Abstract
Objectives:
It has been reported that job demands affect sleep, but how different levels of job demands affect sleep remains unclear. We examined whether curvilinear relationships exist between job demands and multiple sleep health outcomes
Design:
Cross-sectional analyses with linear and quadratic effects, using self-administered survey data
Setting:
A national sample of U.S. adults
Participants:
Workers from Midlife in the United States Study (MIDUS2; n=2,927)
Measurements:
The Job Content Questionnaire assessed overall and five specific aspects of job demands (intensity, role conflict, work overload, time pressure, and interruptions). Habitual sleep health patterns across five dimensions (regularity, satisfaction/quality, daytime alertness, efficiency, and duration) were assessed. Age, sex, race/ethnicity, marital/partnered status, education, job tenure, work hours, body mass index, smoking status, and study sample were covariates
Results:
There were significant linear and quadratic relationships between job demands and sleep outcomes. Specifically, the linear effects indicated that participants with higher job demands had worse sleep health, such as shorter duration, greater irregularity, greater inefficiency, and more sleep dissatisfaction. The quadratic effects, however, indicated that sleep regularity and efficiency outcomes were the best when participants’ job demands were moderate rather than too low or too high. These effects were found for overall job demands as well as for specific aspects of job demands. Stratified analyses further revealed that these curvilinear associations were mainly driven by participants with low job control
Conclusions:
Moderate levels of job demands, especially if combined with adequate job control, are related to optimal sleep health.
Keywords: job demands, job control, job strain, sleep, MIDUS, non-linear relationships
Introduction
Sleep is important to health, and poor sleep is related to negative health outcomes including cardiovascular disease1, dementia2, and mortality1. Therefore, identifying contributors to poor sleep is important to explain downstream health outcomes resulting from poor sleep. Sleep can be influenced by multiple factors at macro (e.g., environmental), social, and individual levels3. Within the social level, work is important and has received much research attention in relation to sleep. Structural aspects of work, including long working hours4 and shift work5, are negatively related to sleep outcomes. While many studies report the negative impact of work-related stressors on sleep6, a complete lack of work-related stressors may also reflect poor engagement at work, which may have its own negative consequences7. Similarly, the job demands-resources theory8 predicts that low job demands under certain conditions result in negative outcomes such as boredom9 and apathy. Additionally, certain types of work-related stressors appear to be more strongly related to negative sleep outcomes than others10. Yet, most research examines only the linear relationship between work-related stressors and sleep (i.e., more work is bad for sleep). This approach may provide biased results if there exists a range of work-related stressors that best promote health, including sleep, in working populations.
There is a theoretical basis for the possibility that some stress at work may facilitate health outcomes. For example, the hormetic stress concept11, motivated by the Yerkes-Dodson Law12, indicates that moderate, relative to low or high, levels of stressor exposure may relate to optimal performance or better health outcomes. Additionally, an ideal amount of stressors may benefit health13. This may apply to sleep health. Much research on work-related stressors is guided by the job demands-control model14, which posits that aspects of work can be categorized as job demands or as control resources. According to this model, many work characteristics (e.g., long work hours, flexible hours, job insecurity, salary) are closely related to either job demands or to control, and the combination of high demands with low control results in job strain14. Indeed, job demands or job strain (i.e., work-related stressors) are the strongest predictors of employee health and well-being outcomes15,16. Recent systematic reviews show that high job demands and job strain are related to sleep disturbances17 and poor sleep quality18. Both demands and strain have evidenced negative linear relationships with sleep outcomes in working adults from Europe19 and Asia20,21. Yet, there may be untested non-linear relationships, such that the levels of sleep health are lower when job demands are too little or too high. For example, research on job autonomy and well-being illustrates that both too much and too little autonomy may relate to poorer well-being22. Regarding non-linear relationships between job demands and sleep outcomes, one study found non-significant quadratic effects for the dimensions of the job demands-control-support model23, but assessed only sleep quality, limiting conclusions regarding other aspects of sleep health. Moreover, most studies assessed job demands broadly, preventing examination of whether specific aspects of job demands may relate to sleep health outcomes both linearly and non-linearly.
The Current Study
Motivated by the hormetic stress concept11, we aimed to assess linear and curvilinear relationships between job demands and sleep health outcomes using a national sample of workers. In examining these relationships, we used an overall job demands composite as well as the individual items of the job demands scale. We also assessed five dimensions of sleep health (i.e., regularity, satisfaction, alertness, efficiency, and duration24). We expected that moderate job demands would be associated with better sleep outcomes, with both low and high job demands associated with worse sleep outcomes. Additionally, we examined differences by the level of job control to tap into the job strain concept14 (i.e., high job demands, low job control).
Participants and Methods
Data Source and Participants
We used data from the National Survey of Midlife in the United States (MIDUS; www.midus.wisc.edu), which assesses behavioral, psychological, and social factors related to variation in mental and physical health in the process of aging25. Specifically, data were from the first longitudinal follow-up (MIDUS2; in 2004–2006) and the refresher sample (MIDUS Refresher; in 2011–2014). Data from the Milwaukee, Wisconsin subsamples that collected information on Black/African American participants were included in the MIDUS2 and MIDUS Refresher samples. All variables were self-reported. Of the combined MIDUS2 and MIDUS Refresher samples (n=9,640), participants were excluded if they (1) did not complete the self-administered questionnaire (SAQ) that included job demands questions (n=2,278), (2) were not currently paid workers (n=3,576), (3) did not work at least 30 hours per week (n=735), and (4) did not have valid data for the job demands composite question (n=124). Thus, the final analytic sample was 2,927 workers. The MIDUS study was approved by all appropriate Institutional Review Boards, and all MIDUS participants provided informed consent. The current study used publicly available, de-identified data and was exempt from local IRB review.
Measures
Sleep Health
Five dimensions of sleep health were included as the dependent variables. These dimensions follow the Ru-SATED model24, which includes sleep regularity, satisfaction, alertness, timing, efficiency, and duration. Sleep timing was not collected in the MIDUS survey; therefore, we did not include this dimension. In the current study, we refer to the available sleep variables as irregularity, dissatisfaction, nap frequency (a proxy for daytime alertness), inefficiency, and duration, respectively.
Sleep irregularity was measured as the absolute value of the difference between weekday and weekend sleep duration; higher scores indicated more irregular sleep. Sleep dissatisfaction (α=.80) was measured as the mean of four items (feeling unrested during the day; trouble falling asleep; waking up during the night and having difficulty going back to sleep; waking up too early in the morning and being unable to go back to sleep) assessed on a 1 to 5 scale; higher scores indicated more dissatisfying sleep. Nap frequency was measured through a question indicating the number of naps that lasted 5+ minutes participants would take during a usual week; higher scores indicated more frequent naps (i.e., less daytime alertness). We assessed nap frequency as it was the only available survey measure related to daytime alertness. In the original conceptualization of sleep health24, alertness, sleepiness, and napping were grouped, because these concepts are all related to levels of homeostatic sleep pressure26. Homeostatic sleep pressure accumulates during the day with continued wakefulness26. Sleep propensity and sleepiness are driven by this homeostatic process and increase the likelihood of napping27. Napping subsequently reduces homeostatic sleep pressure28 and increases alertness and vigilance29.Yet, napping has been related to several negative outcomes27, including cardiovascular events30,31, Alzheimer’s disease32, and mortality30, potentially because it is often accompanied by poor nighttime sleep31. As a result, napping has garnered evidence for its utility as a sleep health measure24 and a proxy for less daytime alertness. Sleep inefficiency was measured by sleep onset latency with a question assessing the time it takes participants to fall asleep at bedtime; higher scores indicated more inefficient sleep (in hours). While some previous research used wake after sleep onset (WASO) together with sleep onset latency33, we chose to use sleep onset latency alone as actigraphy-measured WASO was only available in a sub-sample of MIDUS. Sleep onset latency has been frequently used to indicate sleep inefficiency34. Finally, sleep duration was measured with a question asking how much sleep participants usually get at night on weekdays (in hours).
