Abstract
Coronavirus disease 2019 is a severe communicable pulmonary medical problem that has been a challenging disease for everyone in the globe, but vaccines development and administration against this severe acute respiratory syndrome-inducing disease (coronavirus disease 2019) are currently yielding fabulous results. The mean duration of the coronavirus disease 2019 pandemic for this study spanned from 2020 until 2022. These manifestations are accompanied by symptoms of respiratory tract illnesses such as non-productive cough, sore throat, and nasal discharge. Relevant reviews on coronavirus disease 2019 manifestations and outcomes, consisting mainly of the infections/outbreaks, experimental information, and pre- and post-serovaccination details that occurred, were described. After a typical vaccination course, the study aims to summarize and understand more about the effectiveness of exercise on the pre-and post-coronavirus disease 2019 vaccination and its implementations. Physical activity is an immunological function adjuvant to decrease communicable disease risk and enhance immunity post-viral infection vaccination. Moderate-intensity resistance exercisesession directly before getting the influenza vaccine decreases vaccine responses in older adults, such as redness, pain, or inflammation at the injection spot or other adverse consequences compared to the inactive circumstance. However, it was reported that exercise after a shot is generally safe as long as vaccinated people feel well enough. Though exercise before or after vaccination has no negative impact on the protection afforded by the vaccine, people can exercise immediately after receiving the vaccine, as any changes in blood flow will not affect the vaccine’s response. One episode of light-to-moderate-intensifying exercise after vaccination may improve the antibody reactions to influenza or the coronavirus disease 2019 vaccine. Vaccination administered pre- and post-regular exercise is an effective approach for boosting antibody responses due to its immunostimulant effects. Future research should investigate how different vaccine antibodies respond to low, moderate, and high physical activity levels.
Keywords: COVID-19 pandemic, exercise, physical activity, vaccines
Introduction
The fatality rate from coronavirus disease 2019 (COVID-19) and the occurrence of recent cases in America illustrated both the ineffective federal responsiveness to the pandemic and the critical demand for an organized and explicitly recognized COVID-19 vaccine push.1,2 In the United States, COVID-19 is increasing exponentially, reaching catastrophic proportions, threatening to overwhelm the healthcare system, and causing significant loss of life.3 As well as its debilitating effects on the incidence and outcome of comorbidities such as diabetes mellitus.4 Only 1 year after its emergence, the COVID-19 outbreak had surpassed 97 million cases and 2 million deaths worldwide.5 Being one of the most severe communicable pulmonary diseases, COVID-19 has made 2020/2021 a difficult year for everyone,6 but 58 vaccines against severe acute respiratory syndrome COVID-19 have been developed and are currently being used with significant results. In clinical trials, some vaccines were described to have over 90% efficiency against COVID-19.7 Moreover, numerous vaccine applicants have demonstrated encouraging efficacy and protection profiles, with some of the vaccines previously being approved and rolled out worldwide.8
Presently, The “Pfizer–BioNTech vaccine,” the “Moderna vaccine,” and the “Johnson & Johnson–Janssen vaccine” were all shown in trials to be highly effective against moderate-to-severe disease in adults, with an efficacy of 95% for the Pfizer–BioNTech vaccine, 94% for the “Moderna” and of 72% for the “Johnson & Johnson–Janssen vaccine.”9
Due to an enhanced age-dependent infectious fatality rate,10,11 immunization of the elderly was prioritized ahead of the young which was a global practice.12 A clear exception to this has been the preferred immunization of medical professionals who deal with COVID-19 patients directly. The plan to vaccinate more individuals by postponing the second dosage seems natural at first look given the restricted availability of vaccinations. Hence the idea of a “dose-sparing” strategy was considered because it would prevent surging cases of COVID-19 and reduce fatalities caused by COVID-19. But after the availability of more vaccines, populace were encouraged to receive their second dose for better immunity coverage.13,14
On the other hand, physical activity (PA) is having a vital role against severe and critical COVID-19; Rahmati and Shamsi15 reported that PA is associated with lower hospitalization, intensive care unit admissions, and mortality rates in patients with COVID-19. Immune responses to vaccination may be boosted by PA at the time of immunization. Several studies had shown that exercising before vaccination improved antibody responses.16,17 According to one interpretation of these findings, exercise may work efficiently as a serious insult. Evidence showed that stress might boost antibody responses when pre-vaccination is used.18,19 Eccentric exercise has also been linked to a local inflammatory response, which might lead to increased antigen-presenting cell activation. Some studies have shown excessive activity before vaccination to boost antibody response.20
Vaccination post regular exercise has been reported to be an effective strategy for increasing antibody response, after influenza vaccination; for example, elite athletes have a more remarkable rise in the vaccine-reactive CD4 T cell levels, which attain climax a week following being vaccinated.21 Regular exercise has also been shown to positively affect intervention studies. In particular, a study of 70-year-old sedentary older adults with poor influenza vaccine responses noticed that aerobic exercise (AE) (three times a week lasting up to 60 min/day) demonstrated a significant improvement in “influenza seroprotection” during the whole influenza season in comparison to control group.22 To date, there is no data on the extent of the vaccine’s adverse side effects have been published; as a result, the consequence of the negative impact to engage in PA is unknown.2,23 Furthermore, the COVID-19 vaccine’s effects on physical exercise are also unidentified.24 Currently, no studies have investigated the effectiveness of PA pre- and post-COVID-19 vaccination. Therefore, the purpose of the study is to summarize and understand more about the effect of PA pre- and post-COVID-19 vaccination on the immunological response and its implementation.
