Abstract
Background:
Medial meniscal extrusion (MME) has received significant interest because of its correlation with medial meniscus root tears (MMRTs), its potential as a diagnostic tool, and its significance in the progression of knee osteoarthritis (OA).
Purpose:
To (1) evaluate if MMRTs significantly increase MME compared with nonroot tears (NRTs) and no tears and (2) determine the clinical outcomes of increased MME.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
Electronic database searches of PubMed, Embase, Scopus, Web of Science, and Cochrane Central Register of Controlled Trials were conducted on June 6, 2022, in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 checklist criteria. The searches were conducted using the keywords “meniscus tear” and “extrusion.” No restrictions were placed on the date of publication. Quality and sensitivity assessments were conducted on included studies. Major MME was defined as an extrusion ≥3 mm.
Results:
Twenty-two studies involving 7882 knees were included. Compared with patients with NRTs, those with MMRTs had a 1.12-mm greater mean absolute meniscal extrusion (AME) and were 3.45 times more likely to have major MME (P < .001 for both). Compared with patients with no tears, those with MMRTs had a 2.13-mm greater AME (P < .001). Within patients with MMRT, those with widely displaced MMRT had a 1.01-mm greater AME compared with nondisplaced MMRT (P < .001). Patients with OA had a 0.73-mm greater AME and were 3.86 times more likely to have major MME compared with patients without OA (P < .001 for both). Within patients who were not stratified according to MMRT, NRT, or no tears, those who eventually developed OA had a 0.79-mm greater AME than those who did not have OA (P = .02).
Conclusion:
Patients with MMRTs had higher MME values compared with those with other types of meniscal tears and those without any meniscal tears. Patients with knee OA were more likely to have higher MME compared with those without OA.
Keywords: knee, meniscal extrusion, osteoarthritis, meniscus root tear
There is interest in the study of medial meniscal extrusion (MME) because of its association with medial meniscus root tears (MMRTs) 35 and its predictive value in the early diagnosis of knee osteoarthritis (OA). 40,47 MME is defined as the significant medial displacement of the medial meniscus with respect to the central margin of the medial tibial plateau. The amount of extrusion is significant when the meniscus extends beyond the tibial margin. MME commonly occurs because of the disruption of collagen fibers within the meniscus that provide hoop tension strength. 1 The circumferential fibers in the meniscus provide hoop tension to resist tensile stress and prevent outward extrusion. 25 When a meniscal tear occurs, there is a potential loss of meniscus hoop stresses. This results in increased MME and progressive degeneration of the articulation cartilage with loading. Thus, MME has also been associated with joint effusions, meniscal tears, and degenerative joint disease. 4,41
Patients with MMRT are evaluated with sudden-onset pain at the back of the knee, which worsens with knee flexion; there is usually posteromedial joint line tenderness. 27,34 However, root tears may be hard to visualize on imaging because of the tear size and orientation. MME has been strongly correlated with meniscus root tears 5,38 and have potential clinical utility to improve the detection of meniscus root tears. Currently, there is a lack of consensus on whether a greater MME would indicate MMRTs over nonroot tears (NRTs) or no meniscal tears.
The primary aim of this meta-analysis was to compare the amount of MME among MMRTs, NRTs, and no meniscal tears to determine if a greater MME can be correlated with MMRTs. Our secondary aim was to evaluate the clinical implications arising from increased MME, in particular the association between the severity of MME and incidence of knee OA. We hypothesized that MMRT would result in the greatest MME compared with other meniscal tears or no tears and that increased MME would result in a greater incidence of knee OA.
Methods
Literature Search
Comprehensive searches of published literature were conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 checklist criteria. 44 Clinical articles reporting either the respective cause of a patient’s MME or clinical outcomes of patients with MME were identified via electronic database searches of PubMed, Scopus, Cochrane Central Register of Controlled Trials, Embase, and Web of Science conducted on June 6, 2022. The searches were conducted using the keywords “meniscus tear” and “extrusion.” The detailed search strategy can be found in Appendix Table A1. There were no restrictions placed on the publication date.
Study Selection and Data Extraction
After eliminating duplicates, study evaluation was performed by an independent blinded pair of authors (F.J.Y.F. and B.W.L.O.). Full texts of potentially eligible articles were extracted, and further analysis was conducted. Backward chaining of references from final retrieved papers was also undertaken to further identify potential articles. Only articles that met the predefined inclusion and exclusion criteria (Table 1) were included in the final analysis. Any discrepancies were resolved by achieving consensus with an independent author (Y.H.D.L.).
Table 1.
Study Inclusion and Exclusion Criteria a
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
a MME, medial meniscal extrusion; MRI, magnetic resonance imaging; NOS, Newcastle-Ottawa Scale.
Data Collection
Data from the included studies were extracted by the same pair of independent investigators (F.J.Y.F. and B.W.L.O.) using a standardized protocol and reporting form. Data extraction was performed to extract study characteristics (study period, location, number of knees, age, and body mass index [BMI]) and clinical outcome data (type of meniscal tear and MME). Means and standard deviations were pooled for the collection of continuous data. When means and standard deviations were not available, and medians with ranges were presented instead, we used previously established models by Wan et al 49 to convert data into means and standard deviations.
The following six comparative data were collected:
Major MME: We accepted both definitions of major MME by Costa et al 10 (>3 mm) and Lerer et al 35 (≥3 mm).
Widely displaced MMRT (WD-MMRT): Defined as measurable tear gap on magnetic resonance imaging (MRI). 3
Nondisplaced MMRT (ND-MMRT): Defined as no measurable tear gap on MRI. 3
Non-OA knees: Defined by the OA Initiative as Kellgren and Lawrence (KL) grade 0 or 1. 5
OA knees: Defined by the OA Initiative as KL grades 2 to 4. 48
Absolute MME: Defined as MME recorded during weightbearing MRI.
