Abstract
Lower urinary tract symptoms due to benign prostatic hyperplasia constitute a substantial burden, affecting the quality of life of those affected by this condition. While watchful waiting and medical management using a wide array of pharmaceuticals can be effective, surgery has been one of the most definite solutions for those highly affected by this condition. Transurethral resection of the prostate (TURP) is the gold standard surgical procedure, but other alternatives using laser (HoLEP and ThuLEP) and robotic water jets (Aquablation) are emerging treatments aimed at reducing postoperative morbidity. Minimally invasive procedures conducted in outpatient settings and under local anesthesia or sedation are increasingly being used, especially in those patients with high surgical risk due to comorbidities. These procedures include prostatic arterial embolization, water vapor thermal therapy (Rezum), prostatic urethral lift (Urolift), temporary implantable nitinol device (TIND/iTIND), and transurethral microwave thermotherapy (TUMT). The evidence supporting these treatments is growing, but some uncertainties remain as to what is the magnitude of their advantages and disadvantages compared to TURP. Innovations in the technologies involved in these new procedures may improve their profile for effectiveness and safety. Moreover, new devices are being investigated for marketing approval. Issues around costs and patients’ preferences are also yet to be elucidated, thus their evolving role needs to be weighed against the aforementioned considerations.
Keywords: Benign prostatic hyperplasia, Evidence-based practice, Minimally invasive surgical procedures
1. Introduction
Benign prostatic hyperplasia (BPH) is a noncancerous enlargement of the prostate gland due to androgenic stimulus exerted by dihydrotestosterone, a metabolite derived from testosterone by the action of the enzyme 5-alpha reductase.1 The most important risk factors for developing BPH include age and the presence of functioning testicles (due to their hormonal influence); a family history of this condition and obesity.2 A total of 50% of 60-year-old men and 90% of 85-year-olds have microscopic BPH; however, only 50% of patients with this histological finding will have a macroscopic enlargement of the gland, and about 50% of these will develop symptoms.3 Therefore, the most appropriate name for this entity is “lower urinary tract symptoms” (LUTS), considering that prostate enlargement is only one of the factors related to the presence of symptoms. The prevalence of LUTS is between 10% and 30% for men in their 60–70s and 30% in their 80s.4
Patients may present with obstructive or irritative symptoms.1 Diagnosis is based on clinical history, and complementary studies are very useful to evaluate the degree of obstruction, rule out complications, and exclude other differential diagnoses.1 Disease severity can be assessed using valid questionnaires, including the International Prostate Symptom Score (IPSS), which consist of seven questions rated on a 0–5 Likert scale, and the total score ranges from 0 to 35.5 Based on the sum score, symptoms can be classified as mild (0–7), moderate,8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19 or severe.20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35 An additional question rates from 0 to 6 the overall impact in the quality of life (IPSS-QoL).5 Long-term complications of BPH include acute urinary retention (AUR), recurrent urinary tract infections, bladder stones, and post-obstructive kidney failure. AUR is one of the most frequent complications, and the risk is up to 14% in 10 years in patients with large prostates and moderate to severe symptoms.6.
2. Medical management
The natural history of BPH shows that the progression of symptoms is very slow, and serious complications are infrequent. Watchful waiting and lifestyle modifications may be warranted in those with mild symptoms. Physical activity could reduce the symptoms of prostatism, so the recommendation to exercise regularly could be part of this management strategy.7 Clinicians frequently advise avoiding irritants, such as coffee, spicy foods, and alcohol, although there is little to no evidence to support these recommendations.8
For those with moderate symptoms, alpha-blockers are the first treatment option, reducing symptoms by 30–40% and improving urinary flow by 20–25%.9 Common side effects include hypotension and ejaculatory dysfunction. However, 5-alpha reductase inhibitors (5-ARI) can cause a moderate reduction in symptoms (15–30%) and prostate size, reducing the risk of AUR and the need for surgery, but there is a latency for this improvement (3–6 months), and they are most effective in patients with larger prostates (>30 cc) that will be treated on a long-term basis.9,10 Patients should be warned that side effects include sexual dysfunction (e.g. erectile and ejaculatory disorder). In highly symptomatic patients with large prostates, the combined use of alpha-blockers and 5-ARI can result in faster symptomatic improvement and a reduction in the incidence of long-term complications.
Other drugs can be considered in the presence of specific symptoms. The result of clinical trials of phosphodiesterase inhibitors (PDE-Is) such as tadalafil indicate that they may be marginally beneficial over placebo in reducing LUTS.11 While there is a potential risk of hypotension in combination with alpha-adrenergic blockers, a recent meta-analysis reported that a concomitant treatment with α-blockers and PDE-Is does not increase the rate of adverse events due to hypotension.12 Tadalafil may be considered in patients with persistent symptoms in the context of concomitant erectile sexual dysfunction, although it requires close monitoring of adverse events. Moreover, LUTS due to BPH may coexist with symptoms of urgency, frequency, and incontinence due to detrusor overactivity (i.e. overactive bladder). In these cases, beta-3 adrenergic agonists, such as mirabegron and vibegron, stimulate detrusor relaxation without compromising bladder contractility. According to the available clinical trials, they would be effective in reducing irritative symptoms.13 They can be used alone or in combination with anticholinergics. Common side effects include an increase in blood pressure.
Phytotherapeutic agents, such as Serenoa repens, also called Sabal serrulatum or Saw palmetto, have failed to demonstrate symptomatic relief in multiple clinical trials against placebo.14 Pumpkin seeds (Cucurbita pepo) and African plum (Pygeum africanum) in some small clinical trials have moderate efficacy in reducing symptoms.15 These drugs have fewer adverse events, but considering their limited effectiveness, their role in treating LUTS is limited.
