Abstract
Pre-migration trauma, a psychological risk factor for refugees, is often measured using cumulative indices. However, recent research suggests that trauma subtypes, rather than cumulative trauma, may better predict psychological outcomes. This study investigated the predictive utility of trauma subtypes in the assessment of refugee mental health. Multiple regression was used to determine whether cumulative trauma or trauma subtypes explained more variance in depression, anxiety, and post-traumatic stress disorder (PTSD) symptom scores in 70 Syrian and Iraqi refugees. Subtype models performed better than cumulative trauma models for PTSD (cumulative R2 = 0.138; subtype R2 = 0.32), anxiety (cumulative R2 = 0.061; subtypeR2 = 0.246), and depression (cumulative R2 = 0.041; subtype R2 = 0.184). Victimization was the only subtype significantly associated with PTSD (p < 0.001; r2 = 0.210), anxiety (p < 0.001; r2 = 0.162), and depression (p = 0.002; r2 = 0.140). Cumulative trauma was predictive of PTSD symptoms only (p = 0.003; r2 = 0.125). Trauma subtypes were more informative than cumulative trauma, indicating their utility for improving predictive efforts in research and clinical contexts.
Keywords: Refugees, Trauma, PTSD, Anxiety, Depression
Introduction
Natural disasters and war frequently lead to forced migration. For persons who resettle as refugees, conflict prior to flight, the experience of flight itself, and difficulties finding support in host countries often contribute to unique and potentially traumatic experiences [1, 2].
Previous research has indicated that persons resettled as refugees may have an increased risk of mental health disorders, including post-traumatic stress disorder (PTSD), depression, and anxiety [3, 4]. Additionally, trauma prior to fleeing one’s homeland (e.g., physical assault, persecution) [2, 5] is a contributing factor to this risk [1, 2].
Generally, research in this area utilizes cumulative measures such as the Life Events Checklist of the DSM-5 (LEC-5) [6] to assess for trauma [6, 7]. Such measures typically consist of items probing the presence or absence of a series of potentially traumatic events (PTEs), with total number of traumas endorsed constituting a cumulative trauma score. Recent findings, however, suggest that trauma subtypes (e.g., interpersonal traumas, accidental traumas), rather than number of trauma exposures, may better predict psychological outcomes [5, 8]. As such, relying exclusively on cumulative trauma measures may “flatten” trauma experiences and mask meaningful effects. For instance, general population studies have found that sexual assault has a greater negative impact on self-perception [9] and emotional regulation [10] than other traumas, such as physical assault or loss of a loved one.
Research in refugee populations has yielded similar results [5, 11]. Kira et al. found differences in the effect of certain trauma subtypes on four dimensions of PTSD symptoms in Iraqi refugee adolescents. Here, sexual abuse was positively associated with arousal and re-experiencing symptoms, while having a parent involved in war was associated with detachment/dissociation and had a negative effect on arousal [11]. Likewise, torture has been associated with higher PTSD symptoms for refugees than exposure to other trauma types (e.g., war exposure) [12]. Arnetz et al. used exploratory factor analysis (EFA) to identify five trauma subtypes within the Harvard Trauma Questionnaire (HTQ), with the single subtype “physical trauma to self” explaining more variance in PTSD symptoms for Iraqi refugees than the cumulative HTQ score [5]. Thus, consideration of trauma subtypes may provide better insight into the impact of trauma on psychopathology and improve early identification of those at high risk—potentially informing personalized treatment.
Using EFA to identify subtypes of trauma in cumulative measures, however, is problematic due to the assumptions of factor analysis [13, 14]. Latent variable models, the theoretical basis for factor analysis, assume the existence of a variable that cannot be measured directly, but rather is inferred from a set of observed indicators. For instance, depression cannot be directly quantified; instead, a series of scale items probe the presence or absence of observable indicators (i.e., sleep changes, hopelessness) that are caused by depression (i.e., the latent construct). Applying this model to trauma measurement would require that various trauma exposures were caused by some underlying latent construct—in this instance, the trauma subtype. This is not logical, as experiencing one instance (e.g., exposure to toxic substance) of a trauma subtype (e.g., death threat trauma) does not necessarily cause other instances (e.g., being threatened with a weapon) of that trauma subtype. Latent variable models, therefore, are not compatible with the classification of trauma subtypes [13, 14]. While results from such analyses provide a foundation for further investigation, more applicable statistical methods are needed.
Network analysis, a more theoretically sound method of categorizing events into trauma subtypes, identifies patterns (i.e., networks) of symptoms and PTEs that are most closely associated—thus detecting clusters of PTEs that result in similar outcomes. In a community sample, Contractor et al. (2020) applied this approach to define three PTE clusters (i.e., trauma subtypes) in the LEC-5: accidental/injury traumas, death threat traumas, and victimization traumas.
