Abstract
Background
Sleep disorders are conditions that have long-term effects on health, quality of sexual function, productivity at work, and overall quality of life. Considering that reports on menopausal sleep disorders are heterogeneous, the aim of this research was to determine the global prevalence of sleep disorders during menopause by meta-analysis.
Methods
PubMed, Google Scholar, Scopus, WoS, ScienceDirect, and Embase databases were checked with suitable keywords. All screening stages of articles were reviewed based on PRISMA and their quality was determined based on STROBE. Data analysis, examination of heterogeneity, and publication bias of factors affecting heterogeneity were performed in CMA software.
Results
The overall prevalence of sleep disorders among postmenopausal women was 51.6% (95% CI: 44.6–58.5%). The upper prevalence of sleep disorders was among postmenopausal women at 54.7% (95% CI: 47.2–62.1%). The upper prevalence of sleep disorders in the same population category was related to restless legs syndrome with a prevalence of 63.8% (95% CI: 10.6–96.3%).
Conclusion
In this meta-analysis, sleep disorders during menopause were found to be common and significant. Therefore, it is recommended that health policymakers offer pertinent interventions in relation to the health and hygiene of sleep for women in menopause.
Keywords: Sleep disorders, Menopause, Meta-analysis
Introduction
Menopause is the complete cessation of menstruation and indicates the end of reproduction [1]. Menopause is a normal state in which symptoms are often well managed, but it can be debilitating for some women and therefore can be detrimental to their health [2–4]. A decrease in estrogen production and resulting increase in follicle-stimulating hormone cause follicular atrophy which is the main cause of menopause [4]. Sleep is a complex process with the brain in an active state of anesthesia [5]. Sleep disorders are determined by tools such as self-report questionnaires, polysomnography, and actigraphy [6, 7]. Irregular sleep and daytime sleepiness are common among the general public and are among the most important examples of sleep disorders and resulting symptoms [5–7].
Reports of sleep disorders vary greatly and prevalence has been reported to be between 12 and 79% among women [7, 8]. Sleep disorders have many negative effects on health. These include increased risk of chronic diseases, decreased daily functioning, decreased mood, reduced use of healthcare, and female sexual dysfunction [9–11].
About a third of women’s lives around the world are affected by sleep and menopause, and both of these have a large effect on health [12]. Disturbance in falling asleep, disturbance in staying awake during the day and during work activities, and disturbance in the circadian rhythm are indicators that can help in diagnosis [13].
Studies that have examined the symptoms of postmenopausal women report that most of these women have obstructive sleep apnea [13]. In premenopause ages, the prevalence of such sleep disorders approximates 42%, in perimenopause ages 47%, and in postmenopause ages 60% [13–16]. Given the increasing number of postmenopausal women, as well as the importance of sleep quality in these individuals, the aim of this study was to perform a meta-analysis on sleep disorders during menopause in order to guide health professionals and experts in this field.
Methods
The initial search was conducted in February 2022 and last updated in April 2022. To find relevant articles, the Embase, ScienceDirect, Scopus, WoS, PubMed, and Google Scholar databases were checked.
The keywords examined in order to search in the reported databases included: Sleep Disturbance, Sleep Problems, Sleep Deprivation, Sleep Disorders, Sleep, Menopause, Long Sleeper Syndrome, Restless Leg Syndrome, Short Sleeper Syndrome, Sleep Wake Disorders, Obstructive Sleep Apnea.
Studies included in the review
Observational studies that reported prevalence of sleep disorders, articles written in English, and also, articles with English abstracts translated for non-English speakers.
Studies not included in the review
Studies whose full text was unavailable, case reports, interventional studies.
The method of selecting and extracting studies in the systematic review
Studies were reviewed based on the inclusion and exclusion criteria and irrelevant items were removed. Data were entered into EndNote software in order to remove duplicate articles. All review steps were performed by three reviewers independently in order to avoid mistakes in reviewing studies and extracting data. All stages of reviewing articles followed PRISMA guidelines [14].
Determining the quality of articles and statistical analysis of meta-analysis
The STROBE checklist was used to check the quality of observational studies [15]. Based on the scores reported in STROBE, those studies with scores above 16 were considered high-quality articles. The extracted information was entered into the Comprehensive Meta-Analysis software and publication bias was checked with funnel plot and heterogeneity was checked with the I2 test.
Results
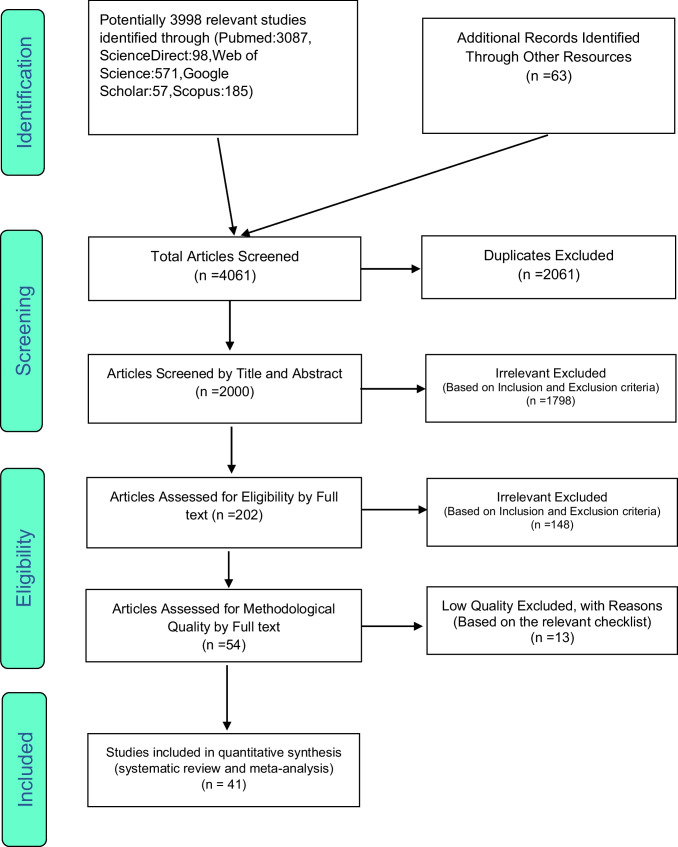
A total of 3998 articles were identified within the searched databases and 63 articles were identified through a manual search. After exclusions, 41 studies remained for the meta-analysis. The studies were identified after following the four steps of the PRISMA guidelines (Fig. 1). The information in these articles is listed in Table 1.