3. Surgery and minimally invasive procedures
Transurethral resection of the prostate (TURP) is one of the most widely used techniques, and the probability of symptomatic improvement with this treatment is between 75% and 96%, and it is considered the “gold standard” treatment. The intervention is brief (usually within 60 minutes) and requires general or spinal anesthesia. The tissue is removed through the urethra using a resectoscope, and the patient remains with a bladder catheter for approximately a couple of days, and after this period, he is discharged from hospital.16 The morbidity associated with TUR varies between 5% and 30%. Intraoperative complications include uncontrollable bleeding and capsular perforation with the consequent massive absorption of irrigation fluid (“post-TURP syndrome”) and its consequences dilutional hyponatremia, acute renal failure due to hemolysis, cerebral edema, and even death.17 Early postoperative complications include hematuria, which may persist for up to six weeks, and infection; whereas, late complications include urethral stricture (<10%), bladder neck fibrosis, and urinary incontinence (∼1%).18,19 The most frequent late adverse effect of TURP is retrograde ejaculation (66% to 86% of operated patients); it can produce sterility but be not accompanied by alterations when achieving orgasm. Between 10% and 15% of patients present with psychogenic erectile dysfunction after TUR, and up to 2% to 5% with surgery-derived erectile dysfunction.20,21 The reoperation rate is close to 3.3%, mostly related to the aforementioned late complications.22,23 Improvements in TURP technique, including the use of bipolar energy, have reduced the risk of post-TUR syndrome and bleeding.23
4. Alternatives to TURP with spinal anesthesia
There are currently several surgical procedures with laser devices for the treatment of BPH, which allow the use of saline solution as an irrigation medium (with the same advantages as bipolar TURP) and are performed on an outpatient basis under spinal anesthesia with a requirement bladder catheter that averages 24 to 48 hours.24 Laser enucleation uses a technique that, similar to open surgery, consists of resecting the middle and lateral lobes from the verumontanum to the bladder neck and then grinding the surgical material in the bladder for pathological study using Holmium (HoLEP) or Thulium (ThuLEP) lasers. This procedure offers results comparable to TURP with less morbidity and hospital stay.24,25
Laser ablation, on the other hand, is a technique that uses lasers to cauterize glandular tissue until an adequately patent prostatic canal is achieved. Similarly, photo-selective vaporization of the prostate (PVP) uses green light for this purpose.26 The disadvantages of ablation and vaporization procedures include the impossibility of obtaining material for biopsy and a time of dysuria that is usually longer than with TURP; whereas, the advantages over the latter are a shorter hospital stay, subsequent bleeding, and the need for a bladder catheter, with similar results in terms of symptom improvement.25,26
Finally, water ablation therapy (also known as Aquablation®) is a recently developed surgical procedure that, using real-time visualization and ultrasound, uses a high-velocity, non-heated, sterile saline water jet to ablate prostate tissue. This procedure is probably as effective as TUR with a lower incidence of ejaculation problems, but no little difference in erectile function.27
5. Alternatives to TURP using local anesthesia or sedation: minimally invasive procedures
Many patients with moderate or severe symptoms are older adults with a high surgical risk, which led to the emergence of minimally invasive alternatives that, unlike the aforementioned procedures, can be performed with local anesthesia, on an outpatient basis, and selective post-procedure catheterization. These procedures, with the exception of arterial embolization, in principle, are not designed for large prostates. These procedures include as follows:
Prostatic arterial embolization (PAE): using femoral or radial artery puncture and guided by a preoperative assessment (using CT or MRI) of the pelvic artery anatomy, super-selective micro-catheterization and embolization is then performed on the prostatic arteries to induce tissue necrosis.28 Particle emboli are used almost exclusively, with wide variation in the type and size of particles.29
Prostatic urethral lift (PUL, Urolift®, Teleflex Inc., Pleasanton, CA, USA): using a handheld pistol grip to which a needle-shaped probe is attached, four hook-shaped implants are placed to pull the urethral wall to expand the inner lumen, and two in each one of the lateral lobes of the prostate. This procedure is generally not used to treat a hypertrophied median lobe of the prostate, which causes obstructive intravesical protrusion of the prostate.30
Temporary implantable nitinol device (TIND®, Medi-Tate Ltd., Hadera, Israel): a cage-like device expands the lumen of the urethra causing necrosis to the adjacent prostatic tissue. This device was modified in its original 4-strout to a 3-intertwined strout to reduce the risk of mucosal damage into a second generation (iTIND®).31
Water vapor thermal therapy (WVTT, Rezum®, NxThera Inc., Maple Grove, MN, USA): it uses radiofrequency to create thermal energy through a jet of water vapor that triggers prostatic necrosis. This procedure is performed with the person in the dorsal lithotomy position, and using a cystoscopy, a treatment needle delivers injections of water vapor lasting approximately 9 seconds.32
Transurethral microwave thermotherapy (TUMT): this is one of the first procedures developed in this category. TUMT uses a transurethral probe to radiate heat to the prostatic tissue causing necrosis.33 A rectal probe may be inserted and can be used to monitor rectal temperature.34 There are different types of devices and manufacturers, including those using high-energy to reduce the time of the procedure and urethral cooling to reduce damage.33
Most of these procedures have a low rate of major complications compared to TURP (see below). Pain, dysuria, urinary retention, and urinary tract infection are common side effects.32,35, 36, 37, 38, 39 In the case of PAE, some of these local and systemic adverse events (dysuria, pain, fever, and nausea) are clustered in a poorly defined “post-PAE-syndrome.”40
