Abstract
Background:
Significant differences exist between feminine and masculine lower extremities, and this region contributes to gender dysphoria in transgender and nonbinary individuals.
Methods:
A systematic review was conducted for primary literature on lower extremity (LE) gender affirmation techniques as well as anthropometric differences between male and female lower extremities, which could guide surgical planning. Multiple databases were searched for articles before June 2, 2021 using Medical Subject Headings. Data on techniques, outcomes, complications, and anthropometrics were collected.
Results:
A total of 852 unique articles were identified: 17 met criteria for male and female anthropometrics and 1 met criteria for LE surgical techniques potentially applicable to gender affirmation. None met criteria for LE gender affirmation techniques specifically. Therefore, this review was expanded to discuss surgical techniques for the LE, targeting masculine and feminine anthropometric ideals. LE masculinization can target feminine qualities, such as mid-lateral gluteal fullness and excess subcutaneous fat in the thigh and hips. Feminization can target masculine qualities like a low waist-to-hip ratio, mid-lateral gluteal concavity, calf hypertrophy, and body hair. Cultural differences and patient body habitus, which influence what is considered “ideal” for both sexes, should be discussed. Applicable techniques include hormone therapy, lipo-contouring, fat grafting, implant placement, and botulinum toxin injection, among others.
Conclusions:
Due to lack of existing outcomes-based literature, gender affirmation of the lower extremities will rely on application of an array of existing plastic surgery techniques. However, quality outcomes data for these procedures is required to determine best practices.
Keywords: body contouring, fat grafting, gender-affirming surgery, liposuction, lower extremity, transgender
Introduction
Typically, gender dysphoria is discussed in the context of incongruence between a individual's gender identify and their facial features, chest/breast anatomy, and/or genitalia. However, the lower extremity (LE), especially the hips, thighs, and feet, also carry considerable dysphoria for many.1
Similar to the upper extremity, the LE, which for the purposes of this review includes all structures caudal to and inclusive of the hips, excluding the genitalia, has been overlooked as a major contributor to gender dysphoria.2 However, it is a highly sexually dimorphic region. Wide hips in transgender men, like large feet in transgender women, may reveal a patient's sex assigned at birth and cause dysphoria. This review will explore sexually dimorphic features of the hips, buttocks, thighs, knees, legs, ankles, and feet, and also discuss surgical and nonsurgical techniques that may afford feminization and masculinization of these areas.
Methods
A literature review of gender-affirmation surgery (GAS) of the LE was conducted. A survey of PubMed, EBSCO, and LILACS databases was performed for articles published before June 2, 2021. Search terms were chosen based on each database's index of search terms and/or researcher consensus as pertinent to GAS of the LE and/or anthropometric norms and ideals of masculine and feminine lower extremities (Supplementary Content S1). Results were screened by two independent reviewers (I.T.N. and E.S.), first by title and abstract and then by full text.
Articles were included if they were primary English-language literature detailing outcomes of gender-affirming surgery for the lower extremities. As secondary inclusion criteria, articles were included if they discussed (1) primary outcomes of surgical techniques applicable to LE feminization and/or masculinization; and (2) if they provided primary outcomes of studies regarding actual or ideal anthropometric measurements of male versus female lower extremities. Data on study methods, surgical techniques, outcomes and complications of surgical procedures, and anthropometric parameters were gathered. As this was a systematic review, this research was IRB exempt.
Results
From our preliminary search, 852 articles were identified after removing duplicates. After screening by title, abstract, and full text, there were no articles that reported primary outcomes of LE GAS (Fig. 1). However, 17 articles met secondary inclusion criteria for anthropometric measurements of the LE in men and/or women; and 1 article met inclusion criteria for surgical techniques applicable to LE feminization and/or masculinization. Our search was further expanded to include additional data, including primary academic literature, review articles, and nonacademic literature. Ultimately, our expanded search identified 29 articles meeting inclusion criteria (i.e., primary literature) for our discussion of anthropometrics and 23 that met criteria for our discussion of surgical techniques (Tables 1 and 2).
FIG. 1.
Search strategy following PRISMA guidelines for systematic review. PRISMA, preferred reporting items for systematic reviews and meta-analyses.
Table 1.
Included Studies Discussing Anthropometrics of Lower Extremity
| First authorRef. | Year | Study population | Characteristic described |
|---|---|---|---|
| Maughan25 | 1983 | 25 Cisgender women, 25 cisgender men | Female lower extremity, actual; male lower extremity, actual |
| Singh20 | 1994 | Survey respondents (physicians) | Female lower extremity, ideal |
| Singh18 | 1995 | Survey respondents (females) | Male lower extremity, ideal |
| McLean5 | 1998 | 16 Cisgender women, 15 cisgender men | Female lower extremity, actual; male lower extremity, actual |
| Tsai31 | 2000 | Survey respondents | Female lower extremity, ideal |
| Swami14 | 2006 | Survey respondents | Female lower extremity, ideal; Male lower extremity, ideal |
| Zifchock40 | 2006 | 77 Cisgender women, 68 cisgender men | Female foot, actual; male foot actual |
| Voracek36 | 2007 | 75 Cisgender women, 75 cisgender men | Female foot, ideal; male foot, ideal |
| Krauss35 | 2008 | 397 Cisgender women, 398 cisgender men | Female foot, actual; male foot actual |
| Maurins11 | 2008 | 3072 Cisgender women and men | Female lower extremity, actual; male lower extremity, actual |
| Ruckley12 | 2008 | 867 Cisgender women, 699 cisgender men | Female lower extremity, actual; male lower extremity, actual |
| Voracek42 | 2010 | 69 Cisgender women, 59 cisgender men | Female foot, actual; male foot actual |
| Sorokowski19 | 2012 | Survey respondents | Female lower extremity, ideal; male lower extremity, ideal |
| Sorokowski22 | 2012 | Survey respondents | Female lower extremity, ideal; male lower extremity, ideal |
| Sanchez39 | 2013 | 199 Cisgender women, 201 cisgender men | Female foot, actual; male foot actual |
| Ahmed34 | 2014 | 376 Women and men | Female lower extremity, actual; male lower extremity, actual |
| Sherk30 | 2014 | 76 Cisgender women, 82 cisgender men | Female lower extremity, actual; male lower extremity, actual |
| Tomassoni37 | 2014 | 528 Cisgender women, 577 cisgender men | Female foot, actual; male foot actual |
| Aenumulapalli38 | 2017 | 250 Cisgender women, 250 cisgender men | Female foot, actual; male foot actual |
| Heidekrueger21 | 2017 | 1032 Survey respondents | Female buttocks, ideal |
| Behan23 | 2018 | 34 Cisgender women, 32 cisgender men | Female thigh, actual; male thigh, actual |
| Otsuka26 | 2018 | 6 Female cadavers, 6 male cadavers | Female thigh, actual; male thigh, actual |
| Şaylı32 | 2018 | Survey respondents | Female foot, actual; male foot actual |
| Vartanian24 | 2018 | Survey respondents | Female buttocks, ideal |
| Rudolph9 | 2019 | 10 Female cadavers, 10 male cadavers | Female buttock, actual; male buttock, actual |
| Bank17 | 2020 | 40 Cisgender women, 48 cisgender men | Female lower extremity, actual; male lower extremity, actual |
| Cotofana10 | 2020 | 75 Cisgender women, 75 cisgender men | Female lower extremity, actual; male lower extremity, actual |
| Wiik45 | 2020 | 11 Transgender women, 12 transgender men | Female lower extremity, actual; male lower extremity, actual |
| Zhao41 | 2020 | 74 Cisgender women, 99 cisgender men | Female foot, actual; male foot actual |
Table 2.
