Abstract
Objectives
This review was designed to update our earlier systematic review which evaluated both published and unpublished evidence on the incidence of traumatic spinal cord injury (TSCI) worldwide.
Methods
We used various search methods including strategic searching, reference checking, searching for grey literature, contacting registries, authors, and organizations requesting unpublished data, browsing related websites, and hand searching key journals. The quality of included studies was evaluated by Joanna Briggs Institute Critical Appraisal Tools. Records published between April 2013 and May 2020 were added to the original systematic review.
Results
Overall, 58 resources including 45 papers, 10 SCI registry reports, 1 book, and 2 theses were retrieved. We found TSCI incidence data for eight new countries, which overall shapes our knowledge of TSCI incidence for 49 countries. The incidence of TSCI ranges from 3.3 to 195.4 cases per million (cpm) based on subnational studies and from 5.1 to 150.48 cpm based on national studies. Most of the studies were low quality, lacked consistent case selection due to unclear definition of TSCI and unclear ascertainment methods.
Conclusions
There is an increasing number of publications in the literature focusing on the epidemiologic data of TSCI. The absence of a standard form of reporting TSCI hinders the comparability of data across different data sources. Use of various definitions for TSCI may lead to heterogeneity in reports. Use of sensitivity analyses based on reasonable classification criteria can aid in offering a uniform set of case identification and ascertainment criteria for TSCI.
Keywords: Spinal cord injury, Incidence, Epidemiology
Abbreviations: TSCI, Traumatic Spinal Cord Injury; CPM, Cases Per Million; InSCI, The International Spinal Cord Injury; PICO, Population, Intervention, Comparator, and Outcome; CoCoPop, Condition, Context, and Population; TSI, Traumatic spinal injuries; PHM, Prehospital mortality; JBI, Joanna Briggs Institute; ASCIR, Australian Spinal Cord Injury Register; AMR, American region; EMR, Eastern Mediterranean region; EUR, European Region; WPR, Western Pacific Region; SEAR, South East Asia Region; ISCoS, International Spinal Cord Society; ICD, International Codes of Disease; SwiSCI, Swiss Spinal Cord Injury
1. Introduction
Rationale: Traumatic Spinal Cord Injury (TSCI) is a devastating but preventable condition with high morbidity and mortality. The lack of curative treatment for TSCI necessitates to understand epidemiology and etiologies of this condition to promote practical preventive strategies. Reports of SCI have been heterogeneous in previous publications among countries and SCI centers mainly because of different data-gathering methods, case defining approaches, and the various socio-economic structures of the countries.1,2 Recently, efforts have been undertaken to homogenously describe the true epidemiology of SCI.3 The International Spinal Cord Injury (InSCI) study is a good example in this regard. This study was conducted in all six WHO regions with a uniform sampling strategy to improve health and function of patients with SCI; however, the impact of this study on the healthcare system of the participating countries is not available yet.
In a previous systematic review, our team addressed the worldwide incidence of TSCI up to April 29th, 2013.4 In that review, after searching the published and grey literature, data was limited to forty-one countries regarding the incidence of TSCI, which are representative of about 20% of countries in the world. Moreover, most of the available literature had evaluated the epidemiologic aspects of TSCI in high-income developed countries.
Objectives: Considering the newly recommended protocols for conduction of SCI epidemiologic assessment,5 we aimed to assess reported publications in compliance with guidelines and update the knowledge on TSCI incidence worldwide.5,6
2. Material and methods
This systematic review has been conducted utilizing methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data.7
3. Eligibility criteria
3.1. Inclusion criteria
Instead of applying conventional population, intervention, comparator, and outcome (PICO) structure as inclusion criteria we used CoCoPop model (condition, context, and population) as suggested by Munn et al.7
3.2. Condition
Spinal cord injury has been defined as “an acute, traumatic lesion of neural elements in the spinal canal (spinal cord and cauda equina) resulting in temporary or permanent sensory deficit, motor deficit, or bladder/bowel dysfunction.8” Such damage can be result of an internal non-traumatic etiology (e.g. tumor or disease), or external etiology (e.g. transport-related injuries, fall, or violence). Therefore, SCI is often described in terms of traumatic or non-traumatic. In this review, we excluded studies of non-traumatic or mixed SCI if they were indistinguishable. Another point to consider is the injury to the spinal cord. We separated Traumatic spinal injuries (TSI) from TSCI. Studies of TSI without mentioning the cord injury were excluded. Studies focusing on a certain injury level (e.g. cervical SCI), specific etiology (e.g. sports-related SCI), or specific target population (e.g. workers) were also excluded.
3.3. Context
We included both national and subnational studies if they reported the incidence rate of TSCI or provided enough information regarding their catchment area and population at risk in order to estimate the incidence. Studies that reported the epidemiology of TSCI in a region within a country such as a state, city, etc. were considered subnational. In contrast those studies that considered the whole population of a country were considered national. Studies reporting only prevalence figures were excluded.
3.4. Population
In the current review we excluded studies of pediatric-onset (<16 years) TSCI.
One major source of heterogeneity among study rates of TSCI is believed to stem from inclusion or exclusion of prehospital mortality (PHM).9 In Order to homogenize the incidence rates, we examined the inclusion of PHM in all studies. There was no restriction for data sources or study designs. All observational epidemiological studies containing relevant information, either survey or registry-based studies were eligible to include.
4. Information sources
We searched EMBASE via Ovid SP and PubMed (including MEDLINE and PubMed Central). We also reviewed the references of our retrieved eligible studies in order to find additional relevant articles that may have been missed from database searching. Relevant abstracts from conference proceedings were also collected and checked for full-text availability. The grey literature was searched manually as previously described.4 In brief, we used 13 grey literature resources and 14 websites, and emailed 306 investigators. The search was performed on 5th may 2020.
5. Search strategy
We adopted our previous search strategy, which is described in details elsewhere.4 In short, for optimal retrieval of available information, we used different search methods including strategic searching, reference checking, searching for grey literature, contacting registries, authors, and organizations requesting for unpublished data, browsing related websites, and hand searching key journals.
We used the terms ‘Spinal cord injury’, ‘incidence’, ‘prevalence’ and ‘epidemiology’ as keywords (Appendix A). In this review, our search was primarily aimed to gather all published and unpublished papers after April 29th, 2013 (last date of the previous search), therefore we restricted the date of search to those records entered into databases (entry date) after April 29th, 2013. However, we checked reference lists of systematic reviews as of 20101,10, 11, 12, 13, 14, 15 to avoid losing any potentially missed paper before 2013. There were no language or country limitation in the search process in all resources.
6. Selection process, data collection process and data items
Two independent reviewers (S.F.M and M.A.D.O) screened the titles and then the abstracts of each retrieved record from the literature. Then the full-texts of selected records were assessed for inclusion based on eligibility criteria. The disagreements between two researchers were resolved either by consensus or the third reviewer (S.B.J) made the final decision. After inclusion of relevant full-texts, two independent authors (M.A.D.O and S.F.M) extracted the following information from each record: type of study (registry-based or survey-based), extent of study (national vs. subnational level), coverage years, raw data of study (if available), number of cases, age and incidence report, type of SCI (traumatic vs. non-traumatic), inclusion or exclusion of PHM, timing of data collection (prospective or retrospective), study design, and study scale (population-based, hospital-based, rehabilitation-based, etc.). The third author (S.B.J) double-checked the extracted data for accuracy and completeness.
7. Critical appraisal
The quality of included studies was evaluated by appropriate Joanna Briggs Institute (JBI) Critical Appraisal Tools based on study design.16 For the aims of this study we used the checklist for case-series. This checklist contains 10 questions which are related to areas of risk of bias assessment including adequate reporting, statistical analysis. Each question in the checklist can be answered as “yes, no, unclear or not applicable”. Each study was assessed by two independent researchers (S.F.M and M.A.D.O). Disagreements between individual judgments were resolved by discussion or decision of a third researcher (S.B.J) whenever needed. We calculated the total score for methodological quality of studies by adding up the “Yes” answers to each question of the quality appraisal tool. Our criteria for answering each question of the described checklist can be found in Appendix B.
Although we did not exclude any study based on critical appraisal, we qualified all papers to identify the areas of potential bias.
8. Data synthesis
Data synthesis was performed by tabular summary approach.7
9. Results
9.1. Study inclusion
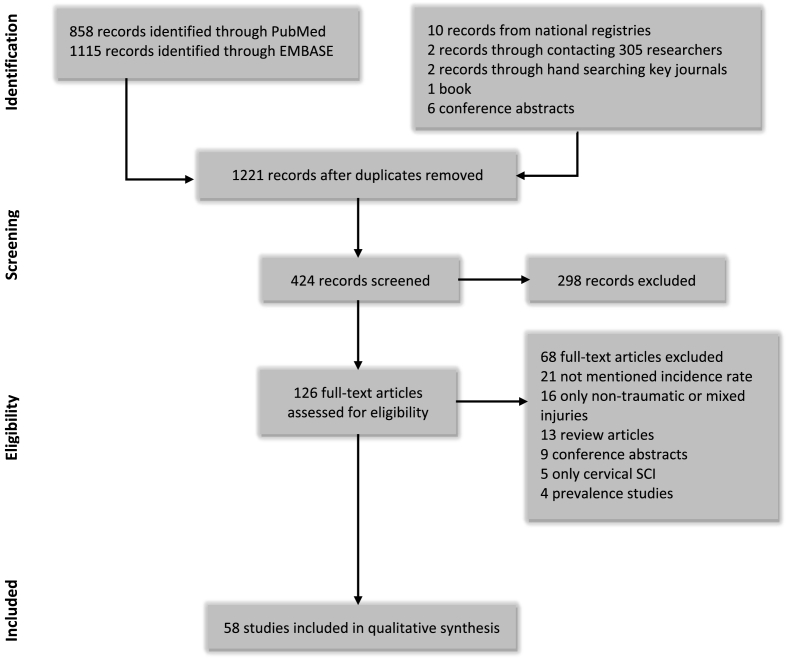
A total of 858 records from Medline and 1115 records from EMBASE were identified and included in the EndNote X8 database. After excluding 752 duplicate records, titles and abstracts of 1221 records were screened by two members of the team (M.C and M.S). After exclusion of 797 irrelevant records, 424 papers were screened and assessed using the inclusion criteria. This process limited the number of papers to 128, of which 70 were excluded: 23 did not mention any incidence rate, 16 reported non-traumatic or mixed injuries, 22 records were either review articles or conference abstracts, five papers only reported cervical SCI, and four were prevalence study. We identified 10 reports from national registries,17, 18, 19, 20, 21, 22, 23, 24, 25, 26 one book,27 as well as data from New Zealand and Russia through personal communications. Overall, we identified 58 reports2,9,14,17, 18, 19, 20, 21, 22, 23, 24, 25, 26,28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71 for 31 countries worldwide as of 2013 (Fig. 1).
Fig. 1.
Flow diagram of studies based on PRISMA statement.
9.2. Methodological quality
The included studies were critically appraised as described in critical appraisal section of methods. The methodology utilized in nine reports from national registry of Australia were similar, therefore we grouped them to one record under “Australian Spinal Cord Injury Register (ASCIR) reports” title.
