Abstract
Background:
African Americans have a higher incidence of early-onset stroke and poorer stroke-related outcomes than other race/ethnic groups.
Objectives:
Our two-arm, randomized controlled trial was implemented to assess efficacy of the nurse-led, Stroke Counseling for Risk Reduction (SCORRE) intervention in reducing stroke risk in young African American adults by improving accuracy of perceived stroke risk and lifestyle behaviors (i.e., diet, physical activity, smoking cessation). Stroke knowledge, behavior change readiness, and perceived competence to live a healthy lifestyle were also explored as secondary outcomes.
Methods:
African Americans aged 20–35 years, recruited from an urban university and surrounding community, were randomized to SCORRE or an attention-placebo control group receiving safe sex education. Data were collected pre-intervention, immediate post-intervention, and at 8 weeks. Multilevel models were used for primary outcome analyses.
Results:
Participants (n = 106) were mostly in their mid-20s, female, college students, and averaged about three modifiable stroke risk factors. Compared to the control group, participants in the intervention group had, on average, a significant increase in accuracy of perceived stroke risk post-intervention, a greater change in perceived competence to live healthy, and greater increase in dietary components at 8 weeks. Significant changes were not found in physical activity and other outcomes.
Discussion:
These findings suggest that SCORRE is a promising intervention to reduce stroke risk among young African American adults. Results will inform a more robust, randomized controlled trial of SCORRE to have an age, culture, and gender-focused intervention that effectively reduces stroke risk among African Americans early in life.
Keywords: African American, behavior change, prevention, risk perception, stroke, young adult
The rise of stroke in young adults calls for greater attention to increase prevention efforts. Over the past decade, researchers have documented increased hospitalizations for stroke, up to 30%, among adults aged 18–44 (George et al., 2017; Kissela et al., 2012). Similarly, a decade of racial and ethnic stroke disparities from prevention to recovery has been documented (Cruz-Flores et al., 2011; Gutierrez & Williams, 2014). Compared to Whites, Black individuals 20–44 years old have a twofold higher incidence of stroke that increases threefold between ages 45–54 (Kissela et al., 2012). Additionally, Black individuals experience more severe, disabling strokes and higher mortality rates (Feng et al., 2009; Tsivgoulis et al., 2014). Studies have demonstrated that hypertension, diabetes, and obesity have contributed to the increase of stroke in young adults, and these factors are disproportionately observed in young African Americans (AA) (Aigner et al., 2017; George et al., 2017). Although stroke pathogenesis and subtype may vary in young adults and by race (George et al., 2017; Yahya et al., 2020), recommendations for early detection and intervention to prevent or delay stroke include control of risk factors and lifestyle change in early adulthood (i.e., 20–35-year-old; Yahya et al., 2020).
Early adulthood is an integral period in which individuals start to make their own lifestyle choices. Researchers of the Coronary Artery Risk Development in Young Adults (CARDIA) study found that maintaining a healthy lifestyle at ages 18 to 30 is associated with reduced cardiovascular disease risk in middle age (Liu et al., 2012). However, many young adults do not associate their health behaviors with risk of future stroke (American Heart Association [AHA], 2011; Aycock & Clark, 2016). We found that young AA had less than ideal cardiovascular health, inadequate knowledge of stroke risk factors, and inaccurate perceptions of future stroke risk (Aycock et al., 2015, 2017). To address this, Aycock et al. (2017) developed the Stroke Counseling for Risk Reduction (SCORRE) intervention, a theory-based, nurse-led, primary stroke prevention intervention that is age- and culturally tailored to young adult AA to increase their stroke knowledge, perceptions, and lifestyle behaviors.
SCORRE is based on the Health Belief Model (HBM; Rosenstock, 1974) and Precaution Adoption Process Model (Weinstein, 1988), which together, propose that preventive behaviors are adopted through a series of decisional changes influenced by individual perceptions and beliefs. SCORRE was designed to change these perceptions by promoting lifestyle behavior change. The initial components of SCORRE that target these theoretical goals are a stroke education brochure and video, a nurse-led, cardiovascular risk counseling session, and a behavioral risk reduction diary (Aycock et al., 2017).
The SCORRE intervention was found to be feasible and acceptable in a sample of AA (N = 30) men and women aged 20–45. Findings from the feasibility study (Aycock et al., 2017) informed refinement of the SCORRE intervention and a plan for more rigorous methods. The age range was narrowed to 20–35 to include adults earlier to have the greatest effect on risk reduction. Readiness for behavior change and perceived competence to live a healthy lifestyle were added to identify potential mechanisms of behavior change action. Motivational text messages were also added and are consistent with the HBM in that they serve as cues to action to influence health behavior change. Lastly, extending the follow-up from 6 to 8 weeks and changing from a control group (stroke education brochure only) to an attention–placebo control group that equates with the same level of interpersonal interaction and intensity as the SCORRE group (i.e., safe sex education brochure, and video and text messages; Aycock et al., 2018), added rigor to the intervention testing.
This paper reports findings from a pilot study testing the refined SCORRE intervention. The study’s aims were twofold: Test the initial efficacy of the SCORRE intervention in improving accuracy of perceived stroke risk and targeted risk reduction behaviors (i.e., diet, physical activity, and smoking cessation). We hypothesized that SCORRE participants (a) would have more accurate perceptions of their risk of stroke at post-intervention, and (b) would be more likely to increase targeted risk reduction behaviors from baseline to 8 weeks than participants receiving the attention–placebo control activities. The second aim was to explore changes in theoretical mechanisms of the interventions (i.e., knowledge of stroke risk factors, readiness for behavior change, and perceived competence to live a healthy lifestyle) from baseline to post-intervention and 8 weeks and the relationships of these mechanisms to risk reduction behaviors.
Methods
Design
The design was a parallel group, two-arm, randomized controlled trial with three data collection time points: baseline/pre-intervention and immediately post-intervention (Visit 1), and an 8-week follow-up (Visit 2). Participants were randomized in a 1:1 ratio in blocks of 10 to SCORRE or the attention–placebo control group. Participants were blinded to treatment group.
Sample and Recruitment
The sample eligibility criteria were self-identified (a) AA or Black, (b) 20–35 years old, (c) had at least one modifiable stroke risk factor, and (c) had a cell phone to receive text messages or email addresses. Individuals were excluded if they had a history of transient ischemic attack (TIA) or stroke. Convenience and snowball sampling were used to recruit participants from a large southeast urban university setting and the surrounding area. The study was advertised using flyers at different sites (e.g., campus, churches, hair and nail salons, barber shops, eateries), word of mouth, and internet sites (e.g., Craigslist).
