Abstract
The co-occurrence of substance use disorder (SUD) and posttraumatic stress disorder (PTSD) is common, and is associated with greater severity of symptoms, poorer treatment prognosis, and increased risk of return to substance use following treatment. Screening for PTSD is not routinely implemented in substance use treatment programs, despite clinical relevance. Identifying screening tools that minimize patient burden and allow for comprehensive treatment in this patient population is critical. The current study examined the utility of the Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) in identifying probable PTSD in a predominantly Black sample of 81 socioeconomically disadvantaged substance misusing hospital patients. The majority of the sample (75.3%; n = 61) were found to meet criteria for probable PTSD using a suggested clinical cut score of 33 on the PTSD Checklist for DSM-5 (PCL-5). Diagnostic utility analyses were completed and determined a cut-score of 5 for the PC-PTSD-5 to demonstrate the best performance (SE = .62, κ(1) = .22; SP = .80, κ(0) = .61; EEF = .67, κ(.5) = .32) in this sample. Results provide preliminary support for the use of the PC-PTSD-5 as a brief screening tool for probable PTSD in substance misusing patient populations. Routine use of the PC-PTSD5 during assessment may be beneficial when treatment planning with those undergoing treatment for SUD because comprehensive assessment and treatment will provide a better chance of longterm recovery.
Keywords: PC-PTSD-5, trauma, PTSD, substance use, alcohol, substance misuse
1.1. Introduction
Individuals struggling with alcohol or substance use have disproportionately high rates of trauma exposure, increasing the likelihood of developing trauma-related psychopathology (Goldstein et al., 2016; Read et al., 2004). In patients diagnosed with a substance use disorder (SUD), rates of co-occurring current posttraumatic stress disorder (PTSD) have been reported as high as 41% (Read et al., 2004) and lifetime PTSD rates have been reported as high as 52% (Reynolds et al., 2005). This high co-occurrence rate is worrisome as patients with both disorders are more prone to experiencing a variety of negative health consequences, such as poor treatment adherence, less symptomatic improvement while in treatment, greater legal issues, greater physical health problems, and an increased rate of suicide attempts compared to patients who have a single diagnosis of either disorder (Foa & Williams, 2010; Mccauley et al., 2013).
In populations suffering from SUD, PTSD and trauma exposure is infrequently measured and often goes untreated (Ford et al., 2007). However, identifying patients with co-occurring psychiatric conditions is critical to ensure the treatment of both disorders, increasing the likelihood of symptom remission from SUD. Indeed, a recent meta-analysis examining the self-medication hypothesis found that drinking to cope accounted for 80% of the variance in the relationship between PTSD and harmful alcohol use (Luciano et al., 2022). Patients with unremitted PTSD have been found to demonstrate fewer percent days abstinent following SUD treatment (Read et al., 2004). Importantly, engagement in PTSD treatment has been found to be a significant predictor of remission following treatment (Ouimette et al., 2003; Ouimette et al., 2015). Thus, there is a clear clinical need for systematic screening for PTSD in SUD treatment centers to ensure comprehensive assessment and treatment. The most used PTSD screener in healthcare settings is the PTSD Checklist for DSM-5 (PCL-5). The PCL-5 is a 20-item self-report questionnaire designed to evaluate a probable diagnosis of PTSD (Weathers et al., 2013). While the PCL-5 has been shown to be reliable and valid across various samples (Blevins et al., 2015; Geier et al., 2020; Kagee et al., 2022; Mekawi et al., 2022), shorter screening measures are available and may be a promising addition to standard intake screening with the appeal of a much lower burden on patients.
The Primary Care Posttraumatic Stress Disorder Screen (PC-PTSD) is a strong candidate as a short, reliable PTSD symptom screening measure for use in community-based SUD treatment centers. Research has explored the applicability, diagnostic efficiency, and validity of using the brief PC-PTSD in Veterans Affairs (VA) and civilian substance misusing populations. Developed originally to use in a primary care setting, the PC-PTSD for DSM-IV consists of four yes/no questions representing each PTSD symptom cluster (Prins et al., 2003). This questionnaire has demonstrated potential as a screener for PTSD in SUD samples as it has good diagnostic accuracy, is brief, and is relatively easy to administer. Kimerling and colleagues (2006) found that the PC-PTSD was suitable for detecting PTSD in majority white, male, VA patients with SUD with high sensitivity and specificity using a cut-score of three. The PC-PTSD showed a similarly high sensitivity and moderate specificity when using a cut-score of two in a majority white, male civilian Dutch SUD patient sample (van Dam et al., 2010). Additional support for the use of the PC-PTSD as a screener was found in a majority Black treatment seeking VA SUD sample, with results showing a PC-PTSD cut-score of three demonstrated optimal sensitivity and adequate specificity (Tiet et al., 2013). Most of these samples were found to meet criteria for an alcohol use disorder.
The PC-PTSD has been updated to reflect the diagnostic criteria of PTSD following the DSM-5 and now includes five items (PC-PTSD-5). Primarily, language has been adjusted to ensure participants are responding to subsequent questions about a criterion A traumatic event. The original validation study for the updated measure found that a cut-score of three optimized sensitivity in a majority white male VA sample (Prins et al., 2016). Recently, Bovin and colleagues (Bovin et al., 2021) validated the PC-PTSD-5 in a VA sample and found high levels of diagnostic accuracy, with the optimal cut-score of four for men and three for women. However, the PC-PTSD-5 has not yet been validated in a substance misusing population.
