Abstract
Background
Suboptimal exposure to antituberculosis (anti-TB) drugs has been associated with unfavourable treatment outcomes. We aimed to investigate estimates and determinants of first-line anti-TB drug pharmacokinetics in children and adolescents at a global level.
Methods
We systematically searched MEDLINE, Embase and Web of Science (1990–2021) for pharmacokinetic studies of first-line anti-TB drugs in children and adolescents. Individual patient data were obtained from authors of eligible studies. Summary estimates of total/extrapolated area under the plasma concentration–time curve from 0 to 24 h post-dose (AUC0–24) and peak plasma concentration (Cmax) were assessed with random-effects models, normalised with current World Health Organization-recommended paediatric doses. Determinants of AUC0–24 and Cmax were assessed with linear mixed-effects models.
Results
Of 55 eligible studies, individual patient data were available for 39 (71%), including 1628 participants from 12 countries. Geometric means of steady-state AUC0–24 were summarised for isoniazid (18.7 (95% CI 15.5–22.6) h·mg·L−1), rifampicin (34.4 (95% CI 29.4–40.3) h·mg·L−1), pyrazinamide (375.0 (95% CI 339.9–413.7) h·mg·L−1) and ethambutol (8.0 (95% CI 6.4–10.0) h·mg·L−1). Our multivariate models indicated that younger age (especially <2 years) and HIV-positive status were associated with lower AUC0–24 for all first-line anti-TB drugs, while severe malnutrition was associated with lower AUC0–24 for isoniazid and pyrazinamide. N-acetyltransferase 2 rapid acetylators had lower isoniazid AUC0–24 and slow acetylators had higher isoniazid AUC0–24 than intermediate acetylators. Determinants of Cmax were generally similar to those for AUC0–24.
Conclusions
This study provides the most comprehensive estimates of plasma exposures to first-line anti-TB drugs in children and adolescents. Key determinants of drug exposures were identified. These may be relevant for population-specific dose adjustment or individualised therapeutic drug monitoring.
Short abstract
Summary estimates and key determinants of anti-TB drug pharmacokinetics in children and adolescents were assessed from globally available data, advocating for dose adjustment or therapeutic drug monitoring in certain groups at risk of suboptimal exposures https://bit.ly/3Vzw4f0
Introduction
Tuberculosis (TB) remains a major global health challenge. Until the coronavirus disease 2019 (COVID-19) pandemic, TB was the leading cause of death from a single infectious agent, ranking above HIV/AIDS [1]. In children <15 years of age, the World Health Organization (WHO) estimated that there were 1.1 million new TB cases and 226 000 TB-related deaths globally in 2020 [1]. Adolescents also suffer a significant burden of the disease, with an estimated 727 000 TB cases among those aged 10–19 years in 2012 [2]. Adequate access to treatment and optimal dosing strategies are essential components of the global strategy to end childhood and adolescent TB [3].
Suboptimal exposures to anti-TB drugs are associated with poor treatment outcomes, including treatment failure, acquired drug resistance and death [4, 5]. Target anti-TB drug exposures in children and adolescents are largely based on pharmacokinetic profiles that approximate adult exposures [6], although pharmacokinetics and pharmacodynamics in young children and adults are potentially different due to maturation factors [7]. Moreover, the sources of pharmacokinetic variability of anti-TB drugs in children and adolescents have not been reviewed systematically. This is likely due to differences between studies in the included study population, study design and methods, drug and dosing characteristics, covariates included in the analysis, and pharmacokinetic assessments and parameters used to interpret the results.
To overcome these challenges, we aimed to summarise pharmacokinetic estimates of first-line anti-TB drugs (i.e. isoniazid, rifampicin, pyrazinamide and ethambutol) in children and adolescents, stratified by study-level characteristics. Furthermore, we aimed to assess patient-level characteristics and key subpopulations in whom pharmacokinetic profiles may differ from the average observed in children with TB. This would identify the potential need for dose adjustment in particular groups or individuals who are at risk of suboptimal drug exposure using currently WHO-recommended dosing strategies.
Methods
Search strategy and selection criteria
This study is registered at PROSPERO with identifier number CRD42018110807. The main outcomes registered in the PROSPERO protocol were analysed in this study. We followed the PRISMA-IPD (Preferred Reporting Items for Systematic Review and Meta-Analyses of Individual Participant Data) guidelines to report the findings [8].
All pharmacokinetic studies of first-line anti-TB drugs in children and adolescents aged 0–18 years treated for drug-susceptible pulmonary and/or extrapulmonary TB were eligible for inclusion in this systematic review and individual patient data meta-analysis. Studies in healthy volunteers and in those receiving first-line drugs for indications other than TB disease (e.g. TB infection and staphylococcal bacteraemia) were excluded, because pathology-mediated pharmacokinetic variations may occur in different disease states [9]. Additionally, review articles, commentaries, editorials and case series with fewer than five patients were excluded.
Relevant studies published between 1 January 1990 and 2 February 2021 were searched in MEDLINE (via PubMed), Embase and Web of Science; the search was updated on 31 December 2021. This timeframe was chosen because of the expected availability of the original datasets. No restrictions with respect to language were applied. A combination of the following MeSH (Medical Subject Headings) terms and key words was used: (tuberculosis or TB) and (first-line anti-TB drugs or isoniazid or rifampicin or pyrazinamide or ethambutol) and (pharmacokinetics or drug concentrations) and (children or adolescents) (supplementary appendix 1).
All articles retrieved by the search strategy were uploaded to Rayyan, a web application for systematic reviews (www.rayyan.ai) [10]. After removing duplicates, all titles and abstracts were screened for eligibility and relevant full-text studies were reviewed by two independent reviewers (F.G. and R.E.W.). Reasons for excluding studies were noted. To find additional studies not retrieved by the search strategy, manual searching was performed from the reference lists of included studies and relevant review articles by two independent reviewers (F.G. and R.E.W.).
In the absence of a validated tool to assess the quality of pharmacokinetic studies, we developed a checklist (supplementary appendix 2) by including relevant criteria according to the ROBINS-I tool for non-randomised studies of interventions [11], supplemented by essential components required for a critical appraisal of clinical pharmacokinetic studies [12]. An expert panel (D.J.T., M.G.G.S., J.S. and J-W.C.A.) evaluated and approved the components to be included in the checklist. Each study was graded as low, moderate or high quality by two independent reviewers (F.G. and R.E.W.).
All discrepancies between the first and second reviewers (F.G. and R.E.W.) during study selection and quality assessment of included studies were resolved by consensus; a third reviewer was not required as there were no persistent disagreements between the two reviewers.
Data management
Authors of eligible studies were asked to provide anonymised patient-level information on demographics (age, sex, weight and height), clinical and laboratory characteristics (type of TB, HIV status, serum creatinine and albumin, arylamine N-acetyltransferase 2 (NAT2) genotypes and solute carrier organic anion transporter family member 1B1 (SLCO1B1) genotypes), medication characteristics (drug dose, drug formulation and administration, dosing time, and dosing interval) and pharmacokinetic characteristics (sampling time and observed plasma concentrations) (supplementary appendix 3).
Ethics approval was provided by the Independent Ethics Committee, University Medical Center Groningen, Groningen, The Netherlands (M21.278329). Data collections were approved by local ethics committees involved in the original studies. Written informed consent from parents or legal guardians and written/verbal assent from older participants was obtained at the time of inclusion.
Study definitions
Children and adolescents with drug-susceptible TB included culture-confirmed cases who were susceptible to at least isoniazid and rifampicin, and clinically diagnosed TB cases who were treated with first-line anti-TB drugs. Anthropometric measurements were transformed into z-score values based on WHO standard reference populations with the zscorer package in R (version 0.3.1). Malnutrition was defined as a weight-for-age and/or height-for-age z-score < −2 but ≥ −3 (moderate) or < −3 (severe) in patients aged <5 years and a height-for-age and/or body mass index-for-age z-score < −2 but ≥ −3 (moderate) or < −3 (severe) in patients aged ≥5 years [13]. Participants were genotypically and phenotypically categorised into rapid, intermediate and slow acetylators based on NAT2 genetic polymorphisms (where available) and isoniazid elimination half-life, respectively (supplementary appendix 4).
Data analysis
Our primary pharmacokinetic measures were total/extrapolated area under the plasma concentration–time curve from 0 to 24 h post-dose (AUC0–24) and peak plasma concentration (Cmax) [14]. AUC0–24 was estimated based on the linear-up/log-down trapezoidal rule and Cmax was derived directly from the concentration–time curves. Pharmacokinetic assessments (supplementary appendix 5) in patients with intensive sampling were performed non-compartmentally with the PKNCA package in R (version 0.9.4); sparse sampling data were excluded.
Study-level summary statistics on geometric means of AUC0–24 and Cmax, and 95% confidence intervals of the geometric mean, were estimated with random-effects meta-analyses using the metafor package in R (version 2.4.0). Heterogeneity was assessed using the I-squared statistic (I2); any level of heterogeneity was allowed to emphasise the importance of between-study variability. To allow a comparison between different doses, AUC0–24 and Cmax were dose-normalised by dividing the individual AUC0–24 and Cmax values by mg·kg−1 dose, then multiplying by the current WHO-recommended paediatric dose for isoniazid (10 mg·kg−1), rifampicin (15 mg·kg−1), pyrazinamide (35 mg·kg−1) and ethambutol (20 mg·kg−1) [15]; data on high-dose rifampicin >35 mg·kg−1 were excluded from this particular analysis as this drug exhibited non-linear kinetics with plasma exposures due to saturation of hepatic clearance [16]. For reporting, AUC0–24 and Cmax estimates were stratified by several groups, including dosing intervals (daily and intermittent (e.g. thrice weekly)), sampling schedules (steady-state (i.e. ≥14 days after the first dose) and non-steady-state) and WHO regions.