Fig. 1.
The process of reviewing, screening, and determining the final articles based on the PRISMA process
Table 1.
Information extracted from final studies
| Author | Year | Country | Age | Instrument | Sample size | Prevalence of sleep disorder |
|---|---|---|---|---|---|---|
| Bairy et al. [17] | 2009 | India | 48.7 | MENQOL1 |
All: 352 Postmenopause:352 |
Difficulty in sleeping in postmenopause:51.7% |
| Fallahzadeh [18] | 2007 | Iran | 47.4 | Structured questionnaire |
All: 346 Postmenopause:346 |
Difficulties sleeping in postmenopause:54.3% |
| Mondi Farsani et al. [4] | 2019 | Iran | 51.7 ± 3.5 | ISI2, PSQI3 |
All: 181 Menopause:181 |
Poor sleep quality in all: poor sleep quality in menopause: 51.4% insomnia in menopause: 48% |
| Rahman et al. [19] | 2011 | Oman |
Premenopause:45.1±4.9 Perimenopause:46.4±5.4 Postmenopause:52.8±6.4 |
MRS4 |
All: 3929 Pre: 190 Peri: 73 Post: 202 |
Sleeping problems In all: 43.20% Sleeping problems In premenopause: 33.7% Sleeping problems In perimenopause: 38.40% Sleeping problems In postmenopause: 52.20% |
| Mohamed et al. [20] | 2010 | Pakistan | 49.4 ± 7.2 | MRS |
All: 3011 Premenopause: 641 |
Sleep problems in premenopause: 80% |
| Fallahzadeh [18] | 2009 | Sri Lankan | 52.3 ± 4.7 | MRS |
All: 683 Premenopause: 144 Perimenopause: 132 Postmenopause: 405 |
Sleep problems in premenopause: 25.7% Sleep problems in perimenopause: 31.1% Sleep problems in postmenopause: 39.6% |
| Waidyasekera et al. [21] | 2010 | Kuching, Sarawak, Malaysia | 45.0±1.3 | MRS |
All: 356 Premenopause: 82 Perimenopause: 141 Postmenopause: 133 |
Sleep problems in all: 52.20% Sleep problems in premenopause: 29.20% Sleep problems in perimenopause: 66.70% Sleep problems in postmenopause: 51.1% |
| Farsani et al. [22] | 2014 | China |
Premenopause: 36.9±7.3 Postmenopause: 59.2±7.0 |
PSQI5 |
All: 1088 Premenopause: 735 Postmenopause: 353 |
Poor sleeper in premenopause: 60.8% Poor sleeper in postmenopause: 73.1% |
| Rahman et al. [23] | 2008 | Finland |
Premenopause: 47.7±2.3 Postmenopause: 63.3±3.6 |
BNSQ6 |
All: 59 Premenopause: 21 Postmenopause: 20 |
Sleep efficiency in premenopause: 84.3% Sleep efficiency in postmenopause: 80.20% |
| Dhillon et al. [24] | 2009 | Spanish | 7.1±57.9 | KI7 |
All: 10,514 Perimenopause: 3298 Postmenopause: 7216 |
Sleep problems in all: 45.7% Sleep problems in perimenopause: 37.5% Sleep problems in postmenopause: 49.40% |
| Hilditch et al. [25] | 2014 | China | 51.7±6.5 | PSQI8, KI |
All: 2046 Premenopause: 930 Perimenopause: 141 Postmenopause: 975 |
Sleep disturbance in all: 33.2% Sleep disturbance in premenopause: 24.8% Sleep disturbance in perimenopause: 34.8% Sleep disturbance in postmenopause: 40.9% |
| Kalleinen et al. [26] | 2012 | Latin America | 47.8± 5.9 | MRS |
All: 8373 Perimenopause: 916 |
Poor sleep quality in all: 46.25 Poor sleep quality in perimenopause: 43.7% Insomnia in all: 43.6% Insomnia in perimenopause: 41.7% |
| Blümel et al. [27] | 2019 | Dharwad and Bagalkote/India | 40.3 to 48.8 | The self-structured questionnaire/MRS |
All: 9512 Postmenopause: 480 |
Sleep problems in postmenopause: 51.66% |
| Pedro et al. [28] | 2006 | Malaysia | 57.1 ± 6.6 | Semi-structured questionnaire |
All: 326 Postmenopause: 326 |
Sleep disturbance in postmenopause: 45.10% |
| Resta et al. [29] | 2006 | Brazil | 7.7±5.5 | ESS9 |
All: 38 Postmenopause: 38 |
Decreased sleep efficiency in postmenopause: 68% Sleep apnea in postmenopause: 50% |
| Blümel et al. [30] | 2014 | India | 49.1 | Questionnaire |
All: 252 Postmenopause: 252 |
Sleep disturbance in postmenopause: 62.7% |
| Matsumodo et al. [31] | 2003 | Italian | 14.7±41.3 | Sleep and Healthy Questionnaire, ESS |
All: 230 Premenopause: 89 Postmenopause: 59 |
Sleep apnea in premenopause: 31.5% Sleep apnea in postmenopause: 67.80% |
| Singh and Pradhan [32] | 2006 | Finland |
Premenopause: 46.2 Postmenopause: 62.5 |
Basic Nordic Sleep Questionnaire, HI10 |
All: 393 Premenopause: 131 Postmenopause:262 |
