Abstract
Objectives:
To investigate the difference in renal function outcomes for patients with oncocytomas undergoing active surveillance (AS) vs. partial nephrectomy (PN).
Methods:
We reviewed our institutional database for patients with biopsy/surgically confirmed oncocytoma from 2000–2020. The primary outcome was to assess for differences in renal function outcomes in patients undergoing AS vs. PN. We fit two generalized estimating equation (GEE) with an interaction term between follow up time and management strategy to predict 1) mean eGFR for patients managed with AS and PN and 2) the probability of progression to CKD stage III or greater.
Results:
We identified 114 eligible patients, of which 32 were managed with AS. Median follow up was 21 months vs. 44 months for PN vs. AS patients. AS patients tended to be older (median: 72 years vs. 65 years, p<0.001) and have lower baseline renal function (median: eGFR: 71 mL/min/1.73m2 vs. 82 mL/min/1.73m2, p<0.001) compared with PN patients. Renal mass size from baseline imaging was similar between patients undergoing PN vs. AS (2.8 cm vs. 2.9 cm, p=0.634). For patients undergoing PN vs. AS, there was not a significant difference in predicted longitudinal eGFR (−0.079, 95% CI −0.18–0.023, p=0.129) or predicted probability of progression to CKD stage III or greater (OR: 0.61, 95% CI: 0.16–2.33, p=0.47).
Conclusions:
In our institutional dataset, patients undergoing AS or PN with an oncocytoma had similar long-term renal function outcomes. Given similar renal function outcomes in patients undergoing AS and PN, surgery should remain reserved for select patients with oncocytomas.
Keywords: active surveillance, partial nephrectomy, oncocytoma, renal function
1.1. Introduction
Optimal treatment of renal masses concerning for malignancies hinges on multiple factors including balancing oncologic control with the preservation of renal function.1 Given the indolent nature of many small renal masses, active surveillance (AS) has emerged as an accepted management strategy for many patients.2, 3 AS aims to maximize preservation of renal function and avoid the morbidity of surgery while still maintaining the ability to treat, cure, and prevent the spread of renal malignancy when, and if, necessary.
A substantial portion of patients diagnosed with small renal masses will have benign lesions4, the majority of which will be oncocytoma.5 When considering management options for a patient with a high suspicion of or a known benign renal mass, the balance between the priorities of optimizing oncological control or maintaining renal function are simplified and tilted towards the preservation of renal function, with less consideration given to oncological control. A recent publication investigating the association of partial nephrectomy (PN) and AS with renal function in patients with oncocytomas suggested patients’ longitudinal renal function may benefit from management with resection over surveillance, presumably by negating potential future effects of a growing renal mass on renal parenchymal loss.6 This finding is incongruent with existing literature which suggests AS and PN have similar renal function outcomes when considering malignant and benign lesions.7, 8
As such, we evaluated our institutional experience with patients harboring oncocytoma managed with AS or PN for potential differences in longitudinal renal function between these management strategies. We hypothesized patients with oncocytomas managed with AS and PN would have similar renal function outcomes.
1.2. Materials and Methods
This is a retrospective review of patients with an oncocytoma managed with active surveillance or partial nephrectomy at the Fox Chase Cancer Center, Philadelphia, PA. We searched our prospectively maintained renal mass database of patients with biopsy or surgically confirmed oncocytomas diagnosed from 2000–2020. The primary objective of the study was to test for the association of management strategy (AS vs. PN) with the longitudinal change in renal function. Active surveillance was defined by both: 1) AS listed as the primary management strategy in the database and 2) no surgery within 12 months of diagnosis. The PN group all underwent open, laparoscopic, or robot assisted PN within 12 months of their initial consultation date. Patients that initially started on AS but underwent delayed PN (>12 months after initial consultation) were classified as AS.
All patients included in the study had a solitary renal mass that was a biopsy proven or surgically resected oncocytoma. Patients with hybrid oncocytic/chromophobe tumors were excluded. Furthermore, patients with bilateral renal masses or multiple renal surgeries (such as multiple partial nephrectomies) were excluded due to the potential influence of these factors on renal function. Serum creatinine was recorded at baseline and then approximately every 6 months from initial consultation for patients managed with AS and from the date for surgery for patients that underwent PN. Patients with missing baseline serum creatinine or without at least one follow up serum creatinine value were excluded. Renal function was displayed as estimated glomerular filtration rate (eGFR) using the CKD-EPI 2009 equation.