Despite these developments, much is unknown regarding the impact of trauma subtypes in refugee populations. Moreover, most research with refugees has focused on PTSD and depression, with few studies addressing anxiety [15]. Recent research suggests, however, that refugees are at increased risk for anxiety: our group found that 40.3% of a sample of Syrian refugees screened positive for high anxiety [16]. Further, as discussed, statistical methods for defining trauma subtypes have been improved—necessitating that prior results regarding PTSD and depression be confirmed. The aims of the current study thus include gaining insight into the qualitative differences between trauma subtypes as compared to cumulative trauma score. We examined the predictive utility of three previously defined trauma subtypes in the LEC-5 [8] for assessing psychological outcomes in a refugee sample. Based on previous work [5], we hypothesized that: (1) models including the LEC-5 trauma subtypes as separate variables would explain more variance in PTSD, depression, and anxiety symptoms than models based on cumulative LEC-5 scores; and (2) individual trauma subtypes of the LEC-5 would differentially predict PTSD, depression, and anxiety symptoms.
Methods
Participants and Procedures
Participants included 78 adults from Iraq and Syria, resettled as refugees in southeast Michigan. All participants were refugees of war and were part of a longitudinal study of refugee health [16]. Participants were invited to join a voluntary research study during primary care screenings in their first month of resettlement. Interested parties were introduced to the researchers by their physician and provided with informed consent documents. For a detailed account of participants and procedures, see prior works [16, 17]. Data used in this analysis was collected approximately two years after participants’ arrival in the U.S. All procedures were carried out in accordance with the Declaration of Helsinki and approved by the Institutional Review Board at Wayne State University—IRB #012416B3F.
Measures
Participant characteristics were obtained via a demographic questionnaire. All measures were administered in both Arabic and English. The LEC-5 [18], which asks participants to report level of exposure to 16 PTEs, was used to assess trauma exposure. To ensure analyses captured personal exposure to a PTE—and as vague definitions of trauma exposure (e.g., having “learned about” an event) may limit interpretation of results—only direct exposure to an event was investigated; thus, “yes” responses to the 16 items probing “Happened to me” were summed to calculate cumulative trauma score and scores within each trauma subtype [19]. The LEC-5 is valid and reliable across cultures [20, 21].
Anxiety- and depression-related symptoms during the past week were measured using the 25-item Hopkins Symptom Checklist (HSCL-25). 10 items probe anxiety symptoms and 15 relate to depression symptoms, with higher mean scores representing greater symptom severity [22]. The HSCL-25 is valid for refugee populations [23], and reliability for the anxiety and depression subscales in this sample was excellent (α = 0.87 and α = 0.90, respectively).
The PTSD Checklist based on the DSM-V (PCL-5) was utilized to measure severity of PTSD-related symptomatology [18]. This variable was operationalized as the sum score on this 20-item measure, with higher scores indicating greater symptom severity. The PCL-5 is valid across multiple cultures and types of trauma exposure [24, 25]. The reliability of this measure in the current study was excellent (α = 0.94).
Statistical Analyses
Analyses were conducted in SPSS version 27.0. Descriptive statistics were examined to assess outliers, distributional properties, and assumptions. Data was screened for normality, demonstrating no significant skew or kurtosis. Pairwise plots revealed no violations of linearity or homoskedasticity assumptions, and pairwise correlations revealed no multi-collinearity issues (all r < 0.9). PCL-5 surveys with more than 5 missing responses were removed (n = 7). Percentages of missing data for cumulative trauma, PTSD, anxiety, and depression were low (0%, 11.5%, 7.6%, and 5.1%, respectively) and MCAR (Little’s x2 = 1561.71). Outliers of more than 2.5 SDs from the mean on outcome variables were removed (n = 1). As missing data was MCAR, a complete case analysis was performed [26], leaving a final sample size of 70.
Three continuous trauma subtype variables were computed by summing “yes” responses to LEC-5 items in each subtype (see Table 1) [8]. To test Hypothesis 1, hierarchical multiple regression analyses were performed to determine whether cumulative trauma score or trauma subtype scoresexplained more variance (R2) in depression-, anxiety-, and PTSD-related symptoms, controlling for age and gender. For Hypothesis 2, the multiple regression models with trauma subtypes entered as predictors were examined for potentially differing associations between specific trauma subtypes and outcome variables.
Table 1.