Witnessed apnea in premenopausal: 49.6% Excessive daytime sleepiness in premenopause: 74.8% Excessive daytime sleepiness in postmenopause: 79.1% |
| Anttalainen et al. [33] | 2001 | Toronto | < 45 years and > 55 years | AHI11 |
All: 1315 Premenopause: 797 Postmenopause: 518 |
Sleep apnea in premenopause: 21% Sleep apnea in postmenopause: 47% |
| Adimi Naghan et al. [3] | 2020 | Iran | 60.4 ± 8.8 | General Health Questionnaire-ISQ12-STOPBANG13 |
All: 4021 Postmenopause: 174 |
Insomnia in postmenopausal: 13.2% |
| Hachul de Campos et al. [34] | 2020 | Egypt | 16.0±47.9 | ESS, STOP-Bang questionnaire |
All: 60 Premenopause: 27 Postmenopause: 33 |
RLS in premenopause:81% RLS in postmenopause:87.9% |
| Dancey et al. [35] | 2018 | Iran | 57.0± 9.4 | RLS Scale14 |
All: 980 Postmenopause: 980 |
RLS in postmenopause: 16.02% |
| Bagheri et al. [36] | 2021 | China | 46.9 | KMI15 |
All: 6745 Menopause: 1227 |
Insomnia in all: 44.7% Insomnia in menopause: 48% |
| Wang et al. [37] | 2005 | Korean |
Premenopause: 43.8±3.5 Perimenopause: 45.7±4.8 Postmenopause: 56.0±7.4 |
DIS16, DMS17, EMA18 |
All: 2400 Premenopause: 926 Perimenopause: 402 Postmenopause: 1072 |
Insomnia in all: 9.7% Insomnia in premenopause: 7.3% Insomnia in perimenopause: 15.9% Insomnia in postmenopause: 19.7% Early morning awakening in premenopause: 3% Early morning awakening in perimenopause: 7.2% Early morning awakening in postmenopause: 11.5% |
| Shin et al. [38] | 2008 | China | 48.9 | Self-reported menopausal symptoms |
All: 9557 Premenopause: 3286 Perimenopause: 2307 Postmenopause: 3964 |
Insomnia in all: 37.2% Insomnia in premenopause: 26.8% Insomnia in perimenopause: 42.7% Insomnia in postmenopause: 42.6% |
| Kapur et al. [39] | 2006 | China |
Premenopause: 47.8 Perimenopause: 49.7 Postmenopause: 52.7 |
GCS19 |
All: 305 Premenopause: 103 Perimenopause: 100 Postmenopause: 102 |
Insomnia in all: 12.8% Insomnia in premenopause: 2.9% Insomnia in perimenopause: 21% Insomnia in postmenopause: 14.7% Troubled sleeping due to waking up in the middle of the night or early morning in premenopause: 4.9% Troubled sleeping due to waking up in the middle of the night or early morning in perimenopause: 19% Troubled sleeping due to waking up in the middle of the night or early morning in postmenopause: 15.75% |
| Yang et al. [40] | 2006 | California |
Premenopause: 43.4± 5.3 Perimenopause: 53.0±4.8 Postmenopause: 60.5±3.4 |
Sleep-EVAL |
All: 3243 Premenopause: 562 Perimenopause: 219 Postmenopause: 201 |
Insomnia in premenopause: 36.5% Insomnia in perimenopause: 56.6% Insomnia in postmenopause: 50.7% |
| Fallahzadeh [18] | 2003 | Brazil | 45-60 | Structured pretested questionnaire |
All: 367 Premenopause: 101 Perimenopause: 68 Postmenopause: 198 |
Insomnia in all: 54.5% Insomnia in premenopause: 40.6% Insomnia in perimenopause: 55.9% Insomnia in postmenopause: 61.1% |
| Kravitz et al. [41] | 2008 | Japan | Mailed to all 50-year-old | Self-administered questionnaire, MI20 |
All: 1169 Premenopause: 702 Perimenopause: 269 Postmenopause: 269 |
Insomnia in all: 54.5% Insomnia in premenopausal: 31.8% Insomnia in perimenopause: 45% Insomnia in postmenopause: 44.6% |
| Ohayon [42] | 2017 | China |
Perimenopause: 48.6±5.5 Postmenopause: 53.0±5.4 |
KMI |
All: 1225 Perimenopause: 868 Postmenopause: 357 |
Insomnia in all: 69.39% Insomnia in perimenopause: 65.86% Insomnia in postmenopause: 77.87% |
| Ruan et al. [43] | 1995 | California | 74±9.3 | RBS21 |
All: 589 Postmenopause: 589 |
Insomnia in postmenopause: 28.1% |
| von Mühlen et al. [44] | 2008 | China |
Premenopause: 46.0 ± 2.5 Perimenopause: 48.1 ± 3.1 Postmenopause: 52.0 ± 3.7 |
Self-reported sleep problems |
All: 1113 Premenopause: 433 Perimenopause: 319 Postmenopause: 361 |
Difficulty initiating sleep in premenopause: 12.3% Difficulty initiating sleep in perimenopause: 20.1% Difficulty initiating sleep in postmenopause: 27.1% Early morning awakenings in premenopause: 2.1% Early morning awakenings in perimenopause: 4.7% Early morning awakenings sleep in postmenopause: 5.9% |
