Abstract
Background:
Extranodal NK/T-cell lymphoma, nasal type (ENKL), is an aggressive tumour with poor prognosis. Its early diagnosis may improve the prognosis of patients; however, it is often overlooked in many cases and misdiagnosed as an inflammatory sinus disease during its initial stage. Identifying the clinical characteristics of ENKL may aid otorhinolaryngologists in indicating cases early for a pathologic examination. In this study, we aimed to investigate the clinical characteristics of ENKL compared with that of diffuse large B-cell lymphoma (DLBCL), which is the most common nasal malignant lymphoma.
Methods:
The backgrounds, clinical symptoms, blood test results, and computed tomography images of patients with nasal/paranasal malignant lymphoma in our hospital between 2012 and 2017 were investigated. The characteristics of ENKL and nasal DLBCL were compared to differentiate them.
Results:
A total of 27 patients with nasal cavity and/or paranasal sinus lymphoma were included. Extranodal NK/T-cell lymphoma, nasal type, was diagnosed in 10 patients, while DLBCL was diagnosed in 17 patients. The median age of patients with ENKL was significantly lower than that of patients with DLBCL. All patients with ENKL had a unilateral lesion in the nasal cavity, with most located at the inferior turbinate. They also experienced nasal symptoms with significantly higher incidence of nasal obstruction and tendency of bleeding.
Conclusion:
ENKL was often unilateral and caused nasal obstruction, unlike DLBCL. Those who are younger in age and have sinonasal tumour with unilateral nasal obstruction and bleeding should be considered for early and repeated biopsies at multiple sites, with ENKL taken into consideration.
Keywords: Early diagnosis, lymphoma, B-cell, lymphoma, extranodal NK/T-cell, nose neoplasms, paranasal sinus neoplasms
Introduction
Malignant lymphoma involving the nasal cavity and paranasal sinuses is rare and comprises less than 1% of head and neck cancers.1,2 Diffuse large B-cell lymphoma (DLBCL) is the most common type and accounts for approximately 80% of all sinonasal lymphomas.3 However, fast-growing malignant lymphomas, such as extranodal NK/T-cell lymphoma, nasal type (ENKL), must be considered as a differential diagnosis.4,5
Extranodal NK/T-cell lymphoma, nasal type, an aggressive type of non-Hodgkin lymphoma (NHL), is derived from NK cells or γδ T-cells. It has a poor prognosis, with only a 5-year overall survival (OS) of 50% in the early clinical stages.6,7 Its incidence is high in Asia, Mexico, and Central and South America,8 constituting approximately 3% to 10% of all NHL cases in these countries.9 In contrast, its incidence is less than 1% in Western countries,10 constituting approximately 0.2% of all NHL cases in a recent European study.11 Extranodal NK/T-cell lymphoma, nasal type, has a male predilection, and patients were usually in their 40s or 50s at the time of diagnosis,9 which was slightly lower than those who have other types of lymphoma. Extranodal NK/T-cell lymphoma, nasal type, frequently occurs within the nasal cavity and pharynx: 80% of nasal/paranasal ENKLs involve the nasal cavity, followed by the maxillary sinus (6%).12 Furthermore, ENKL involving the nasal cavity was often misdiagnosed as an inflammatory sinus disease during its initial stage and detected only after progression.4,13 Moreover, histopathologic examination is required to achieve a definitive diagnosis.14 Polymorphic tumour cell and inflammatory cell infiltration against a background of necrosis and granulation tissue and infiltration of the reticular fibres of blood vessels within the blood vessel wall are typically observed in ENKL.9
As ENKL is an aggressive tumour with a poor prognosis, early diagnosis and treatment are desired; hence, an early biopsy is required. However, as its clinical symptoms and examination findings are often similar to those of inflammatory sinus disease,4 an early biopsy may often not be performed, resulting in a delay in diagnosis. It is difficult to clinically diagnose based on the symptoms during the initial stage. Moreover, a single biopsy may not lead to a definitive diagnosis, necessitating repeated biopsies in suspicious cases.13
If the characteristic signs of ENKL can be observed, otorhinolaryngologists can ensure a prompt diagnosis and facilitate early intervention. Thereby, identifying the characteristic features of ENKL may be useful in determining whether to perform a pathologic examination early. Therefore, this study aimed to identify the characteristic clinical findings of ENKL in relation to nasal and paranasal DLBCL.
