Abstract
BACKGROUND:
The management of mechanical ventilation critically impacts outcome for patients with acute respiratory failure. Ventilator settings in the early post-intubation period may be especially influential on outcome. Low tidal volume ventilation in the prehospital setting has been shown to impact the provision of low tidal volume after admission and influence outcome. However, there is an overall paucity of data on mechanical ventilation for air medical transport patients. The objectives of this study were to characterize air medical transport ventilation practices and assess variables associated with nonprotective ventilation.
METHODS:
This was a multi-center, nationwide (approximately 130 bases) retrospective cohort study conducted on consecutive, adult mechanically ventilated air medical transport patients treated in the prehospital environment. Descriptive statistics were used to assess the cohort; the chi-square test compared categorical variables, and continuous variables were compared using independent samples t test or Mann-Whitney U test. To assess for predictors of nonprotective ventilation, a multivariable logistic regression model was constructed to adjust for potentially confounding variables. Low tidal volume ventilation was defined as a tidal volume of ≤ 8 mL/kg predicted body weight (PBW).
RESULTS:
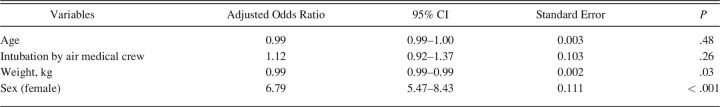
A total of 68,365 subjects were studied. Height was documented in only 4,186 (6.1%) subjects. Significantly higher tidal volume/PBW (8.6 [8.3–9.2] mL vs 6.5 [6.1–7.0] mL) and plateau pressure (20.0 [16.5–25.0] cm H2O vs 18.0 [15.0–22.0] cm H2O) were seen in the nonpro-tective ventilation group (P < .001 for both). According to sex, females received higher tidal volume/PBW compared to males (7.4 [6.6–8.0] mL vs 6.4 [6.0–6.8] mL, P < .001) and composed 75% of those subjects with nonprotective ventilation compared to 25% male, P < .001. After multivariable logistic regression, female sex was an independent predictor of nonprotective ventilation (adjusted odds ratio 6.79 [95% CI 5.47–8.43], P < .001).
CONCLUSIONS:
The overwhelming majority of air medical transport subjects had tidal volume set empirically, which may be exposing patients to nonprotective ventilator settings. Given a lack of PBW assessments, the frequency of low tidal volume use remains unknown. Performance improvement initiatives aimed at indexing tidal volume to PBW are easy targets to improve the delivery of mechanical ventilation in the prehospital arena, especially for females.
Keywords: mechanical ventilation, prehospital, lung-protective ventilation, air medical transport
Introduction
The management of mechanical ventilator settings is a critical determinant of outcome for patients with acute respiratory failure. By mitigating ventilator-associated lung injury (VALI), lung-protective ventilation improves outcome for those with ARDS, and there is increased recognition of benefit in patients without ARDS as well.1-13 The early period of mechanical ventilation may be even more critical, as demonstrated by the prognostic significance of initial lung-protective ventilator settings and survival in ARDS.7 Similarly, efforts to assure early adherence to lung-protective ventilation in the emergency department (ED) have been associated with improved clinical outcomes.8,14,15 Further stressing the importance of early ventilator settings, it has been consistently shown that ventilator settings in the ED hold influence on downstream ventilator settings in ICU and the likelihood of ever receiving lung-protective ventilation.8,14,16-19 Therefore, an emphasis on best practices during the entire period of mechanical ventilation could improve care delivery and increase overall adherence to lung-protective ventilation.20,21
Analogous to the time spent in the ED and early ICU, the approach to prehospital mechanical ventilation could be an important contributor to both overall adherence to lung-protective ventilation and outcome. In a retrospective study of 235 mechanically ventilated adults, low tidal volume ventilation was provided to only 13% of subjects in the prehospital domain, yet prehospital low tidal volume was predictive of ever receiving low tidal volume in both the ED and ICU.22 Similarly, in another cohort study (n = 383), transport tidal volume was a strong predictor of ICU tidal volume such that those subjects exposed to high prehospital tidal volume were > 3 times as likely to also received high tidal volume in the ICU.23 Finally, in a small cohort study of subjects with septic shock, prehospital tidal volume was an independent predictor of mortality.24 However, there is a relative paucity of data regarding mechanical ventilation in the air medical transport domain, as it is overall limited to primarily small and single-center studies.22-26 Therefore, prehospital air medical transport mechanical ventilation practices remain incompletely characterized, which may have important implications for the more than 640,000 patients who require air medical transport annually in the United States alone.27 The obje-ctives of this study were to (1) characterize air medical transport mechanical ventilation practices across a multi-center air medical transport provider and (2) assess variables associated with nonprotective ventilation.
QUICK LOOK.
Current Knowledge
Lung-protective ventilator settings during the early period of respiratory failure have been demonstrated to increase the likelihood of ever receiving lung protection in the ICU and are associated with improved outcomes. Similarly, ventilator settings during air medical transport have been shown to be associated with downstream ventilator settings in the emergency department and ICU. However, there is an overall paucity of data on prehospital mechanical ventilation for air medical transport patients.
What This Paper Contributes to Our Knowledge
The overwhelming majority of air medical transport patients has tidal volume set empirically, which may be exposing patients to nonprotective ventilator settings. Given a lack of height assessments, the frequency of lung-protective settings in air medical transport patients remains unknown. Performance improvement initiatives aimed at indexing tidal volume to predicted body weight are easy targets to improve the delivery of mechanical ventilation in the prehospital arena, especially for females.
