Abstract
Objective:
Few data are available to quantify the Clostridioides difficile infection (CDI) burden in U.S. adults depending on Medicaid insurance status.
Methods:
Retrospective cohort study to identify adults coded for CDI from 2011–2017 in MarketScan Commercial and Medicaid (25–64 years) and CMS Medicare (≥65 years) databases. CDI was categorized as healthcare facility (HCA) and community associated (CA). CDI incidence rates were compared by year, insurer, and age group.
Results:
The overall CDI incidence in the elderly was 3.1-fold higher in persons insured by Medicare + Medicaid compared to Medicare only (1,935 vs. 618/100,000 PY), and 2.7-fold higher in younger adults with Medicaid compared to commercial insurance (195 vs. 73/100,000 PY). From 2011–2017 HCA-CDI rates declined in the younger Medicaid population (124.0 to 95.2/100,000 PY, p < 0.001), but were stable in those commercially insured (25.9 to 24.8/100,000 PY, p = 0.33). In the elderly HCA-CDI rates declined from 2011–2017 in the Medicare only (403 to 318/100,000 PY, p < 0.001) and Medicare + Medicaid populations (1,770 to 1,163/100,000 PY, p < 0.002). Persons with chronic medical and those with immunocompromising conditions insured by Medicaid had 2.8-and 2.7-fold higher CDI incidence compared to the commercially insured, respectively. The incidence of CDI was lowest in Medicaid and commercially insured younger adults without chronic medical or immunosuppressive conditions (67.5 and 45.6/100,000 PY, respectively).
Conclusions:
Although HCA CDI incidence decreased from 2011–2017 in elderly and younger adults insured by Medicaid, the burden of CDI remains much higher in low income adults insured by Medicaid.
Clostridioides difficile is the most common cause of healthcare-associated infection and increasingly recognized as an important pathogen in the community.1 Using laboratory data from ten states participating in the Emerging Infections Program (EIP), the Centers for Disease Control and Prevention (CDC) estimates there were over 462,000 cases of C. difficile infection (CDI) in 2017.2 CDI is associated with increased risk for hospitalization, skilled nursing care, long-term care facility transfer, healthcare costs, and death.3–6 Much remains unknown regarding risk for CDI in younger adults, since most studies focus on infection in the elderly. In addition, there are few data about risk of CDI in adults insured by the Medicaid program, who have higher comorbidity burden compared to adults in general.7,8 Better understanding of CDI burden in younger adults and in those insured by Medicaid is needed to develop newer prevention strategies that can be applied to not just the elderly, but also to younger and medically vulnerable adults.9,10
The IBM MarketScan® Commercial and Multi-State Medicaid Databases include inpatient and outpatient medical claims that can be used to study persons <65 years old. The Chronic Condition Warehouse database contains medical claims for persons enrolled in fee-for-service Medicare plans. We used these data to determine CDI incidence based on type of health insurance in U.S. adults from 2011–2017.
METHODS
This study employed a retrospective cohort design using the 2010–2017 Medicare Chronic Condition Warehouse 5% random sample and the IBM® MarketScan® Commercial and Multi-State Medicaid Databases. Eligibility criteria for the MarketScan populations included age 25–64 years and for the Medicare population age 65 and older with Parts A and B fee-for-service and no health maintenance organization enrollment. Persons with continuous enrollment in Medicare but no claims during the study time frame were excluded, to ensure persons were alive and using their health benefits.
Patients coded for CDI from 2011–2017 were identified using ICD-9-CM diagnosis code 008.45 and ICD-10-CM diagnosis codes A04.71 and A04.72 in the Inpatient, Outpatient Services, or Facility Header files (MarketScan), and the Inpatient, Outpatient, Carrier (i.e., physician) or Skilled Nursing Facility files (Medicare). The date of CDI onset was defined as the first date with a coded diagnosis of CDI, unless coding for diarrhea or claims for bacterial stool cultures or C. difficile testing were available to define an earlier onset.11 To avoid misclassification of recurrent CDI as an incident case, at least 84 consecutive days without coding for CDI was required to be eligible for another incident CDI episode.
The MarketScan and Medicare populations were divided into groups based on enrollment in Medicaid (using dual status indicators in the Medicare data). CDI episodes were categorized as healthcare-associated (HCA, including hospital-onset, other facility onset, healthcare facility associated, and indeterminate classification) or community-associated (CA) using standard surveillance definitions,12 as described previously.13 Long-term care facility stay was identified in the Medicare data using the Centers for Medicare & Medicaid Services Minimum Data Set v3.0 assessment of nursing home patients. For the MarketScan data we used a validated algorithm to identify residents of long-term care facilities.14 We categorized CDI as hospitalized if CDI was coded during a hospitalization, or non-hospitalized if CDI was diagnosed and treated solely outside of a hospitalization.
To determine subgroups at higher risk of CDI in the MarketScan population we calculated one-year CDI incidence rates from 2012 to 2017 based on coding for chronic medical, immunocompromising, or neither chronic medical nor immunocompromising conditions in the first year of insurance enrollment beginning in 2011.15,16 Chronic medical and immunosuppressive conditions included those identified as indications for pneumococcal vaccination in non-elderly adults.17 In calculation of CDI incidence, individuals coded for both chronic medical and immunocompromising conditions were counted only in the immunocompromising category.
Statistical Analysis
CDI incidence rates were calculated using all person-years (PY) of observation from 2011–2017 and individually for each year by insurer and by age group. Comparisons of incidence rates by age group and year were performed using PROC Genmod in SAS software (Cary, NC) with Poisson link and offset using log(PY).18 Tests for linear trend were performed using PROC GLM. Comparisons of incidence rates between commercially- and Medicaid-insured individuals were performed using MedCalc Version 20.018 Software (MedCalc Software Ltd., Ostend, Belgium).
The prevalence of chronic medical and immunosuppressive conditions in the MarketScan Medicaid compared to commercial populations was determined using two one-sided t-tests (TOST) in SAS using PROC TTEST. The null hypothesis for the TOST test is that prevalence values are different, and thus a significant result indicates equivalence. We used equivalence ranges of ±2.5% and ±5.0% for conditions with prevalence < 10% and > 10%, respectively.19
RESULTS
From 2011–2017, 78,166 CDI episodes were identified in 71,668 elderly persons in the Medicare data, for an overall incidence of 798/100,000 PY. Of this, 52,242 episodes occurred in persons insured by Medicare only and 25,924 in persons dually insured by Medicare + Medicaid. Approximately 27% of the younger Medicaid population were Black, and in the elderly population 14% of persons insured by Medicare + Medicaid were Black compared to 4.5% of the Medicare only population (Table 1).The overall incidence from 2011–2017 was 618/100,000 PY in persons insured by Medicare alone and 3.1-fold higher (1,935/100,000 PY) in persons dually insured by Medicare + Medicaid (p < 0.001). In the same time period, 102,240 CDI episodes were identified in 90,587 persons aged 25–64 years in the MarketScan Commercial, and 28,024 episodes in 24,047 persons in the Medicaid database. The overall incidence from 2011–2017 in younger adults was 73/100,000 PY in commercially insured and 2.7-fold higher (195/100,000 PY) in those insured by Medicaid (p < 0.001). CDI incidence by year and Medicaid status for the two populations are shown in Supplemental Table 1.
Table 1.
Characteristics of Patients with CDI, 2011–2017, by Medicaid Status
| Characteristic | Commercial 25–64 Years N = 90,587 n (%) |
Medicaid 25–64 Years N = 24,098 n (%) |
Elderly 65+ Years, Medicare Only N = 47,964 n (%) |
Elderly 65+ Years, Medicare + Medicaid N = 23,704 n (%) |
|---|---|---|---|---|
| Age, mean (SD) | 50.2 (10.8) | 47.4 (11.2) | 80.0 (8.2) | 80.2 (8.8) |
| Female Sex | 56,277 (62.1) | 15,171 (63.0) | 30,822 (64.3) | 17,185 (72.5) |
| Race | ||||
| White | N/A | 13,909 (57.7) | 44,725 (93.2) | 18,273 (77.1) |
| Black | N/A | 6,104 (25.3) | 2,140 (4.5) | 3,351 (14.1) |
| Other/Hispanic/Missing | N/A | 4,085 (17.0) | 1,099 (2.3) | 2,080 (8.8) |
| No. CDI Episodes | 102,240 | 28,024 | 52,242 | 25,924 |
| Healthcare associateda | 30,923 | 14,341 | 25,922 | 18,582 |
| Community associated | 64,553 | 11,060 | 21,216 | 5,129 |
| Indeterminateb | 6,764 | 2,623 | 5,104 | 2,213 |
Healthcare associated CDI using the strict definition of HCA (health care facility-onset CDI or community-onset CDI with patient discharged from a healthcare facility in the prior 4 weeks).
Indeterminate CDI was defined as community-onset CDI and patient was discharged from a healthcare facility within the prior 4–12 weeks.
