Abstract
Background:
Neuroimaging tools, such as functional magnetic resonance imaging, are useful in understanding differences in brain activity that predict behavior change. Designing interventions based on brain activity and response may enhance current self-management regimens. Yet, diverse groups, such as Black women with chronic illness, have historically been left out of neuroimaging research.
Objectives:
To assess (a) the feasibility of conducting neuroimaging research among Black women with hypertension and (b) predictors of willingness to participate in future studies.
Methods:
A survey designed to assess interest in participating in neuroimaging research was distributed through a Facebook campaign targeting metro-Detroit Black with hypertension. A 10-min, 44-item survey queried the women regarding their perspectives related to participation in neuroimaging studies. Logistic regression analyses were conducted to predict willingness to participate in a future study; they included a range of predictors: demographic indicators, history of blood pressure diagnosis, systolic and diastolic blood pressure, and availability of a support person who could accompany the participant to a future study session.
Results:
257 Black women completed the survey. On average, the women were 59 years old, had been diagnosed with hypertension for 14 years, and had a systolic blood pressure of 141 mm Hg. Participants were willing to travel 40 miles to participate, and many preferred to drive a personal vehicle. Some women were claustrophobic (20%) or had metal in their bodies (13%) and, therefore, would likely be ineligible to participate in neuroimaging studies. Some were nervous about the “small space” of a scanner, but others stated they would “enjoy participating” and wanted to “help future people … get well.” Women who had a support person to attend their appointment with them were almost 4 times more likely to state they would participate in future studies. Those who had been diagnosed with hypertension for more than 11 years (the median) were almost three times more likely to report interest in participating in a future study than those participants who had been diagnosed with hypertension for 11 years or less.
Discussion:
Black women with hypertension were interested and eligible to participate in neuroimaging research. Despite some of the facilitators and barriers we identified, the women in our sample were interested in participating in future studies. The presence of a support person and length of time with a hypertension diagnosis are important predictors of willingness to participate in a future study.
Keywords: hypertension, neuroimaging, self-management
There is a long-standing body of research regarding understanding self-management of chronic health conditions. Successful self-management entails acquiring, using, and sharing health information (Baek et al., 2017; Jones et al., 2018). Comprehensive and effective use of health information translates into a cascade of key processes, including making decisions, solving problems, deciding on new strategies, and gaining social support; the ultimate goal is to engage in health behavior change (Allegrante et al., 2019; Jones et al., 2018). The Precision Medicine Initiative called for health care interventions and practices to consider individual differences in lifestyle, environment, and biology (15Collins & Varmus, 2015; 14Mapes et al., 2020). One tool that has been used to examine patient-specific characteristics and subsequent behavior is functional magnetic resonance imaging, or fMRI (Falk et al., 2010; Jack et al., 2013; Kang et al., 2019; Monroe et al., 2016; Nketia et al., 2021).
Previous studies have used neuroimaging, such as fMRI, as a tool to observe brain activity (analytic and empathetic), by measuring how blood flow changes in the brain in response to different prompts (Falk et al., 2012, 2015; Jack et al., 2006, 2013). Prior research has shown that individuals with greater balance in analytic and empathetic neural processing are more likely to formulate and act on their plans (Jack et al., 2013). Using fMRI, researchers have been able to predict how likely patients are to stop smoking, how often individuals will use sunscreen, and reasons that drive sharing of information (Baek et al., 2017; Falk et al., 2010, 2015). Designing interventions based on brain activity and response may enhance current self-management regimens.
In a recent literature review focusing on research assessing the fMRI analyses among individuals with cardiovascular disease, with an overall intent for understanding behavior change, Jones et al. (2020) found that 98% of the articles did not report the race or ethnic background of the study participants. The literature review revealed a lack of fMRI studies that have been conducted with representative numbers of Black participants, especially women with hypertension. Other studies have also highlighted the importance of increasing diversity in neuroimaging studies (Byrd & Rivera-Mindt, 2022; Dotson & Duarte, 2020; Mapes et al., 2020; Nketia et al., 2021). Given that little is known about brain activity patterns, especially among Blacks with cardiac disease (Jones et al., 2020), we conducted our study— MindingMe—which aimed to examine the feasibility of conducting fMRI studies among Black women and examine predictors of willingness to participate in future studies.