Materials and Methods
Ethics approval and consent
This study was approved by the ethics committee of Jikei University School of Medicine (Approval No. 32-428[10517]). The need for informed consent was waived due to the retrospective nature of the study.
Study design and participants
The clinical records of patients histopathologically diagnosed with nasal and paranasal malignant lymphomas at the Department of Otorhinolaryngology, Jikei University School of Medicine, from January 2012 through December 2017 were retrospectively analysed. Patient inclusion was determined as follows: ‘lymphoma’ was set as the search code based on the pathologic diagnosis results, and the search codes, ‘nasal cavity / nose / sinus / paranasal sinus’, were set as sampling sites. The exclusion criteria were as follows: (a) insufficient patient and treatment information and (b) patients aged under 20 years.
Outcomes
The primary outcomes were the characteristic clinical manifestations and laboratory findings of ENKL compared with those of DLBCL. The secondary outcomes were OS in ENKL and DLBCL involving the nasal cavity and paranasal sinuses.
Procedures
The following data were obtained from the clinical records: patient age (at the time of biopsy), sex (male or female), medical history, family history, smoking status (at the first visit), chief complaints and symptoms (at the first visit), presence of systemic symptoms (symptoms during the first visit), blood test findings (lactate dehydrogenase [LDH], albumin, soluble interleukin-2 receptor [s-IL2R], white blood cell, haemoglobin, platelet, peripheral blood lymphocyte), computed tomography (CT) findings, treatment information, OS (from the date of first visit to the date of last visit or death), and progression-free survival (PFS) (from the date of first visit to the date of last visit until progression or death). The periods from the first visit until the biopsy and from the first visit until the start of treatment were also noted to examine their relationship with patient prognosis.
The diagnosis and classification of malignant lymphoma were performed according to the 2017 World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues.14 The clinical staging of malignant lymphoma was determined according to the Ann Arbor staging system.15
Determination of the tumour location
The location of the malignant lymphoma was determined using sinus CT images. These CT images were examined by 3 otorhinolaryngologists based on the following points:
(i) The distribution area in the nasal cavity (olfactory cleft, superior turbinate, middle turbinate, inferior turbinate, and nasal septum) and paranasal sinuses (maxillary sinus, ethmoid sinus, frontal sinus, and sphenoid sinus) with the largest soft tissue concentration were identified;
(ii) If the soft tissue concentration involved multiple regions and occupied 50% or more of that region, it was considered as involved; and
(iii) If there were disagreements regarding the location among the 3 otorhinolaryngologists, the location was selected by a majority vote. If all 3 were different, the opinion of the most experienced otorhinolaryngologist was chosen.
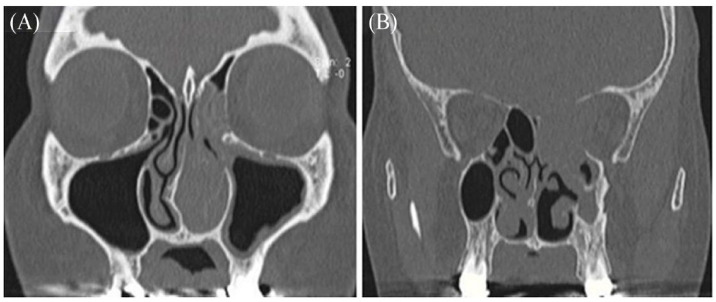
As examples, Figure 1A was a nasal cavity tumour (1 of the slices of the inferior turbinate tumour image) and Figure 1B was a paranasal sinus tumour (1 of the slices of the ethmoid sinus tumour image).
Figure 1.
Sinus computed tomography images of nasal and paranasal lymphoma. (A) Nasal cavity tumour. (B) Paranasal sinus tumour.
Statistical analysis
Continuous and categorical variables are presented as means (standard deviation) and count (%), respectively. The Mann–Whitney U test and Fisher’s exact test were used to compare the differences between ENKL and DLBCL. Differences between the Kaplan–Meier survival curves were analysed using log-rank tests. A 2-sided α value of less than .05 was considered as statistically significant. Statistical analyses were performed using GraphPad Prism version 8.4.3 (Graphpad Software Inc., San Diego, CA, USA).
