Background:
During the COVID-19 pandemic, more health care issues were being managed remotely. Urinary tract infections (UTIs) are being managed more often using telehealth although few reports compare the rate of UTI ancillary service orders placed and fulfilled during these visits.
Objectives:
We aimed to evaluate and compare the rate of ancillary service orders and order fulfillments in incident UTI diagnoses between virtual and in-person encounters.
Research Design:
The retrospective cohort study involved 3 integrated health care systems: Kaiser Permanente (KP) Colorado, KP Georgia, and KP Mid-Atlantic States.
Subjects:
We included incident UTI encounters from adult primary care data from January 2019 to June 2021.
Measures:
Data were categorized as: prepandemic (January 2019–March 2020), COVID-19 Era 1 (April 2020–June 2020), and COVID-19 Era 2 (July 2020–June 2021). UTI-specific ancillary services included medication, laboratory, and imaging. Orders and order fulfillments were dichotomized for analyses. Weighted percentages for orders and fulfillments were calculated using inverse probability treatment weighting from logistic regression and compared between virtual and in-person encounters using χ2 tests.
Results:
We identified 123,907 incident encounters. Virtual encounters increased from 13.4% prepandemic to 39.1% in COVID-19 Era 2. Ancillary service orders from virtual encounters were not placed as often as in-person encounters. However, the weighted percentage for ancillary service order fulfillment across all services remained above 65.3% across sites and eras, with many fulfillment percentages above 90%.
Conclusions:
Our study reported a high rate of order fulfillment for both virtual and in-person encounters. Health care systems should encourage providers to place ancillary service orders for uncomplicated diagnoses, such as UTI, to provide enhanced access to patient-centered care.
Key Words: urinary tract infection, virtual care, telehealth, urology, patient-centered care, health care access
Improvements in health care information technology have led to an increase in virtual care, which may encompass a range of phone, video, chat, and email.1,2 Virtual care is convenient for both the patient and health care provider, and is clinically effective across a range of health modalities.3,4 Virtual encounters can maintain continuity of care when in-person encounters are not feasible, result in similar patient satisfaction compared with in-person encounters, can be cost-effective, reduce administrative burden, and improve patient-provider communication.5–9 Specifically, in primary care virtual care’s acceptance is growing among patients and health care providers especially for commonly diagnosed and uncomplicated infections.10–13
Urinary tract infections (UTIs) are one of the most common bacterial infections that result in >10 million outpatient encounters each year14 with >50% of women experiencing a UTI in their lifetime.15,16 Often, UTIs can be diagnosed based on patient history, patient-reported symptoms, and generally without the need of a urine culture.17,18 In addition, patients prone to UTIs can usually safely identify UTI symptoms and initiate treatment themselves.19,20 Based on the common occurrence and uncomplicated nature of diagnosing most UTIs, remote monitoring and treatment of UTIs may be appropriate and acceptable for most patients.21–23
While the acceptability to use virtual care was increasing before the onset of COVID-19, the COVID-19 pandemic and the Centers for Disease Control and Prevention’s (CDC) encouragement to use virtual care services to deliver care24 significantly increased virtual care utilization.10,25 While reports show virtual encounters increased, and at times were higher than in-person encounters from 2020 to 2021, the impact of virtual encounters on ancillary services orders and order fulfillments, such as orders for medications or laboratory tests, are still poorly understood. Given the acceptability of using virtual care for diagnosing and treating of UTIs,22,23,26 our study aimed to evaluate and compare the rate of ancillary service orders and order fulfillments in incident UTI diagnoses between virtual and in-person encounters.
METHODS
Setting
Our multisite study involved 3 integrated health care systems: Kaiser Permanente (KP) Colorado (KPCO), KP Georgia (KPGA), and KP Mid-Atlantic States (KPMAS). Each of these KP regions is nonhospital based (is not affiliated with a KP-owned hospital) and follows KP’s integrated health care model. As of early 2020, KPCO served >575,000 (86% White race, 4% Black or African-American race, and 16% Hispanic ethnicity) in the Boulder and Denver Colorado area, KPGA served >300,000 members (43% White race, 50% Black or African-American race, and 5% Hispanic ethnicity) in the Atlanta-metropolitan area; and KPMAS served >750,000 members (36% White race, 39% Black or African-American race, and 15% Hispanic ethnicity) in the Baltimore-Washington DC, tri-state area.
Before 2019 and the COVID-19 pandemic, all 3 KP sites were utilizing virtual care. KPCO implemented scheduled telephone encounters and synchronous chat, and KPGA and KPMAS both implemented scheduled telephone and video encounters. In March 2020 at the onset of the COVID-19 pandemic, the CDC encouraged all health care systems to utilize virtual care for health care encounters and 8 KP regions, including KPCO, KPGA, and KPMAS transitioned to a “Virtual First” ambulatory care model.24 The transition of “Virtual First” and the need to enhance KP’s virtual platform was a national and regionally led effort that provided all regions the ability and resources to increase telehealth availability to their members.