A power analysis was conducted using Java Applets 22 computer software (Length, 2018) to estimate the sample size. To detect meaningful changes in diet, physical activity, and cigarette smoking targets, we defined effect sizes as a 60% increase in the number of participants engaging in recommended physical activity (Aycock et al., 2017) and 50% decrease in number of cigarettes smoked (Brown, 2013). Assuming 90% power, .05 level of significance, and a one-tailed test, the needed sample size was 92 participants. Assuming a 20% attrition rate, the target sample size was 116 participants (58 per group).
SCORRE Intervention
SCORRE is an in-person, one-on-one intervention with five components (reported in Aycock et al., 2017); the first three are provided during one 90-min visit and the remaining over 8 weeks. Participants (a) read a brochure about stroke in AA from the former National Stroke Association; (b) watched an investigator-developed, 16-min video of six AA adults ages 20–44, four experienced strokes and discussed how it affected their lives, and two without stroke discussed lifestyle changes made to reduce stroke risk; (c) received the AHA’s Life’s Simple 7 (LS7) cardiovascular risk assessment and education (AHA, 2018) tool coupled with stroke risk reduction counseling from a nurse practitioner who included a comparison of their perceived versus actual stroke risk; (d) completed an 8-week, printed behavior-specific, daily risk reduction diary, based on one less than ideal behavior (i.e., diet, physical activity or smoking cessation), they chose to work on over 8 weeks; and (e) weekly text messages with risk reduction behavior tips and a reminder to complete the daily diary.
Attention-Placebo Control
The attention–placebo control component was a nurse-led, individual session with five components: (a) a safe sex brochure from Planned Parenthood (2016; (b) a 23-min video on HIV/STD prevention from the Centers for Disease Control and Prevention [CDC], (Warner et al., 2008)); (c) printed results of participants’ health indicators (e.g., blood pressure, blood glucose) but no risk reduction counseling or select stroke risk reduction behavior to work on over the 8-week period; (d) a daily diary with an open-ended question of what step was taken each day to improve their health; and, (e) weekly text messages with safe sex tips and a reminder to complete the diary.
Instrumentation
A research team member interviewed participants to obtain their demographics and stroke-risk-related health histories. Primary behavioral and theoretical outcomes were measured with self-report questionnaires and/or physiological health indicators. A diary was used to track the behavioral outcomes during the 8-week period.
Primary Behavioral Outcomes
Dietary Behaviors
Diet was measured with the five dietary components from the AHA LS7 program (2018). Participants completed a self-report questionnaire that asked about their typical average intake of fruit and vegetables in cups per day, servings of fiber-rich whole grains per day, fish per week, sugar-sweetened beverages per week, and sodium intake in general. Participants received one point for each component considered “ideal” for an overall diet score of 0–5; higher scores indicate better dietary behaviors (Table 1). This dietary measure is associated with stroke risk in Black individuals (Kulshreshtha et al., 2013) and consistent with a diet recommended by the AHA to lower stroke risk (Lloyd-Jones et al., 2010). For further validation of the LS7 dietary measure, we also administered the Block Brief 2000 Food Frequency Questionnaire (BBFFQ), a validated 70-item food list (Block et al., 1990). Corresponding dietary components between the LS7 and BBFFQ were significantly correlated at positive, low to moderate intensities in our sample (Perrin et al., 2019).
Table 1.
Definitions of Ideal, Intermediate and Poor for Each Life’s Simple 7 Health Factor
| Health Factor | Ideal (2 points) | Intermediate (1 point) | Poor (0 points) |
|---|---|---|---|
| Healthy Diet Score* | 4–5 components | 2–3 components | 0–1 Components |
| Physical Activity | ≥ 75 min/wka vigorous OR ≥ 150 min/wk moderate | 1–74 min/wk vigorous OR 1–149 min/wk moderate | OR no vigorous of moderate |
| Cigarette Smoking | Never smoked or former smoker and quite > 12 months ago | Former smoker and quit ≤ 12 months ago | Current smoker |
| Body Mass Index | < 25 kg/m2 | 25 to < 30 kg/m2 |
≥ 30 kg/m2 |
| Blood Pressure Systolic and Diastolic | SBP < 120 mm Hg and DBP < 80 mm Hg (not treated) | SBP 120–139 mm Hg or DBP 80–89 mm Hg or treated to goal | SBP ≥ 140 mm Hg or DBP ≥ 90 mm Hg |
| Total Cholesterol | < 200 mg/dL (not treated) | 200–239 mg/dL or treated to goal | ≥ 240 mg/dL |
| Fasting Blood Glucose | < 100 mg/dL (not treated) | 100–125 mg/dL or treated to goal | ≥ 126 mg/dL |
Note: min/wk = minutes per week; kg/m2= kilograms per square meter; mm Hg= millimeters of mercury; mg/dL = milligrams per deciliter
1 point received for each dietary component in ideal range: ≥ 4.5 cups of fruits and vegetables per day; ≥ two 3.5- oz servings of fish per week; ≥ 3 1 ounce-equivalent servings/day of whole grains; ≤ 450 kcal (36 oz)/week of sugar-sweetened beverages; and answered yes to 2 of 3 sodium intake questions (i.e., I do not eat prepackaged or processed foods, I choose lower sodium options, I do not add salt to my food)
Physical Activity
The Godin Leisure-Time Exercise Questionnaire (GLTEQ) was used to assess self-reported minutes of mild, moderate, and vigorous activity during a typical 7-day period (Godin & Shephard, 1985). This established instrument has evidence of construct validity (Jacobs et al., 1993) and test–retest reliability (Reed & Phillips, 2005). The questionnaire has also been used in AA samples (Linder et al., 2018). The weekly frequencies of moderate and vigorous activity in minutes were summed to determine if participants met the AHA recommendations to achieve cardiovascular benefits (Table 1). We dichotomously categorized participants as met recommendations (Yes = 1) or not (No = 0).