The effects of patient-level characteristics on log-transformed AUC0–24 and Cmax were assessed with linear mixed-effects analyses using the lme4 package in R (version 1.1.28), with study-level random effects estimated via restricted maximum likelihood. For these mixed-effects analyses, AUC0–24 and Cmax were not dose-normalised to allow adjustment of the models for drug dose, among other variables. To identify the most relevant variables, base models (adjusted for drug dose only) were developed for each patient characteristic; in each model, observations missing a certain variable were excluded. Next, we adjusted our multivariate models for drug dose, age, sex, severity of malnutrition and HIV status, and completed with variables showing a trend toward association (p<0.1) in the base models. Variance components of a mixed-effects model were estimated, including residual variance, random intercept variance, random slope variance for drug dose, random slope–intercept correlation and intraclass correlation coefficient. The final multivariate models were selected based on the highest total explained variance, the lowest Akaike or Bayesian information criterion value and the largest number of observations included in the models. Fixed-effects regression coefficients (β) were used to assess the degree of change in log-transformed AUC0–24 and Cmax for every 1-unit change in the predictor variable. Statistical significance was accepted at p<0.05.
Subgroup analyses were performed in children aged <5 and <2 years, those weighing ≥25 kg, with steady-state concentrations, with steady-state and daily dosing, and considering the WHO region as a third-level clustering variable.
Results
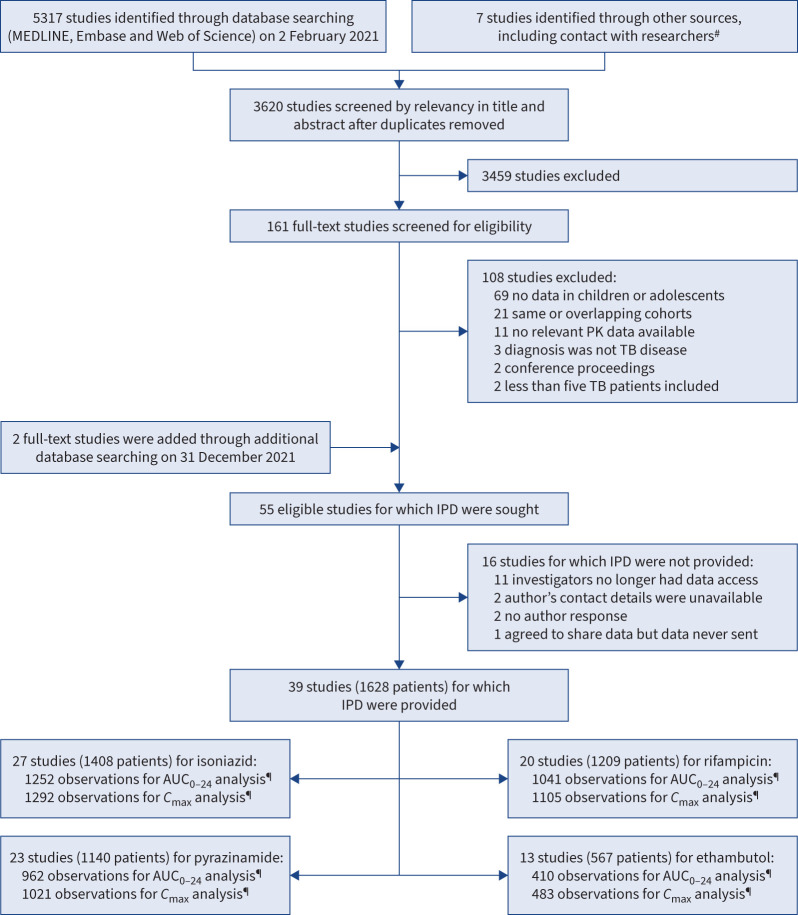
From the 3620 individual articles identified in our search on 2 February 2021, we read titles and abstracts and subsequently screened the full text of 163 studies, including two full-text studies added through an updated search on 31 December 2021 (figure 1). This led to the inclusion of 55 eligible studies and the exclusion of 108 studies, of which 21 had identical or overlapping cohorts with eligible studies (supplementary table E1). Individual patient data were provided for 39 (71%) out of 55 eligible studies (supplementary table E2) [16–53], including unpublished data from one study by Mlotha-Mitole et al. (Blantyre, Malawi). Of these 39 included studies, 26 (67%) were of high quality and 13 (33%) were of moderate quality (supplementary table E3). Of the 16 studies for which individual patient data were not provided, 13 (81%) were conducted in/before the 1990s, when most of the investigators no longer had access to the data (supplementary table E4).
FIGURE 1.
Study selection. #: these included unpublished studies or submitted manuscripts identified through contact with investigators (further details are provided in supplementary table E2); ¶: repeated pharmacokinetic measurements in a patient on different days (different sampling occasions). AUC0–24: area under the plasma concentration–time curve from 0 to 24 h post-dose; Cmax: peak plasma concentration; IPD: individual patient data; PK: pharmacokinetic; TB: tuberculosis.
Among 1628 patients included from 12 countries and three WHO regions, 738 (45.4%) were <5 years of age, 875 (53.7%) were boys, 931 (57.2%) had pulmonary TB, 847 (52.0%) were malnourished and 324 (19.9%) were HIV-positive (table 1). AUC0–24 values were assessed from 1252 (78.6%) out of 1593 observations (i.e. daily occasions) in 1408 patients for isoniazid, 1041 (70.8%) out of 1470 observations in 1209 patients for rifampicin, 962 (73.8%) out of 1304 observations in 1140 patients for pyrazinamide and 410 (72.3%) out of 567 observations in 567 patients for ethambutol (figure 1). A subset of rifampicin data in the study by Denti et al. [49] (n=60/184 observations) was excluded from all AUC0–24 and Cmax analyses based on the use of a poor-quality drug product that has been reported to cause a 61% decrease in rifampicin bioavailability [49], as also confirmed in an earlier study by McIlleron et al. [54]. Details of the observations for which AUC0–24 and Cmax values could not be reliably assessed are presented in supplementary table E5.
TABLE 1.
Demographic and clinical characteristics of children and adolescents with tuberculosis (TB) included in this systematic review and individual patient data meta-analysis
| All patients | Isoniazid | Rifampicin | Pyrazinamide | Ethambutol | |
| Total patients, n | 1628 | 1408 | 1209 | 1140 | 567 |
| Age, years | 5.4 (2.2–9.5) | 5.5 (2.2–9.6) | 5.0 (2.0–9.0) | 5.1 (2.0–9.0) | 5.9 (2.2–9.8) |
| Age | |||||
| <2 years | 356 (21.9) | 311 (22.1) | 301 (24.9) | 274 (24.0) | 121 (21.3) |
| <3 months | 7 (0.4) | 4 (0.3) | 4 (0.3) | 5 (0.4) | 2 (0.3) |
| 3–11 months | 162 (9.9) | 152 (10.8) | 148 (12.2) | 137 (12.0) | 60 (10.6) |
| 12–23 months | 187 (11.5) | 155 (11.0) | 149 (12.3) | 132 (11.6) | 59 (10.4) |
| 2–4 years | 382 (23.5) | 328 (23.3) | 291 (24.1) | 253 (22.2) | 124 (21.9) |
| 5–9 years | 507 (31.1) | 431 (30.6) | 354 (29.3) | 360 (31.6) | 183 (32.3) |
| 10–14 years | 357 (21.9) | 316 (22.4) | 245 (20.3) | 236 (20.7) | 130 (22.9) |
| 15–18 years | 26 (1.6) | 22 (1.6) | 18 (1.5) | 17 (1.5) | 9 (1.6) |
| Sex | |||||
| Female | 753 (46.3) | 641 (45.5) | 549 (45.4) | 512 (44.9) | 270 (47.6) |
| Male | 875 (53.7) | 767 (54.5) | 660 (54.6) | 628 (55.1) | 297 (52.4) |
| WHO region and country | |||||
| African | 827 (50.8) | 721 (51.2) | 678 (56.1) | 570 (50.0) | 377 (66.5) |
| South Africa | 390 (24.0) | 330 (23.4) | 317 (26.2) | 232 (20.3) | 52 (9.2) |
| Ghana | 113 (6.9) | 113 (8.0) | 113 (9.3) | 113 (9.9) | 113 (19.9) |
| Malawi | 150 (9.2) | 105 (7.4) | 103 (8.5) | 128 (11.2) | 121 (21.3) |
| Tanzania | 102 (6.3) | 102 (7.2) | 102 (8.4) | 75 (6.6) | 69 (12.2) |
| Ethiopia | 29 (1.8) | 29 (2.1) | |||
| Zambia | 43 (2.6) | 42 (3.0) | 43 (3.5) | 22 (1.9) | 22 (3.9) |
| Americas | 88 (5.4) | 44 (3.1) | 41 (3.4) | 69 (6.0) | 39 (6.9) |
| Venezuela | 30 (1.8) | 30 (2.1) | 30 (2.5) | 30 (2.6) | 5 (0.8) |
| Paraguay | 15 (0.9) | 14 (1.0) | 11 (0.9) | 15 (1.3) | 15 (2.6) |
| USA | 43 (2.6) | 24 (2.1) | 19 (3.3) | ||
| South-East Asian | 713 (43.8) | 643 (45.7) | 490 (40.5) | 501 (43.9) | 151 (26.6) |
| India | 594 (36.5) | 524 (37.2) | 371 (30.7) | 382 (33.5) | 151 (26.6) |
| Vietnam | 99 (6.1) | 99 (7.0) | 99 (8.2) | 99 (8.7) | |
| Indonesia | 20 (1.2) | 20 (1.4) | 20 (1.6) | 20 (1.7) | |
| Malnourished | |||||
| No | 597 (36.7) | 528 (37.5) | 517 (42.8) | 463 (40.6) | 194 (34.2) |
| Yes, moderate | 373 (22.9) | 339 (24.1) | 328 (27.1) | 281 (24.6) | 151 (26.6) |
| Yes, severe | 474 (29.1) | 404 (28.7) | 355 (29.4) | 358 (31.4) | 196 (34.6) |
| Unknown | 184 (11.3) | 137 (9.7) | 9 (0.7) | 38 (3.3) | 26 (4.6) |
| Type of TB | |||||
| Pulmonary | 931 (57.2) | 809 (57.4) | 721 (59.6) | 652 (57.2) | 413 (72.8) |
| Extrapulmonary | 442 (27.1) | 406 (28.8) | 316 (26.1) | 335 (29.4) | 87 (15.3) |
| Pulmonary+extrapulmonary | 123 (7.6) | 104 (7.4) | 93 (7.7) | 64 (5.6) | 38 (6.7) |
| Unspecified | 132 (8.1) | 89 (6.3) | 79 (6.5) | 89 (7.8) | 29 (5.1) |
| HIV status | |||||
| Negative | 1052 (64.6) | 928 (65.9) | 818 (67.6) | 758 (66.5) | 349 (61.5) |
| Positive | 324 (19.9) | 299 (21.2) | 279 (23.1) | 265 (23.2) | 165 (29.1) |
| Unknown | 252 (15.5) | 181 (12.8) | 112 (9.3) | 117 (10.3) | 53 (9.3) |
| Blood test values | |||||
| Albumin, g·dL−1 (total n=826) | 4.0 (3.6–4.4) | 4.0 (3.6–4.3) | 4.1 (3.6–4.4) | 4.0 (3.6–4.3) | 4.1 (3.7–4.4) |
| Creatinine, mg·dL−1 (total n=609) | 0.5 (0.4–0.7) | 0.5 (0.4–0.6) | 0.5 (0.4–0.7) | 0.5 (0.4–0.6) | 0.4 (0.4–0.5) |
| Drug dose, mg·kg−1 | 9.1 (5.3–11.0) | 11.7 (9.8–15.3) | 30.6 (24.9–35.0) | 20.0 (16.8–23.0) |
Data are presented as n, median (interquartile range) for continuous variables or n (%) for categorical variables, unless otherwise stated. WHO: World Health Organization.