Methods of Measuring MME
Jones et al 23 previously described the various methodologies of assessing MME on MRI scans. The reference standard for assessing MME is the “circular edge of tibia to circular edge of meniscus” (CETCEM) method, in which a 3-dimensional analysis of the meniscus is achieved by segmenting the tibia and the meniscus. Only 1 study included in this paper utilized this method. 15 The majority of the studies included in this review utilized the “coronal slices” method, in which MME was measured using the coronal MRI slice, which showed the greatest extrusion measured using the horizontal distance between the most medial aspect of the tibia and the meniscus, respectively (Figure 1).
Figure 1.
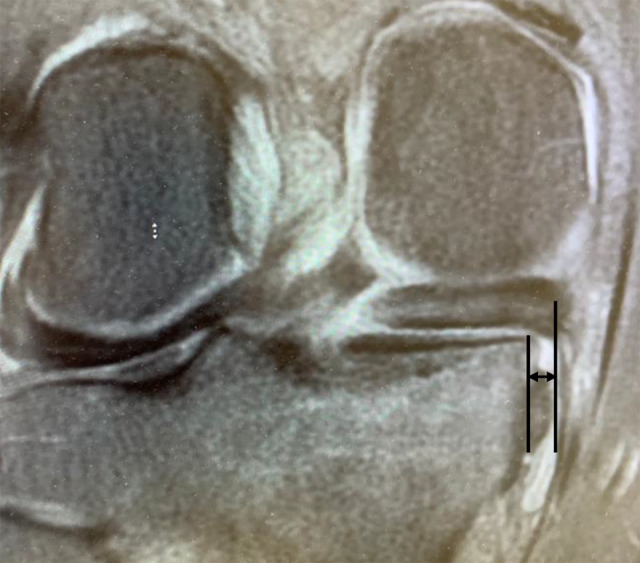
In the coronal slices method, the medial meniscal extrusion (arrows) is measured as the horizontal distance between the most medial aspect of the tibia and the meniscus, respectively (black lines).
Methodological Quality Assessment and Statistical Analysis
The methodological quality of each included article was assessed using the Newcastle-Ottawa Scale (NOS) for the assessment of nonrandomized studies in meta-analyses. 50 The NOS grades each article based on 3 domains: selection of study groups, comparability of groups, and ascertainment of outcome. All 22 studies were of good quality according to the NOS, with a mean score of 8.43 (range, 8-9) (Appendix Table A2).
Comparisons of continuous data such as the mean absolute MME were summarized using the absolute mean difference between groups. For binary data such as incidence of major MME, the odds ratio was summarized using the incidence between groups. All statistical analyses were performed using Review Manager Version 5.3 (RevMan; Cochrane Information Management System) software. Random-effects models were used in all meta-analyses. Heterogeneity between articles was assessed using the I 2 statistic. Interpretations of I 2 were adopted from the Cochrane Handbook, where values of 0% to 50% indicate that heterogeneity might not be important, and 50% to 100% may represent heterogeneity. As all the analyses did not meet the minimum number of studies (>10) required to conduct a meta-regression or funnel plots, subgroup and sensitivity analyses were instead performed to evaluate potential sources of heterogeneity.
Results
Our search strategy yielded 1645 articles after the removal of duplicates. Of these, 1498 articles were excluded based on the title and abstract review. The remaining 147 articles underwent full-text review, of which 22 articles were included in the meta-analysis (Figure 2). All 22 articles selected were retrospective studies. A summary of the study characteristics can be found in Table 2.
Figure 2.
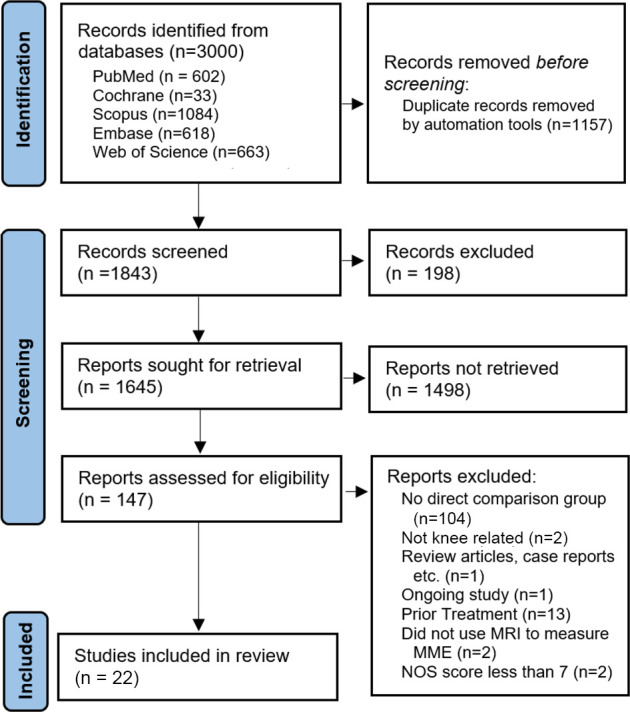
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) diagram of study inclusion and exclusion. MME, medial meniscal extrusion; MRI, magnetic resonance imaging; NOS, Newcastle-Ottawa Scale.
Table 2.