There were nine relevant items in the questionnaire, thus the maximum score was 9. The-included studies’ scores ranged from four to nine. The highest risk of bias was attributed to the process of case selection due to unclear definition of TSCI and ascertainment methods. Results of the methodological quality evaluation are shown in Table 1.
Table 1.
Methodological assessment scores of included studies.
| Country | Source | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Total Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Australia | ASCIR reports | Y | U | Y | Y | Y | Y | Y | NA | Y | Y | 8 |
| Moorin et al | Y | U | Y | Y | Y | N | Y | NA | Y | Y | 7 | |
| Beck et al | Y | U | Y | U | Y | Y | Y | NA | Y | Y | 7 | |
| New et al | Y | U | Y | U | U | Y | Y | NA | Y | U | 5 | |
| Austria | Majdan et al | Y | U | Y | Y | Y | N | Y | NA | Y | Y | 7 |
| Botswana | Löfvenmark et al | U | U | U | U | N | Y | Y | NA | Y | Y | 4 |
| Canada | Thompson et al | Y | U | Y | Y | Y | Y | Y | NA | Y | Y | 8 |
| Lenehan et al | Y | U | Y | Y | Y | Y | Y | NA | Y | Y | 8 | |
| Czech Republic | Kriz et al | Y | U | U | Y | Y | Y | Y | NA | Y | Y | 7 |
| Denmark | Noe et al | Y | U | U | Y | Y | N | Y | NA | Y | Y | 6 |
| Estonia | Sabre et al | Y | U | Y | Y | Y | Y | Y | NA | Y | Y | 8 |
| Sabre et al | Y | U | Y | Y | Y | Y | Y | NA | Y | Y | 8 | |
| Sabre et al | Y | U | Y | Y | Y | N | Y | NA | Y | Y | 7 | |
| Finland | Niemi-nikkola et al | Y | U | Y | Y | Y | N | Y | NA | Y | Y | 6 |
| Koskinen et al | Y | U | U | Y | Y | Y | Y | NA | Y | Y | 7 | |
| Former Yugoslav Republic of Macedonia | Jakimovska et al | U | Y | Y | Y | Y | Y | Y | NA | Y | Y | 8 |
| Iceland | Kristinsdóttir et al. | Y | U | Y | Y | Y | Y | Y | NA | Y | Y | 8 |
| Iran | Sharif-alhoseini and Rahimi-Movaghar | Y | U | U | N | N | Y | Y | NA | Y | Y | 5 |
| Ireland | Smith et al | Y | U | Y | Y | Y | N | U | NA | Y | U | 5 |
| Smith et al | Y | U | U | Y | Y | Y | Y | NA | Y | Y | 7 | |
| Italy | Ferro et al | Y | Y | U | Y | Y | N | Y | NA | Y | Y | 7 |
| Japan | Katoh et al | N | U | U | Y | Y | Y | Y | NA | Y | Y | 6 |
| Kudo et al | Y | Y | Y | Y | Y | Y | Y | NA | Y | Y | 9 | |
| Latvia | Nulle et al | U | U | U | U | Y | Y | Y | NA | Y | Y | 5 |
| Netherland | Nijendijk et al | Y | U | Y | Y | N | N | Y | NA | Y | Y | 6 |
| New Zealand | Mitchell et al | Y | U | U | Y | Y | Y | Y | NA | Y | Y | 7 |
| Norway | Halvorsen et al | Y | U | U | Y | Y | Y | Y | NA | Y | Y | 7 |
| Pakistan | Bilal and Mujeeb-Ur-Rahman | Y | U | U | N | U | Y | Y | NA | Y | U | 4 |
| Russia | Mirzaeva et al | Y | Y | Y | Y | Y | Y | Y | NA | Y | Y | 9 |
| Lobzin et al | Y | Y | Y | Y | Y | Y | Y | NA | Y | Y | 9 | |
| Scotland | McCaughey et al | Y | U | U | Y | Y | Y | Y | NA | Y | Y | 7 |
| South Africa | Joseph et al | Y | U | U | Y | Y | Y | Y | NA | Y | Y | 7 |
| Pefile et al | Y | U | U | Y | N | Y | Y | NA | Y | Y | 6 | |
| Philips et al | Y | Y | Y | Y | Y | Y | Y | NA | Y | Y | 9 | |
| South Korea | Choi et al | Y | U | Y | Y | Y | N | Y | NA | Y | Y | 7 |
| Spain | Montoto-marqués et al | Y | Y | Y | Y | Y | Y | Y | NA | Y | Y | 9 |
| Alcacer et al | Y | Y | Y | Y | Y | Y | Y | NA | Y | Y | 9 | |
| Bárbara-bataller et al | Y | U | Y | Y | Y | Y | Y | NA | Y | Y | 8 | |
| Bárbara-bataller et al | Y | U | U | Y | Y | Y | Y | NA | Y | Y | 7 | |
| Sweden | Joseph et al | Y | Y | Y | Y | Y | Y | Y | NA | Y | Y | 9 |
| Switzerland | Chamberlain et al | Y | U | Y | Y | Y | N | Y | NA | Y | Y | 7 |
| Chamberlain et al | Y | U | U | Y | Y | N | Y | NA | Y | Y | 6 | |
| Taiwan | Wu et al | Y | Y | Y | Y | Y | N | Y | NA | Y | Y | 8 |
| Tanzania | Moshi et al | U | U | U | Y | N | N | Y | NA | Y | Y | 4 |
| United States | Selvarajah et al | Y | U | Y | Y | Y | Y | Y | NA | Y | Y | 8 |
| Jain et al | Y | U | Y | Y | Y | N | Y | NA | Y | Y | 7 | |
| Selassie et al | Y | U | Y | Y | Y | N | Y | NA | Y | Y | 7 |
Q: Question; N, no; U, unclear; Y, yes; NA, not applicable; ASCIR: Australian Spinal Cord Injury Registry.
Q1: Were there clear criteria for inclusion in the case series?.
Q2: Was the condition measured in a standard, reliable way for all participants?.
Q3: Were valid methods used for identification of the condition for all participants included?.
Q4: Did the case series have consecutive inclusion of Participants?.
Q5: Did the case series have complete inclusion of participants?.
Q6: Was there clear reporting of the demographics of the participants in the study?.
Q7: Was the condition measured in a standard, reliable way for all participants?.
Q8: Were the outcomes or follow up results of cases clearly reported?.
Q9: Was there clear reporting of the presenting site(s)/clinic(s) demographic information?.
Q10: Was statistical analysis appropriate?.
9.3. Review findings
Similar to our previous study4 we categorized incidence data based on WHO classification of countries. Extracted data of incidence rates are shown in Table 2.
Table 2.
Summary of the included studies.
| WHO region | Country | Study source | Years of study | Type | Extend | Study design | No. of patients | Incidence rate per million | Prehospital mortality Included? | ISCoS∗ Format Utilized? |
Age range |
|---|---|---|---|---|---|---|---|---|---|---|---|
| AFR E | Botswana | Löfvenmark et al. | 2011–2012 | Survey | Subnational Gaborone |
Prospective hospital-based | 52 | 13 | No | Yes | 0–99 |
| South Africa | Joseph et al. | 2013–2014 | Survey | Subnational Cape Town |
Prospective population-based | 147 | 75.6 | No | Yes | 18–99 | |
| Phillips et al. | 2013–2014 | Survey | Subnational Cape Town |
Prospective population-based | 160 | 61.1 | No | Yes | 18–99 | ||
| Pefile et al. | 2009–2015 | Survey | Subnational KwaZulu-Natal and the Eastern Cape provinces |
Retrospective Hospital-based |
84 | 55.19 | No | Yes | 16–99 | ||
| Tanzania | Moshi et al. | 2010–2014 | Survey | Subnational Kilimanjaro rural region, north-east Tanzania |
Retrospective Hospital-based |
218 | 26 | No | Yes | 0–99 | |
| AMR A | Canada | Thompson et al. | 2000 | Registry | Subnational Québec |
Retrospective Hospital-based | 46 | 10.6 | No | No | 0–99 |
| 2001 | Registry | Subnational Québec |
Retrospective Hospital-based | 54 | 12.4 | No | No | 0–99 | |||
| 2002 | Registry | Subnational Québec |
Retrospective Hospital-based | 61 | 13.9 | No | No | 0–99 | |||
| 2003 | Registry | Subnational Québec |
Retrospective Hospital-based | 53 | 12 | No | No | 0–99 | |||
| 2004 | Registry | Subnational Québec |
Retrospective Hospital-based | 100 | 22.5 | No | No | 0–99 | |||
| 2005 | Registry | Subnational Québec |
Retrospective Hospital-based | 101 | 22.6 | No | No | 0–99 | |||
| 2006 | Registry | Subnational Québec |
Retrospective Hospital-based | 79 | 17.6 | No | No | 0–99 | |||
| 2007 | Registry | Subnational Québec |
Retrospective Hospital-based | 93 | 20.5 | No | No | 0–99 | |||
| 2008 | Registry | Subnational Québec |
Retrospective Hospital-based | 81 | 17.7 | No | No | 0–99 | |||
| 2009 | Registry | Subnational Québec |
Retrospective Hospital-based | 80 | 17.3 | No | No | 0–99 | |||
| 2010 | Registry | Subnational Québec |
Retrospective Hospital-based | 83 | 17.8 | No | No | 0–99 | |||
| 2000–2010 | Registry | Subnational Québec |
Retrospective Hospital-based | 831 | 16.8 | No | No | 0–99 | |||
| Lenehan et al | 1995 | Registry and Survey | Subnational British Columbia |
Prospective Population-based |
102 | 45.6 | No | No | 15–99 | ||
| 1996 | Registry and Survey | Subnational British Columbia |
Prospective Population-based |
106 | 46 | No | No | 15–99 | |||
| 1997 | Registry and Survey | Subnational British Columbia |
Prospective Population-based |
97 | 43.1 | No | No | 15–99 | |||
| 1998 | Registry and Survey | Subnational British Columbia |
Prospective Population-based |
102 | 42.3 | No | No | 15–99 | |||
| 1999 | Registry and Survey | Subnational British Columbia |
Prospective Population-based |
77 | 32.7 | No | No | 15–99 | |||
| 2000 | Registry and Survey | Subnational British Columbia |
Prospective Population-based |
103 | 43.8 | No | No | 15–99 | |||
| 2001 | Registry and Survey | Subnational British Columbia |
Prospective Population-based |
83 | 37.4 | No | No | 15–99 | |||
| 2002 | Registry and Survey | Subnational British Columbia |
Prospective Population-based |
85 | 36.3 | No | No | 15–99 | |||
| 2003 | Registry and Survey | Subnational British Columbia |
Prospective Population-based |
87 | 35.4 | No | No | 15–99 | |||
| 2004 | Registry and Survey | Subnational British Columbia |
Prospective Population-based |
88 | 37 | No | No | 15–99 | |||
| US | Selvarajah et al. | 2007 | Registry | NationalUSA | ProspectiveOther | 13,169 | 57 | No | No | 18–109 | |
| 2008 | Registry | National USA |
Prospective Other |
14,207 | 58.4 | No | No | 18–109 | |||
| 2009 | Registry | National USA |
Prospective Other |
12,526 | 56.4 | No | No | 18–109 | |||
| 2007–2009 | Registry | National USA |
Prospective Other |
43137 | 56.4 | No | No | 18–109 | |||
| Jain et al. | 1993 | Registry | National USA |
Retrospective Population-based |
2659 | 53.1 | No | No | 0–99 | ||
| 1994 | Registry | National USA |
Retrospective Population-based |
2680 | 53.58 | No | No | 0–99 | |||
| 1995 | Registry | National USA |
Retrospective Population-based |
3112 | 54.94 | No | No | 0–99 | |||
| 1996 | Registry | National USA |
Retrospective Population-based |
2983 | 52.87 | No | No | 0–99 | |||
| 1997 | Registry | National USA |
Retrospective Population-based |