Results
Patient characteristics
A total of 29 patients who were diagnosed with nasal cavity and/or paranasal sinus lymphoma during the 6-year period were reviewed. Diffuse large B-cell lymphoma was the most common malignant lymphoma involving the nasal cavity and/or paranasal sinuses and diagnosed in 17 cases (58.6%). The second most common was ENKL, which was diagnosed in 10 patients (34.5%). B-cell lymphoblastic leukaemia and high-grade B-cell lymphoma with MYC and BCL2 and/or BLC6 rearrangements were diagnosed in 1 case each (3.4%).
Characteristics of ENKL
Ten patients with ENKL were identified (Table 1). The median age at diagnosis was 46 years (range, 28-75 years), and half of the patients were in the 40 to 50 age group. The patients included 6 men and 4 women. The most common chief complaints and symptoms were unilateral nasal obstruction (8 cases) and unilateral nasal bleeding (2 cases). Nasal discharge, intranasal pain, cheek swelling, eyelid swelling, and neck swelling were observed in 1 case each. Systemic symptoms (B symptoms), which comprised fever over 38°C, night sweats, and/or unintentional weight loss, were observed in 4 cases. All ENKLs involved only one side of the nasal cavity, with most located at the inferior turbinate (60.0%), followed by the middle turbinate (30.0%), and nasal septum (10.0%). The clinical stages were IE, IIE, and IVE, in 5 (50%), 3 (30%), and 2 cases (20%), respectively, and 80% were diagnosed with early-stage disease.
Table 1.
Characteristics and outcomes of 10 patients with extranodal NK/T-cell lymphoma.
| Case | Age | Sex | Chief complaint | B symptom | Smoking status | Clinical stage | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | (Year) | Nasal obstruction | Nasal bleeding | Other symptoms | Fever | Night sweat | Weight loss | |||
| 1 | 40-49 | 2 | + | – | Cheek pain | – | – | – | Never | Ⅰ |
| 2 | 40-49 | 2 | + | – | – | + | – | – | Never | Ⅰ |
| 3 | 50-59 | 2 | + | – | – | – | – | – | Unknown | Ⅱ |
| 4 | 70-79 | 1 | + | – | – | – | – | + | Current | Ⅱ |
| 5 | 20-29 | 2 | + | + | – | – | – | – | Never | Ⅰ |
| 6 | 40-49 | 1 | + | – | – | + | + | + | Current | Ⅰ |
| 7 | 30-39 | 1 | – | – | Intranasal pain | – | – | – | Unknown | Ⅱ |
| 8 | 60-69 | 1 | + | – | – | – | – | – | Never | Ⅰ |
| 9 | 30-39 | 1 | + | + | Nasal discharge | + | – | + | Never | Ⅳ |
| 10 | 50-59 | 1 | – | – | Eyelid/neck swelling | – | – | – | Current | Ⅳ |
| Case no. | Medical history | Location | Response | Outcome | ||||||
| OS (month) | PFS (month) | |||||||||
| 1 | Hypertension | Inferior turbinate | CR | 30 | 30 | |||||
| 2 | – | Middle turbinate | PD | 17 | 17 | |||||
| 3 | – | Inferior turbinate | CR | 9 | 9 | |||||
| 4 | Hypertension, dyslipidaemia, atrial fibrillation | Inferior turbinate | CR | 10 | 10 | |||||
| 5 | – | Inferior turbinate | CR | 3 | 3 | |||||
| 6 | – | Middle turbinate | CR | 5 | 5 | |||||
| 7 | – | Inferior turbinate | CR | 58 | 58 | |||||
| 8 | Hypertension, dyslipidaemia | Nasal septum | CR | 53 | 53 | |||||
| 9 | Arrhythmia | Inferior turbinate | PR | 10 | 10 | |||||
| 10 | Hypertension | Middle turbinate | PD | 3 | 3 | |||||
Abbreviations: CR, complete response; OS, overall survival; PD, progressive disease; PFS, progression-free survival; PR, partial response.
Regarding the laboratory findings, the median LDH and s-IL2R levels were 187.5 IU/L and 370.5 U/mL, respectively. As for the tissue biopsies, the cell surface markers, CD3, CD56, granzyme B, and Epstein–Barr virus-encoded small RNA in situ hybridisation (EBER-ISH), were positive in 9 cases. Meanwhile, the markers were perforin in 5 cases and T-cell intracytoplasmic antigen in another 5 cases. Bone marrow biopsy showed bone marrow infiltration in 2 cases.