Materials and methods
This is a narrative review that included studies that were independently chosen based on the freely available COVID-19 data. The studies were chosen by identifying all relevant investigations by searching through the various databases, including PubMed, Cochrane, Web of Science, and Google Scholar, using the keywords “Vaccines,” “COVID-19,” “Exercise,” and “physical activity” to screen carefully from 2020 until 2022. Boolean logic and wildcards were used to create an electronic search strategy that maximizes data output by allowing the same search words to be used across all databases without needing modifications. The type of studies selected includes systematic review and meta-analysis, review articles, and original studies. Also, studies with full texts were considered, and the participants included were all COVID-19 patients. Studies outside the aforementioned criterions, and non-peer-reviewed or non-original research, editorials, opinion, and discussions were excluded.
Mechanism and effects of PA on side effects of the vaccine
Vaccination trials on older adults have documented PA as a strong immune adjuvant. Single sessions of exercise before vaccination, as well as maintaining high rates of habitual PA in older adults, had been reported to enhance immune responses to influenza and pneumococcal vaccinations; the trained groups showed higher antibody titers against B and H1N1 strains following vaccination.25 In addition, experimental vaccines containing novel antigens, including keyhole limpet hemocyanin, have been noted by researchers to boost immune responses among the elderly.26 The mechanism is likely due to a combination of localized inflammation, phagocytosis, and antigen-presenting cell infiltration at the spot of vaccination, which eventually leads to coating T cell responses, elevating the “naive T cell” incidence, and causing enhancements in “B cell” activity.27 Regular physical activities could prevent immunosenescence through various mechanisms, which include the natural killer (NK) and T cell redistribution by allowing catecholamine mediation to rise in lymphocytes β2-adrenergic receptors, between the tissues and the blood with each bout of exertion. Subsequently lowering the latent virus load and increasing immune surveillance. Hence, the antigen load on T cells reduces the buildup of fatigued T cells although sustaining the proportion and variety of peripheral naïve T cells. The NK cells are mostly accountable for decreasing the risk of infection.28 In addition, the release of IL-7 and IL-15 (muscle-derived cytokines) is an essential factor for immunity following exercise because IL-7 helps to sustain thymic mass (which otherwise withers with age) and boost lymphoid organs to generate antigen virgin (i.e., “naïve”) T cells; meanwhile, IL-15 aids in the maintenance of NK-cell compartments by ensuring their adequate proliferation and optimal function.29 Hence, by boosting the capacity of T cells to react to antigens, frequent exercise may enhance the immunological response to vaccination.
