Abstract
Purpose
Resilience is viewed as an individual’ positive adaptation and experiences of adversity. The maintenance and recovery of mental health in people with mental disorder is considered a sign of coping with adverse conditions. The purpose of the present meta-analysis was to examine the association between resilience and quality of life in individuals with mental disorders.
Methods
Studies were included if research reported measures of association with resilience, as assessed using self-reported resilience scale and quality of life. A systematic literature search was conducted in PubMed and PsycINFO.
Results
Eight studies involving a total of 1439 patients were included in the meta-analysis. Assuming a random-effects model, the weighted mean Pearson correlation between resilience and quality of life was r = 0.551 (95% confidence interval [0.370; 0.691], p < 0.001). This association was moderate, although the heterogeneity among individual effect sizes was substantial (I2 = 93.35%).
Conclusion
Despite substantial heterogeneity across included studies, the findings suggest a strong association between resilience and quality of life in people with mental disorders. In clinical practice, the promotion of resilience is important to enhance the quality of life among people with mental illness.
Keywords: resilience, quality of life, mental health
Introduction
In recent years, the concept of resilience has increased importance in the field of mental illness as the process of adapting positively to an adversity such as illness.1 In this context, resilience is defined as having the potential or the capacity to maintain or regain mental health or in the context of significant challenges, trauma or adversity. Mental illness commonly indicated that patients with depression and/or anxiety disorders may suffer significantly with a state of failed or lower levels of resilience compared to non-affected participants.2,3 Moreover, further studies suggested that high resilience reduced the risk of suicide in participants with schizophrenia and mood disorders, and had a positive impact on the long-term recovery in schizophrenia.4–7 A study found that lower levels of resilience were associated with an increased number of depressive episodes and higher levels of impulsivity in participants with bipolar disorder.8 Resilience is a dynamic and time-specific process and may vary throughout life.9–13 Resilience plays an important role in the prevention and recovery of psychiatric disorders;14,15, thus, there is a need to examine resilience in people with mental illness.
Quality of life is a broad construct developed to evaluate health status, perceived levels of general well-being and satisfaction in the context of a specific health condition or life as a whole.14 The improvement and maintenance of quality of life were relevant predictors for remission and recovery in people with schizophrenia.15–17 Past studies have shown that a higher level of resilience is correlated with better quality of life in individuals with mental illness.18–20 Other studies found resilience and quality of life to be lower among participants with bipolar disorder compared to the healthy control group.21,22 Hayas and colleagues (2015)13 found that resilience contributed to helping individuals cope positively with illness and promote better quality of life and improve recovery. Resilience was related to the factors with high levels of quality of life, including spirituality and purpose of life.3 Therefore, improving quality of life has been an important outcome for health-related interventions and positive impact on depression, well-being and psychosocial functioning.23,24
The present review examined the resilience and quality of life among people with mental illness. The relationship between resilience and quality of life are acquired and assessed. The goal of this review is to collect data that can help health professionals promote or improve resilience and quality of life in people with mental illness.