Hypertension is a leading cause of morbidity and mortality in the United States, particularly among Black women (Vaughan et al., 2022). Uncontrolled hypertension can lead to stroke, end-stage renal disease, and premature death (Chobanian et al., 2003; James et al., 2014). Black women with hypertension are diagnosed earlier, live with hypertension longer, and die at an earlier age when compared with other women with hypertension (Chen et al., 2019). As a modifiable risk factor, hypertension is highly preventable and can be successfully managed (Carey et al., 2018; Chobanian et al., 2003; Perumareddi, 2019; Roger et al., 2012).
Among Black individuals, there is evidence to support lifestyle modifications to reduce blood pressure readings and maintain blood pressure control, which reduces some of the aforementioned risks (Chan et al., 2015; Chobanian et al., 2003; James et al., 2014). A critical and linked issue to the idea of modifiable risk factors is the general question of understanding self-management of one’s chronic conditions, including elevated blood pressure. Although evidence-based recommendations are available to assist patients in successfully self-managing their blood pressure, Black women have a cumulative lifetime risk for hypertension of 86%—equivalent to both Black and White men in the United States (Chen et al., 2019). Studies that examine ways to tailor interventions to patient-specific characteristics are needed. One approach to better understanding how to tailor self-management programs is using fMRI to better understand brain activity associated with implementing lifestyle modifications.
Methods
Study Design
This study was cross-sectional, descriptive, and deemed exempt by our university’s institutional review board (IRB). Given that there are fewer disparities in internet access via cellphones and use of social media (Smith, 2014), we launched a Facebook campaign with advertisements that specifically targeted Black women, our exemplary diverse group of interest. Several stages and strategies were employed to carry out this study to assess the feasibility of using Facebook as a methodological tool for identifying a Black sample. Key (successive) steps and processes included developing a tailored Facebook campaign that would advertise the study to the key demographic groups of interest for the study; directing viewers to the study Qualtrics (Qualtrics, 2020) link and screening questions; and administering a survey tapping demographic characteristics and possible barriers and facilitators to participating in an fMRI-focused study. The output for this paper was generated using Qualtrics software (2020).
Recruitment
Sample recruitment took place over a 4-month period between July and October 2018. Study team members distributed the online survey tool through a targeted Facebook campaign and via selective posting in a local Black sorority and professional Facebook groups. By the end of October, more than 400 women had participated in the survey.
Screening
All interested individuals completed a screening section at the beginning of the survey. By design, only individuals who entered an age of greater than or equal to 18 years, self-identified as a Black or African American woman, reported that they had been diagnosed with hypertension by a health care professional, and entered a zip code in Southeastern Michigan were invited to continue with the study. See Figure 1 for an enrollment diagram.
Figure 1.