Descriptive statistics for analysis variables
| Range | M | SD | |
|---|---|---|---|
| Age | 18–65 | 35.99 | 11.36 |
| Female, % | 51.4 | ||
| Country of origin, % | |||
| Syria | 88.6 | ||
| Iraq | 10.0 | ||
| Not reported | 1.4 | ||
| Accident/Injury | 0–4 | 0.44 | 0.86 |
| Victimization | 0–1 | 0.09 | 0.28 |
| Death threat | 0–4 | 0.86 | 1.32 |
| Cumulative trauma | 0–8 | 1.47 | 2.08 |
| Anxiety symptoms | 1–3.5 | 1.66 | 0.57 |
| PTSD symptoms | 0–60 | 22.84 | 16.44 |
| Depression symptoms | 1–3.33 | 1.72 | 0.58 |
Ranges refer to the range of the sample, not the possible range of scores on measures (n = 70). LEC-5 items included in each subtype category are as follows: (1) accident/injury (items 1–4 and 12), (2) victimization (items 6, 8, and 9), and (3) death threat (items 5, 7, 10, 11, and 13–16; 7, 8)
Results
Descriptive Statistics
Sample characteristics are presented in Table 1. The mean age for participants was 35.99 years (SD = 11.36) and about half were female (51.4%). Most reported Syria as their country of origin (88.6%), with fewer reporting Iraq (10.0%). The average number of cumulative trauma exposures was 1.47 (SD = 2.08). Of the trauma subtypes, death threat traumas were most prevalent, with 37.1% reporting at least one exposure. The accident/injury trauma subtype and victimization trauma subtypes were less prevalent, with 25.7% and 8.6% of participants reporting at least one exposure, respectively. No sexual assault was reported—thus, the victimization subtype represented physical assault exposures. The average severity of symptoms related to PTSD (M = 22.84, SD = 16.44), anxiety (M = 1.66, SD = 0.57), and depression (M = 1.72, SD = 0.58) in this sample was low-to-moderate.
Cumulative and Trauma Subtype Models
PTSD Models
The first hierarchical regression model with PTSD as the outcome variable included age, gender, and cumulative trauma score and significantly predicted PTSD severity [F(3,66) = 3.51, p = .020; R2 = 0.138; RMSE = 15.61; see Table 2]. There was a significant, positive association between cumulative trauma score and PTSD symptoms, and cumulative trauma explained 12.5% of the variance in PTSD scores. Comparatively, the model including age, gender, accident/injury trauma, death threat trauma, and victimization trauma [F(5,64) = 6.04, p < .001; R2 = 0.32; RMSE = 14.07] explained 18.2% more variance than the cumulative trauma model. In the trauma subtype model, victimization was significantly associated with PTSD (b = 30.64, SE = 6.93, t = 4.42, p < 0.001, LLCI = 16.8, ULCI = 44.48) and uniquely accounted for 21% of the variance in PTSD severity. Death threat (p = 0.320) and accident/injury (p = 0.994) traumas were not significant predictors of PTSD scores (see Table 2).
Table 2.
Prediction of psychological symptoms using trauma subtype model and cumulative trauma model
| Model | Independent variable | PTSD symptoms | Anxiety symptoms | Depression symptoms | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| β | p | r 2 | β | p | r 2 | β | p | r 2 | ||
| Cumulative trauma | ||||||||||
| Step 1 | (Constant) | 16.14 | 0.041 | 1.31 | < 0.001 | 1.58 | < 0.001 | |||
| Age | 0.15 | 0.430 | 0.009 | 0.01 | 0.189 | 0.026 | 0.00 | 0.633 | 0.003 | |
| Gender (female) | 2.84 | 0.494 | 0.007 | 0.09 | 0.553 | 0.005 | 0.06 | 0.704 | 0.002 | |
| Step 2 | (Constant) | 17.38 | 0.020 | 1.33 | < 0.001 | 1.60 | < 0.001 | |||
| Age | −0.03 | 0.882 | 0.000 | 0.01 | 0.428 | 0.009 | 0.00 | 0.978 | 0.000 | |
| Gender (female) | 3.96 | 0.315 | 0.013 | 0.11 | 0.460 | 0.008 | 0.08 | 0.597 | 0.004 | |
| Cumulative trauma score | 2.99* | 0.003 | 0.125 | 0.06 | 0.125 | 0.035 | 0.06 | 0.116 | 0.040 | |
| Trauma subtype | ||||||||||
| Step 1 | (Constant) | 16.14 | 0.041 | 1.31 | < 0.001 | 1.58 | < 0.001 | |||
| Age | 0.15 | 0.430 | 0.009 | 0.01 | 0.189 | 0.026 | 0.00 | 0.633 | 0.003 | |
| Gender (female) | 2.84 | 0.494 | 0.007 | 0.09 | 0.553 | 0.005 | 0.06 | 0.704 | 0.002 | |
| Step 2 | (Constant) | 9.05 | 0.207 | 1.11 | < 0.001 | 1.38 | < 0.001 | |||
| Age | 0.14 | 0.422 | 0.007 | 0.01 | 0.158 | 0.024 | 0.004 | 0.568 | 0.004 | |
| Gender (female) | 8.98* | 0.019 | 0.062 | 0.26 | 0.059 | 0.043 | 0.224 | 0.124 | 0.031 | |
| Accidental injury | −0.02 | 0.994 | 0.000 | −0.12 | 0.151 | 0.025 | −0.06 | 0.463 | 0.007 | |
| Victimization | 30.64* | < 0.001 | 0.210 | 0.95* | < 0.001 | 0.162 | 0.88* | 0.002 | 0.140 | |
| Death threat | 1.69 | 0.320 | 0.010 | 0.06 | 0.349 | 0.010 | 0.04 | 0.510 | 0.005 | |
| Cumulative model R2 | 0.138* | 0.061 | 0.041 | |||||||
| Trauma subtype model R2 | 0.32* | 0.246* | 0.184* | |||||||
| Cumulative model adjusted R2 | 0.098* | 0.018 | −0.002 | |||||||
| Trauma subtype model adjusted R2 | 0.267* | 0.187* | 0.12* | |||||||
Predictor variables are marked significant at the *p < 0.05 level.
