SUMMARY
West Nile virus (WNV) is a member of the Japanese encephalitis serocomplex, which was first described in 1937 as neurotropic virus in Uganda in 1937. Subsequently, WNV was identified in the rest of the old-world and from 1999 in North America.
Birds are the primary hosts, and WNV is maintained in a bird-mosquito-bird cycle, with pigs as amplifying hosts and humans and horses as incidental hosts. WNV transmission is warranted by mosquitoes, usually of the Culex spp., with a tendency to spill over when mosquitoes’ populations build up. Other types of transmissions have been described in endemic areas, as trough transplanted organs and transfused blood, placenta, maternal milk, and in some occupational settings.
WNV infections in North America and Europe are generally reported during the summer and autumn. Extreme climate phenomena and soil degradation are important events which contribute to expansion of mosquito population and consequently to the increasing number of infections. Draught plays a pivotal role as it makes foul water standing in city drains and catch basins richer of organic material.
The relationship between global warming and WNV in climate areas is depicted by investigations on 16,298 WNV cases observed in the United States during the period 2001–2005 that showed that a 5°C increase in mean maximum weekly temperature was associated with a 32–50% higher incidence of WNV infection.
In Europe, during the 2022 season, an increase of WNV cases was observed in Mediterranean countries where 1,041 cases were reported based on ECDC data. This outbreak can be associated to the climate characteristics reported during this period and to the introduction of a new WNV-1 lineage.
In conclusion, current climate change is causing an increase of mosquito circulation that supports the widest spread of some vector-borne virus including WNV diffusion in previously non-permissible areas. This warrant public health measures to control vectors circulation to reduce WNV and to screen blood and organ donations.
Keywords: WNV, encephalitis, meningitis, treatment, complications
INTRODUCTION
West Nile virus (WNV) is a member of the Japanese encephalitis serocomplex, which can cause a spectrum of human diseases with clinical characteristics ranging from a mild febrile disease to a severe meningitis or encephalitis. The Japanese encephalitis serogroup of flaviviruses comprises eight species and two subtypes with a distribution spanning all continents except Antarctica. The main virus species in this group include Japanese encephalitis virus (JEV), the West Nile virus (WNV), Kunjin virus (a subtype of WNV), Murray Valley encephalitis virus (MVEV), and St. Louis encephalitis virus. Other minor members of the group include Usutu, Koutango virus, Yaounde viruses, Cacipacore virus and Alfuy virus (subtype of MVEV). Most members of the Japanese encephalitis serological group have avian and vertebrate hosts and are primarily transmitted by Culex spp. mosquitoes. Unlike other members of the Japanese encephalitis serological group, WNV can be divided genetically into nine lineages, but only WNV lineage 1 (WNV-1) identified in North America, North Africa, Europe and Australia and lineage 2 (WNV-2), which is endemic in Southern Africa and Madagascar, can cause human disease. In recent years, lineage 2 circulation has been identified in central and eastern Europe, in animal and human outbreaks [1]. WNV was first described as a neurotropic virus in Uganda in 1937. Subsequently, it was identified as the causative agent of a mild febrile illness primarily in Africa, Middle East, Russia, and Europe, with the predominant strain being WNV-2. In the mid-1990s, a new strain of WNV-1 emerged as a causative agent of a febrile illness complicated in a high proportion by neurological symptoms, with epizootics occurring in Romania, Russia, and Israel. Since 1999, WNV has been described as the agent of a human outbreak in Northern America, where it is currently considered the most common zoonotic virus causing neuroinvasive disease [2]. The main sequelae reported after WNV infection in western countries are reported in Table 1 [3].
Table 1.
Main sequelae reported in patients with WN disease*.
| Findings |
12 months
% observed |
60 months
% observed |
84 months
% observed |
|---|---|---|---|
| Patients reporting symptoms | 60 | 40 | 40 |
| Fatigue | 37 | 22 | 20 |
| Difficulty walking/ataxia | 15 | 8 | 4 |
| Memory loss | 11 | 7 | 9 |
| Still receiving medical observation/cure | 41 | 14 | 13 |
Modified by reference 3.
Climate change may influence the spread of certain pathogens due to several factors, including increased rates of reproduction and incubation within a vector and increased rates of mosquito bites. Additionally, heavy rainfall and periods of drought can affect the spatial-temporal distribution of vectors.
Here, we systematically review the key epidemiological aspects of WNV spread in Europe and North America and their relationship with the ongoing climate change.