Clinical, demographic, and tumor characteristics were compared for patients managed with AS and PN. Categorical variables were compared with the chi-squared or Fisher’s exact test as appropriate and continuous variables were compared with the Wilcoxon rank sum test. For the primary outcome, change in renal function was modeled in three methods. First, the change in eGFR from baseline was plotted over time for each patient by management strategy (AS vs. PN). Second, we fit a longitudinal linear regression model utilizing generalized estimating equation (GEE) methods to account for within patient correlations to estimate the change in renal function (eGFR) over time for patients managed with AS and PN. Variables in the model included time (months) from initial consultation, management strategy (AS vs. PN) and an interaction term between time and management strategy. We performed a subgroup analysis of patients who remained on AS at their last follow up by excluding those who underwent a delayed intervention. Third, we fit a logistic regression model to estimate the probability of progressing to CKD stage III or greater, defined as an eGFR <60 mL/min/1.73m2, using GEE methods and including only patients with a baseline eGFR >60. Variables included were management strategy (AS vs. PN), baseline eGFR, and follow up time (months). Statistical analysis was performed with SAS version 9.4 (SAS Institute, Cary, NC), with a p-value of <0.05 considered statistically significant. This study was approved by the Fox Chase Cancer Center Institutional Review Board (21–9007).
1.3. Results
We identified 114 patients with a solitary renal mass consistent with biopsy or surgically confirmed oncocytoma diagnosed from 2000 to 2020. Thirty two patients were managed with AS, of which 9 underwent a delayed intervention at a median of 25.6 months (IQR: 18.5–31.5 months) after starting AS. Compared with patients undergoing PN, patients managed with AS tended to be older (median: 72 years vs. 65 years, p<0.001) and have slightly worse baseline renal function (median: eGFR: 71 mL/min/1.73m2 vs. 82 mL/min/1.73m2, p<0.001, Table 1). Maximal tumor diameter on baseline imaging was similar between patients managed with AS compared with PN (median: 2.9cm vs. 2.8cm, p=0.638).
Table 1.
Clinical, demographic, and laboratory parameters of patients with oncocytomas managed with active surveillance vs. PN.
| PN (n=82) | Active Surveillance (n=32) | p | |||
|---|---|---|---|---|---|
| N/Median | %/IQR | N/Median | %/IQR | ||
| Age (years) | 65 | 59–71 | 72 | 64–76 | <0.001 |
| Max Tumor Diameter (cm) | 2.8 | 2.5–3.3 | 2.9 | 2.6–3.4 | 0.634 |
| Baseline Cr | 0.9 | 0.8–1.0 | 1 | 0.9–1.3 | 0.0154 |
| Baseline eGFR | 82 | 73–94 | 71 | 43–84 | <0.001 |
| BMI | 28 | 25–33 | 29 | 26–34 | 0.621 |
| Gender | 0.51 | ||||
| Female | 23 | 28% | 11 | 34% | |
| Male | 59 | 72% | 21 | 66% | |
| Race | 1.00 | ||||
| White | 77 | 94% | 31 | 97% | |
| Non-white | 5 | 6.1% | 1 | 3.10% | |
| Hypertension | 0.13 | ||||
| No | 30 | 37% | 7 | 22% | |
| Yes | 52 | 63% | 25 | 78% | |
Median time from baseline eGFR to last available eGFR was 21.0 months (IQR: 7.5–45.7) for patients undergoing PN and 43.9 months (IQR:24.9–59.7) for patients managed on AS. Change in eGFR overtime with a LOWESS line for patients managed with AS vs PN is shown in Figure 1. To assess for differences in longitudinal renal function for patients with oncocytoma managed with AS vs. PN, we fit a linear regression model with an interaction term between follow up time and management strategy. Figure 2A displays the predicted mean eGFR for patients managed with AS and PN from the longitudinal model. As seen in the model (Table 2) and the graph (Figure 2A), patients managed with PN had a higher predicted mean eGFR, consistent with their higher baseline value. For each month of follow up time, eGFR declined by an estimated 0.09 mL/min/1.73m2. Importantly, the interaction term between follow up time and management strategy was not statistically significant (−0.079, 95% CI −0.18–0.023, p=0.129); this suggests the slope of the predicted mean decline in renal function was not significantly different between patients undergoing AS vs. PN (Table 2A, Figure 2A).