3048 | 48.07 | No | No | 0–99 | |||
| 1998 | Registry | National USA |
Retrospective Population-based |
2848 | 53.63 | No | No | 0–99 | |||
| 1999 | Registry | National USA |
Retrospective Population-based |
2946 | 51.65 | No | No | 0–99 | |||
| 2000 | Registry | National USA |
Retrospective Population-based |
2849 | 47.77 | No | No | 0–99 | |||
| 2001 | Registry | National USA |
Retrospective Population-based |
2611 | 45.06 | No | No | 0–99 | |||
| 2002 | Registry | National USA |
Retrospective Population-based |
3025 | 48.97 | No | No | 0–99 | |||
| 2003 | Registry | National USA |
Retrospective Population-based |
3180 | 51.02 | No | No | 0–99 | |||
| 2004 | Registry | National USA |
Retrospective Population-based |
3993 | 63.86 | No | No | 0–99 | |||
| 2005 | Registry | National USA |
Retrospective Population-based |
3021 | 47.78 | No | No | 0–99 | |||
| 2006 | Registry | National USA |
Retrospective Population-based |
3453 | 54.57 | No | No | 0–99 | |||
| 2007 | Registry | National USA |
Retrospective Population-based |
3357 | 53.66 | No | No | 0–99 | |||
| 2008 | Registry | National USA |
Retrospective Population-based |
3274 | 50.4 | No | No | 0–99 | |||
| 2009 | Registry | National USA |
Retrospective Population-based |
3217 | 50.18 | No | No | 0–99 | |||
| 2010 | Registry | National USA |
Retrospective Population-based |
4106 | 64.3 | No | No | 0–99 | |||
| 2011 | Registry | National USA |
Retrospective Population-based |
3354 | 50.15 | No | No | 0–99 | |||
| 2012 | Registry | National USA |
Retrospective Population-based |
3393 | 54.04 | No | No | 0–99 | |||
| Selassie et al. | 1998 | Registry | Subnational South Carolina |
Cross-sectional Population-based |
N/A | 66.9 | No | No | 22–99 | ||
| 2012 | Registry | Subnational South Carolina |
Cross-sectional Population-based |
N/A | 111.7 | No | No | 22–99 | |||
| 1998–2012 | Registry | Subnational South Carolina |
Cross-sectional Population-based |
3365 | 70.8 | No | No | 22–99 | |||
| EMR B | Iran | Sharif-Alhoseini and Rahimi-Movaghar | 2010–2011 | Survey | Subnational Tehran |
Retrospective Hospital-based |
138 | 10.5 | No | No | 0–99 |
| EMR D | Pakistan | Bilal and Mujeeb-Ur-Rahman | 2008 | Survey | Subnational Khyber Pukhtunkhwa |
Retrospective Rehabilitation-based |
242 | 11 | No | No | 0–99 |
| 2009 | Survey | Subnational Khyber Pukhtunkhwa |
Retrospective Rehabilitation-based |
208 | 9.45 | No | No | 0–99 | |||
| 2010 | Survey | Subnational Khyber Pukhtunkhwa |
Retrospective Rehabilitation-based |
234 | 10.63 | No | No | 0–99 | |||
| 2011 | Survey | Subnational Khyber Pukhtunkhwa |
Retrospective Rehabilitation-based |
228 | 10.36 | No | No | 0–99 | |||
| 2012 | Survey | Subnational Khyber Pukhtunkhwa |
Retrospective Rehabilitation-based |
224 | 10.18 | No | No | 0–99 | |||
| 2008–2012 | Survey | Subnational Khyber Pukhtunkhwa |
Retrospective Rehabilitation-based |
1136 | 10.23 | No | No | 0–99 | |||
| EUR A | Austria | Majdan et al. | 2002 | Registry | National Austria |
Retrospective Population-based | N/A | 15.96 | Yes | No | 0–99 |
| 2003 | Registry | National Austria |
Retrospective Population-based | N/A | 16.26 | Yes | No | 0–99 | |||
| 2004 | Registry | National Austria |
Retrospective Population-based | N/A | 14.07 | Yes | No | 0–99 | |||
| 2005 | Registry | National Austria |
Retrospective Population-based | N/A | 16.05 | Yes | No | 0–99 | |||
| 2006 | Registry | National Austria |
Retrospective Population-based | N/A | 12.57 | Yes | No | 0–99 | |||
| 2007 | Registry | National Austria |
Retrospective Population-based | N/A | 15.07 | Yes | No | 0–99 | |||
| 2008 | Registry | National Austria |
Retrospective Population-based | N/A | 20.79 | Yes | No | 0–99 | |||
| 2009 | Registry | National Austria |
Retrospective Population-based | N/A | 19.66 | Yes | No | 0–99 | |||
| 2010 | Registry | National Austria |
Retrospective Population-based | N/A | 19.02 | Yes | No | 0–99 | |||
| 2011 | Registry | National Austria |
Retrospective Population-based | N/A | 18.12 | Yes | No | 0–99 | |||
| 2012 | Registry | National Austria |
Retrospective Population-based | N/A | 18.75 | Yes | No | 0–99 | |||
| 2002–2012 | Registry | National Austria |
Retrospective Population-based | 1543 | 16.96 | Yes | No | 0–99 | |||
| Czech republic | Kriz et al. | 2006–2015 | Survey | National Czech republic |
Prospective Population-based |
1736 | 16.5 | No | No | 0–99 | |
| Denmark | NOE et al. | 1990–1994 | Survey | Subnational Western Denmark |
Retrospective Rehabilitation-based | 153 | 10.7 | No | Yes | 0–99 | |
| 1995–1999 | Survey | Subnational Western Denmark |
Retrospective Rehabilitation-based | 129 | 8.7 | No | Yes | 0–99 | |||
| 2000–2004 | Survey | Subnational Western Denmark |
Retrospective Rehabilitation-based | 174 | 11.8 | No | Yes | 0–99 | |||
| 2005–2009 | Survey | Subnational Western Denmark |
Retrospective Rehabilitation-based | 159 | 10.6 | No | Yes | 0–99 | |||
| 2010–2012 | Survey | Subnational Western Denmark |
Retrospective Rehabilitation-based | 76 | 8.3 | No | Yes | 0–99 | |||
| 1990–2012 | Survey | Subnational Western Denmark |
Retrospective Rehabilitation-based | 691 | 10.2 | No | Yes | 0–99 | |||
| Finland | Koskinen et al. | 2012–2013 | Survey | Subnational Oulu and Tampere |
Prospective Population-based |
77 | 25.1 | No | Yes | 0–99 | |
| Niemi-Nikkola et al. | 2007–2012 | Survey | Subnational Oulu |
Retrospective Hospital-based | 101 | 36.4 | No | Yes | 0–99 | ||
| Ireland | Smith et al. | 2010 | Survey | National Ireland |
Retrospective Population-based |
57 | 12.5 | No | Yes | 0–99 | |
| 2011 | Survey | National Ireland |
Retrospective Population-based |
56 | 12.2 | No | Yes | 0–99 | |||
| 2012 | Survey | National Ireland |
Retrospective Population-based |
60 | 13.1 | No | Yes | 0–99 | |||
| 2013 | Survey | National Ireland |
Retrospective Population-based |
61 | 13.3 | No | Yes | 0–99 | |||
| 2014 | Survey | National Ireland |
Retrospective Population-based |
53 | 11.5 | No | Yes | 0–99 | |||
| 2015 | Survey | National Ireland |
Retrospective Population-based |
60 | 12.9 | No | Yes | 0–99 | |||
| 2010–2015 | Survey | National Ireland |
Retrospective Population-based |
347 | 12.6 | No | Yes | 0–99 | |||
| Smith et al. | 2016 | Survey | National Ireland |
Prospective Population-based |
61 | 12.8 | No | Yes | 0–99 | ||
| Italy | Ferro et al. | 2013–2014 | Survey | National Italy |
Prospective Population-based |
445 | 14.7 | No | Yes | 0–99 | |
| Speziali et al. | 2013 | Survey | Subnational Umbria |
Prospective Hospital-based |
19 | 21.4 | Not available | Not available | 0–99 | ||
| Netherlands | Nijendijk et al. | 2010 | Registry | National Netherlands |
Retrospective Other |
185 | 14 | No | No | 0–99 | |
| Norway | Sabre et al. | 1997–2001 | Survey | Subnational Western Norway |
Retrospective Population-based |
71 | 24.9 | No | Yes | 0–99 | |
| Halvorsen et al. | 2012 | Registry | National Norway |
Cross-sectional Population-based |
57 | 11.4 | No | Yes | 0–99 | ||
| 2013 | Registry | National Norway |
Cross-sectional Population-based |
60 | 11.9 | No | Yes | 0–99 | |||
| 2014 | Registry | National Norway |
Cross-sectional Population-based |
81 | 15.9 | No | Yes | 0–99 | |||
| 2015 | Registry | National Norway |
Cross-sectional Population-based |
76 | 14.7 | No | Yes | 0–99 | |||
| 2016 | Registry | National Norway |
Cross-sectional Population-based |
75 | 14.4 | No | Yes | 0–99 | |||
| 2012–2016 | Registry | National Norway |
Cross-sectional Population-based |
349 | 13.6 | No | Yes | 0–99 | |||
| United Kingdome | McCaughey et al. | 1994–1998 | Survey | Subnational Scotland |
Retrospective Other |
N/A | 13.3 | No | Yes | 12–99 | |
| 1999–2003 | Survey | Subnational Scotland |
Retrospective Other |
N/A | 15.9 | No | Yes | 12–99 | |||
| 2004–2008 | Survey | Subnational Scotland |
Retrospective Other |
N/A | 17.5 | No | Yes | 12–99 | |||
| 2009–2013 | Survey | Subnational Scotland |
Retropective Other |
N/A | 17 | No | Yes | 12–99 | |||
| 1994–2013 | Survey | Subnational Scotland |
Retrospective Other |
1638 | 15.9 | No | Yes | 12–99 | |||
| Spain | Montoto-Marqués et al. | 1995–2014 | Survey | Subnational Galicia |
Ambispective Hospital-based |
1195 | 21.7 | No | No | 0–99 | |
| 1995–1999 | Survey | Subnational Galicia |
Ambispective Hospital-based |
335 | 23.4 | No | No | 0–99 | |||
| 2000–2004 | Survey | Subnational Galicia |
Ambispective Hospital-based |
292 | 19.7 | No | No | 0–99 | |||
| 2005–2009 | Survey | Subnational Galicia |
Ambispective Hospital-based |
289 | 20.9 | No | No | 0–99 | |||
| 2010–2014 | Survey | Subnational Galicia |
Ambispective Hospital-based |
279 | 16.7 | No | No | 0–99 | |||
| Bárbara-Bataller et al. | 2000–2005 | Survey | Subnational Gran Canaria Islands |
Retrospective Hospital-based |
66 | 17.8 | No | No | 15–99 | ||
| 2006–2010 | Survey | Subnational Gran Canaria Islands |
Retrospective Hospital-based |
41 | 9.7 | No | No | 15–99 | |||
| 2011–2014 | Survey | Subnational Gran Canaria Islands |
Retrospective Hospital-based |
34 | 9.9 | No | No | 15–99 | |||
| 2000–2014 | Survey | Subnational Gran Canaria Islands |
Retrospective Hospital-based |
141 | 12 | No | No | 15–99 | |||
| Bárbara-Bataller et al. | 2001–2005 | Survey | Subnational Canarias region |
Prospective Hospital-based |
116 | 13 | No | No | 15–99 | ||
| 2006–2010 | Survey | Subnational Canarias region |
Prospective Hospital-based |
76 | 7.5 | No | No | 15–99 | |||
| 2011–2015 | Survey | Subnational Canarias region |
Prospective Hospital-based |