To date, no study has yet validated the PC-PTSD-5 in a socioeconomically disadvantaged, substance misusing community sample. Because of the particularly high rates of PTSD within substance misusing populations, the ability to quickly measure a patients’ trauma symptoms becomes critical for appropriate screening and treatment selection. The PC-PTSD-5 may be a brief alternative to lengthier self-report measures of trauma symptom severity, such as the PCL-5. However, it is crucial to ensure the PC-PTSD-5 performs similarly to the PC-PTSD, a measure previously validated in substance misusing samples. Additionally, the majority of past research in this area has involved veteran populations. Validation in community samples is critical for generalizability. The goal of the current study was to determine the diagnostic accuracy and appropriate cut-score of the PC-PTSD-5 compared to the PCL-5 in a sample of predominantly socioeconomically disadvantaged and minoritized substance misusing trauma-exposed individuals. We hypothesized the PC-PTSD-5 would have good overall diagnostic accuracy in the current sample. Finally, the previous studies outlined above found varying cut-scores; however, the cut-score of three appeared in the majority of studies described. Therefore, we hypothesized a cut-score of three for optimal performance.
1.2. Materials and Methods
1.2.1. Participants and Procedure
Data were collected as part of a large, ongoing study of trauma exposure and related symptoms in a healthcare-seeking population. Participants were recruited from waiting rooms at a public hospital in large city in the southeastern United States. Trained interns approached patients in various clinics regarding potential participation. During the COVID-19 pandemic, patients attending medical visits were contacted via telephone and invited to participate. Interns included undergraduate, postbaccalaureate, and graduate students who participated in didactics on research interviewing, shadowed visits, and were observed conducting interviews as training. Data collection and study procedures were approved by Emory University Institutional Review Board and the Grady Research Oversight Committee Institutional Review Board and the Emory University Institutional Review Board and the Grady Research Oversight Committee. Informed consent was obtained from all study participants after the nature of procedures were explained. Trained interns verbally administered a variety of self-report questionnaires to consenting individuals; measures were read aloud to all participants to address potential bias due to low literacy levels. On average, the interview took approximately 45 to 75 minutes and participants were compensated $20 for their time.
Between April 2018 and August 2022, 344 individuals completed the PC-PTSD-5, the PCL-5, and the Alcohol Use Disorder Identification Test (AUDIT) and/or Drug Abuse Screening Test-10 (DAST-10). Seven individuals were removed because they denied trauma exposure. To ensure our sample was comprised of individuals with current substance use concerns, participants were required to endorse a minimum score on the DAST or AUDIT. More specifically, participants were excluded from the current study due to failure to endorse a DAST score of three or greater or an AUDIT score of eight or greater, leaving a final sample of 81 participants. We computed probable DSM-5 PTSD status using participants’ scores on PCL-5 items, such that a score of 33 or greater categorized participants with probable PTSD (Bovin et al., 2016).
Methods were compared against the seven domains identified in the second version of the Quality Assessment of Diagnostic Accuracy Studies guidelines (QUADAS-2; Whiting et al., 2012) for robustness. Patients were enrolled consecutively, case-control design was avoided, there were no inappropriate exclusions, data were gathered then scored after for index and reference measures, all cut scores used were prespecified by the available literature, the reference standard is likely to correctly classify the target condition but the diagnostic gold standard was not used, both the index and reference measures were collected on the same day, all patients received the same measures, all patients meeting study inclusion criteria were included, the utilized sample may differ from other general community samples, there are no concerns about the index test and no concerns about the reference standard other than it is not the gold standard. All methods not meeting domain criteria are further discussed in study limitations.
1.2.2. Measures
1.2.2.1. Drug Abuse Screening Test-10 (DAST-10).
The DAST-10 is a brief, 10-item screening tool assessing a participant’s degree of non-medical drug use and/or prescribed drug use in excess in the last year (Skinner, 1982). Each item is scored dichotomously, and a total score was generated by summing scale items. For the purposes of the current study, a cut-score of three was used to ensure the sample included individuals with current substance use concerns (Bohn, Babor, & Kranzler, 1991; Villalobos-Gallegos et al., 2015); however, a participant was not removed from analyses for failing to endorse a DAST-10 score of three or greater if their AUDIT score was greater 8 in the current study (α = .52).
1.2.2.2. Alcohol Use Disorder Identification Test (AUDIT).
The AUDIT, a 10-item screener, was used to measure a participant’s self-reported alcohol consumption and alcohol-related problems in the last year (Saunders et al., 1993). Participants had to endorse at least a score of eight to be included in analyses (Saunders et al., 1993); similarly to the DAST-10, a participant was not removed from analyses for having scores below the AUDIT cut-scores if their DAST-10 score was greater than three. Cronbach’s alpha was good in the current study (α = .76).
1.2.2.3. Traumatic Events Inventory (TEI).
Lifetime history of trauma exposure was assessed using the Traumatic Events Inventory (Gillespie et al., 2009), a 14-item measure. In the current study, the TEI inquired about exposure to 19 different traumatic events individuals may have directly experienced, witnessed, or been confronted with. Each item was rated on a binary scale (0 = No, 1 = Yes). Participants who endorsed exposure to one or more traumatic events were included in analyses. Construct validity of this measure has been shown in the same hospital patient population (Gillespie et al., 2009).