Methods
Search Strategy
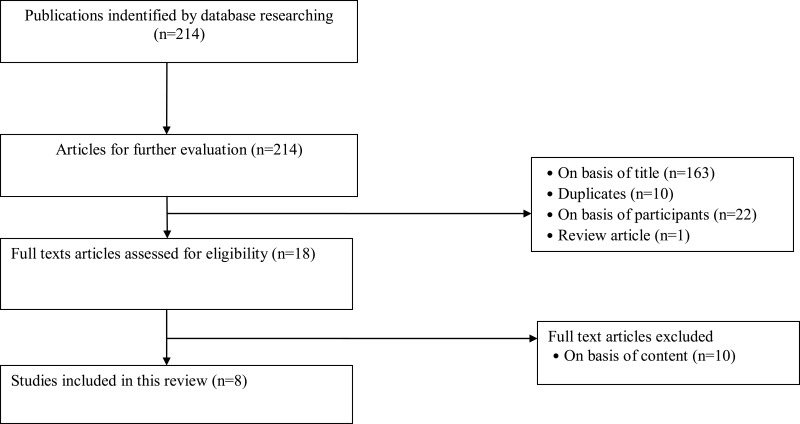
This study was conducted in compliance with the PRISMA statement.25 Relevant articles were identified by searching PubMed and PsycINFO for the publication dates from January 1, 2002, to March 25, 2022, with a combination of keywords. Articles in English available in peer-reviewed journals and resilience and quality of life evaluated by a standardized questionnaire were included in the systematic review. For the systematic search, text word search terms were used as search criteria: (resilience) AND (quality of life OR well-being) AND (mental disorder OR psychiatric disorder OR mental illness). A total of 214 articles were retrieved from two databases, PubMed and PsycINFO. After the exclusion of duplicates (n = 10), review study (n = 1) and on the basis of content and participants (n = 32), 18 records were screened and in total 8 studies were included. The characteristics of the included studies are summarized in Table 1 and an overview of the study selection process is shown in Figure 1. The inclusion criteria for the studies were the following: 1. Mainly investigating the resilience and quality of life in people with a diagnosis of mental disorders. Self-reported using questionnaire on resilience and quality of life and measure of association (correlation coefficient/standardized regression coefficient) were included. 2. Articles were published in scientific journals indexed in JCR and in English.
Table 1.
Summary of Characteristics and Associations Between Resilience and Quality of Life in the Included Studies
| Author, Year | Study (Design; Country) | Participants | Outcome Measures | N | r | 95% CI | p |
|---|---|---|---|---|---|---|---|
| Wartelsteiner et al19, 2016 | Cross sectional; Austria | Schizophrenia stable patients | 1.The resilience scale-25(RS-25) (Wagnild and Young, 1993) 2. Lancashire quality of life (105 items) |
52 | 0.481 | [0.240; 0.666] | 0.000 |
| Post et al20, 2018 | Cross sectional; Austria | BD-Ι stable patients | 1.The resilience scale-25(RS-25) (Wagnild and Young, 1993) 2. Lancashire quality of life (105 items) |
60 | 0.680 | [0.515;0.796] | 0.000 |
| Zizolfi et al31, 2019 | Cross sectional; Italy | Stable schizophrenia spectrum disorder | 1.The resilience scale-10 (Wagnild and Young, 1993) 2.Schizophreia quality of life scale(30 items) |
44 | 0.449 | [0.176;0.658] | 0.002 |
| Mejia-Lancheros et al32, 2021 | Longitudinal study(6-year follow-up); Denmark | Patients with homeless and mental disorders | 1.25-item Connor-Davidson Resilience scale 2.Lehman’s 20-item QOL interview(global quality of life) |
575 | 0.230 | [0.151; 0.306] | 0.000 |
| Pardeller et al33, 2020 | Cross sectional; Austria | MDD or BD-Ι acutely depressive symptoms patients | 1.Resilience scale-25 (RS-25) (Wagnild and Young, 1993) 2.WHOQOL-BREF(28 items) |
60 | 0.362 | [0.119; 0.564] | 0.004 |
| Lee et al34, 2017 | Cross sectional; South Korea | BD-Ι, BD-Π, BD NOS, remitted depressive, hyomainc or manic symptoms patients | 1. 25-itemConnor-Davidson Resilience scale 2.WHOQOL-BREF(28 items) |
68 | 0.820 | [0.723;0.885] | 0.000 |
| Guillen et al35, 2021 | Cross sectional; Spain | BPD patients receiving psychotherapy for six months | 1.The resilience scale-15 (Wagnild and Young, 1993) 2.Quality of life index(10 items) |
196 | 0.740 | [0.658;0.804] | 0.000 |
| Nunes et al36, 2022 | Cross sectional; Brazil | Stable severe mental disorder patients (MDD, BD and schizophrenia) | 1.The resilience scale-25(RS-25) (Wagnild and Young, 1993) 2. WHOQOL-BREF(28 items) |
384 | 0.406 | [0.319;0.486] | 0.000 |
| Mean effect size | 1439 | 0.551 | [0.370;0.691] | 0.000 |
Abbreviations: MDD, Major depressive disorder; BD-Ι, Bipolar Ι disorder; BD-Π, Bipolar Π disorder; BD NOS, Bipolar disorder, not otherwise unspecified; WHOQOL-BREF, WHO quality of life-BREF; QoL, Quality of life; BPD, Borderline personality disorder.