MATERIALS AND METHODS
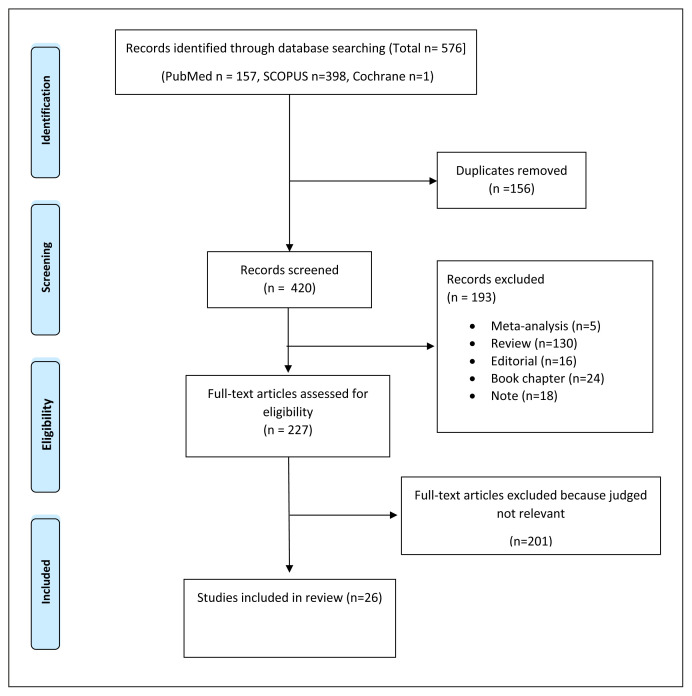
Relevant papers reporting in vivo and in vitro investigations and results of clinical trials until January 1st, 2023, were searched on Medline, Scopus, and Cochranelibrary.com using the key words: “West Nile Virus” and “Climate change”. Articles that evaluated the relationships between spread pattern of WNV diffusion and environmental climate changes were included. A manual search by tracking references of the retrieved studies was also performed to complete the study. Three independent authors (CD, GG, TA) reviewed the results of the literature search according to the inclusion and exclusion criteria. Any disagreement was resolved by PP. For the phase of full-text screening, all articles were downloaded and reviewed for eligibility. Investigations and studies on human populations and patterns of vector dissemination that reported data on WNV epidemiology in the English language, were included in the review. The search was carried out according to the Preferred Reporting Item for Systematic Review and Meta-analyses (PRISMA). The flowchart of the systematic review is reported in Figure 1.
Figure 1.
PRISMA 2009
Flow Diagram.
WNV TRANSMISSION
Mosquito-borne transmission
WNV is primarily transmitted by mosquitoes usually of the Culex spp. Although WNV has also been recovered from ticks in Russia, ticks have an unclear role in maintaining or disseminating the virus and their role may be relevant in preserving the virus during the winter [4].
Birds (in particular, Ardeid birds such as herons and egrets) are the primary hosts, and the virus is maintained in a bird-mosquito-bird cycle. Other animals can serve as amplifying hosts. In fact, WNV has been demonstrated to reproduce in pigs, which can infect mosquitoes when they take blood meals [5]. Humans and other vertebrates, such as horses, are considered incidental hosts and are thought to have an irrelevant role in the transmission cycle of WNV.
Serological data indicate that many species can become infected, but the role of some species in the spread of WNV should be further investigated [6]. Wild birds develop prolonged high levels of viraemia but generally remain asymptomatic; however, significant avian mortality has occurred in Israel and the United States among American crows and other North American corvids. Mammals do not appear to generate viraemia levels of sufficient magnitude to infect mosquitoes and their contribute to transmission is not considered relevant, so birds should be considered the most important amplifying hosts of WNV and local resident, non-migratory birds and long-range migratory birds may both contribute to the spread of WNV. In addition to birds, only a few species should be considered relevant in the transmission of WNV. In fact, viraemia levels sufficient to infect mosquitoes were found after experimental infection of young alligators (Alligator mississippiensis) and the lake frog (Rana ridibunda) [7, 8].
Non-mosquito-borne transmission
Almost all WNV human infections result from mosquito bites, but transmission can also occur by other routes.
WNV transmission through organ transplantation was first described during the 2002 epidemic [9]. This can be a relevant aspect as organ transplant recipients who are chronically immunosuppressed appear to have an increased risk for severe WNV disease, regardless of the transmission route, as it is generally reported in immunocompromised and elderly with CNS infections [10–14].
Transmission of WNV through blood transfusion was first documented during the 2002 outbreak in North America. In this occasion, blood collection agencies in the United States and Canada enhanced donor deferral and began screening blood donations with experimental nucleic acid amplification tests. In 2003 and 2004, more than 1,000 potentially WNV viremic blood donations were identified, and their blood components were discarded. Despite these intensive investigations, 6 transfusion-related cases were documented in 2003, and at least another case was documented in 2004, indicating that infectious blood components with low concentrations of WNV may escape screening tests. One case of possible WNV transmission through dialysis has been reported [15–17].
Some cases of transplacental transmission have been described. A 20-year-old woman had onset of WNV disease in week 27 of gestation. Her infant was born at term with chorioretinitis and cystic damage of cerebral tissue. Intensified surveillance identified four other mothers who had WNV illness during pregnancy, three of whom delivered infants with no evidence of WNV infection. These infants appeared normal at birth and at 6 months of age; the fourth woman delivered prematurely; her infant had neonatal respiratory distress, but was not tested for WNV infection [18]. In 2003, the CDC received reports of seventy-four women infected with WNV during pregnancy, most of whom delivered apparently healthy infants.
Occupational transmission through percutaneous exposure can be reported in sporadic cases and experimental evidence of aerosol transmission in mice has been reported [19]. WNV infection has been occupationally acquired by laboratory workers through percutaneous inoculation and possibly through aerosol exposure. An outbreak of WNV disease among turkey handlers at a turkey farm confirms the possibility of infection after aerosol exposure [20].