Study Design and Data Sources
The retrospective cohort study was conducted using data across KPCO, KPGA, and KPMAS from January 2019 to June 2021. To account for the pandemic-induced rapid shift in virtual care and KP’s “Virtual First” approach, we categorized the January 2019–June 2021 period in to 3 eras: Prepandemic (January 2019–March 2020), COVID-19 Era 1 (April 2020–June 2020), and COVID-19 Era 2 (July 2020–June 2021). These eras were chosen as whole months to best represent the availability and level of access to care and services during the COVID-19 pandemic. Prepandemic time period reflects the level of access KP members had before to any COVID-19 considerations were necessary. COVID-19 Era 1 represents the first 3 months that many health care clinics and businesses had significantly limited in-person interactions, and broad “stay at home” mandates were implemented in each of the 3 regions. COVID-19 Era 2 represents the time period when clinics and businesses were beginning to re-open. Data sources included the electronic health records and the Virtual Data Warehouse for each site.27,28 We included all adult primary care (APC) encounters that were completed with a medical doctor. Nurse only visits were excluded from analyses. APC encounters that were procedure-only, or had a nonvirtual modality comparison (such as a blood pressure follow-up assessment or wellness visit) were excluded from the retrospective cohort. We developed a common data model to identify APC encounters with a primary qualifying International Classification of Diseases, 10th Revision (ICD-10) diagnosis for UTI, and the UTI-specific ancillary services, separately, at all 3 sites. We excluded any UTI-based encounter if that member completed an encounter for the same condition within 30 days prior. The study was reviewed and approved by the Institutional Review Board (IRB) at KPGA, the IRB of record for the project.
Variables
Our primary outcomes were ancillary service orders and order fulfillments. UTI-specific ancillary services included any UTI-antibiotic, UTI-second-line antibiotic, urine culture, urine analysis, or computed tomography/magnetic resonance imaging (CT/MRI). An order for an ancillary service was identified if it was placed within 5 days of the incident UTI encounter. Ancillary service order fulfillment was affirmed if the order was completed by the patient within 30 days. Orders and order fulfillments were dichotomized (yes/no) for analyses.
The primary exposure variable was encounter modality, dichotomized as either virtual or in-person encounter. Scheduled telephone encounters, scheduled video encounters, and synchronous chat were classified as a virtual encounter for KPCO and KPGA, and scheduled telephone encounters and scheduled video encounters were classified as a virtual encounter for KPMAS. All other APC encounters included in the cohort were classified as in-person encounters.
Patient-level covariates included were age at the time of encounter, sex, race and Hispanic ethnicity, Charlson Comorbidity Index,29,30 encounter year, encounter quarter, Area Deprivation Index,31 distance to primary care clinic, health insurance, high-deductible plan (yes/no), and prior use of mail-order prescriptions. Race/ethnicity was categorized across the more populated groups across the KP sites and was defined as Hispanic (yes/no) or Non-Hispanic Black, Non-Hispanic Asian, Non-Hispanic White, Non-Hispanic Other known, and Unknown. The Charlson Comorbidity Index was categorized as no comorbidities, 1 comorbidity, or ≥2 comorbidities with no comorbidities serving as the reference group.
Statistical Analyses
Analyses were conducted for each KP site separately. Figure 1 reports the flow diagram for the final APC UTI cohort for each KP site. Descriptive statistics report the APC UTI encounters by encounter modality. χ2 comparison test compared the frequency of virtual versus in-person encounters for each of the patient covariates within the KP sites. Analyses were focused on comparing virtual versus in-person encounters for ancillary service orders and order fulfillments. Inverse probability treatment weighting (IPTW) was used to weight the virtual and in-person encounters, creating estimates balanced across the 2 groups on each of the patient covariates.32–34 Logistic regression with stabilized average treatment effect without truncation was used to calculate the IPTW. Outcomes were compared between UTI encounters completed virtually and in-person and were weighted by the IPTW to reduce possible confounding due to differences in covariate distributions. Results are presented as weighted percentages of ancillary service orders and order fulfillments for both virtual and in-person encounters. Separate weights were constructed for each outcome. SAS Enterprise Guide, v8.2 was used to conduct all statistical analyses with statistical significance assessed at α=0.05.
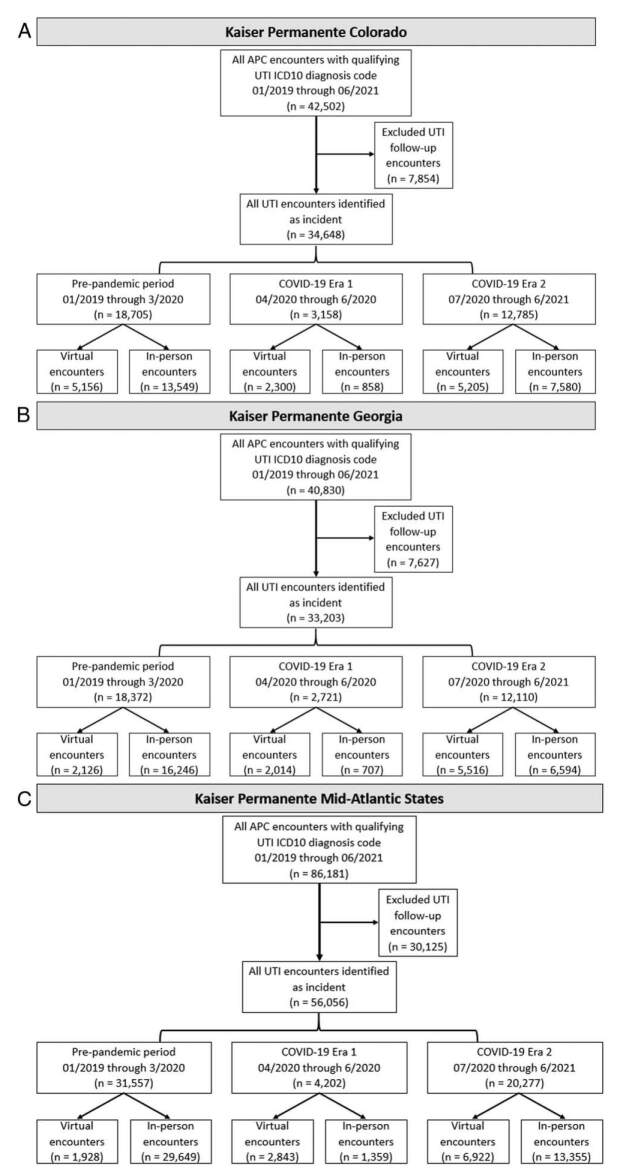
FIGURE 1.