90 | 8.5 | No | No | 15–99 | |||
| 2001–2015 | Survey | Subnational Canarias region |
Prospective Hospital-based |
282 | 9.3 | No | No | 15–99 | |||
| Sebastia-Alcacer et al. | 2001 | Survey | Subnational Valenciana |
Retrospective Hospital-based |
31 | 6 | No | No | 0–99 | ||
| 2002 | Survey | Subnational Valenciana |
Retrospective Hospital-based |
29 | 5.7 | No | No | 0–99 | |||
| 2003 | Survey | Subnational Valenciana |
Retrospective Hospital-based |
30 | 5.8 | No | No | 0–99 | |||
| 2004 | Survey | Subnational Valenciana |
Retrospective Hospital-based |
19 | 3.7 | No | No | 0–99 | |||
| 2005 | Survey | Subnational Valenciana |
Retrospective Hospital-based |
38 | 7.4 | No | No | 0–99 | |||
| 2006 | Survey | Subnational Valenciana |
Retrospective Hospital-based |
17 | 3.3 | No | No | 0–99 | |||
| 2007 | Survey | Subnational Valenciana |
Retrospective Hospital-based |
31 | 6 | No | No | 0–99 | |||
| 2008 | Survey | Subnational Valenciana |
Retrospective Hospital-based |
23 | 4.5 | No | No | 0–99 | |||
| 2009 | Survey | Subnational Valenciana |
Retrospective Hospital-based |
19 | 3.7 | No | No | 0–99 | |||
| 2010 | Survey | Subnational Valenciana |
Retrospective Hospital-based |
24 | 4.7 | No | No | 0–99 | |||
| 2001–2010 | Survey | Subnational Valenciana |
Retrospective Hospital-based |
261 | 5.1 | No | No | 0–99 | |||
| Sweden | Joseph et al. | 2014–2015 | Registry | Subnational greater Stockholm | Prospective Population-based |
45 | 19 | No | Yes | 18–99 | |
| Switzerland | Chamberlain et al. | 2005–2012 | Registry | National Switzerland |
Retrospective Population-based |
932 | 18 | No | Yes | 16–99 | |
| Chamberlain et al. | 2012–2013 | different data sources Registry | National Switzerland |
Retrospective Other |
Ranges from 231 to 621 based on case identification strategy | Ranges from 19.9 to 54.3 | No | Yes | 16–99 | ||
| EUR B | Poland | Tederko et al. | 2005–2008 | Survey | Subnational Lubuskie |
Retrospective Hospital-based |
343 | 14.5 | Not available | Not available | 0–99 |
| EUR C | Estonia | Sabre et al. | 1997–2001 | Survey | National Estonia |
Retrospective Population-based |
244 | 37.4 | No | Yes | 0–99 |
| Sabre et al. | 1997–2007 | Survey | National Estonia |
Retrospective Population-based |
595 | 39.4 | No | Yes | 0–99 | ||
| Sabre et al. | 2005–2007 | Survey | National Estonia |
Retrospective Population-based |
183 without PHM 391 with PHM |
43.8 without PHM 93.9 With PHM |
Yes | No | 0–99 | ||
| Former Yugoslav Republic of Macedonia | Jakimovska et al. | 2015–2016 | Survey | National Former Yugoslav Republic of Macedonia |
Prospective Hospital-based |
38 | 13 | No | Yes | 16–99 | |
| Iceland | Kristinsdóttir et al. | 2010–2014 | Survey | National Iceland |
Retrospective Population-based |
26 | 16 | No | Yes | 4–99 | |
| Lithuania | Juocevicius et al. | 2015 | Survey | National Lithuania |
Retrospective Rehabilitation-based |
NA | 24 | No | No | 18–99 | |
| Latvia | Nulle et al. | 2011 | Survey | National Latvia |
Retrospective Rehabilitation-based |
42 | 21 | No | Yes | 16–99 | |
| 2012 | Survey | National Latvia |
Retrospective Rehabilitation-based |
31 | 15.5 | No | Yes | 16–99 | |||
| 2013 | Survey | National Latvia |
Retrospective Rehabilitation-based |
21 | 10.5 | No | Yes | 16–99 | |||
| 2014 | Survey | National Latvia |
Retrospective Rehabilitation-based |
40 | 20 | No | Yes | 16–99 | |||
| 2011–2014 | Survey | National Latvia |
Retrospective Rehabilitation-based |
134 | 16.75 | No | Yes | 16–99 | |||
| Russia | Mirzaeva et al. | 2012 | Survey | Subnational Saint Petersburg |
Retrospective Population-based |
53 | 12.4 | No | Yes | 18–99 | |
| 2013 | Survey | Subnational Saint Petersburg |
Retrospective Population-based |
91 | 21.2 | No | Yes | 18–99 | |||
| 2014 | Survey | Subnational Saint Petersburg |
Retrospective Population-based |
79 | 18 | No | Yes | 18–99 | |||
| 2015 | Survey | Subnational Saint Petersburg |
Retrospective Population-based |
78 | 17.7 | No | Yes | 18–99 | |||
| 2016 | Survey | Subnational Saint Petersburg |
Retrospective Population-based |
60 | 13.6 | No | Yes | 18–99 | |||
| Lobzin et al. | 2012–2016 | Survey | Subnational Saint Petersburg |
Retrospective Population-based |
361 | 16.6 | No | Yes | 18–99 | ||
| WPR A | Australia | New et al. | 2011 | Survey and registry data | National Australia |
Retrospective Other |
470 or 721 based on case identification criteria | 21 or 32.3 | No | No | 0–99 |
| Moorin et al. | 2003–2008 | Registry | Subnational Western Australia |
Retrospective Population-based |
335 | 33 | No | No | 0–99 | ||
| Beck et al. | 2007–2016 | Registry | Subnational Victoria |
Retrospective Population-based |
706 | 12.5 | No | No | 0–99 | ||
| Tovell & Harrison et al. | 2008 | Registry | National Australia |
Prospective Population-based |
263 | 14 | No | No | 15–99 | ||
| Tovell & Harrison et al. | 2009 | Registry | National Australia |
Prospective Population-based |
227 | 12.3 | No | No | 15–99 | ||
| Tovell & Harrison et al. | 2010 | Registry | National Australia |
Prospective Population-based |
269 | 14.3 | No | No | 15–99 | ||
| Tovell et al. | 2011 | Registry | National Australia |
Prospective Population-based |
220 | 10.9 | No | No | 15–99 | ||
| Tovell et al. | 2012 | Registry | National Australia |
Prospective Population-based |
241 | 12.2 | No | No | 15–99 | ||
| Tovell et al. | 2013 | Registry | National Australia |
Prospective Population-based |
236 | 11.8 | No | No | 15–99 | ||
| Tovell et al. | 2014 | Registry | National Australia |
Prospective Population-based |
264 | 12.8 | No | No | 15–99 | ||
| Tovell et al. | 2015 | Registry | National Australia |
Prospective Population-based |
253 | 12.1 | No | No | 15–99 | ||
| Tovell et al. | 2016 | Registry | National Australia |
Prospective Population-based |
227 | 11.1 | No | No | 15–99 | ||
| Japan | Katoh et al. | 2011 | Survey | Subnational Tokushima |
Retrospective Population-based |
95 | 121.4 | No | No | 16–99 | |
| 2012 | Survey | Subnational Tokushima |
Retrospective Population-based |
91 | 117.1 | No | No | 16–99 | |||
| Kudo et al. | 2012 | Survey | Subnational Akita |
Retrospective Hospital-based |
111 | 104 | No | No | 0–99 | ||
| 2013 | Survey | Subnational Akita |
Retrospective Hospital-based |
90 | 86 | No | No | 0–99 | |||
| 2014 | Survey | Subnational Akita |
Retrospective Hospital-based |
89 | 86 | No | No | 0–99 | |||
| 2015 | Survey | Subnational Akita |
Retrospective Hospital-based |
72 | 70 | No | No | 0–99 | |||
| 2016 | Survey | Subnational Akita |
Retrospective Hospital-based |
87 | 86 | No | No | 0–99 | |||
| 2012–2016 | Survey | Subnational Akita |
Retrospective Hospital-based |
449 | 86 | No | No | 0–99 | |||
| New Zealand | Mitchell et al. | 2007 | Registry | National New Zealand |
Ambispective Population-based |
72 | 17.88 | No | Yes | 16–99 | |
| 2008 | Registry | National New Zealand |
Ambispective Population-based |
81 | 20.11 | No | Yes | 16–99 | |||
| 2009 | Registry | National New Zealand |
Ambispective Population-based |
91 | 22.59 | No | Yes | 16–99 | |||
| 2010 | Registry | National New Zealand |
Ambispective Population-based |
89 | 20.98 | No | Yes | 16–99 | |||
| 2011 | Registry | National New Zealand |
Ambispective Population-based |
92 | 21.69 | No | Yes | 16–99 | |||
| 2012 | Registry | National New Zealand |
Ambispective Population-based |
73 | 17.21 | No | Yes | 16–99 | |||
| 2013 | Registry | National New Zealand |
Ambispective Population-based |
99 | 23.34 | No | Yes | 16–99 | |||
| 2014 | Registry | National New Zealand |
Ambispective Population-based |
91 | 21.45 | No | Yes | 16–99 | |||
| 2015 | Registry | National New Zealand |
Ambispective Population-based |
126 | 29.70 | No | Yes | 16–99 | |||
| 2016 | Registry | National New Zealand |
Ambispective Population-based |
115 | 27.11 | No | Yes | 16–99 | |||
| 2007–2016 | Registry | National New Zealand |
Ambispective Population-based |
929 | 22 | No | Yes | 16–99 | |||
| WPR B | South Korea | Choi et al. | 2007 | Registry | National South Korea |
Retrospective Population-based |
1156 | 25.07 | No | No | 0–99 |
| 2008 | Registry | National South Korea |
Retrospective Population-based |
905 | 25.33 | No | No | 0–99 | |||
| 2009 | Registry | National South Korea |
Retrospective Population-based |
967 | 25.6 | No | No | 0–99 | |||
| 2010 | Registry | National South Korea |
Retrospective Population-based |
1101 | 25.86 | No | No | 0–99 | |||
| 2011 | Registry | National South Korea |
Retrospective Population-based |
1061 | 26.13 | No | No | 0–99 | |||
| 2012 | Registry | National South Korea |
Retrospective Population-based |
1004 | 26.4 | No | No | 0–99 | |||
| 2013 | Registry | National South Korea |
Retrospective Population-based |
1104 | 26.68 | No | No | 0–99 | |||
| 2014 | Registry | National South Korea |
Retrospective Population-based |
1231 | 26.95 | No | No | 0–99 | |||
| 2015 | Registry | National South Korea |
Retrospective Population-based |
1164 | 27.23 | No | No | 0–99 | |||
| 2016 | Registry | National South Korea |
Retrospective Population-based |
1285 | 27.52 | No | No | 0–99 | |||
| 2017 | Registry | National South Korea |
Retrospective Population-based |
1159 | 27.8 | No | No | 0–99 | |||
| 2007–2017 | Registry | National South Korea |
Retrospective Population-based |
12,137 | 26.4 | No | No | 0–99 | |||
| N/A | Taiwan | Wu et al. | 1998–2008 | Registry | National Taiwan |
Prospective Population-based |
25,439 | 150.48 | No | No | 20–99 |
∗ ISCoS: International Spinal Cord Society.