Cigarette Smoking
Cigarette smoking was measured using two items from the CDC Behavioral Risk Factor Surveillance System (CDC, 2009). “Have you smoked at least 100 cigarettes in your entire life?” and “Do you now smoke cigarettes every day, some days, or not at all?” These items have evidence of construct validity (Carabello, 2001). Participants having smoked at least 100 cigarettes in their lifetime and were current smokers or quit within 12 months were considered at risk of stroke. Participants were categorized as smokers (Yes = 1; current smokers or those who had quit within 12 months) or nonsmokers (No = 0).
Diary
8-Week Risk Reduction Diary
Two investigator-developed diaries were used to collect participants’ health behaviors daily during the 8-week risk reduction period. Two diaries—one for the SCORRE group and one for the control group—were used to limit the potential for diary reactivity. The SCORRE group diary was specific to each participant’s targeted risk reduction behavior. Participants tracked their selected health behavior based on units of measurement (i.e., daily minutes, intensity, and type of physical activity; daily servings of the five dietary components in cups, ounces, or mg; daily number of cigarettes smoked). The control group diary—also completed daily—consisted of one item: “List up to three activities you did today to improve your health.” Diary completion rates were assessed by number of participants who returned their diaries at 8 weeks and number of completed daily diary entries out of 56 days.
Theoretical Outcomes
Accuracy of Perceived Stroke Risk
One measure of perceived stroke risk and one of actual stroke risk were compared to assess participants’ accuracy of perceived stroke risk. The perceived risk of stroke was measured by asking participants to rate their risk or chances of having a stroke in the next 10–20 years. A 0–10 scale was used, with 0 being “no risk” and 10 being “high risk.” Similar single-item measures of perceived stroke risk have been used (Aycock et al., 2019). We used the standardized cardiovascular health score from the AHA LS7 (2018) for actual stroke risk. The cardiovascular health score is derived from seven lifestyle-related health factors (Table 1). The self-report measures described earlier were used for diet, physical activity, and cigarette smoking. Height and weight were obtained, and BMI was calculated using a HealthoMeter® digital scale. Blood pressures were measured with an Omron® monitor using standard protocol and a finger prick test for fasting (8 hr); blood glucose and cholesterol were measured using CardioChek®. To obtain the cardiovascular health score, the LS7 program categorizes factors as “ideal” = 2, “intermediate” = 1 and “poor” = 0 (Table 1). The points are summed, divided by the total possible sum (i.e., 14), and multiplied by 10 for possible scores ranging from 0–10; higher scores indicate better cardiovascular health and reduced stroke risk.
For accuracy of perceived stroke risk, the single-item, 0–10 response of the participant’s perceived stroke risk was compared to the reversed 0–10 LS7 cardiovascular health score associated with actual stroke risk. The results were then grouped into three future stroke risk categories: accurate, underestimated, and overestimated. Participants who accurately estimated their risk of future stroke had a perceived risk score within 2 points (+/− 0 to 2) of their LS7 score; those identified as underestimating their risk of future stroke had a perceived risk score of 0 or > 2 points below their LS7 score; those who overestimated their risk had a perceived risk score > 2 points above their LS7 score. This estimation of perceived risk accuracy was guided by prior research (Aycock et al., 2017, 2019). For the analyses, we dichotomously categorized participants as having accurate stroke risk (1) or inaccurate stroke risk (0) underestimated or overestimated their stroke risk.
Knowledge of Stroke Risk Factors
An investigator-developed, self-report measure of stroke knowledge was used, asking participants to indicate “yes/no” or “don’t know” to whether the 14 factors listed were stroke risk factors (i.e., high cholesterol, family history of stroke, smoking cigarettes, AA/Black race, physical inactivity, poor eyesight, diabetes, heavy alcohol use, high blood pressure, arthritis, overweight/obesity, atrial fibrillation, poor diet, and stress). Responses of “don’t know” were coded as “no.” Correct item responses were summed for a total score ranging from 0–14, with higher scores indicating more knowledge. We selected factors based on stroke risk factors identified by the American Stroke Association (2021); internal consistency reliability of coefficients for the scale at each data collection were .60, .70, and .70, respectively.
Readiness for Behavior Change
The Behavior Change Adoption Process, adapted for stroke, was used to identify readiness for behavior change. This one-item survey, with seven responses based on the Precaution Adoption Process Model (Weinstein, 1988), has been validated with a sample of women with lupus to predict stage placement for engaging in behaviors to prevent cardiovascular disease (Weinstein et al., 2014). Readiness ranged from Stage 1: “I don’t think I’m at risk for stroke” to Stage 7: “I have made changes in my behaviors for at least 6 months to decrease my chances of having a stroke.” Participants read the statements and selected the one that best represented their stage of behavior change. Participants who selected responses 1–4 (i.e., pre-contemplation to contemplation phases) were considered not ready for behavior change (No = 0), and those who selected 5–7 (i.e., preparation to action phases) were considered ready for behavior change (Yes = 1). Content validity of the measure, adapted for stroke, was obtained through review by experts in stroke, measurement, and behavior change.
Perceived Competence to Live a Healthy Lifestyle
The Perceived Competence Scale (PCS) is a 4-item scale that refers to an individual’s feelings or perceptions of competence regarding a specific behavior; the items on the PCS can be adapted to that behavior (Williams et al., 1998). For this study, “living a healthy lifestyle” to lower risk of stroke was the specific behavior. Responses are on a 7-point Likert-type scale with responses ranging from 1 = “not at all true” to 7 = “very true”; higher average scores indicate higher perceived competence to live a healthy lifestyle. The original PCS has been validated in prior studies (Williams et al., 1998) and modified for use in other samples of young adult AA (Miller et al., 2018). The internal consistency reliability coefficients in this study ranged from .92–.94.
Procedures and Data Collection
A university institutional review board approved this study. Participants were recruited over 7 months. Individuals interested in participating contacted the researchers by telephone or email. A research team member explained the study and screened individuals for initial inclusion criteria (i.e., race, age). Those meeting the criteria were then scheduled for an in-person visit at an urban university. The principal investigator (PI), an adult health nurse practitioner, conducted the initial screening—the Visit 1 baseline data collection—and administered the SCORRE intervention and the attention-placebo control activity. During Visit 1, the study was explained, written informed consent was obtained, and pre-intervention data were collected. After reviewing data related to eligibility, participants without at least one risk factor for stroke or an LS7 score ≥ 9.3, indicating minimal to no risk, were identified as ineligible. These persons received a copy of their stroke risk assessment results but did not continue in the study. Remaining participants were randomized and received the SCORRE intervention or the attention-placebo control activity.