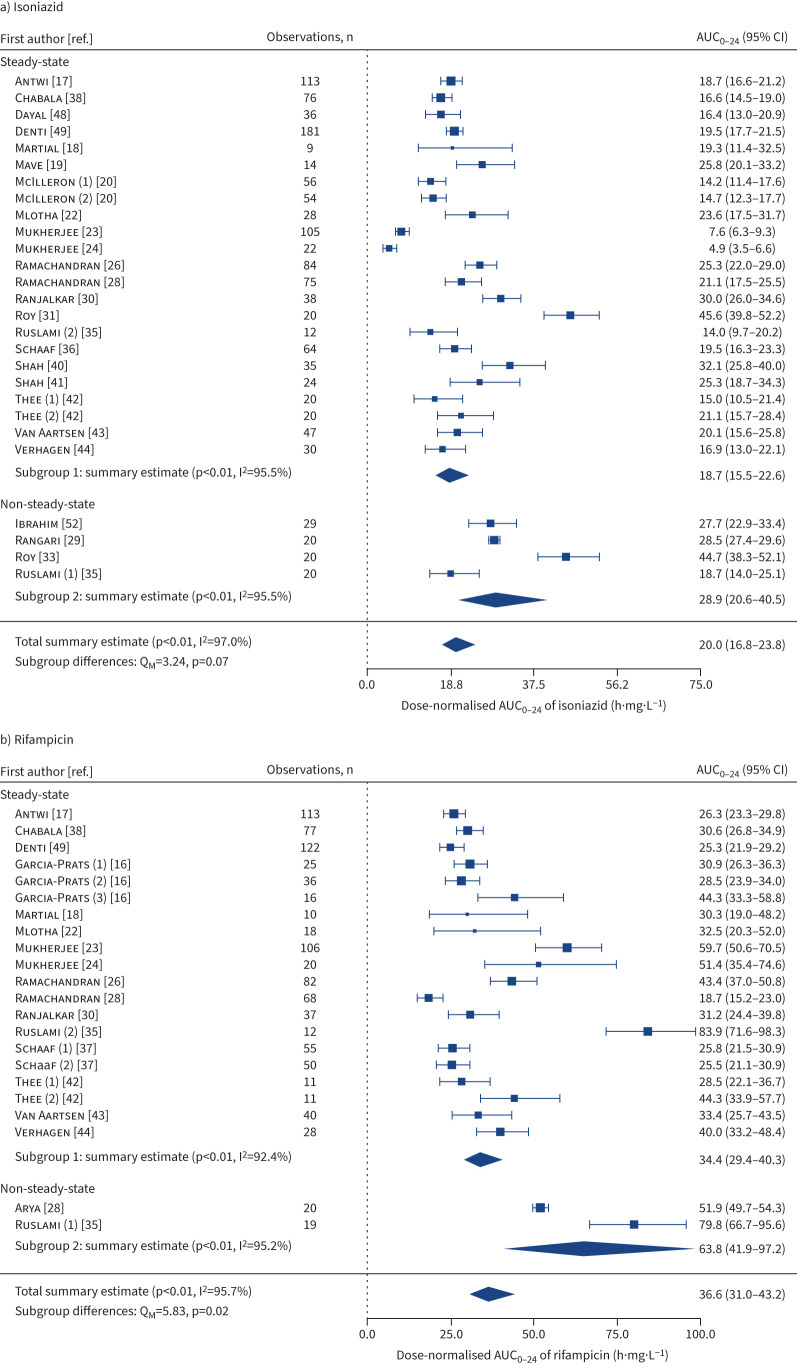
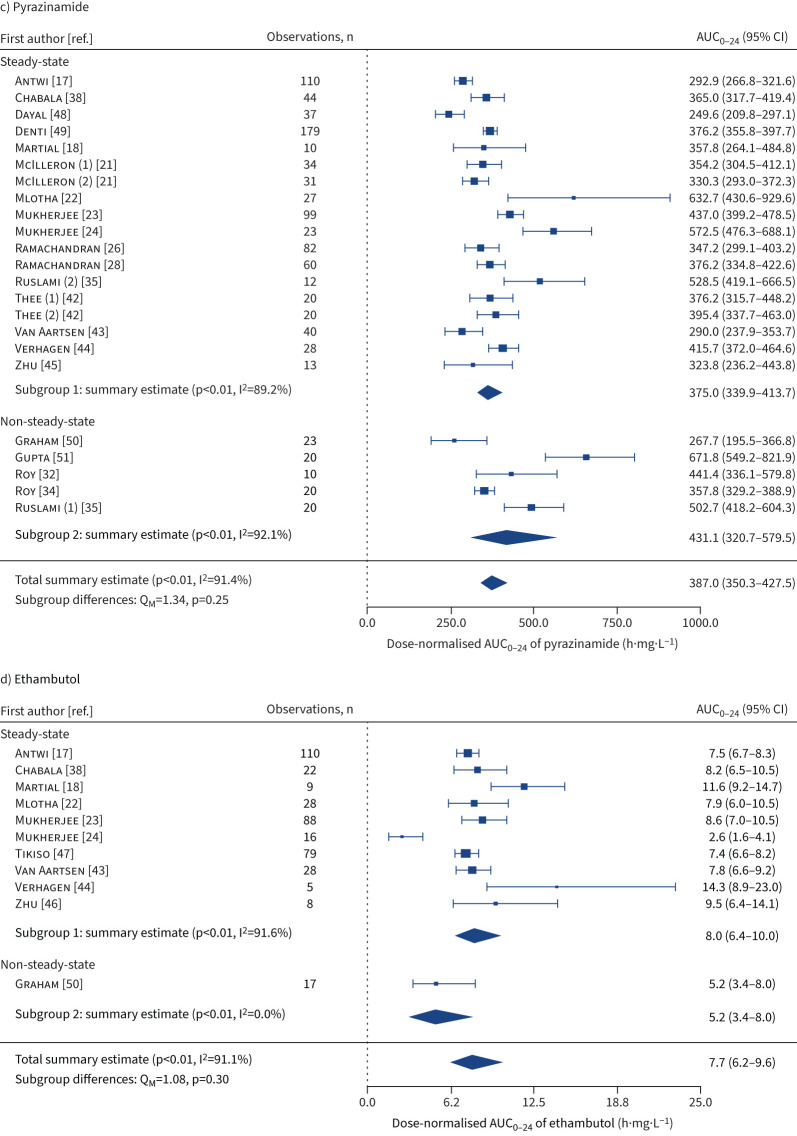
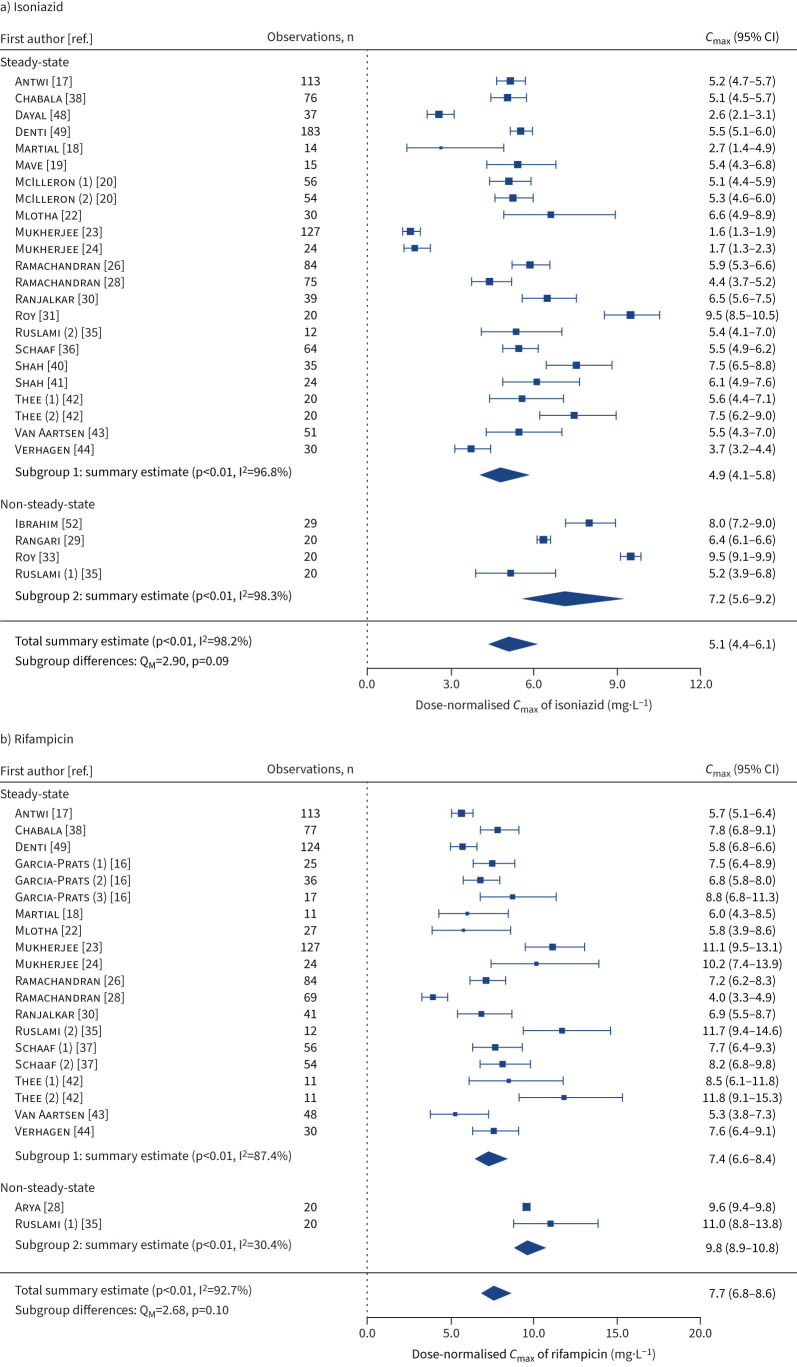
For isoniazid, dose-normalised estimates were summarised for AUC0–24 (geometric mean 18.7 (95% CI 15.5–22.6) h·mg·L−1) (figure 2a) and Cmax (geometric mean 4.9 (95% CI 4.1–5.8) mg·L−1) (figure 3a) in patients with steady-state concentrations, and in other study-level groups (table 2, and supplementary figures E1 and E2). In multivariate mixed-effects analysis (table 3), lower log AUC0–24 values were associated with younger age <2 years (β −0.28 (95% CI −0.40– −0.16)), moderate malnutrition (β −0.10 (95% CI −0.19– −0.01)), severe malnutrition (β −0.15 (95% CI −0.24– −0.06)), HIV-positive status (β −0.15 (95% CI −0.25– −0.04)) and half-life rapid acetylator phenotype (β −0.39 (95% CI −0.50– −0.28)), whereas higher log AUC0–24 values were associated with higher mg·kg−1 doses (β 0.42 (95% CI 0.34–0.51)) and half-life slow acetylator phenotype (β 0.70 (95% CI 0.62–0.77)). Based on NAT2 genotyping, rapid acetylators had lower log AUC0–24 values (β −0.30 (95% CI −0.46– −0.15)), whereas slow acetylators had higher log AUC0–24 values (β 0.71 (95% CI 0.58–0.83)) compared with intermediate acetylators (supplementary table E6). Determinants of isoniazid Cmax were similar to those for AUC0–24, except for moderate malnutrition which had no significant effect on Cmax (table 4).
FIGURE 2.