10. American region (AMR)
In our previous systematic review4 we could find 36 reports on TSCI from the United States (US), Canada, and Brazil in this region. In the current review, five studies were available including three studies from US33, 37, 72 and two from Canada.31, 32 Three studies of US were all registry-based and sourced information from different data repositories such as Nationwide Emergency Department Sample database,33 Nationwide Inpatient Sample database,72 and Spinal Cord Injury Surveillance Registry.37 The Canadian studies were subnational studies from a single hospitals in Quebec31 and the British Colombia Trauma Registry.32
In a study by Selvarajah et al33 using the NEDS database, the incidence of TSCI for adults aged 18 and more was 56.4 cases per million (cpm) in 2007–2009. Patients were managed in a designated trauma center in 70% of the time during the study period. The study published by Jain et al72 reported SCI incidence based on NIS data for 20 years from 1993 to 2012 with a range of 45–64 cpm in the US. They described a substantial decline in TSCI incidence among males between 16 and 24 years (from 144 to 88 cpm) and 25–44 years (from 91 to 71 cpm) between 1993 and 2012 (Table 2).
Selassie et al37 designed a population-based study using statewide TSCI surveillance and follow-up registry in South Carolina between 1998 and 2012. The age-standardized incidence rate of TSCI increased significantly from 66.9 in 1998 to 111.7 cpm in 2012. The overall incidence rate was 84.9 cpm.
TSCI individuals treated in a single center in Quebec, Canada, during an 11-year period from 2000 to 2010 were included in a study by Thompson's et al31 The incidence of TSCI was 10.6 in 2000, 22.6 in 2005, and 17.8 cpm in 2010. The incidence of TSCI between 1995 and 2004 in British Colombia province of Canada is reported in a prospective population-based study, by utilizing data from the main SCI referral center of British Colombia and British Colombia trauma registry.32 The incidence of TSCI in this study ranged between 43.4 cpm in 1996 to 28.7 cpm in 2003 (Table 2).
11. African region (AFR)
In our previous systematic review4 we could find only three papers with TSCI incidence data from Sierra Leone, South Africa and Zimbabwe. In the current review, we identified five reports from Botswana,35 South Africa28, 29, 36 and Tanzania.30 All these reports were subnational studies.
Statistics from a single referral center in Gaborone, the capital city of Botswana showed that TSCI occurs with an estimated annual incidence of 13 cpm.35 Results of the first prospective multicenter study in Cape Town, South Africa showed an incidence of 75.6 cpm TSCI for one year from 2013 to 2014. This study included survivors of acute TSCI who were 18 years or older in all government-funded hospitals within Cape Town.36 Another study in same area with the same inclusion criteria but in the private sector showed a significantly lower rate in TSCI incidence compared to the government sector (20 vs 75.6 cpm).28 Considering both sectors, the incidence of TSCI in Cape Town from 2013 to 2014 would be 61.1 cpm (95% CI 52.4–71.4). The only available study in Tanzania was a retrospective hospital-based study in northeast Tanzania region.30 The authors reviewed case record of patients and estimated the annual incidence rate of 26 cpm (Table 2).
12. Eastern Mediterranean region (EMR)
In our previous systematic review (4) we found six papers in this region form Iran, Jordan, Kuwait, Qatar, Saudi Arabia, and Pakistan. The current study could identify two studies in this region as of 2013.38,39 The first study38 collected information from most (61/68) hospitals treating TSCI in Tehran, capital of Iran and the second source39 collected information from three SCI rehabilitation centers in Khyber Pukhtunkhwa, Pakistan. The incidence rates were similar in two countries (10.5 cpm in Iran and 10.23 cpm in Pakistan) (Table 2).
13. European region (EUR)
European region includes 51 countries within three sub-region EUR A, EUR B and EUR C. In our previous systematic review4 we could find data for 22 countries in this region. The current review identified 29 reports2, 9, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 67, 68, 69, 70, 73, 74, 75 from 19 countries. Five countries were found for the first time in this review including: Former Yugoslav Republic of Macedonia,67 Czech Republic,41 Latvia,74 Lithuania68 and Poland.75 This means that data regarding TSCI incidence is now available for more than half of European countries. We could not find up-to-date reports for Turkey, Romania, Bulgaria, Portugal, Israel and Greece in this review. Most European report are population studies from trauma registries and are being updated periodically. This has brought a wealth of knowledge in this region regarding TSCI epidemiology and has helped planning preventive measures. Such knowledge has led to a decreasing/stable pattern of SCI in most countries of the region (Table 2).
14. Western pacific region (WPR)
In our previous systematic review4 we found 23 reports from seven countries in the region including Australia, New Zealand, Japan, Fiji islands, Malaysia and Vietnam. In this review, we found 17 reports from Australia,18, 19, 20, 21, 22, 23, 24, 25, 26, 60, 61, 62 Japan,64 New Zealand17 and South Korea.65 All of the reports from Australia and New Zealand were national registry-based studies. Annual reports of Australian Spinal Cord Registry (ASCIR) are available from 1986 to 2017. These reports compose most of available data in this region. The New Zealand SCI registry (NZSCIR) is a new SCI registry in this region established in 2016 in partnership with Praxis Spinal Cord Institute (formerly known as Rick Hansen Institute).76 The registry contains data for both traumatic and non-traumatic SCI and has published two annual reports so far.77, 78 The South Korean study was a retrospective population-based cohort study that sourced data from Korea's national health insurance system, which covers 98% of Korean population.65 The registry could identify 12,137 cases in an 11-year period from 2007 to 2017. The average age-standardized incidence rate was 26.4 cpm (Table 2).
15. South East Asia Region (SEAR) and Taiwan
In our previous systematic review4 we found only one report for SEAR region (Thailand) and three reports for Taiwan. In the current review, we found only one report for Taiwan sourced from National Health Insurance Research Database of Taiwan, covering over 99% of the Taiwanese population.66 The incidence rate was 150.48 cpm for the period between 1998 and 2008. This is the highest reported rate from a national study to date (Table 2).
16. Discussion
TSCI is a life-changing condition that imposes a heavy economic burden on individuals, their families, and the society. Existing literature has shown that TSCI epidemiology and etiology varies between countries based on socio-economic development index; given that, transport-related injuries are generally the leading cause of SCI in developing countries whereas in developed countries falls are the main etiology.14,79, 80 Therefore, understanding epidemiology of TSCI at country-level is imperative for planning cost-effective practical preventive plans.
In our previous systematic review4 we found 101 reports regarding TSCI incidence from 41 countries in the world by utilizing an extensive search strategy including both published and unpublished literature. In this systematic review, we repeated our search strategy up to May 5th 2020 and found 58 reports for 31 countries. This number of articles in an 8-year period (2013–2020) is more than 57% (58/101) of all papers we found previously for 78 years from 1935 to 2013. This high number of published papers implies on a trend in increasing number of papers published globally. While single center, individual series are being published from developing and low/middle-income countries around the world, European countries continue to update their knowledge periodically. This pattern of publication in part reflects the importance of infrastructure in such countries. Developed countries have established registry systems, which enables them to accurately monitor and report epidemiological data on SCI. With the advances in information technology in recent years and transformation of paper medical documents into electronic health records, now it is easier to detect and follow-up patients.
The result of our recent search lead to finding TSCI incidence data for eight new countries including Botswana, Czech Republic, Former Yugoslav Republic of Macedonia, Latvia, Lithuania, Poland, South Korea and Tanzania, which overall shapes our knowledge of TSCI for 49 countries of the world. This means that there is still a huge gap to fill if we want to draw a global map for TSCI incidence. Recently InSCI initiative3 has been announced to provide comprehensive and comparable information about the lived experience of disability throughout an international community survey in 28 countries from all six WHO regions. Reports of 19 countries have been published to date and are available to public. We obtained information for Poland and Lithuania from these valuable reports.68, 75
The introduction of International Spinal Cord Society (ISCoS) dataset5,6 has provided a well-instructed data platform especially for developing countries to base their knowledge of TSCI in an evidence-based manner. Seventeen countries including all African countries in our review used ISCoS format to report TSCI. This finding is promising as it provides an international dataset for deeper analysis of TSCI in future.
Despite recent efforts to provide information regarding epidemiology of TSCI, there are some challenges to comparability of TSCI incidence rates. For example, the definition and method of case identification in TSCI was not clear in most of our retrieved reports. In addition, the International Codes of Disease (ICD-codes) used for identification of TSCI among studies were not similar. The method of case definition of studies is depicted in Table 3. On one hand, some studies exclude cauda equina cases, and on the other hand, some studies include The ASIA (American Spinal Injury Association) Impairment Scale (AIS) grade E patients as spinal cord injured patients. Use of various definitions for TSCI may lead to heterogeneity in reports. Use of sensitivity analyses based on reasonable classification criteria can aid in offering a uniform set of case identification and ascertainment criteria for TSCI.
Table 3.