Incidence of Healthcare and Community Associated CDI
HCA-CDI rates declined significantly from 2011–2017 in the MarketScan Medicaid population (124.0 to 95.2/100,000 PY, p = 0.028), but remained stable in the commercially insured population (25.9 to 24.8/100,000 PY, p = 0.85. Figure 1A, Supplemental Table 2). The percentage of CDI cases categorized as HCA decreased from 67.6% to 56.8% in those insured by Medicaid and from 42.5% to 31.6% in the commercially insured (Supplemental Figure 1). In the Medicare population, HCA-CDI rates declined significantly from 2011–2017 in both the Medicare only (403 to 318/100,000 PY, p < 0.001) and Medicare + Medicaid populations (1,770 to 1,163/100,000 PY, p = 0.002, Figure 1B, Supplemental Table 2). CA-CDI rates increased slightly from 2011–2017 In the MarketScan Medicaid population (59.4 to 72.5/100,000 PY, p = 0.14) but more substantially in the commercially insured population (35.0 to 53.7/100,000 PY, p = 0.003, Figure 1C, Supplemental Table 2). CA-CDI rates increased significantly in the Medicare only population (197 to 297/100,000 PY, p < 0.001), but did not change in the Medicare + Medicaid-insured population from 2011–2017 (347 to 358/100,000 PY, p = 0.62, Figure 1D, Supplemental Table 2).