Included Studies Discussing Lower Extremity Treatments Applicable to Gender Affirmation Surgery
| First authorRef. | Year | Study population | Technique discussed |
|---|---|---|---|
| Chamosa28 | 1997 | 108 Cisgender women | Liposuction of knee |
| Chamosa71 | 1997 | 113 Cisgender women | Liposuction of ankle |
| Lemperle60 | 1998 | 15 Cisgender women | Calf contouring through gastrocnemius resection |
| Coughlin33 | 2000 | 53 Cisgender women, 10 cisgender men | Hammertoe correction |
| Lee59 | 2006 | 20 Cisgender women | Calf contouring through gastrocnemius resection |
| Kim61 | 2008 | 20 Cisgender women | Calf contouring through sural neurectomy |
| Veber66 | 2010 | 77 Cisgender men and women | Fat grafting to calf |
| Chugay55 | 2011 | 18 Cisgender women | Implants to thigh |
| Hurwitz50 | 2012 | 17 Cisgender women | Liposuction of thigh |
| Aboueldahab53 | 2013 | 25 Cisgender women | Liposuction of inner thigh |
| Hoppmann65 | 2013 | 3 Cisgender women, 2 cisgender men | Fat grafting to calf |
| Karacaoglu69 | 2013 | 20 Cisgender women, 2 cisgender men | Implants to calf; fat grafting to calf |
| Zelickson47 | 2015 | 42 Cisgender women | Cryotherapy to inner thigh |
| Gusenoff78 | 2016 | 19 Cisgender women, 6 cisgender men | Fat grafting to foot |
| Mundinger68 | 2016 | 10 Cisgender women, 3 cisgender men | Fat grafting to calf |
| Bogari57 | 2017 | 18 Cisgender women | Botulinum injection to calf |
| Niechajev62 | 2017 | 31 Cisgender women, 19 cisgender men | Implants to calf |
| Skorobac67 | 2017 | 48 Cisgender women | Fat grafting to calf |
| Klaver43 | 2018 | 179 Transgender women, 162 transgender men | Hormone therapy |
| Minteer77 | 2018 | 23 Cisgender women, 8 cisgender men | Fat grafting to foot |
| Wanitphakdeedecha58 | 2018 | 22 Cisgender women | Botulinum injection to calf |
| Farber76 | 2019 | 23 Cisgender men and women | Fat grafting to foot |
| Melita64 | 2019 | 13 Cisgender women, 33 cisgender men | Implants to calf |
Masculine and feminine qualities of the LE
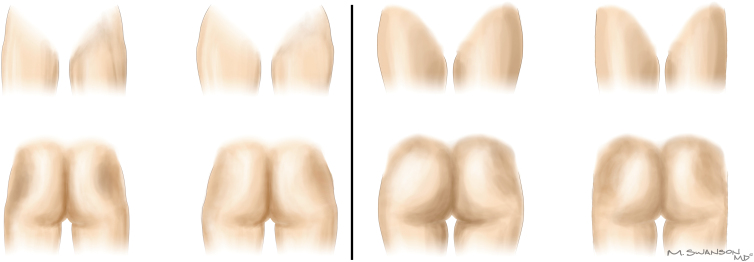
The LE is a highly sexually dimorphic region (Fig. 2). The male LE extends essentially in a straight vertical line from hip to ankle, while the female leg is angled slightly valgus from hip to knee.3,4 The female LE also features a medial convexity that spans from the groin to the ankle.4 The difference in shape is in part created by bony differences, such as a wider pelvis and more angled femurs in females, and also in part due to differences in fat and muscle distribution.
FIG. 2.
Ideal male and female LE. Diagram of idealized masculine and feminine LE. Masculine characteristics include an overall straight contour of the leg from hip to ankle, increased muscularity and decreased subcutaneous fat (left). Feminine characteristics include a slight valgus orientation of the thigh, with increased subcutaneous fat, especially in the buttocks, hips, and thigh regions (right). LE, lower extremity.