TSCI case identification/ascertainment method of studies.
| Reference | TSCI definition/ascertainment method |
|---|---|
| Moorin et al. | ICD-10 codes S14.0; S14.1–S14.13; S14.70–S14.78 S24.0; S24.10–S24.12; S24.70–S24.77 S34.0; S34.70–S34.76 |
| Reports of ASCIR, Beck et al and New et al. | ICD-10 Australian modification (ICD-10-AM) S14.0, S14.10–S14.13, S14.70–S14.78 S24.0, S24.10–S24.12, S24.70–S24.77 S34.0, S34.1, S34.70–S34.76 T06.0, T06.1 and T09.03. |
| Majden et al. | ICD-10 codes For fatal cases: S14.0–14.2, S24.0–24.2, S34.0–34.2, S12.0–12.2, S12.7, S22.0, S22.1, S32.0, S32.1, S32.7 and T91.3. For hospital admissions: S14.0, S14.1, S24.0, S24.1, S34.0 and S34.1 |
| Sabre et al. | ICD-10 codes: G82 S12.0, S12.1, S12.2 S12.7 S13.0, S13.2, S13.4, S14.0, S14.1 S22.0, S23.0, S23.1, S24.0, S24.1 S32.0, S33.0, S33.1 S34.0, S34.1, S34.3 T06.0, T06.1,T09.3, T91.1, T91.3 |
| Niemi-Nikkola et al. | ICD-10 codes: S14.0, S14.1 S24.0,S24.1 S34.0,S34.1 T09.3, T91.3 Nordic Classification of Surgical Procedures codes: NAJ00, NAJ10, NAJ12, NAJ20, NAJ22, NAJ30, NAJ32, NAJ99 |
| Mirzaeva et al and Lobzin et al. | ICD-10 codes S14.0, S14.1 S24.0, S24.1 S34.0, S34.1, S34.3 |
| Choi et al. | ICD-10 code S14.0, S14.1 S24.0, S24.1 S34.0, S34.1 |
| Chamberlain et al. | ICD-10 codes S14.0, S14.1 S24.0, S24.1 S34.0, S34.1, S34.3 T.060, T.061, T.093, and T91.3. |
| Kristinsdóttir et al and Thompson et al. | ICD-10 codes S14.X, S24.X, and S34.X ICD-9 codes 806.X and 952.X |
| Wu et al, Selvarajah et al, Jain et al, Lenehan et al, Selassie et al, Nijendijk et al. | ICD-9 codes 806.X and 952.X |
| Chamberlain et al | Did not mention ICD codes. Traumatic SCI was defined as the event of an acute traumatic lesion of neural elements in the spinal canal (spinal cord and cauda equina) that resulted in temporary or permanent sensory and/or motor deficit. |
| Halvorsen et al. | Did not mention ICD codes. Traumatic SCI was defined as impairment of the spinal cord or cauda equina function resulting from the application of an external force of any magnitude. |
| Ferro et al. | Did not mention ICD codes. A traumatic case was defined as a new hospital admission caused by an acquired traumatic lesion of the spinal cord or cauda equina, resulting in a complete or partial, transient or permanent loss of motor, sensory, bladder or bowel function below the level of the lesion, occurring in the study period |
| NOE et al. | Did not mention ICD codes. A traumatic case was defined as an acute, traumatic lesion of the spinal cord with varying degrees of motor and/or sensory deficit or paralysis. Injury of the cauda equina was included in the definition, but isolated injury of other nerve roots was excluded. |
| Mitchell et al. | Did not mention ICD codes. The NZSCIR defines SCI as impairment of the spinal cord or cauda equina function resulting in either a motor or sensory deficit or both. |
| Kriz et al. | Did not mention ICD codes. A traumatic case was defined as a SCI caused by external force at different levels with a persistent neurological deficit. Cauda equina injury was also included in the data set but not isolated injury of nerve roots. |
| Joseph et al. | Did not mention ICD codes. TSCI case was defined as: 1. abnormal imaging, such as with magnetic resonance imaging scan or multi-slice computerized tomography scan, confirming an acute TSCI or cauda equina lesion; 2. the injury must result in persisting impairment (i.e. not just a concussion) after emergence from neurogenic shock, which generally occurs within the first 24–72 h after injury |
| Philips et al. | Did not mention ICD codes. The presence or absence of a TSCI or quada equina syndrome was assessed by magnetic resonance imaging (MRI). |
| Montoto-Marqués et al. | Did not mention ICD codes. The presence or absence of a traumatic spinal injury was assessed by means of the conduct of a computerized tomography (CT) scan and magnetic resonance imaging (MRI) and was classified as follows: absence of an injury, fracture, dislocation, fracture-dislocation and others. |
| Sebastia-Alcacer et al. | Did not mention ICD codes. The presence or absence of a TSCI was assessed by magnetic resonance imaging (MRI). Patients with cauda equina were excluded. |
| Kudo et al. | Did not mention ICD codes. TSCI was defined as “an acute traumatic lesion of the neural elements in the spinal canal, resulting in temporary or permanent sensory deficit, motor deficit, or bowel/bladder dysfunction” The presence or absence of a TSCI was assessed by magnetic resonance imaging (MRI). |
| Bárbara-Bataller et al, Bilal et al, Jakimovska et al, Joseph et al, Katoh et al Koskinen et al, Löfvenmark et al, McCaughey et al, Moshi et al, Nulle et al, Sharif-Alhoseini et al, Smith et al, Pefile et al | Did not mention ICD codes or definition of TSCI. |
There are also challenges to depict the true incidence of TSCI. Rehabilitation-based studies are prone to coverage bias based on the non-participation rate of patients in rehabilitation programs. This is shown in Swiss Spinal Cord Injury (SwiSCI) cohort study by comparing electronically collected administrative hospital-discharge data to SwiSCI data, which is sourced from rehabilitation centers.58 The difference in incidence of SCI was remarkable (19.9 cpm from SwiSCI study vs 54.3 cpm from hospital-discharge data). Moreover, New et al in Australia also showed the same issue.60 They estimated TSCI incidence using two different population-based hospital discharge data in Australia. They reported a lower 21 cpm and an upper 32.3 cpm incidence rate of TSCI in 2011. The lower estimate came from adult patients admitted to rehabilitation units in Australia during 2006 and pediatric patients admitted to the only pediatric trauma hospital in Victoria between 2000 and 2010, while the upper limit was based on a population-based dataset of all patients discharged from Australian hospitals between July 1st, 1999 and June 30th, 2011. The authors believe that the numbers reported in ASCIR are underestimated. Even the lower estimate was near 30% higher than the Australian Spinal Cord Injury Registry report for 2011.23, 60
Another issue in underestimation of the true incidence of SCI is inclusion of patients who die at the scene of injury or during acute hospitalization. Sabre et al have demonstrated the impact of including prehospital mortality on the true incidence rate of TSCI.9 They recruited medical and autopsy reports of all hospitals in Estonia during 2005–2007 along with the data from Estonian Forensic Science Institute. The impact was striking; TSCI incidence including prehospital mortality was more than two times when they exclude the prehospital fatalities (97.0 cpm compared to 43.8 cpm). Similar studies with notable but less significant differences have been conducted in the US (Mississippi, Minnesota, and Utah),81, 82, 83 Canada (Alberta),34 Portugal,84 and Austria.40 Overall, only sixstudies have included prehospital deaths in their reports of TSCI.9,34, 40, 81, 82, 83
The incidence of TSCI in our previous review ranged from 3.6 to 195.4 cpm from two subnational studies from Canada and Ireland, respectively.4 If we consider only national studies after 2000, the incidence of TSCI would range between 8.3 cpm in Denmark42 to 150.5 cpm in Taiwan.66
17. Conclusion
This study showed that there is major heterogeneity in the identification and report of spinal cord injury among studies. We suggest that future studies clearly report the inclusion or exclusion of patients with cauda equina, AIS E, and prehospital deaths when reporting TSCI incidence. Furthermore, the exact set of ICD codes should be reported accordingly. We found that the mostly shared ICD codes among studies are S14.0, S14.1, S24.0, S24.1, S34.0, and S34.1 for ICD-10 and 806.X and 952.X for ICD-9 codes. Future studies can use this series of ICD codes in order to minimize the heterogeneity in the definition of TSCI. We also suggest using the ISCoS data platform when recording data for patients with TSCI.
Developing countries lack a central organization in registry or report of TSCI and may consider working along with internationally known institutions in designing registries, data reporting templates, and form regional collaborations to overcome the difficulties in data standardization and reporting in TSCI literature. The absence of a standard form of reporting TSCI hinders the comparability of data across different data sources. It is necessary to understand that the incidence rates reported as numbers are not easily comparable due to differences in TSCI definition, identification methods, and different study scales.
Funding
This study was funded by Sina Trauma and Surgery Research Center, Tehran University of Medical Science (TUMS) [Grant No. 96-01-38-34853].
Credit Author Statement
Seyed Behnam Jazayeri: Conceptualization, Methodology, Writing - original draft. Seyed Farzad Maroufi: Formal analysis, Investigation, Validation. Esmaeil Mohammadi: Methodology, Writing - original draft. Mohammad Amin Dabbagh Ohadi: Investigation, Visualisation. Ellen-Merete Hagen: Writing - Review & Editing. Maryam Chalangari: Investigation, Visualisation. Seyed Behzad Jazayeri: Conceptualization, Writing - Review & Editing. Mahdi Safdarian: Investigation, Validation. Shayan Abdollah Zadegan: Investigation, Validation. Zahra Ghodsi: Project administration. Vafa Rahimi-Movaghar: Conceptualization, Supervision
Declaration of competing interest
None.