Forest plots for summary estimates (geometric mean (95% CI)) of dose-normalised area under the plasma concentration–time curve from 0 to 24 h post-dose (AUC0–24) for a) isoniazid, b) rifampicin, c) pyrazinamide and d) ethambutol in children and adolescents with tuberculosis, by sampling schedules (steady-state and non-steady-state). AUC0–24 values were dose-normalised for isoniazid at 10 mg·kg−1, rifampicin at 15 mg·kg−1, pyrazinamide at 35 mg·kg−1 and ethambutol at 20 mg·kg−1. The number in round brackets after the author's name indicates the different sampling occasions within a study. I2: percentage of variation across studies that is due to heterogeneity; QM: omnibus test of all model coefficients.
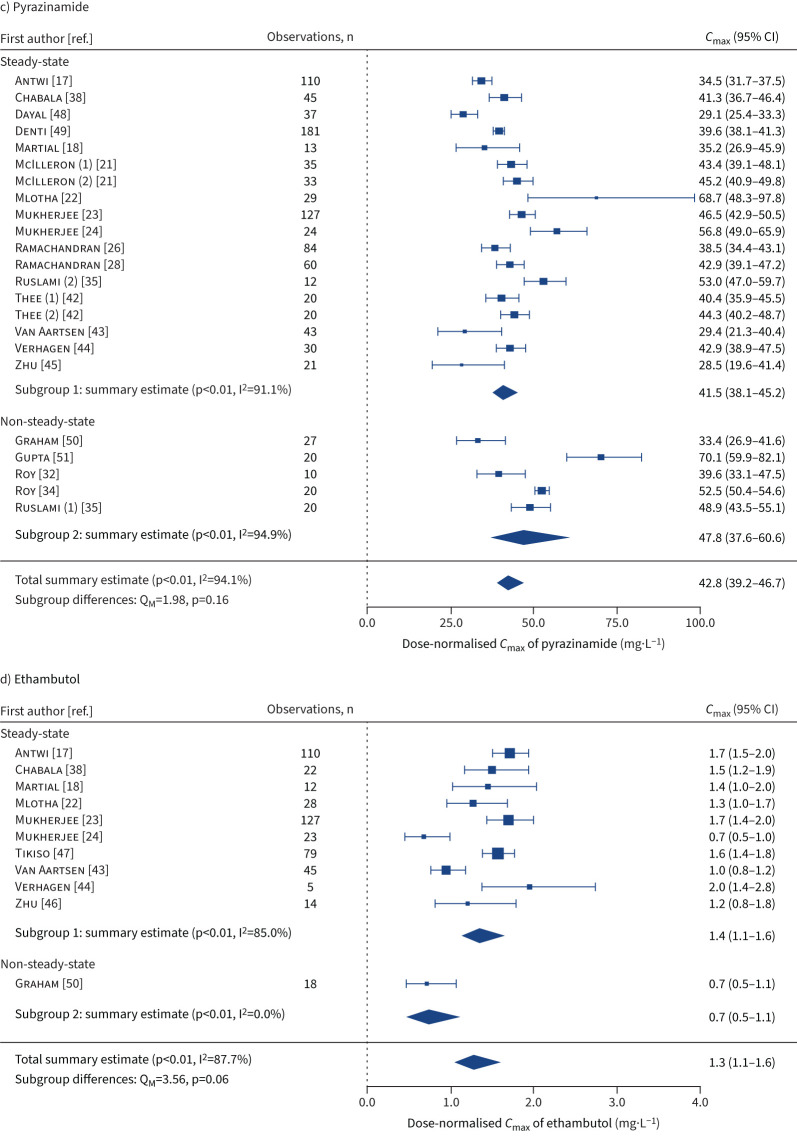
FIGURE 3.
Forest plots for summary estimates (geometric mean (95% CI)) of dose-normalised peak plasma concentration (Cmax) for a) isoniazid, b) rifampicin, c) pyrazinamide and d) ethambutol in children and adolescents with tuberculosis, by sampling schedules (steady-state and non-steady-state). Cmax values were dose-normalised for isoniazid at 10 mg·kg−1, rifampicin at 15 mg·kg−1, pyrazinamide at 35 mg·kg−1 and ethambutol at 20 mg·kg−1. The number in round brackets after the author's name indicates the different sampling occasions within a study. I2: percentage of variation across studies that is due to heterogeneity; QM: omnibus test of all model coefficients.
TABLE 2.