In general, the male LE has increased muscle mass and less subcutaneous fat than the female LE.5–8 Women tend to deposit fat in areas such as the iliac crests, trochanteric region, and superior medial thigh over the adductor muscles.4 Men typically do not have significant LE fat deposits.4 Women are more prone to cellulite in the LE, due to increased superficial fat deposits and the presence of fewer but larger subcutaneous fat lobules in females even at equal body mass index.9,10 Women also typically have increased propensity for varicose veins.11,12
Of note, there has recently been increased diversity in what body proportions are considered to be “ideal.” Particularly, increased media presence and acceptance of fuller buttocks and thighs in women has been noted. Variety in ideal male body proportions of the LE also exists, for example between muscular athletes and fashion models, while both may be considered “ideal.”13,14 Therefore, esthetic ideals for the LE in transgender and nonbinary patients are multifactorial.15
Hips and buttocks
Transgender men and women both have relatively high levels of gender dysphoria attached to their hips and buttocks, although transgender men tend to be more dissatisfied than transgender women.1
Several features of an attractive buttock are relatively sex independent. These include a curved infragluteal fold, maximum projection between the middle and upper thirds, and absence of ptosis below the infragluteal crease.6,16
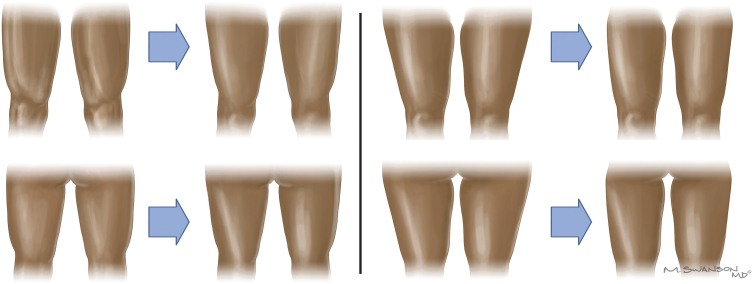
The ideal female buttock is rounder and fuller at the mid- and lower-lateral regions, lacks a lateral convexity, and has a short intergluteal fold, which results in increased buttock separation both superiorly and inferiorly (Fig. 3).6,16,17 The area immediately above the intergluteal crease also features a prominent divot in females termed the “Michaelis rhomboid.”4 The ideal male buttock is characterized by a flatness or concavity of the mid-lateral buttock and relative absence of lateral hip fullness.6
FIG. 3.
Masculinization and feminization of the buttock and hip. Diagram showing feminization of masculine buttocks and hips from anterior and posterior views (left); as well as masculinization of feminine buttocks and hips from anterior and posterior views (right).
Hips also differ between sexes, with women having wider hips as a result both of a wider bony pelvis and of increased fatty deposition. Typical ranges for waist-to-hip ratio (WHR) are 0.65–0.8 in premenopausal women and 0.85–0.96 in men.6 Ideal WHR is around 0.9 in men and 0.7 in women, with significant variability between studies and regions.18–22
Thigh
The female thigh is characterized by a medial longitudinal convexity that results from an angled femur and also proportionally more prominent lateral than medial musculature (Fig. 4).23
FIG. 4.
Masculinization and feminization of the thigh. Diagram showing feminization of masculine thighs from anterior and posterior views (left); as well as masculinization of feminine thighs from anterior and posterior views (right).
The ideal feminine thigh size should be considered in proportion to the buttocks. The angle of the thigh–buttock junction viewed posteriorly is ideally around 170°.24 When viewed laterally, the thigh is ideally 0.7 or 0.8 times the anterior–posterior length of the buttock.24
In contrast, the male thigh is characterized by increased muscle mass and decreased subcutaneous fat.25,26 Desired proportions and level of muscular development may vary considerably between patients. However, the ideal thigh circumference has been described as ∼1.47 times that of the calf, 0.60 times that of the hips, and 0.53 times that of the chest.13,27
Knee, leg, and ankle
The knee is a site of cosmetic concern, particularly among women. Ideally, bony landmarks of the knee should be visible, if permitted by the patient's body habitus. Fat deposition in a number of areas can limit this. For example, fat deposits superior to the patella can create an unsightly “upside-down banana” appearance, and fat deposits flanking the knee, along the upper medial leg and the lateral ankle can create “tubular” legs.28 Similar esthetic ideals of the knee hold true for men, however, men typically do not carry enough fat in this area for it to be a common esthetic concern.
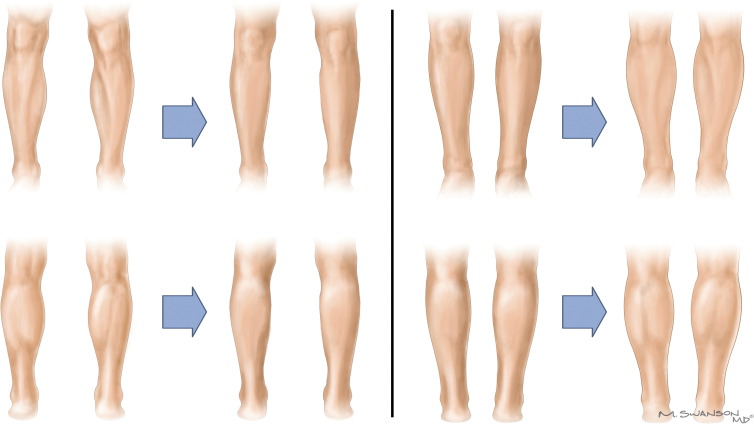
A particular contour of an ideal calf has been described, consistent between sexes (Fig. 5).3 Medially, a convexity spans the upper half of the leg, while a concavity spans the lower half. Viewed laterally, a posterior convexity spans the upper two thirds, while a concavity spans the lower third. The widest anteroposterior and lateral projection of the calf should present at the junction of the proximal and middle thirds of the leg.29
FIG. 5.
Masculinization and feminization of the leg, knee, and ankle. Diagram showing feminization of masculine leg, knee, and ankle from anterior and posterior views (left); as well as masculinization of feminine leg, knee, and ankle from anterior and posterior views (right).