Figure 1.
Selection process of included studies using PRISMA flow diagram.
Data Synthesis and Analysis
Meta-analyses were conducted in Comprehensive Meta-Analysis (CMA) version 2.2. The outcomes across studies, Cohen d and Pearson product-moment correlation coefficient were calculated for the pooled effects. The Pearson product-moment correlation coefficient was chosen as effect size measure (ie correlation coefficient/standardized regression coefficient) or a measure which can be converted into such measure). The weighted mean effect size for the association between resilience and quality of life was calculated using a random-effects model.26 Finally, the pooled Fisher’s z values were converted back to Pearson correlations to improve interpretability. All effect size estimates are stated with 95% confidence intervals [CI]. The magnitude of effect sizes above 0.5 is assumed to be large, 0.30 as moderate, and 0.10 or less to be small.27 Heterogeneity was calculated with Q and I2. I2 > 75% was considered as high heterogeneity, 50% as moderate heterogeneity and 25% as low heterogeneity.28 The potential publication bias on the determined mean effect was evaluated and subgroup and meta-regression were performed. The publication bias used funnel plot, trim-and-fill analysis and Egger’s regression test.29,30 Any disagreements of study selection and data extraction were resolved by two authors.
Results
Participants
In the present systematic review study, the total number of participants included in the 8 articles consisted of 1439 participants with mental disorders. The smallest sample consisted of 44 participants31 and the largest sample had 575 participants.32 The average age was from 29 years to 46 years. In 7 of the 8 studies, the diagnosis of the participants was specified. In three studies, most of the sample had a diagnosis of major depressive disorder or bipolar disorder.20,33,34 Participants from two studies had a diagnosis of schizophrenia or schizophrenia spectrum disorder.19,31 Participants from two studies had a diagnosis of borderline personality disorder35 and a blend of major depressive disorder, bipolar disorder and schizophrenia, respectively.36 Participants were mostly given a diagnosis by psychiatrists according to DSM IV, DSM V, or ICD-1019,20,31,33–36 In one study, the diagnosis of participants was not specified.32 Most studies included stable or remitted patients, and one study included patients with acute symptoms;33 two studies did not specify the symptoms of their participants.32,35 Five studies included healthy participants as a comparison group.19,20,33–35 In one of the studies, psychotherapy was applied to investigate the effect of treatment on the relationship between resilience and quality of life35 and one study used a longitudinal design to investigate the long-term effect of resilience on quality of life.32 In 6 studies, psychological resilience was measured using the original or a translated version of Connor-Davidson Resilience scale37 or Wagnild and Young Resilience scale38 with 25 items.19,20,32–34,36 Two studies used the short version with 10 to 15 items.31,35
Results of Resilience and Quality of Life of Included Studies
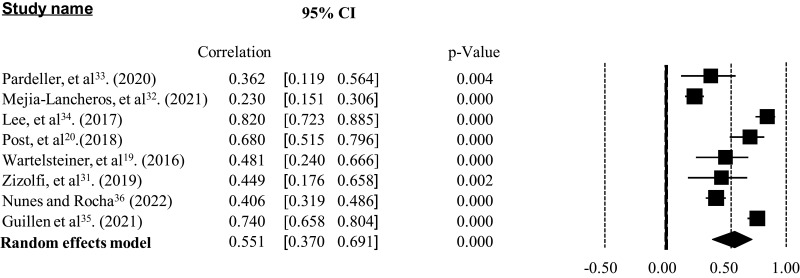
The measures of association in the individual studies varied between r = 0.23032 and r = 0.82034 and showed considerable heterogeneity (Q = 105.259, p < 0.001, I2 = 93.35%) (Figure 2). All individual effect sizes were significant and all study effects showed a significant positive association between resilience and mental health. In five studies a medium effect, and in three studies a large effect was identified.27 The weighted mean correlation across all studies was r = 0.551; (95% confidence interval: [0.370; 0.691], p < 0.001 (Table 1).