5.1. Benefits and harms of minimally invasive procedures
Based on a Cochrane review with network meta-analysis, PUL and PAE are likely to be more effective in reducing urinary symptoms, among other minimally invasive procedures. See Table 1 for a summary of key trials25, 26, 41, 42, 43, 44, 45 and systematic reviews46, 47, 48, 49 for each of these procedures. The evidence is limited and of low to very low certainty and short-term follow-up (<12 months).22,50 Major adverse events across procedures may also be less frequent than TURP. The evidence is insufficient on the effects of minimally invasive procedures on sexual outcomes, including erectile and ejaculatory function. This brings into question the labeling of ”ejaculation-preserving” procedures as they have not been able to demonstrate better sexual outcomes.51 This is due to the fact that most studies did not systematically evaluate these outcomes using validated outcome measures or only assessed them in a subset of participants, breaking the principle of randomization. The rate of retreatments is very uncertain for some procedures for which the trials were unblinded and participants crossed over at three months (WVTT and TIND). Nevertheless, at long-term follow-up, retreatment rates were higher than TURP for PAE and PUL, but specially for TUMT, which was nearly ten times more than TURP.22,50 Following the numerous trials on TUMT in the 1990s and 2000s, prostatic arterial embolization has the largest evidence based on randomized controlled trials, counting seven studies with 488 participants, some with two-year follow-up, in contrast to other technologies with smaller trials with short-term follow-up.46, 47, 48, 49
Table 1.
Summary of the main trials and systematic reviews for minimally invasive procedures.
| Study name (trial period) | Country | n | Follow-up | Main characteristics |
|---|---|---|---|---|
| Convective radiofrequency water vapor therapy (Rezum) | ||||
|
|
|
|
|
| Prostatic arterial embolization (PAE) | ||||
|
|
|
|
|
|
|
|
|
|
| Prostatic urethral lift (PUL) | ||||
|
|
|
|
|
|
|
|
|
|
| Temporary implantable nitinol device (TIND) | ||||
|
|
|
|
|
| Transurethral microwave thermotherapy (TUMT) | ||||
|
|
|
|
|
Footnote: certainty ratings were extracted from corresponding Cochrane reviews. IPSS: International Prostate Symptom Score; RR: risk ratio; MD: mean difference.
5.2. Finding the right spot for new treatments – what comes next?
Currently, TURP remains the most frequently used procedure, but minimally invasive treatments are on the rise, particularly prostatic urethral lift in the US and Australia.52,53 Insurers, third-party authorization, and the incorporation in guidelines are important factors for their implementation. For instance, while PUL is recommended as an alternative for TURP by the American Urological Association (AUA), the National Institute for Care and Excellence (NICE) in the UK, and the European Association of Urology (EAU), TIND and TUMT are either not mentioned or discouraged due to high retreatment rates.9,54,55 Moreover, the NICE and the AUA have conflicting recommendations regarding the use of PAE and the AUA and EAU on the use of WVTT.56 Moreover, considerations about cost-effectiveness are paramount, but determinations may be challenging. For instance, one cost-effectiveness analysis found that PUL and WVTT may not be cost-effective compared to TURP or PVP (green light).57 Other head-to-head economic evaluations found that WVTT was cost-effective compared to PUL at a four-year horizon; however, the effectiveness data for WVTT was extrapolated from the trial that was unblinded and allowed cross-over at three months.58 The results of these analyses should be interpreted with caution due to the emergent data on effectiveness and safety and the evolving changes in the cost base for these procedures.
Technical innovations may also modulate the benefits and harms of each procedure. However, there have not been new models for TUMT and WVTT (Rezum®), and a new generation of PUL (marketed as Urolift®) was launched in March 2022 (UroLift 2®), using the same implant with improved features in the delivery system.59 Moreover, the elements of PAE, including particle type and size, can also provide a better effectiveness profile. Procedures using smaller particle size (<300 μm) may be associated with a greater reduction of IPSS scores60 but a greater incidence of adverse events.61 Promising results have been reported in single-arm trials using newer embolic particles (e.g. polyethylene glycol microspheres also called HydroPearl®) with a tighter calibration of size62. More investigation is needed as to how to better perform this procedure to reduce the dose of radiation and avoid collateral damage to anastomotic pudendal arteries63. Finally, a growing area of development includes newer temporary implantable devices similar to iTIND, including ClearRing®, ZenFlow Spring®, and Butterfly®.64 Small single-arm trials for ClearRing® and Butterfly® indicate a 53% and 40% reduction in IPSS scores, respectively.65,66
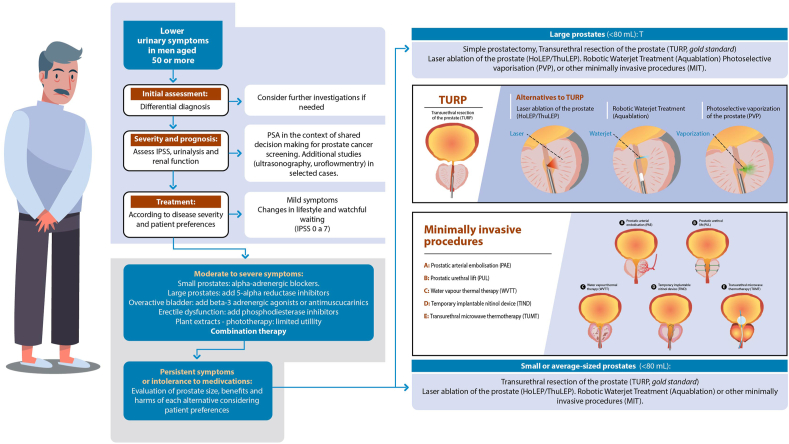
The decision to undergo traditional surgery or a minimally invasive procedure can be led by the balance of benefits and harms based on patients' values and preferences. Men prefer a quick relief, ideally obtaining stable results, but at the same time, they are mindful of the risks and they prefer avoiding sexual side effects and AUR.67 Sexual effects may be less important in those sexually inactive, such as elderly adults, but at the same time, the elderly may also be less prone to choosing surgical options.67 Nevertheless, these studies on values have limitations in their internal validity and generalizability, and an individualized approach eliciting a patient's preferences through shared decision-making is still warranted.68 Evidence-based decision aids are needed to help clinicians throughout these conversations.69 We provide some pointers in Table 2 and a summary of the management of LUTS due to BPH in Fig. 1 so patients can engage in meaningful conversations with their health providers about these treatments.