Trained graduate research assistants ([GRAs], i.e., RNs enrolled in a master’s program), conducted all post-intervention data collection. During Visit 1, a GRA blinded to treatment groups readministered questionnaires immediately following the intervention or control activity. For Visit 2, 8-week follow, a GRA readministered questionnaires and any objective physiological health indicators that were not in the ideal range at baseline. Participants were compensated $20 for Visit 1, $30 for returning diary data at 4 months, and $50 for Visit 2. The study team used a study checklist for consistency in implementing the procedures.
Data Analysis
The SAS Software System, Version 9.4, was used for data analysis. All study measures were summarized with appropriate descriptive statistics. Cronbach alpha reliability coefficients were computed for instruments as appropriate. Complete case analysis was used for calculation of the reliability coefficients.
Multilevel models accounted for the within-subject correlation resulting from repeated measurements on each subject. We developed statistical models for primary outcomes (diet, physical activity, accuracy of perceived stroke risk) and secondary outcomes (knowledge of stroke risk factors, readiness for behavioral change, and perceived competence to live healthily). Five of the six outcomes were categorical measurements and necessitated a generalized linear model framework. Marginal models with population average effects are useful with categorical outcomes (Hayat & Hedlin, 2012). Thus, we developed marginal models with generalized estimating equations for each outcome. For dichotomous outcomes, we developed marginal models with a binomial distribution and logit link function—a type of logistic regression modeling for analyzing the binary outcomes. Ordinal outcomes were modeled with a multinomial distribution and cumulative logit link function. An advantage of marginal models is in their efficient handling of missing data. Partial observations on a participant are included and contribute to the model estimates. The study level of significance was set a priori at .05.
Results
Of the 116 participants, 106 had at least one modifiable risk factor for stroke and were randomized, and 97 completed the study (Figure 1). The sample was primarily female (75%) and in their mid-20s. Most participants had some college education (95%) and health insurance (79%), and more than half worked full/part-time. Participants’ LS7 scores ranged from 4.3 to 8.6, with an average of 7.2 (SD = 1.2) out of 10, considered less than ideal. They averaged almost three of the seven LS7 modifiable risk factors for stroke. The most prevalent factors were: 60% had BMIs ≥ 25 kg/m2 (half were > 30 kg/m2), 47% had elevated blood pressures (i.e., ≥120/80; 30% were SPB 130–139/ DBP 80–89; 12% were SPB ≥140/ DBP ≥90), 99% had diets that were not in ideal range (i.e., < 4 out of 5 dietary components met) and 48% had physical activity levels that were not in ideal range (i.e., < 150 min of moderate and < 75 min of vigorous per week) according to the LS7 recommendations. Seven (7%) participants self-reported current cigarette or cigar use. Baseline characteristics by group are displayed in Table 2.
Figure 1.
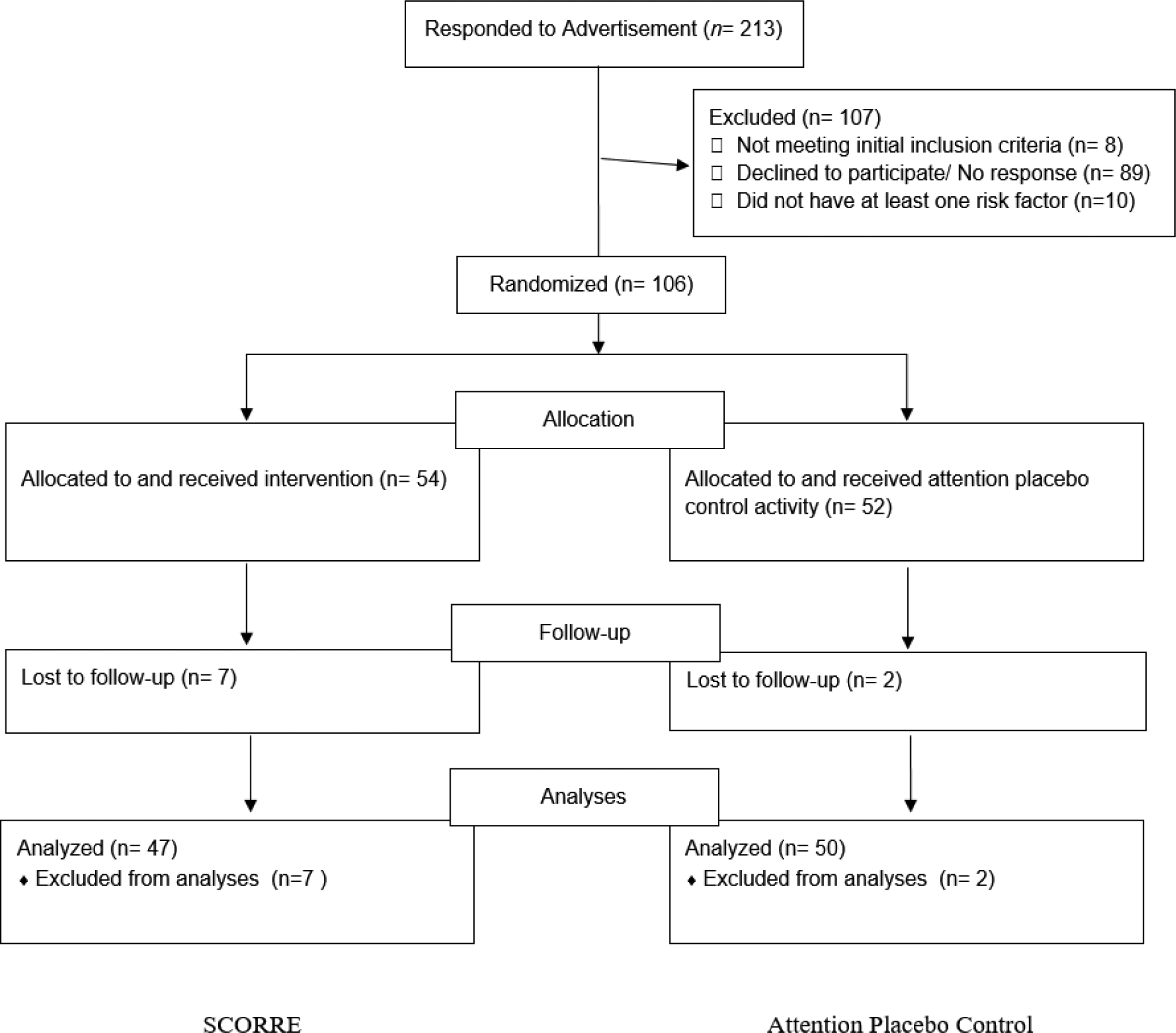
CONSORT Diagram for SCORRE Study
Table 2.