Methods
Study Design
Consecutive, adult mechanically ventilated air medical transport patients treated in the prehospital environment between January 2015–December 2020 were studied in this retrospective cohort study. Air Methods, an air medical transport provider with > 300 bases dispersed across 48 states in the United States, transported and treated all patients. The bases in this study were restricted to the community-based services (approximately 160 bases) as they used the same electronic patient charting system during the study period. The study is reported in accordance with the Strengthening Reporting of Observational Studies in Epidemiology statement.
No consent was required for the study, which was approved prior to study initiation by the Human Research Protection Office (HRPO) at the primary study site (HRPO number 202006068).
Participants
Query of the electronic medical record system used by Air Methods (ie, emsCharts) was used to identify all consecutive mechanically ventilated adult air medical transport patients. The study period began in 2015, owing to the fact that the electronic record system was consistent over the entire study duration, and quality documentation was consistent during this time period. Further, with an estimated sample size of approximately 70,000 subjects, we were confident we would be able to adequately address the prespecified research questions. The inclusion criteria were age ≥ 18 y and receipt of mechanical ventilation via an endotracheal tube by the air medical transport team. Facility-to-facility transfers (eg, ED to ICU) as well as scene flights (eg, patients intubated in the field) were included. Patients without a documented tidal volume were excluded.
Assessments and Outcome Measures
Baseline characteristics included age, weight, sex, race, vital signs, and select laboratory values. In subjects with multiple vital sign variables documented, the median [interquartile range (IQR)] and mean SD values were calculated. The laboratory variables were those that were documented in emsCharts by the air medical crew, and obtained prior to crew arrival, such as in the ED where the crew was dispatched to. These laboratory variables included lactate, creatinine, hemoglobin, platelets, bilirubin, and arterial blood gases. To index tidal volume to predicted body weight (PBW), in subjects with a documented height, PBW was calculated according to the following formula: men, 50 + (2.3 * [height in inches − 60]); females, 45.5 + (2.3 * [height in inches − 60]). Process of care variables included endotracheal intubation (ie, by air medical crew vs prior to arrival), vasopressor use, and duration of care. Duration of care (in hours) was calculated as the elapsed time from crew arrival and their assumption of patient care to handoff of care to clinicians at the receiving facility.
The indication for mechanical ventilation was extrapolated from the documented chief complaint and included sepsis, respiratory failure, cardiac (eg, acute myocardial infarction, congestive heart failure), airway obstruction, sudden cardiac arrest, drug overdose, cerebrovascular accident, intracranial hemorrhage, seizure, traumatic brain injury, altered mental status, trauma, and other. A structured process for adjudication of the indication for mechanical ventilation was developed and followed. In the master data file, each potential indication for mechanical ventilation was given its own column, and binary determinations were made regarding whether the documented chief complaint field contained key words suggesting a given categorization. Chief complaint categories contained either primary causal conditions (eg, airway obstruction, sepsis) or conditions that were not necessarily explanatory (eg, altered mental status). Causal conditions were prioritized for categorization. As an example, a documented chief complaint of “traumatic head injury with altered mental status” would have been adjudicated as “traumatic brain injury” as the indication for mechanical ventilation.
Ventilator-related data included mode of mechanical ventilation, tidal volume, PEEP, FIO2, breathing frequency, peak and plateau pressures, and end-tidal carbon dioxide. Lung-protective ventilation was defined as the use of tidal volume of ≤ 8 mL/kg PBW, as this has been the upper limit of tidal volume in prior work of low tidal volume ventilation in ARDS.3
Statistical Analysis
Patient characteristics were assessed with descriptive statistics and frequency distributions. Categorical characteristics were compared using the chi-square test. Continuous characteristics were compared using independent samples t test or Mann-Whitney U test. Given that height was documented in only 4,186 (6.1%) patients, we felt that statistical approaches to replace 94% of this missing variable in order to calculate PBW would be unreliable. Therefore, comparisons between the lung-protective and nonprotective ventilation groups were restricted to those with PBW measurements available. To give better insight into the provision of lung-protective ventilation, we also assessed the most frequently delivered tidal volumes (ie, the mode) according to sex. This was done given the infrequent availability of PBW values and because it has been proposed that empirically choosing a fixed tidal volume of 350 mL in females and 450 mL in males could improve adherence to low tidal volume ventilation.28
To assess for predictors of nonprotective ventilation, a multivariable logistic regression model was constructed to adjust for potentially confounding variables. Following recommendations that covariates be chosen a priori, we selected variables that could influence the incidence of lung-protective ventilation, including age, weight, sex, and intubation location.29-34 Collinearity was assessed, and the model used variables that were independent of other variables. All tests were 2-tailed, and a P value < .05 was considered statistically significant.