A 40-year-old woman contracted WNV infection from blood transfused shortly after she delivered a healthy infant. WNV nucleic acid was detected in her breast milk, and IgM antibodies were found in her infant, who remained healthy. No other cases of possible WNV transmission through breast milk have been reported [21].
Patterns of WNV transmission to humans unrelated to mosquito bite are depicted in Table 2 [22].
Table 2.
Main non-mosquito related routes of WNV transmission.
| Route | Frequency | Outcome |
|---|---|---|
| Blood transfusion | Negligible in the areas where blood transfusions are screened | Related to underlying disease |
| Organ transplantation | Negligible in the areas where transfusions are screened | Poor due to immunosuppressive treatments |
| Vertical transmission | 72 cases reported in the period | Probably worsened |
| Occupational transmission | Outbreak reported among turkey handlers or laboratory acquired [22] | 1 of 9 infected had encephalitis |
Changing epidemiology of WNV infection
In North America and Europe, WNV disease is reported with the highest frequency in late summer and early autumn. WNV has two patterns of diffusion, one occurring in rural environment with wild birds and mosquitoes as the main drivers of the infection and another in urban ecosystem where domestic birds are the reservoir and mosquitoes feeding both birds and humans are the main vectors. Principal vector is Culex pipiens, which is an urban-dwelling ornithophilic mosquito whose rate of replication is influenced by environmental changes [23]. Studies retrieved by literature search and included in the systematic review are reported in Table 3 (18–22, 24–44). Drought seems to be a relevant driver of Cx. pipiens replication as this mosquito typically breeds underground in the foul water standing in city drains and catch basins, which become richer of organic material during a drought. Moreover, during a drought, some mosquito predators, such as frogs and dragonflies decrease in their abundance and birds congregate around shrinking water sites, where the virus can easily circulate. All these conditions were present in the spring and summer of 1999 in the northeastern and mid-Atlantic states, when a WNV outbreak was reported for the first time into the Western hemisphere [24, 25].
Table 3.
Studies retrieved by literature search on WNV and climate changes included in the systematic review and their contribute to the topic.
| N. Reference | Author | Main characteristics investigated to be included in the study | Findings |
|---|---|---|---|
| 18 | CDC | Intrauterine infection | Low frequency of intrauterine infection |
| 19 | Nir Y, et al. | WNV infection in mice following exposure to a viral aerosol | Experimental investigation supporting possibility of transmission by aerosol |
| 20 | CDC | WNV infection among turkey breeder farm workers | Epidemiologic evidence supporting WNV transmission by close contact with infected birds |
| 21 | CDC | Possible WNV transmission to an infant through breast-feeding | An infant remained healthy despite IgM were positive |
| 22 | CDC | Laboratory-Acquired WNV infections | Two laboratory workers handling WNV infected body fluids acquired the infection |
| 24 | Wang G, et al. | Dry weather induces outbreaks of human WNV infections | Drought favoured Cx. pipiens diffusion |
| 25 | Dohm DJ, et al. | Effect of environmental temperature on the ability of Cx. pipiens to transmit WNV | The best rate of Cx. pipiens infection was found at 30°C |
| 26 | Paz S. | Regional impact of climate change WNV outbreak in Israel (2000) | Heat condition in summer favoured the Israeli outbreak |
| 27 | Paz S, et al. | Warming tendency on Cx. pipiens population abundance and on the probability of WNV outbreaks | warming and season rainfall were associated with higher WNV incidence |
| 28 | Platonov AE, et al. | WNV in Volgograd, Russia, in relation to climate change and mosquito | A mild winter and a relatively hot summer appear to favour WNV |
| 29 | Soverov JE, et al. | Weather influenced WNV in the USA | Warmer temperatures, elevated humidity, and heavy precipitations favours WNV |
| 30 | Harrigan RJ, et al | A continental risk assessment of WNV virus under climate change | Expansion of WNV suitable areas is projected to increase due to higher temperatures and lower annual precipitations |
| 31 | Roiz D, et al. | Climatic effects on mosquito abundance in Mediterranean wetlands | Rainfall during the winter and temperature were related to Cx. pipiens abundance |
| 32 | Marini G, et al. | Cx. pipiens in Northwestern Italy | Inter-seasonal differences in mosquito dynamics are driven by high temperature during the spring |
| 33 | Paz S, et al. | Permissive summer temperatures of the 2010 European WNV upsurge | Heat summer temperatures and different patterns of precipitations including quantities above perennial average in May and dry conditions during the rest of summer favored WNV diffusion |
| 34 | Cotar AI, et al. | Transmission Dynamics of the WNV in Mosquito Vector Populations under the Influence of Weather Factor in the Danube Delta, Romania | Best predictors of WNV infection are temperature and precipitation during the previous 20 and 30 days respectively |
| 35 | Savage, et al. | Entomologic and avian investigation of WNV in 1996 outbreak in Romania | WNV and Cx. pipiens infection was demonstrated during the outbreak and the lineage identified was found to be associated to the WNV strains from North-Africa |
| 36 | ECDC | WNV keeps on moving up in Europe | Epidemiologic data on the diffusion of WNV in Europe during the period 2010–2018 |
| 37 | Barrett ADT | West Nile in Europe: an increasing public health problem | Distribution of WNV the during 2010–2018 period in Europe and climate change |
| 38 | CDC | West Nile Virus Statistics and maps | Statistics and maps of WNV distribution in the USA |
| 39 | Mavrakis A, et al. | Meteorological patterns and the evolution of WNV in an environmentally stressed Mediterranean area | High values of summer precipitation contributed both directly and indirectly to WNV distribution |