Acknowledgments
We would like to thank Dr. Liudmila Mirzaeva, who kindly translated a Russian paper for us and Tracey Croot, the contact person of NZSCIR who provided us two annual reports of New Zealand SCI Registry and raw data of a paper that was not accessible to us.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.wnsx.2023.100171.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.Lee B., Cripps R.A., Fitzharris M., Wing P. The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord. 2014;52(2):110–116. doi: 10.1038/sc.2012.158. [DOI] [PubMed] [Google Scholar]
- 2.Sabre L., Hagen E.M., Rekand T., Asser T., Korv J. Traumatic spinal cord injury in two E uropean countries: why the differences? Eur J Neurol. 2013;20(2):293–299. doi: 10.1111/j.1468-1331.2012.03845.x. [DOI] [PubMed] [Google Scholar]
- 3.Gross-Hemmi M.H., Post M.W., Ehrmann C., et al. Study protocol of the international spinal cord injury (InSCI) community survey. Am J Phys Med Rehab. 2017;96(2):S23–S34. doi: 10.1097/PHM.0000000000000647. [DOI] [PubMed] [Google Scholar]
- 4.Jazayeri S.B., Beygi S., Shokraneh F., Hagen E.M., Rahimi-Movaghar V. Incidence of traumatic spinal cord injury worldwide: a systematic review. Eur Spine J. 2015;24(5):905–918. doi: 10.1007/s00586-014-3424-6. [DOI] [PubMed] [Google Scholar]
- 5.Biering-Sørensen F., DeVivo M., Charlifue S., et al. International spinal cord injury core data set (version 2.0)—including standardization of reporting. Spinal Cord. 2017;55(8):759–764. doi: 10.1038/sc.2017.59. [DOI] [PubMed] [Google Scholar]
- 6.Devivo M., Biering-Sørensen F., Charlifue S., et al. International spinal cord injury core data set. Spinal Cord. 2006;44(9):535–540. doi: 10.1038/sj.sc.3101958. [DOI] [PubMed] [Google Scholar]
- 7.Munn Z., Moola S., Lisy K., Riitano D., Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Base Healthc. 2015;13(3):147–153. doi: 10.1097/XEB.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 8.Thurman D.J., Sniezek J.E., Johnson D., Greenspane A., Smith S.M. Departament of Health and Human Services; 1995. Guidelines for Surveillance of Central Nervous System Injury. [Google Scholar]
- 9.Sabre L., Remmer S., Adams A., et al. Impact of fatal cases on the epidemiology of traumatic spinal cord injury in Estonia. Eur J Neurol. 2015;22(5):768–772. doi: 10.1111/ene.12478. [DOI] [PubMed] [Google Scholar]
- 10.Chiu W.-T., Lin H.-C., Lam C., Chu S.-F., Chiang Y.-H., Tsai S.-H. Epidemiology of traumatic spinal cord injury: comparisons between developed and developing countries. Asia Pac J Publ Health. 2010;22(1):9–18. doi: 10.1177/1010539509355470. [DOI] [PubMed] [Google Scholar]
- 11.Cripps R.A., Lee B.B., Wing P., Weerts E., Mackay J., Brown D. A global map for traumatic spinal cord injury epidemiology: towards a living data repository for injury prevention. Spinal Cord. 2011;49(4):493–501. doi: 10.1038/sc.2010.146. [DOI] [PubMed] [Google Scholar]
- 12.Furlan J.C., Sakakibara B.M., Miller W.C., Krassioukov A.V. Global incidence and prevalence of traumatic spinal cord injury. Can J Neurol Sci. 2013;40(4):456–464. doi: 10.1017/s0317167100014530. [DOI] [PubMed] [Google Scholar]
- 13.Kumar R., Lim J., Mekary R.A., et al. Traumatic spinal injury: global epidemiology and worldwide volume. World neurosurgery. 2018;113:e345–e363. doi: 10.1016/j.wneu.2018.02.033. [DOI] [PubMed] [Google Scholar]
- 14.Rahimi-Movaghar V., Sayyah M.K., Akbari H., et al. Epidemiology of traumatic spinal cord injury in developing countries: a systematic review. Neuroepidemiology. 2013;41(2):65–85. doi: 10.1159/000350710. [DOI] [PubMed] [Google Scholar]
- 15.Vasiliadis A.V. Epidemiology map of traumatic spinal cord injuries: a global overview. Int J Caring Sci. 2012;5(3):335–347. [Google Scholar]
- 16.Munn Z., Moola S., Riitano D., Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Pol Manag. 2014;3(3):123. doi: 10.15171/ijhpm.2014.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mitchell J., Nunnerley J., Frampton C., Croot T., Patel A., Schouten R. Epidemiology of traumatic spinal cord injury in New Zealand (2007–2016) Epidemiology. 2020;(1509):133. [PubMed] [Google Scholar]
- 18.AIHW . INJCAT. Vol. 209. AIHW; Canberra: 2020. Tovell A 2020. Spinal cord injury, Australia, 2016–17. Injury research and statistics series no. 129. Cat. no. [Google Scholar]
- 19.AIHW Tovell A. INJCAT. Vol. 202. AIHW; Canberra: 2019. Spinal cord injury, Australia, 2015–16. Injury research and statistics series no. 122. Cat. no. [Google Scholar]
- 20.AIHW . Cat. no. INJCAT. Vol. 193. AIHW; Canberra: 2018. Tovell A 2018. Spinal cord injury, Australia, 2014–15. Injury research and statistics series no. 113. [Google Scholar]
- 21.AIHW Tovell. INJCAT. Vol. 183. AIHW; Canberra: 2018. A 2018. Spinal cord injury, Australia, 2013–14. Injury research and statistics series no. 107. Cat. no. [Google Scholar]
- 22.AIHW . INJCAT. Vol. 175. AIHW; Canberra: 2018. Tovell A 2018. Spinal cord injury, Australia, 2012–13. Injury research and statistics series no. 99. Cat. no. [Google Scholar]
- 23.AIHW . INJCAT. Vol. 174. AIHW; Canberra: 2018. Tovell A 2018. Spinal cord injury, Australia, 2011–12. Injury research and statistics series no. 98. Cat. no. [Google Scholar]
- 24.AIHW Tovell A, Harrison JE. Cat. no. INJCAT. Vol. 156. AIHW; Canberra: 2018. Spinal cord injury, Australia, 2010–11. Injury research and statistics series no. 80. [Google Scholar]
- 25.AIHW Tovell A, Harrison JE. Cat. no. INJCAT. Vol. 155. AIHW; Canberra: 2018. Spinal cord injury, Australia, 2009–10. Injury research and statistics series no. 79. [Google Scholar]
- 26.AIHW Tovell A, Harrison JE. Cat. no. INJCAT. Vol. 154. AIHW; Canberra: 2018. Spinal cord injury, Australia, 2008–09. Injury research and statistics series no. 78. [Google Scholar]
- 27.Lin V.W. Demos medical publishing; 2010. Spinal Cord Medicine: Principles and Practice. [Google Scholar]
- 28.Phillips J., Braaf J., Joseph C. Another piece to the epidemiological puzzle of traumatic spinal cord injury in Cape Town, South Africa: a population-based study. S Afr Med J. 2018;108(12):1051–1054. doi: 10.7196/SAMJ.2018.v108i12.13134. [DOI] [PubMed] [Google Scholar]
- 29.Pefile N., Mothabeng J.D., Naidoo S. Profile of patients with spinal cord injuries in Kwazulu-Natal, South Africa: implications for vocational rehabilitation. The journal of spinal cord medicine. 2019;42(6):709–718. doi: 10.1080/10790268.2018.1428264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moshi H., Sundelin G., Sahlen K.-G., Sörlin A. Traumatic spinal cord injury in the north-east Tanzania–describing incidence, etiology and clinical outcomes retrospectively. Glob Health Action. 2017;10(1) doi: 10.1080/16549716.2017.1355604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thompson C., Mutch J., Parent S., Mac-Thiong J.-M. The changing demographics of traumatic spinal cord injury: an 11-year study of 831 patients. The journal of spinal cord medicine. 2015;38(2):214–223. doi: 10.1179/2045772314Y.0000000233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lenehan B., Street J., Kwon B.K., et al. The epidemiology of traumatic spinal cord injury in British Columbia, Canada. Spine. 2012;37(4):321–329. doi: 10.1097/BRS.0b013e31822e5ff8. [DOI] [PubMed] [Google Scholar]
- 33.Selvarajah S., Hammond E.R., Haider A.H., et al. The burden of acute traumatic spinal cord injury among adults in the United States: an update. J Neurotrauma. 2014;31(3):228–238. doi: 10.1089/neu.2013.3098. [DOI] [PubMed] [Google Scholar]
- 34.Dryden D.M., Saunders L.D., Rowe B.H., et al. The epidemiology of traumatic spinal cord injury in Alberta, Canada. Can J Neurol Sci. 2003;30(2):113–121. doi: 10.1017/s0317167100053373. [DOI] [PubMed] [Google Scholar]
- 35.Löfvenmark I., Norrbrink C., Nilsson-Wikmar L., Hultling C., Chakandinakira S., Hasselberg M. Traumatic spinal cord injury in Botswana: characteristics, aetiology and mortality. Spinal Cord. 2015;53(2):150–154. doi: 10.1038/sc.2014.203. [DOI] [PubMed] [Google Scholar]
- 36.Joseph C., Delcarme A., Vlok I., Wahman K., Phillips J., Wikmar L.N. Incidence and aetiology of traumatic spinal cord injury in Cape Town, South Africa: a prospective, population-based study. Spinal Cord. 2015;53(9):692–696. doi: 10.1038/sc.2015.51. [DOI] [PubMed] [Google Scholar]
- 37.Selassie A., Cao Y., Saunders L.L. Epidemiology of traumatic spinal cord injury among persons older than 21 years: a population-based study in South Carolina. Top Spinal Cord Inj Rehabil. 2015;21(4):333–344. doi: 10.1310/sci2104-333. 1998–2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sharif-Alhoseini M., Rahimi-Movaghar V. Hospital-based incidence of traumatic spinal cord injury in tehran, Iran. Iran J Public Health. 2014;43(3):331. [PMC free article] [PubMed] [Google Scholar]
- 39.Hazrat Bilal M.-U.-R. The Incidence of traumatic spinal cord injury in Khyber Pukhtunkhwa, Pakistan from 2008 to 2012. Journal of Riphah College of Rehabilitation Sciences. 2016:30–34. [Google Scholar]
- 40.Majdan M., Brazinova A., Mauritz W. Epidemiology of traumatic spinal cord injuries in Austria 2002–2012. Eur Spine J. 2016;25(1):62–73. doi: 10.1007/s00586-015-3985-z. [DOI] [PubMed] [Google Scholar]
- 41.Kriz J., Kulakovska M., Davidova H., Silova M., Kobesova A. Incidence of acute spinal cord injury in the Czech Republic: a prospective epidemiological study 2006–2015. Spinal Cord. 2017;55(9):870–874. doi: 10.1038/sc.2017.20. [DOI] [PubMed] [Google Scholar]
- 42.Noe B.B., Mikkelsen E.M., Hansen R., Thygesen M., Hagen E. Incidence of traumatic spinal cord injury in Denmark, 1990–2012: a hospital-based study. Spinal Cord. 2015;53(6):436–440. doi: 10.1038/sc.2014.181. [DOI] [PubMed] [Google Scholar]
- 43.Koskinen E., Alén M., Väärälä E., Rellman J., Kallinen M., Vainionpää A. Centralized spinal cord injury care in Finland: unveiling the hidden incidence of traumatic injuries. Spinal Cord. 2014;52(10):779–784. doi: 10.1038/sc.2014.131. [DOI] [PubMed] [Google Scholar]
