would be a good way to just give it back to the people.” (Student3).
As the impacts of COVID-19 continued to unfold, participants described how ‘media and government influenced stakeholder decisions,’ particularly hospital executives:
”I felt like a lot of decisions executives were making was on the basis of politics and that they wanted to keep their bosses and the public happy.” (Pharmacist1).
Participants discussed some of the complex interdependencies between the media, government policies, and organisational strategies at national, State and local hospital levels. They often described how clinic staff working on the ‘ground-level’ were impacted by decisions made at a ‘higher-level’ (hospital executives and political agendas). The media emerged as a significant driver for stakeholder behaviour and clinic operation due to its role in influencing public sentiment towards the COVID-19 vaccine:
“I feel like the media plays a part in the whole, get the jab and don't get the jab kind of thing. So, there was a few weekends where it was a little quiet, but then the clinic just opened, just like that. Yeah, so it opened really quickly but nobody knew that it was opened.” (CA4).
In light of this, some participants further discussed how there should be cooperation with the media to help distribute appropriate health information to the public. They also emphasised how the unprecedented nature of COVID-19 required an iterative learning process, where everyone was improving their response to feedback and shifting situations:
“We thought that people were keen to get the vaccinations. But it turned out that 50, probably not even 50, more like 70% or 80% of people wouldn't get the vaccination. Probably because of bad publicity or knowing that the news, it's always the side effects of the medications that are being brought up instead of our how the vaccine would probably protect you from the virus itself.” (CA2).
Participants also reflected on how the PAH vaccination clinic was used to develop and inform the roll-out of larger-scale, community vaccination hubs. They acknowledged that the successful operation of these hubs relied on key stakeholders, such as the government, health professionals and the media, working collaboratively together to optimise service delivery and public health messaging:
“Maybe, what we need to do, is work more with the media for these kinds of things, and spread the word that, hey, this clinic is now open this weekend, or this weekend, which is what they've been doing with the convention centres. Now, the government, the statewide effort has actually gotten better too, as we've travelled along, and everybody's kind of learned some lessons.” (CA4).
4. Discussion
This study explored the preparedness and experiences of the pharmacy team and described their key learnings in contributing to the implementation and provision of the local COVID-19 vaccination service. The unprecedented nature of the COVID-19 pandemic required the mobilisation and recruitment of health staff and the rapid upskilling of the pharmacy workforce to adopt a new vaccination clinic service model. This service model incorporated a diverse pharmacy team which included pharmacists, CAs and undergraduate Bachelor of Pharmacy students. The five identified themes described the factors involved in the successful implementation of the novel COVID-19 vaccine service, the key attributes of a productive inter-disciplinary healthcare team, and the benefits of experiential learning for undergraduate pharmacy students. Adaptive procedures, clear leadership and role clarity, a supportive learning environment, shared goals that benefited society and experiential learning for students were highlighted as essential for implementing a novel COVID-19 vaccine service.
4.1. Novel health service models
The COVID-19 pandemic was the impetus for rapid changes to health service delivery worldwide, including the implementation of interdisciplinary vaccination services.25,26 Ordinarily, adopting new health service models requires extensive research and planning, sufficient funding and governance, and comprehensive staff training prior to implementation.27 The emergent nature of the COVID-19 crisis meant that this process was expedited, placing pressure on the workforce to meet national disease prevention targets. As highlighted by this study, this brought to the forefront the critical role of pharmacists and CAs in disaster management. Recent research suggests that pharmacists in the Australian setting are underprepared to respond to disasters, with no standardised processes for disaster management and limited guidance available to govern response, especially for widespread health crises such as the COVID-19 pandemic.28,29 Similarly, participants in this study detailed how they had to rapidly develop policies, change workflow and adapt training materials in order to effectively and safely deliver the vaccine service.
In 2016, The International Pharmaceutical Federation (FIP) stipulated that pharmacists should be prepared to perform their core business, as well as undertake potentially extended roles during and in the aftermath of a disaster.30 The results from this study support this as respondents discussed their rapid expansion of roles to match the challenge. This included aseptic production, staff training, and staff management, highlighting the challenges of maintaining baseline service delivery during the clinic operation. A key driver for success was the unprecedented recruitment and rapid upskilling of pharmacy students to help alleviate workload pressures on the delivery of pharmaceutical care hospital wide (external to the clinic). Critical to this initiative was the implementation of a structured and thorough training program, utilising both online and practical components, to optimise the preparedness of staff. These training programs were developed by experienced staff with extensive knowledge in aseptic preparation, vaccination, and infectious diseases. According to McCourt et al., the preparedness of staff is vital to ensure a safe and effective health response to disasters.28,29 The training allowed staff, particularly students, to become confident in their role and feel prepared to manage the complexities of the COVID-19 response.