The R2 for significant models based on F statistics are noted with an asterisk
Anxiety Models
For the first anxiety model, the predictor variable of cumulative trauma score and the covariates of age and gender were regressed on the dependent variable of anxiety, yielding a nonsignificant model [F(3,66) = 1.43, p = 0.243; R2 = 0.061; RMSE = 0.568]. Therefore, cumulative trauma score did not significantly predict anxiety. The trauma subtype model was estimated entering age and gender as covariates and the three trauma subtypes as predictors, resulting in a model summary of [F(5,64) = 4.18, p = 0.002; R2 = 0.246; RMSE = 0.517]; thus, the model explained 18.5% more variance in anxiety scores than the cumulative trauma model. Victimization was the only trauma subtype significantly associated with the outcome variable (b = 0.95, SE = 0.25, t = 3.71, p < 0.001, LLCI = 0.44, ULCI = 1.45), and uniquely accounted for 16.2% of the variance in anxiety scores; see Table 2.
Depression Models
The first depression model was estimated entering age and gender as covariates, cumulative trauma score as the predictor, and depression as the outcome variable. This model was not significant [F(3,66) = 0.95, p = 0.424; R2 = 0.041; RMSE = 0.580]. The trauma subtype model was subsequently estimated, regressing age, gender, and the three trauma subtype variables on depression severity. This yielded a model summary of [F(5,64) = 2.88, p = 0.021; R2 = 0.184; RMSE = 0.543], indicating that the model explained 14.3% more variance in depression scores than the cumulative trauma model. Victimization was significantly associated with depression symptoms (b = 0.88, SE = 0.27, t = 3.28, p = 0.002, LLCI = 0.34, ULCI = 1.41), and accounted for 14% of the variance in the outcome variable; see Table 2.
A Bonferroni adjusted p value of 0.008 (0.05/6 models) was used to reassess model significance. The PTSD and anxiety trauma subtype models both remained significant after correction, while the PTSD cumulative trauma model and depression subtype model did not.
Discussion
This study examined the predictive utility of trauma subtypes, as compared to cumulative trauma scores. As anticipated in our first hypothesis, we found that predictive models incorporating trauma subtypes explained more variance in all three outcome variables than cumulative trauma models. Our second hypothesis was also supported, as victimization trauma was a significant predictor of symptoms related to PTSD, depression, and anxiety, while accidental/injury trauma and death threat trauma were not. Further, though cumulative trauma scores were associated with PTSD symptoms, victimization uniquely explained more variance (21%) in PTSD scores than did the cumulative trauma score (12.5%). Cumulative trauma score was not associated with depression or anxiety symptoms. Overall, our investigation supports the consideration of trauma subtypes when utilizing trauma measures to predict PTSD, anxiety, and depression symptom levels and improves upon past investigations by using trauma subtypes identified by network analysis [8]—a superior methodology to factor analysis in this area of study [13].
These results are consistent with prior literature examining PTSD and depression [5, 8], while to our knowledge this is the first study to investigate trauma subtypes in regard to anxiety in refugees. Past investigations of the impact of trauma on PTSD and depression in general populations [8, 9, 10] and refugee populations [5, 11] have similarly indicated that more nuanced subtype models account for more variance in psychological outcomes.
Prior studies have also demonstrated the utility of cumulative trauma scores [13, 27]. Indeed, cumulative trauma scores in the current study predicted PTSD symptom severity; nevertheless, both the subtype model and the victimization variable explained more variance in PTSD than cumulative score. Considering all three psychological outcomes, our results indicate that operationalizing trauma as a cumulative score masked valuable information that was later observable in the subtype models.
Victimization
As no sexual assault was reported in the current sample, victimization represented physical assault only [8]. For all subtype models, victimization was the only subtype significantly associated with the outcome variable. Notably, while all participants had experienced war and forced migration, only the victimization subtype was associated with mean PTSD, anxiety, and depression symptom severity that met diagnostic thresholds (see Fig. 1) [28, 29]. This finding is striking considering the focus on the impact of war and migration as a whole in many refugee studies; perhaps it is not this overall experience that contributes to psychopathology, but rather experiences of victimization transpiring during these broader events.