Summary Characteristics of Included Articles a
| Lead Author (Year) | Indications | No. of Patients (M/F) | Knees per Group, n | Patient Age, y, mean ± SD | BMI | Patients With Major MME (>3 mm), n |
|---|---|---|---|---|---|---|
| Costa (2004) 10 | MMRT vs NRT and no tear | 105 (12/93) |
MMRT: 31 NRT: 52 No tear: 22 |
57.25 ± 8.17 | NR | 58 |
| Lerer (2004) 35 | MMRT vs NRT and no tear | 205 (92/113) |
MMRT: 61 NRT: 167 No tear: 106 |
48.75 ± 12.17 | NR | 93 |
| Choi (2010) 5 | MMRT vs NRT | 248 (98/150) |
MMRT: 66 NRT: 182 |
50.75 ± 11 | NR | 127 |
| Lee (2011) 33 | MMRT vs NRT | 102 (30/72) |
MMRT: 17 NRT: 85 |
52.25 ± 5.83 | NR | 57 |
| Park (2012) 45 | MMRT vs NRT and no tear | 67 (32/35) |
MMRT: 24 NRT: 18 No tear: 25 |
MMRT: 53.7 ± 10.6 NRT: 48.8 ± 10.9 No tear: 36.3 ± 16.4 |
NR | NR |
| Ohishi (2014) 42 | MMRT vs NRT and no tear | 188 (89/99) |
MMRT: 44 NRT: 72 No tear:72 |
MMRT: 62.5 ± 11.6 NRT: 59.1 ± 15.3 No tear: 41.1 ± 20.0 |
NR | NR |
| MacFarlane (2017) 37 | MMRT vs NRT | 224 (93/131) |
MMRT: 42 NRT: 182 |
MMRT: 59 ± 8 NRT: 58.5 ± 7.45 |
MMRT: 30 ± 6 NRT: 29.83 ± 6.28 |
85 |
| Goto (2019) 18 |
|
190 (69/121) |
|
59.4 ± 11.1 | 24.1 ± 3 | 136 |
| Liu (2020) 36 | MMRT vs NRT | 115 (66/49) |
MMRT: 11 NRT: 104 |
MMRT: 53 ± 5.5 NRT: 50.5 ± 5.5 |
MMRT: 26.4 ± 3.2 NRT: 25.9 ± 3.5 |
55 |
| Kim (2020) 25 | MMRT vs no tear | 40 (20/20) |
MMRT: 23 No tear: 17 |
MMRT: 63.5 ± 7.7 NRT: 26.5 ± 6.4 |
MMRT: 24.6 ± 24 NRT: 23.4 ± 2.7 |
NR |
| Hisashi (2022) 21 | MMRT vs NRT | 151 (42/109) |
MMRT: 48 NRT: 103 |
MMRT: 67.9 ± 8.2 NRT: 65.8 ± 8.3 |
NR | NR |
| Yoon (2022) 51 | MMRT vs NRT and no tear | 124 (62/62) |
MMRT: 36 NRT: 31 No tear: 57 |
MMRT: 49.79 ± 10.87 NRT: 45.14 ± 10.48 No tear: 41.78 ± 11.48 |
NR | MMRT: 35/36 NRT: 22/31 No tear: 4/57 |
| Bin (2016) 3 | WD-MMRT vs ND-MMRT | 44 (36/8) |
WD-MMRT: 20 ND-MMRT: 24 |
WD-MMRT: 59.8 ± 10.2 ND-MMRT: 55.1 ± 7.4 |
WD-MMRT: 25.2 ± 2.5 ND-MMRT: 25.3 ± 2.8 |
WD-MMRT: 20/20 ND-MMRT: 10/24 |
| Kim (2019) 29 | WD-MMRT vs ND-MMRT | 109 (26/83) |
WD-MMRT: 79 ND-MMRT: 30 |
58.14 ± 9.64 | 26.02 ± 3 | WD-MMRT: 72/79 ND-MMRT: 17/30 |
| Kim (2019) 28 | WD-MMRT vs ND-MMRT | 97 (19/78) |
WD-MMRT: 86 ND-MMRT: 11 |
58.60 ± 8.90 | 25.98 ± 2.89 | NR |
| Ding (2007) 14 | OA vs non-OA | 294 (192/102) |
OA: 21 Non-OA: 273 |
OA: 47.2 ± 5.4 Non-OA: 45.0 ± 6.6 |
OA: 31.3 ± 7.0 Non-OA: 26.8 ± 4.5 |
OA: 11 Non-OA: 41 |
| Crema (2010) 11 | OA vs non-OA | 152 (52/100) |
OA: 58 Non-OA: 94 |
OA: 57.3 ± 8.2 Non-OA: 56.3 ± 8.29 |
OA: 36.7 ± 5.4 Non-OA: 24.8 ± 4.4 |
NR |
| Emmanuel (2016) 15 | OA vs non-OA | 438 (163/275) |
OA: 206 Non-OA: 232 |
OA: 61.5 ± 8.7 Non-OA: 61.0 ± 9.0 |
OA: 29.1 ± 4.2 Non-OA: 27.6 ± 0.3 |
NR |
| Teichtahl (2017) 48 | OA vs non-OA | 4369 (1834/2535) |
OA: 2249 Non-OA: 2120 |
OA: 62.7 ± 9.0 Non-OA: 59.9 ± 9.1 |
OA: 29.8 ± 4.8 Non-OA: 27.6 ± 4.5 |
OA: 771 Non-OA: 207 |
| Özdemir (2019) 43 | OA vs non-OA | 306 (116/190) |
OA: 274 Non-OA: 32 |
OA: 70.96 ± 4.7 Non-OA: 68.25 ± 3.9 |
NR | OA: 177 Non-OA: 16 |
| Jeon (2021) 22 | OA vs non-OA | 86 (27/59) |
OA: 57 Non-OA: 29 |
61 ± 7 | 26.2 ± 3.7 | NR |
| Kim (2020) 26 | OA vs non-OA | 99 (15/84) |
OA: 59 Non-OA: 40 |
55.54 ± 7.5 | NR | NR |
a All studies were retrospective cohort studies. BMI, body mass index; F, female; M, male; MME, medial meniscal extrusion; MMRT, medial meniscus root tear; ND-MMRT, nondisplaced medial meniscus root tear; NR, not recorded; NRT, nonroot tear; OA, osteoarthritis; WD-MMRT, widely displaced medial meniscus root tear.