The rapid nature of the COVID-19 response required delegation of tasks to optimise the safe implementation and delivery of the vaccine service initiative. This involved utilising work groups to formulate a coordinated response. Senior staff were required to research and develop policies and guidelines, whilst simultaneously providing oversight for the operational responsibilities of the clinic performed by junior staff. This allowed the service to meet the World Health Organisation's goals for quality healthcare, including timely and efficient delivery of health services.31 To further provide timely and efficient care, participants spoke about the ability of the team to utilise their expertise to maximise outcomes and allow staff to operate across a wide range of responsibilities, with senior members liaising with key stakeholders.
Evident in the response to the COVID-19 pandemic, and a pertinent consideration for the vaccination service, was the role of the media in influencing consumer behaviour. In this study, participants reflected that the patronage of the clinic and opinions towards vaccination were directly influenced by media coverage. The evolving and expanding impact of the media influencing public health has been acknowledged in the literature throughout the last two decades.32., 33, 34, 35, 36 The media has previously played a critical role in public health messaging for HIV/AIDs, cancer screening and mental health campaigns.32., 33, 34, 35, 36 Similar to the findings of this study, the crucial role of the media in the COVID-19 pandemic to inform health messaging has been reported internationally.37 However, as highlighted by the COVID-19 response, the role of the media can cause the dissemination of harmful and incorrect information to the public.38,39 Future development of health service models should consider early liaison with media outlets as key stakeholders to help support the distribution of correct and helpful health information to the public.
4.2. Successful healthcare teams
To optimise the safe and effective delivery of medications and pharmaceutical care, the pharmacy profession is continuously seeking to expand its scope of practice and responsibilities. Fundamental to this is the effectiveness of the healthcare team, which was critical to the success of the COVID-19 vaccine service. In addition to the expansion of roles, senior leadership, and staff training, the resilience of the team emerged as an imperative component for the success of the service. Resilience is a trait that is becoming increasingly necessary for health professionals to cultivate and has been recognised as a critical component to successful disaster management.28,40 Although participants did not explicitly state that the team was resilient, key attributes described by the participants indicated that a resilient team was established between all members of the pharmacy team. Ambrose et al. described three key attributes of resilience in healthcare.40 The first attribute was resilience as a dynamic contextual process, indicating that the pandemic created a state of adversity to which healthcare professionals needed to respond.40 Respondents spoke of the ability of the team to adapt to the dynamic situation which meant sudden changes to rosters, clinic opening hours, vaccine production and software updates. Ambrose et al. also highlights that resilience enables the team to maintain a routine level of function and that it is a catalyst for the actualisation of innate and acquired skills and ability within the healthcare team.40 These attributes were reflected in this study as participants acknowledged the diverse skill mix of experienced staff and the ability of the team to effectively prepare colleagues to confidently perform their role and work in conjunction with core pharmacy services. Participants also discussed how the team fostered a supportive environment and the ability of team members to recognise, encourage and utilise the skills of their colleagues, another trait of resilient teams.41 This ability of a team to cultivate a trusting and supportive environment has been recognised as a key component of effective healthcare teams and is essential for the improvement of patient safety.41 For future initiatives, it could be useful to adopt a multidisciplinary approach to clinics. This was mentioned by some students who acknowledged that there was limited interaction with other non-pharmacy staff (i.e., nurses). Collaboration and information sharing between multiple disciplines can improve patient care12; therefore, a multidisciplinary approach could contribute to greater service successes.
In addition to resilience, a shared purpose is a key driver to the success of a healthcare team.42 Whilst participants acknowledged the benefits the clinic provided of acquiring new skills, expanding their career and networking with colleagues, it was their shared purpose for participation that contributed to the team's effectiveness. The key motivator for involvement in the clinic was to provide humanitarian aid in the health crisis and to be of benefit to their community. These findings are similar to another qualitative study that investigated health professionals' attitudes to work during an influenza pandemic.43 Their findings showed that participants had a strong sense of duty to work and help patients.43 This was a result of their perceived professional responsibility and moral duty to help those in need, their work ethic, and/or their loyalty to their employers and colleagues.43 Positively, these findings show the importance that health professionals place on improving healthcare for patients. When establishing new healthcare teams or service models, it is important to acknowledge the underlying motivators for participation and to use these factors to encourage teamwork and perseverance to increase the opportunity for success.