Figure 2.
Forest plot of the relationship between resilience and quality of life (Q = 105.259, p<0.001, I2 = 93.35%).
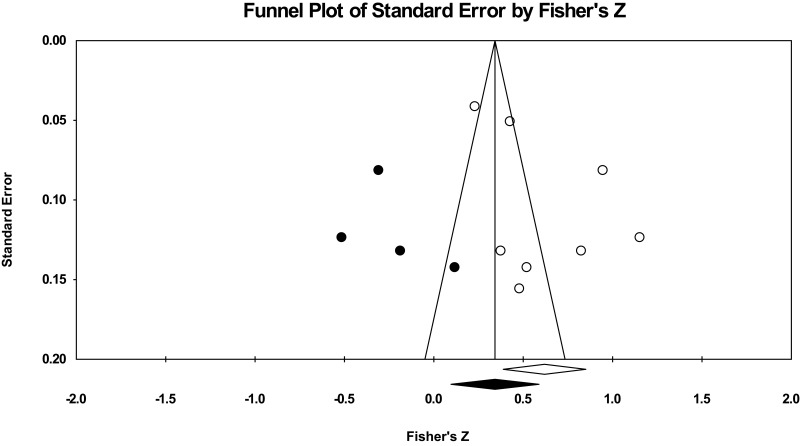
Publication Bias
Under a random-effects model, visual evaluation of the funnel plot revealed no absence of publication bias. The trim-and-fill analysis indicated that 4 studies were missing. The mean effect size adjusted for these studies was r = 0.55. The left-sided test for the asymmetry of the funnel plot using Egger’s regression test was not significant (p = 0.05124) (Figure 3).
Figure 3.
Random-effect funnel plot of Fisher’s Z by standard error detaining publication bias in the studies reporting resilience and quality of life.
Additional Analyses
In addition, other analysis for intervening variables was conducted which could have an effect on the association between resilience and quality of life and may explain the heterogeneity of study effects. A significant negative effect of sample size was identified: The larger the study sample, the weaker the association between resilience and quality of life (p = 0.0364). There was a positive effect of proportion of female study participants (p = 0.0074) and symptoms status (p < 0.001) between resilience and quality of life, respectively, suggesting that female participants and individuals with stable mental disorder symptoms were more likely to have a positive association between resilience and quality of life (Table 2).
Table 2.
Results of Subgroup and Meta-Regression
| Variable | Beta | SE | 95% CI | p |
|---|---|---|---|---|
| Mean age | −0.0333 | 0.0204 | [−0.0732; 0.0066] | 0.1020 |
| Proportion of female study participants | 0.0135 | 0.0050 | [0.0036; 0.0233] | 0.0074 |
| Publication year | −0.0628 | 0.0565 | [−0.1735; 0.0478] | 0.2659 |
| Sample size | −0.0009 | 0.0004 | [−0.0017; −0.0001] | 0.0364 |
| Number of items of resilience scale | −0.0073 | 0.0204 | [−0.0473; 0.0326] | 0.7185 |
| n | r | 95% CI | p | |
| Symptoms status | <0.001 | |||
| Acute | 1 | 0.362 | [0.119; 0.564] | |
| Stable | 5 | 0.593 | [0.376;0.748] |
Notes: Beta, standardized regression coefficient; n, number of included studies (insufficient information in two studies).
Abbreviations: SE, standard error; 95% CI, 95% confidence interval.