| Huang et al. [45] | 2018 | Japan |
Premenopause: 43.7± 5.1 Postmenopause: 63.8±7.6 |
ESS, Poor quality, Excessive daytime sleepiness, PSQI |
All: 7713 Premenopause: Perimenopause: Postmenopause: |
Sleep apnea in premenopause: 0 Sleep apnea in premenopause: 1.2% |
| Chang et al. [46] | 1999 | China |
Premenopause: 47.3 Perimenopause: 49.3 Postmenopause: 51.6 |
Standardized questionnaire |
All: 1900 Premenopause: 1258 Perimenopause: 92 Postmenopause: 540 |
Trouble sleeping in all: 20.79% Trouble sleeping in premenopause: 20.99% Trouble sleeping in perimenopause: 20.65% Trouble sleeping postmenopause: 20.36% |
| Kannur et al. [47] | 2003 | Caucasian, African American, Chinese, Japanese, and Hispanic | Premenopause: 30.1 | Self-reported sleep difficulty |
All: 12,603 Premenopause: 4425 |
Sleep difficulty in premenopause: 31.40% Sleep difficulty in premenopause: 31.4% |
| Sun et al. [48] | 2009 | Indian | 51.8 ± 5.8 | GCS22 |
All: 129 Premenopause: 70 |
Sleep difficulty in premenopause: 20% |
| Bairy et al. [17] | 1999 | Canada | 58.0±5.0 | MENQL23 |
All: 282 Postmenopause: 282 |
Difficulty falling asleep in postmenopause: 52% |
| Ho et al. [49] | 2002 | India |
Premenopause: 46.6 Postmenopause: 45.4 |
SDQ-924 |
All: 200 Premenopause: 100 Postmenopause: 100 |
Sleepless in premenopause: 25% Sleepless in postmenopause: 34% Waking up at night in premenpause: 23% Waking up at night in postmenpause: 34% |
| Aaron et al. [50] | 1981 | Indian | 40–55 | Symptom checklist was prepared mainly based on Neugarten and Kraines’ |
All: 405 Premenopause: 135 Perimenopause: 135 Postmenopause:135 |
Sleepless in premenopause: 54% Sleepless in perimenopause: 67% Sleepless in postmenopause: 64% |
| Sharma et al. [51] | 2003 | Brazil | 53–54 | ESS25 |
All: 1180 Premenopause: 240 Postmenopause: 471 |
Often daytime sleepiness in premenopause: 2.1% Often daytime sleepiness in postmenopause: 1.9% |
| Valiensi et al. [16] | 2019 | Argentina | 54.6±4.4 | PSQI26, ESS27, Oviedo Sleep Questionnaire, DSM-IV28 |
All: 195 Postmenopause: 195 |
Insomnia in postmenopause: 15% Sleep apnea: 10% Sleep problems in post menopause: 46.70% |
1Menopause-Specific Quality of Life
2Insomnia Severity Index
3Pittsburgh Sleep Quality Index
4Menopause Rating Scale
5Pittsburgh Sleep Quality Index
6Basic Nordic Sleep Questionnaire
7Kupperman Index
8The Pittsburgh Sleep Quality Index
9Epworth Sleepiness Scale
10Apnea Hypopnea Index
11Apnea Hypopnea Index
12Insomnia Screening Questionnaire
13Snoring, tiredness, obstruction during sleep, hypertension, body mass index (BMI), neck circumference, age, and gender
14Restless Legs Syndrome Scale
15Kupperman Menopausal Index
16Difficulty initiating sleep
17Difficulty maintaining sleep
18Early morning awakening
19(KI)
20Simplified menopause index
21Rancho Bernardo Scale
22Greene Climacteric Scale
23Menopause-Specific Quality of Life
24Strengths and Difficulties Questionnaire-9
25Epworth Sleepiness Scale
26Pittsburgh Sleep Quality Index
27Epworth Sleepiness Scale
28Diagnostic and Statistical Manual of Mental Disorders
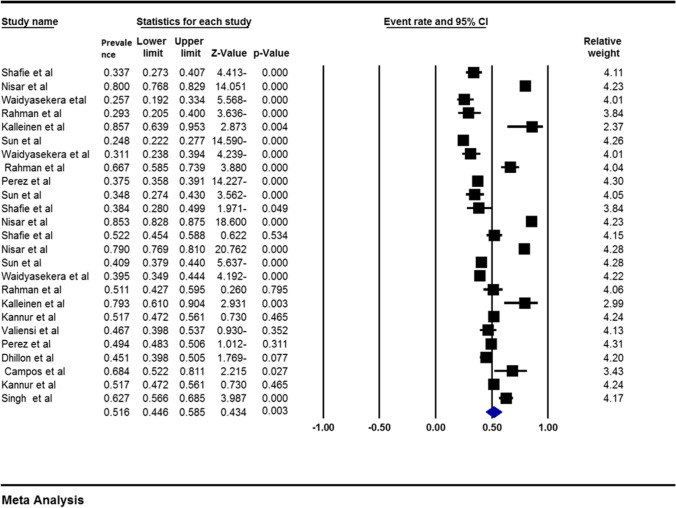
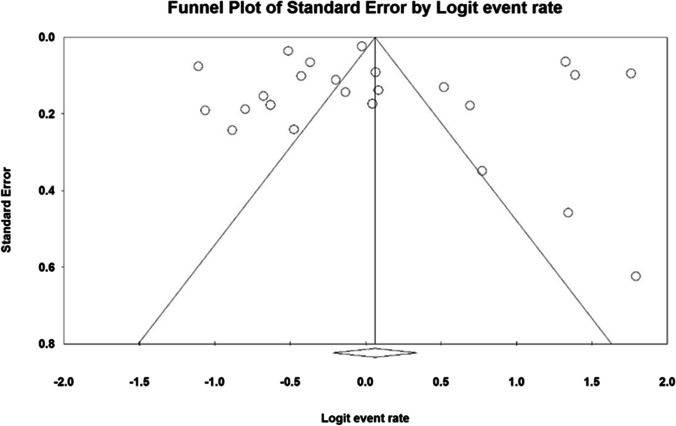
The prevalence of sleep disorders among postmenopausal women was 51.6% (95% CI: 44.6–58.5%) (Fig. 2). Heterogeneity of studies (I2: 98.4) and publication bias in studies were not significant (p: 0.596) (Fig. 3).
Fig. 2.
The overall prevalence of sleep disorders among postmenopausal women
Fig. 3.
Funnel plot to investigate the publication bias in studies
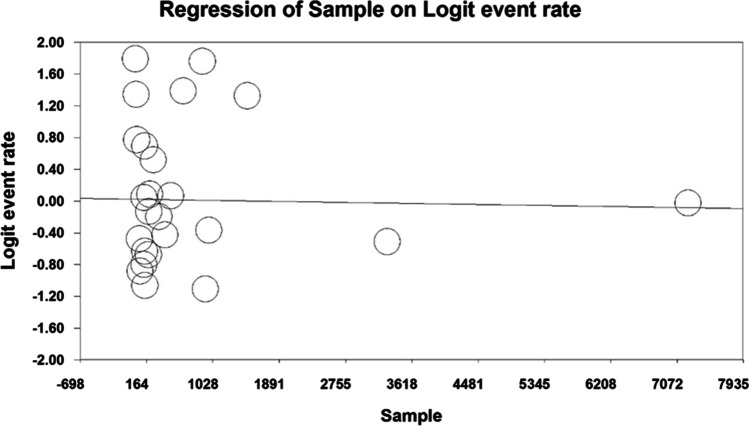
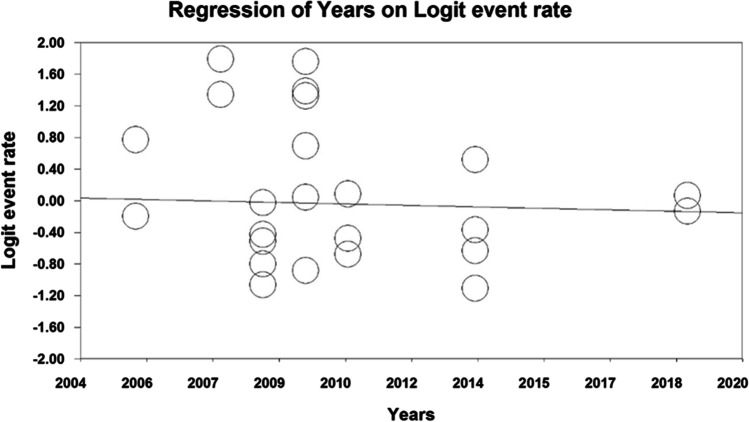
The meta-regression test showed that the larger the sample in the studies, the lower the overall prevalence of sleep disorders in postmenopausal women. (Fig. 4). Also, with the upward and increasing trend of studies until 2020 (Fig. 5), the sleep disorders among postmenopausal women have decreased (p < 0.05).