1.2.2.4. PC-PTSD-5.
The PC-PTSD-5 (Prins et al., 2016) was used to determine the presence of posttraumatic stress symptoms over the last month. Each of five items were rated on a binary scale (0 = No, 1 = Yes). Higher scores indicate increased posttraumatic stress symptoms. Cronbach’s alpha was acceptable in the current study (α = .73).
1.2.2.5. PCL-5.
Posttraumatic stress symptoms were also assessed via the PCL-5 (Weathers et al., 2013), a 20-item self-report measure that corresponds with DSM-5 diagnostic criteria for PTSD and has been found to share strong consistency with the CAPS-5 (Moshier et al., 2018). Respondents indicate the extent to which they were bothered by each symptom in the last month. Items are rated on a 5-point scale ranging from 0 (Not at all) to 4 (Extremely). The PCL-5 has demonstrated high internal consistency and test-retest reliability, as well as strong convergent and discriminant validity (Blevins et al., 2015; Bovin et al., 2016; Mekawi et al., 2022; Wortmann et al., 2016). Cronbach’s alpha was excellent in the current study (α = .94).
1.2.3. Data Analysis
Descriptive analyses were completed using IBM SPSS Statistics Version 28, and diagnostic utility analyses were completed using DAG-Stat (Mackinnon, 2000). We computed scale-level descriptive statistics for the PC-PTSD-5 and PCL-5. Then, we further examined subscale-level descriptive statistics for the PCL-5 and item-level descriptive statistics for the PC-PTSD-5. We computed bivariate correlations between PC-PTSD-5 items, PC-PTSD-5 total score, PCL-5 subscales, PCL-5 total score, and probable PTSD status. We then conducted Receiver Operating Characteristics (ROC) analysis and obtained the area under the curve (AUC) to determine the ability of the PC-PTSD-5 to distinguish between participants with probable PTSD and those without based on response to items on the PCL-5. AUC value was interpreted based on the following guidelines: AUC > 0.9 Excellent, > 0.8 Good, > 0.7 Sub-Adequate, and < 0.7 Poor (Hosmer, Lemeshow, et al., 2013).
We computed sensitivity (SE; i.e., probability of a positive PC-PTSD-5 result among positive PCL-5 cases), specificity (SP; i.e., probability of a negative PC-PTSD-5 result among negative PCL-5 cases), positive predictive value (PPV; i.e., probability that an individual in the sample has probable PTSD on the PCL-5 when the PC-PTSD-5 is positive), negative predictive value (NPV; i.e., probability that an individual in the sample does not have probable PTSD on the PCL-5 when the PC-PTSD-5 is negative), and efficiency (EFF; i.e., the proportion of the total number of PC-PTSD-5 predictions of self-reported probable PTSD that were correct) for each possible PC-PTSD-5 cut-score. We calculated 95% confidence intervals for each performance metric (McKenzie et al., 1997). Lastly, weighted kappa coefficients (κ) were computed as test quality indices adjusted for chance agreement (Agresti, 2013). Kappa coefficients were computed for sensitivity SE [κ(1)], specificity SP [κ(0)], and efficiency EFF [κ(.5)]. We interpreted kappas based on the following guidelines: κ < .2 slight agreement, .21-.40 fair agreement, .41-.60 moderate agreement, .61-.80 substantial agreement, and > .80 nearly perfect agreement (Landis & Koch, 1977).
1.3. Results
The majority of the current substance misusing sample (75.3%; n = 61) were found to have probable PTSD based on their responses to the PCL-5. Three participants were missing a last year DAST-10 score (M = 2.35; SD = 2.24) and all participants had last year AUDIT scores (M = 12.27; SD = 7.63). Fifty-eight percent of the current sample reported misusing only alcohol in the last year (n = 47), 13.6% reported misusing only drugs in the last year (n = 11), and 28.4% reported misusing both alcohol and drugs in the last year (n = 23). Participants were primarily Black (80.2%, n = 65) and female (69.1%, n = 56), with a mean age of 42.4 years (SD = 12.10 years). Most participants reported graduating high school (82.7%, n = 67) and living in poverty (i.e., household monthly income of less than $2,000; 72.6%, n = 53) (see Table 1 for additional demographics).
Table 1.