Regarding sample size, it was fixed as it was restricted to the time periods of investigation. We estimated a priori that over 10,000 patients per year would be included in this analysis. We were, therefore, confident that the sample size would be adequate to provide both a descriptive analysis that had high external validity regarding mechanical ventilation practices in the prehospital domain and allow the conduct of analyses with adequate power and precision and an adequate event per covariable ratio.35,36
Results
Study Population
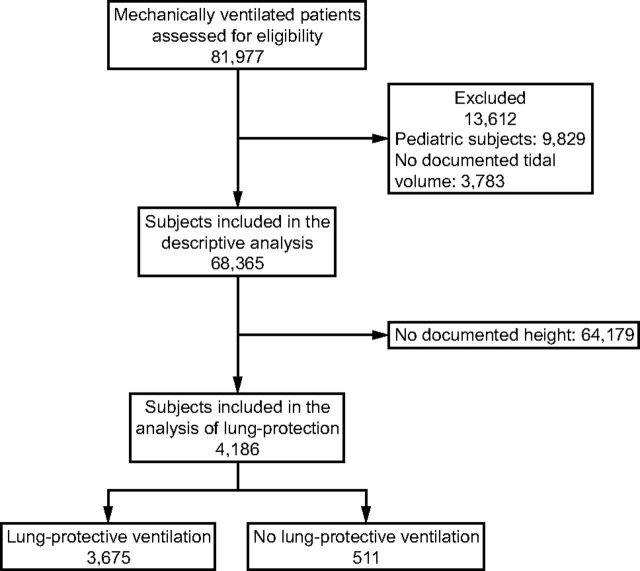
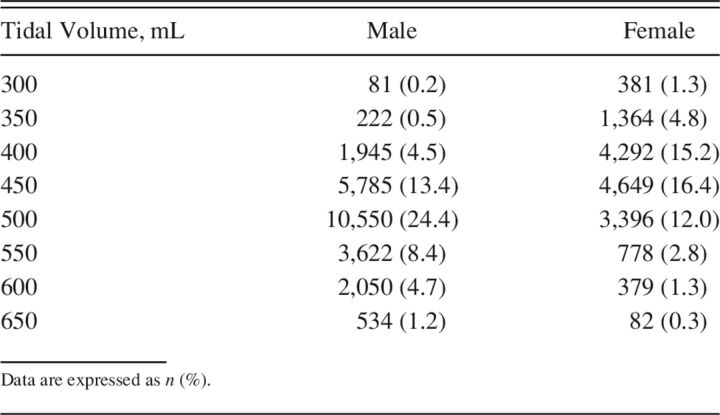
A total of 81,977 mechanically ventilated patients were included in the data set and assessed for eligibility. After exclusion of 13,612 patients who were < 18 y of age or had no documented tidal volume, the final study population for the descriptive objective of the study consisted of 68,365 subjects (Fig. 1). Baseline characteristics of the entire cohort are in Table 1. The most common indication for mechanical ventilation was altered mental status (23.3%), followed by respiratory failure (17.4%). Median (IQR) duration of care was 1.1 h (0.9–1.5).
Fig. 1.
Flow chart.
Table 1.