Figure 1.
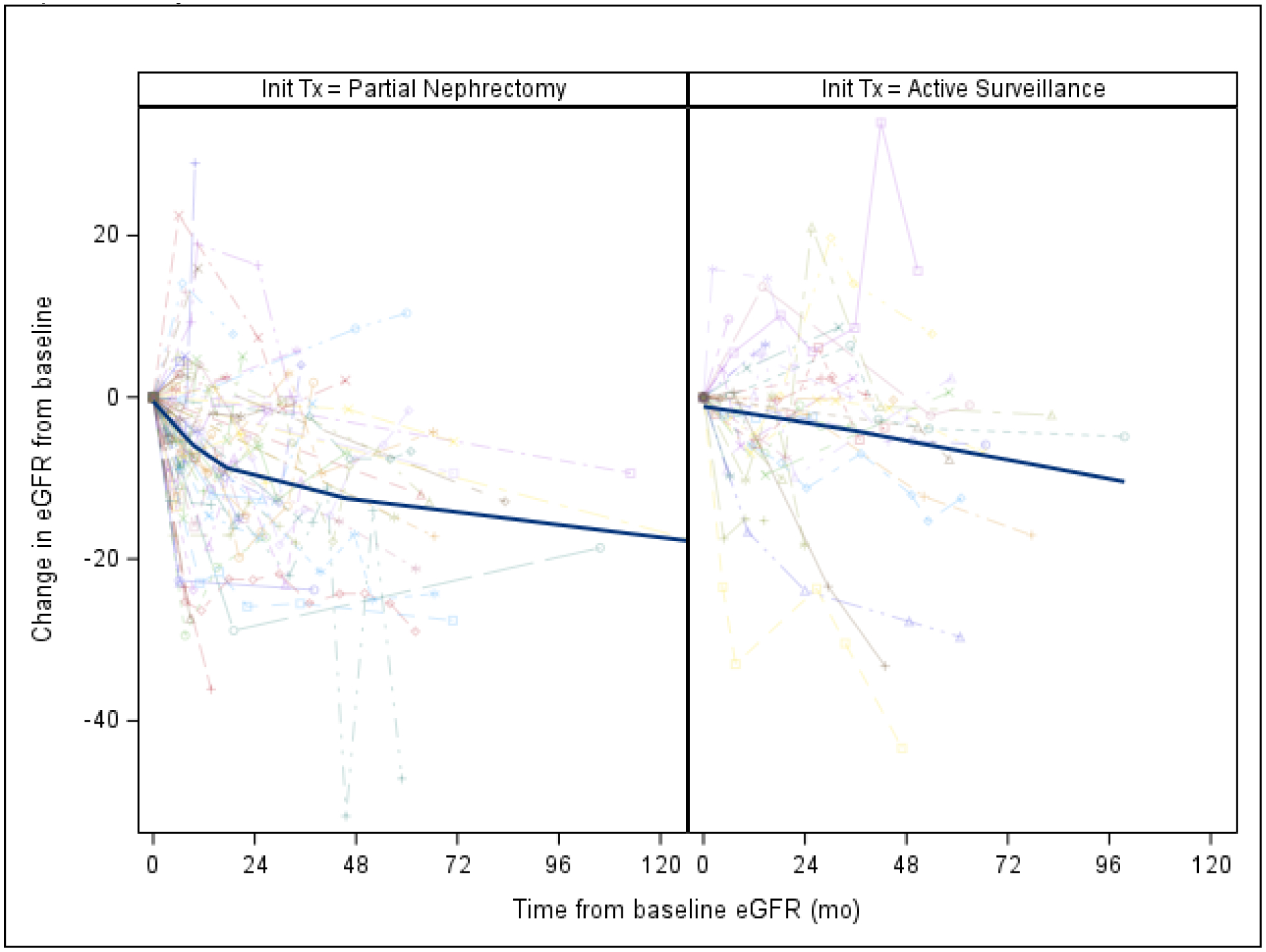
Plots of change in eGFR from baseline for patients managed with partial nephrectomy vs. active surveillance. Solid blue line is the LOWESS line.