Fig. 4.
Evaluate the effect of sample size on the overall prevalence of sleep disorders among postmenopausal women
Fig. 5.
Evaluate the effect of year studies on the overall prevalence of sleep disorders among postmenopausal women
Based on the subgroup analysis results reported in Table 2, the highest sleep disorder among postmenopausal women was 54.7% (95% CI: 47.2–62.1%) (Table 2).
Table 2.
Overall prevalence of sleep disorders among postmenopausal women by menopausal stages
| Menopausal stage | Number of studies | Sample size | I2 | Prevalence |
|---|---|---|---|---|
| Premenopausal | 6 | 2008 | 98.8 | 46.5% (95%CI: 22.6–72.1%) |
| Perimenopausal | 6 | 4677 | 99.08 | 50.3% (95%CI: 27.7–72.7%) |
| Postmenopausal | 13 | 12216 | 97.6 | 54.7% (95%CI: 47.2–62.1%) |
Based on the subgroup analysis results reported in Table 3, the highest sleep disorders among postmenopausal women were related to restless legs syndrome (RLS) with 63.8% (95% CI: 10.6–96.3%) (Table 3).
Table 3.
Prevalence of various sleep disorders among postmenopausal women
| Sleep disorder type | Number of studies | Sample size | I2 | Prevalence |
|---|---|---|---|---|
| Poor sleeper | 4 | 2185 | 97.04 | 57.6% (95%CI: 44.3–69.9%) |
| Sleep apnea | 13 | 8046 | 99.02 | 30.6% (95%CI: 15.5–51.4%) |
| RLS | 3 | 1040 | 97.5 | 63.8% (95%CI: 10.6–96.3%) |
| Insomnia and DIMS | 24 | 15721 | 98.04 | 37.6% (95%CI: 31.8–43.7%) |
| Sleepiness | 9 | 1709 | 97.8 | 35.7% (95%CI: 18.2–58.1%) |
| Wake disorders | 11 | 4018 | 94.2 | 9% (95%CI: 5.5–14.3%) |
Based on Table 4, it was found that for sleep apnea, the highest prevalence was related to postmenopause with a prevalence of 35.2% (95% CI: 12.9–66.5%); for RLS, the highest prevalence was related to postmenopause with a prevalence of 53.1% (95% CI: 3.1–97.6%); for insomnia , the highest prevalence is related to perimenopause with a prevalence of 37.6% (95% CI: 28.5–47.7%); for sleepiness, the highest prevalence was in postmenopause with a prevalence of 34.2% (95% CI: 8.5–74.5%); and for wake disorders, the highest prevalence was in postmenopause with 14.2% (95% CI: 7.1–26.4%) (Table 4).
Table 4.
Prevalence of various sleep disorders in postmenopausal women by menopausal stage
| Sleep disorder type | Menopause | Number of studies | Sample size | I2 | Prevalence |
|---|---|---|---|---|---|
| Sleep apnea | Premenopausal | 5 | 3018 | 98.3 | 25.7% (95%CI: 8.9–55%) |
| Postmenopausal | 8 | 5028 | 99.2 | 35.2% (95%CI: 12.9–66.5%) | |
| RLS | Postmenopausal | 2 | 1013 | 97.7 | 53.1% (95%CI: 3.1–97.6%) |
| Insomnia and DIMS | Perimenopausal | 10 | 5481 | 97.6 | 37.6% (95%CI: 28.5–47.7%) |
| Postmenopausal | 14 | 10240 | 98.3 | 37.4% (95%CI: 29.5–46.2%) | |
| Sleepiness | Premenopausal | 4 | 606 | 97.5 | 29.5% (95%CI: 8.8–64.5%) |
| Postmenopausal | 4 | 968 | 98.6 | 34.2% (95%CI: 8.5–74.5%) | |
| Wake disorders | Premenopausal | 4 | 1562 | 95.5 | 5.4% (95%CI: 1.5–17.2%) |
| Perimenopausal | 3 | 821 | 89.8 | 8.8% (95%CI: 4–18%) | |
| Postmenopausal | 4 | 1635 | 94.3 | 14.2% (95%CI: 7.1–26.4%) |
Discussion
Based on the results of the analysis, the overall prevalence of sleep disorders in all studies was 51.6%. Shafie et al. reported the sleep disorders during postmenopause were 52.2%, in perimenopause 38.4%, and in premenopause 33.7%. These results show that the prevalence of sleep disorders during postmenopause is higher than that in the premenopause and perimenopause stages [19]. Additionally, in a study by Waidyasekera et al., sleep disorders were reported to be 39.6% in the postmenopause stage, 31.1% in perimenopause, and 25.7% among women in the premenopause period [52]. A study by Castro et al. in 2021 in Colombia and during the coronavirus outbreak reported that the sleep disorder was 65.1% in the postmenopause and 54.5% in the premenopause stage [53].
Studies have shown that 47 to 67% of postmenopausal women have OSA [54, 55]. The combination of factors such as weight gain and increase in BMI index as well as an increase in waist-to-hip ratio after menopause leads to changes in the upper airway and causes obstructive sleep apnea and sleep disorders [1, 56]. Dancey et al. reported the prevalence of apnea among women based on menopausal stages to be 47% in postmenopause, yet with a lower prevalence of 21% at the premenopause stage [33]. The study by Heinzer reported the prevalence of OSA at the postmenopause stage as 23%, and 9% at the premenopause stage, showing the higher prevalence of this disorder during postmenopause [56].
Several accelerating and persistent factors, including hormonal changes, menopausal symptoms, and mood disorders contribute to this disorder during menopause [57, 58]. Some studies reported chronic insomnia among 31 to 42% of women at the end of the perimenopause period [59]. A study conducted in China on 305 women reported that the prevalence of this disorder in perimenopause was 21%, which is more than in postmenopausal women with a prevalence of 14.7% [39]. Valiensi et al. reported that insomnia among postmenopausal women was 15% and Yang et al. reported that parasomnia was only 10% higher among the perimenopause population than postmenopause [60]. Based on a study in Brazil, insomnia in postmenopausal was 61.1%, yet this figure was reported at 55.9% among perimenopausal [18].