Baseline Participant Characteristics Stratified by Treatment Group
| Covariate | SCORRE Group n = 54 |
Attention-Control Group n = 52 |
Total n = 106 |
|||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Age in years | 25.37 | 4.79 | 24.29 | 4.31 | 24.84 | 4.57 |
| Years of Education | 14.78 | 1.55 | 15.00 | 1.52 | 14.89 | 1.53 |
| LS7 Cardiovascular Health Score | 7.16 | 1.19 | 7.20 | 1.13 | 7.18 | 1.16 |
| Number of LS7 Risk Factors | 2.75 | 1.08 | 2.78 | 1.03 | 2.77 | 1.05 |
| n | % | n | % | n | % | |
| Sex | ||||||
| Female | 39 | 72 | 40 | 77 | 79 | 74 |
| Male | 15 | 28 | 12 | 23 | 27 | 26 |
| Working | ||||||
| Full/Part-time | 37 | 69 | 33 | 64 | 70 | 66 |
| Not working | 17 | 31 | 19 | 36 | 36 | 34 |
| Yearly Income, n (%) | ||||||
| < $30,000 | 42 | 78 | 29 | 56 | 71 | 67 |
| ≥ $30,000 | 12 | 22 | 23 | 44 | 35 | 33 |
| Had Health Insurance | ||||||
| Yes | 39 | 72 | 45 | 87 | 84 | 79 |
| No | 15 | 28 | 7 | 13 | 22 | 21 |
| Family History of Stroke | ||||||
| Yes | 18 | 33 | 14 | 27 | 32 | 30 |
| No | 36 | 67 | 38 | 73 | 74 | 70 |
Note. SD = standard deviation
Primary Behavioral Outcomes
Descriptive Results
Of the 54 participants randomized to the SCORRE intervention, 37 selected diet, 14 physical activity, and three cigarettes smoking to work on during the 8-week risk reduction period; respectively, 33, 11, and 3 completed the study. Of the participants in both groups who completed the study, 80% of the intervention group compared to 90% of the control group completed 80% (45 out of 56 days) or more of their daily diary entries.
The subset of current cigarette smokers was insufficient to examine differences by group: only diet and physical activity results are reported. Descriptive data of the group comparison results over time for the subset of SCORRE intervention participants based on whether they selected diet or physical activity are described first. Of the 11 SCORRE participants who selected physical activity, 55% improved their physical activity levels at 8 weeks compared to 24% of all control participants. Similarly, of the 33 SCORRE participants selecting diet, 61% improved their diet at 8 weeks compared to 34% of all control participants.
Multilevel Modeling Results
The results of overall group comparisons over time for diet and physical activity (i.e., regardless of the behavior selected) using multilevel modeling are in Tables 3 and 4. The SCORRE intervention effects were assessed using comparative change in the two study arms with a time-by-treatment interaction term in each model. There was no difference in the SCORRE group compared to the control group on physical activity (odds ratio [OR]: 0.73, 95% CI: [0.29, 1.85], p = .505). However, the SCORRE group differed significantly on diet (OR: 0.37, 95% CI: [0.17, 0.83], p = .0162), indicating that participants in the intervention group had, on average, a greater increase in dietary components than participants in the control group.
Table 3.
Results of a Marginal Model with Generalized Estimating Equations Results for Physical Activity Recommendations Met
| Covariate | Odds Ratio Estimate | 95% Confidence Interval | p-value | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Age | 1.09 | 1.00 | 1.18 | .040 | |
| Sex | Male | 0.48 | 0.23 | 1.00 | .049 |
| Female | Reference | ||||
| Annual Income | < $30K | 1.11 | 0.51 | 2.43 | .794 |
| ≥ $30K | Reference | ||||
| Time | 1.57 | 0.81 | 3.06 | .184 | |
| Treatment | SCORRE | 0.93 | 0.42 | 2.03 | .847 |
| Control | Reference | ||||
| Time X Treatment | 0.73 | 0.29 | 1.85 | .505 | |
Note. Physical activity recommendations met was collected at baseline and 8-weeks follow-up. Physical activity recommendations met was measured on a dichotomous yes/no scale. Logistic regression model structure with a Binomial distribution and logit link function.
Table 4.
Results of a Marginal Model with Generalized Estimating Equations Results for Assessing Dietary Change*,**,***
| Covariate | Odds Ratio Estimate | 95% Confidence Interval | p-value | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Age | 0.96 | 0.90 | −1.03 | .270 | |
| Sex | Male | 1.12 | 0.54 | 2.31 | .760 |
| Female | Reference | ||||
| Annual Income | < $30K | 1.06 | 0.54 | 2.08 | .858 |
| ≥ $30K | Reference | ||||
| Time | 0.816 | 0.48 | 1.38 | .447 | |
| Treatment | SCORRE | 0.91 | 0.45 | 1.86 | .804 |
| Control | Reference | ||||
| Time X Treatment | 0.37 | 0.17 | 0.83 | .016 | |
Note. Diet was collected at baseline and 8-week follow-up. Diet was measured on an ordinal 1 thru 5 scale. Ordinal logistic model structure with a multinomial distribution and cumulative logit link function.
Theoretical Outcomes
Changes in health behavior theory variables also were observed from baseline to post-intervention for accuracy of perceived stroke risk (Supplemental Digital Content [SDC] Table 1) and from baseline to post-intervention to 8-week follow-up for knowledge of stroke risk factors, readiness for behavior change, and perceived competence to live a healthy lifestyle (SDC Tables 2, 3, 4). Thirty-three (61%) participants in the intervention group had inaccurate stroke risk perceptions (37% underestimated and 24% overestimated) compared to 25 (48%) in the control group (29% underestimated and 19% overestimated). The odds for participants in the intervention group changing their perception of stroke risk from inaccurate to accurate post-intervention was 10.58 times the odds for the control group, controlling for age, sex, and income (95% CI: 3.99, 28.10, p < .0001). At baseline, mean perceived competence to live a healthy lifestyle was 5.85 (SD = 1.19) for the intervention group and 5.79 (SD = 1.09) for the control group. Using a multilevel model with a gamma distribution for perceived competence to live healthily, the change in competence scores for participants in the intervention group was 1.04 times larger than for the control group, controlling for age, sex, and income (95% CI: 1.01, 1.07, p = .0090). There was no time-by-treatment interaction for knowledge of stroke risk factors and readiness for behavior change. An exploratory analysis with a multilevel ordinal logistic regression model was conducted to investigate the influence of the theoretical variables on changes in dietary components. Higher perceived competence was the only variable associated with an increase in number of healthy dietary components (OR: 0.64, 95% CI: [0.51, 0.81], p = .0002).