Demographic Characteristics of Study Participants
| Characteristic | n | M/% | SD | Range |
|---|---|---|---|---|
| Age | 81 | 42.40 | 12.10 | 21–64 |
| Sex | 81 | |||
| Female | 56 | 69.1% | ||
| Male | 25 | 30.9% | ||
| Gender | 49 | |||
| Woman | 32 | 39.50% | ||
| Man | 16 | 19.8% | ||
| Non-binary/gender-queer | 1 | 1.2% | ||
| Race | 81 | |||
| Black/African American | 65 | 80.2% | ||
| White/Caucasian | 14 | 17.3% | ||
| Hispanic/Latino | 1 | 1.2% | ||
| Mixed | 1 | 1.2% | ||
| Education | 81 | |||
| Less than 12th grade | 14 | 17.3% | ||
| GED | 8 | 9.9% | ||
| High school graduate | 17 | 21.0% | ||
| Some college or technical school | 23 | 28.4% | ||
| Technical school graduate | 1 | 1.2% | ||
| College graduate | 15 | 18.5% | ||
| Graduate school | 3 | 3.7% | ||
| Currently Employed | 80 | |||
| Yes | 35 | 43.2% | ||
| No | 45 | 55.6% | ||
| Monthly Household Income | 73 | |||
| <$250 | 15 | 18.5% | ||
| $250–499 | 3 | 3.7% | ||
| $500–999 | 11 | 13.6% | ||
| $1,000–1,999 | 24 | 29.6% | ||
| ≥$2,000 | 20 | 24.7% |
All participants in the current sample endorsed exposure to one or more trauma types (n = 81). Participants reported exposure to an average of 9.04 trauma types (SD = 3.34). The most frequently reported trauma types were witnessing family violence (92.4%, n = 73), being attacked by non-romantic partner (79%, n = 64), attacked by a romantic partner (71.6%, n = 58), and experiencing a serious accident or injury (71.6%, n = 58).
Descriptive analyses indicate evidence of adequate internal consistency (see Table 2). Computed correlations range from .23-.73 generally indicating evidence for both internal consistency and distinct symptom clusters (see Table 3). The PC-PTSD-5 re-experiencing item, was most highly correlated with the PCL-5 re-experiencing symptom cluster, the altered arousal item was most highly correlated with the altered arousal symptom cluster, and the negative mood and cognitions item most highly correlated with the negative alterations in cognition and mood cluster. Interestingly, the avoidance item was most highly correlated with the re-experiencing cluster, followed closely by alterations in arousal and reactivity cluster. The numbing item was most highly correlated with the alterations in arousal and reactivity cluster. All PC-PTSD-5 items correlated with probable PTSD using the PCL-5 cut score of 33. The AUC was .80 (SE = .07; 95% CI, .67-.92; p < .001), indicating good performance. A cut-score of 5 demonstrated the best performance and quality indices (see Table 4). Performance and quality indices indicated fair sensitivity [SE = .62, κ(1) = .22], substantial specificity [SP = .80, κ(0) = .61], and fair efficiency [EEF = .67, κ(.5) = .32]. Predictive values suggest that approximately 90% of those positive for PTSD at a PC-PTSD-5 cut score of 5 would truly be positive for a diagnosis of PTSD while approximately 41% of those found to be negative for PTSD using a PC-PTSD-5 cut score of 5 would truly be negative for a diagnosis of PTSD.
Table 2.
Descriptive Statistics for PC-PTSD-5 and PCL-5
| Variable | Items | N | M | SD | Possible Range | Range | Skewness | Kurtosis | α |
|---|---|---|---|---|---|---|---|---|---|
| PC-PTSD-5 | |||||||||
| Total Scale | 5 | 81 | 3.99 | 1.40 | 0–5 | 0–5 | −1.50 | 1.56 | .73 |
| 1. Nightmares/Intrusive Memories | -- | 81 | .77 | .43 | 0–1 | 0–1 | −1.28 | −.38 | -- |
| 2. Internal/External Avoidance | -- | 81 | .85 | .36 | 0–1 | 0–1 | −2.02 | 2.13 | -- |
| 3. Hypervigilance/Startle | -- | 81 | .79 | .41 | 0–1 | 0–1 | −1.45 | .11 | -- |
| 4. Emotional Numbness/Withdrawal | -- | 81 | .84 | .37 | 0–1 | 0–1 | −1.89 | 1.59 | -- |
| 5. Persistent Guilt/Distorted Blame | -- | 81 | .74 | .44 | 0–1 | 0–1 | −1.12 | −.77 | -- |
| PCL-5 | |||||||||
| Total Scale | 20 | 81 | 43.53 | 17.95 | 0–80 | 4–72 | −.41 | −.58 | .94 |
| REX Subscale | 5 | 81 | 10.73 | 5.35 | 0–20 | 0–20 | −.32 | −.69 | .86 |
| AV Subscale | 2 | 81 | 4.72 | 2.36 | 0–8 | 0–8 | −.49 | −.58 | .76 |
| NACM Subscale | 7 | 81 | 15.16 | 6.63 | 0–28 | 0–25 | −.29 | −.93 | .83 |
| AAR Subscale | 6 | 81 | 12.93 | 5.43 | 0–24 | 0–24 | −.23 | −.71 | .79 |
Note. N = 81. REX = Reexperiencing; AV = Avoidance; NACM = Negative alterations in cognition and mood; AAR = Alterations in arousal and reactivity.
Table 3.
PC-PTSD-5 Inter-Item Correlations and Bivariate Correlations with PCL-5 and Probable DSM-5 PTSD Status
| Variable | PC-PTSD-5 Item | PC-PTSD-5 Total | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| 1. Re-experiencing | 2. Avoidance | 3. Altered Arousal | 4. Numbing | 5. Negative Mood & Cognitions | ||
| Item 1 | -- | .73** | ||||
| Item 2 | .59** | -- | .70** | |||
| Item 3 | .36** | .38** | -- | .68** | ||
| Item 4 | .31** | .29** | .35** | -- | .70** | |
| Item 5 | .27* | .23* | .25* | .51** | -- | .67** |
|
| ||||||
| PCL-5 REX | .57** | .46** | .34** | .38** | 41** | .63** |
| PCL-5 AV | .45** | .42** | .38** | .38** | .25* | .54** |
| PCL-5 NACM | .44** | 37** | .29** | .49** | .49** | .60** |
| PCL-5 AAR | 44** | .45** | .46** | .54** | .37** | .65** |
| PCL-5 Total | .53** | .47** | .40** | .51** | .45** | .68** |
|
| ||||||
| Probable PTSD | .43** | 41** | .27* | .53** | .32** | .55** |
Note. N = 81.
correlation is significant at the .01 level
correlation is significant at the .05 level. REX = Reexperiencing; AV = Avoidance; NACM = Negative alterations in cognition and mood; AAR = Alterations in arousal and reactivity.