4.3. Experiential learning for students
Pharmacy students played a central role in the effective operation of the COVID-19 vaccination service through the aseptic preparation of the vaccines which alleviated the workload pressures placed on the existing pharmacy service. Student involvement in the clinic was a mutually beneficial arrangement whereby vaccine production was optimised and students were given the opportunity to receive experiential learning in a hospital setting. All pharmacy staff in this study reflected on the benefits of having the students in the team as a way to share knowledge, build skills and maximise clinic efficiency. These findings are supported by international studies that have previously incorporated pharmacy students into vaccination service initiatives.6,44 The importance of experiential learning for healthcare students, including pharmacy students, is widely acknowledged to help facilitate their transition from university to real-world practice.45, 46, 47, 48 This has been traditionally difficult to implement, particularly in a hospital setting, due to the level of organisation, student preparedness and staff resources required.46 This difficulty was exacerbated during the COVID-19 pandemic because students had restricted access to healthcare facilities due to lockdowns and had to undertake online and remote learning activities.49 The vaccine service was beneficial as it gave students invaluable ‘real-world’ skills in aseptic preparation as well as the ability to work side-by-side with pharmacy colleagues. This helped students build confidence in their work within interdisciplinary healthcare teams. Furthermore, the clinic had the added benefit of integrating students into the health service, which optimised the delivery of the vaccinations and eliminated the challenges typically associated with experiential learning.46 This was demonstrated through the expansion of the student's skills pertaining to non-patient facing roles which has received increased focus in overseas settings and has been recognised as vital for future pharmacy practice.50 Increased emphasis has also been placed on education that incorporates pharmaceutical industry and non-clinical pharmacy roles for Bachelor of Pharmacy students.50,51
Based on the success of incorporating students into the vaccination service and the recognition of the value of experiential learning in the pharmacy program, it is vital to consider the expansion of other student-centred service models. In this study, participants suggested that pharmacy students could have an expanded role in clinical settings to help consolidate medication history taking and reconciliation skills, which can simultaneously improve their communication with patients and healthcare teams. Ultimately, this calls for better collaboration between university institutions and teaching hospitals to allow students to be exposed to meaningful learning that incorporates clinical and non-clinical skills (e.g., aseptic production and compounding). Optimising the use of pharmacy students into the workforce will benefit students and help to minimise the challenges of including experiential learning in the Bachelor of Pharmacy program. Additionally, as was the case in this study, it can improve the efficiency and delivery of the healthcare service. Future research and service models should consider effective incorporation of pharmacy students into their programs to enhance delivery of healthcare and optimise student learning.
4.4. Limitations
This study investigated the pharmacy team from a single vaccination clinic and consequently, the findings may not be generalisable or transferrable to other vaccination clinics or settings. However, this was one of the first major vaccination services in Queensland, Australia, and the service was used as a model and foundation for other vaccine services across the State. Consequently, participants were able to provide unique insight into the enablers, barriers and challenges of implementing the new service model. It is acknowledged that there is the potential for bias as participants, particularly students, may have felt obliged to offer socially and/or professionally desirable responses to the interview questions. Student recruitment was difficult, particularly as this was during the university examination period, a busy time for students. While the views presented here may not be representative of all students that worked in the clinic, the focus of the study was on the pharmacy team, and saturation was reached without the need to interview additional students. To minimise the risk of bias and increase rigor and reflexivity of method, it was ensured that interviewers were experienced pharmacists who were independent from the vaccination clinic service and only de-identified transcripts were used for analysis. It is also acknowledged that due to the dynamic nature of the COVID-19 response, participants sentiments towards the clinic could have evolved with time and as a result of changes in vaccination policy. To allow for consistency in their responses, all participants were interviewed after they had completed their role within the clinic.