Fig. 1.
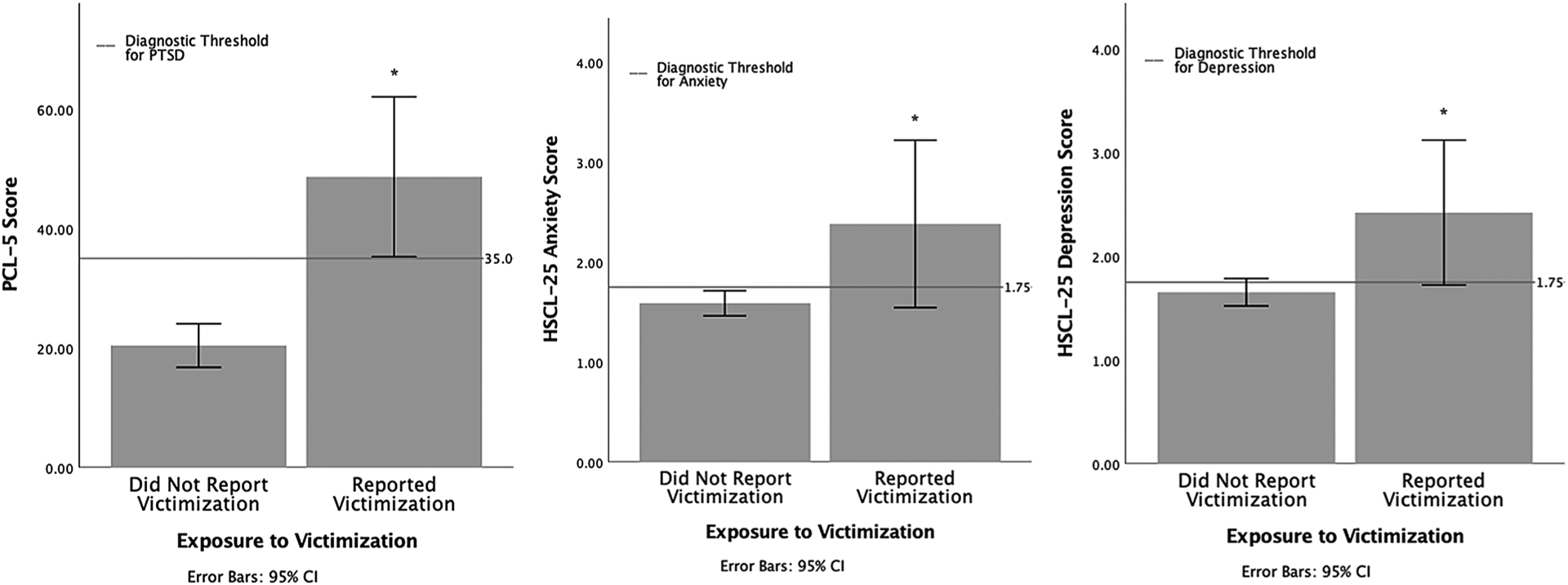
A visual representation of the effect of victimization trauma on PTSD symptoms (β = 30.64; p < 0.001), anxiety symptoms (β = 0.95; p < 0.001), and depression symptoms (β = 0.88; p = 0.002)
There are several potential explanations for the specific significance of victimization traumas. Freyd’s betrayal theory posits that traumas inflicted by another person more reliably lead to psychopathological symptoms than non-inter-personal traumas [30]. While this theory focuses on trauma inflicted by trusted individuals, it is plausible that this phenomenon extends to interpersonal traumas carried out by any fellow human being. Indeed, interpersonal traumas (typically defined as physical and sexual assault; thus, synonymous with victimization) perpetuated by any individual are associated with greater PTSD, anxiety, and depression symptoms than non-interpersonal traumas [31, 32, 33].
Event centrality—or the extent to which a traumatic experience impacts an individual’s identity and worldview [34]—may also explain these findings. Robust evidence links this facet of trauma with PTSD, depression, self-perception, and other outcomes [9, 35]. Additionally, interpersonal traumas are more reliably associated with high event centrality than non-interpersonal traumas [36]. It is therefore possible that event centrality drives the considerable findings indicating that interpersonal/victimization traumas have greater psychological impact. This may also explain inconsistent results regarding trauma types that do not fall clearly into interpersonal and non-interpersonal categories (e.g., death threat traumas) [37, 38]. For instance, a death threat trauma that significantly affects one’s worldview may have as much impact on the development of trauma-related pathology as a victimization trauma. Subsequent studies may obtain greater insight by utilizing measures of both trauma subtype and event centrality in future models.