Available Characteristics of Mechanically Ventilated Air Medical Transport Subjects
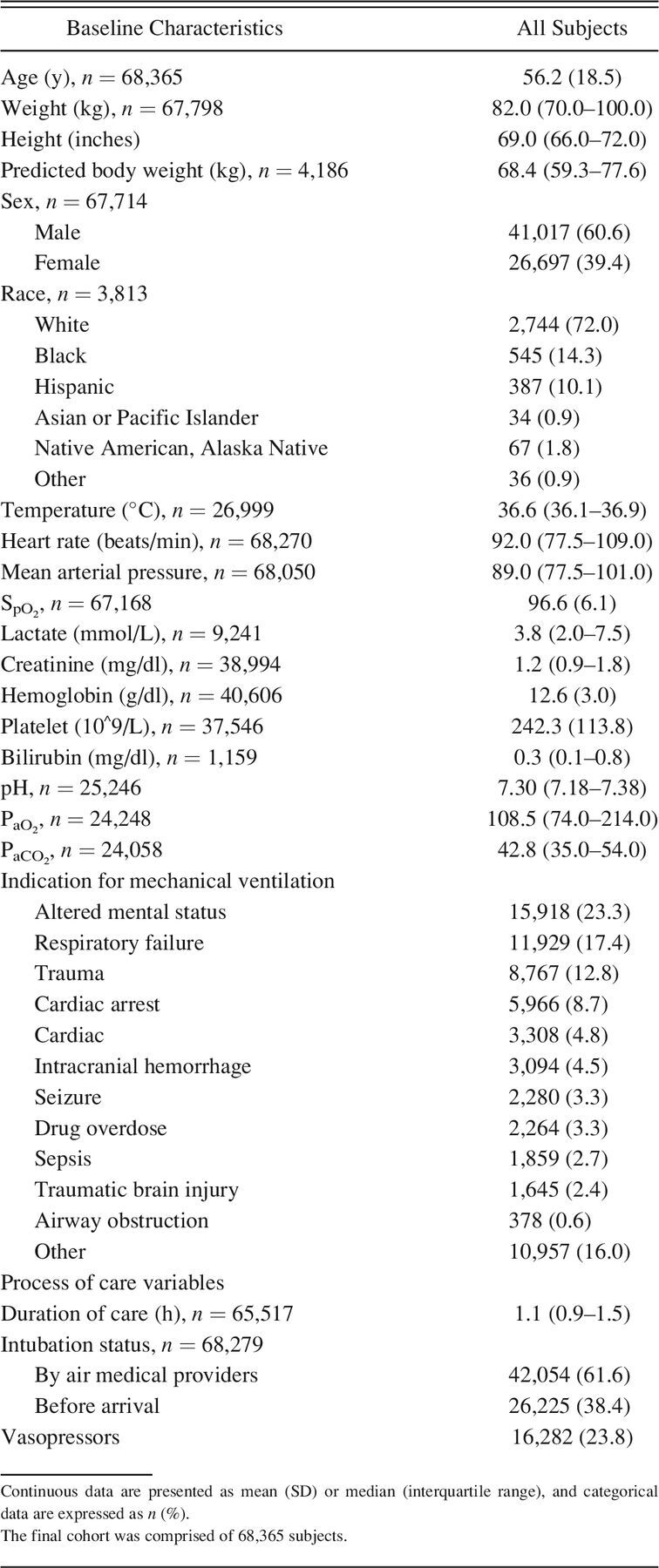
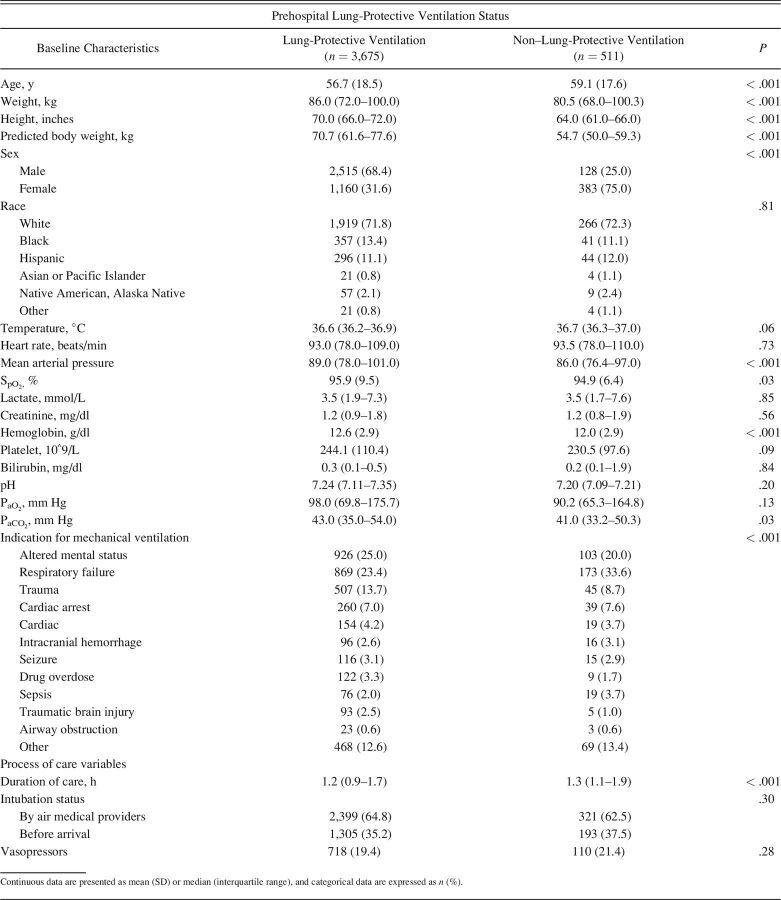
Four thousand one hundred eighty-six (6.1%) subje-cts had a documented height and, therefore, a calculated PBW. Nonprotective ventilation was provided to 511 (12.2%) of the subjects with a documented height. Baseline characteristics according to prehospital lung-protective ventilation status are in Table 2. There were significant differences in age, weight, and PBW between the 2 groups. In addition, females composed 75% of those subjects with nonprotective ventilation compared to 25% males, P < .001.
Table 2.
Characteristics of Mechanically Ventilated Air Medical Transport Patients According to Receipt of Lung-Protective Ventilation
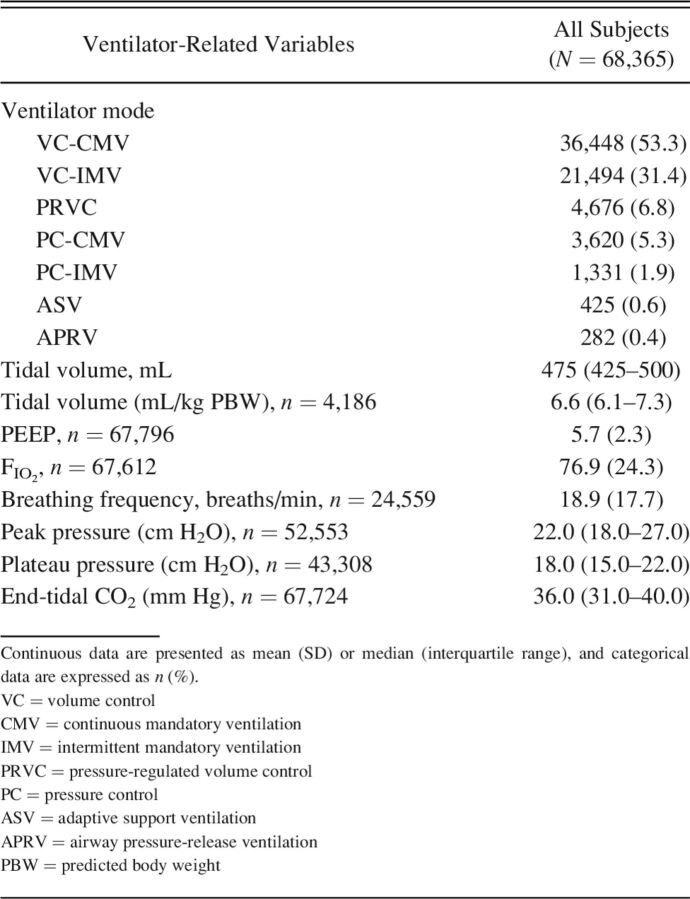
Ventilator-Related Variables
Ventilator variables for the entire cohort are in Table 3. Volume control (VC)–continuous mandatory ventilation (53.3%) and VC–intermittent mandatory ventilation (31.4%) were the most common ventilator modes used. Mean PEEP was 5.7 (2.3) and FIO2 was 76.9% (24.3). Plateau pressure was documented in 43,308 (63.3%) subjects.