Table 2.
Guidance to engage in conversations about minimally invasive treatments
| Steps in shared decision-making | Example of triggers for conversations with the patient |
|---|---|
| Invite the patient to shared decision-making (choice-talk) | I would like to discuss what is the best treatment option for you, would you be interested in talking about it? The decision about having surgery can be complex and we might need to discuss the alternatives and your thoughts about it. Would you like me to discuss the available options? |
| Help explore and compare treatment option (option-talk) | An option may be to continue taking the medication, in your case and because you are stable in relation to your symptoms, surgical treatment may not have additional improvements, however, in the case of not opting for surgical treatment it is important to know that there is a risk of acute urinary retention in the coming years (the probability of this will depend on the size of the prostate and how much urine you retain). On the other hand, if you choose surgical treatment, the risk of acute urinary retention will be lower; however, it is important to consider the risks of postoperative complications of the different procedures, which include: ejaculatory problems (66% to 86%), erectile dysfunction (up to 5%), blood in urine and in some rare cases urinary incontinence All of these could occur less frequently with some minimally invasive procedures, although it is important to consider that these have a high rate of need for long-term retreatment (that means, again for surgery). |
| Inquire into the patient's values and preferences (option-talk) | Looking at the alternatives, benefits, and harms, what is most important to you? How important are the benefits? What do you think about the side effects? |
| Evaluate the decision (decision-talk) | Do you need additional information or consult someone else before making a decision? Do you want to make a decision now or later? How comfortable are you with the decision we made?” |
Fig. 1.
Summary of the current management of lower urinary tract symptoms due to benign prostatic hyperplasia in men.
In a recent analysis of the uncertainties of the evidence surrounding these new procedures, we found ten ongoing trials comparing them to TURP or alternatives to TURP, which would further clarify their role in the treatment of LUTS due to BPH.56 Interestingly, we have identified four trials comparing these procedures with medical management (NCT04245566, NCT02869971, NCT0483876, and NCT04987892), which highlights the emerging role as initial treatment of this condition.56 More recently, it has been proposed that WVTT can be a cost-effective first-line therapy, but this is reliant in the previously described weak evidence base.70 More trials will shed more light into the role of these treatments (see Table 3).
Table 3.
Ongoing studies involving minimally invasive procedures
| Trial identification | Intervention | Comparison |
|---|---|---|
| Comparisons between procedures | ||
| ACTRN12617001235392 | PAE | TURP |
| NCT02006303 | PAE | Green light photo-selective vaporization |
| NCT04084938 | PAE | TURP |
| NCT04236687 | PAE | Holmium laser enucleation |
| NCT02054013 | PAE | TURP |
| NCT04757116 | TIND | TURP |
| NCT04178811 | PUL | Holmium laser enucleation |
| NCT04338776 | PUL | WVTT |
| NCT04987138 | ZenFlow∗ | Sham |
| NCT04807010 | PAE | Sham |
| Minimally invasive treatments versus medical treatment | ||
| NCT04245566 | PAE | 5-alpha reductase inhibitors + Alpha-blockers |
| NCT02869971 | PAE | Dutasteride + Tamsulosin |
| NCT04838769 | WVTT | 5-alpha reductase inhibitors + Alpha-blockers |
| NCT04987892 | PUL | Tamsulosin |
Footnotes: PAE: prostatic arterial embolization, WVTT: water vapor thermal therapy (Rezum); PUL: prostatic urethral lift (Urolift); TIND: temporary implantable nitinol device; TURP: transurethral resection of the prostate. Status in November 2021. (∗) ZenFlow is an implantable device similar to TIND. (∗∗) Follow-up before cross-over.