Job Demands
Job demands indicators, the independent variables, were assessed using the Job Content Questionnaire (JCQ35). Specifically, as suggested previously35, the following five items from the Demands Scale of the JCQ35 were used as individual indicators of job demands, and the composite of the five items was used as the indicator for overall demands: Participants reported how often (1=all of the time, 2=most of the time, 3=some of the time, 4=little of the time, 5=never) the following aspects of their jobs occurred, on average or in the past year: (a) intensity (“do you have to work very intensively?”); (b) role conflict (“do different people or groups at work demand things from you that you think are hard to combine?”); (c) work overload (“do you have too many demands made on you?”); (d) time pressure (“do you have enough time to get everything done?”); and (e) interruptions (“do you have lots of interruptions?”). Intensity, role conflict, work overload, and interruptions were reverse coded such that higher scores indicated more demands. The overall demands item summed the five job demands questions with higher scores indicating higher demands (α=.74).
Job Control
Job control was assessed using the JCQ35-based scales for skill discretion and decision authority, plus an additional question separate from the JCQ that asked participants about their perception of overall job control. The skill discretion score summed three items measuring how often on average (a) participants learned new things at work, (b) participants’ work demanded a high level of skill or expertise, and (c) their job provided them with a variety of things that interested them. The decision authority score summed six items measuring how often participants had (a) to initiate things, (b) a choice in deciding how to do work tasks, (c) a choice in deciding what tasks to do, (d) a say in decisions about their work, (e) a say in planning their work environment, and how often participants could control the amount of time they spent on tasks. The one question that was separate from the JCQ asked how much control participants thought they had over their work situation (0=no control at all to 10=very much control). The two scale scores and the single item were first standardized with z-scores then averaged to create the job control factor (α=.67). Job control was then dichotomized (low job control < median; high job control ≥ median), following prior research36.
Covariates
We considered sociodemographic and health-related covariates that may be associated with work experiences and sleep. Sociodemographic variables included age (years), sex (female=0; male=1), race/ethnicity (non-Hispanic White=0; Other race/ethnicity=1), marital/partnered status (unpartnered [i.e., separated, divorced, widowed, never married, not living with partner]=0; married/cohabitating=1), final education level (1=no school to 12=professional degrees), job tenure (years), and average work hours. Health-related variables included body mass index (BMI) and current smoking status (no=0; yes=1). Additionally, to account for potential sample differences, we adjusted for the sample identifier (MIDUS2=0; MIDUS Refresher=1). Continuous covariates were centered at the sample means.
Statistical Analyses
First, we assessed our main study variables for normality. Results indicated that variables were within an acceptable range, based on previous research with other continuous health variables37,38 (i.e., <3 for skewness and <10 for kurtosis39), to proceed with analyses assuming normality. Second, we conducted descriptive statistics and intercorrelations of study variables. Next, separate hierarchical regression analyses were conducted to assess the relationship between the various job demands indicators and each of the five sleep health dimensions. The six job demands indicators (overall composite + 5 individual items) were centered at the sample mean for analyses. Quadratic effects of the job demands indicators were created by multiplying each of the centered job demands items by itself (e.g., intensity × intensity). Inclusion of quadratic effects improved model fit when significant quadratic effects were found, as indicated by smaller RMSE values and larger adjusted R2 values. Adding cubic effects did not significantly improve model fit—thus, cubic effects were not included in the models. Unadjusted models assessed the linear and quadratic effects of each job demands indicator on sleep health. Adjusted models included covariate effects (Model 1), linear effects of job demands (Model 2), and quadratic effects of job demands (Model 3). Missing data were excluded through listwise deletion for each analysis. To tap into the job strain concept14, we also conducted analyses stratified by level of job control (high and low) to assess whether the effects of demands may depend on job resources available to participants. Finally, dose-response relationships were assessed between job demands and sleep health for all significant quadratic effects. All analyses were conducted with SAS Version 9.4, with significance assessed at p<.05 (two-tailed).
Results
Table 1 includes descriptive statistics of study variables. Participants were approximately 48 years old on average (SD=10.04, Range=24–81), with slightly more than half the sample being male (51.62%), and a majority of the sample being non-Hispanic White (82.32%). The sample was well-educated (≥4-year college education=48.39%; ≥high school diploma or equivalent=96.96%). Most of the sample were either married or cohabitating (72.56%) and were not current smokers (86.16%).
Table 1.
Descriptive Statistics for Study Variables
| Variable | N | Missing | M/N | SD/% |
|---|---|---|---|---|
| Sociodemographic and Health Variables | ||||
| Sample | 2927 | 0 | ||
| MIDUS2 | 1847 | 63.10% | ||
| MIDUS Refresher | 1080 | 36.90% | ||
| Age, years | 2927 | 0 | 48.03 | 10.04 |
| Sex | 2927 | 0 | ||
| Male | 1511 | 51.62% | ||
| Female | 1416 | 48.38% | ||
| Race/Ethnicity | 2919 | 8 | ||
| Non-Hispanic White | 2403 | 82.32% | ||
| Other | 516 | 17.68% | ||
| Marital/Partnered Status | 2923 | 4 | ||
| Not married or partnereda | 802 | 27.44% | ||
| Married or Cohabitating | 2121 | 72.56% | ||
| Educationb | 2924 | 3 | ||
| Less Than High School | 89 | 3.04% | ||
| High School Graduate or Equivalent | 603 | 20.62% | ||
| Some College or 2-Year Degree | 817 | 27.94% | ||
| College Graduate (4+ Years) or Higher | 1415 | 48.39% | ||
| Job Tenure, years | 2877 | 50 | 24.80 | 11.16 |
| Work Hours | 2927 | 0 | 43.28 | 8.02 |
| Body Mass Index | 2800 | 127 | 28.37 | 6.16 |
| Current Smoker | 2927 | 0 | ||
| No | 2522 | 86.16% | ||
| Yes | 405 | 13.84% | ||
| Job Demands Variables | ||||
| Job Demands Composite | 2927 | 0 | 15.41 | 3.12 |
| Intensity | 2919 | 8 | 3.72 | 0.77 |
| Role Conflict | 2917 | 10 | 2.67 | 0.91 |
| Work Overload | 2926 | 1 | 2.89 | 0.87 |
| Time Pressure | 2923 | 4 | 2.63 | 0.98 |
| Interruptions | 2923 | 4 | 3.50 | 0.93 |
| Job Control Variables | ||||
| Job Control | 2917 | 10 | 6.67 | 2.41 |
| Skill Discretion Composite | 2921 | 6 | 10.67 | 2.18 |
| Decision Authority Composite | 2921 | 6 | 21.80 | 4.39 |
| Job Control Composite | 2927 | 0 | 0.00 | 0.78 |
| Sleep Health Variables | ||||
| Sleep Duration | 2915 | 12 | 6.82 | 1.09 |
| Sleep Irregularity | 2866 | 61 | 1.02 | 1.12 |
| Sleep Inefficiency | 2889 | 38 | 0.39 | 0.37 |
| Nap Frequency | 2900 | 27 | 1.47 | 2.16 |
| Sleep Dissatisfaction | 2917 | 10 | 2.46 | 0.82 |
Includes separated, divorced, widowed, never married, not living with partner
There are 12 educational categories in MIDUS that we have grouped into the four categories
Note. Abbreviations: M = mean. SD = standard deviation. Intensity = Work intensively at job. Role Conflict = Work demands hard to combine. Work Overload = Too many demands at job. Time Pressure= Time to get everything done at job. Interruptions = Lot of interruptions at job. Higher scores indicate higher demands
Supplemental Table 1 includes correlations among the main study variables. Job control was weakly related to job demands indicators (rs=.06 to .15). The general associations between job demands indicators and sleep health dimensions indicated higher demands were typically related to poorer sleep health, though not all correlations were significant. One exception was found for nap frequency, in which higher job demands were related to lower nap frequency, but the magnitude of the correlation was very small (r=−.05). Higher job control was related to better sleep health. Correlations among sleep health dimensions were in the expected directions; yet, the relationships were weak overall (rs<|.25|) except a moderate correlation between sleep inefficiency and sleep dissatisfaction (r=.45), indicating that each dimension conveys unique information about sleep health.