Quality of Assessment of Included Studies
In terms of the reliability of instruments, a majority of included studies had a low risk of bias reporting, gaining a good reliability. All studies applied appropriate analysis and satisfactory reporting (Table 3).
Table 3.
Quality Assessment of the Included Studies
| Reliability of Assessments | n | % |
|---|---|---|
| Acceptable reliability/ low risk of bias | 7 | 87.5 |
| Questionable reliability/ high risk of bias | 0 | 0 |
| Insufficient information/ unclear risk of bias | 1 | 12.5 |
| Data analysis | ||
| Appropriate analysis/ low risk of bias | 8 | 100 |
| Inappropriate analysis / high risk of bias | 0 | 0 |
| Reporting | ||
| Satisfactory reporting/ low risk of bias | 8 | 100 |
| Incomplete reporting/ high risk of bias | 0 | 0 |
Notes: n, number of included studies; data analysis, it refers to the methods used appropriately for data analysis; reporting, it refers that the author were specific in their reporting about hypotheses and statistical findings.
Discussion
The present review found an association between resilience and quality of life in people with mental disorders. Across the included studies, a significant effect of r = 0.551 was determined representing a moderate correlation. Individuals with mental disorders who reported having a higher resilience considered their quality of life to be better. The main result of our meta-analysis was consistent with previous findings on the association between higher resilience and quality of life.18,19,39 The resilience scale proved to be a reliable instrument in the included studies. Our findings indicated the association between resilience and quality of life and future studies should examine the efficacy of resiliency training programs to increase levels of quality of life for individuals with mental disorders. The findings were also consistent with previous studies that suggested that increasing quality of life may be a vehicle to achieving recovery.40 From a theoretical view, resilience is considered as a process which will ultimately have a positive effect on subjective satisfaction with aspects of quality of life. Therefore, resilience is a process that is influenced by the physical, social and psychological status of individuals.41 Other studies indicated that interventions based on mindfulness or resilience reinforcement program can contribute to the strengthening of feelings in acceptance and competence.42–46
The main weakness of the meta-analysis results from the research designs of the included studies, because associations identified in most cross-sectional studies do not have causal inferences about the association between resilience and quality of life. Overall, very few prospective studies were available; of these, only one study reported associations between resilience and quality of life for a follow-up.32 Another limitation results from the statistical heterogeneity of the individual study effects which makes it more difficult to generalize the results to people with all mental disorders. However, all studies found positive associations and most were interpreted as moderate to strong. There is no consistent understanding to define resilience as a state or trait. While some researches view resilience as a personality trait, others consider it to be a dynamic and changeable process. Thus, various outcome-based approaches of assessment and operationalization are needed to measure the construct, and longitudinal studies are important to assess for the causality.47 Lastly, meta-analysis findings should be interpreted with caution due to the limited number of included studies in the meta-analysis and included criteria, including criterion type, study design, instruction and participants’ characteristics.48
Conclusion
Despite the limitations mentioned above, the results of the present meta-analysis indicate that a higher level of resilience is associated with better quality of life in people with mental disorders. This study is the first to provide a statistical integration of the effects and the study makes a contribution to resilience research. Resilience appears to be an important factor in the context of psychopathology and improvement of quality of life. On the path to recovery, resilience has its importance and impact on the quality of life of individuals with mental disorders. High resilience does not necessarily prevent mental illness, but it has a significant contribution as part of a comprehensive therapy in the treatment of depression and other psychiatric disorders.11
Prospective studies are needed to clarify the causal nature of the association between resilience and quality of life. Future research should aim to identify individuals with low resilience in clinical practice and offer them support or training, in terms of external resources, to enhance their quality of life.49
Acknowledgment
This study was supported by grant from Zuoying Armed Forces General Hospital, Kaohsiung, Taiwan (KAFGH-ZY-D-111034).
Disclosure
All authors declare no competing interests in this work.
References
- 1.American Psychological Association. The road to resilience; 2010. Available from: http://www.apa.org/helpcenter/road-resilience.aspx/. Accessed February 20, 2023.
