Abstract
A 65-year-old woman with known right dural based lesion and metastatic pancreatic neuroendocrine tumor presented with multiple days of progressive lethargy and left sided weakness culminating with obtundation and dilated pupils. CT scan demonstrated acute right convexity subdural hematoma and frontotemporal intraparenchymal hemorrhage with 1.3 cm of midline shift, uncal herniation and increase in size of now hemorrhagic dural based lesion. She underwent emergency hemicraniectomy for evacuation of subdural hematoma and resection of hemorrhagic meningioma with excellent post-operative result including improvement in midline shift and gross total resection of lesion. Pathology was consistent with World Health Organization Grade II meningioma with chordoid component. She underwent adjuvant stereotactic radiosurgery and cranioplasty and made a full neurological recovery. Identification of hemorrhagic meningioma as the underlying pathology causing multicompartmental hemorrhage is crucial. We recommend single stage decompression with extraaxial clot evacuation and resection of the meningioma when feasible.
Case Illustration:
A 65-year-old woman with metastatic pancreatic neuroendocrine tumor status post pancreatectomy and splenectomy 11 years prior to presentation and hepatic artery embolization 2 months prior to presentation presented to the emergency room with three days of progressive lethargy and acute signs of herniation. In 2014, MR brain performed for cancer staging discovered dural-based right sphenoid wing tumor consistent with meningioma (Figure 1A). Given the lesion was stable and non-avid on follow-up FDG-PET imaging 7 years after initial imaging, no follow-up intervention was recommended by her oncologist. On arrival, she was Glasgow Coma Scale 13 with eyes opening to voice, and moderate left side weakness but decompensated quickly to a stuporous state with minimal eye opening and right sided dilated pupil with a Glascow Coma Scale score of 8. Her platelets and coagulation factors were in appropriate range, and she had no history of thrombophilia or coagulopathy. Her husband denied recent head trauma. CT scan showed acute right convexity subdural hematoma and acute frontotemporal intraparenchymal hemorrhage consistent with venous hemorrhage with 1.3 cm of midline shift (Figure 1B), right uncal herniation (Figure 1C), and effacement of the right lateral ventricle. A previously-identified dural based presumed meningioma was enlarged to 3.3 × 2.7 cm from 2.7 × 1.6 cm on a MRI scan from 7 years earlier. She was taken to the operating room for hemicraniectomy, evacuation of convexity subdural hematoma, and parenchymal clot exploration and potential evacuation. Upon removal of the bone, the brain was severely edematous and without spontaneous pulsations. The dural based tumor was removed from the Sylvian fissure, with significant intratumoral hemorrhage noted. While there was moderate improvement in brain relaxation and pulsatility with removal of the tumor and clot evacuation, the brain was still very swollen. The cranial bone flap was therefore not replaced to prevent injury from further swelling, especially in the setting of suspected venous infarction. Follow-up CT on post-operative day 0 (Figure 1D) and MR diffusion weighted imaging (DWI) (Figure 1E) and T1 post-contrast MR on post-operative day 1 (Figure 1F) showed gross total resection of the meningioma with improvement in subdural and intraparenchymal hemorrhage and expected diffusion restriction in the right temporal lobe. MRA and MRV were negative for vascular malformation or large-vessel venous thrombosis. Pathology was consistent with WHO Grade II meningioma with chordoid component and focally elevated Ki67 approaching or exceeding 10%. Her post-operative course was complicated by seizures, but she was discharged near at her neurological baseline with trace left-sided weakness which subsequently resolved. She received post-operative stereotactic radiosurgery and underwent cranioplasty 2 months postoperatively (Figure 1G). Meningioma presenting with multi-compartmental intracranial hemorrhage is an extremely rare event with high mortality that are often misdiagnosed with few cases reported in the literature.1–3 Proposed pathophysiological mechanisms include hemorrhagic conversion of venous infarction related to acute venous compression, and potentially also rupture of subdural bridging veins stretched by tumor growth.4,5 We recommend surgical decompression coupled with resection of hemorrhagic meningioma as the gold standard for treatment of multicompartmental hemorrhage associated with meningioma.