Table 4.
Diagnostic Accuracy and Efficiency of PC-PTSD-5 for Detecting Probable DSM-5 PTSD Status on PCL-5
| Variable | Test Performance Index | Test Quality Index | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| SE | SP | PPV | NPV | EFF | κ(1) | κ(0) | κ(.5) | |
| 1 | - | .90 (.68–.99) | - | .23 (.14–.34) | .22 (.14–.33) | −.03 | −3.05 | −.05 (−.12–.02) |
| 2 | .05 (.01–.14) | .90 (.68–.99) | .60 (.15–.95) | .24 (.15–35) | .26 (.17–.37) | −.01 | −.62 | −.03 (−.10–.05) |
| 3 | .10 (.04–.20) | .75 (.51–.91) | .55 (.23–.83) | .21 (13–.33) | .26 (.17–.37) | −.04 | −.84 | −.08 (−.20–.03) |
| 4 | .23 (.13–.35) | .85 (.62–.97) | .82 (.57–.96) | .27 (.16– 39) | .38 (.28–.50) | .02 | .29 | 05 (−.06–.16) |
| 5 | .62 (.49–.74) | .80 (.56–.94) | .90 (.77–.97) | .41 (.26–.58) | .67 (.55–.77) | .22 | .61 | .32 (.14–.50) |
Note. N =81. Parentheses indicate 95% confidence interval. SE = Sensitivity; SP = Specificity; PPV = Positive predictive value; NPV = Negative predictive value; EFF = Efficiency/Correct classification rate; κ(1) = quality of SE; κ(0) = quality of SP; κ(.5) = quality of EFF.
1.4. Discussion
To our knowledge, this is the first study to examine the PC-PTSD-5’s performance in a largely minoritized, socioeconomically vulnerable, substance misusing, non-treatment seeking, community population in the United States. Generally, results provide preliminary support for the use of the PC-PTSD-5 as a brief alternative to the PCL-5 in this population. A cut-score of five was found to have optimal sensitivity, specificity, and efficiency for probably PTSD in this sample. Specificity was found to be substantial while sensitivity and efficiency were found to be fair. Predictive values suggest that the PC-PTSD-5 may have greater utility for identifying probable PTSD than for ruling out a diagnosis of PTSD in the current population.
Results of this study provide evidence for the necessity of a higher cut-score in this population than has been demonstrated in past research using both the original PC-PTSD and the PC-PTSD-5. While Bovin and colleagues (2021) found gender differences in their sample, a cut-score of three was found to be optimal for women veterans. It may be that the PC-PTSD-5 demonstrates generally lower sensitivity and specificity in the current population. Indeed, Hawn and colleagues (2020) found that the original PC-PTSD performed poorly in a marginalized college student population. While our group has found that the PC-PTSD-5 seems to perform better than the original PC-PTSD in a marginalized population (under review) and also found that a cut score of 5 performed best in the broader sample, there is likely room to improve assessment of PTSD in a population likely experiencing ongoing race-based stress, systemic racism, and exposure to community-level trauma in addition to problematic alcohol and substance use.
Limitations of this study primarily include reliance on self-report measures. The current study used the DAST-10 and AUDIT to assess for substance and alcohol misuse and a cut score of 33 on the PCL-5 to define probable PTSD. Performance of the PC-PTSD-5 was then assessed using this probable or not-probable PTSD classification. While not a structured clinician-administered assessment, the DAST-10, AUDIT, and PCL-5 are valid measures of drug and alcohol use and PTSD that are widely used across various healthcare settings. Additionally, network comparisons of the PCL-5 and the Clinician Administered PTSD Scale for DSM-5 (CAPS-5) indicate strong consistency between the two measures in a large veteran population, suggesting the PCL-5 would yield results comparable to the CAPS-5 (Moshier et al., 2018). A cut score of 31–33 has also been found to perform well when compared to the CAPS-5 (Bovin, et al., 2016). The current study used the more conservative, evidence-based cut score. Measures were collected in a systematic though not counter balanced way, potentially adding bias in interpretation. Future studies could replicate the current study’s findings using structured clinical interviews such as the Structured Clinical Interview for DSM-5, Diagnostic Interview for Anxiety, Mood, and OCD and Related Neuropsychiatric Disorders, The Mini-International Neuropsychiatric Interview, and the CAPS-5. Lastly, while the study of a largely under-served population is a strength of the current study, the demographic makeup of the study sample may limit generalizability to white or other BIPOC populations. Additional directions for future research could include further examination of possible gender, race, and ethnicity differences with respect to the performance of the PC-PTSD-5 in a substance misusing population.