Discussion
The SCORRE intervention, designed for young AA, improved their accuracy of perceived stroke risk, perceived competence to live a healthy lifestyle, and lifestyle behaviors, specifically dietary behaviors. Similar nurse-led, community-based interventions that used the AHA LS7 program to counsel/coach individuals at risk of cardiovascular disease found the interventions were feasible and improved health behaviors and cardiovascular health outcomes—but in older adults (Hickey et al., 2019; Murphy et al., 2015). Older, White adults and secondary stroke prevention have been the targets for other successful, nurse-led, community-based interventions (Kosub, 2010; Lawrence et al., 2011). SCORRE is the first intervention, to our knowledge, to target AA aged 20–35 years for primary prevention of stroke.
Another unique aspect of SCORRE is that several studies have examined the perceived risk of stroke and found inaccurate stroke risk perceptions; however, few have tested whether the inaccuracies can be corrected (Aycock et al., 2019). The significant increases in accuracy of perceived stroke risk following SCORRE support the need to further explore the effect of counseling—particularly in young adults—to correct inaccurate risk perceptions and their effect on subsequent behaviors. A more accurate stroke risk perception immediately following SCORRE may have motivated initial behavior change among participants; however, the increase in healthy dietary components was not sustained or reflected. Nonetheless, cardiovascular risk awareness remains an integral concept for prevention.
While perceived competence to live a healthy lifestyle to lower risk of stroke was reasonably high among participants at baseline, providing skill building, role-modeling, and goal setting via SCORRE likely contributed to the higher perceived competence and possible change in dietary behaviors. Perceived competence has been associated with better outcomes (Sheeran et al., 2020), and health care professionals have positively influenced individual perceived competence (Martin et al., 2017). No significant treatment by time effects was found for knowledge of stroke risk factors and readiness for behavior change. Overall, participants had fairly high knowledge of stroke risk factors at baseline, and questionnaires completed by both groups that assessed stroke concepts may have primed participants in the control group. Although knowledge of stroke risk factors was high, many had inaccurate perceptions of their own stroke risk. The study was advertised as a health study, not a stroke study; therefore, participants in both groups may have decided to participate with anticipation of learning about one’s health and possibly improving it. Diary return and completion rates were high for both groups; the daily diaries may have served as an overall reminder and motivator to live healthily.
Overall, most participants receiving SCORRE elected to focus on improving their diets. Participants in SCORRE increased healthy dietary components but not physical activity levels. When we examined subsets based on whether SCORRE participants selected diet or physical activity as the behavior to improve, slightly more than half of the subset improved that behavior. Improving diet and physical activity alone can reduce stroke risk by up to 30%; the positive effect of improved diet and physical activity on changing risk factors such as hypertension and obesity may lead to even greater reductions in stroke risk (Benjamin et al., 2018). Even minimal improvements in single health behavior or incremental improvements in the overall LS7 score are associated with lower risk of incident stroke (Kulshreshtha et al., 2013).
We found that fewer AA men than women participated in the study. As a result, there were not enough male participants to determine whether there were differential effects of the intervention by gender. However, some gender differences at baseline were reported elsewhere (Aycock et al., 2019). A study is currently underway to assess the needs and preferences of young AA men for stroke risk reduction with the goal of tailoring the SCORRE intervention to them. Ensuring that SCORRE is age, culture, and gender appropriate may have the greatest effect on behavior change and ultimately address stroke prevention disparities early among AA. If SCORRE is found to be effective with further testing, SCORRE may serve as a nurse-led model of primary stroke prevention in community (e.g., churches, barbershops, schools) and clinical settings frequented by young adult AA, and nurses can collaborate with other providers to enhance promotion and implementation of SCORRE.
Strengths and Limitations
Several strengths of the study include the focus on primary stroke prevention among young AA, an understudied, increasingly at-risk group, strong internal validity of the randomized controlled design, high retention rates, and the use of valid and reliable measures. However, some study limitations should be considered. The sample consisted of primarily college-educated women with health insurance which limits generalizability. Instead of more sensitive objective measures, self-report measures were used to assess the primary behavioral outcomes. During the 8-week follow-up, all participants’ health behaviors were reassessed, but health indicators were only repeated for those with abnormal values at baseline. Therefore, a follow-up LS7 score was not calculated, and the comparison of perceived versus actual risk of stroke at 8 weeks was not obtained.
Additionally, the small sample limited exploration of outcomes by participants who underestimated versus overestimated their perceived stroke risk. Although the 8-week period was sufficient to observe changes in health behaviors, a longer follow-up (e.g., at least 12 weeks) is warranted to assess sustainability of the behaviors and changes in the physiological health indicators. While this study tested a theory-based intervention using a rigorous study design, enhancements to SCORRE and more rigorous testing are needed to determine effectiveness.
Conclusion
The SCORRE intervention addresses a critical barrier in primary stroke prevention by targeting a group that, despite increased risk, has not received appropriate attention. Traditional cardiovascular risk factors develop during young adulthood; therefore, stroke risk factor awareness and promotion of healthy lifestyles should not be limited to mid-to-late life adults. Expanding opportunities for AA to learn about stroke early in life via SCORRE may help minimize disparities in primary stroke prevention.
Supplementary Material
Acknowledgements:
Research reported in this publication was supported by the National Institutes of Nursing Research, Mentored Research Scientist Development Award 5K01NR015494 (10/2015–7/2019) to first author. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors have no conflicts of interest to report.
Clinical Trial Registration: Stroke Counseling for Risk Reduction (SCORRE); ID# NCT03076125; Registration date 03/10/2017; First participant enrolled 03/28/2017; Website link: https://clinicaltrials.gov/ct2/show/NCT03076125?term=SCORRE&draw=2&rank=1
Ethical Conduct of Research: The study reported in this publication received IRB approval from Georgia State University and all participants provided written informed consent prior to data collection.