- 2.Waugh CE, Koster EHW. A resilience framework for promoting stable remission from depression. Clin Psychol Rev. 2015;41:49–60. doi: 10.1016/j.cpr.2014.05.004 [DOI] [PubMed] [Google Scholar]
- 3.Min JA, Jung YE, Kim DJ, et al. Characteristics associated with low resilience in patients with depression and/or anxiety disorders. Quality Life Res. 2013;22:231–241. doi: 10.1007/s11136-012-0153-3 [DOI] [PubMed] [Google Scholar]
- 4.Johnson J, Gooding PA, Wood AM, Taylor PJ, Pratt D, Tarrier N. Resilience to suicidal ideation in psychosis: positive self-appraisals buffer the impact of hopelessness. Behav Res Thera. 2010;48:883–889. doi: 10.1016/j.brat.2010.05.013 [DOI] [PubMed] [Google Scholar]
- 5.Min JA, Lee CU, Chae JH. Resilience moderates the risk of depression and anxiety symptoms on suicidal ideation in patients with depression and/or anxiety disorders. Comprehens Psychiatry. 2015;56:103–111. doi: 10.1016/j.comppsych.2014.07.022 [DOI] [PubMed] [Google Scholar]
- 6.Nrugham L, Holen A, Sund AM. Associations between attempted suicide, violent life events, depressive symptoms, and resilience in adolescents and young adults. J Nerv Ment Dis. 2010;198:131–136. doi: 10.1097/NMD.0b013e3181cc43a2 [DOI] [PubMed] [Google Scholar]
- 7.Torgalsboen AK. Sustaining full recovery in schizophrenia after 15 years: does resilience matter? Clin. Schizophren Relat Psychos. 2012;5:193–200. doi: 10.3371/CSRP.5.4.3 [DOI] [PubMed] [Google Scholar]
- 8.Choi JW, Cha B, Jang J, et al. and impulsivity in euthymic patients with bipolar disorder. J Affect Disord. 2015;170:172–177. doi: 10.1016/j.jad.2014.08.056 [DOI] [PubMed] [Google Scholar]
- 9.Herrman H, Stewart DE, Diaz-Granados N, Berger EL, Jackson B, Yuen T. What is resilience? Can J Psychiatry. 2011;56:258–265. doi: 10.1177/070674371105600504 [DOI] [PubMed] [Google Scholar]
- 10.Masten AS. Resilience in children threatened by extreme adversity: frameworks for research, practice, and translational synergy. Dev Psychopathol. 2011;23:493–506. doi: 10.1017/S0954579411000198 [DOI] [PubMed] [Google Scholar]
- 11.Shrivastava A, Desousa A. Resilience: a psychobiological construct for psychiatric disorders. Ind J Psychiatry. 2006;58:38–43. doi: 10.4103/0019-5545.174365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stainton A, Chisholm K, Kaiser N, et al. Resilience as a multimodal dynamic process. Early Intervent Psychiatry. 2019;13:725–732. doi: 10.1111/eip.12726 [DOI] [PubMed] [Google Scholar]
- 13.Las Hayas C, Padierna JA, Muñoz P, et al. Resilience in eating disorders: a qualitative study. Women Health. 2016;56:576–594. doi: 10.1080/03630242.2015.1101744 [DOI] [PubMed] [Google Scholar]
- 14.Berger ML, Bingefors K, Hedblom EC, Pashos CL, Torrance GW. Health Care Cost, Quality, and Outcomes. Lawrenceville NJ: ISPOR Book of Terms; 2003. [Google Scholar]
- 15.Lambert M, Schimmelmann BG, Naber D, et al. Early- and delayed antipsychotic response and prediction of outcome in 528 severely impaired patients with schizophrenia treated with amisulpride. Pharmacopsychiatry. 2009;42:277. [DOI] [PubMed] [Google Scholar]
- 16.Boden R, Sundstrom J, Lindstrom E, Lindstrom L. Association between symptomatic remission and functional outcome in first-episode schizophrenia. Schizophr Res. 2009;107:232–237. doi: 10.1016/j.schres.2008.10.004 [DOI] [PubMed] [Google Scholar]