Characteristics of DLBCL
A total of 17 patients with DLBCL were identified. The median age at diagnosis was 66 years (range, 36-83 years). The patients included 12 men and 5 women. The most common chief complaints and symptoms were double vision (5 cases) and unilateral nasal obstruction (4 cases). Cheek symptoms were observed in 3 cases. Eye pain and visual field loss were observed in 2 cases each. B symptoms were found in 1 case. Most DLBCL cases involved the paranasal sinuses, with most located at the ethmoidal sinus (35.3%), followed by the maxillary (23.6%), sphenoidal (17.6%), and frontal (5.9%) sinus. The clinical stages were IE, IIE, and IVE, in 13 (76.5%), 1 (5.9%), and 3 (17.6%) cases, respectively, and 82.4% were diagnosed with early-stage disease.
Regarding the laboratory findings, the median LDH and s-IL2R levels were 186 IU/L and 480 U/mL, respectively. As for the tissue biopsies, the cell surface markers, CD20 and CD79a, were positive in all cases, CD10 in 6, BCL2 in 11, and BCL6 in 10. As for the cell of origin, 12 cases were under the germinal centre B-cell type, and 5 were under the activated B-cell type. Bone marrow biopsy showed bone marrow infiltration in 3 cases.
Comparison between ENKL and DLBCL
A total of 27 lymphoma cases were identified (Table 2). Male patients accounted for 60.0% and 70.6% of the patients with ENKL and DLBCL, respectively. Sex distribution did not vary significantly between the 2 groups. The median age at diagnosis of ENKL was significantly lower than that of DLBCL (46.00 ± 13.83 years vs 66.00 ± 13.63 years, P < 0.05). The presence of systemic symptoms was significantly higher in patients with ENKL (40.0% vs 5.9%, P < 0.05). The Ann Arbor stages at the diagnosis of ENKL and DLBCL did not reach statistical significance (IE, IIE, IIIE, and IVE, respectively). Regarding the lesion distribution within the nasal cavity and paranasal sinuses (maxillary, ethmoidal, frontal, and sphenoidal sinus), most ENKLs originated from the nasal cavity (P < 0.05), with most involving the inferior turbinate (60.0%), followed by the middle turbinate (30.0%) and nasal septum (10.0%). In contrast, two-thirds of DLBCL cases were located within the paranasal sinuses (P < 0.05), with most involving the ethmoidal sinus (35.3%), followed by the maxillary (23.6%), sphenoidal (17.6%), and frontal (5.9%) sinus. Most DLBCL cases that involve the nasal cavity originated from the middle turbinate (17.6%), followed by the inferior turbinate (5.9%).
Table 2.
Demographic/histopathologic characteristics and chief complaints of ENKL and DLBCL.
| Total (n = 27) | ENKL (n = 10) | DLBCL (n = 17) | P value | |
|---|---|---|---|---|
| Age (y, median, SD) | ||||
| 59.00 ± 16.05 | 46.00 ± 13.83 | 66.00 ± 13.63 | .003* | |
| Sex (no.) | ||||
| Male | 18 | 6 | 12 | .683 |
| Female | 9 | 4 | 5 | |
| Smoking status (no.) | ||||
| Smoking | 9 | 3 | 6 | .650 |
| Non-smoking | 10 | 5 | 5 | |
| Unknown | 8 | 2 | 6 | |
| B symptoms (no.) | ||||
| Present | 5 | 4 | 1 | .047* |
| Absent | 22 | 6 | 16 | |
| Ann Arbor stage (no.) | ||||
| IE | 18 | 5 | 13 | .219 |
| IIE | 4 | 3 | 1 | .128 |
| IIIE | 0 | 0 | 0 | |