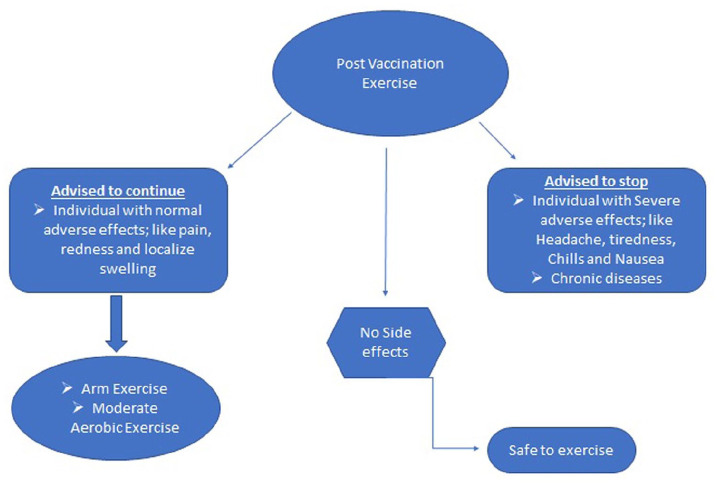
According to exercise immunology studies, PA is an immunological function adjuvant to decreasing communicable disease risk and enhancing immunity post-viral infection vaccination.29 In older persons, moderate-intensity aerobic exercise (MIAE) may reduce the risk of influenza-related illness and boost immune reactions to influenza and pneumonia vaccinations.30 The experience of side effects, like pain, and swelling on the arm where the jab was given, and headache, muscle pain, fever, and nausea, determine whether vaccinated people feel well enough to exercise after receiving the COVID-19 vaccine (Figure 1). However, it was stated that exercise after a shot is generally safe as long as vaccinated people feel well enough, but, at the same time, people should be aware of some of the common vaccine side effects, such as headache, tiredness, chills, and nausea that may interfere with exercise plans.31 Yet, people are still debating whether exercise is safe after the COVID-19 immunization, with some claiming that exercise may affect the vaccine bioavailability in the body. However, exercise before or after vaccination has no life-threatening effects on the protection afforded by the vaccine. PA lowers the threat of community-acquired communicable diseases and death, boosts the immune system’s first line of defense, and boosts vaccination potency.32
Figure 1.
Diagrammatic presentation of post-vaccination exercise.
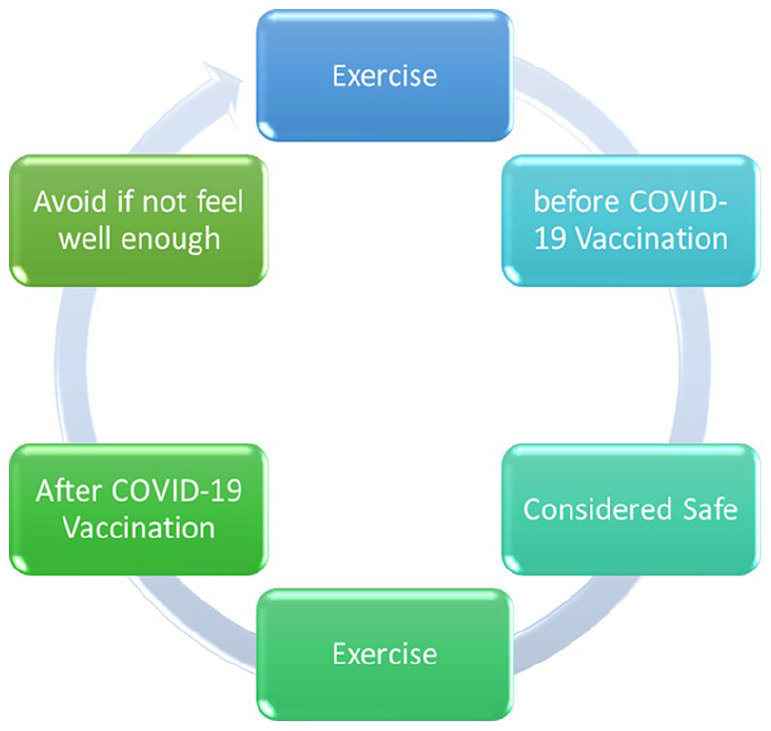
It is suggested that people should exercise regularly before and after receiving the COVID-19 vaccine. However, overtraining syndrome could occur when participating in high exercise workloads, resulting in impaired sports performance, immune dysfunction, and an elevated acute respiratory risk.33,34 Moreover, there are no proofs that exercise immediately before or after receiving the COVID-19 vaccination decreases the effectiveness of the vaccine; PA may be linked to a better favorable reaction to vaccination, suggesting that acquired immunity may be higher in a physically energetic population.28 The only limitations are the possibility of adverse effects from the COVID-19 vaccine itself (Figure 2). A previous study reported no difference in vaccine efficacy with exercise anytime from 2 to 26 h after inoculation against COVID-19.35
Figure 2.
Physical activity and vaccination choice.