Contributor Information
Dawn M. Aycock, Georgia State University School of Nursing, Atlanta, GA.
Patricia C. Clark, Georgia State University School of Nursing, Atlanta, GA.
Matthew J. Hayat, Georgia State University School of Public Health, Atlanta, GA.
Laura F. Salazar, Georgia State University School of Public Health, Atlanta, GA.
Michael Eriksen, Georgia State University School of Public Health, Atlanta, GA.
References
- Aigner A, Grittner U, Rolfs A, Norrving B, Siegerink B, & Busch MA (2017). Contribution of established stroke risk factors to the burden of stroke in young adults. Stroke, 48, 1744–1751. 10.1161/STROKEAHA.117.016599 [DOI] [PubMed] [Google Scholar]
- American Heart Association. (2011). Young adults’ beliefs about their health clash with risky behaviors.
- American Heart Association. (2018). Life’s Simple 7. Retrieved from https://www.heart.org/en/healthy-living/healthy-lifestyle/my-life-check--lifes-simple-7
- American Stroke Association. (2021). Stroke Risk Factors. Retrieved from https://www.stroke.org/en/about-stroke/stroke-risk-factors
- Aycock DM, & Clark PC (2016). Incongruence between perceived long-term risk and actual risk of stroke in rural African Americans. Journal of Neuroscience Nursing, 48, 35–41. 10.1097/JNN.0000000000000180 [DOI] [PubMed] [Google Scholar]
- Aycock DM, Clark PC, & Araya S (2019). Measurement and outcomes of the perceived risk of stroke: A review. Western Journal of Nursing Research, 41, 134–154. 10.1177/0193945917747856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aycock DM, Clark PC, & Hayat MJ (2017). Reducing stroke risk in young adult African Americans: A feasibility study. Research in Nursing & Health, 40, 153–164. 10.1002/nur.21776 [DOI] [PubMed] [Google Scholar]
- Aycock DM, Hayat MJ, Helvig A, Dunbar SB, & Clark PC (2018). Essential considerations in developing attention control groups in behavioral research. Research in Nursing & Health, 41, 320–328. 10.1002/nur.21870 [DOI] [PubMed] [Google Scholar]
- Aycock DM, Kirkendoll KD, Coleman KC, Clark PC, Albright KC, & Alexandrov AW (2015). Family history of stroke among African Americans and its association with risk factors, knowledge, perceptions, and exercise. Journal of Cardiovascular Nursing, 30, e1–e6. 10.1097/JCN.0000000000000125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, … Muntner P (2018). Heart disease and stroke statistics—2018 update: A report from the American Heart Association. Circulation, 137, e67–e492. 10.1161/CIR.0000000000000558 [DOI] [PubMed] [Google Scholar]
- Block G, Hartman AM, & Naughton D (1990). A reduced dietary questionnaire: Development and validation. Epidemiology, 1, 58–64. 10.1097/00001648-199001000-00013 [DOI] [PubMed] [Google Scholar]
- Brown J (2013). A review of the evidence on technology-based interventions for the treatment of tobacco dependence in college health. Worldviews on Evidence-Based Nursing, 10, 150–162. 10.1111/wvn.12000 [DOI] [PubMed] [Google Scholar]
- Caraballo RS, Giovino GA, Pechacek TF, & Mowery PD (2001). Factors associated with discrepancies between selfreports on cigarette smoking and measured serum cotinine levels among persons aged 17 years or older: Third National Health and Nutrition Examination Survey, 1988–1994. American Journal of Epidemiology, 153, 807–814. doi: 10.1.1.606.2817 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2009). State-specific secondhand smoke exposure and current cigarette smoking among adults―United States, 2008. MMWR Morbidity Mortality Weekly Report, 58, 1232–1235. [PubMed] [Google Scholar]
- Cruz-Flores S, Rabinstein A, Biller J, Elkind MSV, Griffith P, Gorelick PB, Howard G, Leira EC, Morgenstern LB, Ovbiagele B, Peterson E, Rosamond W, Trimble B, & Valderrama AL (2011). Racial-ethnic disparities in stroke care: The American experience: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 42, 2091–2116. 10.1161/STR.0b013e3182213e24 [DOI] [PubMed] [Google Scholar]
- Feng W, Nietert PJ, & Adams RJ (2009). Influence of age on racial disparities in stroke admission rates, hospital charges, and outcomes in South Carolina. Stroke, 40, 3096–3101. 10.1161/STROKEAHA.109.554535 [DOI] [PubMed] [Google Scholar]
- George MG, Tong X, & Bowman BA (2017). Prevalence of cardiovascular risk factors and strokes in young adults. JAMA Neurology, 74, 695–703. 10.1001/jamaneurol.2017.0020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godin G, & Shephard RJ (1985). A simple method to measure exercise behavior in the community. Canadian Journal of Applied Sports Science, 10, 141–146. [PubMed] [Google Scholar]
- Gutierrez J, & Williams OA (2014). A decade of racial and ethnic stroke disparities in the United States. Neurology, 82, 1080–1082. 10.1212/WNL.0000000000000237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayat MJ, & Hedlin H (2012). Modern statistical modeling approaches for analyzing repeated-measures data. Nursing Research, 61, 188–194. 10.1097/NNR.0b013e31824f5f58 [DOI] [PubMed] [Google Scholar]
- Hickey KT, Wan E, Garan H, Biviano AB, Morrow JP, Sciacca RR, Reading M, Koleck TA, Caceres B, Zhang Y, Goldenthal I, Riga TC, & Masterson Creber R (2019). A nurse-led approach to improving cardiac lifestyle modification in an atrial fibrillation population. Journal of Innovations in Cardiac Rhythm Management, 10, 3826–3835. 10.19102/icrm.2019.100902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs DR Jr., Ainsworth BE, Hartman TJ, & Leon AS (1993). A simultaneous evaluation of 10 commonly used physical activity questionnaires. Medicine & Science in Sports & Exercise, 25, 81–91. 10.1249/00005768-199301000-00012 [DOI] [PubMed] [Google Scholar]