A total of 7882 knees were included in the meta-analysis. Twelve studies § (n = 1888 knees; 37.34% male patients) compared MME between MMRT and NRT or no tears. There were 539 knees in the MMRT, 1050 knees in the NRT, and 299 knees in the no-tear groups. Three papers 3,28,29 (250 knees; 32.4% male patients) reported WD-MMRT versus ND-MMRT, with 185 knees in the WD-MMRT group and 65 knees in the ND-MMRT group. Seven papers 11,14,15,22,26,43,48 (n = 5744 knees; 41.77% male patients), reported OA versus non-OA. There were 2924 knees in the OA group and 2820 knees in the non-OA group.
Subgroup Analysis Involving Patients With MMRT Versus NRT
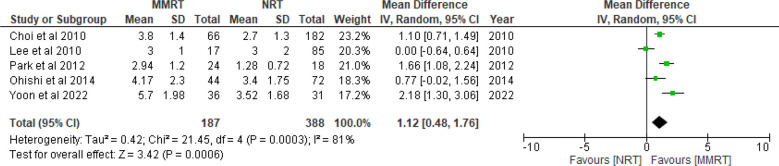
Mean AME
The pooled mean absolute meniscal extrusion (AME) from 5 studies 5,33,42,45,51 (n = 575) was 4.00 ± 1.82 mm for the MMRT group (n = 187) and 2.79 ± 1.47 mm for the NRT group (n = 388). Calculating the standard difference in means of AME between MMRT versus NRT from these studies resulted in a pooled estimate of 1.12 (95% CI, 0.48-1.76; P < .001; I 2 = 81%) (Figure 3). This finding indicates that the mean AME was significantly greater by 1.12 mm for patients with MMRT versus NRT.
Figure 3.
Mean AME between MMRT and NRT. IV, inverse variance.
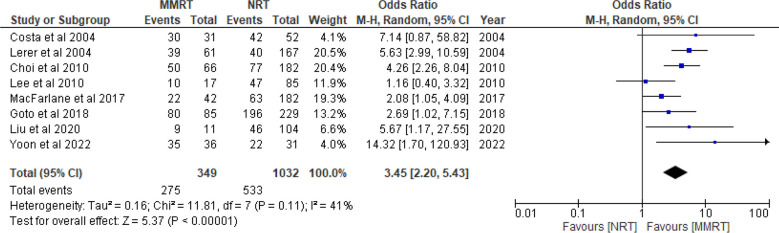
Incidence of Major MME
The pooled number of knees with major MME from 8 studies 5,10,18,33,35 –37,51 (n = 1381) was 275 for the MMRT group (n = 349) and 533 for the NRT group (n = 1032). Calculating the pooled odds ratio of knees that had major MME from these studies resulted in a pooled estimate of 3.45 (95% CI, 2.20-5.43; P < .001; I 2 = 41%) (Figure 4). This finding indicates that patients who had MMRT were 3.45 times more likely to have major MME compared with those who had NRT.
Figure 4.
Incidence of MME between MMRT and NRT. M-H, Mantel-Haenszel.
Subgroup Analysis Involving Patients With MMRT Versus No Meniscal Tears
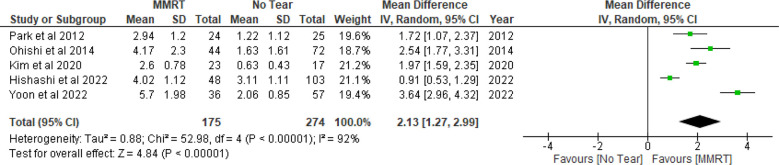
Mean AME
The pooled mean AME from 5 studies 21,25,42,45,51 (n = 449) was 4.07 ± 1.93 mm for the MMRT group (n = 175) and 2.18 ± 1.43 mm for the no-tear group (n = 274). Calculating the standard difference in means of AME between MMRT versus no tears from these studies resulted in a pooled estimate of 2.13 (95% CI, 1.27-2.99; P < .001; I 2 = 92%) (Figure 5). The finding indicates that the mean AME was significantly greater by 2.13 mm for patients with MMRT versus no tears.
Figure 5.
Mean AME between MMRT and NRT.
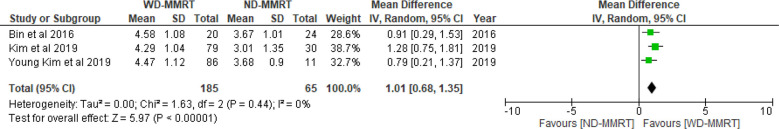
Subgroup Analysis Involving Patients With WD-MMRT vs ND-MMRT
Mean AME
The pooled AME from 3 studies 3,28,29 (n = 250) was 4.41 ± 1.08 mm for the WD-MMRT group (n = 185) and 3.67 ± 1.20 mm for the ND-MMRT group (n = 65). Calculating the standard difference in means of AME between WD-MMRT versus ND-MMRT from these studies resulted in a pooled estimate of 1.01 (95% CI, 0.68-1.35; P < .001; I 2 = 0%) (Figure 6). The finding indicates that the mean AME was significantly greater by 1.01 mm in patients with WD-MMRT versus ND-MMRT.
Figure 6.
Mean AME between WD-MMRT and ND-MMRT.