Figure 1.
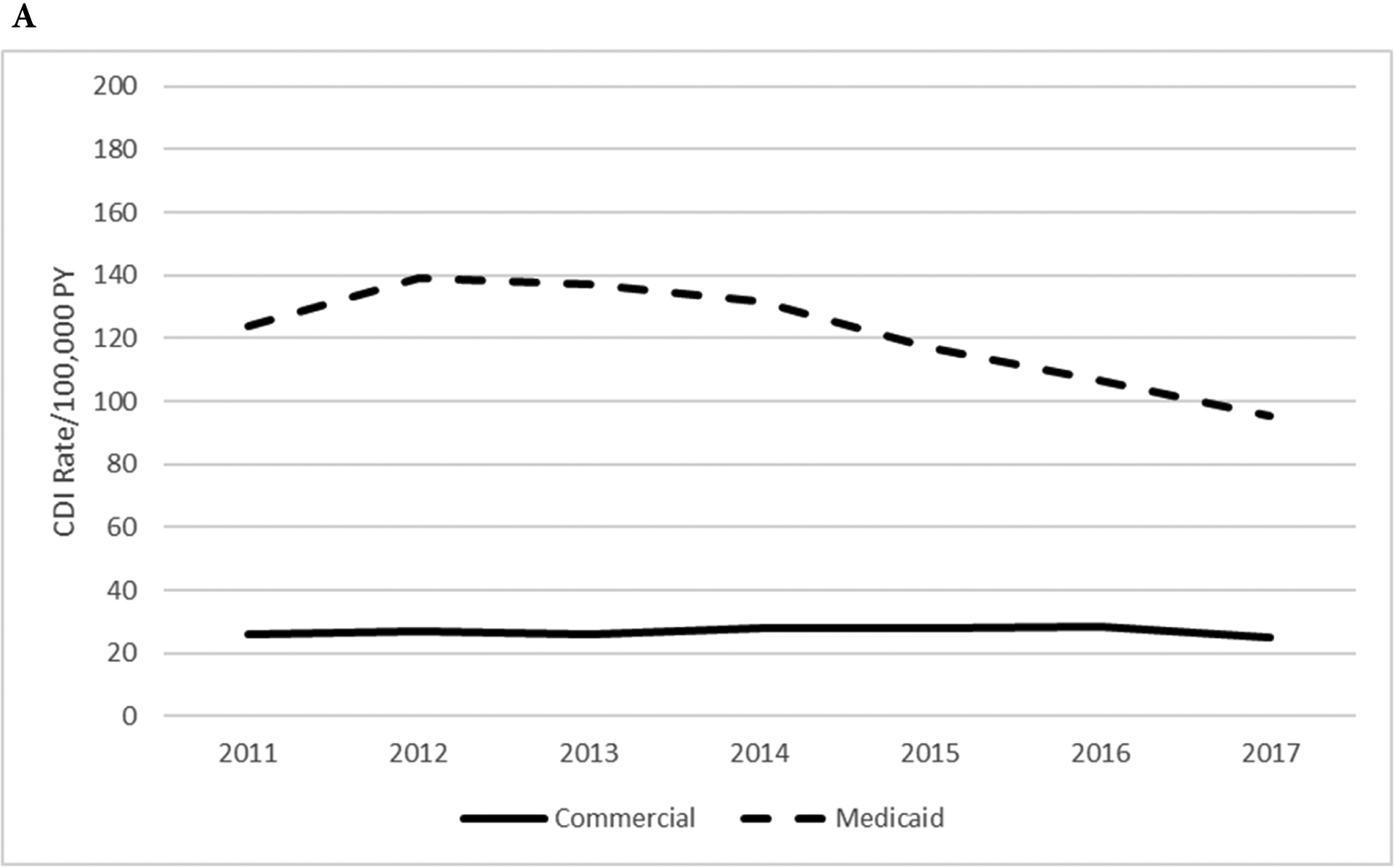
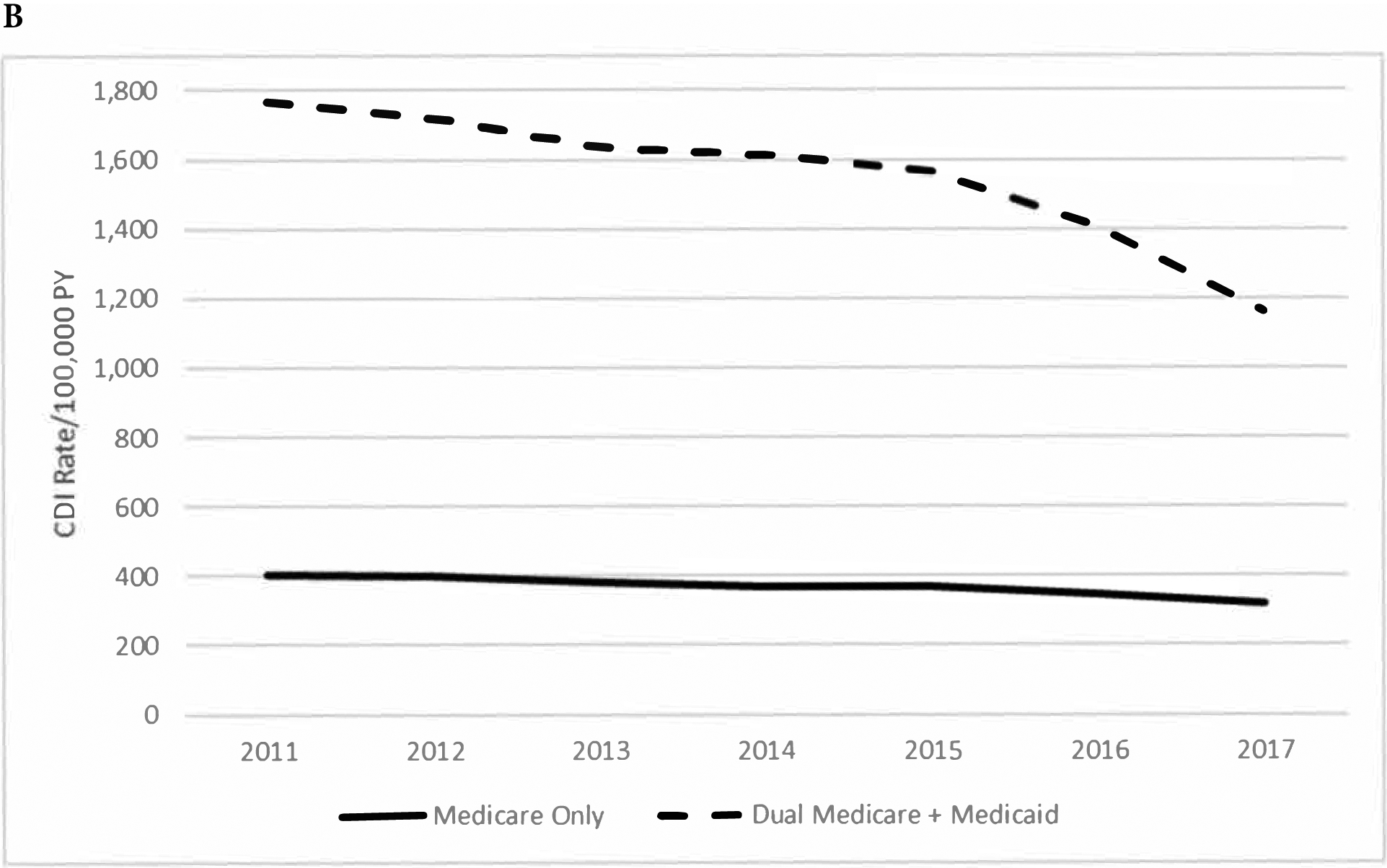
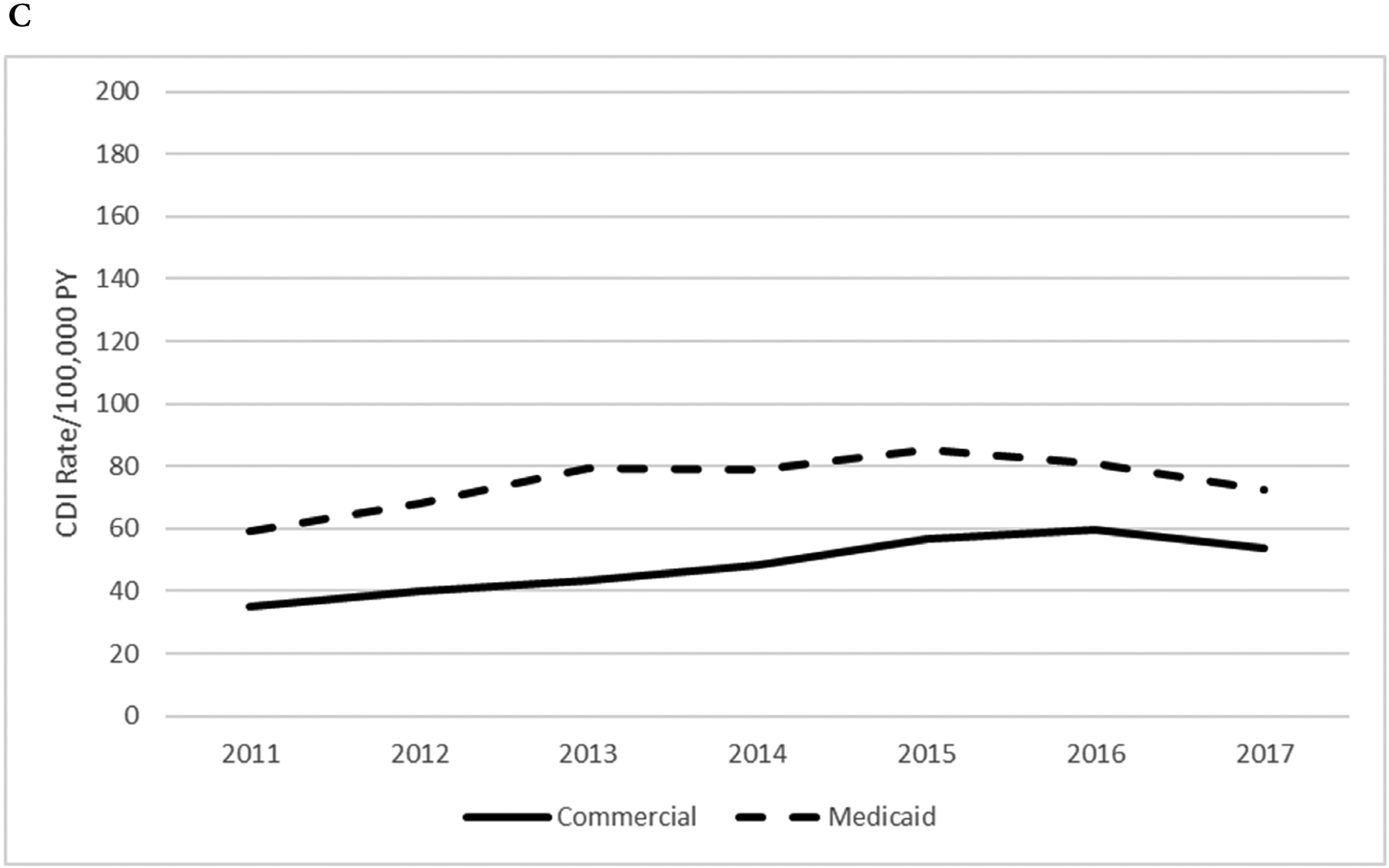
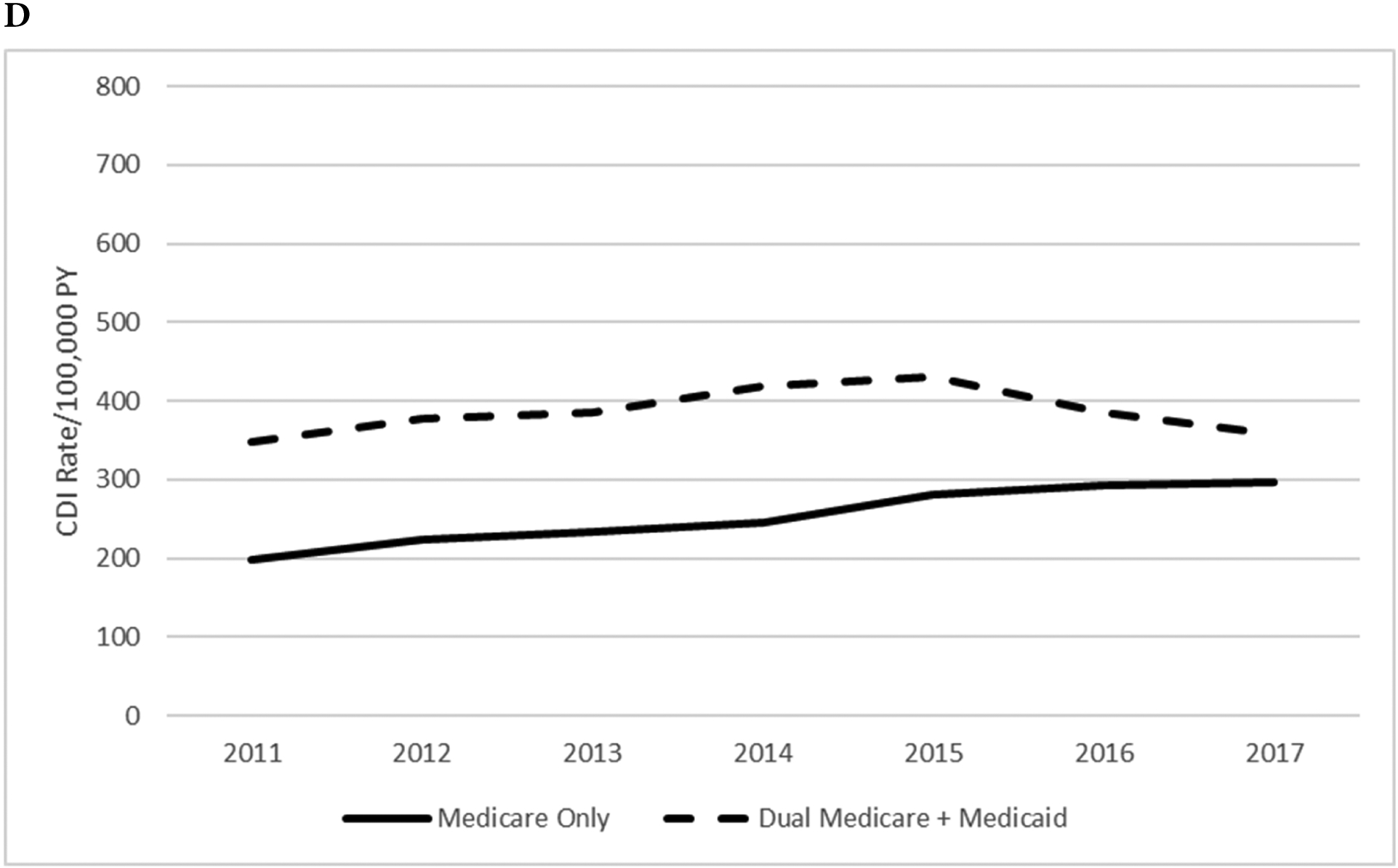
Healthcare Associated and Community Associated CDI Rates/100,000 Person Years of Observation, 2011–2017
A. MarketScan aged 25–64 years, Healthcare associated CDI
B. Medicare aged 65 years and older, Healthcare associated CDI
C. MarketScan aged 25–64 years, Community associated CDI
D. Medicare aged 65 years and older, Community associated CDI
Incidence of Healthcare and Community Associated CDI by Age Group
Incidence rates of HCA from 2011–2017 by age group are shown in Figure 2 and Supplementary Table 3. The incidence of HCA-CDI rose significantly with age in younger and elderly persons insured by Medicaid. The HCA CDI incidence rates were lowest in commercially insured younger adults in all years. The reduction in HCA incidence in those insured by Medicaid from 2011–2017 was most pronounced in the older age groups in both the younger adult (50–64 years) and elderly (75 and older) populations.
Figure 2.