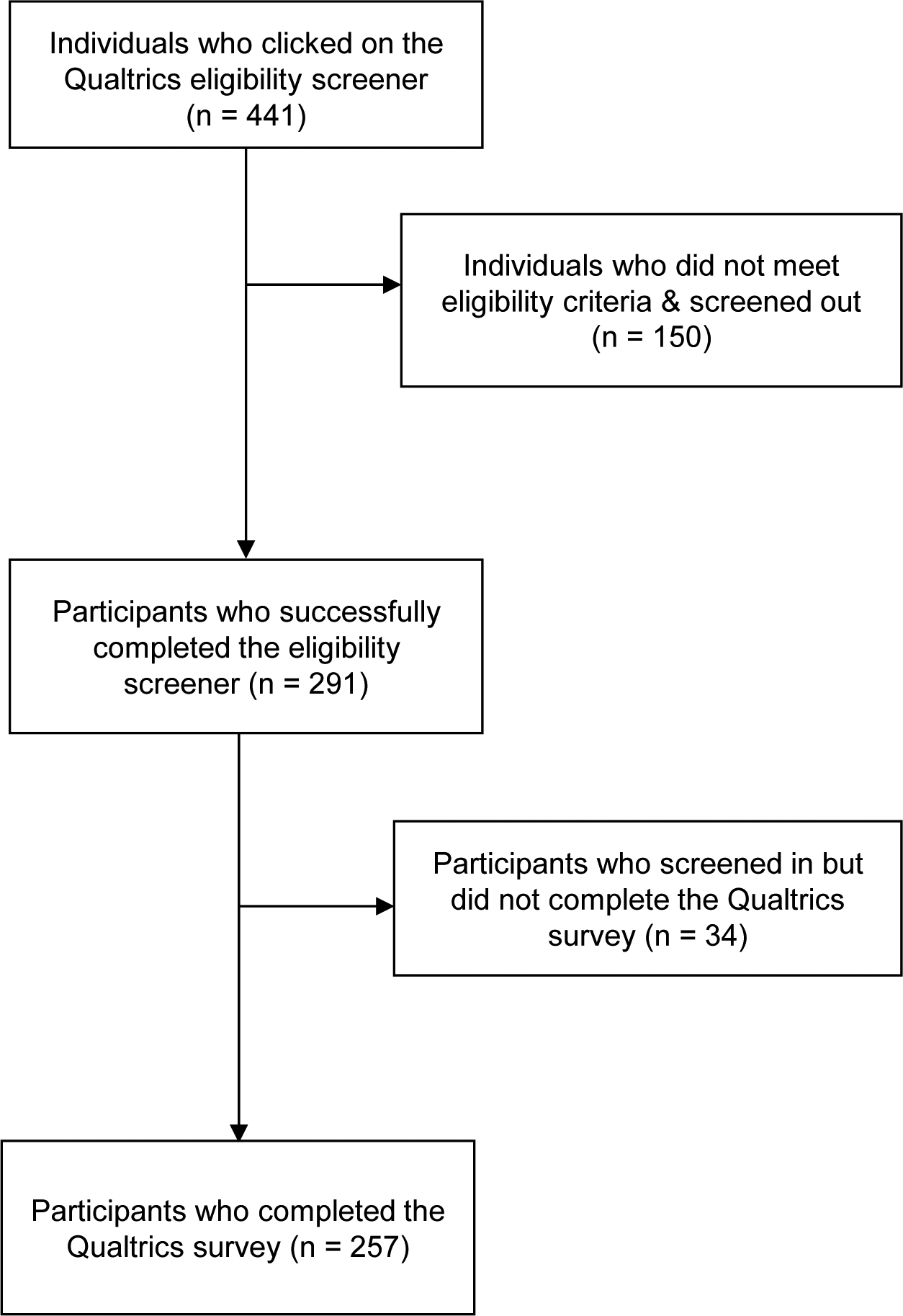
Participant Enrollment
Data Collection
After successfully completing the screening questions, eligible individuals were directed to the main Qualtrics survey. The first page of the survey contained an information sheet for informed consent. The information sheet had a description of the study’s purpose, risks, benefits of participating in the study and contact information for the researchers conducting the study and the IRB. By clicking “I Agree” at the bottom of the information page, individuals agreed to participate in the study. Participants were then directed to the first page of survey questions.
The Facebook campaign was designed to reach an audience of adult Black women. The goal was to identify women who may have been interested in participating in neuroimaging research, including our next study. Our fMRI scanner was located in metro Detroit, so we specifically targeted women who lived in the metro-Detroit area.
Measures
The 10-min, 44-item survey queried the women regarding their demographics, health status, interest in participating in neuroimaging research, conditions that may prevent participation, as well as facilitators and barriers related to participation in fMRI studies.