Flow diagram of for each of the three integrated healthcare systems reporting the selection of adult primary care (APC) encounters with an incident urinary tract infection (UTI) diagnosis code. The flow diagrams show the participating healthcare systems: Kaiser Permanente Colorado (A), Kaiser Permanente Georgia (B), and Kaiser Permanente Mid-Atlantic States (C).
RESULTS
Our study and common data model identified 169,513 APC encounters with an ICD-10 UTI diagnosis code (KPCO=42,502; KPGA=40,803; KPMAS=86,181), with 73.1% (n=123,907) being incident UTI encounters (Fig. 1). Within KPCO, we identified 18,705 UTI incident encounters occurring in the prepandemic (January 2019–March 2020) era with 27.6% (n=5156) encounters being virtual, 3158 UTI encounters (72.8% virtual) during COVID-19 Era 1 (April 2020–June 2020), and 12,785 UTI encounters during COVID-19 Era 2 (July 2020–June 2021) with 40.7% (n=5205) completed virtually. KPGA had similar proportions of UTI encounters and virtual encounters completed, as KPCO, across eras. KPMAS had 4202 and 20,277 encounters during COVID-19 Era 1 and Era 2, respectively, with 67.7% and 34.1% being virtual encounters. Across all the KP sites, there were a total of 45,172 UTI incident encounters during the COVID-19 Era 2 (July 2020–June 2021), 39.1% were virtual encounters, an increase from 13.4% during the prepandemic era.
To provide an understanding of the population demographics each site was serving before the COVID-19 pandemic, Table 1 reports the patient characteristics across the 3 KP sites for patients completing a UTI encounter between January 2019 and March 2020 (prepandemic era). In KPCO, a higher percentage of members completing virtual encounters were members age 65 years and older (29%), females (93.6%) and patients within the lowest area deprivation quartile (62.8%). In KPGA members self-reporting as Black (43.2%) or White (43.4%) comprised the majority of virtual encounters for a UTI diagnosis. Males (22.3%) and members with a Charlson Comorbidity Index of 1 (16%) were less likely to complete a virtual encounter compared with individuals with a Charlson Comorbidity Index of 0.
TABLE 1.
Patient Characteristics of Patients Diagnosed With Incident Urinary Tract Infections (UTIs) Before COVID-19 Onset, January 2019–March 2020, Stratified Across Kaiser Permanente (KP) Sites
| KP Colorado | KP Georgia | KP Mid-Atlantic States | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Encounter mode | Encounter mode | Encounter mode | |||||||
| Patient/encounter characteristics at time of encounter | Virtual mode | In-person mode | P | Virtual mode | In-person mode | P | Virtual mode | In-person mode | P |
| No. incident UTI encounters | 5156 | 13,549 | 2126 | 16,246 | 1928 | 29,649 | |||
| Age group (y) | |||||||||
| 19–34 | 1207 (23.4) | 2066 (15.2) | <0.0001 | 482 (22.7) | 3410 (21) | <0.0001 | 256 (13.3) | 6693 (22.6) | <0.0001 |
| 35–49 | 1177 (22.8) | 2132 (15.7) | 645 (30.3) | 3837 (23.6) | 422 (21.9) | 6150 (20.7) | |||
| 50–64 | 1278 (24.8) | 3256 (24) | 614 (28.9) | 4749 (29.2) | 550 (28.5) | 8061 (27.2) | |||
| ≥65 | 1494 (29) | 6095 (45) | 385 (18.1) | 4250 (26.2) | 700 (36.3) | 8745 (29.5) | |||
| Sex | |||||||||
| Female | 4824 (93.6) | 9962 (73.5) | <0.0001 | 1990 (93.6) | 13,214 (81.3) | <0.0001 | 1498 (77.7) | 22,599 (76.2) | 0.1398 |
| Male | 332 (6.4) | 3587 (26.5) | 136 (6.4) | 3032 (18.7) | 430 (22.3) | 7050 (23.8) | |||
| Race/ethnicity | |||||||||
| Hispanic | 911 (17.7) | 2492 (18.4) | <0.0001 | 69 (3.2) | 854 (5.3) | 0.0001 | 273 (14.2) | 5242 (17.7) | <0.0001 |
| Non-Hispanic Black | 160 (3.1) | 556 (4.1) | 918 (43.2) | 7136 (43.9) | 691 (35.8) | 11,822 (39.9) | |||
| Non-Hispanic Asian | 108 (2.1) | 402 (3) | 72 (3.4) | 702 (4.3) | 212 (11) | 2846 (9.6) | |||
| Non-Hispanic White | 3704 (71.8) | 9323 (68.8) | 922 (43.4) | 6475 (39.9) | 651 (33.8) | 8416 (28.4) | |||
| Non-Hispanic Other known | 173 (3.4) | 485 (3.6) | 17 (0.8) | 111 (0.7) | 90 (4.7) | 1208 (4.1) | |||