| IVE | 5 | 2 | 3 | >.999 |
| Original sites (no.) | ||||
| Nasal cavity | 16 | 10 | 6 | .001* |
| Paranasal sinus | 12 | 0 | 12 | .0004* |
| Maxillary sinus | 4 | 0 | 4 | |
| Ethmoidal sinus | 6 | 0 | 6 | |
| Frontal sinus | 1 | 0 | 1 | |
| Sphenoidal sinus | 3 | 0 | 3 | |
| Chief complaints | ||||
| Nasal symptoms (no.) | ||||
| Nasal obstruction | 12 | 8 | 4 | .007* |
| Nasal bleeding | 2 | 2 | 0 | .128 |
| Nasal discharge | 2 | 1 | 1 | >.999 |
| Intranasal pain | 1 | 1 | 0 | .370 |
| Eye symptoms (no.) | ||||
| Double vision | 5 | 0 | 5 | .124 |
| Eye pain | 2 | 0 | 2 | .516 |
| Visual field loss | 2 | 0 | 2 | .516 |
| Eyelid swelling | 2 | 1 | 1 | >.999 |
| Blurred vision | 1 | 0 | 1 | >.999 |
| Cheek symptoms (no.) | ||||
| Cheek pain | 2 | 1 | 1 | >.999 |
| Cheek swelling | 1 | 0 | 1 | >.999 |
| Cheek discomfort | 1 | 0 | 1 | >.999 |
| Others (no.) | 3 | 1 | 2 | >.999 |
| Blood test (median, SD) | ||||
| LDH (UI/L) | 186 ± 76 | 188 ± 105 | 186 ± 56 | .421 |
| s-IL2R (U/mL) | 444 ± 1445 | 371 ± 2260 | 480 ± 287 | .856 |
Abbreviations: DLBCL, diffuse large B-cell lymphoma; ENKL, extranodal NK/T-cell lymphoma, nasal type; LDH, lactate dehydrogenase; s-IL2R, soluble interleukin-2 receptor.
Age and blood test results were analysed using the Mann–Whitney U test. The other factors were analysed using Fisher’s exact test. Statistical significance was set at P < .05.
Table 2 shows the chief complaints of the patients during their initial visit to our hospital. Patients with ENKL tended to complain of nasal symptoms, with nasal obstruction being significantly higher (P < .05). Nasal bleeding was also more frequent in ENKL, although the difference was not significant. Eye symptoms (eg, double vision) were more common in DLBCL; however, this difference was not statistically significant (P = .091).
In the blood test results, the number of peripheral blood lymphocytes was significantly higher in DLBCL than in ENKL (1.90 ± 0.79 × 103/µL vs 1.20 ± 0.59 × 103/ µL, P = .013), although the other results were not significantly different.
In addition, there was no significant difference between ENKL and DLBCL in terms of the interval from the first visit until biopsy (15.0 ± 24.39 days vs 1.00 ± 24.41 days, P = .179). In all cases, a biopsy was performed only once, with no cases requiring multiple biopsies to obtain a diagnosis.
Patient survival
Figure 2 depicts the Kaplan–Meier survival curve for ENKL and DLBCL. The median observation periods of ENKL and DLBCL were 11.5 and 27.0 months, respectively, and the OS rates were 80% and 100%, respectively. For ENKL, 3 cases had a complete response, 1 had a partial response, and 2 had progressive disease. The OS and PFS rates for ENKL were significantly lower than those for DLBCL (10.0 ± 20.5 months vs 26.0 ± 18.4 months, hazard ratio = 29.23, 95% confidence interval = 1.385-616.8, P < .05). However, no significant difference was observed regarding staging. There was also no correlation observed between the period until biopsy and OS for ENKL. All patients with ENKL were treated with chemotherapy, and 80% were treated with combined radiation therapy.
Figure 2.