1.4.1. Conclusions
The current study contributes to the literature on assessment of PTSD within racially and economically marginalized, substance misusing populations. Generally, we found preliminary evidence for the utility of the PC-PTSD-5 in identifying those with probable PTSD in this population. The optimal cut-score of five found in this investigation is higher than reported previously in other populations, and when examining the original PC-PTSD. Future research should further examine potential gender, race, and ethnicity differences in a substance misusing population by recruiting large, diverse samples and by collecting gold-standard clinical interviews in addition to self-report measures. Screening for PTSD is critical for comprehensive assessment and treatment in the substance misusing population and results of the current study demonstrate the possibility for quick screening with minimal patient and clinician burden.
Figure 1.
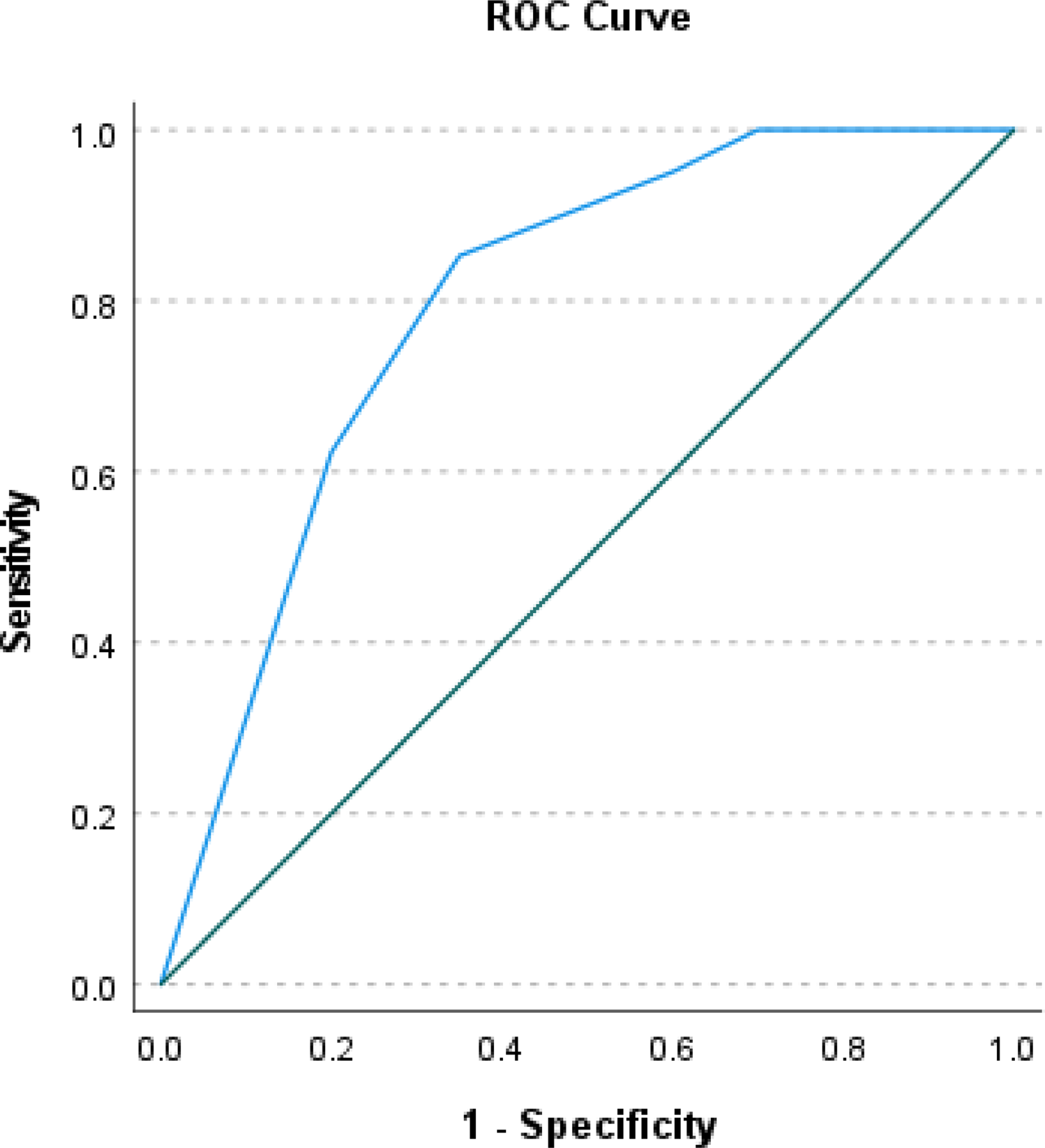
ROC Curves for PC-PTSD-5 Total Score Predicting Probable DSM-5 PTSD Status on PCL-5
Note. N = 81.
Screening for posttraumatic stress disorder (PTSD) is not routinely conducted in substance use disorder (SUD) programs, despite clinical relevance
Screening for PTSD can be completed using a brief five item screening tool
A cut-score of 5 was found to be optimal in the current study population
Acknowledgments
This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We would like to thank the entire Grady Trauma Project team for their assistance in data collection and management for this project as well as the Grady Trauma Project participants for their willingness to be involved in our research.