| Unknown | 100 (1.9) | 291 (2.1) | 128 (6) | 968 (6) | 11 (0.6) | 115 (0.4) | |||
| Charlson Comorbidity classes | |||||||||
| 0 (none) | 3310 (64.2) | 6961 (51.4) | <0.0001 | 1544 (72.6) | 9870 (60.8) | <0.0001 | 1084 (56.2) | 18,260 (61.6) | <0.0001 |
| 1 | 872 (16.9) | 2264 (16.7) | 307 (14.4) | 2637 (16.2) | 308 (16) | 4587 (15.5) | |||
| ≥2 | 974 (18.9) | 4324 (31.9) | 275 (12.9) | 3739 (23) | 536 (27.8) | 6802 (22.9) | |||
| Area Disadvantage Index | |||||||||
| Lowest quartile | 3236 (62.8) | 7677 (56.7) | <0.0001 | 586 (27.6) | 4095 (25.2) | 0.0039 | 1073 (55.7) | 14,678 (49.5) | <0.0001 |
| Lower mid-quartile | 1686 (32.7) | 5096 (37.6) | 770 (36.2) | 5618 (34.6) | 455 (23.6) | 8214 (27.7) | |||
| Upper mid-quartile | 178 (3.5) | 574 (4.2) | 476 (22.4) | 3975 (24.5) | 253 (13.1) | 4354 (14.7) | |||
| Highest quartile | 56 (1.1) | 202 (1.5) | 294 (13.8) | 2558 (15.7) | 147 (7.6) | 2403 (8.1) | |||
When assessing the weighted percentages of virtual encounters completed for each of the ancillary service orders across eras, KPCO and KPGA experienced a significant decrease in virtual encounters between the prepandemic and COVID-19 Era 1 for urine cultures (KPCO: prepandemic=31.9%, Era 1=25.4%, P<0.001; KPGA: prepandemic=43.0%, Era 1=25.5%, P<0.001) and second-line antibiotics (KPCO: prepandemic=36.2%, Era 1=30.6%, P<0.001; KPGA: prepandemic=19.2%, Era 1=11.0%, P<0.001). KPMAS saw an increase in urine cultures (prepandemic=17.7%, Era 1=24.6%, P<0.001) and any antibiotic (prepandemic=21.3%, Era 1=25.8%, P=0.0004) during the same eras (Table 2). Comparing the COVID-19 Era 1 (April 2020–June 2020) and Era 2 (July 2020–June 2021) for KPCO and KPGA for any antibiotic, there were no statistical significant difference in service orders during a virtual encounter (KPCO, P=0.4108; KPGA, P=0.9482), while KPMAS experienced a decrease in these orders during COVID-19 Era 2 (Era 1=25.7%, Era 2=21.3%, P<0.001).
TABLE 2.
Comparison of Ancillary Services Orders by Service Class and by Era (Prepandemic, COVID-19 Era 1, and COVID-19 Era 2) for All Virtual, Urinary Tract Infection–related Encounters Across 3 Integrated Health Care Systems Accounting for the Inverse Probability Treatment Weights by Era
| Percent of encounters with an ancillary service order | ||||||
|---|---|---|---|---|---|---|
| Integrated health care system | Era comparisons | Any antibiotic | Second-line antibiotic | Urine culture | Urine analysis | CT/MRI |
| Kaiser Permanente Colorado | Prepandemic (January 2019–March 2020) | 38.6% | 36.2% | 31.9% | 45.8% | 2.7% |
| COVID-19 Era 1 (April 2020–June 2020) | 35.6% | 30.6% | 25.4% | 39.3% | 4.7% | |
| P | 0.0118 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |
| COVID-19 Era 1 (April 2020–June 2020) | 35.0% | 29.8% | 25.0% | 39.4% | 5.6% | |
| COVID-19 Era 2 (July 2020–June 2021) | 34.1% | 29.5% | 23.1% | 35.7% | 5.7% | |
| P | 0.4108 | 0.7878 | 0.0808 | 0.0019 | 0.7846 | |
| Kaiser Permanente Georgia | Prepandemic (January 2019–March 2020) | 28.3% | 19.2% | 43.0% | 42.6% | 2.5% |
| COVID-19 Era 1 (April 2020–June 2020) | 26.0% | 11.0% | 25.5% | 31.2% | 2.5% | |
| P | 0.0839 | <0.0001 | <0.0001 | <0.0001 | 0.9054 | |
| COVID-19 Era 1 (April 2020–June 2020) | 25.7% | 11.1% | 25.5% | 31.6% | 2.7% | |
| COVID-19 Era 2 (July 2020–June 2021) | 25.6% | 12.7% | 32.4% | 37.1% | 2.9% | |
| P | 0.9482 | 0.053 | <0.0001 | <0.0001 | 0.5541 | |
| Kaiser Permanente Mid-Atlantic States | Prepandemic (January 2019–March 2020) | 21.3% | 6.2% | 17.1% | 35.2% | 8.2% |
| COVID-19 Era 1 (April 2020–June 2020) | 25.8% | 5.8% | 24.6% | 46.6% | 5.9% | |
| P | 0.0004 | 0.5908 | <0.0001 | <0.0001 | 0.0021 | |
| COVID-19 Era 1 (April 2020–June 2020) | 25.7% | 5.7% | 24.8% | 47.1% | 6.1% | |
| COVID-19 Era 2 (July 2020–June 2021) | 21.3% | 6.6% | 26.2% | 53.7% | 8.9% | |
| P | <0.0001 | 0.0976 | 0.1524 | <0.0001 | <0.0001 | |
CT/MRI indicates computed tomography/magnetic resonance imaging.