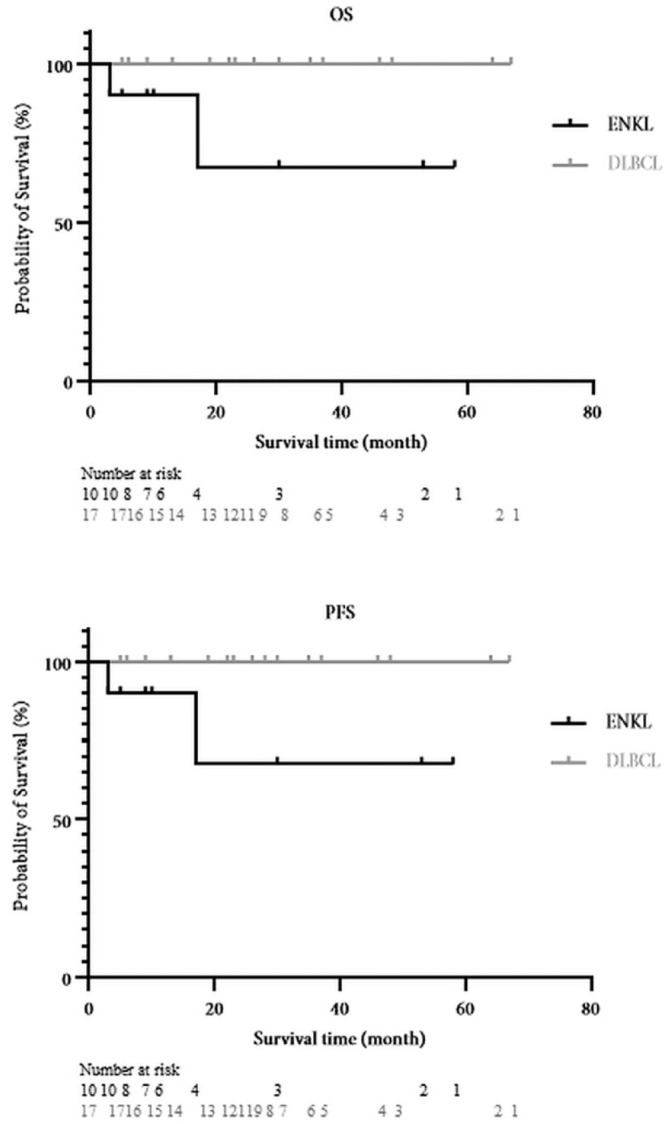
Survival curves for ENKL and DLBCL. DLBCL indicates diffuse large B-cell lymphoma; ENKL, extranodal NK/T-cell lymphoma, nasal type; OS, overall survival; PFS, progression-free survival.
Discussion
This study provided 2 important findings. First, ENKL exhibited the following characteristics in comparison with DLBCL: younger patient age, distinctive tumour location within the nasal cavity, nasal obstruction symptoms, and B symptoms. Second, the OS and PFS rates in ENKL were worse than those in DLBCL.
Characteristics of ENKL in comparison with DLBCL
The age at diagnosis of ENKL was generally 40s to 50s in Asia, suggesting that our patient population was similar to that of previous epidemiologic studies.9
Extranodal NK/T-cell lymphoma, nasal type, more commonly involves the nasal cavity than the paranasal sinuses; however, possible causes have not been reported. A unique characteristic of the development of ENKL is the infection of NK/T cells with Epstein–Barr virus,9,16 unlike other lymphomas. The heterogeneous distribution of NK/T cells within the nasal/paranasal mucosa may be associated with the apparent localisation of ENKL. As there was a report that NK cells were major immune cells in the nasal lavage fluid,17 ENKL might develop more often in the nasal cavity. Nevertheless, there are no reports comparing the NK/T-cell distribution in the nasal/paranasal mucosa or major immune cells in the paranasal lavage fluid; thus, further studies are required to investigate the cause of this localisation.
Extranodal NK/T-cell lymphoma, nasal type, often presents with nasal symptoms, particularly nasal obstruction and bleeding.18 Given the fact that ENKL is common within the nasal cavity, nasal symptoms may likely occur more than eye and/or cheek symptoms. In this study, there was no significant difference regarding nasal bleeding; however, it was more prevalent in ENKL. Therefore, ENKL must be considered in the diagnosis of nasal tumours with nasal obstruction and bleeding.
B symptoms were also significantly higher in patients with ENKL because the OS and PFS rates were significantly worse. B symptoms are characteristic systemic symptoms of lymphoma and observed in 30% to 50%9 of cases with ENKL in Asia, which is consistent with the percentage observed in our study.
Furthermore, 31% of lymphomas manifest with eye symptoms, which was observed in the DLBCL cases in our study. In another case series of sinonasal lymphomas,4,5 eye symptoms were present in approximately 20% to 40% of cases, which was less than that of nasal symptoms, such as nasal obstruction; however, these symptoms were remarkable. Two-thirds of the other lymphomas in this study were localised in the paranasal sinuses, especially in the ethmoid and maxillary sinuses, which are present around the orbit; hence, this may account for many of the eye symptoms.