Role of Funding Sources
This work was supported by the National Institute of Mental Health (MH115174, MH117009), National Institute on Aging (AG062334), and National Center for Complementary & Integrative Health (AT009713). NIMH, NIA, and NCCIH had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Conflict of Interest
Dr. Welsh has received consulting fees from Applied Clinical Intelligence (ACI Clinical). All other authors declare that they have no potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agresti A. (2013). Categorical Data Analysis (3rd ed.). John Wiley & Sons. [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. Journal of Traumatic Stress, 28(6), 489–498. 10.1002/JTS.22059 [DOI] [PubMed] [Google Scholar]
- Bohn MJ., Babor TF., & Kranzler HR. (1991). Validity of the Drug Abuse Screening Test (DAST-10) in inpatient substance abusers: Problems of drug dependence. Proceedings of the 53rd Annual Scientific Meeting, The Committee on Problems of Drug Dependence, Inc., DHHS Publication No. (ADM) 92–1888, NIDA Research Monograph, 119, 233. [Google Scholar]
- Bovin MJ, Kimerling R, Weathers FW, Prins A, Marx BP, Post EP, & Schnurr PP (2021). Diagnostic Accuracy and Acceptability of the Primary Care Posttraumatic Stress Disorder Screen for the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) Among US Veterans. JAMA Network Open, 4(2), e2036733–e2036733. 10.1001/JAMANETWORKOPEN.2020.36733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379–1391. 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Foa EB, & Williams MT (2010). Methodology of a randomized double-blind clinical trial for comorbid posttraumatic stress disorder and alcohol dependence. Mental Health and Substance Use: dual diagnosis, 3(2), 131–147. 10.1080/17523281003738661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford JD, Hawke J, Alessi S, Ledgerwood D, & Petry N. (2007). Psychological trauma and PTSD symptoms as predictors of substance dependence treatment outcomes. Behaviour Research and Therapy, 45(10), 2417–2431. 10.1016/J.BRAT.2007.04.001 [DOI] [PubMed] [Google Scholar]
- Geier TJ, Hunt JC, Hanson JL, Heyrman K, Larsen SE, Brasel KJ, & deRoon-Cassini TA (2020). Validation of Abbreviated Four- and Eight-Item Versions of the PTSD Checklist for DSM-5 in a Traumatically Injured Sample. Journal of Traumatic Stress, 33(3), 218–226. 10.1002/JTS.22478 [DOI] [PubMed] [Google Scholar]
- Gillespie CF, Bradley B, Mercer K, Smith AK, Conneely K, Gapen M, Weiss T, Schwartz AC, Cubells JF, & Ressler KJ (2009). Trauma Exposure and Stress-Related Disorders in Inner City Primary Care Patients. Gen Hosp Psychiatry, 31(6), 505–514. 10.1016/j.genhosppsych.2009.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein RB., Smith SM., Chou SP., Saha TD., Jung J., Zhang H., Pickering RP., Ruan WJ., Huang B., & Grant BF. (2016). The epidemiology of DSM-5 posttraumatic stress disorder in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Social Psychiatry and Psychiatric Epidemiology, 51(8), 1137–1148. 10.1007/S00127-016-1208-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawn SE, Cusack SE, George B, Sheerin CM, Group S. for S. W, Dick D, & Amstadter AB (2020). Diagnostic validity of the PC-PTSD screen in college students. Journal of American College Health, 1–11. 10.1080/07448481.2020.1841768 [DOI] [PMC free article] [PubMed]
- Hosmer DW, Lemeshow S, & Sturdivant RX (2013). Applied Logistic Regression, 3rd Ed (Shewhart WA & Wilks SS, Eds.). John Wiley & Sons, Inc. [Google Scholar]
- Kagee A, Bantjes J, Saal W, & Sterley A. (2022). Predicting Posttraumatic Stress Disorder Caseness Using the PTSD Checklist for DSM-5 Among Patients Receiving Care for HIV. Journal of Traumatic Stress, 35(1), 13–21. 10.1002/JTS.22654 [DOI] [PubMed] [Google Scholar]
- Kimerling R, Trafton JA, & Nguyen B. (2006). Validation of a brief screen for Post-Traumatic Stress Disorder with substance use disorder patients. Addictive Behaviors, 31(11), 2074–2079. 10.1016/J.ADDBEH.2006.02.008 [DOI] [PubMed] [Google Scholar]
- Landis JR, & Koch GG (1977). The Measurement of Observer Agreement for Categorical Data. Biometrics, 33(1), 159. 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- Lathan EC, Petri JM, Haynes T, Sonu SC, Mekawi Y, Michopoulos V, & Powers A. (2023). Evaluating the performance of the Primary Care Posttraumatic Stress Disorder Screen for DSM-5 (PC-PTSD-5) in a trauma-exposed, socioeconomically vulnerable patient population. Journal of Clinical Psychology in Medical Settings, 1–13. [DOI] [PMC free article] [PubMed]
- Luciano MT., Acuff SF., Olin CC., Lewin RK., Strickland JC., McDevitt-Murphy ME., Murphy JG. (2022). Posttraumatic stress disorder, drinking to cope, and harmful alcohol use: A multivariate meta-analysis of the self-medication hypothesis. Journal of Psychopathology and Clinical Science, 131(5), 447–456. 10.1037/abn0000764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackinnon A. (2000). A spreadsheet for the calculation of comprehensive statistics for the assessment of diagnostic tests and inter-rater agreement. Computers in Biology and Medicine, 30(3), 127–134. 10.1016/S0010-4825(00)00006-8 [DOI] [PubMed] [Google Scholar]