A study by Smith et al. showed that the incidence of insomnia at any stage of menopause could not predict the incidence of this disorder at other stages of menopause [61]. The most common sleep disorder in postmenopausal women is RLS at 63.8% [1, 62]. A study in Egypt reported the RLS, with incidences showing 87.9% among postmenopausal and 81% in premenopause [34]. In the present meta-analysis, parasomnia was most prevalent in the postmenopausal period, then in the perimenopause period, and the least prevalent in the premenopausal period. In general, the least common sleep disorder among postmenopausal was wakefulness disorder with a prevalence of 9% [16].
Conclusion
In view of the growing population of postmenopausal women, the importance of understanding the frequency and the effect of sleep disorders in this demographic group has taken on new urgency. Policymakers may use the results of the present meta-analysis to plan future healthcare, emphasizing the importance of sleep health education, treatment of sleep disorders, and improving the health of menopausal women as a research priority.
Funding
All the costs were provided by the Deputy for Research and Technology, KUMS (4010163).
Data availability
Datasets are available upon reasonable request.
Declarations
Ethical approval
All steps of this study were in accordance with the ethical standards of the KUMS Ethics Committee (IR.KUMS.REC.1401.096) and the Declaration of Helsinki.
Informed consent
This article is a review study and does not include any studies with human participants.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nader Salari, Email: n_s_514@yahoo.com.
Razie Hasheminezhad, Email: Ho.raziehasheminezhad@gmail.com.
Amin Hosseinian-Far, Email: amin.hosseinianfar@northampton.ac.uk.
Shabnam Rasoulpoor, Email: Sh.rasoulpur@gmail.com.
Marjan Assefi, Email: Massefi@aggies.ncat.edu.
Sohila Nankali, Email: drsoheilanankali98@gmail.com.
Anisodowleh Nankali, Email: Anis_nankali@yahoo.com.
Masoud Mohammadi, Email: Masoud.mohammadi1989@yahoo.com.
References
- 1.Lee J, Han Y, Cho HH, Kim M-R. Sleep disorders and menopause. J Menopausal Med. 2019;25(2):83–87. doi: 10.6118/jmm.19192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mundhra R, Dhiman N, Chaturvedi J, Chowdhuri S. Measurement of menopausal symptoms using Greene climacteric scale in a tertiary care Centre in Uttarakhand, India. J Clin Diagn Res. 2018;12(11):QC04–QC07. [Google Scholar]
- 3.Adimi Naghan P, Hassani S, Sadr M, Malekmohammad M, Khoundabi B, Setareh J, et al. Sleep disorders and mental health in menopausal women in Tehran. Tanaffos. 2020;19(1):31–37. [PMC free article] [PubMed] [Google Scholar]
- 4.Moradi Farsani H, Afshari P, Sadeghniiat Haghighi K, Gholamzadeh Jefreh M, Abedi P, Haghighizadeh MH. The effect of group cognitive behavioural therapy for insomnia in postmenopausal women. J Sleep Res. 2021;30(5):e13345. doi: 10.1111/jsr.13345. [DOI] [PubMed] [Google Scholar]
- 5.Brinkman JE, Reddy V, Sharma S. Physiology of sleep. In: StatPearls. Treasure Island (FL): StatPearls Publishing [PubMed]
- 6.Copyright © 2022, StatPearls Publishing LLC.; 2022
- 7.Liang M, Guo L, Huo J, Zhou G. Prevalence of sleep disturbances in Chinese adolescents: a systematic review and meta-analysis. PLoS One. 2021;16(3):e0247333-e. doi: 10.1371/journal.pone.0247333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang B, Duan R, Duan L. Prevalence of sleep disorder in irritable bowel syndrome: a systematic review with meta-analysis. Saudi Journal of Gastroenterology: official journal of the Saudi Gastroenterology Association. 2018;24(3):141–150. doi: 10.4103/sjg.SJG_603_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gürler M, Kızılırmak A, Baser M. The effect of aromatherapy on sleep and quality of life in menopausal women with sleeping problems: a non-randomized, placebo-controlled trial. Complement Med Res. 2020;27(6):421–430. doi: 10.1159/000507751. [DOI] [PubMed] [Google Scholar]
- 10.Caretto M, Giannini A, Simoncini T. An integrated approach to diagnosing and managing sleep disorders in menopausal women. Maturitas. 2019;128:1–3. doi: 10.1016/j.maturitas.2019.06.008. [DOI] [PubMed] [Google Scholar]
- 11.Baker FC, Lampio L, Saaresranta T, Polo-Kantola P. Sleep and sleep disorders in the menopausal transition. Sleep Med Clin. 2018;13(3):443–456. doi: 10.1016/j.jsmc.2018.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kling JM, Kapoor E, Mara K, Faubion SS. Associations of sleep and female sexual function: good sleep quality matters. Menopause. 2021;28(6):619–625. doi: 10.1097/GME.0000000000001744. [DOI] [PubMed] [Google Scholar]
- 13.Zhou Y, Yang R, Li C, Tao M. Sleep disorder, an independent risk associated with arterial stiffness in menopause. Sci Rep. 2017;7(1):1904. doi: 10.1038/s41598-017-01489-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, The PRISMA Statement: an updated guideline for reporting systematic reviews. BMJ (Clinical Research ed) 2020;2021:372. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Initiative S. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 16.Valiensi SM, Belardo MA, Pilnik S, Izbizky G, Starvaggi AP, Castelo BC. Sleep quality and related factors in postmenopausal women. Maturitas. 2019;123:73–77. doi: 10.1016/j.maturitas.2019.02.008. [DOI] [PubMed] [Google Scholar]
- 17.Bairy L, Adiga S, Bhat P, Bhat R. Prevalence of menopausal symptoms and quality of life after menopause in women from South India. Aust N Z J Obstet Gynaecol. 2009;49(1):106–109. doi: 10.1111/j.1479-828X.2009.00955.x. [DOI] [PubMed] [Google Scholar]
- 18.Fallahzadeh H. Age at natural menopause in Yazd, Islamic Republic of Iran. Menopause (New York, NY) 2007;14(5):900–904. doi: 10.1097/gme.0b013e318032b2e6. [DOI] [PubMed] [Google Scholar]