Age was assessed with a simple open-ended question; participants were asked to reply in years. Education was measured with a single question asking participants to select their highest level of education achieved. Multiple response categories were provided, including some high school, high school diploma/GED, through doctoral degrees. For analysis purposes, a number representing years of education was attached to each degree category, 11 years through 17. Time since blood pressure diagnosis was measured with a single open-ended item: “How long have you had hypertension (high blood pressure)?” (Please enter number of years). Participants were asked to self-report their latest systolic and diastolic blood pressure readings. The availability of a support person was measured with a single item: “Do you have someone who could come with you to the research lab if you decided to participate in a research study?” Participants could respond “yes,” “no,” or “unsure.” Our outcome of interest, willingness to participate in a future study, was assessed with a single question. Participants could respond “yes,” “maybe,” or “no.”
Results
Although more than 400 women responded to our ad, 257 Black women completed the survey and were included in our final sample. Table 1 presents the characteristics of our sample. The mean age was approximately 59 years old (SD = 8.80). Our sample was well-educated; more than half of the sample completed 14 or more years of education. The mean time since being diagnosed with high blood pressure was just over 14 years (range = 1–50).
Table 1.
Sample Demographic Characteristics
| Variable | n | % |
|---|---|---|
| Education | ||
| 11–13 years | 112 | 43 |
| 14–17 years | 145 | 57 |
| Systolic blood pressure (130 mm Hg and above) | 197 | 77 |
| Diastolic blood pressure (80 mm Hg and above) | 195 | 77 |
| Support person to accompany to a future study session | ||
| Yes | 103 | 40 |
| No | 54 | 21 |
| Unsure | 67 | 26 |
| Willing to participate in a future study | 151 | 59 |
Participants reported that they were willing to travel approximately 40 miles to participate in a research study and could spend 94 min completing all study activities. Most participants preferred to take a shuttle (90%) from home to the study visit. Many said they would drive a personal vehicle (72%), while others were willing to take an Uber/Lyft (65%). Some women were claustrophobic (20%) or had metal in their bodies (13%), so they would be ineligible to participate in future fMRI studies. Some were nervous about the “small space” of an fMRI or the “length of time” for the scan, but others stated they would “enjoy participating” and wanted to “help future people … get well.”
More than 40% of the sample reported having a support person who could accompany them to an upcoming study visit; 21% and 26% responded “no” or “unsure” regarding a possible support person, respectively. Over half of the participants (58%) responded that they would be willing to participate in a future study.
Table 2 includes the results of the logistic regression analysis predicting willingness to participate in an upcoming study (1= yes, 0 = maybe). We included a range of predictors, including demographics, blood pressure history, blood pressure self-reports, and presence of a support person. We found two significant sets of predictors: time since high blood pressure diagnosis and presence of a possible support person. Splitting time since high blood pressure diagnosis at the median (11 years), participants above the median are just over 2.5 times more likely than those below the median to report willingness to participate in a future study (p = .024). Participants who responded that they did have a support person were more than 3.7 times more likely than those who reported not having a support person to be willing to participate in a future study (p = 0.003). Similarly, participants who reported that she was unsure regarding the availability of a support person were more than 3.5 times more likely than those who responded that not having a support person to report interest in a future study (p = 0.008).
Table 2.
Logistic Regression Analysis Predicting Willingness to Participate in a Future Study
| Variable | O.R. [95% CI] |
|---|---|
| Age (reference: below the median) | 1.29 [0.58–2.88] |
| Education (reference: below the median) | 1.26 [0.60–2.68] |
| Time since high blood pressure diagnosed (reference: below the median) | 2.52 [1.12–5.67]* |
| Systolic blood pressure (reference: < 130 mm Hg) | 1.98 [0.83–4.70] |
| Diastolic blood pressure (reference: < 80 mm Hg) | 1.46 [0.61–3.52] |
| Support person to accompany to a future study session (reference: no) | |
| Accompany – yes | 3.67 [1.51–8.90]* |
| Accompany – unsure | 3.53 [1.36–9.13]* |
Note.
p < .01
Discussion
The aim of this study was two-pronged: first, to explore the feasibility of conducting fMRI research among Black women with hypertension, and second, to examine the predictors of willingness to participate in future studies. The women in this study were eligible and reported that they were interested and available to participate in hypertension studies that included fMRI scans. Components that would facilitate participation, as well as factors that would hinder it, were identified.