References
- 1.Partin A.W., Peters C.A., Kavoussi L.R., Dmochowski R.R., Wein A.J. Elsevier; 2020. Campbell Walsh Wein Urology: 4-Volume Set. [Google Scholar]
- 2.Ng M., Baradhi K.M. StatPearls. StatPearls Publishing; 2022. Benign Prostatic Hyperplasia. [PubMed] [Google Scholar]
- 3.Roehrborn C.G. Benign prostatic hyperplasia: an overview. Rev Urol. 2005;7(Suppl 9):S3–S14. [PMC free article] [PubMed] [Google Scholar]
- 4.Parsons J.K., Bergstrom J., Silberstein J., Barrett-Connor E. Prevalence and characteristics of lower urinary tract symptoms in men aged > or = 80 years. Urology. 2008;72(2):318–321. doi: 10.1016/j.urology.2008.03.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barry M.J., Fowler F.J., O’Leary M.P., Bruskewitz R.C., Logan Holtgrewe H., Mebust W.K., et al. The American Urological Association Symptom Index for Benign Prostatic Hyperplasia. J Urol. 1992;148(5 Part 1):1549–1557. doi: 10.1016/s0022-5347(17)36966-5. [DOI] [PubMed] [Google Scholar]
- 6.Jacobsen S.J., Girman C.J., Lieber M.M. Natural history of benign prostatic hyperplasia. Urology. 2001;58(6 Suppl 1):5–16. doi: 10.1016/s0090-4295(01)01298-5. discussion 16. [DOI] [PubMed] [Google Scholar]
- 7.Silva V., Grande A.J., Peccin M.S. Physical activity for lower urinary tract symptoms secondary to benign prostatic obstruction. Cochrane Database Syst Rev. 2019;4:CD012044. doi: 10.1002/14651858.CD012044.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bradley C.S., Erickson B.A., Messersmith E.E., Pelletier-Cameron A., Lai H.H., Kreder K.J., et al. Evidence of the impact of diet, fluid intake, caffeine, alcohol and tobacco on lower urinary tract symptoms: a systematic review. J Urol. 2017;198(5):1010–1020. doi: 10.1016/j.juro.2017.04.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.European Association of Urology . EAU; 2022. Management of Non-Neurogenic Male Lower Urinary Tract Symptoms (LUTS), incl. Benign Prostatic Obstruction (BPO)https://uroweb.org/guidelines/management-of-non-neurogenic-male-luts Published. [Google Scholar]
- 10.Gacci M., Corona G., Salvi M., Vignozzi L., McVary K.T., Kaplan S.A., et al. A systematic review and meta-analysis on the use of phosphodiesterase 5 inhibitors alone or in combination with α-blockers for lower urinary tract symptoms due to benign prostatic hyperplasia. Eur Urol. 2012;61(5):994–1003. doi: 10.1016/j.eururo.2012.02.033. [DOI] [PubMed] [Google Scholar]
- 11.Wang Y., Bao Y., Liu J., Duan L., Cui Y. Tadalafil 5 mg Once Daily Improves Lower Urinary Tract Symptoms and Erectile Dysfunction: A Systematic Review and Meta-analysis. Low Urin Tract Symptoms. 2018;10(1):84–92. doi: 10.1111/luts.12144. [DOI] [PubMed] [Google Scholar]
- 12.Adamou C., Ntasiotis P., Athanasopoulos A., Kallidonis P. The hemodynamic interactions of combination therapy with α-blockers and phosphodiesterase-5 inhibitors compared to monotherapy with α-blockers: a systematic review and meta-analysis. Int Urol Nephrol. 2020;52(8):1407–1420. doi: 10.1007/s11255-020-02454-6. [DOI] [PubMed] [Google Scholar]
- 13.Sebastianelli A., Russo G.I., Kaplan S.A., McVary K.T., Moncada I., Gravas S., et al. Systematic review and meta-analysis on the efficacy and tolerability of mirabegron for the treatment of storage lower urinary tract symptoms/overactive bladder: Comparison with placebo and tolterodine. Int J Urol. 2018;25(3):196–205. doi: 10.1111/iju.13498. [DOI] [PubMed] [Google Scholar]
- 14.Trivisonno L.F., Sgarbossa N., Alvez G.A., Fieiras C., Escobar Liquitay C.M., Jung J.H., et al. Serenoa repens for the treatment of lower urinary tract symptoms due to benign prostatic enlargement: A systematic review and meta-analysis. Investig Clin Urol. 2021;62(5):520–534. doi: 10.4111/icu.20210254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilt T., Ishani A., Mac Donald R., Rutks I., Stark G. Pygeum africanum for benign prostatic hyperplasia. Cochrane Database Syst Rev. 2002;1:CD001044. doi: 10.1002/14651858.CD001044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stormont G., Chargui S. StatPearls. StatPearls Publishing; 2021. Transurethral Resection Of The Prostate. [PubMed] [Google Scholar]
- 17.Demirel I., Ozer A.B., Bayar M.K., Erhan O.L. TURP syndrome and severe hyponatremia under general anaesthesia. BMJ Case Rep. 2012;2012 doi: 10.1136/bcr-2012-006899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Castellani D., Rubilotta E., Fabiani A., Maggi M., Wroclawski M.L., Teoh J.Y-C., et al. Correlation between transurethral interventions and their influence on type and duration of postoperative urinary incontinence: results from a systematic review and meta-analysis of comparative studies. J Endourol. 2022;13 doi: 10.1089/end.2022.0222. Published online June. [DOI] [PubMed] [Google Scholar]
- 19.Garza-Montúfar M.E., Cobos-Aguilar H., Treviño-Baez J.D., Pérez-Cortéz P. Factors associated with urethral and bladder neck stricture after transurethral resection of the prostate. J Endourol. 2021;35(9):1400–1404. doi: 10.1089/end.2020.0847. [DOI] [PubMed] [Google Scholar]
- 20.Pavone C., Abbadessa D., Scaduto G., Caruana G., Scalici Gesolfo C., Fontana D., et al. Sexual dysfunctions after transurethral resection of the prostate (TURP): evidence from a retrospective study on 264 patients. Arch Ital Urol Androl. 2015;87(1):8–13. doi: 10.4081/aiua.2015.1.8. [DOI] [PubMed] [Google Scholar]