- Kissela BM, Khoury JC, Alwell K, Moomaw CJ, Woo D, Adeoye O, Flaherty ML, Khatri P, Ferioli S, La Rosa FDLR, Broderick JP, & Kleindorfer DO (2012). Age at stroke: Temporal trends in stroke incidence in a large, biracial population. Neurology, 79, 1781–1787. 10.1212/WNL.0b013e318270401d [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosub E. (2010). Community stroke prevention programs: An overview. Journal of Neuroscience Nursing, 42, 143–149. 10.1097/jnn.0b013e3181d4a395 [DOI] [PubMed] [Google Scholar]
- Kulshreshtha A, Vaccarino V, Judd SE, Howard VJ, McClellan WM, Muntner P, Hong Y, Safford MM, Goyal A, & Cushman M (2013). Life’s Simple 7 and risk of incident stroke: The reasons for geographic and racial differences in stroke study. Stroke, 44, 1909–1914. 10.1161/STROKEAHA.111.000352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence M, Kerr S, McVey C, & Godwin J (2011). A systematic review of the effectiveness of secondary prevention lifestyle interventions designed to change lifestyle behaviour following stroke. JBI Library of Systematic Reviews, 9, 1782–1827. 10.11124/jbisrir-2011-106 [DOI] [PubMed] [Google Scholar]
- Length R. (2018). Java applets for power and sample size. http://www.stat.uiowa.edu/~rlenth/Power/
- Linder AD, Lui H-Y, Woodson-Smith A, & Jung J (2018). Physical activity behaviors among non-traditional and traditional college students: An application of Ajzen’s theory of planned behavior. Negro Educational Review, 69, 33–50, 142–143. [Google Scholar]
- Liu K, Daviglus ML, Loria CM, Colangelo LA, Spring B, Moller AC, & Lloyd-Jones DM (2012). Healthy lifestyle through young adulthood and the presence of low cardiovascular disease risk profile in middle age: The Coronary Artery Risk Development in (Young) Adults (CARDIA) study. Circulation, 125, 996–1004. 10.1161/CIRCULATIONAHA.111.060681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, … Rosamond WD (2010). Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic impact goal through 2020 and beyond. Circulation, 121, 586–613. 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- Martin JJ, Byrd B, Wooster S, & Kulik N (2017). Self-determination theory: The role of the health care professional in promoting mindfulness and perceived competence. Journal of Applied Biobehavioral Research, 22, e12072. 10.1111/jabr.12072 [DOI] [Google Scholar]
- Miller JM, Wolfson J, Laska MN, Nelson TF, & Pereira MA (2018). The Minne-Loppet Motivation Study: An intervention to increase motivation for outdoor winter physical activity in ethnically and racially diverse elementary schools. American Journal of Health Promotion, 32, 1706–1713. 10.1177/0890117118768119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy MP, Coke L, Staffileno BA, Robinson JD, & Tillotson R (2015). Improving cardiovascular health of underserved populations in the community with Life’s Simple 7. Journal of the American Association of Nurse Practitioners, 27, 615–623. 10.1002/2327-6924.12231 [DOI] [PubMed] [Google Scholar]
- Perrin S. (2019). Factors associated with dietary patterns for stroke prevention in young adult African Americans. Scholarworks. Retrieved January 8, 2022 from https://scholarworks.gsu.edu/nursing_diss/52/
- Planned Parenthood. (2016). Sexual health series: What you should know about safer sex. https://marketplace.plannedparenthood.org/marketplace/brochures/sexual-health.html
- Reed JA, & Phillips DA (2005). Relationships between physical activity and the proximity of exercise facilities and home exercise equipment used by undergraduate university students. Journal of American College Health, 53, 285–290. 10.3200/JACH.53.6.285-290 [DOI] [PubMed] [Google Scholar]
- Rosenstock IM (1974). Historical origins of the health belief model. Health Education Monographs, 2, 328–335. 10.1177/109019817400200403 [DOI] [PubMed] [Google Scholar]
- Sheeran P, Wright CE, Avishai A, Villegas ME, Lindemans JW, Klein W, Rothman AJ, Miles E, & Ntoumanis N (2020). Self-determination theory interventions for health behavior change: Meta-analysis and meta-analytic structural equation modeling of randomized controlled trials. Journal of consulting and clinical psychology, 88(8), 726–737. 10.1037/ccp0000501 [DOI] [PubMed] [Google Scholar]
- Tsivgoulis G, Putaala J, Sharma V, Balucani C, Martin-Schild S, Giannopoulos S, Batala L, Krogias C, Palazzo P, Shahripour RB, Arvaniti C, Barlinn K, Strbian D, Haapaniemi E, Flamouridou M, Vadikolias K, Heliopoulos I, Voumvourakis K, Triantafyllou N, … Alexandrov AV (2014). Racial disparities in early mortality in 1,134 young patients with acute stroke. Neurological Sciences, 35, 1041–1049. 10.1007/s10072-014-1640-9 [DOI] [PubMed] [Google Scholar]
- Warner L, Klausner JD, Rietmeijer CA, Malotte CK, O’Donnell L, Margolis AD, Greenwood GL, Richardson D, Vrungos S, O’Donnell CR, Borkowf CB, & Safe in the City Study Group (2008). Effect of a brief video intervention on incident infection among patients attending sexually transmitted disease clinics. PLoS medicine, 5(6), e135. 10.1371/journal.pmed.0050135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein ND (1988). The precaution adoption process. Health Psychology, 7, 355–386. 10.1037/0278-6133.7.4.355 [DOI] [PubMed] [Google Scholar]
- Weinstein PK, Amirkhosravi A, Angelopoulos TJ, Bushy A, Covelli MM, Dennis KE (2014). Reducing cardiovascular risk in women with lupus: Perceptions of risk and predictors of risk-reduction behaviors. Journal of Cardiovascular Nursing, 29, 130–139. 10.1097/JCN.0b013e31827f0d53 [DOI] [PubMed] [Google Scholar]
- Williams GC, Freedman ZR, & Deci EL (1998). Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care, 21, 1644–1651. 10.2337/diacare.21.10.1644 [DOI] [PubMed] [Google Scholar]
- Yahya T, Jilani MH, Khan SU, Mszar R, Hassan SZ, Blaha MJ, Blankstein R, Virani SS, Johansen MC, Vahidy F, Cainzos-Achirica M, & Nasir K (2020). Stroke in young adults: Current trends, opportunities for prevention and pathways forward. American Journal of Preventive Cardiology, 3, 100085. 10.1016/j.ajpc.2020.100085 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