Subgroup Analysis Involving Patients With OA Versus Non-OA
Mean AME
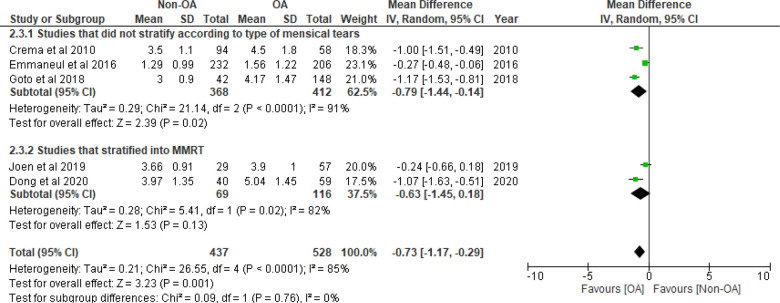
The pooled AME for non-OA from 5 studies 11,15,18,22,26 (n = 965) was 2.33 ± 1.53 mm for the non-OA group (n = 437) and 3.27 ± 1.95 mm for the OA group (n = 528). Calculating the standard difference in means of AME between non-OA and OA from these studies resulted in a pooled estimate of –0.73 mm (95% CI, –1.17 to –0.29; P = .001; I 2 = 85%) (Figure 7). The finding suggests that the mean AME was significantly smaller by 0.73 mm in non-OA patients versus those with OA.
Figure 7.
Mean AME between OA and non-OA.
In a subgroup analysis of 3 studies 11,15,18 (n = 780) comparing the mean AME between non-OA and OA patients who were not specified to have MMRT, NRT, or no tears, the baseline AME for non-OA was significantly lower compared with OA (–0.79 mm; 95% CI, –1.44 to –0.14; P = .02; I 2 = 91%).
In a subgroup analysis of 2 studies 22,26 (n = 185) comparing AME between non-OA and OA patients with MMRT, the baseline AME in non-OA was not significantly lower compared with OA (–0.63 mm; 95% CI, –1.45 to 0.18; P = .13; I 2 = 82%).
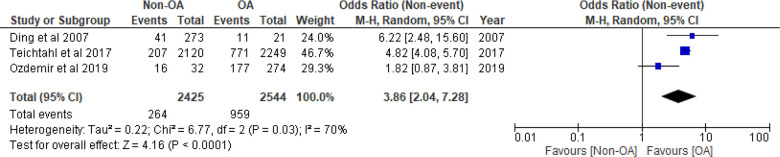
Incidence of Major Meniscal Extrusion
The pooled number of knees that had major MME from 3 studies 14,48 (n = 4969) was 595 for the OA group (n = 2544) and 264 for the non-OA group (n = 2425). Calculating the pooled odds ratio of MME between the OA and non-OA groups from these studies resulted in a pooled estimate of 3.86 (95% CI, 2.04-7.28; P < .001; I 2 = 70%) (Figure 8). This finding indicates that patients with OA were 3.86 times more likely to have major MME compared with those who did not have OA.
Figure 8.
Incidence of MME between OA and non-OA.
Discussion
The most important finding of this study was that MMRTs had a significantly greater mean AME compared with NRTs and no tears. Furthermore, MMRTs had a 3.45 times higher likelihood of major MME compared with NRTs.
For patients with MMRTs, WD-MMRTs had a significantly greater mean AME compared with ND-MMRTs. A cadaveric biomechanical study found that when physiological loading (1800 N) was applied, the torn meniscus root had a wider gap compared with an absence of a load (0 N). 20 The results highlight that prolonged weightbearing after an MMRT results in greater displacement of the tear gap and MME, which exposes the tibial articular surface, increasing the risk of chondral wear progression. Although some previous studies have reported a lack of correlation between major MME and MMRTs, 3,33 Bin et al 3 hypothesized that these differences arose due to MMRTs having different stages depending on tear site displacement. Hence, these studies could have assessed the knee in different time points after an MMRT. Overall, the majority of the studies show that MME is sensitive for MMRTs. 10,39
Patients with no meniscal tears and knees without OA had mean meniscal extrusions of 2.18 ± 1.43 and 2.33 ± 1.53 mm, respectively. This may be related to a variety of possible origins that result in meniscal extrusion, including meniscus degeneration. With meniscus degeneration, the meniscus increases in size due to the formation of microcysts and separation of fibrils. This alteration in meniscal morphology affects the meniscus’ ability to resist hoop strain, 19 stretching the fibers outward and causing MME. 10 Krych et al 31 also observed that isolated meniscal extrusions are associated with meniscotibial ligament abnormality.
It has been suggested that varus malalignment is a risk factor for increased MME. 16,18 There were insufficient papers to perform a proper subanalysis, and therefore, we were unable to draw conclusions for it as a risk factor. Both Erquicia et al 16 and Goto et al 18 reported that there was no significant correlation between the degree of meniscal extrusion and varus alignment in non-OA knees and nonmajor MME knees, respectively. 16 However, both Crema et al 12 and Goto et al 18 noted correlation between the degree of MME and varus alignment in knees with major MME. When structurally intact, the meniscus can offset the influence of the varus alignment. However, once the structural integrity of the meniscus is compromised, such as in meniscus degeneration or with a root tear, the varus malalignment becomes significant, increasing the risk of OA progression. 30
Ding et al 14 reported that obese individuals had nearly a 5-fold increased risk of having MME. They also reported that those with past knee injury were nearly 4 times more likely to have increased MME. Further studies are required to investigate the effect of these risk factors (varus malalignment, obesity, and previous knee injury) on MME. These factors could account for the incidence of meniscal extrusion seen in the patients with no MMRTs in this review study.
For patients who had MMRTs, there was no significant difference in mean AME between OA and non-OA knees. Therefore, increased MME is a pathognomonic finding of MMRTs (regardless of the OA severity) and aids the diagnosis of MMRTs.
In this study, we also report that patients with knee OA had a greater mean AME than non-OA knees; OA knees tended to have 3.86 times more likelihood of having major MME. For studies that did not stratify patients according to types of meniscal tears, those who had OA knees had a significantly greater mean AME compared with those who had non-OA knees. This reinforces the relationship we know that exists between MME, cartilage degeneration, and OA development.