The calf is more muscular and less fatty in men than in women.28,30 For both sexes, a calf that is ∼1.62 times the circumference of the ankle is traditionally considered esthetic.27 However, some males may also prefer larger, stronger-appearing calves (approximately the same circumference as the flexed bicep is considered aesthetic by bodybuilders).27 In women, and especially in certain demographic groups, such as subsets of Asian women, a small calf that affords a straight medial leg contour may be considered more desirable.31
Foot
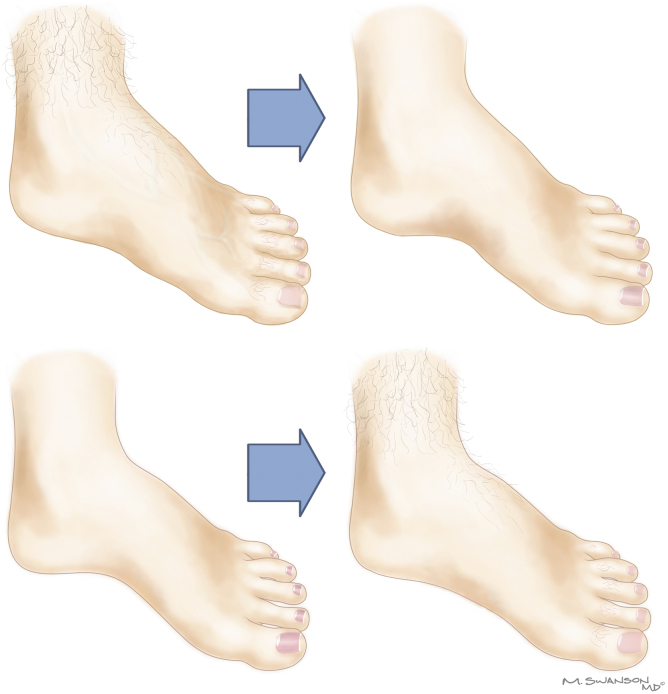
Feet are also sexually dimorphic.32,33 Men tend to have wider and longer feet, and wider ankles as well (Fig. 6).34–36 In contrast, high arches can lend a feminine appearance to the foot, although it is unclear whether women actually tend to have higher arches.37–42
FIG. 6.
Masculinization and feminization of the foot. Diagram showing feminization of masculine foot (upper); as well as masculinization of feminine foot (lower).
Feminizing and masculinizing techniques for the LE
As evidenced by our literature review, no surgical literature exists detailing outcomes of GAS of the LE. Therefore, this discussion of gender-affirming techniques for the LE will largely be an application of existing medical and surgical treatments aimed toward bringing patients' lower extremities more in line with the esthetic norms and ideals discussed above.
Nonsurgical techniques for masculinization and feminization of the LE
Nonsurgical techniques involve hormone therapy as well as minimally invasive treatments typically indicated for improved cosmesis in cisgender patients.
Hormone therapy has demonstrated efficacy in both feminization and masculinization of the LE.43,44 Patients who seek LE GAS will likely have had some amount of hormone therapy. After 1 year on hormone therapy, transgender women can expect increased subcutaneous fat deposition, particularly in the leg and gynoid regions, as well as a decreased WHR, largely from increased hip circumference.43 In contrast, testosterone therapy reduces subcutaneous fat in the leg and gynoid region, decreases hip circumference, and slightly increases WHR.43,45
Noninvasive body contouring techniques may be used strategically to achieve a more masculine or feminine LE. Fatty tissue volume reduction can be achieved by radiofrequency, mechanical forces, ultrasound, lasers, thermal energy, although evidence levels are limited, and generally only a modest change in circumference is observed.46,47 Various nonsurgical hair removal techniques may also be utilized to feminize the LE.
Surgical techniques for masculinization and feminization of the LE
Cosmetic and reconstructive techniques, such as liposuction, fat grafting, and implants, may be used in various combinations for LE GAS.48
Hips and buttocks
Traditionally speaking, feminization of the LE will likely involve augmentation of the hips and/or buttocks, while masculinization of the LE will likely involve reduction of these areas. Details of hip and buttocks techniques for transgender patients have been described in detail elsewhere, but we provide a brief overview6:
Fat grafting to the buttocks can achieve a more feminine appearance, especially if volume is preferentially added to areas of typical gynoid fat distribution, including the mid-lateral buttock convexity, lateral thighs, and hips.6 Buttock implants and the so-called “Brazilian Butt Lift” may also provide desired gluteal augmentation, however, these procedures are associated with significant complications.49
Masculinization of the hips and buttocks should aim to increase the WHR toward male ranges, and/or to contour the buttocks and thighs into a more typically male shape. Liposuction or noninvasive body contouring of the hips may help to reduce the WHR by decreasing hip size.48 Targeted liposuction of the lower lateral buttock may recreate a masculine separation between the buttocks and hip. Additionally, targeting of cellulite may also help to masculinize the thigh.
Thigh
Hormone therapy may sufficiently alter fatty deposition and musculature of the thigh for some patients. Others may desire further intervention. The best-established techniques for the thigh are reductive and include liposuction and thigh lift.
Liposuction to the thigh can reduce stereotypically feminine fat deposition in the lateral thigh.50 In transgender men, the technique may be similar to the analogous procedure in cisgender women, but with a more pronounced end esthetic result as transgender men will likely desire further fatty reduction.
Another reductive option is the medial thigh lift, with or without liposuction, which has traditionally been used in bariatric patients and those with excessive medial thigh skin laxity.51–53 This procedure may play a role for transgender men with thigh laxity. However, complication rates are very high (43%, according to a recent review).54
Feminization of the thigh involves augmentation of the lateral thigh to create an hourglass figure. As with other body regions, augmentation with fat grafting and/or implants can be considered, although these are typically not performed. Fat grafting to the thigh is typically not performed due to the large volume of fat that would be required to significantly augment such a large region of the body. Lateral thigh augmentation through implant is also not typically attempted, although a very small cohort does exist of cisgender women undergoing placement of a silicone implant into a plane beneath the tensor fascia lata.55 All women reported high satisfaction and no major complications were confirmed.
Knee, leg, and ankle
Desired calf esthetics may vary considerably between patients of similar gender identity. Nonetheless, feminization generally may be achieved by reducing the muscular appearance of the calf, and masculinization may be achieved by enhancing the appearance of musculature.