| 40 | ECDC | West Nile transmission season | Distribution of WNV cases during the 2022 season |
| 41 | Barzon L, et al. | Rapid spread of a new WNV lineage 1 in northern Italy | A new lineage diffusion can cause a new WNV severe outbreak with neuroinvasive cases |
| 42 | Barzon L. et al. | Early start of seasonal transmission and co-circulation of WNV-2 and WNV-1 | WNV-1 and WNV-2 circulate since 2021 in Padua region |
| 43 | Liu-Helmersson J. et al. | Distribution of Arbovirus and climate change | Climate change mitigation can affect the rapid diffusion of vectors |
| 44 | Semenza JC, et al. | Climate change projections of West Nile virus infections in Europe: implications for blood safety practices | Climate change projections for 2025 reveal a higher probability of WNV infection particularly at the edges of the current transmission areas |
The same relationship between climate change and WNV diffusion could be observed in a limited case-series reported in 1999 in Israel, where two of three cases identified as WNV fever (WNF) died. After these cases were diagnosed, during the summer of 2000, a large outbreak of WNF occurred, causing 417 serologically confirmed cases and 35 deaths. Many cases occurred in densely populated areas. These cases followed the extremely hot summer of 1998 and epidemiologic investigations demonstrated a close relationship between high temperature and the number of WNF diagnosed cases. Interestingly, during this outbreak, the main association was found between WNF occurrence and mosquito abundance, which was influenced by temperature, but was not affected by the amount of rain [26, 27].
Other interesting relationships between an increase of temperature and the number of reported WNF cases were highlighted by the analysis of the outbreak in the Volgograd (Russia) area in the period 2000–2007. In this area, high temperature in the period from July to September (therefore, the number of hours with temperature above 25°C) and relatively high temperature in the winter period were found to be correlated with the number of WNF cases [28].
Further investigations confirmed the close relationship between the increase of WNF cases and warmer temperatures, elevated humidity, and heavy precipitation. Investigations on 16,298 WNV cases observed across 17 states in the United States of America during the period 2001–2005 showed that a 5°C increase in average weekly maximum temperature was associated with a 32–50% higher incidence of WNV infection. Moreover, a 4–8% increase of WNV infection was reported 1–2 weeks later after a 20-mm rise in cumulative weekly precipitation. When periods with heavy precipitations (>50 mm per day) were evaluated a correspondent 33% rise in WNV cases incidence was observed. This association was attenuated when the analysis was extended to the days with precipitations greater than 30 or 40 mm per day and no association was reported when only the days in the period June–August were considered. It can be speculated that heavy rainfall can stimulate disease transmission by increasing humidity, which stimulates mosquitoes to oviposit and seek hosts [29].
A study of WNV prevalence in the United States over 8 years found that temperature and precipitation patterns were linked to the presence of WNV in vectors, primary hosts, and secondary hosts. The study’s mathematical model predicts that as temperatures increase in northern and western regions, the distribution of vectors and circulation of WNV will also rise [30].
Investigations considering Mediterranean basin linked the abundance of Cx. pipiens to annual maximum temperatures and winter rainfalls but has failed to identify a linear relationship between temperatures and mosquito abundance, probably due to reduced survival of some mosquitoes to temperature above 40°C [31].
Based on a study proposing a model of Cx. pipiens distribution in regions of Western-Italy, the greatest number of vectors can be found between the 27th and the 31st week of the year. Other models were not predictive of vectors circulation as several factors including the number of precipitations or wind direction can influence the local distribution. In any case, mosquito distribution was found to be associated with high temperatures in the spring and with a rainy period during the first 3 months of the year, which provides more sites where larvae can feed [32].
WNV recognizes two main patterns of transmission, one occurring in urban areas, where humans and horses can be accidentally involved, and one observed in rural regions where wetlands serve as bird-nesting areas that provide ideal conditions for establishing WNV endemic cycles. The first outbreak in Europe receiving extensive investigations was reported in 1996 in southeast Romania, an area which is crossed by a main migration flyway connecting Africa to Europe which includes the fluvial Danube Delta. During this outbreak 352 neuroinvasive infections were reported. After this outbreak, WNV was again reported in many European countries in 2010, favored by extremely heat summer temperatures and by different patterns of precipitations including quantities above perennial average in May and dry conditions during the rest of summer [33]. A study on the prevalence of vectors and WNV demonstrates that the number of vectors peaks between June and late August and the highest rate of WNV vectors could be found in late August, although a great variability could be observed because of the influence of high temperatures in some areas. Based on the results of this study, we can speculate that beside heavy precipitations, drought can increase the number of mosquitoes in the environment. In fact, heat and drought led to a shrinking of the water bodies where the eutrophication caused by water evaporation increases the organic matter available for mosquito’s feeding. In any case, no infected vector was found after mid-September as after this period weather cooling and shorter periods of daylight are triggers of diapause induction, when the mosquitoes do not show attraction to the hosts [34].