- McCauley JL, Killeen T, Gros DF, Brady KT, & Back SE (2012). Posttraumatic Stress Disorder and Co-Occurring Substance Use Disorders: Advances in Assessment and Treatment. Clinical psychology : a publication of the Division of Clinical Psychology of the American Psychological Association, 19(3), 10.1111/cpsp.12006. 10.1111/cpsp.12006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie DP, Vida S, Mackinnon AJ, Onghena P, & Clarke DM (1997). Accurate confidence intervals for measures of test performance. Psychiatry Research, 69(2–3), 207–209. 10.1016/S0165-1781(96)02952-6 [DOI] [PubMed] [Google Scholar]
- Mekawi Y., Silverstein MW., Walker A., Ishiekwene M., Carter S., Michopoulos V., Stevens JS., & Powers A. (2022). Examining the psychometric properties of the PCL-5 in a black community sample using item response theory. Journal of Anxiety Disorders, 87, 102555. 10.1016/J.JANXDIS.2022.102555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moshier SJ, Bovin MJ, Gay NG, Wisco BE, Mitchell KS, Lee DJ, Sloan DM, Weathers FW, & Schnurr PP (2018). Examination of Posttraumatic Stress Disorder Symptom Networks Using Clinician-Rated and Patient-Rated Data HHS Public Access. J Abnorm Psychol, 127(6), 541–547. 10.1037/abn0000368.supp [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouimette PC, Moos RH, & Finney JW (2015). Two-year mental health service use and course of remission in patients with substance use and posttraumatic stress disorders. Journal of Studies on Alcohol, 61(2), 247–253. 10.15288/JSA.2000.61.247 [DOI] [PubMed] [Google Scholar]
- Ouimette P, Moos RH, & Finney JW (2003). PTSD treatment and 5-year remission among patients with substance use and posttraumatic stress disorders. Journal of Consulting and Clinical Psychology, 71(2), 410–414. [DOI] [PubMed] [Google Scholar]
- Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, Kaloupek DG, Schnurr PP, Kaiser AP, Leyva YE, & Tiet QQ (2016). The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5): Development and Evaluation Within a Veteran Primary Care Sample. Journal of General Internal Medicine. 10.1007/s11606-016-3703-5 [DOI] [PMC free article] [PubMed]
- Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, Thrailkill A, Gusman FD, & Sheikh JL (2003). The primary care PTSD Screen (PC-PTSD): Development and operating characteristics see Corrigendum. Primary Care Psychiatry, 9(1), 9–14. 10.1185/135525703125002360 [DOI] [Google Scholar]
- Read JP, Brown PJ, & Kahler CW (2004). Substance use and posttraumatic stress disorders: Symptom interplay and effects on outcome. Addictive Behaviors, 29(8), 1665–1672. 10.1016/J.ADDBEH.2004.02.061 [DOI] [PubMed] [Google Scholar]
- Reynolds M., Mezey G., Chapman M., Wheeler M., Drummond C., & Baldacchino A. (2005). Co-morbid post-traumatic stress disorder in a substance misusing clinical population. Drug and Alcohol Dependence, 77(3), 251–258. 10.1016/J.DRUGALCDEP.2004.08.017 [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, & Grant M. (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction (Abingdon, England), 88(6), 791–804. 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- Skinner HA (1982). The drug abuse screening test. Addictive Behaviors, 7(4), 363–371. 10.1016/0306-4603(82)90005-3 [DOI] [PubMed] [Google Scholar]
- Tiet QQ, Schutte KK, & Leyva YE (2013). Diagnostic accuracy of brief PTSD screening instruments in military veterans. Journal of Substance Abuse Treatment, 45(1), 134–142. 10.1016/j.jsat.2013.01.010 [DOI] [PubMed] [Google Scholar]
- van Dam D, Ehring T, Vedel E, & Emmelkamp PMG (2010). Validation of the Primary Care Posttraumatic Stress Disorder screening questionnaire (PC-PTSD) in civilian substance use disorder patients. Journal of Substance Abuse Treatment, 39(2), 105–113. 10.1016/J.JSAT.2010.05.005 [DOI] [PubMed] [Google Scholar]
- Villalobos-Gallegos L, Pérez-López A, Mendoza-Hassey R, Graue-Moreno J, & Marín-Navarrete R. (2015). Psychometric and diagnostic properties of the Drug Abuse Screening Test (DAST): Comparing the DAST-20 vs. the DAST-10. Salud Mental, 38(2), 89–94. [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). PTSD Checklist for DSM-5 (PCL-5). http://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp Try it yourself: http://traumadissociation.com/pcl5-ptsd
- Whiting PF, Rutjes AWS, Westwood ME, Mallett S, Deeks JJ, Reitsma JB,... Bossuyt PMM (2012). QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Annals of Internal Medicine, 155(8), 529–536. 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- Wortmann JH., Jordan AH., Weathers FW., Resick PA., Dondanville KA., Hall-Clark B., Foa EB., Young-McCaughan S., Yarvi JS., Hembree EA., Mintz J., Peterson AL., & Litz BT. (2016). Psychometric analysis of the PTSD checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment, 28(11). 10.1037/pas0000260 [DOI] [PubMed] [Google Scholar]