Summary estimates of dose-normalised area under the plasma concentration–time curve from 0 to 24 h post-dose (AUC0–24) and peak plasma concentration (Cmax) values for first-line antituberculosis drugs in children and adolescents with tuberculosis, by dosing intervals, sampling schedules and World Health Organization regions
| Dose-normalised AUC0–24#,¶ | Dose-normalised Cmax#,¶ | |||
|
Summary geometric mean,
h·mg·L−1 (95% CI) |
Heterogeneity I2, % |
Summary geometric mean,
mg·L−1 (95% CI) |
Heterogeneity I2, % | |
| Isoniazid | ||||
| All patients | 20.0 (16.8–23.8) | 97.0 | 5.1 (4.4–6.1) | 98.2 |
| Dosing interval | ||||
| Daily | 18.1 (14.9–22.1) | 95.0 | 4.8 (4.0–5.8) | 96.8 |
| Intermittent | 25.1 (22.7–27.7) | 14.8 | 5.4 (4.7–6.2) | 59.2 |
| Single-dose | 32.7 (24.2–44.2) | 94.3 | 7.8 (6.2–9.9) | 98.3 |
| Sampling schedule | ||||
| Steady-state | 18.7 (15.5–22.6) | 95.5 | 4.9 (4.1–5.8) | 96.8 |
| Non-steady-state | 28.9 (20.6–40.5) | 95.5 | 7.2 (5.6–9.2) | 98.3 |
| WHO region | ||||
| African | 18.8 (16.7–21.1) | 78.4 | 5.8 (5.2–6.4) | 82.6 |
| South-East Asian | 21.1 (15.2–29.2) | 98.4 | 4.9 (3.7–6.6) | 99.1 |
| Americas | 17.4 (13.7–22.0) | 0.0 | 3.6 (2.9–4.4) | 8.8 |
| Rifampicin | ||||
| All patients | 36.6 (31.0–43.2) | 95.7 | 7.7 (6.8–8.6) | 92.7 |
| Dosing interval | ||||
| Daily | 36.5 (30.8–43.4) | 92.8 | 7.8 (6.9–8.7) | 83.7 |
| Intermittent | 29.4 (17.9–48.4) | 95.2 | 5.8 (3.9–8.4) | 90.2 |
| Single-dose | 51.9 (49.7–54.3) | 0.0 | 9.6 (9.4–9.8) | 0.0 |
| Sampling schedule | ||||
| Steady-state | 34.4 (29.4–40.3) | 92.4 | 7.4 (6.6–8.4) | 87.4 |
| Non-steady-state | 63.8 (41.9–97.2) | 95.2 | 9.8 (8.9–10.8) | 30.4 |
| WHO region | ||||
| African | 29.9 (27.1–33.0) | 68.3 | 7.3 (6.4–8.2) | 79.8 |
| South-East Asian | 47.9 (34.0–67.6) | 97.7 | 8.5 (6.6–10.9) | 95.8 |
| Americas | 37.9 (30.4–47.2) | 16.4 | 7.1 (5.8–8.7) | 28.4 |
| Pyrazinamide | ||||
| All patients | 387.0 (350.3–427.5) | 91.4 | 42.8 (39.2–46.7) | 94.1 |
| Dosing interval | ||||
| Daily | 384.1 (343.5–429.4) | 90.8 | 42.0 (38.2–46.2) | 92.1 |
| Intermittent | 326.1 (257.5–413.1) | 82.4 | 38.5 (33.2–44.7) | 73.5 |
| Single-dose | 470.4 (323.9–683.2) | 92.4 | 52.7 (38.6–72.1) | 94.7 |
| Sampling schedule | ||||
| Steady-state | 375.0 (339.9–413.7) | 89.2 | 41.5 (38.1–45.2) | 91.1 |
| Non-steady-state | 431.1 (320.7–579.5) | 92.1 | 47.8 (37.6–60.6) | 94.9 |
| WHO region | ||||
| African | 349.9 (318.4–384.5) | 78.2 | 40.6 (37.4–44.2) | 83.0 |
| South-East Asian | 429.9 (360.2–513.1) | 93.3 | 46.6 (40.2–54.0) | 95.4 |
| Americas | 384.3 (328.6–449.4) | 33.3 | 36.9 (29.4–46.4) | 64.7 |
| Ethambutol | ||||
| All patients | 7.7 (6.2–9.6) | 91.1 | 1.3 (1.1–1.6) | 87.7 |
| Dosing interval | ||||
| Daily | 8.0 (6.4–10.0) | 91.6 | 1.4 (1.1–1.6) | 85.6 |
| Intermittent | 5.2 (3.4–8.0) | 0.0 | 0.7 (0.5–1.1) | 0.0 |
| Sampling schedule | ||||
| Steady-state | 8.0 (6.4–10.0) | 91.6 | 1.4 (1.1–1.6) | 85.0 |
| Non-steady-state | 5.2 (3.4–8.0) | 0.0 | 0.7 (0.5–1.1) | 0.0 |
| WHO region | ||||
| African | 7.5 (7.0–8.0) | 0.0 | 1.3 (1.0–1.6) | 89.4 |
| South-East Asian | 4.8 (1.5–15.6) | 95.3 | 1.1 (0.4–2.7) | 94.5 |
| Americas | 11.5 (9.5–13.8) | 0.0 | 1.5 (1.2–2.0) | 41.8 |
#: AUC0–24 and Cmax values were dose-normalised for isoniazid at 10 mg·kg−1, rifampicin at 15 mg·kg−1, pyrazinamide at 35 mg·kg−1 and ethambutol at 20 mg·kg−1; ¶: forest plots for summary estimates of dose-normalised AUC0–24 and Cmax for isoniazid, rifampicin, pyrazinamide and ethambutol are presented in supplementary figures E1–E8.
TABLE 3.
Multivariate linear mixed-effects regression analyses of determinants affecting log-transformed area under the plasma concentration–time curve from 0 to 24 h post-dose (AUC0–24) values for first-line antituberculosis drugs in children and adolescents
| Isoniazid | Rifampicin | Pyrazinamide | Ethambutol | |||||
|
β
(95% CI) |
Percentage
change, % (95% CI)# |
β (95% CI) |
Percentage
change, % (95% CI)# |
β (95% CI) |
Percentage
change, % (95% CI)# |
β (95% CI) |
Percentage
change, % (95% CI)# |
|
| (Intercept) | 2.56 (2.37–2.74)*** |
3.86 (3.66–4.06)*** |
6.04 (5.90–6.17)*** |
2.44 (2.17–2.71)*** |
||||
| Dose, mg·kg−1¶ | 0.42 (0.34–0.51)*** |
53 (40–66) |
0.65 (0.44–0.85)*** |
91 (55–135) |
0.17 (0.10–0.23)*** |
18 (11–26) |
0.15 (0.05–0.24)** |
16 (5–27) |
| Age | ||||||||
| <2 years+ | −0.28 (−0.40– −0.16)*** |
−24 (−33– −15) |
−0.48 (−0.64– −0.33)*** |
−38 (−47– −28) |
−0.28 (−0.38– −0.17)*** |
−24 (−32– −16) |
−0.55 (−0.76– −0.33)*** |
−42 (−53– −28) |
| 2–4 years | −0.07 (−0.18–0.04) |
−7 (−17–4) |
−0.35 (−0.50– −0.21)*** |
−30 (−39– −19) |
−0.24 (−0.34– −0.14)*** |
−21 (−29– −13) |
−0.35 (−0.55– −0.14)** |
−29 (−42– −13) |
| 5–9 years | −0.04 (−0.14–0.06) |
−4 (−13–6) |
−0.12 (−0.26–0.01)‡ |
−12 (−23–1) |
−0.12 (−0.21– −0.03)** |
−11 (−19– −3) |
−0.19 (−0.37– −0.001)* |
−17 (−31– −0.1) |
| 10–14 years§ | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| 15–18 years | 0.05 (−0.24–0.33) |
5 (−21–40) |
0.22 (−0.16–0.60) |
25 (−15–83) |
−0.004 (−0.27–0.26) |
0.4 (−24–30) |
0.32 (−0.25–0.90) |
38 (−22–145) |
| Sex | ||||||||
| Female | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| Male | −0.03 (−0.10–0.04) |
−3 (−9–4) |
−0.05 (−0.13–0.04) |
−4 (−12–4) |
−0.08 (−0.14– −0.02)** |
−8 (−13– −2) |
−0.03 (−0.16–0.10) |
−3 (−15–11) |
| Malnourished ƒ | ||||||||
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| Yes, moderate | −0.10 (−0.19– −0.01)* |
−9 (−17– −1) |
0.02 (−0.09–0.12) |
2 (−9–13) |
−0.03 (−0.10–0.05) |
−3 (−10–5) |
−0.09 (−0.25–0.08) |
−8 (−22–9) |
| Yes, severe | −0.15 (−0.24– −0.06)** |
−14 (−22– −6) |
−0.02 (−0.13–0.10) |
−2 (−12–10) |
−0.08 (−0.16– −0.005)* |
−8 (−15– −0.5) |
−0.08 (−0.25–0.09) |
−7 (−22–10) |
| Unknown | 0.13 (−0.13–0.39) |
14 (−12–47) |
−0.05 (−0.61–0.51) |
−5 (−46–66) |
−0.002 (−0.23–0.23) |
−0.2 (−21–26) |
−0.04 (−0.56–0.47) |
−4 (−43–60) |
| HIV status | ||||||||
| Negative | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| Positive | −0.15 (−0.25– −0.04)** |
−14 (−22– −4) |
−0.25 (−0.39– −0.11)*** |
−22 (−32– −11) |
−0.19 (−0.29– −0.10)*** |
−18 (−25– −9) |
−0.39 (−0.56– −0.21)*** |
−32 (−43– −19) |
| Unknown | −0.06 (−0.30–0.18) |
−6 (−26–20) |
−0.33 (−0.64– −0.01)* |
−28 (−47– −1) |
0.01 (−0.18–0.20) |
1 (−16–22) |
−0.08 (−0.51–0.35) |
−8 (−40–42) |
| Acetylator status, t1/2 phenotype## | ||||||||
| Slow | 0.70 (0.62–0.77)*** |
100 (85–117) |
||||||
| Intermediate | Reference | Reference | ||||||
| Rapid | −0.39 (−0.50– −0.28)*** |
−32 (−40– −24) |
||||||
| Unknown | 0.44 (0.25–0.63)*** |
55 (29–88) |
||||||
| Random effects | ||||||||
| σ2 (mean±sd) | 0.35±0.59 | 0.47±0.68 | 0.21±0.46 | 0.44±0.66 | ||||
| τ00 studies (mean±sd) | 0.12±0.35 | 0.11±0.32 | 0.04±0.21 | 0.08±0.27 | ||||
| τ11 studies×doses (mean±sd) | 0.03±0.16 | 0.12±0.34 | 0.01±0.10 | |||||
| ρ01 studies | −0.74 | −0.25 | −0.15 | |||||
| ICC | 0.27 | 0.35 | 0.21 | 0.15 | ||||
| Nstudies | 27 | 22 | 23 | 11 | ||||
| Observations | 1252 | 1041 | 962 | 410 | ||||
| Conditional R2 | 0.59 | 0.63 | 0.34 | 0.28 | ||||
β: fixed-effects regression coefficient; t1/2: elimination half-life; σ2: residual variance; τ00: random intercept variance; τ11: random slope variance; ρ01: random slope–intercept correlation, ICC: interclass correlation estimate; Nstudies: number of included studies (studies or study occasions); conditional R2: proportion of variance explained by both the fixed and random effects. #: percentage change was calculated as: (eβ−1)×100%; ¶: dose was mean-centred by subtracting the mean from each data point, then standardised by dividing each point by the standard deviation; +: among children <2 years of age, AUC0–24 values were significantly higher in patients aged 3–11 months compared with those aged 12–23 months for pyrazinamide (p<0.001), but no significant differences were found for isoniazid, rifampicin and ethambutol (the results were adjusted for drug dose in mg·kg−1, sex, nutritional status and HIV status); §: we used children aged 10–14 years as a reference group, assuming that they were the most adult-like among children under <15 years of age, and also to assess the statistical difference with older adolescents aged 15–18 years; ƒ: moderate malnutrition was defined as weight-for-age or height-for-age z-score ≥ −3 but < −2 in children aged <5 years and height-for-age or body mass index-for-age z-score ≥ −3 but < −2 in children aged ≥5 years, and severe malnutrition was defined as weight-for-age or height-for-age z-score < −3 in children aged <5 years and height-for-age or body mass index-for-age z-score < −3 in children aged ≥5 years; ##: acetylator phenotypes of isoniazid were rapid (t1/2 <1.25 h), intermediate (t1/2 1.25–2 h) and slow (t1/2 >2 h). ***: p<0.001; **: p<0.01; *: p<0.05; ‡: p<0.1.