5. Conclusion
The COVID-19 vaccination service initiative provided a novel and valuable opportunity for pharmacists, CAs and students to work collaboratively in a team and extend their scope of practice. This study highlighted the key learnings from the service which included the need for adaptive team and work procedures, clear leadership, team preparedness, a supportive learning environment and shared purpose. These attributes enabled the pharmacy team to work within a multidisciplinary service to effectively acquire, reconstitute and prepare COVID-19 vaccinations and the learnings were able to guide the development of larger community vaccination clinics. The service provided an opportunity for students to receive experiential learning in a hospital setting, whilst simultaneously contributing to improved service efficiencies and enhanced patient care. Attributes for a resilient healthcare team and the benefits of experiential learning for pharmacy undergraduate students were emphasised. Students were able to translate their learning into practice, build further skills, and develop confidence towards their journey for employment readiness. Participants expressed their support for future initiatives involving pharmacy students and staff working together in hospital settings.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
None
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rcsop.2023.100241.
Appendix A. Supplementary data
Supplementary file 1: Semi-structured interview guide
Supplementary file 2: Mind-map of initial patterns and codes identified from participant transcripts
Supplementary file 3–Trustworthiness and Reflexivity
References
- 1.Australian Government Australia's COVID-19 Vaccine National Roll-Out Strategy. 2022. https://www.health.gov.au/sites/default/files/documents/2021/01/covid-19-vaccination-australia-s-covid-19-vaccine-national-roll-out-strategy.pdf
- 2.Dawoud D. Emerging from the other end: key measures for a successful COVID-19 lockdown exit strategy and the potential contribution of pharmacists. Res Social Adm Pharm. 2021;17(1):1950–1953. doi: 10.1016/j.sapharm.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rogers T. A Set of Principles Underpin Good Pharmaceutical Expertise for the Vaccination Programme; these are Independent of the Vaccine Brand. 2022. https://www.health.gov.au/covid-19-vaccination-training-program Published 2021. Accessed 1 May.
- 4.Centre for Disease Control and Prevention (CDC) US Department of Health and Human Services; 2022. FAQs for Private and Public Healthcare Providers About Implementing the CDC COVID-19 Vaccination Program in Provider Practices.https://www.cdc.gov/vaccines/covid-19/vaccine-providers-faq.html [Google Scholar]
- 5.Society of Hospital Pharmacists Australia (SHPA) Standards of Practice. 2022. https://www.shpa.org.au/publications-resources/standards-of-practice
- 6.Church D., Johnson S., Raman-Wilms L., Schneider E., Waite N., Pearson Sharpe J. A literature review of the impact of pharmacy students in immunization initiatives. Can Pharm J (Ott) 2016;149(3):153–165. doi: 10.1177/1715163516641133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hill J.D., Anderegg S.V., Couldry R.J. Development of a pharmacy technician–driven program to improve vaccination rates at an academic medical center. Hosp Pharm. 2017;52(9):617–622. doi: 10.1177/0018578717722788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Demarco M., Carter C., Houle S.K.D., Waite N.M. The role of pharmacy technicians in vaccination services: a scoping review. J Am Pharm Assoc. 2022;62(1):15–26.e11. doi: 10.1016/j.japh.2021.09.016. [DOI] [PubMed] [Google Scholar]
- 9.McKeirnan K.C., McDonough R.P. Transforming pharmacy practice: advancing the role of technicians. Pharm Today. 2018;24(6):54–61. [Google Scholar]
- 10.Snoswell C.L., Cossart A.R., Chevalier B., Barras M. Benefits, challenges and contributors to the introduction of new hospital-based outpatient clinic pharmacist positions. Explor Res Clin Soc Pharm. 2022;5 doi: 10.1016/j.rcsop.2022.100119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomas E.E., de Camargo Catapan S., Haydon H.M., Barras M., Snoswell C. Exploring factors of uneven use of telehealth among outpatient pharmacy clinics during COVID-19: a multi-method study. Res Social Adm Pharm. 2022;18(9):3602–3611. doi: 10.1016/j.sapharm.2022.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Snoswell C.L., De Guzman K.R., Barras M. Pharmacists reducing medication risk in medical outpatient clinics: a retrospective study of 18 clinics. Intern Med J. 2023;53(1):95–103. doi: 10.1111/imj.15504. [DOI] [PubMed] [Google Scholar]