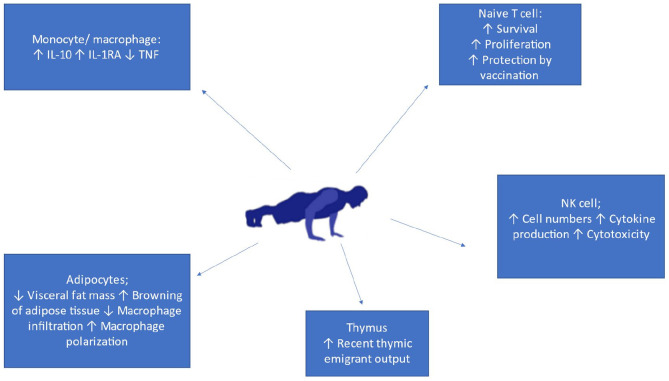
Mechanism of PA and support of the immune system
The input of age-linked falls in PA to immunosenescence has attracted healthcare providers’ interest and the populace to explore the omics science of physical fitness because the significance of being physically active in human on immune aging remained largely under-explored. This is probably because most research on the “long-term” effects of higher PA has only been carried out for less duration (6–12) months. Finding the mechanism of immune cells in active individuals with a prolonged period of elevated level of PA for many parts of the livelihood showed satisfactory changes in physiological function, including sarcopenia, decreased sensitivity of insulin, normal cholesterol, and high immunity.36 During exercise, exerting muscles produce and distribute immune cells, like IL-6, and IL-7.37 IL-6 promotes monocytes and macrophages to produce regulatory mediators (like IL-10).38 It also causes the adrenal glands to release cortisol, which produces a secondary anti-inflammatory response. IL-7 is required for thymocyte production, and it, along with IL-15, are lymphocyte proliferation factors (particularly for naïve T cells). However, the serum concentration of both cytokines decreases with age.27 Through these myokines, regular exercise exerts a constructive stimulation on thymic outcome and T cells by ensuring their secretion. Myokines explain the relationship between active muscle and a better lifestyle in humans, particularly during aging, when a lack of activity and age-linked sarcopenia restrict the immunologically regulating muscle’s role. With the success of omics science, other proteins such as RNA or micro RNA distributed from the muscle that has been investigated might also offer an additional understanding of the exercise–immune system interaction mechanism39 (Figure 3).
Figure 3.
Mechanism of physical activity and support of the immune system.
Exercise as an immune adjuvant
The use of the COVID-19 vaccine may support PA in mitigating the effects of the pandemic facilitating PA during a pandemic, and reducing the seriousness of strict public rules, which aim to increase PA for the population. It’s also important to note the side effect of the vaccine.24 The most frequent post-vaccination complications, such as headaches, and fever, were in people under 60 years old, while injection site pain was found to be more common in people over 60.40
It was reported that the effect of AE on elderly women who engaged in aerobic walking greater than 18,509 steps per day for 14 days after receiving an influenza virus immunization had significantly higher innate immune activation 2 days after vaccination, greater adaptive immune responses 1 week following the vaccination, and increased antibody responses after a second vaccination than those who walked less than 10,927 steps per day.41 Hallam and Jones42 investigated the impact of a 90-min cycle ergometer or outdoor AE conducted once after vaccination on serum antibody response to three distinct vaccines (“2009 pandemic influenza H1N1, seasonal influenza, and COVID-19”). In a mouse model, exercise for 90 min enhanced serum antibodies to each vaccine 4 weeks after vaccination, suggesting that IFNα might have a part in the exercise-related effect. After receiving the COVID-19 vaccine, exercise had no influence on adverse effects.42
Physically fit older men who had conducted AE three times a week for at least 2 years had higher antibody responses to a new immunological challenge than their contemporaries who had not exercised for at least the preceding 2 years.43 In addition, compared to active or sedentary older persons, adults aged 62 who participated in 20 min of intense exercise three times a week exhibited enhanced immunological responses to an influenza virus vaccination.44
A 45-min moderate-intensity resistance exercise session directly before having the influenza vaccine decreases vaccine response in older adults, such as pain, redness, swelling at the spot of injection, or other side effects contrasted to the resting circumstance.45 Aerobic cardiovascular training for 24 weeks demonstrated a significant increase in the seroprotective level of the immune system as well as improved fitness assessment indices such as maximal oxygen uptake and degree of fitness parameters following influenza vaccination. However, flexibility and balance training for the same duration demonstrated no significant improvement in the seroprotective levels following influenza vaccination.22 Thus, these findings suggest that PA plays a role in vaccine responses to both novel and well-known antigens. However, there is no evidence that exercising immediately after the COVID-19 vaccination is harmful but vaccinated people might need to wait a few days if their side effects are severe, such as fever, chills, or headache.46 If they only have soreness or fatigue at the injection site, exercise may help alleviate the immunization symptoms. It was stated that physically active individuals are more prone to be resistant to infection due to improved immunosurveillance against pathogens.47 It is recommended that 150 min of MIAE or 75 min of vigorous-intensity AE per week, with a couple of days of resistance training, improve the quality of life and immune systems such as reducing the risk, duration, or severity of viral infections, particularly in vulnerable people with compromised immune systems.48 Whereas other studies have found that heightened exercise on the antibody response