The upcoming aspects of WNV circulation
Some European countries are experiencing an increase in WNV circulation with many neuroinvasive cases. WNV fever was reported as sporadic cases in Europe starting in 1963, when the virus was isolated from patients and mosquitoes in the Rhône Delta as well as from patients and Hyalommamarginatum ticks in the Volga Delta. In these occasions the virus identified was found to be like the strains circulating in North-Africa [35, 45]. WNV lineage 2 has re-emerged in central Europe since the early 2000s, when it was first detected in Hungary in 2004, associated with sporadic cases in birds and mammals. Then it spread to eastern Austria and southern European countries, where it caused large outbreaks such as the 2010 outbreak in Greece. Another strain of WNV-2 was detected in southern Russia in 2004. WNV-2 infections continued to be reported in the European area in the period 2010–2018 and the cases reported in 2018 exceeded the sum of those reported between 2010 and 2017 [36].
Confirming the data available for other vector-borne viruses, outbreaks of WNF tend to take place each year, but differ greatly in magnitude and geographic location. Similarly, since the new introduction of WNV in Europe in 1996, cases peaked in the period 2012–2013 and in 2018, showing an increase in terms of the number of endemic areas. Looking at the demographic characteristics of the cases reported in European countries in this period, overall male: female ratio was 1.5:1 and the median age of WNV neuroinvasive cases was slightly higher [69 years (IQR: 57–77)] than reported for WNV infection [66 years (interquartile range (IQR): 52–76] [37]. A similar pattern was observed analyzing the distribution of WNV infections reported in North American countries in the period 1999–2020, where outbreaks are reported every 8–10 years [38].
A paper reporting on the data from the Hellenic Centre for Disease Control & Prevention for the period 2010–2019 confirmed that the summer and early autumn months have the highest rates of WNV transmission. Precipitation during 2018, the year with the highest frequency of cases, was extremely high, reaching 500% above climatological values in some cases, as observed in West Attica, contributing to a massive increase of the soil moisture anomaly, particularly in regions, such as West Attica, where weather conditions were favorable for replication of mosquitoes’ population. The authors speculate that high values of precipitation for this time of the year and environmental degradation by wildfires recorded in 2018 favored the expansion of the areas reporting WNV infections in humans [39].
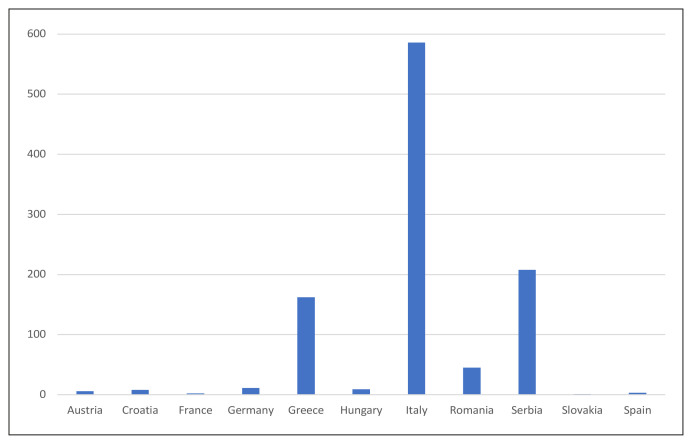
Reports referring to the 2022 season demonstrate an increase of WNV infections in the USA and European countries (Figure 2). As of August 2022, 100 cases of WNV fever were reported to the Centers for Disease Control and Prevention (CDC) in the USA. The latest data reported by the European Centre for Disease Prevention and Control (ECDC) (accessed on 15th January) highlights 1041 human cases, with most of these reported in the Mediterranean area (586 in Italy and 162 in Greece). Other cases were reported from EU-neighboring countries such as Albania, Kosovo, Montenegro, North Macedonia, Serbia, and Turkey, confirming that the current outbreak affects the areas surrounding Mediterranean countries [40]. Further investigations on the ongoing European outbreak demonstrates the rapid spreading of a new lineage of WNV-1, which is suspected to have greater neuroinvasive properties, as suggested by the fact that it is reported more frequently in those with neuroinvasive WNV than in asymptomatic blood donors, as compared to the lineage WNV-2 [41]. Current WNV-1 lineage was detected in 2021 in the Padova province (Veneto region, Italy) where it is reporting a higher prevalence than WNV-2, probably due to warm spring temperatures and prolonged drought, which anticipated WNV amplification and dispersal among a susceptible bird population [42].
Figure 2.
Total number of confirmed human WNV infections in Europe during 2022 season based on ECDC data.
DISCUSSION
We are currently experiencing an era of global warming caused by human activities, which promote climate change. Altered rainfall, flooding and an increased likelihood of extreme weather events are commonly observed and contribute to the expansion of the geographic range and favor the replication of certain vectors. All these events support the potential increase and spread of a range of arboviral threats including WNV [43, 44]. The main reservoirs of WNV are mosquitoes and birds and transmission to mammals has no impact on virus circulation, as the viral load reported in these cases is not sufficient to sustain transmission to vectors. The human disease can be acquired by mosquito’s bite, but transmission by blood transfusion or organ transplantation can occur.