Liposuction to the calf can decrease its size, which is feminizing.48 In liposuction of the leg and ankle, special care must be taken to avoid the saphenous veins and sural nerve, which lie in the subcutaneous plane of liposuction.56 Additionally, the fat of the medial leg is typically softer compared with the lateral subcutaneous fat, and force used during canalization should be modified accordingly.56
Modest calf size reduction may also be achieved through botulinum toxin injection, which induces gastrocnemius atrophy, although this procedure needs to be repeated frequently.57,58 Proper technique causes only nominally decreased calf strength and does not meaningfully affect gait. More invasive techniques, such as total gastrocnemius resection and sural nerve resection, have been reported for large-volume cosmetic calf reduction in cisgender women, but these are likely impractical due to relative morbidity.59–61
Calf augmentation, which may be masculinizing due to the appearance of increased muscular volume, may be accomplished by fat grafting and/or implants.
Calf implants may be symmetric or cigar shaped, and asymmetric or anatomic.29,62,63 They may be placed in subfascial or submuscular (between the soleus and gastrocnemius) planes. Complication rates are relatively low, but are higher for subfascial implants (5.7%) than submuscular (0.92%).64 Reported complications of subfascial implants include seroma (2%), migration (0.8% vs. 0.2% in submuscular placement), dehiscence (0.6% vs. 0.2%), and infection (0.3%); patients likely should also be monitored for compartment syndrome.64
Fat grafting to the calf can provide more modest increases in calf size.65–68 Fat may be injected intramuscularly or subcutaneously.67 Rates of fat resorption appear to be low, at least to 6 months follow-up.67 Complications are rare (around 1.5%), most commonly including hyperpigmented scar formation (1%) and hypoesthesia (0.4%), without any major complications being reported for these procedures.64,69
Liposuction of the knee has also been described in cisgender women, and may create a less characteristically feminine leg shape for transgender men.28 Fatty deposits of the superior, medial, and lateral knees may be targeted. This technique should be performed in a plane tangential to the joint capsule and may require multiple incisions to do so. Similarly, liposuction of the ankle may be performed, targeting four typical areas of fat deposition: anteriorly over the lateral and medial malleolus, and posteriorly on either side of the Achilles' tendon.56,70,71
Foot
Cosmetic foot surgery is typically not advocated by professional societies due to relatively high risk for morbidity related to mobility and foot function.72–74 However, no professional societies have released position statements regarding gender-affirming foot surgery.1 Feminization will most commonly depend on relatively noninvasive methods like skin treatments, chemical peels, hair removal, and grooming.75–78
Discussion
As evidenced by our systematic literature search, there is currently no primary academic plastic surgery literature detailing gender-affirming surgery of the LE. However, as is true for all of surgery, practice precedes evidence. Therefore, this discussion is largely a consideration of adaptations of familiar cosmetic and reconstructive techniques for use in transgender patients. Such adaptations will likely require special technical and esthetic considerations.
For example, transgender men may desire a greater degree of thigh reduction through liposuction than cisgender women would, due to the esthetic ideals of male versus female legs (male legs being less fatty, generally). Similarly, a transgender woman undergoing hip or buttocks augmentation may require a greater degree of augmentation to achieve the same end cosmesis, since transgender women will likely start with a smaller bony and soft tissue architecture to the hip preoperatively than cisgender women would. However, further outcomes-based study is required to determine whether these technical adaptations are safe and/or effective.
The role of LE GAS will likely be different for each patient, depending on their body habitus, gender identity, and specific areas that contribute most to their gender dysphoria. The timing of LE GAS relative to other forms of GAS (genital, facial, and breast/chest) will also vary. However, transmasculine patients should be counseled that reductive manipulation of the thigh through liposuction may preclude anterolateral thigh (ALT) flap phalloplasty in some cases. For these patients, alternatives such as radial forearm free flap should be considered. ALT phalloplasty donor-site closure may also slightly reduce the width of the thigh, which may address dysphoric thigh width, but also will likely result in a slightly asymmetric outcome that may require contralateral reduction for balancing.
Additionally, as is the case for most other domains of GAS, the effects of hormone therapy on long-term outcomes of LE masculinization and feminization are unknown. There exists no algorithm for timing of LE surgery after hormones. Most transgender patients will see significant changes in body composition after about 1 year of hormone therapy.43 For this reason, it is generally recommended that any transgender body contouring surgery be deferred until hormones are administered for at least 1 year. However, it is unclear whether fatty and muscular changes stabilize after this period, or if changes will continue. It is therefore difficult to make informed medical and surgical algorithms regarding optimal LE masculinization and feminization.
Further expansion our methods to include additional primary literature, review articles, and nonacademic literature augmented our systematic search. Therefore, our review of LE techniques as applicable to gender affirmation is not exhaustive. Throughout, we have cited high-quality review articles, which will provide readers with a more comprehensive understanding of applicable techniques than what could be provided within the scope of this review.
Conclusion
Despite the highly sexually dimorphic nature of the lower extremities and their documented contribution to gender dysphoria, no literature exists regarding outcomes of gender-affirming procedures for this region. Therefore, feminization and masculinization of the lower extremities will rely on application of an array of existing plastic surgery techniques to achieve the ideal thigh, knee, leg, and ankle contours of a patient's identified gender. Techniques, such as lipocontouring, fat augmentation, and soft tissue rearrangement, may be used to achieve a more “hourglass” figure in transfeminine patients or straighter, more muscular legs in transmasculine patients. However, lack of studies providing outcomes evidence of gender-affirming surgery to the LE limits conclusions.
Supplementary Material
Abbreviations Used
- ALT
anterolateral thigh
- GAS
gender affirmation surgery
- LE
lower extremity
- WHR
waist-to-hip ratio
Authors' Contributions
Each listed author contributed significantly to this article. Specific tasks for each author include: I.T.N.: Conceptualization, literature search, data analysis, and article preparation. E.S.: Conceptualization, literature search, data analysis, and article preparation. M.S.: Conceptualization, article preparation, and figure preparation. S.D.M.: Conceptualization and article preparation. A.H.: Conceptualization and article preparation.