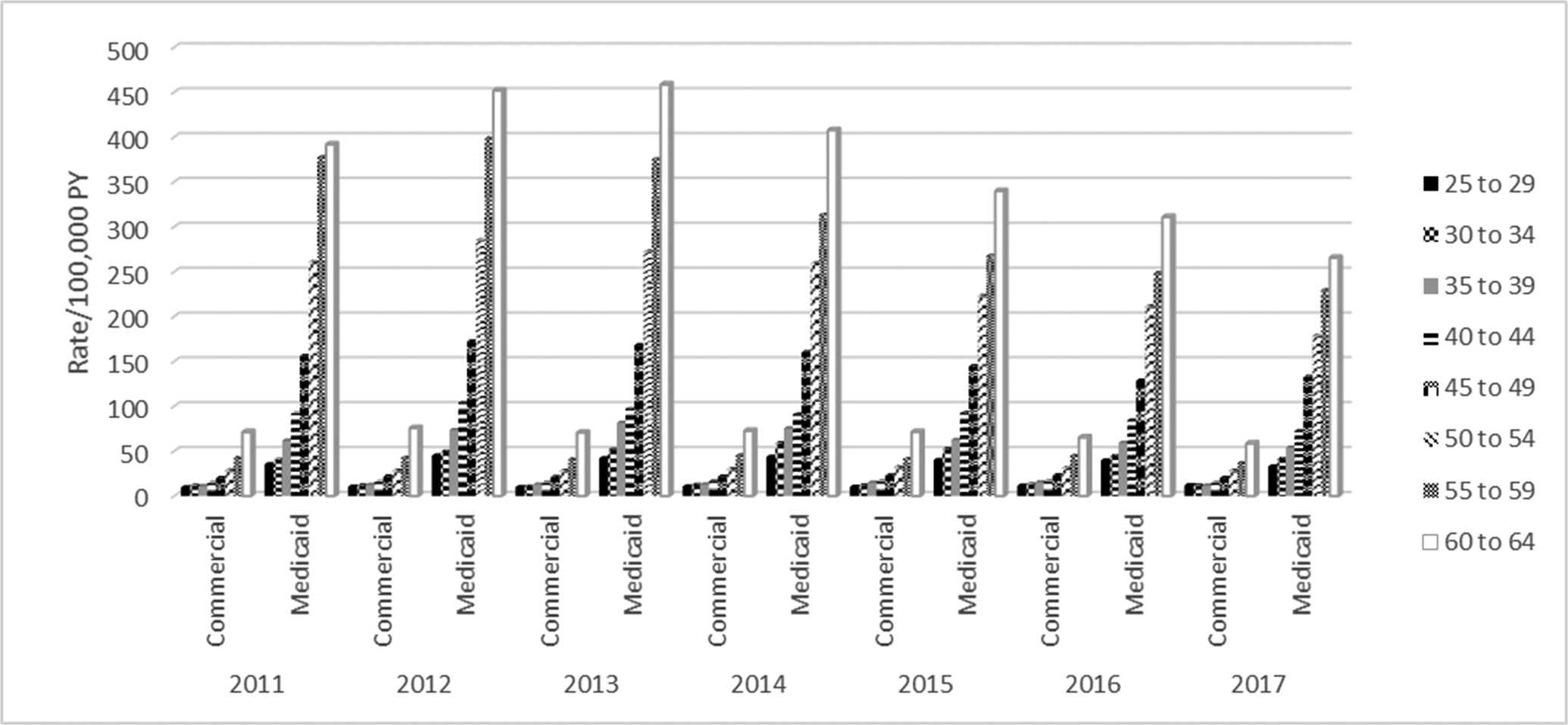
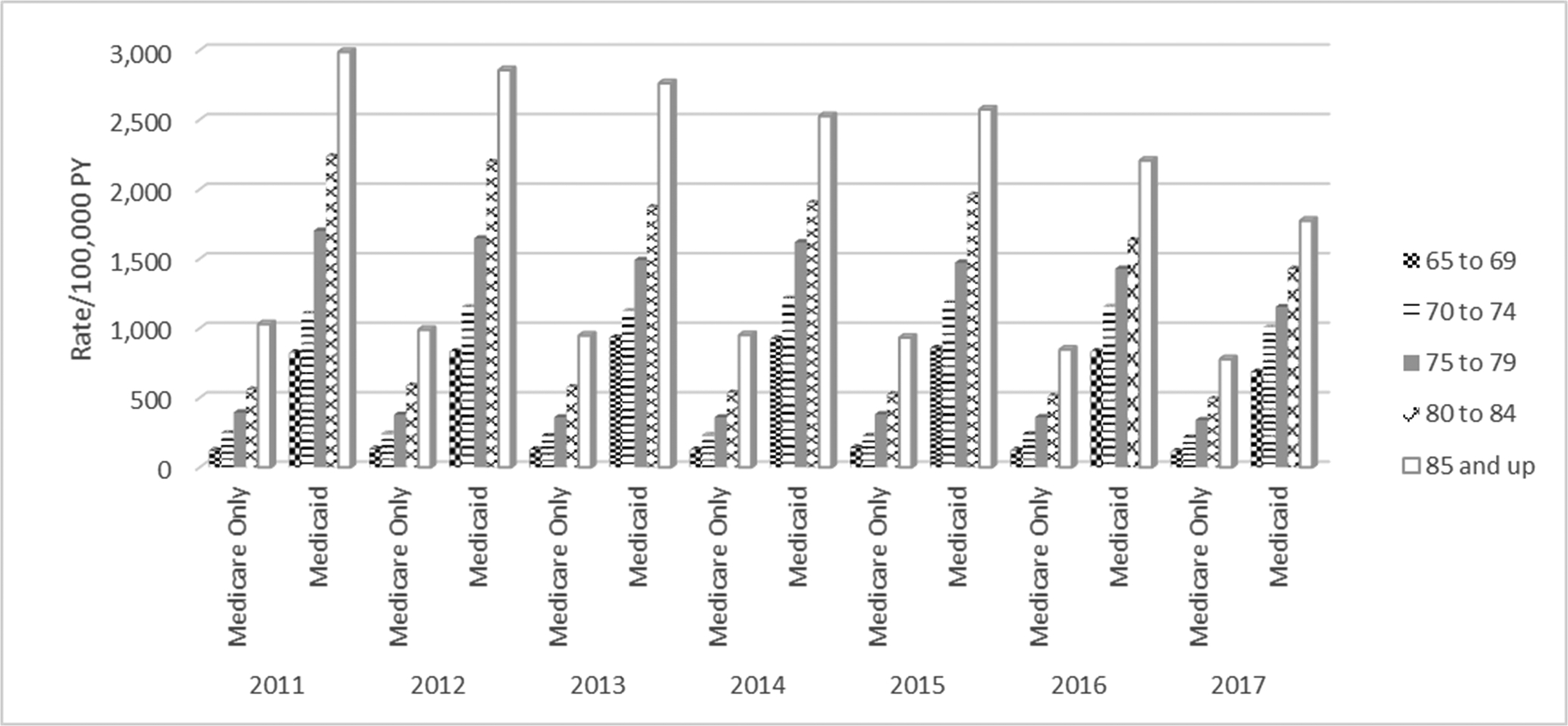
Healthcare Associated CDI Rates, 2011–2017, by Age Group and Insurer
A. MarketScan Aged 25–64 Years B. Medicare Aged 65 Years and Older
Rates of CA-CDI increased with age in younger commercially and Medicaid insured adults and elderly persons insured by Medicare only (Figure 3, Supplemental Table 4). Although CA CDI rates increased with age in older Medicare + Medicaid dually insured adults, the trend of increasing rates with age was not significant from 2014–2016.
Figure 3.
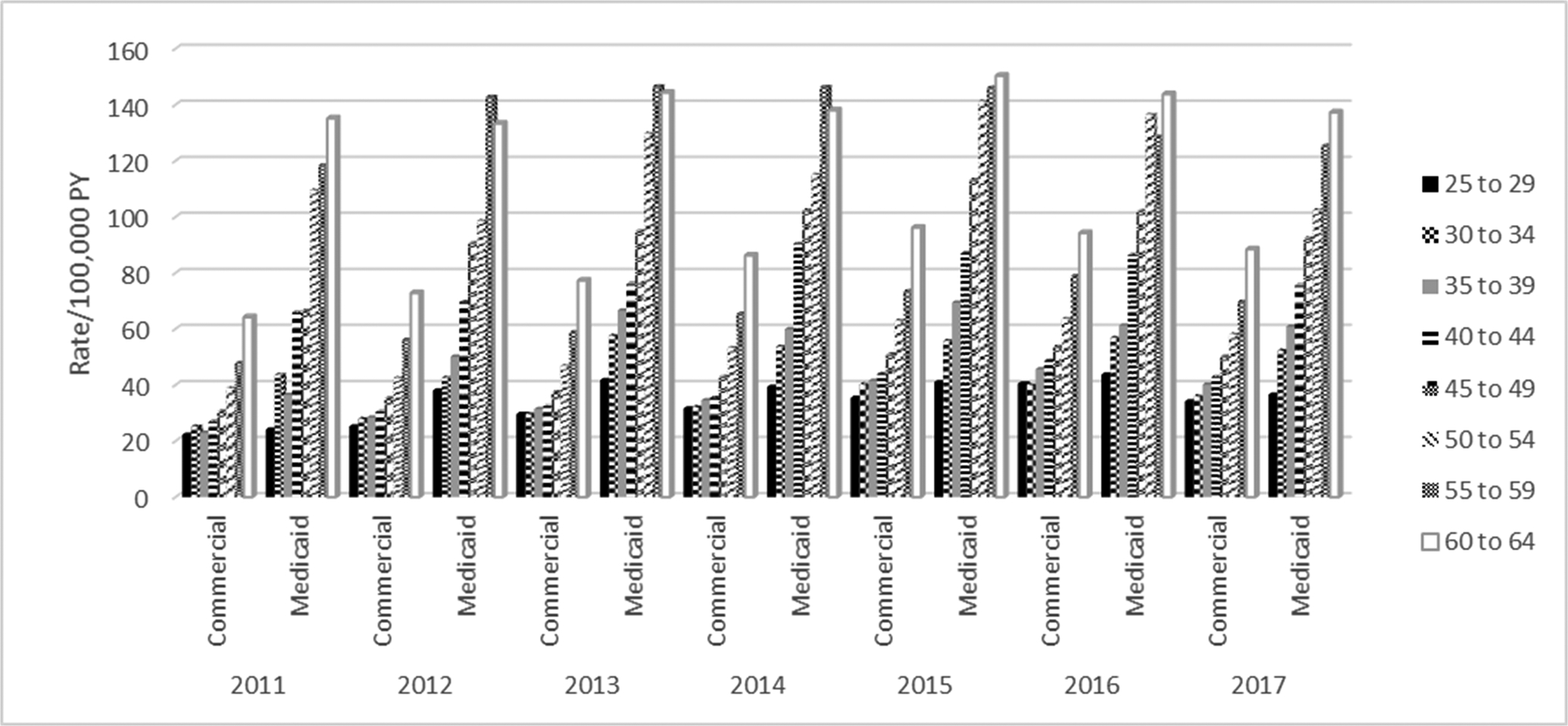
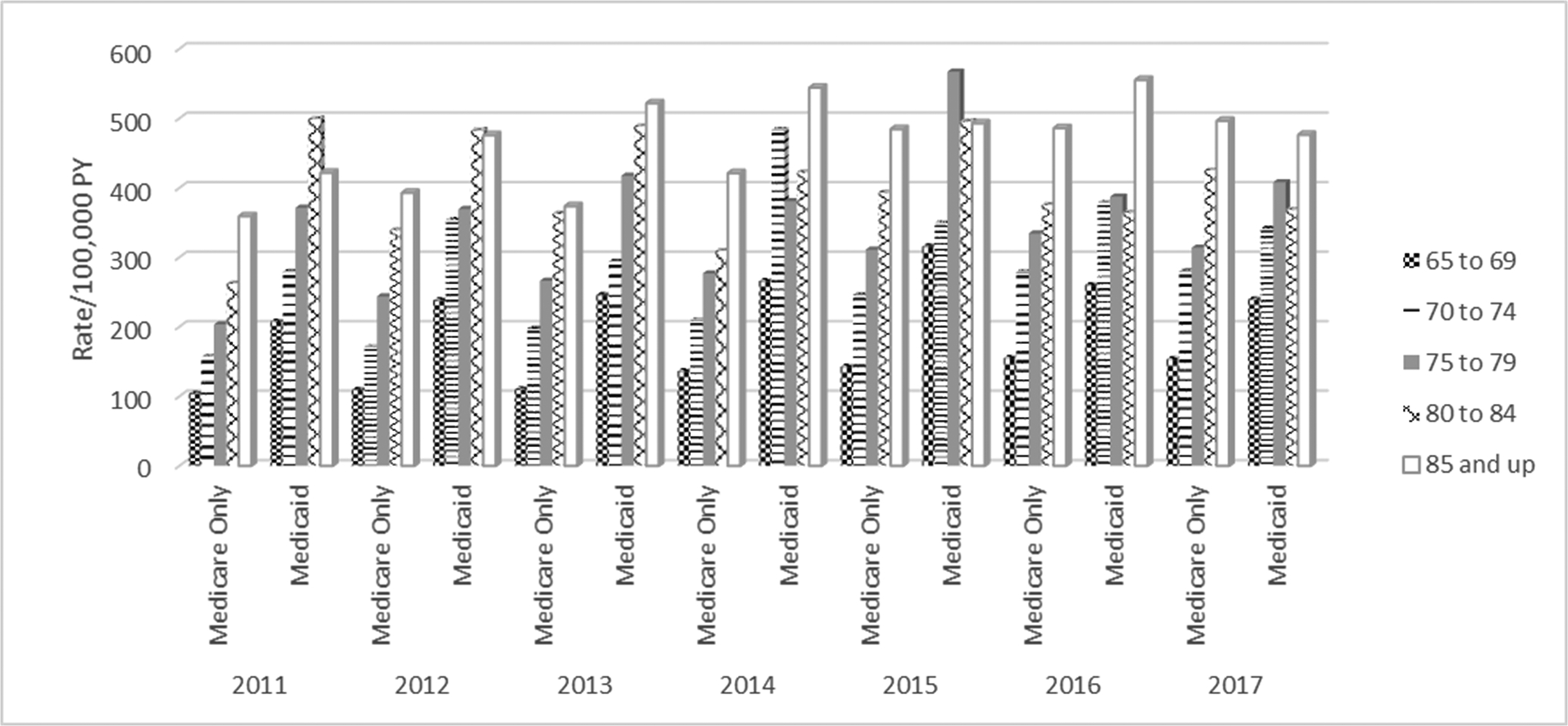
Community Associated CDI Rates, 2011–2017, by Age Group and Insurer
A. MarketScan Aged 25–64 Years B. Medicare Aged 65 Years and Older
Incidence of CDI Treated During a Hospitalization
Rates of CDI treated in-hospital in the younger Medicaid-insured MarketScan population decreased from 151.9 in 2011 to 116.8/100,000 PY in 2017 (p = 0.022). In contrast, rates of CDI treated in-hospital in the commercially insured population were stable from 2011 to 2017 (35.8 to 36.6/100,000 PY, respectively, p = 0.28). In the Medicare + Medicaid population rates of CDI treated in-hospital decreased significantly from 2011–2017 (1,201 to 778/100,000, p = 0.004), while CDI treated in-hospital in the Medicare only population decreased from 363 to 299/100,000 PY during this time frame (p = 0.007, Supplemental Figure 2, Supplemental Table 5).
Incidence of CDI in Younger Adults with and without Chronic Medical and Immunosuppressive Condition
To further investigate disease burden in the younger MarketScan population by payer we determined the prevalence and CDI incidence in persons coded for chronic medical and immunocompromised conditions. For comparison we determined CDI incidence in persons with neither chronic medical nor immunocompromised conditions.