- 13.Seston E.M., Ashcroft D.M., Lamerton E., Harper L., Keers R.N. Evaluating the implementation and impact of a pharmacy technician-supported medicines administration service designed to reduce omitted doses in hospitals: a qualitative study. BMC Health Serv Res. 2019;19(1):325. doi: 10.1186/s12913-019-4146-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tong A., Sainsbury P., Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International J Qual Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 15.Braun V.C.V. Sage Publication Ltd; 2013. Successful Qualitative Research - a Practical Guide for Beginners. [Google Scholar]
- 16.Noy C. Sampling knowledge: the hermeneutics of snowball sampling in qualitative research. Int J Soc Res Methodol. 2008;11(4):327–344. [Google Scholar]
- 17.Sedgwick P. Snowball sampling. BMJ. 2013;347 (dec20 2):f7511-f7511. [Google Scholar]
- 18.Patton M. 4th ed. 2015. Qualitative Research and Evaluation Methods. [Google Scholar]
- 19.Lincoln Y.S.G.E. SAGE Publications; London: 1985. Naturalistic Inquiry (SAGE Publications, London) [Google Scholar]
- 20.Nowell L.S., Norris J.M., White D.E., Moules N.J. Thematic analysis. Int J Qual Methods. 2017;16(1) 160940691773384. [Google Scholar]
- 21.Elo S., Kääriäinen M., Kanste O., Pölkki T., Utriainen K., Kyngäs H. Qualitative content analysis. SAGE Open. 2014;4(1) 215824401452263. [Google Scholar]
- 22.Amin M.E.K., Norgaard L.S., Cavaco A.M., et al. Establishing trustworthiness and authenticity in qualitative pharmacy research. Res Social Adm Pharm. 2020;16(10):1472–1482. doi: 10.1016/j.sapharm.2020.02.005. [DOI] [PubMed] [Google Scholar]
- 23.Daly K. Qualitative Methods for Family Studies & Human Development. 2007. https://sk.sagepub.com/books/qualitative-methods-for-family-studies-and-human-development In: Thousand Oaks, California. Accessed 2022/12/06.
- 24.Malterud K. Qualitative research: standards, challenges, and guidelines. Lancet. 2001;358(9280):483–488. doi: 10.1016/S0140-6736(01)05627-6. [DOI] [PubMed] [Google Scholar]
- 25.Andrade J., Slaby M., DeAngelis J., et al. Implementation of a pharmacist-led COVID-19 vaccination clinic at a community teaching hospital. Am J Health Syst Pharm. 2021;78(12):1038–1042. doi: 10.1093/ajhp/zxab135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Garofoli G.K., Gálvez-Peralta M., Barrickman A.L., et al. Establishment and evaluation of scalable COVID-19 vaccine clinics at a large university. J Am Pharm Assoc (2003) 2022;62(4):1430–1437. doi: 10.1016/j.japh.2022.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.State of Queensland (Queensland Health) Guide to Health Service Planning (Version 3) https://www.health.qld.gov.au/publications/portal/health-services-planning/guideline-health-service-planning.pdf
- 28.McCourt E., Singleton J., Tippett V., Nissen L. Disaster preparedness amongst pharmacists and pharmacy students: a systematic literature review. Int J Pharm Pract. 2021;29(1):12–20. doi: 10.1111/ijpp.12669. [DOI] [PubMed] [Google Scholar]
- 29.McCourt E.M., Singleton J.A., Tippett V., Nissen L.M. Evaluation of disaster preparedness and preparedness behaviors among pharmacists: a cross-sectional study in Australia. Prehosp Disaster Med. 2021;36(3):354–361. doi: 10.1017/S1049023X21000133. [DOI] [PubMed] [Google Scholar]
- 30.International Pharmaceutical Federation (FIP) 2016. Responding to Disasters: Guidelines for Pharmacy 2016. [Google Scholar]
- 31.World Health Organization (WHO) Quality of Care. https://www.who.int/health-topics/quality-of-care#tab=tab_1
- 32.Institute of Medicine Committee on Assuring the Health of the Public in the 21st C . National Academies Press (US) Copyright 2003 by the National Academy of Sciences. All rights reserved; Washington (DC): 2002. The Future of the Public's Health in the 21st Century. [Google Scholar]
- 33.Plackett R., Kaushal A., Kassianos A.P., et al. Use of social media to promote cancer screening and early diagnosis: scoping review. J Med Internet Res. 2020;22(11) doi: 10.2196/21582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Durkin S., Broun K., Guerin N., Morley B., Wakefield M. Impact of a mass media campaign on participation in the Australian bowel cancer screening program. J Med Screen. 2020;27(1):18–24. doi: 10.1177/0969141319874372. [DOI] [PubMed] [Google Scholar]