to vaccination during 6 months of follow-up did not affect the antibody responses.45 Endurance exercise for 40–45 min before influenza or pneumococcal vaccination had no consistent immunostimulatory effects in young or old adults, though women benefited more from exercise compared to their corresponding men.17,49 The effectiveness of vaccinations as a public health strategy varies depending on the population. Adjuvants boost the effectiveness of vaccines but often raise reactogenicity. PA at the time of vaccination is a novel behavioral “adjuvant.” Hallam et al.42 investigated the impact of a single 90-min bout of mild to moderate intensity aerobic activity on a cycle ergometer or walking on antibody response to three different vaccinations (2009 pandemic influenza H1N1, seasonal influenza, and COVID-19). After receiving the influenza vaccine or the first dose of the Pfizer BioNTech COVID-19 vaccine, exercise increases serum antibody without an increase in side effects. An influenza mouse model Anti-IFN antibody was administered to mice as part of an immunization to study the impact of exercise on antibody response and the possible function of IFN as a mechanism. The findings demonstrated that 4 weeks after vaccination, 90 min of exercise consistently boosted serum antibody levels for each vaccine, and that IFN may be partly responsible for this effect. These results indicate that a single session of exercise after vaccination may improve antibody response to the influenza or COVID-19 vaccine in persons who routinely exercise.42
Discussion
We found that vaccination administered pre- and post-regular exercise is an effective approach for boosting antibody responses due to its immunostimulant effects, indicating that exercise decreases vaccine response, such as pain, redness, swelling at the spot of injection, or other adverse effects. Policymakers might employ the findings of this study to promote vaccination and reduce the isolation brought on by COVID-19, which encourages the development of several non-communicable diseases in many individuals. The results of this study agree with those of a previous study that included 443 students and found that the majority of students (about 94%) reported no adverse effects that interfered with their daily lives, maintaining health, or performing physical exercise. However, fatigue, weakness, and muscular soreness were experienced by 30–40% of the students. In addition, students who had only received one dose of the COVID-19 vaccination and those who had received two doses reported the same answers regarding how the vaccine affected their daily lifestyle.46
Previous studies have shown that the vaccine has no harmful effects on health, thus individuals should be encouraged to be vaccinated.50,51 Hallam and Jones42 reported that low-to-moderate intensity exercise improves the immune system’s response to the COVID-19 vaccine. Considering that the exercise paradigm is simple to apply and does not require specialized equipment, these findings may have immediately applicable public health value. The exercise intervention is feasible for individuals who frequently exercise at low intensities, such as walking, and participants with various health features were able to complete the activity. According to two different studies, there were less adverse effects for exercisers than for non-exercisers.45,52 In other studies, the effects of 45 min of dynamic or aerobic activity were mixed, with an increase in antibody response to one antigenic component of the influenza vaccination but not to both influenza A antigens, and findings by sex were inconsistent.17,53 It was stated that AE lasting 45 min or less does not improve the antibody response to influenza A vaccination.42
In summary, our findings show that the COVID-19 vaccination antibody response was enhanced by exercise without an increase in adverse effects. Also, longer-duration light- to moderate-intensity exercise increases antibody response across different vaccine formulations, and exercise-induced alterations of IFNα may partially contribute to this effect. Additionally, longer-duration light- to moderate-intensity exercise boosts antibody response to various vaccine formulations; this effect could be attributed to exercise-induced changes in IFNα. This study has several strengths. It is the first study to investigate the effectiveness of PA pre- and post-COVID-19 vaccinations. This study’s findings may effectively mitigate COVID-19 vaccine hesitancy, which would allow people to live normal lives and minimize isolation. The limitation of this study is that we endeavored to decrease publication bias by searching through several databases without regard to language and examining the reference lists of all relevant papers for extra information. Unarguably, we cannot say with absolute certainty that we have found all the studies in this area. The study did not highlight the specific forms of PA that were most associated with the high PA outcome before and after COVID-19 immunizations, which would have provided critical details regarding the frequently reported PA. We could not explain this due to the limited informations we had in our review. Furthermore, case reports, short communications, and conference papers were also excluded. Another limitation of the current study was the heterogeneity of included studies that reported on different types of Vaccines, which makes it difficult to say anything about one specific type of exercise. Apart from this, there was no such limitation for the review process.