Increased MME in an MMRT can be likened to a “total meniscectomy” in terms of knee joint contact pressure and kinematics. 2 The nonoperative treatment for MMRTs often leads to poor treatment outcomes in patients with large meniscal extrusion ratio. 32 Clinicians should consider routinely measuring MME with serial repeat MRI scans to aid in the treatment decision. When treating MMRTs, meniscal repairs have been shown to achieve superior clinical outcomes compared with partial meniscectomy. 9 A recent cadaveric biomechanical study found that the utilization of an anatomic transtibial pull-out root repair with centralization suture techniques achieved better restoration of the contact mechanics of the knee and meniscal extrusion when compared with nonanatomic repairs. 13
However, there are studies that have shown that meniscus root repair does not significantly decrease postoperative MME 6,24,46 or OA progression. 8 A recent meta-analysis found that 33.5% of patients treated via meniscal repair underwent conversion to total knee arthroplasty within 10 years. 17 Chung et al 7 observed that preoperative varus alignment and increased postoperative meniscal extrusions were poor prognostic factors of meniscal repair. Future studies are required to investigate the efficacy of meniscus root repair in decreasing meniscal extrusions and preventing OA progression.
Limitations
We acknowledge several limitations in this study. First, all included articles were retrospective in nature. To minimize the inherent bias of retrospective studies, we utilized the NOS to appraise the methodology of each included article. Two articles that scored less than 7 were excluded. The final articles included had a mean score of 8.43 (range, 8-9). Second, high heterogeneity was observed between the studies. This could be due to the differences in the way papers report their data. A majority of papers utilized the coronal slices method when measuring MME, and a study by Jones et al 23 found that the coronal slices method tends to overestimate maximal extrusion compared with the reference CETCEM method, reducing the accuracy of the values measured. However, as most of the studies utilized the same coronal slices method to measure MME in NRTs and no tears, the inaccuracy of the conclusions drawn from the results is minimized. All efforts were taken to standardize the data analyzed, and subgroup analysis was undertaken, when appropriate, to further minimize the I 2 values. Third, as there were inadequate studies investigating the temporal relationship between MME and the risk of development of knee OA, it is challenging to form a temporal relationship between MME and the development of OA.
Conclusion
Patients with MMRT have higher MME compared with other types of meniscal tears and those without any meniscal tears. Patients who had OA were more likely to have higher meniscal extrusion compared with patients who did not have knee OA.
APPENDIX
Table A1.
Search Strategy
| PICO | MeSH | Keywords |
|---|---|---|
| Meniscus Tear | “Tibial Meniscus Injuries” [MeSH] | “Menisc* injur*” / “Menisc* tear*” / “Menisc* torn*” / “Flap tear*” / “Flap torn*” / “Bucket Handle Tear*” / “Bucket handle torn*” |
| Extrusion | — | extrusion* / sublux* / protru* |
| Databases Searched | ||
PubMed, Embase, Web of Science:
| ||
Scopus:
| ||
Cochrane:
| ||
Table A2.
Newcastle-Ottawa Scale. a
| Selection | Comparability | Outcome | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Lead Author (Year) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | Total |
| Costa (2004) 10 | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | 8 |
| Lerer (2004) 35 | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | 8 |
| Choi (2010) 5 | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | 8 |
| Lee (2011) 33 | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | 8 |
| Park (2012) 45 | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | 8 |
| Ohishi (2014) 42 | ◊ | ◊ | ◊ | ◊ | ◊◊ | ◊ | ◊ | ◊ | 9 |
| MacFarlane (2017) 37 | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | 8 |
| Goto (2019) 18 | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | 8 |
| Liu (2020) 36 | ◊ | ◊ | ◊ | ◊ | ◊◊ | ◊ | ◊ | ◊ | 9 |
| Kim (2020) 25 | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | 8 |
| Hisashi (2022) 21 | ◊ | ◊ | ◊ | ◊ | ◊◊ | ◊ | ◊ | ◊ | 9 |
| Yoon (2022) 51 | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | 8 |
| Bin (2016) 3 | ◊ | ◊ | ◊ | ◊ | ◊◊ | ◊ | ◊ | ◊ | 9 |
| Kim (2019) 29 | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | 8 |
| Kim (2019) 28 | ◊ | ◊ | ◊ | ◊ | ◊◊ | ◊ | ◊ | ◊ | 9 |
| Ding (2007) 14 | ◊ | ◊ | ◊ | ◊ | ◊◊ | ◊ | ◊ | ◊ | 9 |
| Crema (2010) 11 | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | 8 |
| Emmanuel (2016) 15 | ◊ | ◊ | ◊ | ◊ | ◊◊ | ◊ | ◊ | ◊ | 9 |
| Teichtahl (2017) 48 | ◊ | ◊ | ◊ | ◊ | ◊◊ | ◊ | ◊ | ◊ | 9 |
| Özdemir (2019) 43 | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | 8 |
| Jeon (2021) 22 | ◊ | ◊ | ◊ | ◊ | ◊◊ | ◊ | ◊ | ◊ | 9 |
| Kim (2020) 26 | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | ◊ | 8 |
a One diamond indicates 1 point. A maximum of 2 diamonds can be awarded for the “Selection” and “Outcome” categories (columns 1-4 and 6-8). A maximum of 2 diamonds can be awarded for “Comparability” (column 5). Newcastle-Ottawa Scale items: 1 = representativeness of exposed cohort; 2 = selection of nonexposed cohort; 3 = ascertainment of exposure; 4 = demonstration that outcome of interest was not present at start of study; 5 = comparability of cohorts based on basis of design or analysis; 6 = assessment of outcomes; 7 = follow-up long enough for outcomes to occur; 8 = adequacy of follow-up of cohorts.