The majority of the sample had elevated blood pressures greater than 130/80 mm Hg. Although this was self-report data, it is clear that many of the participants had uncontrolled blood pressure levels. There are evidence-based strategies to assist Black women in achieving and maintaining blood pressure control (Carey et al., 2018; Roger et al., 2012). Hypertension, particularly among Black women, remains a public health issue that deserves continued attention from the scientific community and the community at large.
Scientists are using unique approaches, like the use of neuroimaging, to examine patient-specific characteristics and behaviors (Baek et al., 2017; Kang et al., 2019; Moshfeghi et al., 2016). However, in many fMRI studies, diverse groups—such as Black women, have been underrepresented or not included (Jones et al., 2020; Mapes et al., 2020). While studies have highlighted how brain activity in the scanner can be used to better understand behavior, these studies traditionally do not represent diverse populations by disease or race/ethnicity (Byrd & Rivera-Mindt, 2022; Jones et al., 2020; Mapes et al., 2020). Few studies have focused on Black individuals with elevated blood pressure (Jones et al., 2019; Moore et al., 2019; Wright et al., 2020). Additional fMRI studies that center on the unique characteristics of diverse groups, such as Black women with hypertension, are needed (Dotson & Duarte, 2020; Nketia et al., 2021). In future studies that collect data from participants remotely, it would also be essential to explain the requirements of participating in an in-person, neuroimaging study.
Similar to other studies (Allegrante et al., 2019), we found that time since blood pressure diagnosis is a crucial predictor of willingness to participate in a future study. Women that lived more years with a chronic illness may have been more interested in learning how to better manage it. They may also have been aware that living with chronic disease longer puts individuals at a higher risk of negative outcomes and may be interested in studies that may help reduce their risk (Chen et al., 2019).
In addition, we found that the presence of a support person who could accompany the participant is also a significant predictor of interest in a future blood pressure management study. Similar to our study, other researchers often query distance to travel, time and compensation. Fewer studies ask about support or others who can come to appointments with participants. While the COVID-19 pandemic and other factors might limit the number of individuals allowed in one space—if being accompanied by a support person would increase the likelihood of participation in future studies, it is important to consider how to facilitate support persons including compensating them for their time (Monroe et al., 2016).
Limitations
As with any research study, this study was not without limitations. First, the measure that we used was not validated. Although it had not been deemed a valid and reliable tool, we were able to gather critical and meaningful data from our sample. Second, our sample was restricted to Facebook users in a specific geographic area if they were interested in participating in our future studies. Therefore, these are the perspectives of Black women who are Facebook users in one geographic area, which may not be generalizable to all women. Third, because we did not directly interact with participants in this study, we could not administer a cognitive assessment. Thus, we were unable to determine if there were any memory deficits in our sample.
Conclusion
Metro-Detroit Black women with hypertension are interested in and eligible to participate in fMRI studies. These findings directly informed our current and future studies in mitigating certain barriers to participation (transportation, time, reservations about undergoing an fMRI). Our goal is to develop interventions tailored to patient-specific characteristics, to minimize health disparities and maximize favorable health outcomes for Black women. This study was a first step in examining the feasibility of conducting neuroimaging studies among our diverse group of interest. These findings can facilitate the development of study protocols that focus on assessing the needs of diverse groups for participation in neuroimaging research, as well as assessing which factors predict willingness to participate in future studies.
Acknowledgments
Research reported in this publication was supported by the National Institutes of Health - National Heart, Lung, and Blood Institute, National Institute of Nursing Research, National Institute of Aging P20NR015331, 2P30AG015281, 5P30AG053760, 1K01HL145366, and 5P30AG053760-S1; Betty Irene Moore Foundation for Nurse Leaders and Innovators, and the University of Michigan School of Nursing. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors would like to thank Robert J. Ploutz-Snyder, PhD, PStat® (Assistant Dean of Research and Scholarship, Director of the Applied Biostatistics Laboratory, University of Michigan School of Nursing) for his statistical expertise and recommendations.