Recommendations
PA is regarded as a free therapy for the disease, as well as physical fitness maintenance. Exercise pre- and post-vaccination can help to counter the negative impacts of stress-induced immuno-vaccine response. Clinicians should be knowledgeable about the vaccine types, efficacy, and side effects. Adequate sensitization of the populace on the pandemic consequences by adhering to health-control protocols, avoiding crowding, and maintaining a healthy lifestyle is required. Maintaining a healthy immune system requires regular AE, good nutrition, sleep, and stress reduction. Mild side effects such as body aches, fever, or chills can occur post-vaccine, which may deny the scope for such individuals from exercising because it could be counterproductive to attempt to perform the exercise forcefully; hence, it is better to engage in light walking or let the body recover for an extra day before commencing exercise.35
Conclusion
Compared to healthy persons who did not engage in exercise, healthy individuals who engaged in chronic AE raised their influenza antibodies in response to vaccination. This study implemented that vaccination pre- and post-regular exercise is an effective strategy for increasing antibody responses because it acts as an immunostimulant. A single session of light- to moderate-intensity exercise performed after vaccination may improve antibody response to influenza or COVID-19 vaccine in individuals who regularly exercise. The level of the CD4 count was reported to be elevated in pre-and post-vaccinated exercising individuals. Frequent PA should be advocated in the general populace to reduce the threat of community-acquired infections and communicable disease mortality, boost the effectiveness of immunization plans, and assist in mitigating the effects of the COVID-19 pandemic. Future studies should examine the effects of acute, chronic, and high amounts of PA on various vaccination antibodies. Future research should investigate the relationship between vaccine effectiveness and levels of exercise and PA, as well as the health state of those receiving the immunization. Future research should thus focus on inflammatory indicators or catecholamines that affect the effectiveness of immunization.
Acknowledgments
The authors acknowledge the Universiti Sains Malaysia and the school of medical sciences USM, supporting project number (304.PPSP.6315639) for providing the avenue to carry out this study.
Footnotes
Author contributions: SBAM, AH, and WSWG conceived and designed the study, conducted research, provided research materials, and collected and organized data. AHA, MSZ, and AM analyzed and interpreted data. MM, NA, and YBM wrote initial and final draft of article and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Artak Heboyan  https://orcid.org/0000-0001-8329-3205
https://orcid.org/0000-0001-8329-3205
References
- 1. Latkin C, Dayton LA, Yi G, et al., COVID-19 vaccine intentions in the United States, a social-ecological framework. Vaccine 2021; 39(16): 2288–2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Billon-Denis E, Tournier J-N. COVID-19 and vaccination: a global disruption. Med Sci 2020; 36(11): 1034–1037. [DOI] [PubMed] [Google Scholar]
- 3. Woolf SH, Chapman DA, Lee JH. COVID-19 as the leading cause of death in the United States. JAMA 2021; 325(2): 123–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rahmati M, Keshvari M, Mirnasuri S, et al. The global impact of COVID-19 pandemic on the incidence of pediatric new-onset type 1 diabetes and ketoacidosis: a systematic review and meta-analysis. J Med Virol 2022; 94(11): 5112–5127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Copper FA, de Vázquez CC, Bell A, et al. Preparing for COVID-19 vaccine roll-out through simulation exercises. The Lancet Global Health 2021; 9(6): e742–e743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Teillaud J-L. Médecine/sciences en 2022, une passion pour la recherche [medecine/sciences 2022, a passion for research…]. Med Sci 2022; 38(1): 7–8. [DOI] [PubMed] [Google Scholar]