Footnotes
Final revision submitted October 19, 2022; accepted October 26, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: Y.H.D.L. has received speaking fees from Arthrex, DePuy Mitek, and Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Adams JG, McAlindon T, Dimasi M, Carey J, Eustace S. Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin Radiol. 1999;54(8):502–506. [DOI] [PubMed] [Google Scholar]
- 2. Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90(9):1922–1931. [DOI] [PubMed] [Google Scholar]
- 3. Bin SI, Jeong TW, Kim SJ, Lee DH. A new arthroscopic classification of degenerative medial meniscus root tear that correlates with meniscus extrusion on magnetic resonance imaging. Knee. 2016;23(2):246–250. [DOI] [PubMed] [Google Scholar]
- 4. Breitenseher MJ, Trattnig S, Dobrocky I, et al. MR imaging of meniscal subluxation in the knee. Acta Radiol. 1997;38(5):876–879. [DOI] [PubMed] [Google Scholar]
- 5. Choi CJ, Choi YJ, Lee JJ, Choi CH. Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy. 2010;26(12):1602–1606. [DOI] [PubMed] [Google Scholar]
- 6. Chung KS, Ha JK, Ra HJ, Kim JG. A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1455–1468. [DOI] [PubMed] [Google Scholar]
- 7. Chung KS, Ha JK, Ra HJ, Kim JG. Preoperative varus alignment and postoperative meniscus extrusion are the main long-term predictive factors of clinical failure of meniscal root repair. Knee Surg Sports Traumatol Arthrosc. 2021;29(12):4122–4130. [DOI] [PubMed] [Google Scholar]
- 8. Chung KS, Ha JK, Ra HJ, et al. Pullout fixation for medial meniscus posterior root tears: clinical results were not age-dependent, but osteoarthritis progressed. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):189–196. [DOI] [PubMed] [Google Scholar]
- 9. Chung KS, Ha JK, Ra HJ, Yu WJ, Kim JG. Root repair versus partial meniscectomy for medial meniscus posterior root tears: comparison of long-term survivorship and clinical outcomes at minimum 10-year follow-up. Am J Sports Med. 2020;48(8):1937–1944. [DOI] [PubMed] [Google Scholar]
- 10. Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol. 2004;183(1):17–23. [DOI] [PubMed] [Google Scholar]
- 11. Crema MD, Guermazi A, Li L, et al. The association of prevalent medial meniscal pathology with cartilage loss in the medial tibiofemoral compartment over a 2-year period. Osteoarthritis Cartilage. 2010;18(3):336–343. [DOI] [PubMed] [Google Scholar]
- 12. Crema MD, Roemer FW, Felson DT, et al. Factors associated with meniscal extrusion in knees with or at risk for osteoarthritis: the multicenter osteoarthritis study. Radiology. 2012;264(2):494–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Daney BT, Aman ZS, Krob JJ, et al. Utilization of transtibial centralization suture best minimizes extrusion and restores tibiofemoral contact mechanics for anatomic medial meniscal root repairs in a cadaveric model. Am J Sports Med. 2019;47(7):1591–1600. [DOI] [PubMed] [Google Scholar]
- 14. Ding C, Martel-Pelletier J, Pelletier JP, et al. Knee meniscal extrusion in a largely non-osteoarthritic cohort: association with greater loss of cartilage volume. Arthritis Res Ther. 2007;9(2):R21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Emmanuel K, Quinn E, Niu J, et al. Quantitative measures of meniscus extrusion predict incident radiographic knee osteoarthritis—data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2016;24(2):262–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Erquicia J, Gelber PE, Cardona-Munoz JI, et al. There is no relation between mild malalignment and meniscal extrusion in trauma emergency patients. Injury. 2012;43(suppl 2):S68–S72. [DOI] [PubMed] [Google Scholar]
- 17. Faucett SC, Geisler BP, Chahla J, et al. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: clinical and economic effectiveness. Am J Sports Med. 2019;47(3):762–769. [DOI] [PubMed] [Google Scholar]
- 18. Goto N, Okazaki K, Akiyama T, et al. Alignment factors affecting the medial meniscus extrusion increases the risk of osteoarthritis development. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2617–2623. [DOI] [PubMed] [Google Scholar]
- 19. Hajek PC, Gylys-Morin VM, Baker LL, et al. The high signal intensity meniscus of the knee. Magnetic resonance evaluation and in vivo correlation. Invest Radiol. 1987;22(11):883–890. [DOI] [PubMed] [Google Scholar]
- 20. Hein CN, Deperio JG, Ehrensberger MT, Marzo JM. Effects of medial meniscal posterior horn avulsion and repair on meniscal displacement. Knee. 2011;18(3):189–192. [DOI] [PubMed] [Google Scholar]
- 21. Hisashi K, Muneta T, Kohno Y, et al. MRI study of medial meniscus degeneration of osteoarthritic knees with or without posterior root tear. J Exp Orthop. 2022;9(1):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jeon SW, Jung M, Choi CH, Kim SG, Kim SH. Factors related to meniscal extrusion and cartilage lesions in medial meniscus root tears. J Knee Surg. 2021;34(2):178–186. [DOI] [PubMed] [Google Scholar]
- 23. Jones LD, Mellon SJ, Kruger N, et al. Medial meniscal extrusion: a validation study comparing different methods of assessment. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1152–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kaplan DJ, Alaia EF, Dold AP, et al. Increased extrusion and ICRS grades at 2-year follow-up following transtibial medial meniscal root repair evaluated by MRI. Knee Surg Sports Traumatol Arthrosc. 2018;26(9):2826–2834. [DOI] [PubMed] [Google Scholar]