The prevalence of chronic medical conditions was 17.2% in persons aged 25–64 insured by Medicaid compared to 8.6% in the commercially insured (nonequivalent, 5% threshold). The prevalence of immunocompromising conditions was slightly higher but equivalent in persons insured by Medicaid compared to commercially insured (4.7% and 3.6%, respectively). The prevalence of chronic medical conditions increased progressively with age, with prevalence 2.2–2.8-fold higher in the Medicaid compared to commercially insured population (Figure 4). The prevalence of immunocompromising conditions was similar in those aged 25–34 years, but increased with age more in the MarketScan Medicaid compared to commercially insured persons (Medicaid:private prevalence ratios 1.9 and 1.8 in the two older age groups, Figure 4).
Figure 4.
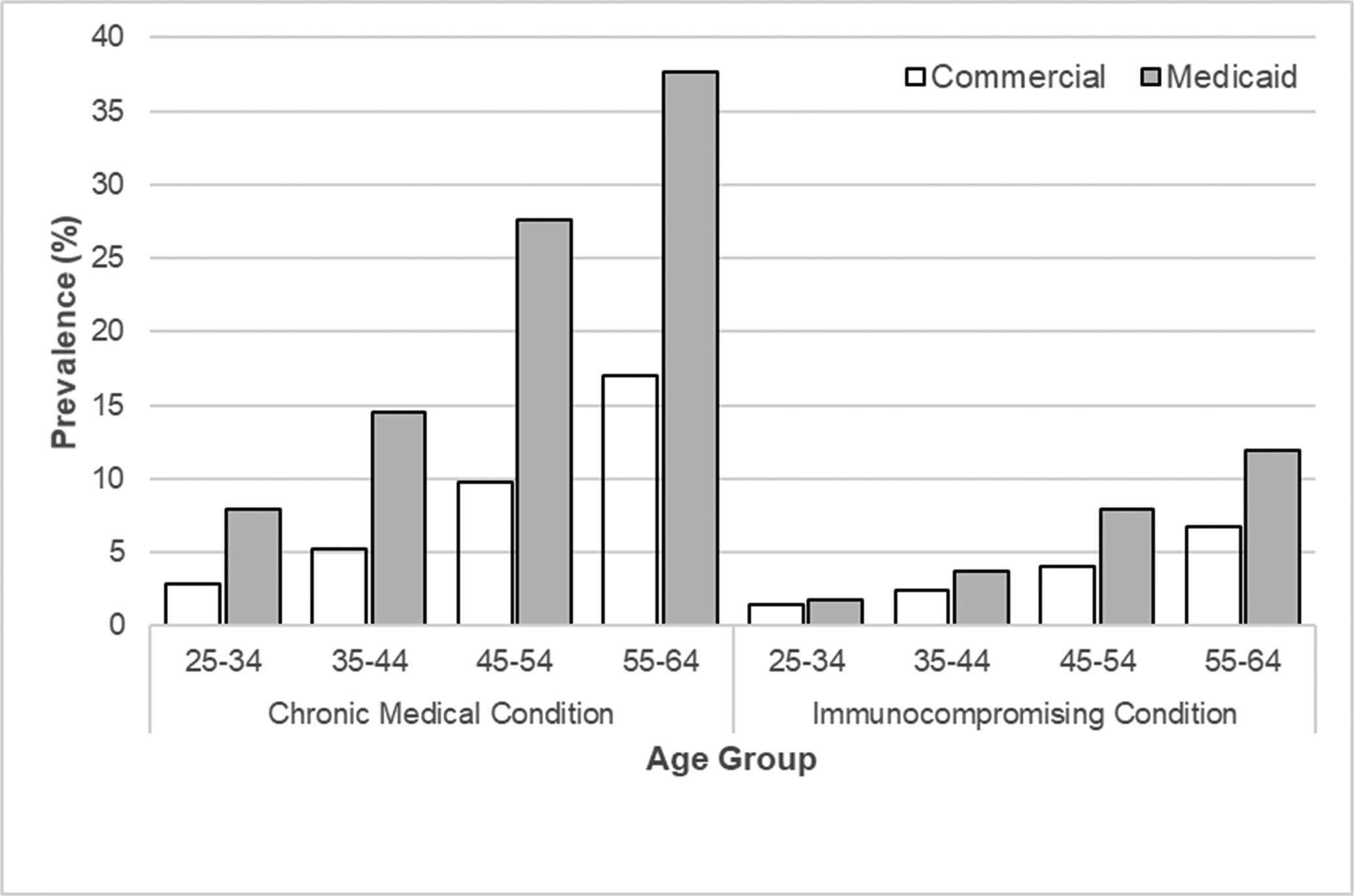
Prevalence of Chronic Medical and Immunocompromising Conditions with Age, MarketScan Aged 25–64 Years
CDI incidence in those with chronic medical conditions was 2.8-fold higher in persons insured by Medicaid compared to commercially insured persons (432.7 vs. 156.1 PY, p < .001, Table 2). Similarly, the incidence of CDI was 2.7-fold higher in persons insured by Medicaid with an immunocompromising condition(s) compared to commercially insured persons (1359.9 vs. 504 PY, p < .001, Table 2). The incidence of CDI was much lower in persons with neither a chronic medical nor immunocompromised condition in both the Medicaid and commercially insured populations (67.6 and 45.6/100,000 PY, respectively). CDI incidence rates for all individual conditions were significantly higher in persons with Medicaid compared to commercial insurance (Table 2).