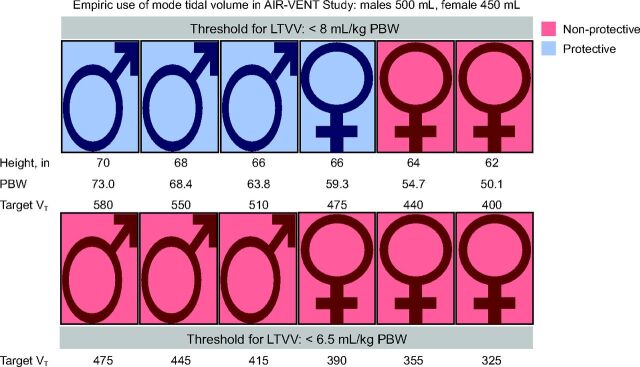
Table 3.
Ventilator Variables and Care During Air Medical Transport
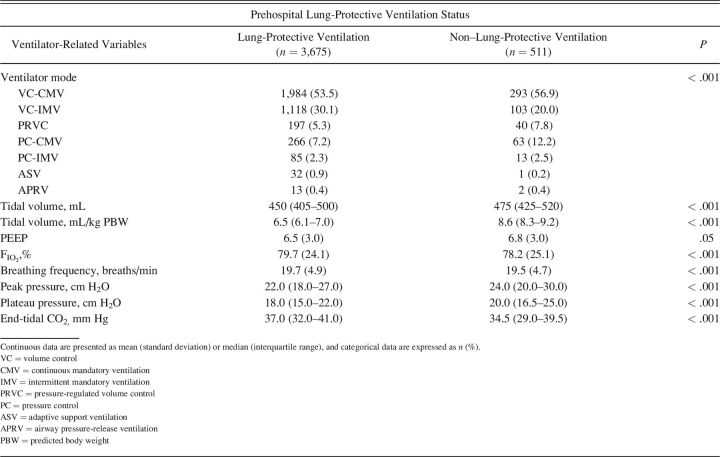
Ventilator variables according to prehospital lung-protective ventilation status are in Table 4. Subjects with nonprotective ventilation received higher tidal volume when compared to those with lung-protective ventilation (475 [425–520] mL vs 450 [405–500] mL, P < .001). Significantly higher tidal volume/PBW (8.6 [8.3–9.2) mL vs 6.5 (6.1–7.0] mL) and plateau pressure (20.0 [16.5–25.0] cm H2O vs 18.0 [15.0– 22.0] cm H2O) were also seen in the nonprotective ventilation group (P < .001 for both). According to sex, males received higher tidal volume when compared to females (500 [450–525] mL vs 440 [400–475] mL, P < .001). However, females received higher tidal volume/PBW compared to males (7.4 [6.6–8.0] mL vs 6.4 [6.0–6.8] mL, P < .001). The most frequent tidal volumes delivered according to sex are in Table 5. The mode value for males was 500 mL (24.4%) and 450 mL (16.4%) for females. Figure 2 demonstrates the impact of mechanical ventilation with an empiric choice of tidal volume, using the mode tidal volume settings. For shorter patients, it is more difficult to attain low tidal volume ventilation, especially in females.
Table 4.
Ventilator Variables and Care During Air Medical Transport According to Receipt of Lung-Protective Ventilation
Table 5.
Modus Tidal Volumes Delivered During Air Medical Transport According to Sex
Fig. 2.
The impact of mechanical ventilation with an empiric choice of tidal volume using the most common (ie, mode) tidal volume settings observed in the AIR-VENT Study. For shorter patients, it is more difficult to attain low tidal volume ventilation, especially in females. The bottom panel demonstrates that in a setting of a lower threshold (ie, 6.5 mL/kg predicted body weight [PBW]) for defining low tidal volume, indicated for patients with ARDS, empiric tidal volumes that are not indexed to PBW will result in injurious settings to all patients with these heights.
Predictors of Nonprotective Ventilation
Table 6 shows the multivariable logistic regression model with nonprotective ventilation as the dependent variable. After adjusting for covariates in the model, female sex was an independent predictor of nonprotective ventilation (adjusted odds ratio 6.79 [95% CI 5.47–8.43], P < .001), whereas lower weight was associated with a higher odds of receiving nonprotective ventilation (adjusted odds ratio 0.996 [95% CI 0.992–0.999], P = .03).
Table 6.
Multivariable Logistic Regression Analysis With Nonprotective Ventilation as the Dependent Variable
Discussion
Early work on VALI demonstrated that the mechanical ventilator can cause harm over the course of a few hours.37-39 Clinical studies from the operating room have shown that the use of lung-protective ventilation for relatively short durations can reduce systemic and pulmonary inflammation and is associated with better clinical outcomes.9,40,41 In addition, data from the ED demonstrate that early adherence to lung protection is associated with increased overall adherence in the ICU and improved clinical outcomes.8,14 For these reasons, one can view VALI as a time-sensitive emergency, and clinicians should strive to optimize ventilator settings from the onset of mechanical ventilation. Unfortunately, the provision of lung-protective ventilation remains suboptimal as demonstrated by a number of studies.5,7,42 Given the overall lack of data on mechanical ventilation in the prehospital domain, and the potential importance that this clinical arena could play across the entire chain of survival with respect to lung protection, we conducted this large cohort study to characterize mechanical ventilation practices and assess predictors of nonprotective ventilation.