Order fulfillment weighted percentages for all virtual UTI-related encounters remained above 65% for all ancillary services, across eras and KP sites (Table 3). In KPGA, during the Era 2 (July 2020–June 2021), order fulfillment rate was 91.1%, 90.4%, 93.4%, 91.2%, and 70.8% for any antibiotic, second-line antibiotics, urine culture, urine analysis, and CT/MRI, respectively. This pattern during the COVID-19 Era 2 was similar for KPCO and KPMAS. KPMAS maintained an order fulfillment above 90% for COVID-19 Era 1 and Era 2 for any antibiotic, second-line antibiotics, and urine cultures.
TABLE 3.
Comparison of Ancillary Services Order Fulfillments by Service Class and by Era (Prepandemic, COVID-19 Era 1, and COVID-19 Era 2) for All Virtual, Urinary Tract Infection–related Encounters Across 3 Integrated Health Care Systems Accounting for the Inverse Probability Treatment Weights by Era
| Percent of encounters with an ancillary service order fulfillment | ||||||
|---|---|---|---|---|---|---|
| Integrated health care system | Era comparisons | Any antibiotic | Second-line antibiotic | Urine culture | Urine analysis | CT/MRI |
| Kaiser Permanente Colorado | Prepandemic (January 2019–March 2020) | 92.1% | 92.3% | 99.1% | 87.2% | 71.1% |
| COVID-19 Era 1 (April 2020–June 2020) | 91.0% | 90.8% | 98.8% | 82.5% | 75.8% | |
| P | 0.3186 | 0.1955 | 0.5609 | 0.0005 | 0.3953 | |
| COVID-19 Era 1 (April 2020–June 2020) | 91.1% | 90.9% | 98.5% | 82.7% | 76.3% | |
| COVID-19 Era 2 (July 2020–June 2021) | 87.9% | 87.4% | 98.0% | 86.3% | 70.8% | |
| P | 0.016 | 0.0157 | 0.5144 | 0.0126 | 0.2267 | |
| Kaiser Permanente Georgia | Prepandemic (January 2019–March 2020) | 88.6% | 90.2% | 71.2% | 66.9% | 79.6% |
| COVID-19 Era 1 (April 2020–June 2020) | 85.3% | 86.6% | 93.7% | 88.8% | 67.7% | |
| P | 0.0921 | 0.1433 | <0.0001 | <0.0001 | 0.1533 | |
| COVID-19 Era 1 (April 2020–June 2020) | 85.5% | 86.3% | 94.0% | 89.3% | 65.0% | |
| COVID-19 Era 2 (July 2020–June 2021) | 91.1% | 90.4% | 93.4% | 91.2% | 70.8% | |
| P | 0.0003 | 0.0736 | 0.6495 | 0.13 | 0.3958 | |
| Kaiser Permanente Mid-Atlantic States | Prepandemic (January 2019–March 2020) | 92.5% | 90.2% | 94.4% | 72.9% | 83.7% |
| COVID-19 Era 1 (April 2020–June 2020) | 93.0% | 92.2% | 94.2% | 81.2% | 83.2% | |
| P | 0.758 | 0.5449 | 0.9021 | <0.0001 | 0.9166 | |
| COVID-19 Era 1 (April 2020–June 2020) | 92.9% | 92.3% | 94.4% | 81.0% | 82.6% | |
| COVID-19 Era 2 (July 2020–June 2021) | 91.3% | 90.1% | 95.2% | 82.0% | 84.4% | |
| P | 0.1936 | 0.3834 | 0.4221 | 0.4051 | 0.5522 | |
CT/MRI indicates computed tomography/magnetic resonance imaging.
The weighted percentage of ancillary service orders and order fulfillments comparing prepandemic and COVID-19 Era 2 (July 2020–June 2021) for KPCO, KPGA, and KPMAS are reported in Table 4. The weighted percentage of UTI encounters with any antibiotic order decreased between the prepandemic and Era 2 in KPCO for virtual encounters (prepandemic=38.2%, Era 2=34.9%, P<0.05), while any antibiotic order increased for in-person UTI encounters (prepandemic=37.8%, Era 2=41.2%, P<0.005). The percentage of ancillary service orders placed during a virtual encounter remained lower than the percentage of orders placed during an in-person encounter, regardless of service or era. However, the percentage for order fulfillments remained above 65.4% for all ancillary services, across sites and eras. Any antibiotic order fulfillment in KPCO remained above 83% for both virtual and in-person UTI encounters in the prepandemic era and COVID-19 Era 2. In the COVID-19 Era 2, KPGA order fulfillments associated with a virtual encounter were between 90.0%-93.2% for any antibiotic, second-line antibiotic, urine culture, and urine analysis. KPMAS increased their urine analysis and CT/MRI orders and order fulfillments between prepandemic era and Era 2, regardless of encounter modality.
TABLE 4.