Footnotes
The authors have no conflicts of interest to report.
The study associated with this protocol was conducted ethically. It was reviewed by the University of Michigan Institutional Review Board and received a Notice of Exemption –HUM00142075.
References
- Allegrante JP, Wells MT, & Peterson JC (2019). Interventions to support behavioral self-management of chronic diseases. Annual Review of Public Health, 40, 127–146. 10.1146/annurev-publhealth-040218-044008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baek EC, Scholz C, O’Donnell MB, & Falk EB (2017). The value of sharing information: A neural account of information transmission. Psychological Science, 28, 851–861. 10.1177/0956797617695073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrd DA, & Rivera-Mindt MG (2022). Neuropsychology’s race problem does not begin or end with demographically adjusted norms. Nature Reviews Neurology, 18, 125–126. 10.1038/s41582-021-00607-4 [DOI] [PubMed] [Google Scholar]
- Carey RM, Muntner P, Bosworth HB, & Whelton PK (2018). Reprint of: Prevention and control of hypertension: JACC Health Promotion Series. Journal of the American College of Cardiology, 72, 2996–3011. 10.1016/j.jacc.2018.10.022 [DOI] [PubMed] [Google Scholar]
- Chan Q, Stamler J, & Elliott P (2015). Dietary factors and higher blood pressure in African-Americans. Current Hypertension Reports, 17, 10. 10.1007/s11906-014-0517-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen V, Ning H, Allen N, Kershaw K, Khan S, Lloyd-Jones DM, & Wilkins JT (2019). Lifetime risks for hypertension by contemporary guidelines in African American and white men and women. JAMA Cardiology, 4, 455–459. 10.1001/jamacardio.2019.0529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr., Jones DW, Materson BJ, Oparil S, Wright JT Jr., & Roccella EJ (2003). The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA, 289, 2560–2572. 10.1001/jama.289.19.2560 [DOI] [PubMed] [Google Scholar]
- Collins FS, & Varmus H (2015). A new initiative on precision medicine. New England Journal of Medicine, 372, 793–795. 10.1056/NEJMp1500523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dotson VM, & Duarte A (2020). The importance of diversity in cognitive neuroscience. Annals of the New York Academy of Sciences, 1464, 181–191. 10.1111/nyas.14268 [DOI] [PubMed] [Google Scholar]
- Falk EB, Berkman ET, Mann T, Harrison B, & Lieberman MD (2010). Predicting persuasion-induced behavior change from the brain. Journal of Neuroscience, 30, 8421–8424. 10.1523/JNEUROSCI.0063-10.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falk EB, O’Donnell MB, & Lieberman MD (2012). Getting the word out: Neural correlates of enthusiastic message propagation. Frontiers in Human Neuroscience, 6, 313. 10.3389/fnhum.2012.00313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falk EB, O’Donnell MB, Cascio CN, Tinney F, Kang Y, Lieberman MD, Taylor SE, An L, Resnicow K, & Strecher VJ (2015). Self-affirmation alters the brain’s response to health messages and subsequent behavior change. Proceedings of the National Academy of Sciences, 112, 1977–1982. 10.1073/pnas.1500247112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack AI, Dawson AJ, Begany KL, Leckie RL, Barry KP, Ciccia AH, & Snyder AZ (2013). fMRI reveals reciprocal inhibition between social and physical cognitive domains. NeuroImage, 66, 385–401. 10.1016/j.neuroimage.2012.10.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack AI, Sylvester CM, & Corbetta M (2006). Losing our brainless minds: How neuroimaging informs cognition. Cortex, 42, 418–421. 10.1016/S0010-9452(08)70373-3 [DOI] [PubMed] [Google Scholar]
- James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr., Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr., Narva AS, & Ortiz E (2014). 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA, 311, 507–520. 10.1001/jama.2013.284427 [DOI] [PubMed] [Google Scholar]