Linear and Quadratic Relationships Between Job Demands and Sleep Health
Table 2 includes results from unadjusted and adjusted models for sleep duration. Controlling for study sample, age, sex, race/ethnicity, marital/partnered status, education, job tenure, work hours, BMI, and smoking status, significant linear associations were found for two of the job demands indicators. Specifically, higher overall job demands (b=−0.02, SE=0.01, p=.014) and intensity (b=−0.09, SE=0.03, p=.002) were related to shorter sleep duration. No significant quadratic effects were found in fully adjusted models (ps≥.054).
Table 2.
Linear and Quadratic Associations Between Job Demands and Sleep Duration
| Variable | Unadjusted Sleep Duration | Adjusted Sleep Duration | ||||
|---|---|---|---|---|---|---|
| b | SE | p | b | SE | p | |
| Overall Demands | −0.01 | 0.01 | .032 | −0.02 | 0.01 | .014 |
| Overall Demands2 | −0.002 | 0.001 | .259 | −0.001 | 0.001 | .652 |
| Intensity | −0.09 | 0.03 | <.001 | −0.09 | 0.03 | .002 |
| Intensity2 | −0.01 | 0.02 | .662 | 0.002 | 0.02 | .927 |
| Role Conflict | 0.01 | 0.02 | .689 | −0.003 | 0.02 | .906 |
| Role Conflict2 | −0.05 | 0.02 | .003 | −0.04 | 0.02 | .054 |
| Work Overload | −0.03 | 0.02 | .203 | −0.03 | 0.02 | .220 |
| Work Overload2 | −0.05 | 0.02 | .005 | −0.03 | 0.02 | .074 |
| Time Pressure | −0.01 | 0.02 | .603 | −0.03 | 0.02 | .274 |
| Time Pressure2 | −0.03 | 0.02 | .090 | −0.01 | 0.02 | .431 |
| Interruptions | −0.03 | 0.02 | .116 | −0.04 | 0.02 | .050 |
| Interruptions2 | −0.03 | 0.02 | .172 | −0.01 | 0.02 | .604 |
Note. Overall job demands and specific items were entered in separate models. Bolded values indicate significant effects. Abbreviations: b = unstandardized regression estimate. SE = standard error. Overall Demands = Job demands composite score (n = 2915 unadjusted; n = 2734 adjusted). Intensity = Work intensively at job (n = 2908 unadjusted; n = 2729 adjusted). Role Conflict = Work demands hard to combine (n = 2905 unadjusted; n = 2727 adjusted). Work Overload = Too many demands at job (n = 2914 unadjusted; n = 2733 adjusted). Time Pressure=Time to get everything done at job (n = 2912 unadjusted; n = 2732 adjusted). Interruptions = Lot of interruptions at job (n = 2911 unadjusted; n = 2731 adjusted). Adjusted models controlled for study sample, age, sex, race/ethnicity, marital status, education, job tenure, work hours, body mass index, and whether the participant currently smoked. Continuous covariates and main predictors were centered at the sample mean
Table 3 includes results from adjusted models for sleep irregularity, sleep inefficiency, nap frequency, and sleep dissatisfaction (unadjusted effects in Supplemental Table 2). Beginning with sleep irregularity, in fully adjusted models, there were linear associations between each of the six job demands indicators and sleep irregularity, such that higher job demands overall and each domain (intensity, role conflict, work overload, time pressure, and interruptions) were related to more irregular sleep. There were also significant quadratic effects of overall demands and work overload on sleep irregularity (Figure 1A and B). Sleep was most regular around moderate levels of both overall demands and work overload.
Table 3.
Linear and Quadratic Associations Between Job Demands and Sleep Health Dimensions
| Variable | Sleep Irregularity | Nap Frequency | ||||
|---|---|---|---|---|---|---|
| b | SE | p | b | SE | p | |
| Overall Demands | 0.03 | 0.01 | <.001 | −0.01 | 0.01 | .548 |
| Overall Demands2 | 0.003 | 0.002 | .031 | −0.004 | 0.003 | .187 |
| Intensity | 0.08 | 0.03 | .006 | −0.11 | 0.05 | .042 |
| Intensity2 | 0.03 | 0.03 | .185 | −0.09 | 0.05 | .067 |
| Role Conflict | 0.06 | 0.03 | .018 | 0.07 | 0.05 | .137 |
| Role Conflict2 | 0.03 | 0.02 | .110 | −0.03 | 0.04 | .371 |
| Work Overload | 0.06 | 0.03 | .017 | 0.03 | 0.05 | .605 |
| Work Overload2 | 0.04 | 0.02 | .039 | −0.06 | 0.04 | .145 |
| Time Pressure | 0.05 | 0.02 | .027 | −0.04 | 0.05 | .426 |
| Time Pressure2 | 0.02 | 0.02 | .316 | −0.04 | 0.04 | .285 |
| Interruptions | 0.07 | 0.02 | .003 | −0.05 | 0.05 | .287 |
| Interruptions2 | 0.04 | 0.02 | .078 | −0.04 | 0.04 | .251 |
| Sleep Inefficiency | Sleep Dissatisfaction | |||||
| b | SE | p | b | SE | P | |
| Overall Demands | 0.005 | 0.002 | .048 | 0.04 | 0.01 | <.001 |
| Overall Demands2 | 0.001 | 0.001 | .246 | −0.0003 | 0.001 | .775 |
| Intensity | 0.02 | 0.01 | .011 | 0.06 | 0.02 | .003 |
| Intensity2 | 0.001 | 0.01 | .920 | −0.01 | 0.02 | .623 |
| Role Conflict | 0.01 | 0.01 | .505 | 0.10 | 0.02 | <.001 |
| Role Conflict2 | 0.01 | 0.01 | .124 | −0.01 | 0.01 | .275 |
| Work Overload | 0.02 | 0.01 | .054 | 0.16 | 0.02 | <.001 |
| Work Overload2 | 0.02 | 0.01 | <.001 | −0.01 | 0.01 | .695 |
| Time Pressure | −0.003 | 0.01 | .725 | 0.08 | 0.02 | <.001 |
| Time Pressure2 | 0.002 | 0.01 | .781 | −0.02 | 0.01 | .110 |
| Interruptions | 0.02 | 0.01 | .048 | 0.09 | 0.02 | <.001 |
| Interruptions2 | −0.005 | 0.01 | .461 | −0.02 | 0.01 | .102 |
Note. Sample sizes for analyses ranged from n = 2685 to n = 2737. Overall job demands and specific items were entered in separate models. Bolded values indicate significant effects. Abbreviations: b = unstandardized regression estimate. SE = standard error. Overall Demands = Job demands composite score. Intensity = Work intensively at job. Role Conflict = Work demands hard to combine. Work Overload = Too many demands at job. Time Pressure = Time to get everything done at job. Interruptions = Lot of interruptions at job. Models controlled for study sample, age, sex, race/ethnicity, marital status, education, job tenure, work hours, body mass index, and whether the participant currently smoked. Continuous covariates and main predictors were centered at the sample mean
Figure 1.