Comparison of Prepandemic (January 2019–March 2020) and COVID-19 Era 2 (July 2020–June 2021) Weighted Percentages for Ancillary Service Orders and Ancillary Service Order Fulfillments Across Virtual and In-person Encounters for Each 3 Integrated Health Care Systems
| Kaiser Permanente Colorado | Kaiser Permanente Georgia | Kaiser Permanente Mid-Atlantic States | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Virtual | In-person | Virtual | In-person | Virtual | In-person | |||||||
| Ancillary service | Prepandemic | COVID-19 Era 2 | Prepandemic | COVID-19 Era 2 | Prepandemic | COVID-19 Era 2 | Prepandemic | COVID-19 Era 2 | Prepandemic | COVID-19 Era 2 | Prepandemic | COVID-19 Era 2 |
| Any antibiotic | ||||||||||||
| Order | 38.20% | 34.90% | 37.80% | 41.20% | 28.30% | 25.90% | 37.10% | 40.00% | 21.20% | 21.40% | 36.20% | 39.70% |
| Order fulfillment | 92.00% | 87.60% | 95.40% | 95.40% | 88.70% | 91.10% | 83.30% | 81.10% | 92.40% | 91.30% | 90.50% | 85.20% |
| Second-line antibiotic | ||||||||||||
| Order | 35.80% | 30.50% | 31.80% | 34.20% | 19.10% | 13.00% | 17.30% | 25.00% | 6.20% | 6.70% | 17.70% | 25.20% |
| Order fulfillment | 92.20% | 87.10% | 95.00% | 94.70% | 90.30% | 90.10% | 65.40% | 69.00% | 91.50% | 90.20% | 80.30% | 72.70% |
| Urine culture | ||||||||||||
| Order | 31.50% | 23.20% | 57.30% | 56.00% | 42.70% | 32.80% | 62.00% | 63.20% | 16.90% | 26.20% | 52.90% | 60.20% |
| Order fulfillment | 99.10% | 98.00% | 99.70% | 99.50% | 71.40% | 93.20% | 99.40% | 99.50% | 94.20% | 95.20% | 99.00% | 99.00% |
| Urine analysis | ||||||||||||
| Order | 45.80% | 35.30% | 74.20% | 71.90% | 42.50% | 37.10% | 89.00% | 90.70% | 35.20% | 53.50% | 71.60% | 82.60% |
| Order fulfillment | 86.90% | 86.50% | 97.10% | 96.90% | 67.50% | 91.00% | 99.00% | 99.40% | 72.80% | 82.10% | 97.10% | 98.00% |
| CT/MRI | ||||||||||||
| Order | 2.90% | 5.00% | 16.40% | 18.50% | 2.60% | 2.80% | 13.50% | 16.90% | 8.30% | 8.90% | 16.70% | 23.60% |
| Order fulfillment | 73.30% | 70.70% | 78.40% | 82.30% | 79.30% | 70.60% | 86.00% | 91.30% | 83.50% | 84.50% | 94.70% | 96.20% |
Bold text represents a statistical significant difference between prepandemic (January 2019–March 2020) and COVID-19 Era 2 (July 2020–June 2021) with α=0.05.
CT/MRI indicates computed tomography/magnetic resonance imaging.
DISCUSSION
To our knowledge, our study is the first multisite study utilizing 3 integrated health care system databases to compare ancillary service orders and order fulfillments between virtual and in-person encounters. Our study found the percent of virtual UTI encounters increased from 13.4% prepandemic (January 2019–March 2020) to 39.1% during the COVID-19 Era 2 (July 2020–June 2021). Our assessment of ancillary service orders found that orders associated with a virtual UTI encounter were not placed as often as those associated with in-person encounters. However, the weighted percentage for ancillary service order fulfillment across all services remained above 65.4% across KP sites and eras, with many order fulfillment percentages above 90%.
Virtual care has been shown to improve access to care for patients,25,35,36 and lower administrative costs and burdens for health care systems while maintaining patient and provider satisfaction.5–9,37–40 Virtual care is becoming more acceptable in APC settings, especially for treating noncomplicated conditions such as UTIs.21–23,41,42 A systematic review of virtual care in urology reported 5 retrospective studies that assessed using virtual care to manage UTIs.42 Blozik et al22 reported virtual care as an effective and safe modality to manage uncomplicated UTIs with a 92% reduction of UTI symptoms after a virtual consultation, and the remaining 8% were referred to an in-person encounter. The finding of virtual care being effective and safe is echoed by a recent report stating the increased utilization of virtual care from 2008 to 2017 to diagnosis and treat UTIs.23
Despite the growing evidence of virtual care being an acceptable, safe, and effective way to manage members with UTIs, there are few reports on ancillary service orders and order fulfillments resulting from virtual encounters.26,43,44 Rastogi et al26 reported on UTI management in a large nationwide, direct-to-consumer virtual care platform with >20,000 adults in the cohort. The authors report 94% of UTI patients getting direct-to-consumer virtual care received an antibiotic, which is higher than the Schoenfield et al44 report that showed clinicians associated with a direct-to-consumer virtual care company were performing below adherence guidelines. However, a study comparing virtual care and office visits across 4 APC practices found that while an oral antibiotic was prescribed to 99% patients diagnosed with a UTI during a virtual encounter versus 49% of patients diagnosed during an in-person encounter, physicians only ordered a urine culture for 7% of the virtual care UTI patients versus 31% of the in-person UTI encounters.43 None of these studies, though, compared UTI management between virtual and in-person encounters across 3 large integrated health care systems with a focus on ancillary service orders and order fulfillment.
Our study built upon existing literature by comparing ancillary service order fulfillments across 3 KP sites. Our multisite study found similar results of ancillary service order patterns that Mehrotra et al43 reported when comparing urine culture orders between virtual and in-person encounters. Overall, the weighted percentage of UTI virtual encounters with an ancillary service order remained below 54%, while the order fulfillment for virtual encounters remained above 65%. Our findings show that while health care providers may be hesitant to place an order for an UTI ancillary service (such as urine culture, or antibiotic prescription), patients are not hesitant to fill or complete these orders. There is a growing body of evidence reporting high patient and health care provider satisfaction with virtual care, especially since the onset of the COVID-19 pandemic.5,40 health care systems should continue to promote virtual care and encourage their health care providers to place ancillary service orders when necessary. Health care providers should feel confident that, despite an encounter taking place using a virtual modality, the patient will likely fill or complete these orders.