- 17.Lambert M, Karow A, Leucht S, Schimmelmann BG, Naber D. Remission in schizophrenia: validity, frequency, predictors, and patients’ perspective 5 years later. Dialogues Clin Neurosci. 2010;12:393–407. doi: 10.31887/DCNS.2010.12.3/mlambert [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mizuno Y, Hofer A, Suzuki T, et al. Clinical and biological correlates of resilience in patients with schizophrenia and bipolar disorder: a cross-sectional study. Schizophrenia Res. 2016;175:148–153. doi: 10.1016/j.schres.2016.04.047 [DOI] [PubMed] [Google Scholar]
- 19.Wartelsteiner F, Mizuno Y, Frajo‐Apor B, et al. Quality of life in stabilized patients with schizophrenia is mainly associated with resilience and self‐esteem. Acta Psychiatrica Scand. 2016;134:360–367. doi: 10.1111/acps.12628 [DOI] [PubMed] [Google Scholar]
- 20.Post F, Pardeller S, Frajo-Apor B, et al. Quality of life in stabilized outpatients with bipolar I disorder: associations with resilience, internalized stigma, and residual symptoms. J Affect Disord. 2018;238:399–404. doi: 10.1016/j.jad.2018.05.055 [DOI] [PubMed] [Google Scholar]
- 21.Hofer A, Mizuno Y, Frajo-Apor B, et al. Resilience, internalized stigma, self-esteem, and hopelessness among people with schizophrenia: cultural comparison in Austria and Japan. Schizophr Res. 2016;171:86–91. doi: 10.1016/j.schres.2016.01.027 [DOI] [PubMed] [Google Scholar]
- 22.Hofer A, Mizuno Y, Wartelsteiner F, et al. Quality of life in schizophrenia and bipolar disorder: the impact of symptomatic remission and resilience. Eur Psychiatry. 2017;46:42–47. doi: 10.1016/j.eurpsy.2017.08.005 [DOI] [PubMed] [Google Scholar]
- 23.Kuehner C. Subjective quality of life: validity issues with depressed patients. Acta Psychiatrica Scand. 2002;106:62–70. doi: 10.1034/j.1600-0447.2002.02204.x [DOI] [PubMed] [Google Scholar]
- 24.Ay-Woan P, Sarah CP, LyInn C, Tsyr-Jang C, Ping-Chuan H. Quality of Life in Depression: predictive Models. Quality of Life Res. 2006;15:39–48. doi: 10.1007/s11136-005-0381-x [DOI] [PubMed] [Google Scholar]
- 25.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta‐analysis protocols (PRISMA‐P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hedges LV, Olkin I. Statistical Methods for Meta-Analysis. 7 ed. San Diego: Academic Press; 1999. [Google Scholar]
- 27.Cohen J. Statistical Power Analysis for the Behavioral Sciences. second ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 28.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Duval S, Tweedie R. Trim and Fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341X.2000.00455.x [DOI] [PubMed] [Google Scholar]
- 30.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zizolfi D, Poloni N, Caselli I. Resilience and recovery style: a retrospective study on associations among personal resources, symptoms, neurocognition, quality of life and psychosocial functioning in psychotic patients. Psychol Res Beh Manag. 2019;12:385–395. doi: 10.2147/PRBM.S205424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mejia-Lancheros C, Woodhall-Melnik J, Wang R, Hwang SW, Stergiopoulos V, Durbin A. Associations of resilience with quality of life levels in adults experiencing homelessness and mental illness: a longitudinal study. Health Qual Life Outcomes. 2021;19:74. doi: 10.1186/s12955-021-01713-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pardeller S, Kemmler G, Hoertnagl CM, Hofer A. Associations between resilience and quality of life in patient experiencing a depressive episode. Psychiatry Res. 2020;292:113353. doi: 10.1016/j.psychres.2020.113353 [DOI] [PubMed] [Google Scholar]