Figure Legend:
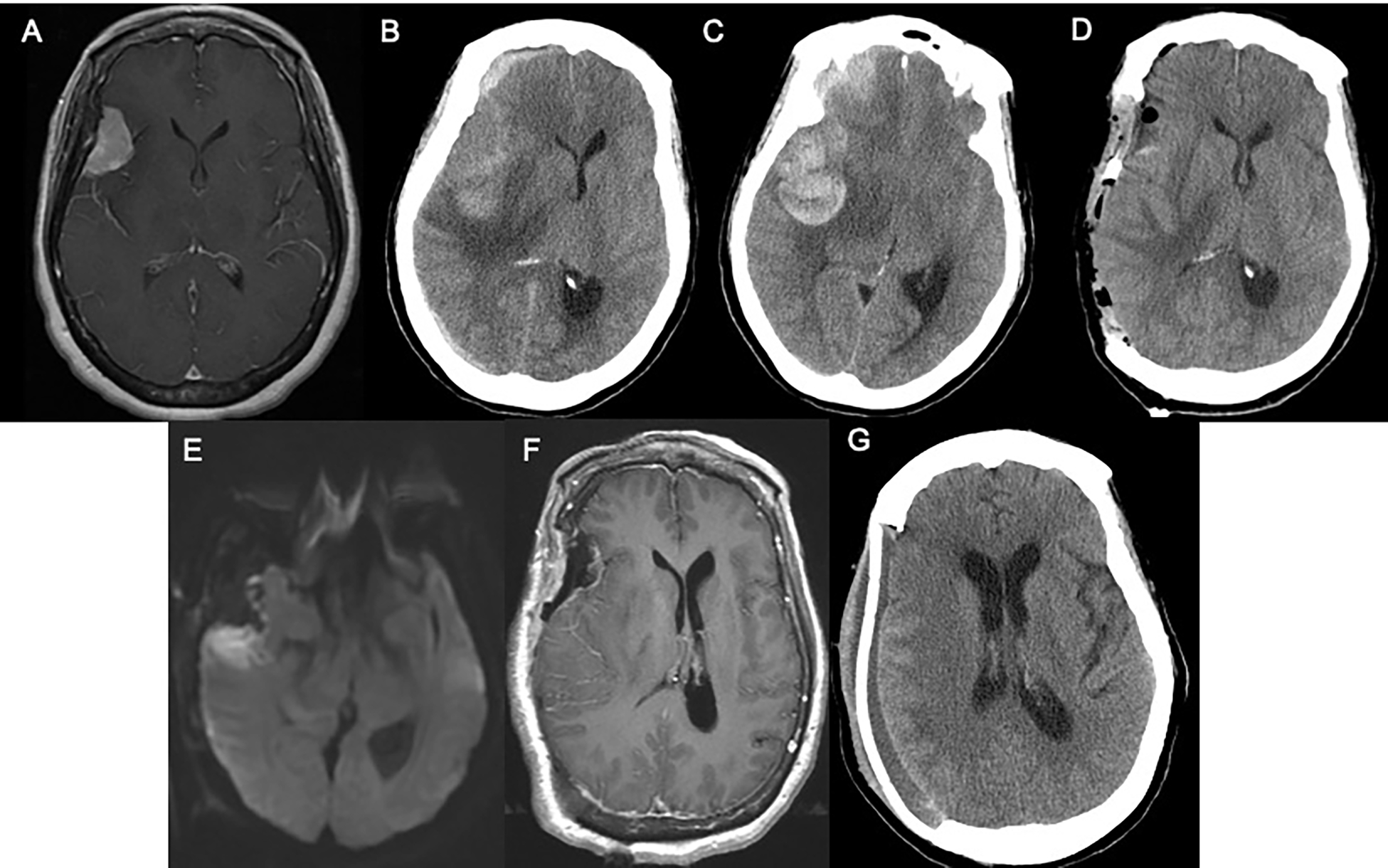
A 65-year-old woman with metastatic pancreatic neuroendocrine tumor and right sphenoid wing meningioma (A) presented with three days of progressive lethargy and acute obtundation with dilated ipsilateral pupil. Emergent CT scan (B,C) demonstrated an acute right convexity subdural hematoma and frontotemporal intraparenchymal hemorrhage with 1.3 cm of midline shift, effacement of the right lateral ventricle and right uncal herniation, and hemorrhagic expansion of the dural based lesion. She underwent emergent hemicraniectomy with resection of the meningioma with significant decompression of the subjacent brain structures as shown on postoperative CT obtained on day 0 (D) and post-contrast T1 DWI (E) MR sequences obtained on day 1 (F). Pathology was consistent with World Health Organization Grade II meningioma with chordoid component and she underwent cranioplasty (G). By 2 months postoperatively she experienced full neurological recovery.
Glossary
- DWI
Diffusion Weighted Imaging
- GCS
Glasgow Coma Scale
Footnotes
Conflict of Interest:
Alexandra M. Giantini Larsen, MD has no financial or personal relationships with other people or organizations that could inappropriately bias this work.
The other co-authors listed have confirmed there are no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Abolfotoh M, Brzezicki G, Fiester P, Tavanaiepour D. A Rare Case of Life-Threatening Multicompartmental Spontaneous Intracranial Hemorrhage From a Grade 1 Convexity Meningioma. Cureus. 2021;13(11):e19178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang RB, Chen LJ, Su SY, et al. Misdiagnosis and Delay of Diagnosis in Hemorrhagic Meningioma: A Case Series and Review of the Literature. World Neurosurg. 2021;155:e836–e846. [DOI] [PubMed] [Google Scholar]
- 3.Bosnjak R, Derham C, Popović M, Ravnik J. Spontaneous intracranial meningioma bleeding: clinicopathological features and outcome. J Neurosurg. 2005;103(3):473–484. [DOI] [PubMed] [Google Scholar]
- 4.Sumi K, Otani N, Mori F, Yamamuro S, Oshima H, Yoshino A. Venous hypertension caused by a meningioma involving the sigmoid sinus: case report. BMC Neurology. 2021;21(1):119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martínez-Lage JF, Poza M, Martínez M, Esteban JA, Antúnez MC, Sola J. Meningiomas with haemorrhagic onset. Acta Neurochir (Wien). 1991;110(3–4):129–132. [DOI] [PubMed] [Google Scholar]