Author Disclosure Statement
None of the authors has any relevant conflicts of interest.
Funding Information
No funding was provided for this study.
Supplementary Material
Cite this article as: Nolan IT, Shepard E, Swanson M, Morrison SD, Hazen A (2023) Techniques and applications of lower extremity feminization and masculinization, Transgender Health 8:1, 45–55, DOI: 10.1089/trgh.2020.0178.
References
- 1. van de Grift TC, Cohen-Kettenis PT, Steensma TD, et al. Body satisfaction and physical appearance in gender dysphoria. Arch Sex Behav. 2016;45:575–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lee J, Nolan IT, Swanson M, et al. A review of hand feminization and masculinization techniques in gender affirming therapy. Aesthetic Plast Surg. 2021;45:589–601. [DOI] [PubMed] [Google Scholar]
- 3. Benslimane F. The Benslimane's artistic model for leg beauty. Aesthetic Plast Surg. 2012;36:803–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Martin MC. Comprehensive liposuction of lower limbs: basic concepts. Aesthetic Plast Surg. 1996;20:49–52. [DOI] [PubMed] [Google Scholar]
- 5. McLean SP, Hinrichs RN. Sex differences in the centre of buoyancy location of competitive swimmers. J Sports Sci. 1998;16:373–383. [DOI] [PubMed] [Google Scholar]
- 6. Morrison SD, Wilson SC, Mosser SW. Breast and body contouring for transgender and gender nonconforming individuals. Clin Plast Surg. 2018;45:333–342. [DOI] [PubMed] [Google Scholar]
- 7. Coleman KM, Lawrence N. Male body contouring. Dermatol Surg. 2017;43(Suppl 2):S188–S193. [DOI] [PubMed] [Google Scholar]
- 8. Van Caenegem E, Wierckx K, Taes Y, et al. Body composition, bone turnover, and bone mass in trans men during testosterone treatment: 1-year follow-up data from a prospective case-controlled study (ENIGI). Eur J Endocrinol. 2015;172:163–171. [DOI] [PubMed] [Google Scholar]
- 9. Rudolph C, Hladik C, Hamade H, et al. Structural gender dimorphism and the biomechanics of the gluteal subcutaneous tissue: implications for the pathophysiology of cellulite. Plast Reconstr Surg. 2019;143:1077–1086. [DOI] [PubMed] [Google Scholar]
- 10. Cotofana S, Hexsel D, Avelar LE, et al. Calculating the thickness of the superficial fatty layer of the body using age, gender, and body mass index. J Drugs Dermatol. 2020;19:36–44. [DOI] [PubMed] [Google Scholar]
- 11. Maurins U, Hoffmann BH, Losch C, et al. Distribution and prevalence of reflux in the superficial and deep venous system in the general population—results from the Bonn Vein Study, Germany. J Vasc Surg. 2008;48:680–687. [DOI] [PubMed] [Google Scholar]
- 12. Ruckley CV, Evans CJ, Allan PL, et al. Telangiectasia in the Edinburgh Vein Study: epidemiology and association with trunk varices and symptoms. Eur J Vasc Endovasc Surg. 2008;36:719–724. [DOI] [PubMed] [Google Scholar]
- 13. Butt C. Your Muscular Potential: How to Predict Your Maximum Muscular Body Weight and Measurements, 4th ed. Washington, DC: Myogenic Enterprises, 2009. [Google Scholar]
- 14. Swami V, Tovee MJ. Does hunger influence judgments of female physical attractiveness? Br J Psychol. 2006;97:353–363. [DOI] [PubMed] [Google Scholar]
- 15. Abu-Ghname A, Patel V, Davis MJ, et al. Does portrayal of skin tone in gender-affirming literature represent diversity? LGBT Health. 2020;7:461–463. [DOI] [PubMed] [Google Scholar]
- 16. Richter DF, Stoff A. Circumferential body contouring: the lower body lift. Clin Plast Surg. 2014;41:775–788. [DOI] [PubMed] [Google Scholar]
- 17. Bank J, Teplica D. Anatomy of flank adipose: the Y configuration and hip extension and their effects on the perception of gender. Plast Reconstr Surg. 2020;146:836e–838e. [DOI] [PubMed] [Google Scholar]
- 18. Singh D. Female judgment of male attractiveness and desirability for relationships: role of waist-to-hip ratio and financial status. J Pers Soc Psychol. 1995;69:1089–1101. [DOI] [PubMed] [Google Scholar]
- 19. Sorokowski P, Sorokowska A. Judgments of sexual attractiveness: a study of the Yali tribe in Papua. Arch Sex Behav. 2012;41:1209–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Singh D. Waist-to-hip ratio and judgment of attractiveness and healthiness of female figures by male and female physicians. Int J Obes Relat Metab Disord. 1994;18:731–737. [PubMed] [Google Scholar]
- 21. Heidekrueger PI, Sinno S, Tanna N, et al. The ideal buttock size: a sociodemographic morphometric evaluation. Plast Reconstr Surg. 2017;140:20e–32e. [DOI] [PubMed] [Google Scholar]
- 22. Sorokowski P, Sorokowska A, Mberira M. Are preferences for legs length universal? Data from a semi-nomadic Himba population from Namibia. J Soc Psychol. 2012;152:370–378. [DOI] [PubMed] [Google Scholar]
- 23. Behan FP, Maden-Wilkinson TM, Pain MTG, Folland JP. Sex differences in muscle morphology of the knee flexors and knee extensors. PLoS One. 2018;13:e0190903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vartanian E, Gould DJ, Hammoudeh ZS, et al. The ideal thigh: a crowdsourcing-based assessment of ideal thigh aesthetic and implications for gluteal fat grafting. Aesthet Surg J. 2018;38:861–869. [DOI] [PubMed] [Google Scholar]