Since two cases of encephalitis were reported in New York City in late august 1999, many cases of WNV infection were diagnosed heralding an outbreak interesting approximately 8,200 patients. Currently, the disease is endemic in many Western countries and the large proportion of patients with a low-symptomatic disease warrant screening for WNV when a blood transfusion or an organ transplantation is planned [38].
In European countries, WNV was sporadically reported until the 1996 outbreak in Romania. Subsequently, after the introduction of WNV-2 in the European Mediterranean area, there was a constant increase in countries reporting WNV isolation from birds, mosquitoes and occasionally mammalians and cases peaked in the period 2012–2013 and in the 2018 season, when cases recorded exceeded the sum of those reported in the period 2010–2017. The exceptionally high temperatures recorded in the Mediterranean area in 2018 and environmental degradation caused by wildfires contributed to the exceptional expansion of the cases [36].
Our systematic review (Table 3) clearly demonstrate that current climate changes are sustaining a global increase of WNV vectors and a change of migratory birds’ routes, which tend more frequently to stand in Northern areas. In these settings, the expansion of Cx. pipiens population favored by drought periods and heavy precipitations sustain an expansion of the number of region where WNV is endemic because of the diffusion of WNV to the resident avian population. This phenomenon involves both urban and rural areas, as was first demonstrated in the 1996 outbreak in Romania [35]. In Europe 315 human cases of WNV infection were observed during the 2020 transmission season, but some countries reporting low numbers of infections had detected higher numbers of human WNV infections (e.g., Austria, Hungary, Serbia, Romania) in previous years, probably due to the herd immunization enhanced by high-level circulation in earlier periods. It is notable that the high temperature favors the selection of mutant strains that can evade host immune response and support WNV outbreak in previously apparently protected areas [45, 46].
Ongoing investigations on a model collecting meteorologic data from New York and Connecticut and on mosquitoes’ diffusion show that an increase in the endemic areas in the USA can be expected in the coming years. This scenario is being observed in Europe, where the introduction of a new WNV-1 lineage caused several cases with many patients experiencing neurologic symptoms.
In conclusion, current climate change is causing an increase of mosquito circulation that supports the widest spread of some vector-borne virus, such as Dengue Virus and Chikungunya virus, previously reported in tropical and sub-tropical countries [47]. Similarly, the spread of WNV is increasing in many countries due to climate change, which create a favorable environment in previously non-permissible areas [48]. This warrants public health measures to control vectors circulation to reduce circulation of WNV and other vector-borne viruses which can cause infections in humans.
Footnotes
Conflict of interest
The authors declare that no conflict of interest exists.
Funding
No funding was received for this paper
REFERENCES
- 1. Petersen LR, Brault AC, Nasci RS. West Nile virus: review of the literature. JAMA. 2013;310(3):308–315. doi: 10.1001/jama.2013.8042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ronca SE, Ruff JC, Murray KO. A 20-year historical review of West Nile virus since its initial emergence in North America: Has West Nile virus become a neglected tropical disease? PLoS Negl Trop Dis. 2021;15(5):e0009190. doi: 10.1371/journal.pntd.0009190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Murray KO, Garcia MN, Rahbar MH, et al. Survival analysis, long-term outcomes, and percentage of recovery up to 8 years post-infection among the houston West Nile Virus Cohort. PLoS One. 2014;9(7):e102953. doi: 10.1371/journal.pone.0102953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shartova N, Mironova V, Zelikhinan S, Korennoy F, Grishchenko M. Spatial patterns of West Nile virus distribution in the Volgograd region of Russia, a territory with long-existing foci. PLoS Negl Trop Dis. 2022;16(1):e0010145. doi: 10.1371/journal.pntd.0010145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Habarugira G, Moran J, Colmant AMG, et al. Mosquito-Independent Transmission of West Nile virus in Farmed Saltwater Crocodiles (Crocodylus porosus] Viruses. 2020;12(2):198. doi: 10.3390/v12020198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vilibic-Cavlek T, Savic V, Petrovic T, et al. Emerging Trends in the Epidemiology of West Nile and Usutu Virus Infections in Southern Europe. Front Vet Sci. 2019;6:437. doi: 10.3389/fvets.2019.00437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Riccetti N, Fasano A, Ferraccioli F, Gomez-Ramirez J, Stilianakis NI. Host selection and forage ratio in West Nile virus-transmitting Culex mosquitoes: Challenges and knowledge gaps. PLoS Negl Trop Dis. 2022;16(10):e0010819. doi: 10.1371/journal.pntd.0010819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hayes EB, Komar N, Nasci RS, Montgomery SP, O’Leary DR, Campbell GL. Epidemiology and Transmission Dynamics of West Nile Virus Disease. Emerg Infect Dis. 2005;11(8):1167–1173. doi: 10.3201/eid1108.050289a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. O’Leary DR, Marfin AA, Montgomery SP, et al. The epidemic of West Nile virus in the United States, 2002. Vector Borne Zoonotic Dis. 2004;4(1):61–70. doi: 10.1089/153036604773083004. [DOI] [PubMed] [Google Scholar]