TABLE 4.
Multivariate linear mixed-effects regression analyses of determinants affecting log-transformed peak plasma concentration (Cmax) values for first-line antituberculosis drugs in children and adolescents
| Isoniazid | Rifampicin | Pyrazinamide | Ethambutol | |||||
|
β
(95% CI) |
Percentage
change, % (95% CI)# |
β
(95% CI) |
Percentage
change, % (95% CI)# |
β
(95% CI) |
Percentage
change, % (95% CI)# |
β
(95% CI) |
Percentage
change, % (95% CI)# |
|
| (Intercept) | 1.46 (1.27–1.65)*** |
2.21 (2.01–2.41)*** |
3.74 (3.62–3.86)*** |
0.75 (0.49–1.00)*** |
||||
| Dose, mg·kg−1¶ | 0.40 (0.29–0.52)*** |
50 (33–68) |
0.52 (0.33–0.72)*** |
69 (38–106) |
0.16 (0.11–0.22)*** |
18 (11–25) |
0.13 (0.05–0.22)** |
14 (5–24) |
| Age | ||||||||
| <2 years+ | −0.28 (−0.40– −0.16)*** |
−24 (−33– −15) |
−0.42 (−0.57– −0.27)*** |
−34 (−43– −24) |
−0.18 (−0.28– −0.09)*** |
−17 (−24– −8) |
−0.68 (−0.90– −0.46)*** |
−50 (−59– −37) |
| 2–4 years | −0.07 (−0.18–0.04) |
−7 (−16–4) |
−0.18 (−0.32– −0.04)** |
−17 (−28– −4) |
−0.15 (−0.25– −0.06)** |
−14 (−22– −6) |
−0.32 (−0.53– −0.11)** |
−27 (−41– −11) |
| 5–9 years | −0.03 (−0.13–0.06) |
−3 (−12–6) |
−0.09 (−0.22–0.04) |
−8 (−19–4) |
−0.10 (−0.18– −0.02)* |
−9 (−16– −2) |
−0.12 (−0.31–0.06) |
−12 (−26–6) |
| 10–14 years§ | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| 15–18 years | −0.03 (−0.31–0.26) |
−3 (−27–29) |
0.06 (−0.31–0.42) |
6 (−27–52) |
−0.02 (−0.26–0.23) |
−2 (−23–25) |
0.10 (−0.51–0.70) |
10 (−40–101) |
| Sex | ||||||||
| Female | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| Male | −0.04 (−0.11–0.03) |
−4 (−10–3) |
0.02 (−0.07–0.10) |
2 (−6–11) |
−0.05 (−0.11–0.001)‡ |
−5 (−10– −0.1) |
−0.03 (−0.17–0.10) |
−3 (−15–10) |
| Malnourishedƒ | ||||||||
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| Yes, moderate | −0.06 (−0.14–0.03) |
−5 (−13–3) |
−0.03 (−0.14–0.07) |
−3 (−13–8) |
−0.02 (−0.09–0.05) |
−2 (−8–5) |
−0.10 (−0.27–0.07) |
−10 (−24–7) |
| Yes, severe | −0.09 (−0.18– −0.003)* |
−9 (−17– −0.3) |
−0.12 (−0.24– −0.01)* |
−12 (−21– −1) |
−0.10 (−0.18– −0.03)** |
−10 (−16– −3) |
−0.12 (−0.29–0.06) |
−11 (−25–6) |
| Unknown | 0.07 (−0.20–0.34) |
7 (−18–40) |
−0.14 (−0.67–0.39) |
−13 (−49–48) |
0.05 (−0.15–0.26) |
6 (−14–30) |
−0.33 (−0.78–0.12) |
−28 (−54–12) |
| HIV status | ||||||||
| Negative | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| Positive | −0.17 (−0.28– −0.06)** |
−16 (−24– −6) |
−0.25 (−0.39– −0.11)*** |
−22 (−32– −10) |
−0.11 (−0.20– −0.03)* |
−11 (−18– −3) |
−0.35 (−0.53– −0.17)*** |
−29 (−41– −15) |
| Unknown | 0.05 (−0.20–0.29) |
5 (−18–33) |
−0.19 (−0.49–0.11) |
−17 (−49–12) |
−0.05 (−0.22–0.12) |
−5 (−20–13) |
0.04 (−0.34–0.43) |
4 (−29–53) |
| Acetylator status, t1/2 phenotype## | ||||||||
| Slow | 0.23 (0.15–0.31)*** |
26 (16–36) |
||||||
| Intermediate | Reference | Reference | ||||||
| Rapid | −0.13 (−0.25– −0.02)* |
−12 (−22– −2) |
||||||
| Unknown | −0.38 (−0.53– −0.23)*** |
−31 (−40– −20) |
||||||
| Random effects | ||||||||
| σ2 (mean±sd) | 0.35±0.59 | 0.49±0.73 | 0.19±0.43 | 0.53±0.73 | ||||
| τ00 studies (mean±sd) | 0.13±0.35 | 0.11±0.36 | 0.03±0.19 | 0.06±0.24 | ||||
| τ11 studies×doses (mean±sd) | 0.05±0.22 | 0.10±0.25 | 0.01±0.09 | |||||
| ρ01 studies | −0.33 | 0.02 | −0.15 | |||||
| ICC | 0.31 | 0.32 | 0.18 | 0.10 | ||||
| Nstudies | 27 | 22 | 23 | 11 | ||||
| Observations | 1292 | 1105 | 1021 | 483 | ||||
| Conditional R2 | 0.51 | 0.55 | 0.30 | 0.23 | ||||
β: fixed-effects regression coefficient; t1/2: elimination half-life; σ2: residual variance; τ00: random intercept variance; τ11: random slope variance; ρ01: random slope–intercept correlation, ICC: interclass correlation estimate; Nstudies: number of included studies (studies or study occasions); conditional R2: proportion of variance explained by both the fixed and random effects. #: percentage change was calculated as: (eβ−1)×100%; ¶: dose was mean-centred by subtracting the mean from each data point, then standardised by dividing each point by the standard deviation; +: among children <2 years of age, Cmax values were not significantly different in patients aged 3–11 months compared with those aged 12–23 months for isoniazid, rifampicin, pyrazinamide and ethambutol (the results were adjusted for drug dose in mg·kg−1, sex, nutritional status and HIV status); §: we used children aged 10–14 years as a reference, assuming that they were the most adult-like among children under <15 years of age, and also to assess the statistical difference with older adolescents aged 15–18 years; ƒ: moderate malnutrition was defined as weight-for-age or height-for-age z-score ≥ −3 but < −2 in children aged <5 years and height-for-age or body mass index-for-age z-score ≥ −3 but < −2 in children aged ≥5 years, and severe malnutrition was defined as weight-for-age or height-for-age z-score < −3 in children aged <5 years, and height-for-age or body mass index-for-age z-score < −3 in children aged ≥5 years; ##: acetylator phenotypes of isoniazid were rapid (t1/2 <1.25 h), intermediate (t1/2 1.25–2 h) and slow (t1/2 >2 h). ***: p<0.001; **: p<0.01; *: p<0.05; ‡: p<0.1.
For rifampicin, dose-normalised estimates were summarised for AUC0–24 (geometric mean 34.4 (95% CI 29.4–40.3) h·mg·L−1) (figure 2b) and Cmax (geometric mean 7.4 (95% CI 6.6–8.4) mg·L−1) (figure 3b) in patients with steady-state concentrations, and in other study-level groups (table 2, and supplementary figures E3 and E4). In multivariate mixed-effects analysis (table 3), lower log AUC0–24 values were associated with younger age, including ages <2 years (β −0.48 (95% CI −0.64– −0.33)) and 2–4 years (β −0.35 (95% CI −0.50– −0.21)). Furthermore, lower log AUC0–24 values were associated with HIV-positive status (β −0.25 (95% CI −0.39– −0.11)), whereas higher log AUC0–24 values were associated with higher mg·kg−1 doses (β 0.65 (95% CI 0.44−0.85)). Determinants of rifampicin Cmax were similar to those for AUC0–24, with addition of severe malnutrition which was associated with lower log Cmax values (β −0.12 (95% CI −0.24– −0.01)) (table 4).