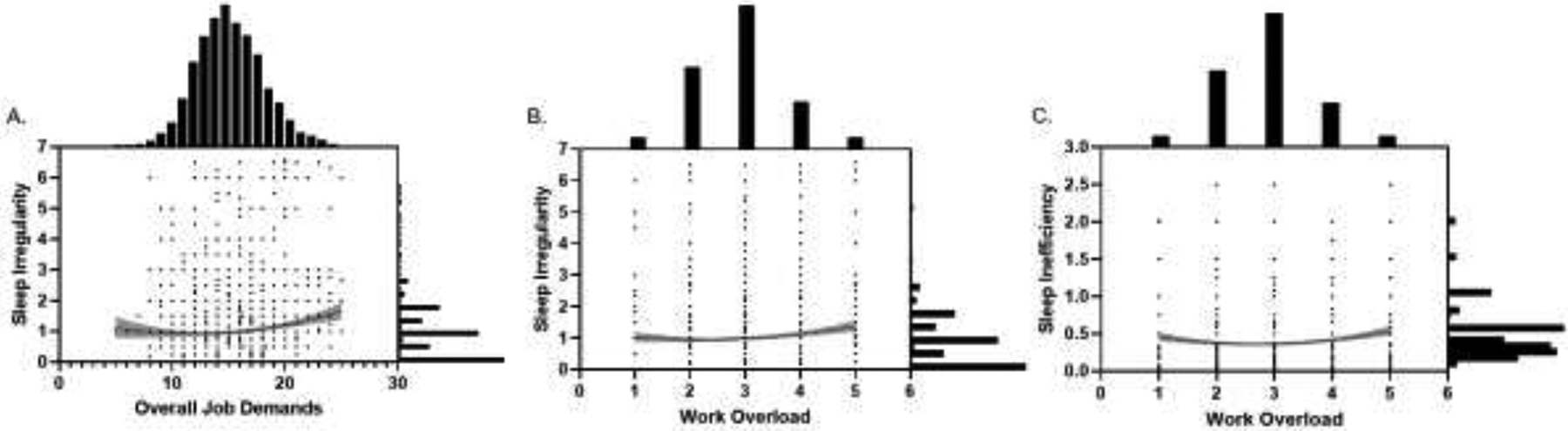
Curvilinear Relationships Between Job Demands Indicators and Sleep Health Dimensions. Overall job demands (M=15.41) and work overload (M=2.89) were mean centered for analyses. Work overload represents the frequency (1=never, 2=little of the time, 3=some of the time, 4=most of the time, 5=all of the time) with which participants had too many demands made on them. Overall job demands represents the composite of the 5 job demands indicators (range = 5 to 25). Higher values on sleep health variables represent poorer sleep. All figures include bar graphs with frequency (%) of responses for sleep health (right) and job demands (top). A scatterplot represents the responses participants provided. Shaded regions represent 95% confidence intervals. A) A significant quadratic relationship exists between overall job demands and sleep irregularity (b=0.003, SE=0.002, p<.001), such that moderate demands were associated with more regular sleep. B) A significant quadratic relationship exists between work overload and sleep irregularity (b=0.04, SE=0.02, p=.039), such that moderate demands were associated with more regular sleep. C) A significant quadratic relationship exists between work overload and sleep inefficiency (b=0.02, SE=0.01, p<.001), such that moderate demands were associated with more efficient sleep.
Next, results for sleep inefficiency revealed significant linear relationships, such that higher overall demands (b=0.005, SE=0.002, p=.048), intensity (b=0.02, SE=0.01, p=.011), and interruptions (b=0.02, SE=0.01, p=.048) were related to more inefficient sleep. A significant quadratic relationship appeared between work overload and sleep inefficiency (b=0.02, SE=0.01, p<.001). Figure 1C illustrates that sleep inefficiency was lowest around moderate levels of work overload. Results for nap frequency revealed a significant linear association with intensity (b=0.11, SE=0.05, p=.042), with more intense work associated with less frequent naps (i.e., more alertness). There were no significant quadratic relationships between any of the job demands indicators and nap frequency (ps≥.067).
Finally, fully adjusted models for sleep dissatisfaction revealed linear relationships between all six job demands indicators and sleep dissatisfaction. Higher overall demands (b=0.04, SE=0.01, p<.001), intensity (b=0.06, SE=0.02, p=.003), role conflict (b=0.10, SE=0.02, p<.001), work overload (b=0.16, SE=0.02, p<.001), time pressure (b=0.08, SE=0.02, p<.001), and interruptions (b=0.09, SE=0.02, p<.001) were related to more dissatisfied sleep. No significant quadratic relationships appeared between any of the job demands indicators and sleep dissatisfaction (ps≥.102).
Associations Between Job Demands and Sleep Health Stratified by Job Control
Table 4 includes results from unadjusted and adjusted models for overall demands and sleep health for participants with low and high job control. In fully adjusted models, overall demands were linearly associated with sleep inefficiency (b=0.01, SE=0.003, p<.001) only for participants with low job control. Overall demands were related to greater sleep irregularity (low control: b=0.03, SE=0.01, p<.001; high control: b=0.02, SE=0.01, p=.048) and greater sleep dissatisfaction (low and high control: b=0.04, SE=0.01, p<.001) in both participants with low and high job control. No significant quadratic effects of overall demands appeared for sleep health stratified by job control (ps≥.079).
Table 4.