- 21.Taher A. Erectile dysfunction after transurethral resection of the prostate: incidence and risk factors. World J Urol. 2004;22(6):457–460. doi: 10.1007/s00345-004-0449-1. [DOI] [PubMed] [Google Scholar]
- 22.Franco J.V.A., Jung J.H., Imamura M., Borofsky M., Omar M.I., Liquitay C.M.E., et al. Minimally invasive treatments for lower urinary tract symptoms in men with benign prostatic hyperplasia: a network meta-analysis. Cochrane Database Syst Rev. 2021;(7). doi: 10.1002/14651858.CD013656.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alexander C.E., Scullion M.M., Omar M.I., Yuan Y., Mamoulakis C., N’Dow J.M., et al. Bipolar versus monopolar transurethral resection of the prostate for lower urinary tract symptoms secondary to benign prostatic obstruction. Cochrane Database Syst Rev. 2019;12:CD009629. doi: 10.1002/14651858.CD009629.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang S.W., Tsai C.Y., Tseng C.S., Shih M.C., Yeh Y.C., Chien K.L., et al. Comparative efficacy and safety of new surgical treatments for benign prostatic hyperplasia: systematic review and network meta-analysis. BMJ. 2019;367:l5919. doi: 10.1136/bmj.l5919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hartung F.O., Kowalewski K.F., von Hardenberg J., Worst T.S., Kriegmair M.C., Nuhn P., et al. Holmium Versus Thulium Laser Enucleation of the Prostate: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Eur Urol Focus. 2022;8(2):545–554. doi: 10.1016/j.euf.2021.03.024. [DOI] [PubMed] [Google Scholar]
- 26.Lai S., Peng P., Diao T., Hou H., Wang X., Zhang W., et al. Comparison of photoselective green light laser vaporisation versus traditional transurethral resection for benign prostate hyperplasia: an updated systematic review and meta-analysis of randomised controlled trials and prospective studies. BMJ Open. 2019;9(8) doi: 10.1136/bmjopen-2018-028855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hwang E.C., Jung J.H., Borofsky M., Kim M.H., Dahm P. Aquablation of the prostate for the treatment of lower urinary tract symptoms in men with benign prostatic hyperplasia. Cochrane Database Syst Rev. 2019;2 doi: 10.1002/14651858.CD013143.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carnevale F.C., Antunes A.A., da Motta Leal Filho J.M., et al. Prostatic artery embolization as a primary treatment for benign prostatic hyperplasia: preliminary results in two patients. Cardiovasc Intervent Radiol. 2010;33(2):355–361. doi: 10.1007/s00270-009-9727-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DeMeritt J.S., Elmasri F.F., Esposito M.P., Rosenberg G.S. Relief of benign prostatic hyperplasia-related bladder outlet obstruction after transarterial polyvinyl alcohol prostate embolization. J Vasc Intervent Radiol. 2000;11(6):767–770. doi: 10.1016/s1051-0443(07)61638-8. [DOI] [PubMed] [Google Scholar]
- 30.McNicholas T.A. Benign prostatic hyperplasia and new treatment options - a critical appraisal of the UroLift system. Med Devices. 2016;9:115–123. doi: 10.2147/MDER.S60780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amparore D., De Cillis S., Volpi G., Checcucci E., Manfredi M., Morra I., et al. First- and second-generation temporary implantable nitinol devices as minimally invasive treatments for BPH-related LUTS: systematic review of the literature. Curr Urol Rep. 2019;20(8):47. doi: 10.1007/s11934-019-0912-6. [DOI] [PubMed] [Google Scholar]
- 32.Dixon C.M., Cedano E.R., Pacik D., Vit V., Varga G., Wagrell L., et al. Two-year results after convective radiofrequency water vapor thermal therapy of symptomatic benign prostatic hyperplasia. Res Rep Urol. 2016;8:207–216. doi: 10.2147/RRU.S119596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Walmsley K., Kaplan S.A. Transurethral microwave thermotherapy for benign prostate hyperplasia: separating truth from marketing hype. J Urol. 2004;172(4 Pt 1):1249–1255. doi: 10.1097/01.ju.0000129967.30558.ca. [DOI] [PubMed] [Google Scholar]
- 34.Rubeinstein J.N., McVary K.T. Transurethral microwave thermotherapy for benign prostatic hyperplasia. Int Braz J Urol. 2003;29(3):251–263. doi: 10.1590/s1677-55382003000300013. [DOI] [PubMed] [Google Scholar]
- 35.Porpiglia F., Fiori C., Amparore D., Kadner G., Manit A., Valerio M., et al. Second-generation of temporary implantable nitinol device for the relief of lower urinary tract symptoms due to benign prostatic hyperplasia: results of a prospective, multicentre study at 1 year of follow-up. BJU Int. 2019;123(6):1061–1069. doi: 10.1111/bju.14608. [DOI] [PubMed] [Google Scholar]
- 36.Chin P.T., Bolton D.M., Jack G., Rashid P., Thavaseelan J., Yu R.J., et al. Prostatic urethral lift: two-year results after treatment for lower urinary tract symptoms secondary to benign prostatic hyperplasia. Urology. 2012;79(1):5–11. doi: 10.1016/j.urology.2011.10.021. [DOI] [PubMed] [Google Scholar]
- 37.Woo H.H., Bolton D.M., Laborde E., Jack G., Chin P.T., Rashid P., et al. Preservation of sexual function with the prostatic urethral lift: a novel treatment for lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Sex Med. 2012;9(2):568–575. doi: 10.1111/j.1743-6109.2011.02568.x. [DOI] [PubMed] [Google Scholar]