The first significant finding revolves around the provision of low tidal volume ventilation across the entire cohort. Lung volume is largely determined by sex and height, so tidal volume should be indexed to PBW. In those with height documented and, therefore, an available PBW, tidal volume was 6.6 (6.1–7.3) mL/kg PBW, and low tidal volume was observed in 3,675 (87.8%) subjects. If these findings could be extrapolated to the entire cohort or confirmed with future studies in which PBW was available, this suggests that air medical transport crews are providing lung protection to a much higher percentage of patients than that seen in prior work from the ED or ICU.5,7,8,14,16,17 Unfortunately, as height was available for only 6% of the cohort, it currently remains impossible to say with confidence how frequently low tidal volume ventilation is de-livered in the prehospital domain. Further, there were observed differences in ventilator modes according to lung-protective ventilation status. Going forward, understanding factors associated with all chosen ventilator settings will be informative with respect to future quality improvement work. Due to a lack of PBW availability, we assessed the mode values for tidal volume according to sex, as it has been proposed that empirically choosing a fixed tidal volume of 350 mL in females and 450 mL in males could improve adherence to low tidal volume ventilation.28 Table 5 demonstrates that tidal volume adjustments based on sex do seem to be occurring in air medical transport patients. However, as demonstrated in Figure 2, the current amount of sex-based tidal volume adjustment may be insufficient, especially in shorter females. This is especially true, even for both sexes, if a stricter definition of low tidal volume ventilation was applied, as is the standard of care for patients with established ARDS. The current study has identified an easily fixed variable for performance improvement: height assessment and documentation in order to index tidal volume to PBW and assure adherence to low tidal volume ventilation. Recognizing potential logistical challenges in measuring height during flight, surrogate values for height, such as ulna/forearm length, have been shown to be easily obtainable in emergency settings and an accurate way to index tidal volume to PBW.43,44
A second important finding relates to the provision of low tidal volume ventilation in relation to sex. In subjects with an available PBW, females composed 75% of those receiving nonprotective ventilation. In addition, female sex was an independent predictor of nonprotective ventilation in multivariable analysis. It was shown over a decade ago that female sex is a risk for nonprotective ventilation.30 Recent work demonstrates similar findings in the ICU population.45 Our current finding is important as it reinforces the sex inequity in lung-protective ventilation and is the first to demonstrate this in the prehospital environment. It also shows that empiric tidal volume, without accurate assessment of height, is likely to leave a significant proportion of females without low tidal volume ventilation (Fig. 2).
Finally, almost 40% of air medical transport subjects did not have plateau pressure assessed. As a surrogate for end-inspiratory stretch and marker for overdistention, plateau pressure has been demonstrated to carry important prognostic significance.46,47 Whereas it is encouraging the plateau pressures were not high in this study, and below the recommended threshold of 30 cm H2O, routine monitoring of this important parameter should be a part of ensuring safe mechanical ventilation.
Overall, the data from the AIR-VENT study demonst-rate performance improvement possibilities in air medical transport patients. This includes indexing tidal volume to PBW by obtaining accurate height (or ulna length), paying special attention to ventilator settings in females, and assessing and limiting inspiratory plateau pressure.
Limitations
Prior work on mechanical ventilation in air medical transport patients has been limited to primarily small sample sizes. Whereas this large, nationwide study addresses that limitation, pertinent limitations exist. First, we have no clinical data beyond that obtained from the flight, so we cannot comment on the impact of prehospital ventilator settings on downstream care or on subject outcomes. Since multiple studies have shown the influence of immediate post-intubation ventilator settings on ED and ICU settings, we hypothesize that low tidal volume ventilation in the prehospital setting is associated with better downstream adherence and improved outcomes. However, future studies are needed to test this hypothesis. The AIR-VENT Study is a retrospective cohort study and carries all of the inherent limitations with this study design, such as lack of causation and data accuracy. Whereas all ventilator data are easily abstracted from the electronic record, they are subject to inaccuracy during routine documentation. Further, a lack of documentation of key variables (eg, height, plateau pressure) and missing data for other key variables (ie, laboratory variables and illness severity) limit our ability to comment on the quality of prehospital mechanical ventilation and compare differences between the 2 groups. However, it has allowed us to identify key areas for quality improvement. Going forward, future studies will also need to assess the impact of air medical transport ventilator settings as they relate to other key variables, such as respiratory effort, asynchrony, sedation depth, and neuromuscular blocker use.
Conclusions
The overwhelming majority of air medical transport subjects had tidal volume set empirically, which may be exposing patients to nonprotective ventilator settings. Given a lack of PBW assessments, the frequency of low tidal volume use remains unknown. Performance improvement initiatives aimed at indexing tidal volume to PBW and documenting plateau pressure are easy targets to improve the delivery of mechanical ventilation in the prehospital arena, especially for females.
Footnotes
See the Related Editorial on Page 774
The authors have disclosed no conflicts of interest.
A version of this paper was presented by Dr Fuller at SCCM 2022, held virtually April 18–21, 2022. Some of the demographic data were also used in a manuscript that was focused on prehospital sedation practices, which has been accepted for publication in Critical Care Explorations.
Dr Kollef is supported by the Barnes-Jewish Hospital Foundation. Dr Fuller is supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award number R34HL150404. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Funders played no role in the features of the study.
This study was performed at Washington University School of Medicine, Washington University in St. Louis, St. Louis, Missouri.