Limitations
This study has several limitations, including the low-to-moderate symptom levels reported; however, as the study was not focused only on individuals meeting diagnostic criteria, the results may have greater relevance to refugee populations regardless of diagnostic status. A continuous approach to symptomatology also aligns with NIH’s RDoC guidelines and was better powered for this sample. Secondly, the victimization subtype in our sample was limited to physical assault, and few participants (n = 6) endorsed victimization, limiting generalizability and designating these findings as preliminary. Notably, however, the percentage of participants reporting victimization (8.6%) was consistent with the 8–10% of trauma-exposed persons who tend to develop PTSD [39], possibly implicating victimization as a key contributor to the development of clinically significant symptoms. Studies in which victimization includes sexual assault are required to confirm these findings. It should also be noted that the current group was primarily Syrian, and refugees from different countries of origin may differ in symptom prevalence [40]; future studies should investigate the generalizability of these associations.
Contribution and Implications
Overall, these findings indicate that a more nuanced conceptualization of trauma should be considered when assessing psychological outcomes in persons resettling as refugees. While studies of refugee mental health often focus on the impact of war and migration overall, classifications of war trauma may be improved through a more fine-grained approach. Though the current findings are preliminary, these results and those from civilian populations suggest a consistent pattern of high impact associated with victimization. Future studies investigating whether certain trauma experiences are more effectively treated through specific interventions for refugees are indicated [17, 34, 35, 36].
Clinically, the findings emphasize the need for mental health practitioners to understand the specific traumatic events their patients have experienced, in addition to their cumulative trauma exposure. Increased specificity in clinical assessment—rather than clustering patients based on, for example, migration status—may improve prevention and early intervention efforts, as those at highest risk for trauma-related psychopathology may be more accurately identified. Particularly given the considerable number of people who have resettled as refugees—and will likely continue to do so in response to changing political and global dynamics—a fine-grained understanding of trauma outcomes is essential to providing effective mental health care.
Acknowledgements
The authors would like to thank all the participants who engaged in this research, contributed their data, and shared their stories. The authors would also like to thank Tarek Almasaddi, Heba Al-Saghir, Mohammed Alsaud, Michael Kabbash, Suzanne Manji, Luna Nasry, Dalya Saleem, Safa Sankari, Rajaa Shoukfeh, and Samantha Sonderman for their assistance with data collection and data entry. Many thanks as well to Dr. Alireza Amirsadri and Dr. Luay Haddad. Finally, thank you to the organizations and institutions who have provided financial support for this research—including the State of Michigan Lycaki/Young Foundation and the Department of Psychiatry and Behavioral Neuroscience. Ms. Grasser’s effort is supported by F31MH120927 (PI: Grasser) and Dr. Javanbakht’s effort is supported by R01HD099178 (PI: Javanbakht).
Funding
This work was supported by the National Institute of Health (Grant No. R01HD099178) and the National Institute of Mental Health (Grant No. F31MH120927). The funding sources had no involvement in the collection, analysis and interpretation of data; in the writing of the report; nor in the decision to submit the article for publication.
Footnotes
Conflict of interest The authors have no financial disclosures nor conflicts of interest to report.
Ethical Approval All study procedures were carried out in accordance with the latest version of the Declaration of Helsinki and approved by the Institutional Review Board at Wayne State University—IRB #012416B3F.
Consent to Participate Participants were given the opportunity to join a paid, voluntary research study during health screenings at primary care clinics during their first month of resettlement. Interested parties were introduced to the research group by their physician and provided with informed consent documents. All participants included in this analysis provided informed consent prior to any study procedures.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1.Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. The Lancet. 2005;365(9467):1309–14. 10.1016/S0140-6736(05)61027-6. [DOI] [PubMed] [Google Scholar]