Table 2.
One-Year Incidence of CDI/100,000 Person-Years from 2012–2017 in Persons with Commercial or Medicaid Health Insurance By Coding for Immunocompetent and Immunocompromising Conditions During their First Year of Enrollmenta
| Commercially Insured | Medicaid Insured | |||||||
|---|---|---|---|---|---|---|---|---|
| Conditions | PY | # of Episodes | Incidence (Episodes/100,000 PY) | PY | # of Episodes | Incidence (Episodes/100,000 PY) | IRR (Medicaid: Commercial) | P |
| Chronic Medical Conditions | ||||||||
| Any chronic medical condition | 2813966.0 | 4393 | 156.1 | 535050.6 | 2315 | 432.7 | 2.8 | <0.001 |
| Chronic lung disease | 723646.3 | 1562 | 215.9 | 239638.8 | 1099 | 458.6 | 2.1 | <0.001 |
| Diabetes | 1619289.6 | 2164 | 133.6 | 223661.9 | 1034 | 462.3 | 3.5 | <0.001 |
| Heart disease | 542857.3 | 1212 | 223.3 | 95301.6 | 615 | 645.3 | 2.9 | <0.001 |
| Alcohol abuse | 98399.1 | 373 | 379.1 | 87704.3 | 547 | 623.7 | 1.6 | <0.001 |
| Liver disease | 93867.8 | 475 | 506.0 | 32572.0 | 364 | 1117.5 | 2.2 | <0.001 |
| Cystic fibrosis | 47305.4 | 88 | 186.0 | 3752.4 | 20 | 533.0 | 2.9 | <0.001 |
| Immunocompromising conditions | ||||||||
| Any immunocompromising condition | 1313330.8 | 6619 | 504.0 | 166340.4 | 2262 | 1359.9 | 2.7 | <0.001 |
| AIDs | 48893.3 | 145 | 296.6 | 16338.4 | 187 | 1144.5 | 3.9 | <0.001 |
| Chronic kidney disease | 95622.1 | 918 | 960.0 | 24917.1 | 483 | 1938.4 | 2.0 | <0.001 |
| End stage renal disease | 28686.1 | 786 | 2740.0 | 6980.9 | 268 | 3839.1 | 1.4 | <0.001 |
| Nephrotic disease | 2397.9 | 15 | 625.5 | 353.1 | 8 | 2265.6 | 3.6 | 0.002 |
| Inflammatory bowel disease | 111345.6 | 1356 | 1217.8 | 10235.6 | 348 | 3399.9 | 2.8 | <0.001 |
| Rheumatoid arthritis/connective tissue disease | 492888.8 | 1291 | 261.9 | 51962.7 | 352 | 677.4 | 2.6 | <0.001 |
| Bone marrow/stem cell transplant | 5108.0 | 184 | 3602.2 | 644.6 | 35 | 5429.5 | 1.5 | 0.025 |
| Solid organ transplant | 28019.6 | 438 | 1563.2 | 1564.1 | 40 | 2557.4 | 1.6 | 0.003 |
| Immunodeficiency | 51754.8 | 1020 | 1970.8 | 17331.9 | 584 | 3369.5 | 1.7 | <0.001 |
| Leukemia | 19413.8 | 307 | 1581.3 | 2039.9 | 63 | 3088.4 | 2.0 | <0.001 |
| Lymphoma | 47858.5 | 539 | 1126.2 | 4721.4 | 92 | 1948.6 | 1.7 | <0.001 |
| Solid tumor | 469804.1 | 1791 | 381.2 | 49455.2 | 579 | 1170.8 | 3.1 | <0.001 |
| Metastatic cancer | 55728.0 | 693 | 1243.5 | 14074.1 | 247 | 1755.0 | 1.4 | <0.001 |
| Radiotherapy | 74112.7 | 572 | 771.8 | 17617.8 | 224 | 1271.4 | 1.6 | <0.001 |
| No Chronic Medical Conditions And No Immunocompromised Conditions | 32662276.6 | 14904 | 45.6 | 3006447.5 | 2033 | 67.6 | 1.5 | <0.001 |
The first year of enrollment in the Commercial or Medicaid Database, 2011–2017.
All comparisons of incidence rates between Commercially- and Medicaid-insured persons were significant with p < 0.001, except cystic fibrosis (p = 0.0253) and nephrotic syndrome (p = 0.0016).
CDI incidence in persons with chronic medical conditions increased significantly with age (p = 0.002 in commercially-insured and p < 0.001 in the Medicaid-insured), although CDI incidence in all ages was higher in the Medicaid- than commercially-insured population (ranging from 2.3–3.6-fold, Figure 5). In contrast, CDI incidence in those with immunocompromised conditions increased slightly with age in the Medicaid population (p = 0.05) but was stable with increasing age in those commercially-insured (p = 0.70). As with chronic medical conditions, the incidence of CDI was much higher in Medicaid compared to commercially-insured persons with immunocompromised conditions in all age groups (ranging from 2.0–3.2-fold). Although CDI incidence increased with age in both commercially and Medicaid-insured persons with neither chronic medical nor immunocompromising conditions (both p < .001), the incidence rate ratio in those aged 60–64 vs. 25–29 years was greater in those insured by Medicaid (3.7) than commercially insured (2.5, Figure 5).
Figure 5.
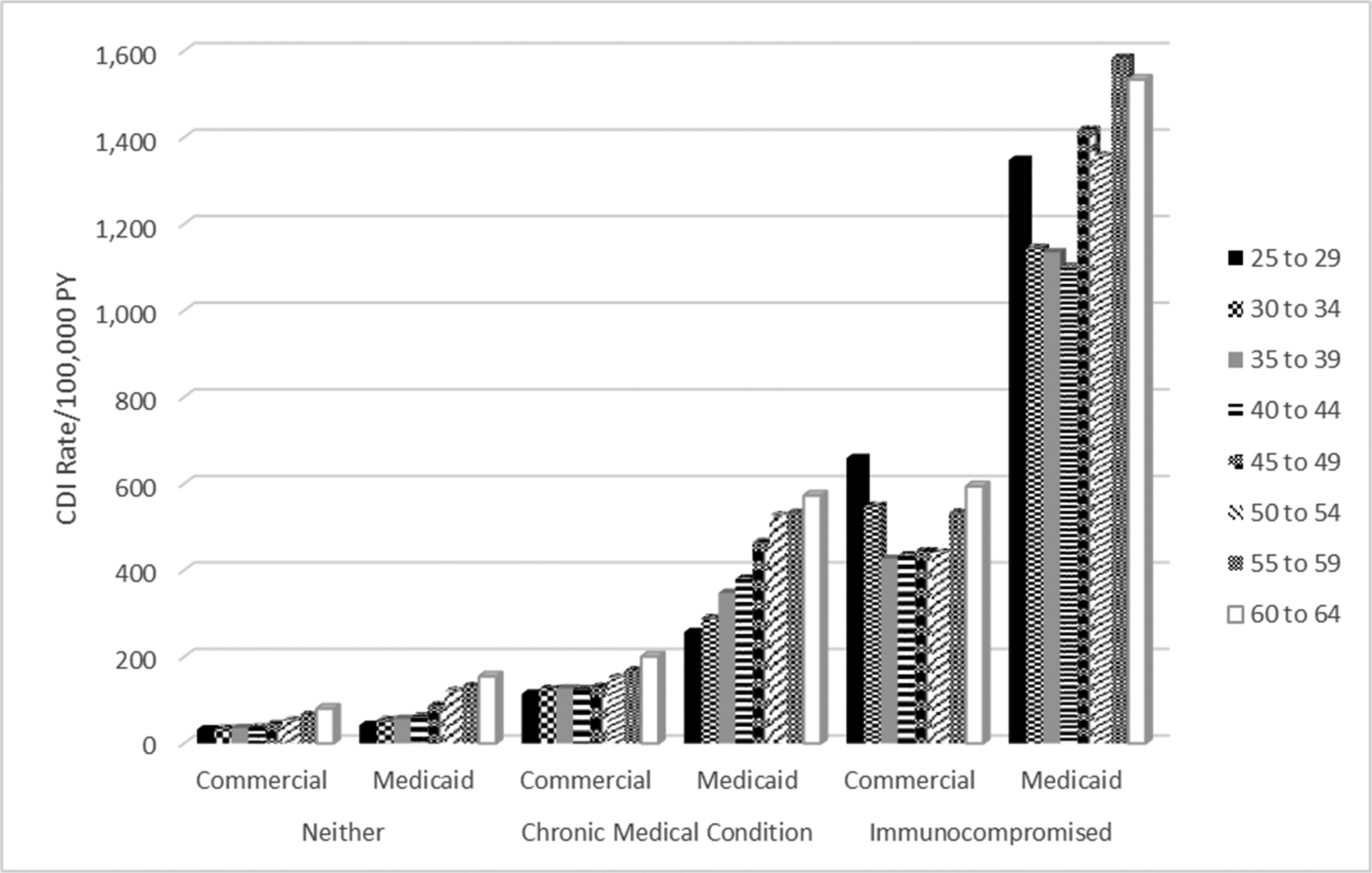
One-Year Incidence of CDI/100,000 Person Years from 2012 to 2017 Based on Prevalence of Chronic Medical Conditions, Immunocompromised Conditions, and Neither Conditions in the MarketScan Commercial and Medicaid Populations by Age Group
DISCUSSION
In this study we found that the overall burden of CDI from 2011–2017 was 3-fold higher in lower-income U.S. elderly persons dually insured by Medicare + Medicaid compared to elderly persons insured by Medicare only, and 2.7-fold higher in the younger population of Medicaid recipients compared to those privately insured. The yearly incidence of CDI declined substantially in elderly persons insured by Medicare + Medicaid, with a smaller decline in younger persons insured by Medicaid, due to decreases in HCA CDI. Similarly, rates of CDI resulting in a hospitalization declined by approximately one-third from 2011–2017 in both younger and elderly persons insured by Medicaid, with a smaller decrease in older persons insured by Medicare only. In younger commercially insured and elderly persons with Medicare insurance only, CA CDI rates increased about 50% from 2011–2017. CA-CDI incidence also increased about 20% in younger adults with Medicaid insurance, but remained relatively stable in the elderly insured by both Medicare + Medicaid.