- 38.Pisco J.M., Bilhim T., Pinheiro L.C., Fernandes L., Pereira J., Costa N.V., et al. Medium- and long-term outcome of prostate artery embolization for patients with benign prostatic hyperplasia: results in 630 patients. J Vasc Intervent Radiol. 2016;27(8):1115–1122. doi: 10.1016/j.jvir.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 39.Feng S., Tian Y., Liu W., Li Z., Deng T., Li H., et al. Prostatic arterial embolization treating moderate-to-severe lower urinary tract symptoms related to benign prostate hyperplasia: a meta-analysis. Cardiovasc Intervent Radiol. 2017;40(1):22–32. doi: 10.1007/s00270-016-1516-x. [DOI] [PubMed] [Google Scholar]
- 40.Svarc P., Taudorf M., Nielsen M.B., Stroomberg H.V., Røder M.A., Lönn L. Postembolization syndrome after prostatic artery embolization: a systematic review. Diagnostics. 2020;10(9) doi: 10.3390/diagnostics10090659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chughtai B., Elterman D., Shore N., Gittleman M., Motola J., Pike S., et al. The iTind temporarily implanted nitinol device for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia: a multicenter, randomized, controlled trial. Urology. 2021;153:270–276. doi: 10.1016/j.urology.2020.12.022. [DOI] [PubMed] [Google Scholar]
- 42.Roehrborn C.G., Gange S.N., Shore N.D., Giddens J.L., Bolton D.M., Cowan B.E., et al. The prostatic urethral lift for the treatment of lower urinary tract symptoms associated with prostate enlargement due to benign prostatic hyperplasia: the L.I.F.T. Study. J Urol. 2013;190(6):2161–2167. doi: 10.1016/j.juro.2013.05.116. [DOI] [PubMed] [Google Scholar]
- 43.Gratzke C., Barber N., Speakman M.J., Berges R., Wetterauer U., Greene D., et al. Prostatic urethral lift vs transurethral resection of the prostate: 2-year results of the BPH6 prospective, multicentre, randomized study. BJU Int. 2017;119(5):767–775. doi: 10.1111/bju.13714. [DOI] [PubMed] [Google Scholar]
- 44.McVary K.T., Gange S.N., Gittelman M.C., Goldberg K.A., Patel K., Shore N.D., et al. Minimally invasive prostate convective water vapor energy ablation: a multicenter, randomized, controlled study for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol. 2016;195(5):1529–1538. doi: 10.1016/j.juro.2015.10.181. [DOI] [PubMed] [Google Scholar]
- 45.Pisco J.M., Bilhim T., Costa N.V., Torres D., Pisco J., Pinheiro L.C., et al. Randomised clinical trial of prostatic artery embolisation versus a sham procedure for benign prostatic hyperplasia. Eur Urol. 2020;77(3):354–362. doi: 10.1016/j.eururo.2019.11.010. [DOI] [PubMed] [Google Scholar]
- 46.Jung J.H., McCutcheon K.A., Borofsky M., Young S., Golzarian J., Kim M.H., et al. Prostatic arterial embolization for the treatment of lower urinary tract symptoms in men with benign prostatic hyperplasia. Cochrane Database Syst Rev. 2022;3:CD012867. doi: 10.1002/14651858.CD012867.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Franco J.V.A., Garegnani L., Liquitay C.M.E., Borofsky M., Dahm P. Transurethral microwave thermotherapy for the treatment of lower urinary tract symptoms in men with benign prostatic hyperplasia. Cochrane Database Syst Rev. 2021;(6) doi: 10.1002/14651858.CD004135.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jung J.H., Reddy B., McCutcheon K.A., Borofsky M., Narayan V., Kim M.H., et al. Prostatic urethral lift for the treatment of lower urinary tract symptoms in men with benign prostatic hyperplasia. Cochrane Database Syst Rev. 2019;5:CD012832. doi: 10.1002/14651858.CD012832.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kang T.W., Jung J.H., Hwang E.C., Borofsky M., Kim M.H., Dahm P. Convective radiofrequency water vapour thermal therapy for lower urinary tract symptoms in men with benign prostatic hyperplasia. Cochrane Database Syst Rev. 2020;3 doi: 10.1002/14651858.CD013251.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Franco J.V., Jung J.H., Imamura M., Borofsky M., Omar M.I., Escobar Liquitay C.M., et al. Minimally invasive treatments for benign prostatic hyperplasia: a Cochrane network meta-analysis. BJU Int. 2021;25 doi: 10.1111/bju.15653. Published online November. [DOI] [PubMed] [Google Scholar]
- 51.Sokolakis I., Pyrgidis N., Russo G.I., Sountoulides P., Hatzichristodoulou G. Preserving ejaculation: a guide through the landscape of interventional and surgical options for benign prostatic obstruction. Eur Urol Focus. 2022;8(2):380–383. doi: 10.1016/j.euf.2022.03.008. [DOI] [PubMed] [Google Scholar]
- 52.Dalimov∗ Z., Hamann H., Alavi-Dunn N., Ernst M., Chevli K. PD29-09 trends in minimally invasive surgical therapies for benign prostatic hyperplasia: treatment substitution or treatment expansion effect by prostatic urethral lift? J Urol. 2020 doi: 10.1097/JU.0000000000000893.09. Published online. [DOI] [Google Scholar]
- 53.Morton A., Williams M., Perera M., Teloken P.E., Donato P., Ranasinghe S., et al. Management of benign prostatic hyperplasia in the 21st century: temporal trends in Australian population-based data. BJU Int. 2020;126(Suppl 1):18–26. doi: 10.1111/bju.15098. [DOI] [PubMed] [Google Scholar]
- 54.Lerner L.B., McVary K.T., Barry M.J., Bixler B.R., Dahm P., Das A.K., et al. Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA GUIDELINE PART II-surgical evaluation and treatment. J Urol. 2021;206(4):818–826. doi: 10.1097/JU.0000000000002184. [DOI] [PubMed] [Google Scholar]
- 55.Overview | Lower urinary tract symptoms in men: management | Guidance | NICE. Accessed November 29, 2021. https://www.nice.org.uk/guidance/cg97.