For pyrazinamide, dose-normalised estimates were summarised for AUC0–24 (geometric mean 375.0 (95% CI 339.9–413.7) h·mg·L−1) (figure 2c) and Cmax (geometric mean 41.5 (95% CI 38.1–45.2) mg·L−1) (figure 3c) in patients with steady-state concentrations, and in other study-level groups (table 2, and supplementary figures E5 and E6). In multivariate mixed-effects analysis (table 3), lower log AUC0–24 values were associated with younger age, including ages <2 years (β −0.28 (95% CI −0.38– −0.17)), 2–4 years (β −0.24 (95% CI −0.34– −0.14)) and 5–9 years (β −0.12 (95% CI −0.21– −0.03)). Furthermore, lower log AUC0–24 values were associated with male sex (β −0.08 (95% CI −0.14– −0.02)), severe malnutrition (β −0.08 (95% CI −0.16– −0.005)) and HIV-positive status (β −0.19 (95% CI −0.29– −0.10)), whereas higher log AUC0–24 values were associated with higher mg·kg−1 doses (β 0.17 (95% CI 0.10–0.23)). Determinants of pyrazinamide Cmax were similar to those for AUC0–24, except for male sex which had no significant effect on Cmax (table 4).
For ethambutol, dose-normalised estimates were summarised for AUC0–24 (geometric mean 8.0 (95% CI 6.4–10.0) h·mg·L−1) (figure 2d) and Cmax (geometric mean 1.4 (95% CI 1.1–1.6) mg·L−1) (figure 3d) in patients with steady-state concentrations, and in other study-level groups (table 2, and supplementary figures E7 and E8). In multivariate mixed-effects analysis (table 3), lower log AUC0–24 values were associated with younger age, including ages <2 years (β −0.55 (95% CI −0.76– −0.33)), 2–4 years (β −0.35 (95% CI −0.55– −0.14)) and 5–9 years (β −0.19 (95% CI −0.37– −0.001)). Furthermore, lower log AUC0–24 values were associated with HIV-positive status (β −0.39 (95% CI −0.56– −0.21)), whereas higher log AUC0–24 values were associated with higher mg·kg−1 doses (β 0.15 (95% CI 0.05–0.24)). Determinants of ethambutol Cmax were similar to those for AUC0–24, except for ages 5–9 years which had no significant effect on Cmax (table 4).
In dose-adjusted mixed-effects analyses, we identified additional determinants of lower log AUC0–24 values, including severe stunting (i.e. height-for-age z-score < −3) for isoniazid (β −0.13 (95% CI −0.24– −0.02)), rifampicin (β −0.13 (95% CI −0.25– −0.01)), pyrazinamide (β −0.16 (95% CI −0.24– −0.07)) and ethambutol (β −0.19 (95% CI −0.37– −0.02)); moderate stunting (i.e. height-for-age z-score ≥ −3 but < −2) for pyrazinamide (β −0.09 (95% CI −0.17– −0.02)); severe underweight (i.e. weight-for-age z-score < −3) for pyrazinamide (β −0.10 (95% CI −0.19– −0.01)); and SLCO1B1 (rs4149032) TT genotype for rifampicin (β −0.34 (95% CI −0.61– −0.08)). Detailed results of the dose-adjusted analyses for AUC0–24 and Cmax are presented in supplementary tables E7–E14.
The determinants of AUC0–24 and Cmax remained consistent and largely unchanged in several subgroup analyses among children aged <5 years (supplementary tables E15 and E16), patients with steady-state concentrations (supplementary tables E19 and E20), patients with steady-state concentrations and daily dosing (supplementary tables E21 and E22), and considering WHO region as a third-level clustering variable (supplementary tables E23 and E24). Additionally, the adult doses recommended for children weighing ≥25 kg were associated with lower log AUC0–24 values for isoniazid (4–6 mg·kg−1; β −1.01 (95% CI −1.27– −0.76)) and rifampicin (8–10 mg·kg−1; β −0.35 (95% CI −0.63– −0.07)) compared with paediatric doses (supplementary tables E25 and E26). Additional pharmacokinetic estimates for time to Cmax, elimination half-life and elimination rate constant are presented in supplementary table E27.
Discussion
In this individual patient data meta-analysis, we summarised plasma AUC0–24 and Cmax estimates for first-line anti-TB drugs in several study-level groups of children and adolescents with TB from globally representative studies. We also identified patient-level determinants of plasma exposures to first-line anti-TB drugs in these children and adolescents.
Compared with adult data, our summary estimates for steady-state AUC0–24 were comparable for isoniazid (geometric mean 18.7 (95% CI 15.5–22.6) versus median range 11.6–26.3 h·mg·L−1) [55], pyrazinamide (geometric mean 375.0 (95% CI 339.9–413.7) versus median range 233–429 h·mg·L−1) [55] and rifampicin (geometric mean 34.4 (95% CI 29.4−40.3) versus mean 38.7 (95% CI 34.4–43.0) h·mg·L−1) [56], but were lower for ethambutol (geometric mean 8.0 (95% CI 6.4–10.0) versus median range 16–28 h·mg·L−1) [55], regardless of significant methodological heterogeneities among studies included in two systematic reviews assessing these estimates for adult TB patients [55, 56]. Ideally, target AUC0–24 and Cmax values are established based on pharmacokinetic/pharmacodynamic knowledge, taking drug efficacy, safety and tolerability into account [14]. However, unlike pharmacokinetic studies in adults, most paediatric studies lack data on clinical and bacteriological responses to TB treatment, probably due to the paucibacillary disease and the difficulty in obtaining microbiological specimens. This has resulted in a significant challenge in establishing target AUC0–24 and Cmax values based on pharmacokinetic/pharmacodynamic analyses. Until these pharmacokinetic/pharmacodynamic targets are available, our summary AUC0–24 and Cmax estimates can serve as real-life reference values for clinicians and researchers working on dosing of first-line anti-TB drugs in children and adolescents.
In general, children <15 years of age have high TB treatment success rates (88–96%) [1, 57, 58], although among those with severe disease like TB meningitis, mortality rates are high (10–30%) [59–61]. In the present study, the relationship between pharmacokinetics and treatment outcomes was not the primary focus, and the outcome data were unavailable from the majority of included studies (n=34/39 (87%)). It should be noted that pharmacokinetic studies of anti-TB drugs in paediatric patients typically have a smaller sample size and are therefore not powered to analyse the impact of drug exposure on treatment outcome. It is therefore important to include pharmacokinetic data in large outcome studies [14, 62].
Young children are most vulnerable to severe forms of disease, including miliary TB and TB meningitis. Lower drug exposures in young children, especially those <2 years of age, are likely attributed to the non-linear effect of weight on clearance due to allometric scaling, which results in reduced exposures in smaller children when dosed at the same mg·kg−1 as bigger children and adolescents [63]. Additionally, these could be due to lower bioavailability of isoniazid and rifampicin in children <2–3 years of age [49]. For TB meningitis, these low plasma exposures could lead to extremely low exposures at the site of infection in the meninges, especially for rifampicin and ethambutol which have poor cerebrospinal fluid penetration [25, 35]. Higher rifampicin doses can be considered for paediatric TB meningitis [64], and for paediatric TB in general [16], with good safety profiles [16]. However, higher ethambutol doses may increase the risk of ocular toxicity [65], highlighting the importance of exploring substitutes for ethambutol such as ethionamide or fluoroquinolones (e.g. levofloxacin).
Importantly, children and adolescents weighing ≥25 kg who received WHO-recommended adult doses had lower isoniazid and rifampicin exposures than those on WHO-recommended paediatric doses. The use of adult fixed-dose combination doses has also resulted in suboptimal exposures in South African and Zambian children weighing ≥25 kg [38]. Further investigation on paediatric formulation and revision of weight bands are needed to optimise dosing of first-line anti-TB drugs [49], including those for children weighing ≥25 kg.
Different levels of low exposures to first-line anti-TB drugs in children and adults living with HIV have recently been reported in two systematic reviews, but the estimates were not adjusted for confounders, and consistent results could not be obtained due to methodological and statistical heterogeneities among the included studies [55, 66]. The impact of HIV on reducing exposures to first-line anti-TB drugs has been hypothesised to be due to malabsorption of the drugs in patients with advanced HIV co-infection [67]. However, as antiretroviral data were unavailable in our dataset, further research is needed to assess the potential impact of antiretroviral therapy on anti-TB drug pharmacokinetics in children and adolescents living with HIV.
Severe malnutrition was found to have small but significant negative effects on isoniazid and pyrazinamide exposures. For highly protein-bound rifampicin [68], the protein-unbound fraction may be higher in patients with severe protein-energy malnutrition, which may have resulted in similar plasma exposures to protein-unbound rifampicin between patients with and without malnutrition, as supported by an adult study [69]. In our dose-adjusted models, lower exposures to all first-line drugs were observed in severely stunted patients, but our results varied among underweight and wasted patients. Importantly, the same enteropathogens that cause stunting have recently been demonstrated to negatively impact first-line anti-TB drug pharmacokinetics in malnourished children [43]. Taken together, we suspect various degrees and predispositions to malnutrition may have different impacts on physiological alterations that affect anti-TB drug pharmacokinetics [70].
The potential benefits of NAT2 genotype-guided isoniazid dosing in reducing toxicity and treatment failure have been reported in adult patients [71]. In resource-limited settings where genotyping is rarely available, an automated assay on the GeneXpert platform can be used as an alternative option to detect NAT2 polymorphisms and guide isoniazid dosing [72]. Next, our results showed that SLCO1B1 polymorphisms had moderate negative effects on rifampicin exposures, although these results were only obtained from two studies among African children [17, 49]. SLCO1B1 polymorphisms associated with lower rifampicin exposures have been reported to be more common in African adult patients [73] and these might partly explain the lower rifampicin exposures in our patients from African versus non-African regions.
There has been growing interest in the use of shorter TB treatment regimens. Recent clinical trials have shown that 4 months of anti-TB treatment with a rifapentine-based regimen containing moxifloxacin in adults with pulmonary TB [74], and with a standard first-line anti-TB drug regimen in children with non-severe TB [58], were non-inferior to the standard 6-month regimen and showed excellent treatment outcomes. High-yield opportunities for stratified and personalised medicine approaches, including differential dosing for key subpopulations, should be explored as potential alternatives to the traditional one-size-fits-all strategy [75]. Although programmatic TB treatment may be suitable for most patients, stratification of treatment and a more person-centred approach in certain groups is necessary to ensure high-quality care, such as in patients at risk of suboptimal exposure to anti-TB drugs, patients at risk of developing drug-related toxicity and patients who could benefit from therapeutic drug monitoring [62]. In addition, less invasive therapeutic drug monitoring methods using saliva, hair and dried blood spot samples should be explored in further studies to reduce the burden of venous blood sampling in this population [14, 62, 76].