- 10. Kumar D, Prasad GVR, Zaltzman J, Levy GA, Humar A. Community-acquired West Nile virus infection in solid-organ transplant recipients. Transplantation. 2004;77(3):399–402. doi: 10.1097/01.TP.0000101435.91619.31. [DOI] [PubMed] [Google Scholar]
- 11. Hayes EB, O’Leary DR. West Nile Virus Infection: a pediatric perspective. Pediatrics. 2004;113(3):1375–1381. doi: 10.1542/peds.113.5.1375. [DOI] [PubMed] [Google Scholar]
- 12. Iwamoto M, Jernigan DB, Guasch A, et al. Transmission of West Nile virus from an organ donor to four transplant recipients. N Engl J Med. 2003;348(22):2196–2203. doi: 10.1056/NEJMoa022987. [DOI] [PubMed] [Google Scholar]
- 13. Pagliano P, Boccia G, de Caro F, Esposito S. Bacterial meningitis complicating the course of liver cirrhosis. Infection. 2017;45(6):795–800. doi: 10.1007/s15010-017-1039-7. [DOI] [PubMed] [Google Scholar]
- 14. Pagliano P, Attanasio V, Rossi M, et al. Listeria monocytogenes meningitis in the elderly: Distinctive characteristics of the clinical and laboratory presentation. J Infect. 2015;71(1):134–136. doi: 10.1016/j.jinf.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 15. Lanteri MC, Lee TH, Wen L, et al. West Nile virus nucleic acid persistence in whole blood months after clearance in plasma: Implication for transfusion and transplantation safety. Transfusion (Paris) 2014;54(12):3232–3241. doi: 10.1111/trf.12764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Centers for Disease Control and Prevention (CDC) Transfusion-associated transmission of West Nile virus - Arizona, 2004. MMWR Morb Mortal Wkly Rep. 2004;53(36):842–844. [PubMed] [Google Scholar]
- 17. Centers for Disease Control and Prevention (CDC) Possible dialysis-related West Nile virus transmission-Georgia, 2003. MMWR Morb Mortal Wkly Rep. 2004;53(32):738–739. [PubMed] [Google Scholar]
- 18. Centers for Disease Control and Prevention (CDC) Intrauterine West Nile virus infection - New York, 2002. MMWR Morb Mortal Wkly Rep. 2002;51(50):1135–1136. [PubMed] [Google Scholar]
- 19. Nir Y, Beemer A, Goldwasser RA. West Nile Virus infection in mice following exposure to a viral aerosol. Br J Exp Pathol. 1965;46(4):443–449. [PMC free article] [PubMed] [Google Scholar]
- 20. Centers for Disease Control and Prevention (CDC) West Nile virus infection among turkey breeder farm workers - Wisconsin, 2002. MMWR Morb Mortal Wkly Rep. 2003;52(42):1017–1019. [PubMed] [Google Scholar]
- 21. From the Centers for Disease Control and Prevention. Possible West Nile virus transmission to an infant through breast-feeding-Michigan, 2002. JAMA. 2002;288(16):1976–1977. [PubMed] [Google Scholar]
- 22. Centers for Disease Control and Prevention (CDC) Laboratory-acquired West Nile virus infections - United States, 2002. MMWR Morb Mortal Wkly Rep. 2002;51(50):1133–1135. [PubMed] [Google Scholar]
- 23. Brault AC. Changing patterns of West Nile virus transmission: altered vector competence and host susceptibility. Vet Res. 2009;40(2):43. doi: 10.1051/vetres/2009026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wang G, Minnis RB, Belant JL, Wax CL. Dry weather induces outbreaks of human West Nile virus infections. BMC Infect Dis. 2010;10:38. doi: 10.1186/1471-2334-10-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dohm DJ, O’Guinn ML, Turell MJ. Effect of environmental temperature on the ability of Culex pipiens (Diptera: Culicidae) to transmit West Nile virus. J Med Entomol. 2002;39(1):221–225. doi: 10.1603/0022-2585-39.1.221. [DOI] [PubMed] [Google Scholar]
- 26. Paz S. The West Nile Virus outbreak in Israel (2000) from a new perspective: the regional impact of climate change. Int J Environ Health Res. 2006;16(1):1–13. doi: 10.1080/09603120500392400. [DOI] [PubMed] [Google Scholar]
- 27. Paz S, Albersheim I. Influence of warming tendency on Culex pipiens population abundance and on the probability of West Nile fever outbreaks (Israeli Case Study: 2001–2005) Ecohealth. 2008;5(1):40–48. doi: 10.1007/s10393-007-0150-0. [DOI] [PubMed] [Google Scholar]
- 28. Platonov AE, Fedorova MV, Karan LS, Shopenskaya TA, Platonova OV, Zhuravlev VI. Epidemiology of West Nile infection in Volgograd, Russia, in relation to climate change and mosquito (Diptera: Culicidae) bionomics. Parasitol Res. 2008;103(Suppl 1):S45–53. doi: 10.1007/s00436-008-1050-0. [DOI] [PubMed] [Google Scholar]