Linear and Quadratic Associations Between Overall Demands and Sleep Characteristics
| Variable | Unadjusted Effects | Covariate Adjusted Effects | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low Control | High Control | Low Control | High Control | |||||||||
| b | SE | p | b | SE | p | b | SE | p | b | SE | p | |
| Sleep Duration a | ||||||||||||
| Overall Demands | −0.02 | 0.01 | .047 | −0.01 | 0.01 | .162 | 0.02 | 0.01 | .062 | −0.02 | 0.01 | .072 |
| Overall Demands2 | 0.003 | 0.002 | .103 | 0.0004 | 0.002 | .847 | 0.003 | 0.002 | .198 | 0.002 | 0.002 | .441 |
| Sleep Irregularity b | ||||||||||||
| Overall Demands | 0.03 | 0.01 | <.001 | 0.03 | 0.01 | .007 | 0.03 | 0.01 | <.001 | 0.02 | 0.01 | .048 |
| Overall Demands2 | 0.004 | 0.002 | .064 | 0.005 | 0.002 | .029 | 0.004 | 0.002 | .079 | 0.003 | 0.002 | .127 |
| Sleep Inefficiency c | ||||||||||||
| Overall Demands | 0.01 | 0.003 | .015 | 0.0005 | 0.003 | .884 | 0.01 | 0.003 | .010 | 0.0002 | 0.003 | .963 |
| Overall Demands2 | 0.001 | 0.001 | .077 | 0.001 | 0.001 | .114 | 0.001 | 0.001 | .431 | 0.001 | 0.001 | .269 |
| Nap Frequency d | ||||||||||||
| Overall Demands | −0.02 | 0.02 | .378 | −0.05 | 0.02 | .009 | 0.01 | 0.02 | .790 | −0.01 | 0.02 | .492 |
| Overall Demands2 | 0.005 | 0.004 | .245 | 0.001 | 0.004 | .821 | 0.01 | 0.004 | .112 | 0.001 | 0.004 | .789 |
| Sleep Dissatisfaction e | ||||||||||||
| Overall Demands | 0.04 | 0.01 | <.001 | 0.04 | 0.01 | <.001 | 0.04 | 0.01 | <.001 | 0.04 | 0.01 | <.001 |
| Overall Demands2 | 0.0003 | 0.001 | .842 | 0.0005 | 0.002 | .774 | 0.005 | 0.002 | .767 | 0.0004 | 0.002 | .930 |
Unadjusted low control (n = 1458), unadjusted high control (n = 1457), adjusted low control (n = 1363), adjusted high control (n = 1371)
Unadjusted low control (n = 1433), unadjusted high control (n = 1433), adjusted low control (n = 1342), adjusted high control (n = 1349)
Unadjusted low control (n = 1440), unadjusted high control (n = 1449), adjusted low control (n = 1345), adjusted high control (n = 1364)
Unadjusted low control (n = 1453), unadjusted high control (n = 1447), adjusted low control (n = 1358), adjusted high control (n = 1362)
Unadjusted low control (n = 1460), unadjusted high control (n = 1457), adjusted low control (n = 1365), adjusted high control (n = 1372)
Note. Bolded values indicate significant effects. Adjusted models controlled for study sample, age, sex, race/ethnicity, marital status, education, job tenure, work hours, body mass index, and whether the participant currently smoked. Low control and high control were stratified based on a median split (≥median = high, < median = low). Continuous covariates and main predictors were centered at the sample mean. Abbreviations: b = unstandardized regression estimate. SE = standard error
Supplemental Tables 3–7 include results for linear and quadratic relationships between each of the specific job demands indicators and each sleep health outcome stratified by job control. For the sake of parsimony, results consistently found between unadjusted and adjusted models are described here. There were nuanced differences by models, yet overall, the negative linear relationship between job demands and sleep was more apparent for individuals with low job control. The quadratic relationship was consistently found for specific job demands indicators, such that moderate job demands were associated with better sleep health (i.e., longest sleep duration, more regular sleep, and more efficient sleep; Figure 2) mostly for individuals with low job control. A notable exception was observed in sleep dissatisfaction. Each of the five job demands indicators were linearly related to sleep dissatisfaction, such that higher demands were related to more dissatisfied sleep similarly for participants with low and high job control.
Figure 2.
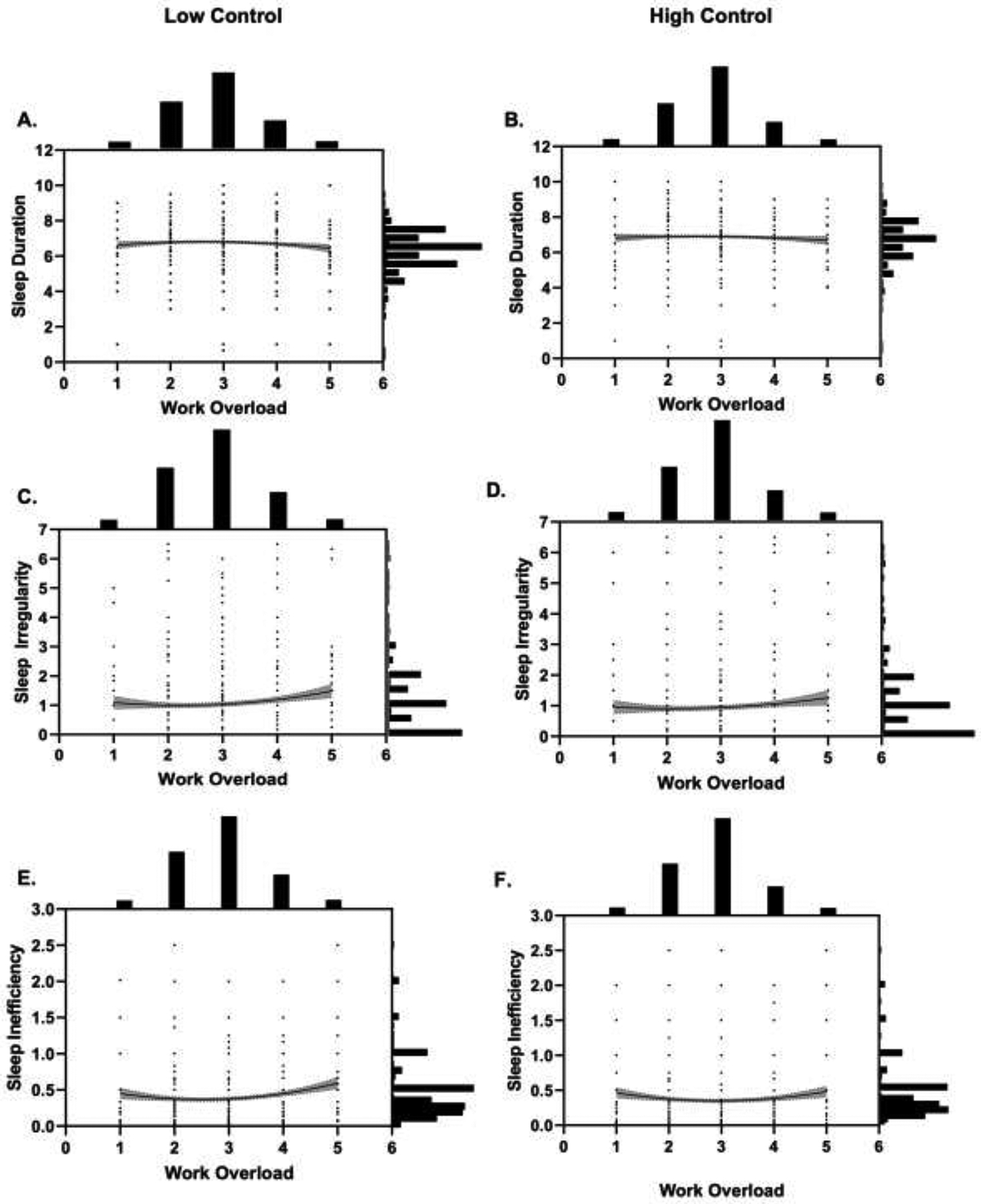
Curvilinear Relationships Between Work Overload and Sleep Health Dimensions Stratified by Job Control. Work overload (M=2.89) was mean centered for analyses. Work overload represents the frequency (1=never, 2=little of the time, 3=some of the time, 4=most of the time, 5=all of the time) with which participants had too many demands made on them. Lower values on sleep duration represent poorer sleep (Panels A and B) whereas higher values on sleep irregularity and sleep inefficiency represent poorer sleep (Panels C-F). Analyses were stratified by job control (left: low control; right: high control). All figures include bar graphs with frequency (%) of responses for sleep health (right) and work overload (top). A scatterplot represents the responses participants provided. Shaded regions represent 95% confidence intervals. Significant quadratic relationships exist between work overload and sleep duration (A: low control), sleep irregularity (C: low control), and sleep inefficiency (E: low control; F: high control). Moderate demands were associated with longer sleep duration, and more regular and efficient sleep. Relationships between work overload, sleep duration, and sleep irregularity were non-significant for participants with high job control. There were no significant quadratic relationships between work overload and either nap frequency or sleep dissatisfaction. There were also no other significant quadratic effects of the remaining job demands indicators for any of the sleep health dimensions in stratified analyses.