Prognosis of ENKL in comparison with DLBCL
Extranodal NK/T-cell lymphoma, nasal type, has a relatively poor prognosis among malignant lymphomas. Dubal et al19 compared sinonasal ENKL and DLBCL and reported that the overall 1-, 5-, and 10-year disease-specific survival was significantly lower in ENKL, with no significant difference in Ann Arbor staging. Our results were similar to those of previous studies, in which there was no significant difference in the time to diagnosis. Therefore, ENKL is likely to have a worse prognosis than DLBCL. In our study, all cases were diagnosed after a single biopsy; however, if the diagnosis was delayed due to inappropriate or repeated biopsies, the results could have been different.
The blood test results showed a significant decrease only in the peripheral blood lymphocyte count in patients with ENKL, which might also reflect the poor OS and PFS rates. As no previous report showed a significant decrease in peripheral blood lymphocyte count in ENKL, it may be difficult to consider this decrease as a characteristic of ENKL based on our results alone as the number of ENKL cases in this study was small, and 1 patient was in extremely poor health at the time of diagnosis.
Epidemiology of lymphoma in Asia in comparison with European studies
The patients included in this study were all Asians, and their epidemiology was similar to that of previous reports in Asia and Latin America.9,10 However, some differences were observed in comparison with a recent large-scale cohort study in Europe.11 First, the median age of the patients in ENKL in Europe was 65.7 years, which was higher than that of the patients in our study and previous reports in Asia and Latin America.9,10 Extranodal NK/T-cell lymphoma, nasal type, is a rare disease in Europe, and race, Epstein–Barr virus strain mutations, and environmental factors are considered as some of the reasons for this geographical difference.9 These elements may also partly account for the delayed age of onset in Europe. Second, pain and swelling were more frequently seen than nasal bleeding and B symptoms with patients in ENKL in Europe. In an Asian report, the most common symptoms of ENKL were nasal obstruction, nasal bleeding, and B symptoms,9 suggesting that there may be some regional differences in the symptoms. In addition, patients with sinonasal DLBCL in Europe also had other different characteristics in other aspects from our results. In Europe,3 the median age was higher than in our results (72.8 years), and nasal symptoms were more frequent than eye symptoms. Thus, additional research is needed to further elucidate the epidemiologic differences between ENKL and sinonasal DLBCL.
Limitations
One limitation of our study was that lymphoma distribution was determined only through CT imaging. A more accurate evaluation of the location could be achieved if there were detailed medical records describing the distribution and transnasal endoscopic images. Another limitation was that the evaluation of the presence or absence of symptoms was based on the patient’s chief complaints. As the presence or absence of all major nasal and eye symptoms could not be confirmed retrospectively, the frequency of the symptoms could not be evaluated accurately. The retrospective and single-centre design of the study was also a limitation. Although the number of cases in this study was small and the treatment and prognostic findings were limited, our study focused on determining the characteristics of ENKL, which may facilitate its early diagnosis. In addition, because this study only included Asian patients, the results may not apply to some regions, such as Europe.
Conclusion
Extranodal NK/T-cell lymphoma, nasal type, has a worse prognosis than DLBCL; therefore, performing diagnostic methods earlier if ENKL is suspected must be considered. In particular, younger patients who have sinonasal tumour with unilateral nasal obstruction and bleeding should be considered for an early biopsy and repeated biopsies at multiple sites, with ENKL taken into consideration.
Acknowledgments
The authors thank Editage (www.editage.com) for English language editing.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author Contributions: Hirotaka Tanaka: Conceptualisation, data collection and analysis, funding acquisition, investigation, methodology and resources.
Eri Mori: Conceptualisation, investigation, methodology, writing, review, and editing of the manuscript, and total project administration and supervision.
Taisuke Akutsu: Writing, data collection, and analysis,
Shota Saito: Data collection.
Masayoshi Tei: Review and editing of the manuscript.
Nobuyoshi Otori: Supervision, review, and editing of the final manuscript.