Figure 2A.
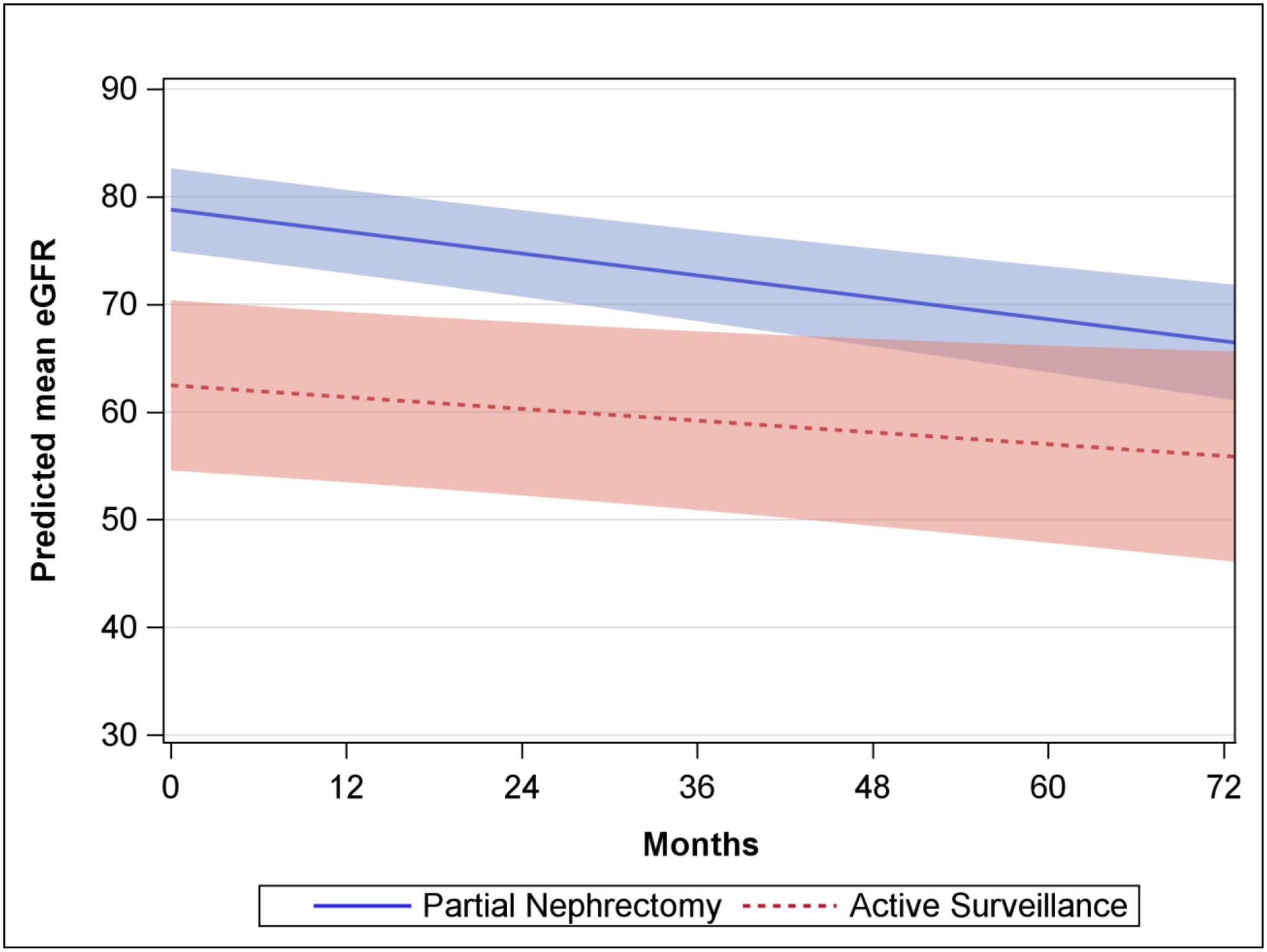
Predicted mean eGFR from the generalized estimating equation for patients managed with oncocytoma managed with partial nephrectomy vs. active surveillance. Shaded area represents the 95% confidence interval.