Dose-Response Relationships Between Job Demands and Sleep Health
Dose-response relationships were assessed for all significant quadratic effects. For the association between overall demands and sleep irregularity, the most regular sleep was estimated for job demands around 14 out of 25. This can be translated as “moderate”, or having job demands “little” (=2) to “some” (=3) of the time across the five items. For the association between work overload and irregularity, the most regular sleep was estimated for job demands 2 out of 5. For the association between work overload and sleep inefficiency, the most efficient sleep was estimated for job demands corresponding to 3 out of 5.
For the stratified analyses (Figure 2), the most optimal sleep health for participants with low job control was estimated at 2 out of 5 on work overload for both sleep duration (longest duration) and sleep irregularity (most regular sleep). Efficient sleep was estimated for work overload corresponding to 3 out of 5 for both participants with low and high job control.
Discussion
We found initial empirical evidence that not all work-related stressors may be harmful for sleep health, providing support for the use of the hormetic stress concept11 in sleep research. We assessed linear and curvilinear relationships between job demands and sleep health. Consistent with prior research, we found a general pattern that higher job demands were related to poorer sleep health. However, for some sleep health dimensions, as hypothesized, we found a nonlinear pattern of relationships. Specifically, curvilinear relationships did exist between job demands and certain sleep health dimensions (i.e., irregularity, inefficiency), with moderate demands related to more regular and efficient sleep. Results stratified by job control further revealed that these linear and quadratic relationships appeared stronger for participants with low job control, indicating a potential exacerbating effect of low job control. Evidence suggests that both too low—potentially reflecting disengagement at work—and too high job demands may be maladaptive7 to sleep health (consistent with the hormetic stress concept11), indicating that a moderate amount of stressor exposure is associated with optimal sleep.
Overall, findings support the job demands-control model14, which suggests job demands are related to different workplace and health outcomes that may be attenuated by level of job control. Instead of only examining whether the combination of high job demands with low job control was associated with worse sleep outcomes, we assessed whether certain levels of job demands were associated with sleep outcomes, based on the hormetic stress concept11. The application of this dose-response approach between job demands and sleep outcomes results in a more nuanced understanding of relationships between work-related stressors and health, suggesting that an ideal level of psychosocial stressors may be best for sleep health (c.f., eustress40). Specifically, we found that exposure to moderate levels of job demands can be beneficial for sleep health.
Moderate job demands were associated with more optimal sleep regularity and efficiency. While high job demands are expected to be associated with adverse health outcomes, it is less so for low job demands. In terms of sleep regularity, it may be that workers with low job demands have work schedules that are disruptive to regular sleep schedules. In contrast, workers with too many job demands may have more irregular sleep schedules driven by extensive work hours during the week. On the weekends, these workers with high job demands may need to extend their weekend awakenings due to the need for recovery from the workweek41. For sleep efficiency, the time needed to fall asleep at night could be influenced by how much restoration is needed and whether rumination is occurring. For example, having too few job demands may reflect a low intellectual engagement at work and limit the need for the restorative role of sleep42 thereby lowering the propensity for sleep. On the other hand, higher job demands have been found to relate to worse sleep quality due to rumination43. Sleep efficiency may be affected if an individual is unable to disconnect from work and engages in rumination because of their job demands.
We also found that the relationship between job demands and sleep health depended on the sleep dimension of focus. The most consistent linear relationships with overall and specific job demands indicators were found for sleep irregularity and sleep dissatisfaction. Regardless of the type of job demands, higher demands were related to more irregular and dissatisfied sleep. For the other sleep health dimensions (sleep duration, nap frequency, sleep inefficiency), effects of job demands were limited to certain types of demands, but similar linear relationships appeared. The one exception was the association between job intensity and nap frequency, which exhibited a negative linear relationship. It may be that workers with more intense work are too engaged in their work or too busy to take naps resulting in greater alertness during the day.
For stratified analyses, we found evidence suggesting that job control was a buffer for job demands, with results appearing mainly for participants with low job control. Thus, the negative effects of job demands on sleep health outcomes seem to be attenuated by higher job resources. One exception was sleep dissatisfaction—individuals with higher demands report more dissatisfied sleep regardless of their level of job control. Some evidence suggests that job demands, but not factors related to job resources, were related to future sleep problems21. Others have also found that higher job demands were directly associated with poorer sleep quality, whereas higher job control was indirectly associated with better sleep quality through increased job satisfaction and reduced chronic fatigue20. It could be that job demands have a strong negative linear relationship with sleep quality or satisfaction regardless of job control, possibly due to the cumulative effects of this stressor exceeding individuals’ stress resilience capacity11.
Taken together, an increase in job demands–even to a moderate level–may not allow satisfying/restorative sleep in workers. However, for other sleep dimensions, quadratic effects were found more prevalently for individuals with low job control, with sleep inefficiency as the only sleep health dimension exhibiting a significant quadratic effect for participants with high job control. Overall, results revealed that sleep health in workers was optimal when the levels of job demands were moderate, and this was particularly so for those with low job control. This novel finding extends previous literature on work stress and sleep.
Strengths, Limitations, and Future Directions
Our study has several strengths. We used a national sample of adults, which offered the opportunity to test our new hypotheses in a large and general sample of full-time workers. The assessment of overall demands and specific aspects of job demands (i.e., intensity, role conflict, work overload, time pressure, and interruptions) and comparison of results across the six job demands indicators in relation to sleep outcomes are also strengths. We included five dimensions of sleep health, based on a well-validated conceptual model (Ru-SATED24), which extends past work examining single sleep measures (e.g., sleep duration or sleep quality only).
There are also some limitations. First, although we focused on job demands and job control given their potentially salient effects on employee health15,16, there may be other work characteristics not captured by the job demands-control model that we did not include but may be important for sleep health, such as perceived inequality at work6, shift work5,17, work precarity44,45, salary/income (e.g., experiences of poverty46), or commute time47. Moreover, as the context for work is increasingly shifting to remote work arrangements, there is the need to understand how the context of work (i.e., office environment vs. home environment) may relate to sleep health48. Additionally, there may be non-work-related factors that workers have to balance with their workloads such as demands from family/personal life49 or caregiving50 that may also influence sleep health. Although beyond the scope of the current study, future research would benefit from considering both (a) other work-related and (b) non-work-related characteristics when assessing sleep health outcomes to have a more nuanced understanding of the relationships among various factors that may relate to sleep.
Second, the cross-sectional design prevents examination of causal relationships between job demands and sleep. Inclusion of multiple time points would allow assessment of directionality of effects between job demands and sleep health. Third, we used self-reported measures of job demands and sleep health, which might have inflated the relationship due to the common self-report method51. Including objective measures of job demands and control (e.g., peer or supervisor ratings) and sleep (e.g., actigraphy) could expand our understanding of the relationships between these variables.
Fourth, some components of the Ru-SATED24 model (i.e., sleep timing and WASO for sleep inefficiency) were not available in the MIDUS core survey and were not included. Fifth, the MIDUS sample was mostly non-Hispanic White; therefore, we do not know whether our findings would replicate in racially and ethnically diverse samples. Future research could assess whether patterns are similar across races/ethnicities and different age groups. Future research could also consider other potential moderators. For example, job tenure (a proxy for exposure to specific working conditions) may moderate the associations between job demands, job control, and sleep, but we did control for this variable in analyses. Cumulative exposure to the stress of job demands could lead to either (a) loss spirals or (b) job crafting8 which could intensify or attenuate the effect of job demands on health outcomes, respectively. Further, cumulative exposure to chronic stressors is related to negative health outcomes11. Examining moderations by specific job conditions and demographic characteristics would be fruitful directions for future research.