Higher risk of CDI in elderly persons dually insured with Medicaid, an indicator of low socioeconomic status, has been reported previously.3 Using New Mexico EIP data, Hudspeth found higher incidence of community-acquired CDI in census tracts with a higher proportion of uninsured persons and in Black and American Indian/Native Alaskan men and women.20 Using 2014–2015 EIP data Skrobarcek found higher CA-CDI rates in lower-income U.S. census tracts and in tracts with a higher percentage of persons publically insured.21 Our work expands on these findings by demonstrating higher risk of CDI in both younger and elderly persons insured by Medicaid, including higher risk of HCA CDI across the age span in persons insured by Medicaid.
To investigate the higher CDI burden in younger adults insured by Medicaid, we determined the prevalence of chronic medical and immunocompromising conditions. We found the prevalence of chronic medical conditions was almost three-fold higher in adults aged 25–54 insured by Medicaid compared to those commercially insured, and the prevalence of immunocompromising conditions was almost 2-fold higher in Medicaid-insured adults aged 45–64 compared to those commercially insured. This is consistent with prior findings that more than 50% of non-elderly adults insured by Medicaid have at least one chronic condition, which is higher than the overall burden of chronic conditions in all adults (including the elderly).7,8 In analyses of CDI burden we found that the incidence of CDI was almost 3-fold higher in Medicaid-insured younger adults with a chronic medical condition(s) or with an immunocompromising condition compared to commercially insured adults. Medicaid- and commercially-insured younger adults without a chronic medical or immunocompromising condition had much lower incidence of CDI. The incidence of CDI increased substantially with age in persons with chronic medical conditions, especially in the Medicaid population. The finding of increased burden of CDI in persons with immunocompromising conditions is not surprising, since it is known that persons with diseases such as leukemia/lymphoma, end-stage renal disease, and others are at high risk of CDI.22,23 We speculate that the increased burden of CDI in persons with chronic medical conditions, particularly those insured by Medicaid, is likely due to high exposure to antibiotics. Antibiotic utilization is higher in persons with some chronic medical conditions (e.g., diabetes, chronic kidney disease, chronic lung disease, including asthma) than in persons without those conditions,23–26 even in the absence of documented infection.27 The increased antibiotic exposure could explain the increased CDI incidence in these persons, particularly in comparison to those without a chronic medical or immunocompromising condition.
During the same time period as our study, the CDC EIP surveillance reported a decrease in HCA CDI from 93 to 67/100,000 persons, and corresponding increase in CA CDI (from 48 to 63/100,000 persons).2 A similar increase in CA CDI occurred in Quebec from 2008 to 2015.28 Consistent with the reported increase in CA CDI, the proportion of community acquired CDI in patients admitted to a Southeastern network hospital increased from 49% in 2013 to 61% in 2017.29 The percentage of CDI categorized as CA also increased in Veteran’s Administration patients aged 18–64 years, ranging from 41% in 2011 to 56% in 2016, with higher CA proportions in younger compared to older veterans.30
We found that the decrease in overall CDI incidence during this time period in persons insured by Medicaid was due to decrease in HCA CDI. In the Medicare-only population the decline in HCA rates from 2011 to 2017 was offset by the increase in CA CDI incidence, such that the overall CDI incidence increased slightly. Among persons insured by Medicaid, the decreases in HCA CDI incidence were most pronounced in the oldest age groups (50–64 years in the younger population and 75 years and older in the elderly). Similarly, we found that the incidence of CDI treated during a hospitalization decreased significantly in persons insured by Medicaid from 2011 to 2017 in both the younger population and elderly dually insured by Medicaid + Medicare, but changed only slightly for commercially and Medicare-only insured individuals.
The observed decrease in HCA CDI rates may be due in part to implementation of antibiotic stewardship programs in U.S. hospitals. By 2017 76% of acute care hospitals reported meeting the CDC’s core stewardship elements, compared to 41% in 2014.31,32 Several investigators have found an association of antibiotic stewardship programs with decreased hospital-onset CDI,33–35 which may explain the decrease we and others noted in HCA CDI in recent years. In contrast, antibiotic stewardship programs have gained much less traction in the outpatient setting,36,37 despite the fact that the majority of antibiotics are prescribed in ambulatory settings and an estimated 30–50% of these antibiotic prescriptions are considered inappropriate.27,38 We speculate that the increased CA CDI rates, particularly in younger commercially insured and older persons with only Medicare coverage, may be due to continued over-utilization of antibiotics in the community, in addition to increasing use of nucleic acid amplification tests (NAAT), associated with increased CDI test positivity when used as a single test.39 Although NAATs have been increasingly used for CDI testing in hospitals, the widespread implementation of antibiotic stewardship and also diagnostic stewardship programs may have indirectly resulted in less testing for CDI in hospitalized patients,40,41 contributing to the decrease in HCA rates observed in our study and by others.
Limitations of our study were the identification of CDI using ICD-9/10 diagnosis codes, which may result in inaccuracy, lack of information on antibiotic utilization in hospitals, and incomplete availability of outpatient prescriptions. The similarity of our overall calculated CDI incidence rates to those reported by the EIP system suggests that inaccuracy in CDI identification based on diagnosis codes was likely minimal. Our analyses of CDI incidence in the elderly was restricted to the fee-for-service population, and thus may not be generalizable to the elderly insured by Medicare Advantage plans.
The finding of higher risk in Medicaid-insured younger adults with underlying chronic medical conditions and in both commercially and Medicaid-insured younger adults with immunocompromising conditions is particularly important, suggesting heightened awareness of CDI risk and increased emphasis on appropriate utilization of antibiotics are needed in these medically vulnerable persons. Additional broad-based strategies to prevent CDI, including vaccination, are urgently needed to prevent morbidity and mortality, particularly in lower income persons.
Supplementary Material
Key Points:
The incidence of Clostridioides difficile infection in US adults was significantly higher in persons insured by Medicaid compared to non-Medicaid plans. The incidence of healthcare facility associated CDI decreased from 2011–2017, particularly in persons insured by Medicaid.
ACKNOWLEDGEMENTS
FUNDING:
This work was supported by Pfizer, Inc. The sponsor participated in study design, interpretation of the data and final review of the manuscript. Access to data and additional services were provided by the Washington University Center for Administrative Data Research, supported in part by grant UL1 TR002345 from the National Center for Advancing Translational Sciences of the National Institutes for Health.
POTENTIAL CONFLICTS OF INTEREST
Margaret A. Olsen: Dr. Olsen reports receipt of grant funding from Pfizer in the past 36 months and personal fees from Pfizer for consulting work.
Dustin Stwalley: Mr. Stwalley reports stock ownership in Abbvie, Inc. and Bristol-Myers Squibb.
Erik R. Dubberke: Dr. Dubberke reports receipt of grant funding from Pfizer, Synthetic Biologics, and Ferring in the past 36 months and personal fees from Ferring, Rebiotix, Summit, Merck, Pfizer, and Seres.