- 19.Rahman SA, Zainudin SR, Mun VL. Assessment of menopausal symptoms using modified menopause rating scale (MRS) among middle age women in Kuching, Sarawak, Malaysia. Asia Pac Fam Med. 2010;9(1):5. doi: 10.1186/1447-056X-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mohamed AO, Makhouf HA, Ali SB, Mahfouz OT. Patterns of sleep disorders in women. Egypt J Bronchol. 2019;13(5):767–773. doi: 10.4103/ejb.ejb_41_19. [DOI] [Google Scholar]
- 21.Waidyasekera H, Wijewardena K, Lindmark G, Naessen T. Menopausal symptoms and quality of life during the menopausal transition in Sri Lankan women. Menopause. 2009;16(1):164–170. doi: 10.1097/gme.0b013e31817a8abd. [DOI] [PubMed] [Google Scholar]
- 22.Farsani HM, Afshari P, Abedi P, Haghighi KS, Haghighizadeh MH. Evaluation of the frequency and factors related to sleep disorders in menopause women admitted to menopause Clinic of Imam Khomeini Hospital in Ahwaz City in 2018. J Adv Pharm Educ Res. 2019;9(S2):95. [Google Scholar]
- 23.Rahman SA, Coborn JE, Russell JA, Wiley A, Margo ND, Joffe H. Association of sleep architecture with self-reported sleep quality and sleepiness in women exposed to repeated experimental sleep fragmentation to model menopause-related sleep changes. Sleep. 2019;42:1. doi: 10.1093/sleep/zsz067.279. [DOI] [Google Scholar]
- 24.Dhillon HK, Singh HJ, Shuib R, Hamid AM, Mahmood NMZN. Prevalence of menopausal symptoms in women in Kelantan. Malaysia Maturitas. 2006;54(3):213–221. doi: 10.1016/j.maturitas.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 25.Hilditch JR, Chen S, Norton PG, Lewis J. Experience of menopausal symptoms by Chinese and Canadian women. Climacteric : the journal of the International Menopause Society. 1999;2(3):164–173. doi: 10.3109/13697139909038058. [DOI] [PubMed] [Google Scholar]
- 26.Kalleinen N, Polo O, Himanen SL, Joutsen A, Polo-Kantola P. The effect of estrogen plus progestin treatment on sleep: a randomized, placebo-controlled, double-blind trial in premenopausal and late postmenopausal women. Climacteric : the journal of the International Menopause Society. 2008;11(3):233–243. doi: 10.1080/13697130802112033. [DOI] [PubMed] [Google Scholar]
- 27.Blumel JE, Cano A, Mezones-Holguin E, Baron G, Bencosme A, Benitez Z, et al. A multinational study of sleep disorders during female mid-life. Maturitas. 2012;72(4):359–366. doi: 10.1016/j.maturitas.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 28.Pedro AO, Pinto-Neto AM, Costa-Paiva LHS, Osis MJD, Hardy EE. Climacteric syndrome: a population-based study in Brazil. Revista de saude publica. 2003;37(6):735–742. doi: 10.1590/S0034-89102003000600008. [DOI] [PubMed] [Google Scholar]
- 29.Resta O, Caratozzolo G, Pannacciulli N, Stefano A, Giliberti T, Carpagnano GE, et al. Gender, age and menopause effects on the prevalence and the characteristics of obstructive sleep apnea in obesity. Eur J Clin Investig. 2003;33(12):1084–1089. doi: 10.1111/j.1365-2362.2003.01278.x. [DOI] [PubMed] [Google Scholar]
- 30.Blümel JE, Cano A, Mezones-Holguín E, Barón G, Bencosme A, Benítez Z, et al. A multinational study of sleep disorders during female mid-life. Maturitas. 2012;72(4):359–366. doi: 10.1016/j.maturitas.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 31.Matsumoto T, Murase K, Tabara Y, Gozal D, Smith D, Minami T, et al. Impact of sleep characteristics and obesity on diabetes and hypertension across genders and menopausal status: the Nagahama study. Sleep. 2018;41(7):zsy071. doi: 10.1093/sleep/zsy071. [DOI] [PubMed] [Google Scholar]
- 32.Singh A, Pradhan SK. Menopausal symptoms of postmenopausal women in a rural community of Delhi, India: a cross-sectional study. J Mid-Life Health. 2014;5(2):62–67. doi: 10.4103/0976-7800.133989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Anttalainen U, Saaresranta T, Aittokallio J, Kalleinen N, Vahlberg T, Virtanen I, et al. Impact of menopause on the manifestation and severity of sleep-disordered breathing. Acta Obstet Gynecol Scand. 2006;85(11):1381–1388. doi: 10.1080/00016340600935649. [DOI] [PubMed] [Google Scholar]
- 34.Hachul de Campos H, Brandão LC, D’Almeida V, Grego BHC, Bittencourt LR, Tufik S, et al. Sleep disturbances, oxidative stress and cardiovascular risk parameters in postmenopausal women complaining of insomnia. Climacteric : the journal of the International Menopause Society. 2006;9(4):312–319. doi: 10.1080/13697130600871947. [DOI] [PubMed] [Google Scholar]
- 35.Dancey DR, Hanley PJ, Soong C, Lee B, Hoffstein V. Impact of menopause on the prevalence and severity of sleep apnea. Chest. 2001;120(1):151–155. doi: 10.1378/chest.120.1.151. [DOI] [PubMed] [Google Scholar]
- 36.Bagheri R, Abedi P, Mousavi P, Azimi N. The prevalence of restless legs syndrome and its relationship with demographic characteristics and medical disorders in postmenopausal Iranian women. Health Care Women Int. 2018;39(12):1317–1325. doi: 10.1080/07399332.2018.1435662. [DOI] [PubMed] [Google Scholar]
- 37.Wang XY, Wang LH, Di JL, Zhang XS, Zhao GL. Prevalence and risk factors for menopausal symptoms in middle-aged Chinese women: a community-based cross-sectional study. Menopause-J N Am Menopause Soc. 2021;28(11):1271–1278. doi: 10.1097/GME.0000000000001850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shin C, Lee S, Lee T, Shin K, Yi H, Kimm K, et al. Prevalence of insomnia and its relationship to menopausal status in middle-aged Korean women. Psychiatry Clin Neurosci. 2005;59(4):395–402. doi: 10.1111/j.1440-1819.2005.01391.x. [DOI] [PubMed] [Google Scholar]
- 39.Kapur P, Sinha B, Pereira BM. Measuring climacteric symptoms and age at natural menopause in an Indian population using the Greene climacteric scale. Menopause (New York, NY) 2009;16(2):378–384. doi: 10.1097/gme.0b013e31818a2be9. [DOI] [PubMed] [Google Scholar]