Table 2A.
Linear regression model with GEE for factors associated with eGFR
| Coefficient | 95% CI | p | |
|---|---|---|---|
| Time from Diagnosis (months) | −0.091 | −0.18–0.005 | 0.038 |
| Management Type | |||
| Active Surveillance | ref | ref | ref |
| PN | 16.3 | 7.51–25.1 | <0.001 |
| Interaction Term Time Since Diagnosis x PN |
−0.079 | −0.18–0.023 | 0.129 |
Due to the potential influence of delayed intervention, we excluded 9 AS patients which underwent a delayed partial nephrectomy. Consistent with the primary analysis, the interaction term between follow up time and management strategy was not statistically significant in the subgroup of patients which remained in AS at last follow up (Table 2B, Figure 2B).
Table 2B.
Linear regression model with GEE for factors associated with eGFR excluding 11 AS patients that underwent delayed intervention.
| Coefficient | 95% CI | p | |
|---|---|---|---|
| Time from Diagnosis (months) | −0.117 | −0.249–0.0144 | 0.081 |
| Management Type | |||
| Active Surveillance | ref | ref | ref |
| PN | 23.0 | 13.6–32.4 | <0.001 |
| Interaction Term Time Since Diagnosis x PN |
−0.05 | −0.194–0.0897 | 0.47 |
Figure 2B.
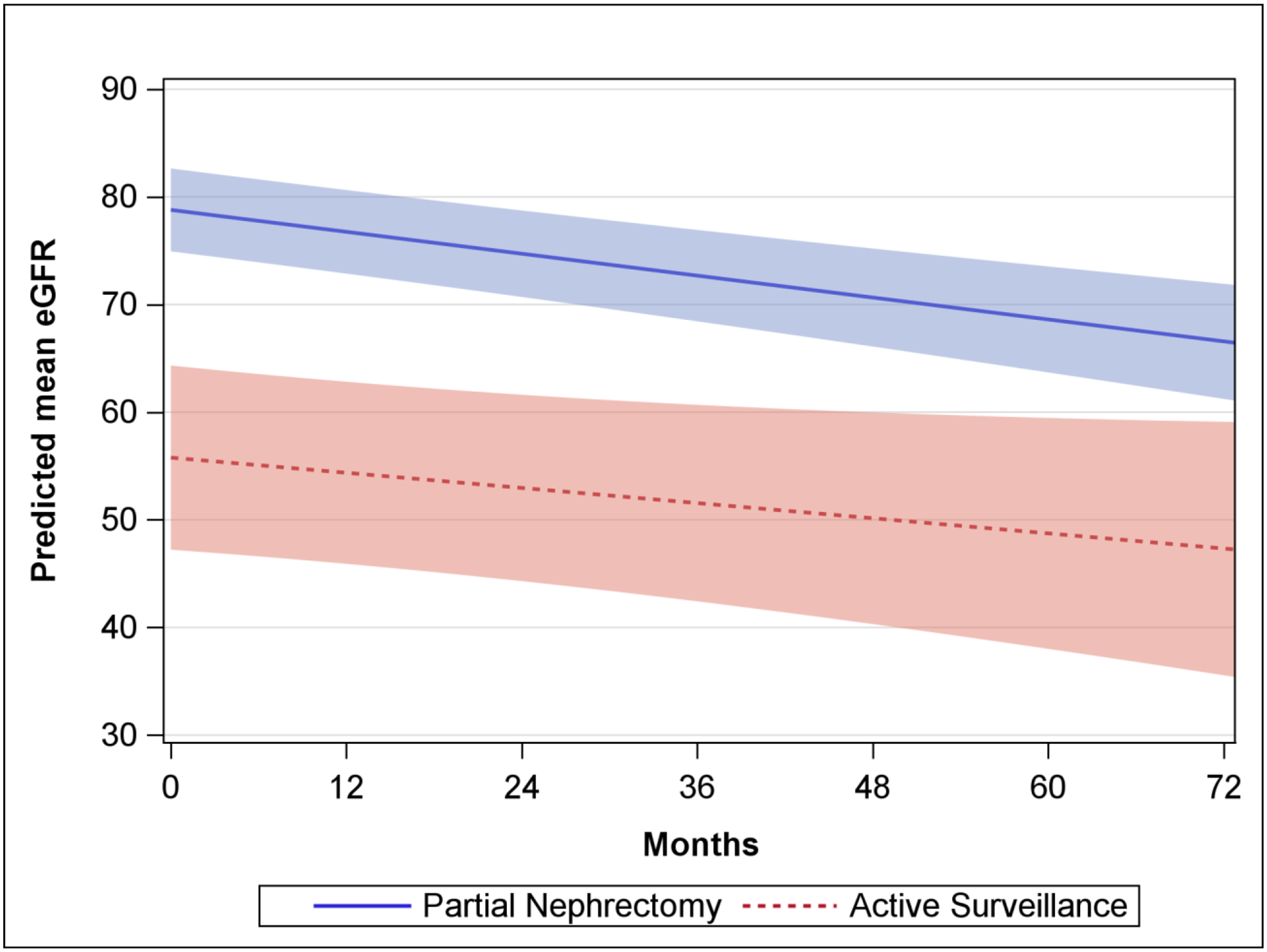
Predicted mean eGFR from the generalized estimating equation for patients managed with oncocytoma managed on AS and with PN excluding 11 AS patients that underwent delayed intervention. Shaded area represents the 95% confidence interval.