- 29. Soverow JE, Wellenius GA, Fisman DN, Mittleman MA. Infectious disease in a warming world: how weather influenced West Nile virus in the United States (2001–2005) Environ Health Perspect. 2009;117(7):1049–1052. doi: 10.1289/ehp.0800487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Harrigan RJ, Thomassen HA, Buermann W, Smith TB. A continental risk assessment of West Nile virus under climate change. Glob Chang Biol. 2014;20(8):2417–2425. doi: 10.1111/gcb.12534. [DOI] [PubMed] [Google Scholar]
- 31. Roiz D, Ruiz S, Soriguer R, Figuerola J. Climatic effects on mosquito abundance in Mediterranean wetlands. Parasit Vectors. 2014;7:333. doi: 10.1186/1756-3305-7-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Marini G, Poletti P, Giacobini M, Pugliese A, Merler S, Rosà R. The role of climatic and density dependent factors in shaping mosquito population dynamics: the case of Culex pipiens in Northwestern Italy. PLoS One. 2016;11(4):e0154018. doi: 10.1371/journal.pone.0154018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Paz S, Malkinson D, Green MS, et al. Permissive summer temperatures of the 2010 European West Nile fever upsurge. PLoS One. 2013;8(2):e56398. doi: 10.1371/journal.pone.0056398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Cotar AI, Falcuta E, Prioteasa LF, Dinu S, Ceianu CS, Paz S. Transmission dynamics of the West Nile Virus in mosquito vector populations under the influence of weather factors in the danube delta, Romania. Ecohealth. 2016;13(4):796–807. doi: 10.1007/s10393-016-1176-y. [DOI] [PubMed] [Google Scholar]
- 35. Savage HM, Ceianu C, Nicolescu G, et al. Entomologic and avian investigations of an epidemic of West Nile fever in Romania in 1996, with serologic and molecular characterization of a virus isolate from mosquitoes. Am J Trop Med Hyg. 1999;61:600–611. doi: 10.4269/ajtmh.1999.61.600. [DOI] [PubMed] [Google Scholar]
- 36.European Centre for Disease Prevention and Control (ECDC) Surveillance atlas of infectious diseases. Stockholm: ECDC; [Accessed: 15th January 2023]. Available from: http://atlas.ecdc.europa.eu/public/index.aspx?Dataset=27&HealthTopic=60. [Google Scholar]
- 37. Barrett ADT. West Nile in Europe: an increasing public health problem. J Travel Med. 2018;25(1):1–2. doi: 10.1093/jtm/tay096. [DOI] [PubMed] [Google Scholar]
- 38.CDC. West Nile Virus. Statistics and maps. [Accessed 15th January 2023]. Available at https://www.cdc.gov/westnile/statsmaps/index.html.
- 39. Mavrakis A, Papavasileiou C, Alexakis D, Papakitsos EC, Salvati L. Meteorological patterns and the evolution of West Nile virus in an environmentally stressed Mediterranean area. Environ Monit Assess. 2021;193(4):227. doi: 10.1007/s10661-021-09011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weekly updates: 2022 West Nile virus transmission season. [Accessed 15th January 2023]. Available at https://www.ecdc.europa.eu/en/west-nile-fever/surveillanceand-disease-data/disease-data-ecdc.
- 41. Barzon L, Pacenti M, Montarsi F, et al. Rapid spread of a new West Nile virus lineage 1 associated with increased risk of neuroinvasive disease during a large outbreak in northern Italy, 2022: One Health analysis. J Travel Med. 2022:taac125. doi: 10.1093/jtm/taac125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Barzon L, Montarsi F, Quaranta E, et al. Early start of seasonal transmission and co-circulation of West Nile virus lineage 2 and a newly introduced lineage 1 strain, northern Italy, June 2022. Euro Surveill. 2022;27(29):2200548. doi: 10.2807/1560-7917.ES.2022.27.29.2200548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hubálek Z, Halouzka J. West Nile fever - a reemerging mosquito - borne viral disease in Europe. Emerg Infect Dis. 1999;5(5):643–650. doi: 10.3201/eid0505.990505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Semenza JC, Rocklöv J, Ebi KL. Climate change and cascading risks from infectious disease. Infect Dis Ther. 2022;11(4):1371–1390. doi: 10.1007/s40121-022-00647-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bakonyi T, Haussig JM. West Nile virus keeps on moving up in Europe. Euro Surveill. 2020;25(46):2001938. doi: 10.2807/1560-7917.ES.2020.25.46.2001938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Fay RL, Ngo KA, Kuo L, Willsey GG, Kramer LD, Ciota AT. Experimental Evolution of West Nile Virus at Higher Temperatures Facilitates Broad Adaptation and Increased Genetic Diversity. Viruses. 2021;13(10):1889. doi: 10.3390/v13101889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Liu-Helmersson J, Brännström Å, Sewe MO, Semenza JC, Rocklöv J. Estimating past, present, and future trends in the global distribution and abundance of the arbovirus vector aedes aegypti under climate change scenarios. Front Public Health. 2019;7:148. doi: 10.3389/fpubh.2019.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Semenza JC, Tran A, Espinosa L, Sudre B, Domanovic D, Paz S. Climate change projections of West Nile virus infections in Europe: implications for blood safety practices. Environ Health. 2016;15(Suppl 1):28. doi: 10.1186/s12940-016-0105-4. [DOI] [PMC free article] [PubMed] [Google Scholar]