- 25. Kim C, Bin SI, Lee BS, et al. Volumetric assessment of extrusion in medial meniscus posterior root tears through semi-automatic segmentation on 3-tesla magnetic resonance images. Orthop Traumatol Surg Res. 2020;106(5):963–968. [DOI] [PubMed] [Google Scholar]
- 26. Kim DH, Lee GC, Kim HH, Cha DH. Correlation between meniscal extrusion and symptom duration, alignment, and arthritic changes in medial meniscus posterior root tear: research article. Knee Surg Relat Res. 2020;32(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kim JH, Chung JH, Lee DH, et al. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011;27(12):1644–1653. [DOI] [PubMed] [Google Scholar]
- 28. Kim JY, Bin SI, Kim JM, et al. A novel arthroscopic classification of degenerative medial meniscus posterior root tears based on the tear gap. Orthop J Sports Med. 2019;7(3):2325967119827945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kim JY, Bin SI, Kim JM, et al. Tear gap and severity of osteoarthritis are associated with meniscal extrusion in degenerative medial meniscus posterior root tears. Orthop Traumatol Surg Res. 2019;105(7):1395–1399. [DOI] [PubMed] [Google Scholar]
- 30. Kozaki T, Fukui D, Yamamoto E, et al. Medial meniscus extrusion and varus tilt of joint line convergence angle increase stress in the medial compartment of the knee joint in the knee extension position—finite element analysis. J Exp Orthop. 2022;9(1):49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Krych AJ, Bernard CD, Leland DP, et al. Isolated meniscus extrusion associated with meniscotibial ligament abnormality. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3599–3605. [DOI] [PubMed] [Google Scholar]
- 32. Kwak YH, Lee S, Lee MC, Han HS. Large meniscus extrusion ratio is a poor prognostic factor of conservative treatment for medial meniscus posterior root tear. Knee Surg Sports Traumatol Arthrosc. 2018;26(3):781–786. [DOI] [PubMed] [Google Scholar]
- 33. Lee DH, Lee BS, Kim JM, et al. Predictors of degenerative medial meniscus extrusion: radial component and knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):222–229. [DOI] [PubMed] [Google Scholar]
- 34. Lee JH, Lim YJ, Kim KB, Kim KH, Song JH. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25(9):951–958. [DOI] [PubMed] [Google Scholar]
- 35. Lerer DB, Umans HR, Hu MX, Jones MH. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33(10):569–574. [DOI] [PubMed] [Google Scholar]
- 36. Liu X, Ding R, Liu C, Yang B, Wang W. Factors associated with medial meniscal subluxation in knees with medial meniscus tears: a cross-sectional study. Research Square. Preprint posted online August 11, 2020. doi:10.21203/rs.3.rs-35269/v2 [Google Scholar]
- 37. MacFarlane LA, Yang H, Collins JE, et al. Associations among meniscal damage, meniscal symptoms and knee pain severity. Osteoarthritis Cartilage. 2017;25(6):850–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Magee T. MR findings of meniscal extrusion correlated with arthroscopy. J Magn Reson Imaging. 2008;28(2):466–470. [DOI] [PubMed] [Google Scholar]
- 39. Magee T, Shapiro M, Williams D. Prevalence of meniscal radial tears of the knee revealed by MRI after surgery. AJR Am J Roentgenol. 2004;182(4):931–936. [DOI] [PubMed] [Google Scholar]
- 40. Mahmoudian A, Lohmander LS, Jafari H, Luyten FP. Towards classification criteria for early-stage knee osteoarthritis: a population-based study to enrich for progressors. Semin Arthritis Rheum. 2021;51(1):285–291. [DOI] [PubMed] [Google Scholar]
- 41. Miller TT, Staron RB, Feldman F, Cepel E. Meniscal position on routine MR imaging of the knee. Skeletal Radiol. 1997;26(7):424–427. [DOI] [PubMed] [Google Scholar]
- 42. Ohishi T, Suzuki D, Yamamoto K, et al. Medial extrusion of the posterior segment of medial meniscus is a sensitive sign for posterior horn tears. Knee. 2014;21(1):112–118. [DOI] [PubMed] [Google Scholar]
- 43. Özdemir M, Kavak R. Meniscal lesions in geriatric population: prevalence and association with knee osteoarthritis. Curr Aging Sci. 2019;12(1):67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Park HJ, Kim SS, Lee SY, et al. Medial meniscal root tears and meniscal extrusion transverse length ratios on MRI. Br J Radiol. 2012;85(1019):E1032–E1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Perry AK, Lavoie-Gagne O, Knapik DM, et al. Examining the efficacy of medial meniscus posterior root repair: a meta-analysis and systematic review of biomechanical and clinical outcomes. Am J Sports Med. Published online April 6, 2022. doi:10.1177/3635465221077271 [DOI] [PubMed] [Google Scholar]
- 47. Sasaki E, Ota S, Chiba D, et al. Early knee osteoarthritis prevalence is highest among middle-aged adult females with obesity based on new set of diagnostic criteria from a large sample cohort study in the Japanese general population. Knee Surg Sports Traumatol Arthrosc. 2020;28(3):984–994. [DOI] [PubMed] [Google Scholar]
- 48. Teichtahl AJ, Cicuttini FM, Abram F, et al. Meniscal extrusion and bone marrow lesions are associated with incident and progressive knee osteoarthritis. Osteoarthritis Cartilage. 2017;25(7):1076–1083. [DOI] [PubMed] [Google Scholar]
- 49. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of non-randomised studies in meta-analyses. Accessed January 3, 2023. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 51. Yoon SJ, Ahn JM, Kang Y, Kim BR, Kang HS. Morphological changes in the superficial medial collateral ligament on knee MR imaging: association with medial meniscal extrusion and posterior root medial meniscus abnormality. Skeletal Radiol. 2022;51(7):1399–1405. [DOI] [PubMed] [Google Scholar]