References
- 1.Gajic O, Dara SI, Mendez JL, Adesanya AO, Festic E, Caples SM, et al. Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med 2004;32(9):1817-1824. [DOI] [PubMed] [Google Scholar]
- 2.Hickling K, Henderson S, Jackson R. Low mortality associated with low volume pressure limited ventilation with permissive hypercapnia in severe adult respiratory distress syndrome. Intensive Care Med 1990;16(6):372-377. [DOI] [PubMed] [Google Scholar]
- 3.The Acute Respiratory Distress Syndrome Network; Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000;342(18):1301-1308. [DOI] [PubMed] [Google Scholar]
- 4.Gajic O, Frutos-Vivar F, Esteban A, Hubmayr RD, Anzueto A. Ventilator settings as a risk factor for acute respiratory distress syndrome in mechanically ventilated patients. Intensive Care Med 2005;31(7):922-926. [DOI] [PubMed] [Google Scholar]
- 5.Needham DM, Colantuoni E, Mendez-Tellez PA, Dinglas VD, Sevransky JE, Himmelfarb CRD, et al. Lung-protective mechanical ventilation and two year survival in patients with acute lung injury: prospective cohort study. BMJ 2012;344:e2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fuller BM, Mohr NM, Drewry AM, Carpenter CR. Lower tidal volume at initiation of mechanical ventilation may reduce progression to acute respiratory distress syndrome: a systematic review. Crit Care 2013;17(1):R11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Needham DM, Yang T, Dinglas VD, Mendez-Tellez PA, Shanholtz C, Sevransky JE, et al. Timing of low tidal volume ventilation and intensive care unit mortality in acute respiratory distress syndrome. A prospective cohort study. Am J Respir Crit Care Med 2015;191(2):177-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fuller BM, Ferguson IT, Mohr NM, Drewry AM, Palmer C, Wessman BT, et al. Lung-protective ventilation initiated in the emergency department (LOV-ED): a quasi-experimental, before-after trial. Ann Emerg Med 2017;70(3):406-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Futier E, Constantin J-M, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, et al. ; IMPROVE Study Group. A trial of intraoperative low tidal volume ventilation in abdominal surgery. N Engl J Med 2013;369(5):428-437. [DOI] [PubMed] [Google Scholar]
- 10.Neto AS, Cardoso SO, Manetta JA, Pereira VGM, Espósito DC, Pasqualucci MOP, et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA 2012;308(16):1651-1659. [DOI] [PubMed] [Google Scholar]
- 11.Determann RM, Royakkers A, Wolthuis EK, Vlaar AP, Choi G, Paulus F, et al. Ventilation with lower tidal volumes as compared with conventional tidal volumes for patients without acute lung injury: a preventive randomized controlled trial. Crit Care 2010;14(1):R1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pasero D, Davi A, Guerriero F, Rana N, Merigo G, Mastromauro I, et al. High tidal volume as an independent risk factor for acute lung injury after cardiac surgery. Intensive Care Med 2008;34(Suppl 1):398. [Google Scholar]
- 13.Mascia L, Zavala E, Bosma K, Pasero D, Decaroli D, Andrews P, et al. High tidal volume is associated with the development of acute lung injury after severe brain injury: an international observational study. Crit Care Med 2007;35(8):1815-1820. [DOI] [PubMed] [Google Scholar]
- 14.Fuller BM, Ferguson IT, Mohr NM, Drewry AM, Palmer C, Wessman BT, et al. A quasi-experimental, before-after trial examining the impact of an emergency department mechanical ventilator protocol on clinical outcomes and lung-protective ventilation in acute respiratory distress syndrome. Crit Care Med 2017;45(4):645-652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fernando SM, Fan E, Rochwerg B, Burns KEA, Brochard LJ, Cook DJ, et al. Lung-protective ventilation and associated outcomes and costs among patients receiving invasive mechanical ventilation in the ED. Chest 2021;159(2):606-618. [DOI] [PubMed] [Google Scholar]
- 16.Fuller BM, Mohr NM, Dettmer M, Kennedy S, Cullison K, Bavolek R, et al. Mechanical ventilation and acute lung injury in emergency department patients with severe sepsis and septic shock: an observational study. Acad Emerg Med 2013;20(7):659-669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fuller BM, Mohr NM, Miller CN, Deitchman AR, Levine BJ, Castagno N, et al. Mechanical ventilation and ARDS in the ED: a multi-center, observational, prospective, cross-sectional study. Chest 2015;148(2):365-374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Foley TM, Philpot BA, Davis AS, Swanson MB, Harland KK, Kuhn JD, et al. Implementation of an ED-based bundled mechanical ventilation protocol improves adherence to lung-protective ventilation. Am J Emerg Med 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prekker ME, Donelan C, Ambur S, Driver BE, O'Brien-Lambert A, Hottinger DG, et al. Adoption of low tidal volume ventilation in the emergency department: a quality improvement intervention. Am J Emerg Med 2020;38(4):763-767. [DOI] [PubMed] [Google Scholar]
- 20.Parhar KKS, Stelfox HT, Fiest KM, Rubenfeld GD, Zuege DJ, Knight G, et al. Standardized management for hypoxemic respiratory failure and ARDS: systematic review and meta-analysis. Chest 2020;158(6):2358-2369. [DOI] [PubMed] [Google Scholar]
- 21.Fuller BM. Help for adherence to lung-protective ventilation… for those who will accept it. Chest 2020;158(6):2247-2248. [DOI] [PubMed] [Google Scholar]