The study is not without limitations. First, our analyses were conducted across 3 KP sites: KPCO, KPGA, and KPMAS. While our sample is geographically and demographically diverse, each member has some level of insurance coverage and this may reduce the generalizability of our findings. Second, KP’s virtual care platform was already established before the COVID-19 pandemic and KP’s ability to rapidly shift a large percentage of health care encounters to a virtual modality may not be easily replicated across other health care systems, limiting the ability of patients to schedule virtual encounters and health care providers to place service orders during a virtual encounter. Future studies should replicate these analyses in different health care systems with a variety of virtual care integration to determine the applicability of UTI management using virtual encounters. Third, most the cohort resided in neighborhoods with low area deprivation and our findings may not be as applicable to patients living in high area deprivation neighborhoods. However, recent public policy to promote and build infrastructure to bring reliable, high-speed broadband to >35% of rural Americans, may help improve access to virtual care services for all neighborhoods.45 Fourth, our analyses were limited to the initial APC encounter for UTI and did not include follow-up visits. While our analyses accounted for the volume of initial UTI visits, we do not account for follow-up visits that may be needed to fully resolve the UTI diagnosis. Future studies should include UTI encounters and any follow-up encounters that occur within 30 days of initial appointment to determine the effectiveness of UTI management using telehealth. Fifth, our analyses were limited to January 2019 through June 2021; as the COVID-19 pandemic continued past June 2021 our study may have missed practice variation during the 2012 and 2022 COVID-19 surges. Future studies should expand the analyses to encompass recent data to determine if the ancillary service order and order fulfillment patterns changed. Sixth, IPTW can only address observed between group differences and is not able to assess unobserved and unmeasured factors, such a patient preference, and may lead to unobserved response bias. Future studies could collect information that is typically unobserved in an administrative database (patient preference, likelihood to repeat telehealth visit, satisfaction) and assess group differences among these factors.
CONCLUSIONS
Virtual care is becoming more widely accepted by patients and health care providers, while maintaining effectiveness and safety, especially for uncomplicated diagnoses such as an UTI. Our study showed the increase utilization of virtual encounters for UTI management across 3 integrated health care systems from January 2019 through June 2021. We found that although UTI ancillary service orders were placed less often during virtual encounters compared with in-person encounters, patient order fulfillment remained high across all UTI ancillary services regardless of encounter modality. Health care systems should continue to expand their virtual care platform while encouraging their health care providers to place ancillary service orders to ensure complete, patient-centered care.
Footnotes
The authors declare no conflict of interest.
Contributor Information
Jennifer C. Gander, Email: jennifer.c.gander@kp.org.
Glenn Goodrich, Email: Glenn.K.Goodrich@kp.org.
Bennet McDonald, Email: Bennett.X.McDonald@kp.org.
Courtney E. McCracken, Email: Courtney.E.McCracken@kp.org.
Heather M. Tavel, Email: Heather.M.Tavel@kp.org.
Teaniese L. Davis, Email: Teaniese.L.Davis@kp.org.
Nancy S. Weinfield, Email: Nancy.S.Weinfield@kp.org.
Debra P. Ritzwoller, Email: Debra.Ritzwoller@kp.org.
Douglas W. Roblin, Email: Douglas.W.Roblin@kp.org.
REFERENCES
- 1.Gajarawala SN, Pelkowski JN. Telehealth benefits and barriers. J Nurse Pract. 2021;17:218–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balestra M. Telehealth and legal implications for nurse practitioners. J Nurse Pract. 2018;14:33–39. [DOI] [PubMed] [Google Scholar]
- 3.Snoswell CL, Chelberg G, De Guzman KR, et al. The clinical effectiveness of telehealth: a systematic review of meta-analyses from 2010 to 2019. J Telemed Telecare. 2021:1357633X211022907. doi: 10.1177/1357633X211022907. https://pubmed.ncbi.nlm.nih.gov/34184580/ [DOI] [PubMed] [Google Scholar]
- 4.Snoswell CL, Taylor ML, Comans TA, et al. Determining if telehealth can reduce health system costs: scoping review. J Med Internet Res. 2020;22:e17298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang JE, Lai AY, Gupta A, et al. Rapid transition to telehealth and the digital divide: implications for primary care access and equity in a post‐COVID era. Milbank Q. 2021;99:340–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dhaliwal JK, Hall TD, LaRue JL, et al. Expansion of telehealth in primary care during the COVID-19 pandemic: benefits and barriers. J Am Assoc Nurse Pract. 2022;34:224–229. [DOI] [PubMed] [Google Scholar]
- 7.Greenhalgh T, Vijayaraghavan S, Wherton J, et al. Virtual online consultations: advantages and limitations (VOCAL) study. BMJ Open. 2016;6:e009388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McKinstry B, Hammersley V, Burton C, et al. The quality, safety and content of telephone and face-to-face consultations: a comparative study. Qual Saf Health Care. 2010;19:298–303. [DOI] [PubMed] [Google Scholar]
- 9.Kruse CS, Krowski N, Rodriguez B, et al. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7:e016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koonin LM, Hoots B, Tsang CA, et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic—United States, January–March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Demeke HB, Merali S, Marks S, et al. Trends in use of telehealth among health centers during the COVID-19 pandemic—United States, June 26–November 6, 2020. MMWR Morb Mortal Wkly Rep. 2021;70:240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karimi M, Lee EC, Couture SJ, et al. National Survey Trends in Telehealth Use in 2021: disparities in utilization and audio vs. video services. 2022. https://aspe.hhs.gov/sites/default/files/documents/4e1853c0b4885112b2994680a58af9ed/telehealth-hps-ib.pdf. [Google Scholar]