- 2.LeMaster JW, Broadbridge CL, Lumley MA, Arnetz JE, Arfken C, Fetters MD, Jamil H, Pole N, Arnetz BB. Acculturation and post-migration psychological symptoms among Iraqi refugees: a path analysis. Am J Orthopsychiatr. 2018;88(1):38–47. 10.1037/ort0000240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bustamante LHU, Cerqueira RO, Leclerc E, Brietzke E. Stress, trauma, and posttraumatic stress disorder in migrants: a comprehensive review. Braz J Psychiatr. 2017. 10.1590/1516-4446-2017-2290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lindert J, von Ehrenstein OS, Priebe S, Mielck A, Brähler E. Depression and anxiety in labor migrants and refugees—a systematic review and meta-analysis. Soc Sci Med. 2009;69(2):246–57. 10.1016/j.socscimed.2009.04.032. [DOI] [PubMed] [Google Scholar]
- 5.Arnetz BB, Broadbridge CL, Jamil H, Lumley MA, Pole N, Barkho E, Fakhouri M, Talia YR, Arnetz JE. Specific trauma subtypes improve the predictive validity of the harvard trauma questionnaire in Iraqi refugees. J Immigr Minor Health. 2014;16(6):1055–61. 10.1007/s10903-014-9995-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jensen TK, Skårdalsmo EMB, Fjermestad KW. Development of mental health problems—a follow-up study of unaccompanied refugee minors. Child Adolesc Psychiatr Mental Health. 2014;8(1):1–10. 10.1186/1753-2000-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nosè M, Turrini G, Imoli M, Ballette F, Ostuzzi G, Cucchi F, Padoan C, Ruggeri M, Barbui C. Prevalence and correlates of psychological distress and psychiatric disorders in asylum seekers and refugees resettled in an Italian catchment area. J Immigr Minor Health. 2018;20(2):263–70. 10.1007/s10903-017-0629-x. [DOI] [PubMed] [Google Scholar]
- 8.Contractor AA, Weiss NH, Batley N, Elhai JD. Clusters of trauma types as measured by the Life Events Checklist for DSM–5. Int J Stress Manage. 2020. 10.1037/str0000179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Keshet H, Foa EB, Gilboa-Schechtman E. Women’s self-perceptions in the aftermath of trauma: the role of trauma-centrality and trauma-type. Psychol Trauma: Theory Res Pract Policy. 2019;11(5):542–50. 10.1037/tra0000393. [DOI] [PubMed] [Google Scholar]
- 10.Raudales AM, Short NA, Schmidt NB. Emotion dysregulation mediates the relationship between trauma type and PTSD symptoms in a diverse trauma-exposed clinical sample. Pers Indiv Differ. 2019;139:28–33. 10.1016/j.paid.2018.10.033. [DOI] [Google Scholar]
- 11.Kira I, Lewandowski L, Somers CL, Yoon JS, Chiodo L. The effects of trauma types, cumulative trauma, and PTSD on IQ in two highly traumatized adolescent groups. Psychol Trauma: Theory Res Pract Policy. 2012;4(1):128–39. 10.1037/a0022121. [DOI] [Google Scholar]
- 12.Silove D, Steel Z, McGorry P, Miles V, Drobny J. The impact of torture on post-traumatic stress symptoms in war-affected Tamil refugees and immigrants. Compr Psychiatr. 2002;43(1):49–55. 10.1053/comp.2002.29843. [DOI] [PubMed] [Google Scholar]
- 13.Hodgdon HB, Suvak M, Zinoviev DY, Liebman RE, Briggs EC, Spinazzola J. Network analysis of exposure to trauma and childhood adversities in a clinical sample of youth. Psychol Assess. 2019;31(11):1294–306. 10.1037/pas0000748. [DOI] [PubMed] [Google Scholar]
- 14.King DW, King LA, Gudanowski DM, Vreven DL. Alternative representations of war zone stressors: relationships to posttraumatic stress disorder in male and female Vietnam veterans. J Abnorm Psychol. 1995;104(1):184–96. 10.1037/0021-843X.104.1.184. [DOI] [PubMed] [Google Scholar]
- 15.Abu Suhaiban H, Grasser LR, Javanbakht A. Mental health of refugees and torture survivors: a critical review of prevalence, predictors, and integrated care. Int J Environ Res Public Health. 2019. 10.3390/ijerph16132309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Javanbakht A, Amirsadri A, Abu Suhaiban H, Alsaud MI, Alobaidi Z, Rawi Z, Arfken CL. Prevalence of possible mental disorders in syrian refugees resettling in the United States screened at primary care. J Immigr Minor Health. 2019;21(3):664–7. 10.1007/s10903-018-0797-3. [DOI] [PubMed] [Google Scholar]
- 17.Javanbakht A, Grasser LR, Kim S, Arfken CL, Nugent N. Perceived health, adversity, and posttraumatic stress disorder in Syrian and Iraqi refugees. Int J Soc Psychiatr. 2020. 10.1177/0020764020978274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The ptsd checklist for dsm-5 (pcl-5). Scale available from the National Center for PTSD at https://www.ptsd.va.gov. 2013. Accessed 1 Oct 2021. [Google Scholar]
- 19.Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11(4):330–41. 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- 20.Lima EP, Vasconcelos AG, Berger W, Kristensen CH, Nascimento ED, Figueira I, Mendlowicz MV, Universidade Federal de Minas Gerais, Brazil, Universidade Federal do Rio de Janeiro, Brazil, Pontifícia Universidade Católica do Rio Grande do Sul, Brazil, & Universidade Federal Fluminense, Brazil. Cross-cultural adaptation of the Posttraumatic Stress Disorder Checklist 5 (PCL-5) and Life Events Checklist 5 (LEC-5) for the Brazilian context. Trends Psychiatry Psychother. 2016;38(4):207–15. 10.1590/2237-6089-2015-0074. [DOI] [PubMed] [Google Scholar]