Conclusions
To ensure the good health of workers, it is important to determine the most ideal levels of demands and control needed for the best working conditions and subsequent health outcomes that may be driven by sleep health. We found that moderate levels of job demands were related to optimal sleep health, especially for workers with low job control. Tailoring the work environment by assigning not too high and not too low job demands can assure that the workplace provides a fitting level of responsibilities that benefit employee sleep health. Alternatively, if extensive levels of job demands cannot be reduced to a moderate level, enhancing employees’ job control in these situations may be another way to promote sleep health in workers.
Supplementary Material
Acknowledgements
Disclosure Statement Outside of the current work, Orfeu M. Buxton discloses that he received subcontract grants to Penn State from Proactive Life (formerly Mobile Sleep Technologies), doing business as SleepSpace (National Science Foundation grant #1622766 and NIH/National Institute on Aging Small Business Innovation Research Program R43AG056250, R44 AG056250); received honoraria/travel support for lectures from Boston University, Boston College, Tufts School of Dental Medicine, University of Miami, Eric H. Angle Society of Orthodontists, Harvard Chan School of Public Health, New York University and Allstate; receives consulting fees from SleepNumber; and receives an honorarium for his role as the Editor in Chief of Sleep Health sleephealthjournal.org.
Funding Details
This work was supported by the National Institute on Aging under Grant: R56AG065251 to Soomi Lee (PI). The National Institute on Aging was not involved in the design or conduct of the study; data management, analyses, or interpretation; or preparation, review, or submission of the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kwok CS, Kontopantelis E, Kuligowski G, et al. Self-reported sleep duration and quality and cardiovascular disease and mortality: A dose-response meta-analysis. J Am Heart Assoc. 2018;7(15):1–26. doi: 10.1161/JAHA.118.008552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sabia S, Fayosse A, Dumurgier J, et al. Association of sleep duration in middle and old age with incidence of dementia. Nat Commun. 2021;12(1): 1–10. doi: 10.1038/s41467-021-22354-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grandner MA. Sleep, health, and society. Sleep Med Clin. 2020;15(2):319–340. doi: 10.1016/j.jsmc.2020.02.017 [DOI] [PubMed] [Google Scholar]
- 4.Bannai A, Tamakoshi A. The association between long working hours and health: A systematic review of epidemiological evidence. Scand J Work Environ Health. 2014;40(1):5–18. 10.5271/sjweh.3388 [DOI] [PubMed] [Google Scholar]
- 5.Jehan S, Zizi F, Pandi-Perumal SR, et al. Shift work and sleep: Medical implications and management. Sleep Med Disord Int J. 2017;1(2):36–42. doi: 10.15406/smdij.2017.01.00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee S, Mogle JA, Jackson CL, Buxton OM. What’s not fair about work keeps me up: Perceived unfairness about work impairs sleep through negative work-to-family spillover. Soc Sci Res. 2019;81:23–31. doi: 10.1016/j.ssresearch.2019.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lawton MP. Environment and other determinants of well-being in older people. Gerontologist. 1983;23(4):349–357. doi: 10.1093/geront/23.4.349 [DOI] [PubMed] [Google Scholar]
- 8.Bakker AB, Demerouti E. Job demands-resources theory: Taking stock and looking forward. J Occup Health Psychol. 2017;22(3):273–285. doi: 10.1037/ocp0000056 [DOI] [PubMed] [Google Scholar]
- 9.Reijseger G, Schaufeli WB, Peeters MCW, Taris TW, van Beek I, Ouweneel E. Watching the paint dry at work: psychometric examination of the Dutch Boredom Scale. Anxiety, Stress Coping. 2013;26(5):508–525. doi: 10.1080/10615806.2012.720676 [DOI] [PubMed] [Google Scholar]
- 10.French KA, Allen TD, Henderson TG. Challenge and hindrance stressors in relation to sleep. Soc Sci Med. 2019;222(November 2018):145–153. doi: 10.1016/j.socscimed.2019.01.009 [DOI] [PubMed] [Google Scholar]
- 11.Epel ES. The geroscience agenda: Toxic stress, hormetic stress, and the rate of aging. Ageing Res Rev. 2020;63:101167. doi: 10.1016/j.arr.2020.101167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yerkes RM, Dodson JD. The relation of strength of stimulus to rapidity of habit-formation. J Comp Neurol Psychol. 1908;18:459–482. doi: 10.1002/cne.920180503 [DOI] [Google Scholar]
- 13.Calabrese EJ. Converging concepts: Adaptive response, preconditioning, and the Yerkes-Dodson Law are manifestations of hormesis. Ageing Res Rev. 2008;7(1):8–20. doi: 10.1016/j.arr.2007.07.001 [DOI] [PubMed] [Google Scholar]
- 14.Karasek RA, Theorell T. Healthy Work: Stress, Productivity and the Reconstruction of Working Life. Basic Books; 1990. [Google Scholar]
- 15.Xanthopoulou D, Bakker AB, Dollard MF, et al. When do job demands particularly predict burnout? The moderating role of job resources. J Manag Psychol. 2007;22(8):766–786. doi: 10.1108/02683940710837714 [DOI] [Google Scholar]
- 16.Litwiller B, Snyder LA, Taylor WD, Steele LM. The relationship between sleep and work: A meta-analysis. J Appl Psychol. 2017;102(4):682–699. doi: 10.1037/apl0000169 [DOI] [PubMed] [Google Scholar]
- 17.Linton SJ, Kecklund G, Franklin KA, et al. The effect of the work environment on future sleep disturbances: A systematic review. Sleep Med Rev. 2015;23:10–19. doi: 10.1016/j.smrv.2014.10.010 [DOI] [PubMed] [Google Scholar]
- 18.Van Laethem M, Beckers DGJ, Kompier MAJ, Dijksterhuis A, Geurts SAE. Psychosocial work characteristics and sleep quality: A systematic review of longitudinal and intervention research. Scand J Work Environ Heal. 2013;39(6):535–549. doi: 10.5271/sjweh.3376 [DOI] [PubMed] [Google Scholar]
- 19.Garefelt J, Platts LG, Hyde M, Magnusson Hanson LL, Westerlund H, Åkerstedt T. Reciprocal relations between work stress and insomnia symptoms: A prospective study. J Sleep Res. 2020;29(2):1–11. doi: 10.1111/jsr.12949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li Y, Fang J, Zhou C. Work-related predictors of sleep quality in Chinese nurses: Testing a path analysis model. J Nurs Res. 2019;27(5):1–10. doi: 10.1097/jnr.0000000000000319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Muhamad Nasharudin NA, Idris MA, Young LM. The effect of job demands on health and work outcomes: A longitudinal study among Malaysian employees. PsyCh J. 2020;9(5):691–706. doi: 10.1002/pchj.378 [DOI] [PubMed] [Google Scholar]
- 22.Stiglbauer B, Kovacs C. The more, the better? Curvilinear effects of job autonomy on well-being from vitamin model and PE-fit theory perspectives. J Occup Health Psychol. 2018;23(4):520–536. doi: 10.1037/ocp0000107 [DOI] [PubMed] [Google Scholar]