- 22.Stoltze AJ, Wong TS, Harland KK, Ahmed A, Fuller BM, Mohr NM. Prehospital tidal volume influences hospital tidal volume: a cohort study. J Crit Care 2015;30(3):495-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Husson EG, Burney CP, Atchinson PR, Roginski MA. Influence of critical care transport ventilator management on ICU care and opportunities for improvement. Air Med Journal 2020;39(4):245-246. [DOI] [PubMed] [Google Scholar]
- 24.Jouffroy R, Saade A, Pegat-Toquet A, Philippe P, Carli P, Vivien B. Pre-hospital mechanical ventilation in septic shock patients. Amer J Emerg Med 2019;37(10):1860-1863. [DOI] [PubMed] [Google Scholar]
- 25.Wilcox SR, Saia MS, Waden H, Frakes M, Wedel SK, Richards JB. Mechanical ventilation in critical care transport. Air Med Journal 2016;35(3):161-165. [DOI] [PubMed] [Google Scholar]
- 26.Wilcox SR, Saia MS, Waden H, Genthon A, Gates JD, Cocchi MN, et al. Improved oxygenation after transport in patients with hypoxemic respiratory failure. Air Med Journal 2015;34(6):369-376. [DOI] [PubMed] [Google Scholar]
- 27.Reimer AP, Hobensack M. Establishing transport statistics: results from the medevac transport statistics survey. Air Med J 2019;38(3):174-177. [DOI] [PubMed] [Google Scholar]
- 28.Kilickaya O, Gajic O. Initial ventilator settings for critically ill patients. Crit Care 2013;17(2):1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maslove DM, Leisman DE. Causal inference from observational data: new guidance from pulmonary, critical care, and sleep journals. Crit Care Med 2019;47(1):1-2. [DOI] [PubMed] [Google Scholar]
- 30.Han S, Martin GS, Maloney JP, Shanholtz C, Barnes KC, Murray S, et al. Short women with severe sepsis-related acute lung injury receive lung-protective ventilation less frequently: an observational cohort study. Crit Care 2011;15(6):R262-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schultz MJ, Karagiannidis C. Is gender inequity in ventilator management a “women's issue”? Eur Resp Journal 2019;54(4):1-4. [DOI] [PubMed] [Google Scholar]
- 32.Dickson RP, Hyzy RC. Short people got no reason: gender, height, and disparities in the management of acute lung injury. Crit Care 2011;15(6):1010-1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kalra SS, Siuba M, Panitchote A, Mireles-Cabodevila E, Chatburn RL, Krishnan S, et al. Higher class of obesity is associated with delivery of higher tidal volumes in subjects with ARDS. Respir Care 2020;65(10):1519-1526. [DOI] [PubMed] [Google Scholar]
- 34.Isenberg DL, Bloom B, Gentile N, Reimer H, Glaze OD, Palumbo P, et al. Males receive low tidal volume component of lung-protective ventilation more frequently than females in the emergency department. West J Emerg Med 2020;21(3):684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peduzzi P, Concato J, Feinstein AR, Holford TR. Importance of events per independent variable in proportional hazards regression analysis II. Accuracy and precision of regression estimates. J Clin Epi 1995;48(12):1503-1510. [DOI] [PubMed] [Google Scholar]
- 36.Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epi 1996;49(12):1373-1379. [DOI] [PubMed] [Google Scholar]
- 37.Dreyfuss D, Soler P, Basset G, Saumon G. High inflation pressure pulmonary edema: respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am Rev Respir Dis 1988;137(5):1159-1164. [DOI] [PubMed] [Google Scholar]
- 38.Webb HH, Tierney DF. Experimental pulmonary edema due to intermittent positive-pressure ventilation with high inflation pressures. Protection by positive end-expiratory pressure. Amer Rev Respir Dis 1974;110(5):556-565. [DOI] [PubMed] [Google Scholar]
- 39.Muscedere J, Mullen J, Gan K, Slutsky A. Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med 1994;149(5):1327-1334. [DOI] [PubMed] [Google Scholar]
- 40.Licker M, Diaper J, Villiger Y, Spiliopoulos A, Licker V, Robert J, et al. Impact of intraoperative lung-protective interventions in patients undergoing lung cancer surgery. Crit Care 2009;13(2):R41-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Michelet P, D’Journo X-B, Roch A, Doddoli C, Marin V, Papazian L, et al. Protective ventilation influences systemic inflammation after esophagectomy: a randomized controlled study. Anesthesiology 2006;105(5):911-919. [DOI] [PubMed] [Google Scholar]
- 42.Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. ; ESICM Trials Group. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 2016;315(8):788-800. [DOI] [PubMed] [Google Scholar]
- 43.Barbosa V, Stratton R, Lafuente E, Elia M. Ulna length to predict height in English and Portuguese patient populations. Eur J Clin Nutr 2012;66(2):209-215. [DOI] [PubMed] [Google Scholar]
- 44.Rivers J, Brown J, Dolphin K, Squire Y. A calibrated measuring tape accurately predicts tidal volumes from ulna length. J Intensive Care Soc 2015;16(4):302-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McNicholas BA, Madotto F, Pham T, Rezoagli E, Masterson CH, Horie S, et al. Demographics, management, and outcome of females and males with acute respiratory distress syndrome in the LUNG SAFE prospective cohort study. Eur Respir J 2019;54(4):1900609. [DOI] [PubMed] [Google Scholar]
- 46.Hager DN, Krishnan JA, Hayden DL, Brower RG; ARDS Clinical Trials Network. Tidal volume reduction in patients with acute lung injury when plateau pressures are not high. Am J Respir Crit Care Med 2005;172(10):1241-1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Villar J, Martín-Rodríguez C, Domínguez-Berrot AM, Fernández L, Ferrando C, Soler JA, et al. A quantile analysis of plateau and driving pressures: effects on mortality in patients with acute respiratory distress syndrome receiving lung-protective ventilation. Crit Care Med 2017;45(5):843-850. [DOI] [PubMed] [Google Scholar]