- 34.Lee D, Cha B, Park CS, et al. Effects of resilience on quality of life in patients with bipolar disorder. J Affect Dis. 2017;207:434–441. doi: 10.1016/j.jad.2016.08.075 [DOI] [PubMed] [Google Scholar]
- 35.Guillén V, Tormo ES, Fonseca-Baeza S, et al. Resilience as a predictor of quality of life in participants with borderline personality disorder before and after treatment. BMC Psychiatry. 2021;21:305. doi: 10.1186/s12888-021-03312-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nunes KG, Da Rocha NS. Resilience in severe mental disorders: correlations to clinical measures and quality of life in hospitalized patients with major depression, bipolar disorder, and schizophrenia. Qual Life Res. 2022;31:507–516. doi: 10.1007/s11136-021-02920-3 [DOI] [PubMed] [Google Scholar]
- 37.Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18:76–82. doi: 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- 38.Wagnild G, Young H. Development and psychometric evaluation of the Resilience Scale. J Nurs Meas. 1993;1:165–178. [PubMed] [Google Scholar]
- 39.Laird KT, Lavretsky H, Paholpak P, et al. Clinical correlates of resilience factors in geriatric depression. Int Psychogeriat. 2019;31:193–202. doi: 10.1017/S1041610217002873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mitchison D, Dawson L, Hand L, Mond J, Hay P. Quality of life as a vulnerability and recovery factor in eating disorders: a community-based study. BMC Psychiatry. 2016;16:328. doi: 10.1186/s12888-016-1033-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Windle G. What is resilience? A review and concept analysis. Rev Clin Gerontol. 2011;21:152–169. doi: 10.1017/S0959259810000420 [DOI] [Google Scholar]
- 42.Wanden-Berghe RG, Sanz-Valero J, Wanden-Berghe C. The application of mindfulness to eating disorders treatment: a systematic review. Eat Behav. 2010;19:34–48. [DOI] [PubMed] [Google Scholar]
- 43.Chou LN, Hunter A. Factors affecting quality of life in Taiwanese survivors of childhood cancer. J Adv Nurs. 2009;65:2131–2141. doi: 10.1111/j.1365-2648.2009.05078.x [DOI] [PubMed] [Google Scholar]
- 44.Xu J, Ou L. Resilience and quality of life among Wenchuan earthquake survivors: the mediating role of social support. Public Health. 2014;128:430–437. doi: 10.1016/j.puhe.2014.03.002 [DOI] [PubMed] [Google Scholar]
- 45.Alriksson-Schmidt AI, Wallander J, Biasini F. Quality of life and resilience in adolescents with a mobility disability. J Pediatr Psychol. 2007;32:370–379. doi: 10.1093/jpepsy/jsl002 [DOI] [PubMed] [Google Scholar]
- 46.Mueser KT, Penn DL, Addington J, et al. The NAVIGATE program for first-episode psychosis: rationale, overview, and description of psychosocial components. Psychiatr Serv. 2015;66:680–690. doi: 10.1176/appi.ps.201400413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kunzler AM, Gilan DA, Kalisch R, Tüscher O, Lieb K. Aktuelle Konzepte der Resilienzforschung [Current concepts of resilience research]. Nervenarzt. 2018;89:747–753. German. doi: 10.1007/s00115-018-0529-x [DOI] [PubMed] [Google Scholar]
- 48.Antes AL, Murphy ST, Waples EP, et al. A meta-analysis of ethics instruction effectiveness in the sciences. Ethics Behav. 2009;19(5):379–402. doi: 10.1080/10508420903035380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hu T, Zhang D, Wang J. A meta-analysis of the trait resilience and mental health. Pers Individ Dif. 2015;76:18–27. doi: 10.1016/j.paid.2014.11.039 [DOI] [Google Scholar]