Lastly, we fit a logistic model to predict progression to CKD stage III or greater for the 91 patients with a baseline eGFR >60 (Table 2C). As expected, patient with a higher baseline eGFR (OR: 0.87, 95% CI: 0.82–0.92, p<0.001) had decreased odds while longer follow up time (OR 1.03, 95% CI: 1.02–1.04, p<0.001) was associated with a higher odds of progression to CKD stage III or greater. There was no significant difference in the odds of progression to CKD stage III or greater for patients with oncocytoma managed with AS vs. PN (OR 0.61, 95% CI 0.16–2.33, p=0.47, Table 2C and Figure 2C).
Table 2C.
Generalized Estimating Equation testing the association of factors associated with progression to CKD stage III or greater for patients with a baseline eGFR >60.
| OR | 95% CI | p | |
|---|---|---|---|
| Follow up time (continuous, months) | 1.03 | 1.02–1.04 | <0.001 |
| Management Strategy | |||
| Active Surveillance | Ref | Ref | Ref |
| PN | 0.61 | 0.16–2.33 | 0.47 |
| Baseline eGFR (continuous, per 1 unit mL/min/1.73m2) | 0.87 | 0.82–0.92 | <0.001 |
Figure 2C.
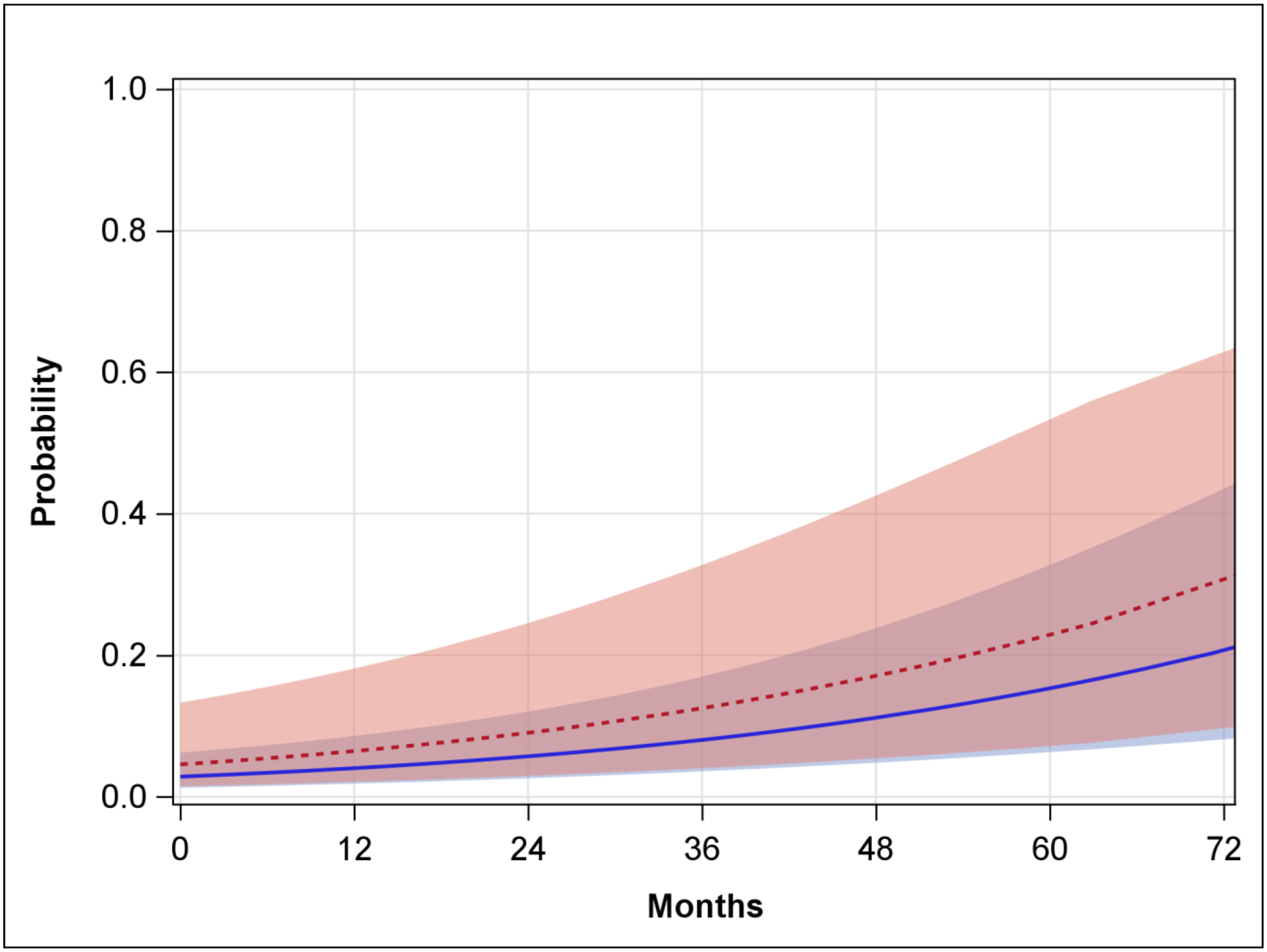
Predicted probability of progression to CKD stage III or greater for patients with a baseline eGFR >60 managed with AS compared with PN. Red line is predicted probability for AS patients and blue is the predicted probability for PN patients. Shaded areas represent the 95% confidence intervals.
1.4. Discussion
The decision to surgically intervene on an asymptomatic solitary renal mass pivots on the balance of potential benefit from intervention and the estimated risks of perioperative morbidity, mortality, and likelihood for long-term renal dysfunction. To aid in the medical decision-making process for patients with oncocytomas, a benign renal tumor, we investigated the association of renal function decline in patients managed with AS and PN. Our findings demonstrate that patients on AS, when compared those who underwent PN, had a similar decline in renal function over time and a similar probability of progressing to CKD stage III or greater. Neither AS nor PN provided a superior outcome with regard to preservation of renal function for patients with an oncocytoma.
A recently published retrospective, multi-institutional cohort of patients with oncocytomas investigated the association of renal function outcomes with PN vs. AS.6 In this cohort, PN was associated with a lower decline in renal function compared with AS. Although the exact underlying mechanism for these findings remains unknown, the authors suggested that expansion of the lesion into adjacent renal tissue may impair renal function. Neves et al. recently addressed this hypothesis. In their cohort of 98 patients with oncocytomas on AS, lesion growth rate was not associated with an accelerated decline in renal function.9 In a manner consistent with Neves et al., our findings suggest renal function decline over time is likely a multi-factorial process, which is independent of management strategy for patients with oncocytomas.