- 35.Cheng J., Benassi P., De Oliveira C., Zaheer J., Collins M., Kurdyak P. Impact of a mass media mental health campaign on psychiatric emergency department visits. Can J Public Health. 2016;107(3):e303–e311. doi: 10.17269/CJPH.107.5265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bou-Karroum L., El-Jardali F., Hemadi N., et al. Using media to impact health policy-making: an integrative systematic review. Implement Sci. 2017;12(1):52. doi: 10.1186/s13012-017-0581-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu Q., Zheng Z., Zheng J., et al. Health communication through news media during the early stage of the COVID-19 outbreak in China: digital topic modeling approach. J Med Internet Res. 2020;22(4) doi: 10.2196/19118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mheidly N., Fares J. Leveraging media and health communication strategies to overcome the COVID-19 infodemic. J Public Health Policy. 2020;41(4):410–420. doi: 10.1057/s41271-020-00247-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zarocostas J. How to fight an infodemic. Lancet. 2020;395(10225):676. doi: 10.1016/S0140-6736(20)30461-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ambrose J.W., Layne D.M., Nemeth L.S., Nichols M. A systematic concept analysis of healthcare team resilience in times of pandemic disasters. Nurs Forum. 2022;57(4):671–680. doi: 10.1111/nuf.12723. [DOI] [PubMed] [Google Scholar]
- 41.Rosen M.A., DiazGranados D., Dietz A.S., et al. Teamwork in healthcare: key discoveries enabling safer, high-quality care. Am Psychol. 2018;73(4):433–450. doi: 10.1037/amp0000298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mirkov S. Teamwork for innovation in pharmacy practice: from traditional to flexible teams. Drugs Ther Perspect. 2018;34(6):274–280. [Google Scholar]
- 43.Ives J., Greenfield S., Parry J.M., et al. Healthcare workers’ attitudes to working during pandemic influenza: a qualitative study. BMC Public Health. 2009;9(1):56. doi: 10.1186/1471-2458-9-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.George D.L., O’Neal K.S., Johnson E.J., Smith M.J. Student preferences regarding didactic content and practical experiences of influenza vaccination clinic business operations in a pharmacy business and entrepreneurship elective. Curr Pharm Teach Learn. 2016;8(2):207–212. [Google Scholar]
- 45.Hattingh H.L., Robinson D., Kelly A. Evaluation of a simulation-based hospital pharmacy training package for pharmacy students. Int J Educ Technol High Educ. 2018;15(1) [Google Scholar]
- 46.Jacob S.A., Boyter A.C. Nationwide survey of experiential learning in MPharm programmes in UK universities. Int J Pharm Pract. 2020;28(2):121–129. doi: 10.1111/ijpp.12521. [DOI] [PubMed] [Google Scholar]
- 47.McCartney J., Boschmans S.-A. South African pharmacy student perspectives of a hospital-based experiential learning programme. Pharm Educ. 2018;18(0):29–40. [Google Scholar]
- 48.Noble C., McKauge L., Clavarino A. Pharmacy student professional identity formation: a scoping review. Integr Pharm Res Pract. 2019;8:15–34. doi: 10.2147/IPRP.S162799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fuller K.A., Heldenbrand S.D., Smith M.D., Malcom D.R. A paradigm shift in US experiential pharmacy education accelerated by the COVID-19 pandemic. Am J Pharm Educ. 2020;84(6) doi: 10.5688/ajpe8149. ajpe8149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Donovan M.D., Byrne E.M., Griffin B.T. Perspectives of pharmacists on facilitating experiential learning placements for pharmacy students in non-patient facing settings. Curr Pharm Teach Learn. 2020;12(8):901–909. doi: 10.1016/j.cptl.2020.04.011. [DOI] [PubMed] [Google Scholar]
- 51.Hartman R., Blustein L., Morel D., Davis L. A pharmaceutical industry elective course on practice experience selection and fellowship pursuit by pharmacy students. Am J Pharm Educ. 2014;78(6):126. doi: 10.5688/ajpe786126. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary file 1: Semi-structured interview guide
Supplementary file 2: Mind-map of initial patterns and codes identified from participant transcripts
Supplementary file 3–Trustworthiness and Reflexivity