- 7. Knoll MD, Wonodi C. Oxford–AstraZeneca COVID-19 vaccine efficacy. Lancet 2021; 397(10269): 72–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cavaleri M, Enzmann H, Straus S, et al. The European Medicines Agency’s EU conditional marketing authorisations for COVID-19 vaccines. Lancet 2021; 397(10272): 355–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rosenberg ES, Dorabawila V, Easton D, et al. COVID-19 vaccine effectiveness in New York state. N Engl J Med 2022; 386(2): 116–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bubar KM, Reinholt K, Kissler SM, et al. Model-informed COVID-19 vaccine prioritization strategies by age and serostatus. Science 2021; 371(6532): 916–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Moore S, Hill EM, Dyson L, et al. Modelling optimal vaccination strategy for SARS-CoV-2 in the UK. PLoS Computat Biol 2021; 17(5): e1008849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Butt RT, Janjua OS, Qureshi SM, et al. Dental healthcare amid the covid-19 pandemic. Int J Environ Res Public Health 2021; 18(21): 11008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Paltiel AD, Zheng A, Schwartz JL. Speed versus efficacy: quantifying potential tradeoffs in COVID-19 vaccine deployment. Ann Intern Med 2021; 174(4): 568–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tuite AR, Zhu L, Fisman DN, et al. Alternative dose allocation strategies to increase benefits from constrained COVID-19 vaccine supply. Ann Intern Med 2021; 174(4): 570–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rahmati M, Shamsi MM, Khoramipour K, et al. Baseline physical activity is associated with reduced mortality and disease outcomes in COVID-19: a systematic review and meta-analysis. Rev Med Virol 2022: 32(5) e2349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Edwards KM, Pung MA, Tomfohr LM, et al. Acute exercise enhancement of pneumococcal vaccination response: a randomised controlled trial of weaker and stronger immune response. Vaccine 2012; 30(45): 6389–6395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ranadive SM, Cook M, Kappus RM, et al. Effect of acute aerobic exercise on vaccine efficacy in older adults. Med Sci Sports Exerc 2014; 46(3): 455–461. [DOI] [PubMed] [Google Scholar]
- 18. Silberman DM, Wald MR, Genaro AMA. Acute and chronic stress exert opposing effects on antibody responses associated with changes in stress hormone regulation of T-lymphocyte reactivity. J Neuroimmunol 2003; 144(1–2): 53–60. [DOI] [PubMed] [Google Scholar]
- 19. Pretty IA. Caries detection and diagnosis: novel technologies. J Dent 2006; 34(10): 727–739. [DOI] [PubMed] [Google Scholar]
- 20. Pacheco-López G, Engler H, Niemi M-B, et al. Expectations and associations that heal: immunomodulatory placebo effects and its neurobiology. Brain Behav Immun 2006; 20(5): 430–446. [DOI] [PubMed] [Google Scholar]
- 21. Ledo A, Schub D, Ziller C, et al. Elite athletes on regular training show more pronounced induction of vaccine-specific T-cells and antibodies after tetravalent influenza vaccination than controls. Brain Behav Immun 2020; 83: 135–145. [DOI] [PubMed] [Google Scholar]
- 22. Woods JA, Keylock KT, Lowder T, et al. Cardiovascular exercise training extends influenza vaccine seroprotection in sedentary older adults: the immune function intervention trial. J Am Geriatr Soc 2009; 57(12): 2183–2191. [DOI] [PubMed] [Google Scholar]
- 23. Feraoun Y, Maisonnasse P, Le Grand R, et al. COVID-19, des vaccins à la vitesse de l’éclair. Med Sci 2021; 37(8–9): 759–772. [DOI] [PubMed] [Google Scholar]
- 24. Ghram A, Moalla W, Lavie CJ. Vaccine and physical activity in the era of COVID-19 pandemic. Prog Cardiovasc Dis 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. de Araújo AL, Silva LCR, Fernandes JR, et al. Elderly men with moderate and intense training lifestyle present sustained higher antibody responses to influenza vaccine. Age 2015; 37(6): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pascoe AR, Singh MAF, Edwards KM. The effects of exercise on vaccination responses: a review of chronic and acute exercise interventions in humans. Brain Behav Immun 2014; 39: 33–41. [DOI] [PubMed] [Google Scholar]
- 27. Duggal NA, Pollock RD, Lazarus NR, et al. Major features of immunesenescence, including reduced thymic output, are ameliorated by high levels of physical activity in adulthood. Aging Cell 2018; 17(2): e12750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Nieman DC. Coronavirus disease-2019: a tocsin to our aging, unfit, corpulent, and immunodeficient society. J Sport Health Sci 2020; 9(4): 293–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Duggal NA, Niemiro G, Harridge SDR, et al. Can physical activity ameliorate immunosenescence and thereby reduce age-related multi-morbidity? Nat Rev Immunol 2019; 19(9): 563–572. [DOI] [PubMed] [Google Scholar]
- 30. Song Y, Ren F, Sun D, et al. Benefits of exercise on influenza or pneumonia in older adults: a systematic review. Int J Environ Res Public Health 2020; 17(8): 2655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Tissot N, Brunel A-S, Bozon F, et al. Patients with history of covid-19 had more side effects after the first dose of covid-19 vaccine. Vaccine 2021; 39(36): 5087–5090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chastin SFM, Abaraogu U, Bourgois JG, et al. Effects of regular physical activity on the immune system, vaccination and risk of community-acquired infectious disease in the general population: systematic review and meta-analysis. Sports Med 2021; 51(8): 1673–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Denay KL, Breslow RG, Turner MN, et al. ACSM call to action statement: COVID-19 considerations for sports and physical activity. Curr Sports Med Rep 2020; 19(8): 326–328. [DOI] [PubMed] [Google Scholar]