- 56.Franco J.V.A., Jung J.H., Liquitay C.M.E., Dahm P. What is the role of minimally invasive surgical treatments for benign prostatic enlargement? BMJ. 2022;377 doi: 10.1136/bmj-2021-069002. [DOI] [PubMed] [Google Scholar]
- 57.Ulchaker J.C., Martinson M. Cost-effectiveness analysis of six therapies for the treatment of lower urinary tract symptoms due to benign prostatic hyperplasia. Clinicoecon Outcomes Res. 2017;10:29–43. doi: 10.2147/CEOR.S148195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chughtai B., Rojanasarot S., Neeser K., Gultyaev D., Amorosi S.L., Shore N.D. Cost-effectiveness and budget impact of emerging minimally invasive surgical treatments for benign prostatic hyperplasia. J Health Econ Outcomes Res. 2021;8(1):42–50. doi: 10.36469/jheor.2021.22256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Teleflex LLC. UroLift UL2. Accessed December 24, 2022. https://www.urolift.com/ul2.
- 60.Geevarghese R., Harding J., Parsons N., Hutchinson C., Parsons C. The relationship of embolic particle size to patient outcomes in prostate artery embolisation for benign prostatic hyperplasia: a systematic review and meta-regression. Clin Radiol. 2020;75(5):366–374. doi: 10.1016/j.crad.2019.12.019. [DOI] [PubMed] [Google Scholar]
- 61.Torres D., Costa N.V., Pisco J., Pinheiro L.C., Oliveira A.G., Bilhim T. Prostatic artery embolization for benign prostatic hyperplasia: prospective randomized trial of 100-300 μm versus 300-500 μm versus 100- to 300-μm + 300- to 500-μm Embospheres. J Vasc Intervent Radiol. 2019;30(5):638–644. doi: 10.1016/j.jvir.2019.02.014. [DOI] [PubMed] [Google Scholar]
- 62.Insausti I., Galbete A., Lucas-Cava V., de Ocáriz A.S., Solchaga S., Monreal R., et al. Prostatic Artery Embolization (PAE) using polyethylene glycol microspheres: safety and efficacy in 81 patients. Cardiovasc Intervent Radiol. 2022;45(9):1339–1348. doi: 10.1007/s00270-022-03165-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Maclean D., Francis Bryant C.T., Vigneswaran G., Bryant T.J., Harris M., Somani B., et al. Comprehensive review on current controversies and debate in prostate artery embolization. Turk J Urol. 2022;48(3):166–173. doi: 10.5152/tud.2022.21337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Srinivasan A., Wang R. An update on minimally invasive surgery for benign prostatic hyperplasia: techniques, risks, and efficacy. World J Mens Health. 2020;38(4):402–411. doi: 10.5534/wjmh.190076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Benign prostatic hyperplasia: surgical therapy & new technology I (MP01) J Urol. 2022 doi: 10.1097/JU.0000000000002513. [cited 24 Dec 2022]. [DOI] [Google Scholar]
- 66.Vjaters E., Nitsan D., Mullerad M., Engelstein D., Leibovitch I., Feld Y. First-in-man safety and efficacy of the ClearRing implant for the treatment of benign prostatic hyperplasia. Eur Urol Focus. 2020;6(1):131–136. doi: 10.1016/j.euf.2018.09.013. [DOI] [PubMed] [Google Scholar]
- 67.Malde S., Umbach R., Wheeler J.R., Lytvyn L., Cornu J.N., Gacci M., et al. A systematic review of patients’ values, preferences, and expectations for the diagnosis and treatment of male lower urinary tract symptoms. Eur Urol. 2021;79(6):796–809. doi: 10.1016/j.eururo.2020.12.019. [DOI] [PubMed] [Google Scholar]
- 68.Dahm P., Franco J. Re: a systematic review of patients' values, preferences, and expectations for the diagnosis and treatment of male lower urinary tract symptoms. Eur Urol. 2021;26 doi: 10.1016/j.eururo.2021.04.009. Published online April. [DOI] [PubMed] [Google Scholar]
- 69.Elwyn G., Durand M.A., Song J., Aarts J., Barr P.J., Berger Z., et al. A three-talk model for shared decision making: multistage consultation process. BMJ. 2017;359:j4891. doi: 10.1136/bmj.j4891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sahakyan Y., Erman A., Bhojani N., Chughtai B., Zorn K.C., Sander B., et al. Cost-utility of minimally invasive therapies vs. pharmacotherapy as initial therapy for benign prostatic hyperplasia: a Canadian healthcare payer perspective. Can Urol Assoc J. 2022;6 doi: 10.5489/cuaj.8045. Published online December. [DOI] [PMC free article] [PubMed] [Google Scholar]