Holly Yu: Ms. Yu is an employee of Pfizer, Inc.
None of the other authors report any conflicts of interest.
Footnotes
Preliminary results of this study were presented at the 31st European Congress of Clinical Microbiology and Infectious Diseases (ECCMID), July 9–12, 2021.
REFERENCES
- 1.Magill SS, Edwards JR, Bamberg W, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med 2014;370:1198–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guh AY, Mu Y, Winston LG, et al. Trends in U.S. Burden of Clostridioides difficile Infection and Outcomes. N Engl J Med 2020;382:1320–1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Olsen MA, Stwalley D, Demont C, Dubberke ER. Clostridium difficile infection increases acute and chronic morbidity and mortality. Infect Control Hosp Epidemiol 2019;40:65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nanwa N, Kwong JC, Krahn M, et al. The Economic Burden of Hospital-Acquired Clostridium difficile Infection: A Population-Based Matched Cohort Study. Infect Control Hosp Epidemiol 2016;37:1068–1078. [DOI] [PubMed] [Google Scholar]
- 5.Nanwa N, Sander B, Krahn M, et al. A population-based matched cohort study examining the mortality and costs of patients with community-onset Clostridium difficile infection identified using emergency department visits and hospital admissions. PLoS One 2017;12:e0172410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwon JH, Olsen MA, Dubberke ER. The morbidity, mortality, and costs associated with Clostridium difficile infection. Infect Dis Clin North Am 2015;29:123–134. [DOI] [PubMed] [Google Scholar]
- 7.Chapel JM, Ritchey MD, Zhang D, Wang G. Prevalence and Medical Costs of Chronic Diseases Among Adult Medicaid Beneficiaries. Am J Prev Med 2017;53(6s2):S143–S154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boersma PBL, Ward BW. Prevalence of Multiple Chronic Conditions Among US Adults, 2018. Prev Chronic Dis 2020;17:200130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guh AY, Adkins SH, Li Q, et al. Risk Factors for Community-Associated Clostridium difficile Infection in Adults: A Case-Control Study. Open Forum Infect Dis 2017;4:ofx171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Czepiel J, Drozdz M, Pituch H, et al. Clostridium difficile infection: review. Eur J Clin Microbiol Infect Dis 2019;38:1211–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dubberke ER, Olsen MA, Stwalley D, et al. Identification of Medicare Recipients at Highest Risk for Clostridium difficile Infection in the US by Population Attributable Risk Analysis. PLoS One 2016;11:e0146822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen SH, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA) Infect Control Hosp Epidemiol. 2010;31:431–455. [DOI] [PubMed] [Google Scholar]
- 13.Olsen MA, Young-Xu Y, Stwalley D, et al. The burden of clostridium difficile infection: estimates of the incidence of CDI from U.S. Administrative databases. BMC Infect Dis 2016;16:177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yun H, Kilgore ML, Curtis JR, et al. Identifying types of nursing facility stays using Medicare claims data: an algorithm and validation. Health Serv Outcomes Res Method 2010;10:100–110. [Google Scholar]
- 15.Elixhauser A, Steiner C, Harris DR, Coffey RN. Comorbidity measures for use with administrative data. Med Care 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- 16.Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol 2000;53:1258–1267. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Recommended Adult Immunization Schedule, United States, 2019. https://www.cdc.gov/vaccines/schedules/downloads/adult/adult-combined-schedule.pdf. Accessed October 19, 2020.
- 18.Chu X Using SAS to Calculate Incidence and Prevalence Rates in a Dynamic Population. 2012. https://www.lexjansen.com/wuss/2012/103.pdf. Accessed December 10, 2021.
- 19.Tatem KS, Romo ML, McVeigh KH, et al. Comparing Prevalence Estimates From Population-Based Surveys to Inform Surveillance Using Electronic Health Records. Prev Chronic Dis 2017;14:E44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hudspeth WB, Qeadan F, Phipps EC. Disparities in the incidence of community-acquired Clostridioides difficile infection: An area-based assessment of the role of social determinants in Bernalillo County, New Mexico. Am J Infect Control 2019;47:773–779. [DOI] [PubMed] [Google Scholar]
- 21.Skrobarcek KA, Mu Y, Ahern J, et al. Association between Socioeconomic Status and Incidence of Community-Associated Clostridioides difficile Infection - United States, 2014–2015. Clin Infect Dis 2021;73:722–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Werkhoven CH, van der Tempel J, Jajou R, et al. Identification of patients at high risk for Clostridium difficile infection: development and validation of a risk prediction model in hospitalized patients treated with antibiotics. Clin Microbiol Infect 2015;21:786–788. [DOI] [PubMed] [Google Scholar]
- 23.Ramesh MS, Yee J. Clostridioides difficile Infection in Chronic Kidney Disease/End-Stage Renal Disease. Adv Chronic Kidney Dis 2019;26:30–34. [DOI] [PubMed] [Google Scholar]
- 24.Mor A, Berencsi K, Nielsen JS, et al. Rates of Community-based Antibiotic Prescriptions and Hospital-treated Infections in Individuals With and Without Type 2 Diabetes: A Danish Nationwide Cohort Study, 2004–2012. Clin Infect Dis 2016;63:501–511. [DOI] [PubMed] [Google Scholar]
- 25.Kim EJ, Ha KH, Kim DJ, Choi YH. Diabetes and the Risk of Infection: A National Cohort Study. Diabetes Metab J 2019;43:804–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chang CH, Fan PC, Kuo G, et al. Infection in Advanced Chronic Kidney Disease and Subsequent Adverse Outcomes after Dialysis Initiation: A Nationwide Cohort Study. Sci Rep 2020;10:2938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of Inappropriate Antibiotic Prescriptions Among US Ambulatory Care Visits, 2010–2011. JAMA 2016;315:1864–1873. [DOI] [PubMed] [Google Scholar]
- 28.Zanichelli V, Garenc C, Villeneuve J, et al. Increased Community-Associated Clostridioides difficile Infections in Quebec, Canada, 2008–2015(1). Emerg Infect Dis 2020;26:1291–1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Turner NA, Grambow SC, Woods CW, et al. Epidemiologic Trends in Clostridioides difficile Infections in a Regional Community Hospital Network. JAMA Netw Open 2019;2:e1914149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Russo EM, Kuntz J, Yu H, et al. Incidence of Clostridioides difficile infections among young and middle-aged adults: Veterans Health Administration. Infect Control Hosp Epidemiol 2019;40:997–1005. [DOI] [PubMed] [Google Scholar]
- 31.Pollack LA, van Santen KL, Weiner LM, Dudeck MA, Edwards JR, Srinivasan A. Antibiotic Stewardship Programs in U.S. Acute Care Hospitals: Findings From the 2014 National Healthcare Safety Network Annual Hospital Survey. Clin Infect Dis 2016;63:443–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Neuhauser M Antibiotic Stewardship: Optimizing Antibiotic Use in Inpatient Setting. Annual NHSN Training – March 29, 2019; https://www.cdc.gov/nhsn/pdfs/training/2019/antibiotic-stewardship-508.pdf. Accessed June 11, 2022. [Google Scholar]
- 33.Morgan F, Belal M, Lisa B, Ford F, LeMaitre B, Psevdos G. Antimicrobial stewardship program achieved marked decrease in Clostridium difficile infections in a Veterans Hospital. Am J Infect Control 2020;48:1119–1121. [DOI] [PubMed] [Google Scholar]
- 34.Gaffin N, Spellberg B. Sustained reductions in unnecessary antimicrobial administration and hospital Clostridioides difficile rates via stewardship in a nonacademic setting. Infect Control Hosp Epidemiol 2021:1–3. [DOI] [PubMed] [Google Scholar]
- 35.Tamma PD, Miller MA, Dullabh P, et al. Association of a Safety Program for Improving Antibiotic Use With Antibiotic Use and Hospital-Onset Clostridioides difficile Infection Rates Among US Hospitals. JAMA Netw Open 2021;4:e210235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eudy JL, Pallotta AM, Neuner EA, et al. Antimicrobial Stewardship Practice in the Ambulatory Setting From a National Cohort. Open Forum Infect Dis 2020;7:ofaa513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Trusts TPC. National Survey Reveals Barriers to Outpatient Antibiotic Stewardship Efforts. 2020.
- 38.Sanchez GV, Fleming-Dutra KE, Roberts RM, Hicks LA. Core Elements of Outpatient Antibiotic Stewardship. MMWR Recomm Rep 2016;65:1–12. [DOI] [PubMed] [Google Scholar]
- 39.Polage CR, Gyorke CE, Kennedy MA, et al. Overdiagnosis of Clostridium difficile Infection in the Molecular Test Era. JAMA Int Med 2015;175:1792–1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kang M, Abeles SR, El-Kareh R, et al. The Effect of Clostridioides difficile Diagnostic Stewardship Interventions on the Diagnosis of Hospital-Onset Clostridioides difficile Infections. Jt Comm J Qual Patient Saf 2020;46:457–463. [DOI] [PubMed] [Google Scholar]
- 41.Cook PP, Nichols S, Coogan M, Opera J, DeHart M. Reduction in testing and change in testing algorithm associated with decrease in number of nosocomial Clostridioides (Clostridium) difficile infections. Am J Infect Control 2020;48:1019–1022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