- 40.Yang DZ, Haines CJ, Pan P, Zhang QX, Sun YM, Hong SJ, et al. Menopausal symptoms in mid-life women in southern China. Climacteric : the journal of the International Menopause Society. 2008;11(4):329–336. doi: 10.1080/13697130802239075. [DOI] [PubMed] [Google Scholar]
- 41.Kravitz HM, Ganz PA, Bromberger J, Powell LH, Sutton-Tyrrell K, Meyer PM. Sleep difficulty in women at midlife: a community survey of sleep and the menopausal transition. Menopause (New York, NY) 2003;10(1):19–28. doi: 10.1097/00042192-200310010-00005. [DOI] [PubMed] [Google Scholar]
- 42.Ohayon MM. Severe hot flashes are associated with chronic insomnia. Arch Intern Med. 2006;166(12):1262–1268. doi: 10.1001/archinte.166.12.1262. [DOI] [PubMed] [Google Scholar]
- 43.Ruan XY, Cui YM, Du J, Jin FY, Mueck AO. Prevalence of climacteric symptoms comparing perimenopausal and postmenopausal Chinese women. J Psychosom Obstet Gynecol. 2017;38(3):161–169. doi: 10.1080/0167482X.2016.1244181. [DOI] [PubMed] [Google Scholar]
- 44.von Mühlen DG, Kritz-Silverstein D, Barrett-Connor E. A community-based study of menopause symptoms and estrogen replacement in older women. Maturitas. 1995;22(2):71–78. doi: 10.1016/0378-5122(95)00917-A. [DOI] [PubMed] [Google Scholar]
- 45.Hung HC, Lu FH, Ou HY, Wu JS, Yang YC, Chang CJ. Menopause is associated with self-reported poor sleep quality in women without vasomotor symptoms. Menopause (New York, NY) 2014;21(8):834–839. doi: 10.1097/GME.0000000000000183. [DOI] [PubMed] [Google Scholar]
- 46.Cheng MH, Hsu CY, Wang SJ, Lee SJ, Wang PH, Fuh JL. The relationship of self-reported sleep disturbance, mood, and menopause in a community study. Menopause (New York, NY) 2008;15(5):958–962. doi: 10.1097/gme.0b013e318160dafa. [DOI] [PubMed] [Google Scholar]
- 47.Kannur D, Itagi S. Prevalence of menopause and menopausal problems in Dharwad and Bagalkote districts, India. Int J Curr Microbiol App Sci. 2019;8(7):2618–2626. doi: 10.20546/ijcmas.2019.807.322. [DOI] [Google Scholar]
- 48.Sun DM, Shao HF, Li CB, Tao MF. Sleep disturbance and correlates in menopausal women in Shanghai. J Psychosom Res. 2014;76(3):237–241. doi: 10.1016/j.jpsychores.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 49.Ho SC, Chan SG, Yip YB, Cheng A, Yi Q, Chan C. Menopausal symptoms and symptom clustering in Chinese women. Maturitas. 1999;33(3):219–227. doi: 10.1016/S0378-5122(99)00056-0. [DOI] [PubMed] [Google Scholar]
- 50.Aaron R, Muliyil J, Abraham S. Medico-social dimensions of menopause: a cross-sectional study from rural South India. Natl Med J India. 2002;15(1):14–17. [PubMed] [Google Scholar]
- 51.Sharma VK, Saxena MS. Climacteric symptoms: a study in the Indian context. Maturitas. 1981;3(1):11–20. doi: 10.1016/0378-5122(81)90014-1. [DOI] [PubMed] [Google Scholar]
- 52.Nusrat N, Sohoo N. Severity of menopausal symptoms and the quality of life at different status of menopause: a community based survey from rural Sindh, Pakistan. Int J Collab Res Intern Med Public Health. 2010;2(5):18–130. [Google Scholar]
- 53.Jansson C, Johansson S, Lindh-Åstrand L, Hoffmann M, Hammar M. The prevalence of symptoms possibly related to the climacteric in pre- and postmenopausal women in Linköping. Sweden Maturitas. 2003;45(2):129–135. doi: 10.1016/S0378-5122(03)00127-0. [DOI] [PubMed] [Google Scholar]
- 54.Chung KF, Tang MK. Subjective sleep disturbance and its correlates in middle-aged Hong Kong Chinese women. Maturitas. 2006;53(4):396–404. doi: 10.1016/j.maturitas.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 55.Castro AM, Beltran-Barrios T, Mercado-Lara M. Assessment of the frequency of sleep complaints and menopausal symptoms in climacteric women using the Jenkins sleep scale. Sleep Sci. 2021;14(2):92–100. doi: 10.5935/1984-0063.20200041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Resta O, Bonfitto P, Sabato R, De Pergola G, Barbaro M. Prevalence of obstructive sleep apnoea in a sample of obese women: effect of menopause. Diabetes Nutr Metab. 2004;17(5):296–303. [PubMed] [Google Scholar]
- 57.Heinzer R, Marti-Soler H, Marques-Vidal P, Tobback N, Andries D, Waeber G, et al. Impact of sex and menopausal status on the prevalence, clinical presentation, and comorbidities of sleep-disordered breathing. Sleep Med. 2018;51:29–36. doi: 10.1016/j.sleep.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 58.Rösner S, Englbrecht C, Wehrle R, Hajak G, Soyka M. Eszopiclone for insomnia. Cochrane Database Syst Rev. 2018;10(10):CD010703-CD. doi: 10.1002/14651858.CD010703.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Proserpio P, Marra S, Campana C, Agostoni EC, Palagini L, Nobili L, et al. Insomnia and menopause: a narrative review on mechanisms and treatments. Climacteric : the journal of the International Menopause Society. 2020;23(6):539–549. doi: 10.1080/13697137.2020.1799973. [DOI] [PubMed] [Google Scholar]
- 60.Ishizuka B, Kudo Y, Tango T. Cross-sectional community survey of menopause symptoms among Japanese women. Maturitas. 2008;61(3):260–267. doi: 10.1016/j.maturitas.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 61.Ciano C, King TS, Wright RR, Perlis M, Sawyer AM. Longitudinal study of insomnia symptoms among women during perimenopause. Journal of Obstetric, Gynecologic, and Neonatal Nursing : JOGNN. 2017;46(6):804–813. doi: 10.1016/j.jogn.2017.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Smith RL, Flaws JA, Mahoney MM. Factors associated with poor sleep during menopause: results from the midlife Women’s health study. Sleep Med. 2018;45:98–105. doi: 10.1016/j.sleep.2018.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Datasets are available upon reasonable request.