- 13.Bleyel C, Hoffmann M, Wensing M, et al. Patients’ perspective on mental health specialist video consultations in primary care: qualitative preimplementation study of anticipated benefits and barriers. J Med Internet Res. 2020;22:e17330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schappert SM, Rechtsteiner EA. Ambulatory medical care utilization estimates for 2007. Vital Health Stat 13. 2011;169:1–38. [PubMed] [Google Scholar]
- 15.Griebling TL. Urologic diseases in America project: trends in resource use for urinary tract infections in women. J Urol. 2005;173:1281–1287. [DOI] [PubMed] [Google Scholar]
- 16.Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med. 2002;113:5–13. [DOI] [PubMed] [Google Scholar]
- 17.Bent S, Saint S. The optimal use of diagnostic testing in women with acute uncomplicated cystitis. Am J Med. 2002;113:20–28. [DOI] [PubMed] [Google Scholar]
- 18.Little P, Moore M, Turner S, et al. Effectiveness of five different approaches in management of urinary tract infection: randomised controlled trial. BMJ. 2010;340:c199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gupta K, Hooton TM, Roberts PL, et al. Patient-initiated treatment of uncomplicated recurrent urinary tract infections in young women. Ann Intern Med. 2001;135:9–16. [DOI] [PubMed] [Google Scholar]
- 20.Glover M, Moreira CG, Sperandio V, et al. Recurrent urinary tract infections in healthy and nonpregnant women. Urol Sci. 2014;25:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barry HC, Hickner J, Ebell MH, et al. A randomized controlled trial of telephone management of suspected urinary tract infections in women. J Fam Pract. 2001;50:589–589. [PubMed] [Google Scholar]
- 22.Blozik E, Sommer-Meyer C, Cerezo M, et al. Effectiveness and safety of telemedical management in uncomplicated urinary tract infections. J Telemed Telecare. 2011;17:78–82. [DOI] [PubMed] [Google Scholar]
- 23.Bruxvoort KJ, Bider-Canfield Z, Casey JA, et al. Outpatient urinary tract infections in an era of virtual healthcare: trends from 2008 to 2017. Clin Infect Dis. 2020;71:100–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Using Telehealth Services. 2020. https://www.cdc.gov/phlp/publications/topic/telehealth.html
- 25.Qian L, Sy LS, Hong V, et al. Disparities in outpatient and telehealth visits during the COVID-19 pandemic in a large integrated health care organization: retrospective cohort study. J Med Internet Res. 2021;23:e29959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rastogi R, Martinez KA, Gupta N, et al. Management of urinary tract infections in direct to consumer telemedicine. J Gen Intern Med. 2020;35:643–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holmes JH, Elliott TE, Brown JS, et al. Clinical research data warehouse governance for distributed research networks in the USA: a systematic review of the literature. J Am Med Inform Assoc. 2014;21:730–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ross TR, Ng D, Brown JS, et al. The HMO Research Network Virtual Data Warehouse: a public data model to support collaboration. EGEMS (Wash DC). 2014;2:1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–1251. [DOI] [PubMed] [Google Scholar]
- 30.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 31.Knighton AJ, Savitz L, Belnap T, et al. Introduction of an area deprivation index measuring patient socioeconomic status in an integrated health system: implications for population health. EGEMS. 2016;4:1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34:3661–3679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rosenbaum PR. Model-based direct adjustment. J Am Stat Assoc. 1987;82:387–394. [Google Scholar]
- 34.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 35.Neeman E, Kolevska T, Reed M, et al. Cancer care telehealth utilization ratesand provider attitudes in the wake of the novelcoronavirus pandemic: The Kaiser Permanente Northern California experience. Clin Cancer Res. 2020;26:S06-03. [Google Scholar]
- 36.Bernstein P, Ko KJ, Israni J, et al. Urgent and non-emergent telehealth care for seniors: findings from a multi-site impact study. J Telemed Telecare. 2021;171:1357633X211004321. [DOI] [PubMed] [Google Scholar]
- 37.Polinski JM, Barker T, Gagliano N, et al. Patients’ satisfaction with and preference for telehealth visits. J Gen Intern Med. 2016;31:269–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reed ME, Huang J, Parikh R, et al. Patient-provider video telemedicine integrated with clinical care: patient experiences. Ann Intern Med. 2019;171:222–224. [DOI] [PubMed] [Google Scholar]
- 39.Reed ME, Parikh R, Huang J, et al. Real-time patient-provider video telemedicine integrated with clinical care. N Engl J Med. 2018;379:1478–1479. [DOI] [PubMed] [Google Scholar]
- 40.Andrews E, Berghofer K, Long J, et al. Satisfaction with the use of telehealth during COVID-19: an integrative review. Int J Nurs Stud Adv. 2020;2:100008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Andino JJ, Lingaya M-A, Daignault-Newton S, et al. Video visits as a substitute for urological clinic visits. Urology. 2020;144:46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Novara G, Checcucci E, Crestani A, et al. Telehealth in urology: a systematic review of the literature. How much can telemedicine be useful during and after the COVID-19 pandemic? Eur Urol. 2020;78:786–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mehrotra A, Paone S, Martich GD, et al. A comparison of care at e-visits and physician office visits for sinusitis and urinary tract infection. JAMA Intern Med. 2013;173:72–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schoenfeld AJ, Davies JM, Marafino BJ, et al. Variation in quality of urgent health care provided during commercial virtual visits. JAMA Intern Med. 2016;176:635–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.The White House. FACT SHEET: The American Jobs Plan. 2021.