- 21.Rzeszutek M, Lis-Turlejska M, Palich H, Szumiał S. The Polish adaptation of the Life Events Checklist (LEC-5) for PTSD criteria from DSM-5. Psychiatr Pol. 2018;52(3):499–510. 10.12740/PP/OnlineFirst/69218. [DOI] [PubMed] [Google Scholar]
- 22.Hesbacher PT, Rickels K, Morris RJ, Newman H, Rosenfeld H. Psychiatric illness in family practice. J Clin Psychiatr. 1980;41(1):6–10. [PubMed] [Google Scholar]
- 23.Lavik NJ, Laake P, Hauff E, Solberg Ø. The use of self-reports in psychiatric studies of traumatized refugees: validation and analysis of HSCL-25. Nord J Psychiatr. 1999;53(1):17–20. 10.1080/080394899426666. [DOI] [Google Scholar]
- 24.Ashbaugh AR, Houle-Johnson S, Herbert C, El-Hage W, Brunet A. Psychometric validation of the English and French versions of the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5). PLoS ONE. 2016;11(10):e0161645. 10.1371/journal.pone.0161645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, Keane TM. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychol Assess. 2016;28(11):1379–91. 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- 26.Newman DA. Missing data: five practical guidelines. Organiz Res Methods. 2014;17(4):372–411. 10.1177/1094428114548590. [DOI] [Google Scholar]
- 27.Layne CM, Briggs EC, Courtois CA. Introduction to the special section: using the trauma history profile to unpack risk factor caravans and their consequences. Psychol Trauma: Theory Res Pract Policy. 2014;6(Suppl 1):1–8. 10.1037/a0037768. [DOI] [Google Scholar]
- 28.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19(1):1–15. 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 29.Mat SMN, Ismail H, Mohd YH. Reliability and validity of a post-traumatic checklist-5 (PCL-5) among fire and rescue officers in Selangor, Malaysia. J Health Res. 2020;35(4):379–87. 10.1108/JHR-11-2019-0243. [DOI] [Google Scholar]
- 30.Freyd J Betrayal trauma: traumatic amnesia as an adaptive response to childhood abuse. Ethics Behav. 1994;4:307–29. 10.1207/s15327019eb0404_1. [DOI] [Google Scholar]
- 31.Breslau N Gender differences in trauma and posttraumatic stress disorder. J Gender Spec Med. 2002;5(1):34–40. [PubMed] [Google Scholar]
- 32.Chen LP, Murad MH, Paras ML, Colbenson KM, Sattler AL, Goranson EN, Elamin MB, Seime RJ, Shinozaki G, Prokop LJ, Zirakzadeh A. Sexual abuse and lifetime diagnosis of psychiatric disorders: systematic review and meta-analysis. Mayo Clinic Proc. 2010;85(7):618–29. 10.4065/mcp.2009.0583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Preston TJ, Gorday JY, Bedford CE, Mathes BM, Schmidt NB. A longitudinal investigation of trauma-specific rumination and PTSD symptoms: the moderating role of interpersonal trauma experience. J Affect Disord. 2021;292:142–8. 10.1016/j.jad.2021.05.049. [DOI] [PubMed] [Google Scholar]
- 34.Berntsen D, Rubin DC. The centrality of event scale: a measure of integrating a trauma into one’s identity and its relation to post-traumatic stress disorder symptoms. Behav Res Ther. 2006;44(2):219–31. 10.1016/j.brat.2005.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gehrt TB, Berntsen D, Hoyle RH, Rubin DC. Psychological and clinical correlates of the Centrality of Event Scale: a systematic review. Clin Psychol Rev. 2018;65:57–80. 10.1016/j.cpr.2018.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reiland SA, Clark CB. Relationship between event type and mental health outcomes: event centrality as mediator. Pers Indiv Differ. 2017;114:155–9. 10.1016/j.paid.2017.04.009. [DOI] [Google Scholar]
- 37.Macia KS, Raines AM, Maieritsch KP, Franklin CL. PTSD networks of veterans with combat versus non-combat types of indextrauma. J Affect Disord. 2020;277:559–67. 10.1016/j.jad.2020.08.027. [DOI] [PubMed] [Google Scholar]
- 38.Belleville G, Marchand A, St-Hilaire M, Martin M, Silva C. PTSD and depression following armed robbery: patterns of appearance and impact on absenteeism and use of health care services. J Trauma Stress. 2012;25(4):465–8. 10.1002/jts.21726. [DOI] [PubMed] [Google Scholar]
- 39.National Institute of Mental Health. 2021. Post-traumatic stress disorder (PTSD). https://www.nimh.nih.gov/health/statistics/post-traumatic-stress-disorder-ptsd. Accessed 5 Dec 2021.
- 40.Grasser LR, Haddad L, Manji S, Assari S, Arfken C, Javanbakht A. Trauma-related psychopathology in Iraqi refugee youth resettled in the united states, and comparison with an ethnically similar refugee sample: a cross-sectional study. Front Psychol. 2021;12:704. 10.3389/fpsyg.2021.574368. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