- 34. MacKinnon LT. Overtraining effects on immunity and performance in athletes. Immunol Cell Biol 2000; 78(5): 502–509. [DOI] [PubMed] [Google Scholar]
- 35. Quek. Exercising Right After Taking the Vaccine, 2021. https://aktivintel.com/exercising-right-after-taking-the-vaccine/
- 36. Pollock RD, Carter S, Velloso CP, et al. An investigation into the relationship between age and physiological function in highly active older adults. J Physiol 2015; 593(3): 657–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rao RR, Long JZ, White JP, et al. Meteorin-like is a hormone that regulates immune-adipose interactions to increase beige fat thermogenesis. Cell 2014; 157(6): 1279–1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Whitham M, Chan MHS, Pal M, et al. Contraction-induced interleukin-6 gene transcription in skeletal muscle is regulated by c-Jun terminal kinase/activator protein-1. J Biol Chem 2012; 287(14): 10771–10779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Whitham M, Parker BL, Friedrichsen M, et al. Extracellular vesicles provide a means for tissue crosstalk during exercise. Cell Metab 2018; 27(1): 237–251. [DOI] [PubMed] [Google Scholar]
- 40. El-Shitany NA, Harakeh S, Badr-Eldin S, et al. Minor to moderate side effects of Pfizer-BioNTech COVID-19 vaccine among Saudi residents: a retrospective cross-sectional study. Int J Gen Med 2021; 14: 1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wong GCH, Narang V, Lu Y, et al. Hallmarks of improved immunological responses in the vaccination of more physically active elderly females. Exercise Immunol Rev 2019; 25: 20–33. [PubMed] [Google Scholar]
- 42. Hallam J, Jones T, Alley J, et al. Exercise after influenza or COVID-19 vaccination increases serum antibody without an increase in side effects. Brain Behav Immun 2022; 102: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Smith TP, Kennedy SL, Fleshner M. Influence of age and physical activity on the primary in vivo antibody and T cell-mediated responses in men. J Appl Physiol 2004; 97(2): 491–498. [DOI] [PubMed] [Google Scholar]
- 44. Kohut ML, Cooper MM, Nickolaus MS, et al. Exercise and psychosocial factors modulate immunity to influenza vaccine in elderly individuals. J Gerontol A: Biol Sci Med Sci 2002; 57(9): M557–M562. [DOI] [PubMed] [Google Scholar]
- 45. Bohn-Goldbaum E, Pascoe A, Singh MF, et al. Acute exercise decreases vaccine reactions following influenza vaccination among older adults. Brain Behav Immun Health 2020; 1: 100009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Laar RA, Zhang Z, Menhas R, et al. Impact of coronavirus disease of 2019 vaccine on health and physical activities among physical education students in China. Front Public Health 2022; 10: 889311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Nieman DC, Wentz LM. The compelling link between physical activity and the body’s defense system. J Sport Health Sci 2019; 8(3): 201–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Laddu DR, Lavie CJ, Phillips SA, et al. Physical activity for immunity protection: inoculating populations with healthy living medicine in preparation for the next pandemic. Prog Cardiovasc Dis 2021; 64: 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Long JE, Ring C, Drayson M, et al. Vaccination response following aerobic exercise: can a brisk walk enhance antibody response to pneumococcal and influenza vaccinations? Brain Behav Immun 2012; 26(4): 680–687. [DOI] [PubMed] [Google Scholar]
- 50. Tande AJ, Pollock BD, Shah ND, et al. Impact of the COVID-19 vaccine on asymptomatic infection among patients undergoing pre-procedural COVID-19 molecular screening. Clin Infect Dis 2021; 7(1): 59–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Romero-Brufau S, Chopra A, Ryu AJ, et al. Public health impact of delaying second dose of BNT162b2 or mRNA-1273 covid-19 vaccine: simulation agent based modeling study. BMJ 2021; 373: n1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lee VY, Booy R, Skinner SR, et al. The effect of exercise on local and systemic adverse reactions after vaccinations–outcomes of two randomized controlled trials. Vaccine 2018; 36(46): 6995–7002. [DOI] [PubMed] [Google Scholar]
- 53. Edwards KM, Burns VE, Reynolds T, et al. Acute stress exposure prior to influenza vaccination enhances antibody response in women. Brain Behav Immun 2006; 20(2): 159–168. [DOI] [PubMed] [Google Scholar]