- Jones LM, Ginier E, Debbs J, Eaton JL, Renner C, Hawkins J, Rios-Spicer R, Tang E, Schertzing C, & Giordani B (2020). Exploring representation of diverse samples in fMRI studies conducted in patients with cardiac-related chronic illness: A focused systematic review. Frontiers in Human Neuroscience, 14, 108. 10.3389/fnhum.2020.00108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones LM, Veinot TC, Pressler SJ, Coleman-Burns P, & McCall A (2018). Exploring predictors of information use to self-manage blood pressure in midwestern African American women with hypertension. Journal of Immigrant and Minority Health, 20, 569–576. 10.1007/s10903-017-0573-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones LM, Wright KD, Jack AI, Friedman JP, Fresco DM, Veinot T, Lu W, & Moore SM (2019). The relationships between health information behavior and neural processing in African Americans with prehypertension. Journal of the Association for Information Science and Technology, 70, 968–980. 10.1002/asi.24098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones LM, Wright KD, Wallace MK, & Veinot T (2018). “Take an opportunity whenever you get it”: Information sharing among African-American women with hypertension. Journal of the Association for Information Science and Technology, 69, 168–171. 10.1002/asi.23923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang Y, Strecher VJ, Kim E, & Falk EB (2019). Purpose in life and conflict-related neural responses during health decision-making. Health Psychology, 38, 545–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mapes BM, Foster CS, Kusnoor SV, Epelbaum MI, AuYoung M, Jenkins G, Lopez-Class M, Richardson-Heron D, Elmi A, Surkan K, Cronin RM, Wilkins CH, Pérez-Stable EJ, Dishman E, Denny JC, & Rutter JL (2020). Diversity and inclusion for the All of Us research program: A scoping review. PloS ONE, 15, e0234962. 10.1371/journal.pone.0234962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe TB, Gibson SJ, Bruehl SP, Gore JC, Dietrich MS, Newhouse P, Atalla S, & Cowan RL (2016). Contact heat sensitivity and reports of unpleasantness in communicative people with mild to moderate cognitive impairment in Alzheimer’s disease: A cross-sectional study. BMC Medicine, 14, 74. 10.1186/s12916-016-0619-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore SM, Musil CM, Jack AI, Alder ML, Fresco DM, Webel A, Wright KD, Sattar A, & Higgins P (2019). Characterization of brain signatures to add precision to self-management health information interventions. Nursing Research, 68, 127–134. 10.1097/NNR.0000000000000331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moshfeghi Y, Triantafillou P, & Pollick FE (2016). Understanding information need: An fMRI study. In Proceedings of the 39th International ACM SIGIR conference on Research and Development in Information Retrieval, 335–344. 10.1145/2911451.2911534 [DOI] [Google Scholar]
- Nketia J, Amso D, & Brito NH (2021). Towards a more inclusive and equitable developmental cognitive neuroscience. Developmental Cognitive Neuroscience, 52, 101014. 10.1016/j.dcn.2021.101014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perumareddi P (2019). Prevention of hypertension related to cardiovascular disease. Primary Care: Clinics in Office Practice, 46, 27–39. 10.1016/j.pop.2018.10.005 [DOI] [PubMed] [Google Scholar]
- Qualtrics. (2020). Qualtrics. Qualtrics. [Google Scholar]
- Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, … Turner MB (2012). Heart disease and stroke statistics—2012 update: A report from the American Heart Association. Circulation, 125, e2–e220. 10.1161/CIR.0b013e31823ac046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A (2014). African Americans and technology use: A demographic portrait. Pew Research Center. [Google Scholar]
- Vaughan AS, Coronado F, Casper M, Loustalot F, & Wright JS (2022). County‐level trends in hypertension‐related cardiovascular disease mortality—United States, 2000 to 2019. Journal of the American Heart Association, 11, e024785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright KD, Jack AI, Friedman JP, Jones LM, Sattar A, Fresco DM, & Moore SM (2020). Neural processing and perceived discrimination stress in African Americans. Nursing Research, 69, 331–338. 10.1097/NNR.0000000000000441 [DOI] [PMC free article] [PubMed] [Google Scholar]