Our current study is consistent with the prevailing understanding that renal function in patients with renal masses undergoing various treatments and AS are similar between AS and PN.7, 8 Removal of an entire renal unit with a radical nephrectomy appears to have the largest effect on renal function, while PN, AS, and thermal ablation exhibit a less pronounced effect on renal function. In general, the literature has reached consensus that the less manipulation, collateral damage, and resection of adjacent normal kidney, the more postoperative renal function will be preserved. Given the retrospective and/or non-randomized nature of these studies, any potential benefit of either AS or PN with regards to preservation of renal function in patients with small renal masses is potentially due to selection bias. If a true association is present and PN or AS is superior to the other management strategy, the magnitude of this benefit is likely small and not clinically meaningful. As such, active surveillance for patients with oncocytomas delivers both safety and renal function preservation. The decision for intervention should be individualized and employed cautiously. Considerations for renal function preservation appear to be orthogonal to the management decision.
As with any retrospective comparative effectiveness analysis of pre-selected cohorts, there are several limitations of this study. In addition to possible selection bias, this study is limited to patients who underwent biopsy or harbored surgically proven oncocytomas. Biopsy is not uniformly performed prior to surgery or initiation of AS in our cohort. Thus, there exists the potential to miss patients with renal mass on AS who did not undergo a biopsy and who harbor oncocytomas. Also, given the relatively small sample size, we were unable to adjust for comorbid conditions in our models which may influence longitudinal renal function. Given the small number of AS patients that underwent delayed intervention, we are unable to analyze this group separately. The potential remains that these results may be underpowered to detect a small clinical difference, if present.
1.5. Conclusions
AS and PN for patients with an oncocytoma in our cohort was associated with a small and similar decline in renal function and probability of progression to CKD stage III or greater. In our cohort, neither strategy demonstrated superiority in the preservation of longitudinal renal function in patients with an oncocytoma. Management with partial nephrectomy or active surveillance should be considered equivalent when considering long term effect on renal function in patients with oncocytomas.
Funding:
No direct or indirect funding
Footnotes
Conflicts of Interest:
None of the authors have any direct or indirect conflicts of interest pertaining to this research
References
- 1.Chandrasekar T, Boorjian SA, Capitanio U, Gershman B, Mir MC, Kutikov A. Collaborative Review: Factors Influencing Treatment Decisions for Patients with a Localized Solid Renal Mass. Eur Urol. 2021;80:575–588. [DOI] [PubMed] [Google Scholar]
- 2.Campbell SC, Clark PE, Chang SS, Karam JA, Souter L, Uzzo RG. Renal Mass and Localized Renal Cancer: Evaluation, Management, and Follow-Up: AUA Guideline: Part I. J Urol. 2021;206:199–208. [DOI] [PubMed] [Google Scholar]
- 3.Motzer RJ, Jonasch E, Boyle S, et al. NCCN Guidelines Insights: Kidney Cancer, Version 1.2021. J Natl Compr Canc Netw. 2020;18:1160–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kutikov A, Fossett LK, Ramchandani P, et al. Incidence of benign pathologic findings at partial nephrectomy for solitary renal mass presumed to be renal cell carcinoma on preoperative imaging. Urology. 2006;68:737–740. [DOI] [PubMed] [Google Scholar]
- 5.Thompson RH, Kurta JM, Kaag M, et al. Tumor size is associated with malignant potential in renal cell carcinoma cases. J Urol. 2009;181:2033–2036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meagher MF, Lane BR, Capitanio U, et al. Comparison of renal functional outcomes of active surveillance and partial nephrectomy in the management of oncocytoma. World J Urol. 2021;39:1195–1201. [DOI] [PubMed] [Google Scholar]
- 7.Danzig MR, Ghandour RA, Chang P, et al. Active Surveillance is Superior to Radical Nephrectomy and Equivalent to Partial Nephrectomy for Preserving Renal Function in Patients with Small Renal Masses: Results from the DISSRM Registry. J Urol. 2015;194:903–909. [DOI] [PubMed] [Google Scholar]
- 8.Patel HD, Pierorazio PM, Johnson MH, et al. Renal Functional Outcomes after Surgery, Ablation, and Active Surveillance of Localized Renal Tumors: A Systematic Review and Meta-Analysis. Clin J Am Soc Nephrol. 2017;12:1057–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neves JB, Varley R, Agnesi S, et al. Growth and renal function dynamics of renal oncocytomas on active surveillance. BJU international. 2021. [DOI] [PubMed] [Google Scholar]