- 23.Gadinger MC, Fischer JE, Schneider S, Fischer GC, Frank G, Kromm W. Female executives are particularly prone to the sleep-disturbing effect of isolated high-strain jobs: A cross-sectional study in German-speaking executives. J Sleep Res. 2009;18(2):229–237. doi: 10.1111/j.1365-2869.2008.00715.x [DOI] [PubMed] [Google Scholar]
- 24.Buysse DJ. Sleep health: Can we define it? Does it matter? Sleep. 2014;37(1):9–17. doi: 10.5665/sleep.3298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ryff CD, Krueger RF, ‘Approaching Human Health as an Integrative Challenge: Introduction and Overview’, in Ryff CD, Krueger RF (eds), The Oxford Handbook of Integrative Health Science (pp. 3-22). Oxford University Press, New York; 2018. doi: 10.1093/oxfordhb/9780190676384.001.0001 [DOI] [Google Scholar]
- 26.Dijk DJ, Beersma DGM, Daan S. EEG Power Density during Nap Sleep: Reflection of an Hourglass Measuring the Duration of Prior Wakefulness. J Biol Rhythms. 1987;2(3):207–219. doi: 10.1177/074873048700200304 [DOI] [PubMed] [Google Scholar]
- 27.Mantua J, Spencer RMC. Exploring the nap paradox: are mid-day sleep bouts a friend or foe? Sleep Med. 2017;37:88–97. doi: 10.1016/j.sleep.2017.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cousins JN, Leong RLF, Jamaluddin SA, Ng ASC, Ong JL, Chee MWL. Splitting sleep between the night and a daytime nap reduces homeostatic sleep pressure and enhances long-term memory. Sci Rep. 2021;11(1):1–15. doi: 10.1038/s41598-021-84625-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Milner CE, Cote KA. Benefits of napping in healthy adults: Impact of nap length, time of day, age, and experience with napping. J Sleep Res. 2009;18(2):272–281. doi: 10.1111/j.1365-2869.2008.00718.x [DOI] [PubMed] [Google Scholar]
- 30.Pan Z, Huang M, Huang J, Yao Z, Lin Z. Association of napping and all-cause mortality and incident cardiovascular diseases: a dose–response meta analysis of cohort studies. Sleep Med. 2020;74:165–172. doi: 10.1016/j.sleep.2020.08.009 [DOI] [PubMed] [Google Scholar]
- 31.Lee S, Smith CE, Wallace ML, et al. Cardiovascular risks and sociodemographic correlates of multidimensional sleep phenotypes in two samples of US adults. SLEEP Adv. 2022;3(1):1–11. doi: 10.1093/sleepadvances/zpac005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li P, Gao L, Yu L, et al. Daytime napping and Alzheimer’s dementia: A potential bidirectional relationship. Alzheimer’s Dement. 2022;(December 2021):1–11. doi: 10.1002/alz.12636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dalmases M, Benítez ID, Mas A, et al. Assessing sleep health in a European population: Results of the catalan health survey 2015. PLoS One. 2018;13(4):1–13. doi: 10.1371/journal.pone.0194495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee S, Mu CX, Wallace ML, et al. Sleep health composites are associated with the risk of heart disease across sex and race. Sci Rep. 2022;12(1):1–11. doi: 10.1038/s41598-022-05203-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karasek RA, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): An instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3(4):322–355. doi: 10.1037/1076-8998.3.4.322 [DOI] [PubMed] [Google Scholar]
- 36.Andel R, Crowe M, Kareholt I, Wastesson J, Parker MG. Indicators of job strain at midlife and cognitive functioning in advanced old age. Journals Gerontol - Ser B Psychol Sci Soc Sci. 2011;66(3):287–291. doi: 10.1093/geronb/gbq105 [DOI] [PubMed] [Google Scholar]
- 37.Hawkins MAW, Gathright EC, Gunstad J, et al. The MoCA and MMSE as screeners for cognitive impairment in a heart failure population: A study with comprehensive neuropsychological testing. Hear Lung J Acute Crit Care. 2014;43(5):462–468. doi: 10.1016/j.hrtlng.2014.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hickman RJ, Khambaty T, Stewart JC. C-reactive protein is elevated in atypical but not nonatypical depression: Data from the National Health and Nutrition Examination Survey (NHANES) 1999–2004. J Behav Med. 2014;37(4):621–629. doi: 10.1007/s10865-013-9510-0 [DOI] [PubMed] [Google Scholar]
- 39.Kline RB. Principles and Practice of Structural Equation Modeling. 2nd ed. Guilford Press; 2005. [Google Scholar]
- 40.Parker KN, Ragsdale JM. Effects of distress and eustress on changes in fatigue from waking to working. Appl Psychol Heal Well-Being. 2015;7(3):293–315. doi: 10.1111/aphw.12049 [DOI] [PubMed] [Google Scholar]
- 41.Myllyntausta S, Kronholm E, Pulakka A, et al. Association of job strain with accelerometer-based sleep duration and timing of sleep among older employees. J Sleep Res. 2022;31(2):1–10. doi: 10.1111/jsr.13498 [DOI] [PubMed] [Google Scholar]
- 42.Åkerstedt T, Nilsson PM, Kecklund G. Sleep and recovery. Res Occup Stress Well Being. 2009;7(2009):205–247. doi: 10.1108/S1479-3555(2009)0000007009 [DOI] [Google Scholar]
- 43.Van Laethem M, Beckers DGJ, Geurts SAE, Garefelt J, Magnusson Hanson LL, Leineweber C. Perseverative Cognition as an Explanatory Mechanism in the Relation Between Job Demands and Sleep Quality. Int J Behav Med. 2018;25(2):231–242. doi: 10.1007/s12529-017-9683-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mai QD, Jacobs AW, Schieman S. Precarious sleep ? Nonstandard work, gender, and sleep disturbance in 31 European countries. Soc Sci Med. 2019;237(July):112424. doi: 10.1016/j.socscimed.2019.112424 [DOI] [PubMed] [Google Scholar]
- 45.Salas-Nicás S, Sembajwe G, Navarro A, Moncada S, Llorens C, Buxton OM. Job insecurity, economic hardship, and sleep problems in a national sample of salaried workers in Spain. Sleep Heal. 2020;6(3):262–269. doi: 10.1016/j.sleh.2020.02.014 [DOI] [PubMed] [Google Scholar]
- 46.Patel NP, Grandner MA, Xie D, Branas CC, Gooneratne N. “Sleep disparity” in the population : poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health. 2010;10:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim S, Kim Y, Lim SS, Ryoo JH, Yoon JH. Long Commute Time and Sleep Problems with Gender Difference in Work–Life Balance: A Cross-sectional Study of More than 25,000 Workers. Saf Health Work. 2019;10(4):470–475. doi: 10.1016/j.shaw.2019.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Allen TD, Golden TD, Shockley KM. How effective is telecommuting? Assessing the status of our scientific findings. Psychol Sci Public Interes. 2015;16(2):40–68. doi: 10.1177/1529100615593273 [DOI] [PubMed] [Google Scholar]
- 49.Buxton OM, Lee S, Beverly C, et al. Work-family conflict and employee sleep: Evidence from IT workers in the Work, Family and Health Study. Sleep. 2016;39(10):1871–1882. doi: 10.5665/sleep.6172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gao C, Chapagain NY, Scullin MK. Sleep Duration and Sleep Quality in Caregivers of Patients With Dementia A Systematic Review and Meta-analysis. JAMA Netw Open. 2019;2(8):1–15. doi: 10.1001/jamanetworkopen.2019.9891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: A critical review of the literature and recommended remedies. J Appl Psychol. 2003;88(5):879–903. doi: 10.1037/0021-9010.88.5.879 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