ORCID iD: Hirotaka Tanaka  https://orcid.org/0000-0002-5322-5479
https://orcid.org/0000-0002-5322-5479
References
- 1. Doshi DV, Tripathi U, Dave RI, Pandya SJ, Shukla HK, Parikh BC. Rare tumors of sinonasal track. Indian J Otolaryngol Head Neck Surg. 2010;62:111-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Das S, Kirsch CF. Imaging of lumps and bumps in the nose: a review of sinonasal tumours. Cancer Imaging. 2005;5:167-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Eriksen PRG, Clasen-Linde E, Nully Brown P, et al. Sinonasal B-cell lymphomas: a nationwide cohort study, with an emphasis on the prognosis and the recurrence pattern of primary diffuse large B-cell lymphoma. Hematol Oncol. 2022;40:160-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Peng KA, Kita AE, Suh JD, Bhuta SM, Wang MB. Sinonasal lymphoma: case series and review of the literature. Int Forum Allergy Rhinol. 2014;4:670-674. [DOI] [PubMed] [Google Scholar]
- 5. Steele TO, Buniel MC, Mace JC, El Rassi E, Smith TL. Lymphoma of the nasal cavity and paranasal sinuses: a case series. Am J Rhinol Allergy. 2016;30:335-339. [DOI] [PubMed] [Google Scholar]
- 6. Takahara M, Kishibe K, Bandoh N, Nonaka S, Harabuchi Y. P53, N- and K-Ras, and beta-catenin gene mutations and prognostic factors in nasal NK/T-cell lymphoma from Hokkaido, Japan. Hum Pathol. 2004;35:86-95. [DOI] [PubMed] [Google Scholar]
- 7. Isobe K, Uno T, Tamaru J, et al. Extranodal natural killer/T-cell lymphoma, nasal type: the significance of radiotherapeutic parameters. Cancer. 2006;106:609-615. [DOI] [PubMed] [Google Scholar]
- 8. Wajda BN, Rabinowitz MR, Nyquist GG, Mardekian SK, Rosen MR, Rabinowitz MP. Paranasal sinus lymphoma: retrospective review with focus on clinical features, histopathology, prognosis, and relationship to systemic lymphoma. Head Neck. 2017;39:1065-1070. [DOI] [PubMed] [Google Scholar]
- 9. Harabuchi Y, Takahara M, Kishibe K, Nagato T, Kumai T. Extranodal natural killer/T-cell lymphoma, nasal type: basic science and clinical progress. Front Pediatr. 2019;7:141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sánchez-Romero C, Bologna-Molina R, Paes de, Almeida O, et al. Extranodal NK/T cell lymphoma, nasal type: an updated overview. Crit Rev Oncol Hematol. 2021;159:103237. [DOI] [PubMed] [Google Scholar]
- 11. Eriksen PRG, Clasen-Linde E, Brown PN, et al. NK- and T-cell lymphoma of the nasal cavity and paranasal sinuses in Denmark 1980-2017: a nationwide cohort study. Leuk Lymphoma. 2022;63:2579-2588. [DOI] [PubMed] [Google Scholar]
- 12. Vazquez A, Khan MN, Blake DM, Sanghvi S, Baredes S, Eloy JA. Extranodal natural killer/T-cell lymphoma: a population-based comparison of sinonasal and extranasal disease. Laryngoscope. 2014;124:888-895. [DOI] [PubMed] [Google Scholar]
- 13. Gomes PS, Caselhos S, Vide AT, Fonseca R. Extranodal natural killer/T cell lymphoma, nasal type: a diagnostic challenge. BMJ Case Rep. 2019;12:e232404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Swerdlow SH, Campo E, Harris NL, et al. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Revised 4th ed. World Health Organization; 2017. [Google Scholar]
- 15. Carbone PP, Kaplan HS, Musshoff K, Smithers DW, Tubiana M. Report of the committee on Hodgkin’s disease staging classification. Cancer Res. 1971;31:1860-1861. [PubMed] [Google Scholar]
- 16. Kimura H. EBV in T-/NK-cell tumorigenesis. Adv Exp Med Biol. 2018;1045:459-475. [DOI] [PubMed] [Google Scholar]
- 17. Horvath KM, Herbst M, Zhou H, et al. Nasal lavage natural killer cell function is suppressed in smokers after live attenuated influenza virus. Respir Res. 2011;12:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wu X, Li P, Zhao J, et al. A clinical study of 115 patients with extranodal natural killer/T-cell lymphoma, nasal type. Clin Oncol (R Coll Radiol). 2008;20:619-625. [DOI] [PubMed] [Google Scholar]
- 19. Dubal PM, Dutta R, Vazquez A, Patel TD, Baredes S, Eloy JA. A comparative population-based analysis of sinonasal diffuse large B-cell and extranodal NK/T-cell lymphomas. Laryngoscope. 2015;125:1077-1083. [DOI] [PubMed] [Google Scholar]