- 25. Maughan RJ, Watson JS, Weir J. Strength and cross-sectional area of human skeletal muscle. J Physiol. 1983;338:37–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Otsuka S, Yakura T, Ohmichi Y, et al. Site specificity of mechanical and structural properties of human fascia lata and their gender differences: a cadaveric study. J Biomech. 2018;77:69–75. [DOI] [PubMed] [Google Scholar]
- 27. Willoughby DP, Weaver GR. The Complete Guide to Muscular Measurements. Los Angeles, CA: Weider Publications, 1947. [Google Scholar]
- 28. Chamosa M. Liposuction of the kneecap area. Plast Reconstr Surg. 1997;99:1433–1436; discussion 1437–1438. [DOI] [PubMed] [Google Scholar]
- 29. Cuenca-Guerra R, Daza-Flores JL, Saade-Saade AJ. Calf implants. Aesthetic Plast Surg. 2009;33:505–513. [DOI] [PubMed] [Google Scholar]
- 30. Sherk VD, Thiebaud RS, Chen Z, et al. Associations between pQCT-based fat and muscle area and density and DXA-based total and leg soft tissue mass in healthy women and men. J Musculoskelet Neuronal Interact. 2014;14:411–417. [PMC free article] [PubMed] [Google Scholar]
- 31. Tsai CC, Lin SD, Lai CS, Lin TM. Aesthetic analysis of the ideal female leg. Aesthetic Plast Surg. 2000;24:303–305. [DOI] [PubMed] [Google Scholar]
- 32. Şaylı U, Altunok EC, Guven M, et al. Prevalence estimation and familial tendency of common forefoot deformities in Turkey: a survey of 2662 adults. Acta Orthop Traumatol Turc. 2018;52:167–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Coughlin MJ, Dorris J, Polk E. Operative repair of the fixed hammertoe deformity. Foot Ankle Int. 2000;21:94–104. [DOI] [PubMed] [Google Scholar]
- 34. Ahmed AA. A study of correlations within the dimensions of lower limb parts for personal identification in a Sudanese population. ScientificWorldJournal. 2014;2014:541408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Krauss I, Grau S, Mauch M, et al. Sex-related differences in foot shape. Ergonomics. 2008;51:1693–1709. [DOI] [PubMed] [Google Scholar]
- 36. Voracek M, Fisher ML, Rupp B, et al. Sex differences in relative foot length and perceived attractiveness of female feet: relationships among anthropometry, physique, and preference ratings. Percept Mot Skills. 2007;104:1123–1138. [DOI] [PubMed] [Google Scholar]
- 37. Tomassoni D, Traini E, Amenta F. Gender and age related differences in foot morphology. Maturitas. 2014;79:421–427. [DOI] [PubMed] [Google Scholar]
- 38. Aenumulapalli A, Kulkarni MM, Gandotra AR. Prevalence of flexible flat foot in adults: a cross-sectional study. J Clin Diagn Res. 2017;11:AC17–AC20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sanchez Rodriguez R, Martinez Nova A, Escamilla Martinez E, et al. The foot posture index: anthropometric determinants and influence of sex. J Am Podiatr Med Assoc. 2013;103:400–404. [DOI] [PubMed] [Google Scholar]
- 40. Zifchock RA, Davis I, Hillstrom H, Song J. The effect of gender, age, and lateral dominance on arch height and arch stiffness. Foot Ankle Int. 2006;27:367–372. [DOI] [PubMed] [Google Scholar]
- 41. Zhao X, Gu Y, Yu J, et al. The influence of gender, age, and body mass index on arch height and arch stiffness. J Foot Ankle Surg. 2020;59:298–302. [DOI] [PubMed] [Google Scholar]
- 42. Voracek M, Dressler SG. Relationships of toe-length ratios to finger-length ratios, foot preference, and wearing of toe rings. Percept Mot Skills. 2010;110:33–47. [DOI] [PubMed] [Google Scholar]
- 43. Klaver M, de Blok CJM, Wiepjes CM, et al. Changes in regional body fat, lean body mass and body shape in trans persons using cross-sex hormonal therapy: results from a multicenter prospective study. Eur J Endocrinol. 2018;178:163–171. [DOI] [PubMed] [Google Scholar]
- 44. Klaver M, Dekker M, de Mutsert R, et al. Cross-sex hormone therapy in transgender persons affects total body weight, body fat and lean body mass: a meta-analysis. Andrologia. 2017;49:5. [DOI] [PubMed] [Google Scholar]
- 45. Wiik A, Lundberg TR, Rullman E, et al. Muscle strength, size, and composition following 12 months of gender-affirming treatment in transgender individuals. J Clin Endocrinol Metab. 2020;105:3. [DOI] [PubMed] [Google Scholar]
- 46. Nassab R. The evidence behind noninvasive body contouring devices. Aesthet Surg J. 2015;35:279–293. [DOI] [PubMed] [Google Scholar]
- 47. Zelickson BD, Burns AJ, Kilmer SL. Cryolipolysis for safe and effective inner thigh fat reduction. Lasers Surg Med. 2015;47:120–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bellini E, Grieco MP, Raposio E. A journey through liposuction and liposculture: review. Ann Med Surg (Lond). 2017;24:53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Asserson DB, Kulinich AG, Orbay H, et al. Differences in complication rates of gluteoplasty procedures that utilize autologous fat grafting, implants, or local flaps. Ann Plast Surg. 2019;82:S342–s344. [DOI] [PubMed] [Google Scholar]
- 50. Hurwitz D, Smith D. Treatment of overweight patients by radiofrequency-assisted liposuction (RFAL) for aesthetic reshaping and skin tightening. Aesthetic Plast Surg. 2012;36:62–71. [DOI] [PubMed] [Google Scholar]
- 51. Bertheuil N, Carloni R, De Runz A, et al. Medial thighplasty: current concepts and practices. Ann Chir Plast Esthet. 2016;61:e1–e7. [DOI] [PubMed] [Google Scholar]