- 44.Niemi-Nikkola V., Saijets N., Ylipoussu H., et al. Traumatic spinal injuries in Northern Finland. Spine. 2018;43(1):E45–E51. doi: 10.1097/BRS.0000000000002214. [DOI] [PubMed] [Google Scholar]
- 45.Smith E., Fitzpatrick P., Murtagh J., Lyons F., Morris S., Synnott K. Epidemiology of traumatic spinal cord injury in Ireland. Neuroepidemiology. 2018;51(1–2):19–24. doi: 10.1159/000488146. 2010–2015. [DOI] [PubMed] [Google Scholar]
- 46.Smith É., Fitzpatrick P., Lyons F., Morris S., Synnott K. Prospective epidemiological update on traumatic spinal cord injury in Ireland. Spinal cord series and cases. 2019;5(1):1–4. doi: 10.1038/s41394-019-0152-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ferro S., Cecconi L., Bonavita J., Pagliacci M., Biggeri A., Franceschini M. Incidence of traumatic spinal cord injury in Italy during 2013–2014: a population-based study. Spinal Cord. 2017;55(12):1103–1107. doi: 10.1038/sc.2017.88. [DOI] [PubMed] [Google Scholar]
- 48.Speziali L.M.S., Maschke R., Zampolini M., Pegliacci M.C. Traumatic and non-traumatic spinal cord incidence and care paths in a region in the center of Italy. 2023 [Google Scholar]
- 49.Nijendijk J.H., Post M.W., Van Asbeck F.W. Epidemiology of traumatic spinal cord injuries in The Netherlands in 2010. Spinal Cord. 2014;52(4):258–263. doi: 10.1038/sc.2013.180. [DOI] [PubMed] [Google Scholar]
- 50.Halvorsen A., Pettersen A., Nilsen S., Halle K.K., Schaanning E.E., Rekand T. Epidemiology of traumatic spinal cord injury in Norway in 2012–2016: a registry-based cross-sectional study. Spinal Cord. 2019;57(4):331–338. doi: 10.1038/s41393-018-0225-5. [DOI] [PubMed] [Google Scholar]
- 51.McCaughey E., Purcell M., McLean A., et al. Changing demographics of spinal cord injury over a 20-year period: a longitudinal population-based study in Scotland. Spinal Cord. 2016;54(4):270–276. doi: 10.1038/sc.2015.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Montoto-Marqués A., Ferreiro-Velasco M., Salvador-De La Barrera S., Balboa-Barreiro V., Rodriguez-Sotillo A., Meijide-Failde R. Epidemiology of traumatic spinal cord injury in Galicia, Spain: trends over a 20-year period. Spinal Cord. 2017;55(6):588–594. doi: 10.1038/sc.2017.13. [DOI] [PubMed] [Google Scholar]
- 53.Bárbara-Bataller E., Méndez-Suárez J.L., Alemán-Sánchez C., Ramírez-Lorenzo T., Sosa-Henríquez M. Epidemiology of traumatic spinal cord injury in Gran Canaria. Neurocirugía (English Edition) 2017;28(1):15–21. doi: 10.1016/j.neucir.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 54.Bárbara-Bataller E., Méndez-Suárez J.L., Alemán-Sánchez C., Sánchez-Enríquez J., Sosa-Henríquez M. Change in the profile of traumatic spinal cord injury over 15 years in Spain. Scand J Trauma Resuscitation Emerg Med. 2018;26(1):27. doi: 10.1186/s13049-018-0491-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sebastia-Alcacer V., Alcanyis-Alberola M., Giner-Pascual M., Gomez-Pajares F. Are the characteristics of the patient with a spinal cord injury changing? Spinal Cord. 2014;52(1):29–33. doi: 10.1038/sc.2013.128. [DOI] [PubMed] [Google Scholar]
- 56.Joseph C., Andersson N., Bjelak S., Giesecke K., Hultling C. 2017. Incidence, Aetiology and Injury Characteristics of Traumatic Spinal Cord Injury in Stockholm, Sweden: A Prospective, Population-Based Update. [DOI] [PubMed] [Google Scholar]
- 57.Chamberlain J.D., Deriaz O., Hund-Georgiadis M., et al. Epidemiology and contemporary risk profile of traumatic spinal cord injury in Switzerland. Injury epidemiology. 2015;2(1):28. doi: 10.1186/s40621-015-0061-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chamberlain J.D., Ronca E., Brinkhof M.W. Estimating the incidence of traumatic spinal cord injuries in Switzerland: using administrative data to identify potential coverage error in a cohort study. Swiss Med Wkly. 2017;147(1112) doi: 10.4414/smw.2017.14430. [DOI] [PubMed] [Google Scholar]
- 59.Sabre L., Pedai G., Rekand T., Asser T., Ü Linnamägi, Kõrv J. High incidence of traumatic spinal cord injury in Estonia. Spinal Cord. 2012;50(10):755–759. doi: 10.1038/sc.2012.54. [DOI] [PubMed] [Google Scholar]
- 60.New P.W., Baxter D., Farry A., Noonan V.K. Estimating the incidence and prevalence of traumatic spinal cord injury in Australia. Arch Phys Med Rehabil. 2015;96(1):76–83. doi: 10.1016/j.apmr.2014.08.013. [DOI] [PubMed] [Google Scholar]
- 61.Moorin R., Miller T.R., Hendrie D. Population-based incidence and 5-year survival for hospital-admitted traumatic brain and spinal cord injury, Western Australia. J Neurol. 2014;261(9):1726–1734. doi: 10.1007/s00415-014-7411-y. 2003–2008. [DOI] [PubMed] [Google Scholar]
- 62.Beck B., Cameron P.A., Braaf S., et al. Traumatic spinal cord injury in Victoria. Med J Aust. 2019;210(8):360–366. doi: 10.5694/mja2.50143. 2007–2016. [DOI] [PubMed] [Google Scholar]
- 63.Katoh S., Enishi T., Sato N., Sairyo K. High incidence of acute traumatic spinal cord injury in a rural population in Japan in 2011 and 2012: an epidemiological study. Spinal Cord. 2014;52(4):264–267. doi: 10.1038/sc.2014.13. [DOI] [PubMed] [Google Scholar]
- 64.Kudo D., Miyakoshi N., Hongo M., et al. An epidemiological study of traumatic spinal cord injuries in the fastest aging area in Japan. Spinal Cord. 2019;57(6):509–515. doi: 10.1038/s41393-019-0255-7. [DOI] [PubMed] [Google Scholar]
- 65.Choi S.H., Sung C-h, Heo D.R., Jeong S.-Y., Kang C.-N. Incidence of acute spinal cord injury and associated complications of methylprednisolone therapy: a national population-based study in South Korea. Spinal Cord. 2020;58(2):232–237. doi: 10.1038/s41393-019-0357-2. [DOI] [PubMed] [Google Scholar]
- 66.Wu J.-C., Chen Y.-C., Liu L., et al. Effects of age, gender, and socio-economic status on the incidence of spinal cord injury: an assessment using the eleven-year comprehensive nationwide database of Taiwan. J Neurotrauma. 2012;29(5):889–897. doi: 10.1089/neu.2011.1777. [DOI] [PubMed] [Google Scholar]
- 67.Jakimovska V.M., Biering-Sørensen F., Lidal I.B., Kostovski E. Epidemiological characteristics and early complications after spinal cord injury in Former Yugoslav Republic of Macedonia. Spinal Cord. 2020;58(1):86–94. doi: 10.1038/s41393-019-0342-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Juocevicius A., Jamontaite I.E., Adomaviciene A. People with spinal cord injury in Lithuania. Am J Phys Med Rehab. 2017;96(2):S86–S89. doi: 10.1097/PHM.0000000000000658. [DOI] [PubMed] [Google Scholar]
- 69.Kristinsdóttir E.A., Knútsdóttir S., Sigvaldason K., Jónsson H., Ingvarsson P.E. 2016. Mænuskaði Af Völdum Slysa Á Íslandi Á Árunum 1975-2014. [DOI] [PubMed] [Google Scholar]
- 70.Lobzin S.V., Mirzaeva L.M., Tcinzerling N.V., Dulaev A.К., Tamaev T.I., Tyulikov K.V. Acute traumatic spinal cord injury in saint petersburg. Epidemiological data: incidence rate, gender and age characteristics. HERALD of North-Western State Medical University named after II Mechnikov. 2019;11(2):27–34. [Google Scholar]
- 71.Kristinsdottir E.A., Knutsdottir S., Sigvaldason K., Jonsson H., Jr., Ingvarsson P.E. Epidemiology of spinal cord injury in Iceland from 1975 to 2014. Laeknabladid. 2016;102(11):491–496. doi: 10.17992/lbl.2016.11.106. [DOI] [PubMed] [Google Scholar]
- 72.Jain N.B., Ayers G.D., Peterson E.N., et al. Traumatic spinal cord injury in the United States, 1993-2012. JAMA. 2015;313(22):2236–2243. doi: 10.1001/jama.2015.6250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mirzaeva L., Gilhus N.E., Lobzin S., Rekand T. Incidence of adult traumatic spinal cord injury in Saint Petersburg, Russia. Spinal Cord. 2019;57(8):692–699. doi: 10.1038/s41393-019-0266-4. [DOI] [PubMed] [Google Scholar]
- 74.Nulle A., Tjurina U., Erts R., Vetra A. A profile of traumatic spinal cord injury and medical complications in Latvia. Spinal cord series and cases. 2017;3(1):1–6. doi: 10.1038/s41394-017-0002-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tederko P., Jagodzinski R., Krasuski M., Tarnacka B. People with spinal cord injury in Poland. Am J Phys Med Rehabil. 2017;96(2):S102–S105. doi: 10.1097/PHM.0000000000000639. [DOI] [PubMed] [Google Scholar]
- 76.Howard-Brown C., Civil I. New Zealand spinal cord registry: a new milestone. People ageing with spinal cord injury in New Zealand: a hidden population? The need for a spinal cord injury registry. 2016;129(1438) [PubMed] [Google Scholar]
- 77.New Zealand Spinal Cord Injury Registry . New Zealand Spinal Cord Injury Registry Annual Summary Report 2018. 2020. [Google Scholar]
- 78.Rick Hansen Institute . New Zealand Spinal Cord Injury Registry Annual Summary Report 2016/17. 2018. [Google Scholar]
- 79.Elshahidi M.H., Monir N.Y., Elzhery M.A., et al. Epidemiological characteristics of traumatic spinal cord injury (TSCI) in the middle-east and north-Africa (MENA) region: a systematic review and meta-analysis. Bulletin of emergency and trauma. Apr 2018;6(2):75–89. doi: 10.29252/beat-060201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kang Y., Ding H., Zhou H., et al. Epidemiology of worldwide spinal cord injury: a literature review. 神经修复. 2018;6(1):1–9. [Google Scholar]
- 81.Griffin M.R., Opitz J.L., Kurland L.T., Ebersold M.J., O'Fallon W. Traumatic spinal cord injury in Olmsted County, Minnesota, 1935–1981. Am J Epidemiol. 1985;121(6):884–895. doi: 10.1093/oxfordjournals.aje.a114058. [DOI] [PubMed] [Google Scholar]
- 82.Surkin J., Gilbert B.J.C., Harkey H.L., III, Sniezek J., Currier M. Spinal cord injury in Mississippi: findings and evaluation. Spine. 2000;25(6):716–721. doi: 10.1097/00007632-200003150-00011. 1992–1994. [DOI] [PubMed] [Google Scholar]
- 83.Thurman D.J., Burnett C., Jeppson L., Beaudoin D., Sniezek J.E. Surveillance of spinal cord injuries in Utah, USA. Spinal Cord. 1994;32(10):665–669. doi: 10.1038/sc.1994.107. [DOI] [PubMed] [Google Scholar]
- 84.Martins F., Freitas F., Martins L., Dartigues J.F., Barat M. Spinal cord injuries–epidemiology in Portugal's central region. Spinal Cord. 1998;36(8):574–578. doi: 10.1038/sj.sc.3100657. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.