- 52. Michaels J. Vertical medial thigh contouring. Clin Plast Surg. 2019;46:91–103. [DOI] [PubMed] [Google Scholar]
- 53. Aboueldahab AK. Liposuction-assisted medial thigh lift in obese and non obese patients. J Cutan Aesthet Surg. 2013;6:217–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Sisti A, Cuomo R, Zerini I, et al. Complications associated with medial thigh lift: a comprehensive literature review. J Cutan Aesthet Surg. 2015;8:191–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Chugay NV, Chugay PN. Thigh augmentation: giving the average woman curves in the right places. Am J Cosmet Surg. 2011;28:255–260. [Google Scholar]
- 56. Weniger FG, Calvert JW, Newton ED. Liposuction of the legs and ankles: a review of the literature. Plast Reconstr Surg. 2004;113:1771–1785. [DOI] [PubMed] [Google Scholar]
- 57. Bogari M, Tan A, Xin Y, et al. Treatment of gastrocnemius muscle hypertrophy with botulinum toxin injection followed by magnetic resonance imaging assessment and 3-dimensional evaluation. Aesthet Surg J. 2017;37:1146–1156. [DOI] [PubMed] [Google Scholar]
- 58. Wanitphakdeedecha R, Ungaksornpairote C, Kaewkes A, et al. A pilot study comparing the efficacy of two formulations of botulinum toxin type A for muscular calves contouring. J Cosmet Dermatol. 2018;17:984–990. [DOI] [PubMed] [Google Scholar]
- 59. Lee JT, Wang CH, Cheng LF, et al. Subtotal resection of gastrocnemius muscles for hypertrophic muscular calves in Asians. Plast Reconstr Surg. 2006;118:1472–1483. [DOI] [PubMed] [Google Scholar]
- 60. Lemperle G, Exner K. The resection of gastrocnemius muscles in aesthetically disturbing calf hypertrophy. Plast Reconstr Surg. 1998;102:2230–2236. [DOI] [PubMed] [Google Scholar]
- 61. Kim SC, Kang MH, Ock JJ. Calf-contouring surgery of gastrocnemius hypertrophy: selective neurectomy of the sural nerve. Aesthetic Plast Surg. 2008;32:889–893. [DOI] [PubMed] [Google Scholar]
- 62. Niechajev I, Krag C. Calf augmentation and restoration: long-term results and the review of the reported complications. Aesthetic Plast Surg. 2017;41:1115–1131. [DOI] [PubMed] [Google Scholar]
- 63. von Szalay L. Calf augmentation: a new calf prosthesis. Plast Reconstr Surg. 1985;75:83–87. [DOI] [PubMed] [Google Scholar]
- 64. Melita D, Innocenti A. Surgical calf augmentation techniques: personal experience, literature review and analysis of complications. Aesthetic Plast Surg. 2019;43:973–979. [DOI] [PubMed] [Google Scholar]
- 65. Hoppmann R, Meruane M, Gonzalez D, et al. Calf lipo-reshaping. J Plast Reconstr Aesthet Surg. 2013;66:956–961. [DOI] [PubMed] [Google Scholar]
- 66. Veber M Jr., Mojallal A. Calf augmentation with autologous tissue injection. Plast Reconstr Surg. 2010;125:423–424; author reply 424–425. [DOI] [PubMed] [Google Scholar]
- 67. Skorobac AV, Sopta J. Lower leg augmentation with fat grafting, MRI and histological examination. Aesthetic Plast Surg. 2017;41:108–116. [DOI] [PubMed] [Google Scholar]
- 68. Mundinger GS, Vogel JE. Calf augmentation and reshaping with autologous fat grafting. Aesthet Surg J. 2016;36:211–220. [DOI] [PubMed] [Google Scholar]
- 69. Karacaoglu E, Zienowicz RJ, Balan I. Calf contouring with endoscopic fascial release, calf implant, and structural fat grafting. Plast Reconstr Surg Glob Open. 2013;1:e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Serdev NP. Lower Body and Extremities Sculpting, Beautification, Changing of Proportions, Body Contouring and Sculpting. London, UK: IntechOpen, 2016. [Google Scholar]
- 71. Chamosa M. Suction lipectomy of the ankle area. Plast Reconstr Surg. 1997;100:1047–1052; discussion 1053. [DOI] [PubMed] [Google Scholar]
- 72. American College of Foot and Ankle Surgeons. ACFAS position statement on cosmetic surgery. 2020. Available at: https://www.acfas.org.Policy-Statements Accessed June 15, 2020.
- 73. American Orthopedic Foot and Ankle Society. Position Statement: Cosmetic Foot and Ankle Surgery. Available at: https://www.aofas.org/docs/default-source/research-and-policy/position-statement-cosmetic-foot-and-ankle-surgery.pdf?sfvrsn=c416380b_4 Accessed June 15, 2021.
- 74. American Podiatric Medical Association. Position statements: cosmetic foot surgery. 2014. Available at: https://www.apma.org/Media/position.cfm?ItemNumber=996 Accessed June 15, 2021.
- 75. Lipner SR, Scher RK. Onychomycosis: treatment and prevention of recurrence. J Am Acad Dermatol. 2019;80:853–867. [DOI] [PubMed] [Google Scholar]
- 76. Farber SE, Minteer D, Gusenoff BR, Gusenoff JA. The influence of fat grafting on skin quality in cosmetic foot grafting: a randomized, cross-over clinical trial. Aesthet Surg J. 2019;39:405–412. [DOI] [PubMed] [Google Scholar]
- 77. Minteer DM, Gusenoff BR, Gusenoff JA. Fat grafting for pedal fat pad atrophy in a 2-year, prospective, randomized, crossover, single-center clinical trial. Plast Reconstr Surg. 2018;142:862e–871e. [DOI] [PubMed] [Google Scholar]
- 78. Gusenoff JA, Mitchell RT, Jeong K, et al. Autologous fat grafting for pedal fat pad atrophy: a prospective randomized clinical trial. Plast Reconstr Surg. 2016;138:1099–1108. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.