This study has limitations that should be acknowledged. First, summary pharmacokinetic estimates in study-level groups showed high heterogeneities, although we were able to correct these estimates by individual-level covariates and variance components in mixed-effects models. Second, although dose-normalised exposures for high-dose rifampicin >35 mg·kg−1 were not estimated due to saturation of hepatic clearance (4% of all observations) [16], the effect on standard doses cannot be ruled out [49] and therefore the rifampicin estimates should be interpreted carefully. Third, we were unable to reliably assess AUC0–24 and Cmax on sparse sampling data from three published studies [25, 39, 53] and one unpublished study (Mlotha-Mitole et al., Blantyre, Malawi). Further studies using pharmacokinetic/pharmacodynamic modelling and Monte Carlo simulations are needed to better characterise the relationships of physiologically sensible covariates with pharmacokinetic parameters (e.g. drug clearance and volume of distribution) and to design more optimal dosing strategies [14], by including both intensive and sparse sampling data. In addition, given that only protein-unbound concentrations are generally considered to exhibit pharmacological effects, the inclusion of a protein binding parameter in future pharmacokinetic/pharmacodynamic models may be important, especially for rifampicin, as only ∼10–20% of the total drug concentration can freely penetrate to the site of infection [68, 77]. Fourth, none of the included studies were from European countries, and there was a lack of data in children aged <3 months and adolescents aged 15–18 years. The latter is likely due to the historically fragmented approach of only classifying persons aged <15 years as children, excluding those aged 15–18 years from both paediatric and adult studies [78]. Despite these limitations, our findings provide the most comprehensive study-level estimates of plasma exposures to first-line anti-TB drugs by including ∼30 years of available data worldwide and therefore the results can be generalised to the global population of children aged >3 months to 14 years. Additionally, our mixed-effects models include a wide range of variables and our results are consistent in various subgroup analyses.
In conclusion, our systematic review and individual patient data meta-analysis summarised pharmacokinetic estimates of first-line anti-TB drugs in children and adolescents using a large amount of globally available data. Although children and adolescents with TB generally have good treatment outcomes with standardised treatment approaches in previous reports, certain subgroups at risk of suboptimal drug exposures, especially children <2 years of age and those with severe malnutrition or HIV, may require population-specific dose adjustment or individualised therapeutic drug monitoring. Designing more optimal dosing strategies using pharmacokinetic/pharmacodynamic modelling and simulations is warranted in these vulnerable groups. This is important for policymakers and TB programmes to ensure the best treatment outcome in children and adolescents with TB.
Supplementary material
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplementary material ERJ-01596-2022.Supplement (6MB, pdf)
Shareable PDF
Acknowledgements
This paper is a tribute to the late Bob Wilffert (University of Groningen, Groningen, The Netherlands), who contributed to the conception and design of this study, but sadly passed away in July 2021. We thank Sjoukje van der Werf (University Medical Center Groningen, Groningen, The Netherlands) for helping with developing the initial search strategy and Taichi Ochi (University of Groningen, Groningen, The Netherlands) for helping with the interpretation of genetic data. We also thank all contributing institutions, investigators, parents or legal guardians and patients involved in the original studies.
Footnotes
Author contributions: F. Gafar, B. Wilffert† and J-W.C. Alffenaar designed the study and protocol. F. Gafar, R.E. Wasmann, H.M. McIlleron, R.E. Aarnoutse, H.S. Schaaf, D. Agarwal, S. Antwi, N.D. Bang, A. Bekker, D.J. Bell, C. Chabala, L. Choo, G.R. Davies, J.N. Day, R. Dayal, P. Denti, P.R. Donald, E. Engidawork, A.J. Garcia-Prats, D. Gibb, S.M. Graham, A.C. Hesseling, S.K. Heysell, M.I. Idris, S.K. Kabra, A. Kinikar, A.K.H. Kumar, A. Kwara, R. Lodha, C. Magis-Escurra, N. Martinez, B.S. Mathew, V. Mave, E. Mduma, R. Mlotha-Mitole, S.G. Mpagama, A. Mukherjee, H.M. Nataprawira, C.A. Peloquin, T. Pouplin, G. Ramachandran, J. Ranjalkar, V. Roy, R. Ruslami, I. Shah, Y. Singh, E.M. Svensson, S. Swaminathan, U. Thatte, S. Thee, T.A. Thomas, T. Tikiso, A. Turkova, T. Velpandian, L.M. Verhagen, J.L. Winckler, H. Yang and V. Yunivita contributed individual patient data. F. Gafar analysed the data and created tables and figures under the supervision of J. Stevens and J-W.C. Alffenaar. F. Gafar wrote the initial draft of the manuscript under the supervision of K. Taxis, J. Stevens and J-W.C. Alffenaar. R.E. Wasmann, H.M. McIlleron, R.E. Aarnoutse, H.S. Schaaf and B.J. Marais were members of the writing committee, and helped revise the drafted manuscript before and after circulation to all co-authors. All authors provided critical input and revisions to manuscript drafts and approved the final version of the manuscript before submission for publication.
This article has an editorial commentary: https://doi.org/10.1183/13993003.02003-2022
Conflict of interest: H.S. Schaaf reports grants from the NIH/IMPAACT; and honoraria from Ann Lake publications (sponsored by Johnson & Johnson) for an educational publication on the management of MDR-TB in children. A. Bekker reports grants from IMPAACT, UNITAID; lecture honoraria from Sandoz; support for attending PENTA PIM meeting; and received generic LPV/r, 3TC and ABC for the PETITE study. D.J. Bell reports support for attending a meeting from ViiV pharmaceuticals; and attendance fees for an advisory board meeting from ViiV pharmaceuticals. L. Choo reports grants from the UKRI MRC DFID Wellcome NIHR Joint Global Health Trials, TB Alliance Support for trial drug purchase and UKRI COVID-19 Grant Extension Allocation Award. P. Denti reports a grant for WHO expert review for TB drugs in children. S.M. Graham reports participation on a data safety monitoring board for the TB CHAMP trial; and leadership roles as a co-chair for the Guidelines Development Committee of the WHO updated recommendations and consolidated guidelines on child and adolescent TB, and as a core member for the WHO Child and Adolescent TB Working Group. S.K. Heysell reports grants from the NIH, DANIDA and EDTCP; royalties or licences from UpToDate; and honoraria for lectures from Henry Stewart Talks. A. Kwara reports a grant from the NIH/NICHD. V. Mave reports grants from the NIH and CDC. C.A. Peloquin reports a grant from the NIH. V. Roy reports a grant from the Delhi State TB Association; and leadership roles as a member of the Delhi State TB Association and the MAMC TB Committee. E.M. Svensson reports grants from the NWO personal Veni, IMI UNITE4TB consortium, TB Alliance, UNITAID BenefitKids consortium, WHO expert review, NIH support for IMPAACT studies, Blueprint, Probex, ACTG study Clo-FAST, Janssen Pharmaceuticals, EDCTP support PanTB-HM and Legochem; and leadership or fiduciary roles in the ISOP DI&E committee and BenNeLux PMX organising committee. U. Thatte reports participation on a data safety monitoring board for an ICMR TB trial. T.A. Thomas reports grants from the NIH and the University of Virginia. D.J. Touw reports a grant from Chiesi; consulting fees from Pure IMS and Sanguin; and participation on a data safety monitoring board for the FORMAT trial. A. Turkova reports grants from the UKRI MRC DFID Wellcome NIHR Joint Global Health Trials and MRC Grants for core funding of the Medical Research Council Clinical Trials Unit at the UCL; and TB Alliance Support for SHINE trial drug purchase. All of this work was declared by the authors to be outside the submitted work. All other authors declare no competing interests.
Support statement: Funding for this systematic review and individual patient data meta-analysis was received from the Indonesia Endowment Fund for Education (LPDP; 201711220412046) through the University of Groningen, awarded as a PhD scholarship to F. Gafar. This funding body had no role in the study conception and design, data collection and analysis, writing and reviewing of the manuscript or decision to publish. For the original studies included in this individual patient data meta-analysis, financial supports were received from the Eunice Kennedy Shriver National Institute of Child Health and Human Development at the National Institutes of Health (HD071779 and R01HD069175), the UK Medical Research Council (MRC) and the Department for International Development (DFID) Wellcome NIHR Joint Global Health Trials (MR/L004445/1), the TB Alliance through the UNITAID-funded STEP-TB project, the Wellcome Trust UK, the Armauer Hansen Research Institute, the National Institute of Allergy and Infectious Diseases at the National Institutes of Health (K23AI097197 and U01AI115594), the Department of Clinical Pharmacology of the University Medical Center Groningen through the Stichting Suppletiefonds Sonnevanck, the Clinical Pharmacology Unit Department Fund and the Institutional Fluid Research Grant of the Christian Medical College and Hospital Vellore, the Bristol-Myers Squibb “Secure the Future” Foundation, the Indian Council of Medical Research, the Delhi Tapedic Unmulan Samiti, the Delhi State TB Association, the Academic Leadership Grant of the Universitas Padjadjaran, the Indonesia Endowment Fund for Education, and the General Clinical Research Center Grant of the National Institutes of Health (M01RR00051 and 1RO1AI37845). The findings and conclusions of this systematic review and individual patient data meta-analysis are those of the authors and do not represent the views of these grant providers. Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.World Health Organization . Global tuberculosis report 2021. 2021. www.who.int/publications/i/item/9789240037021 Date last accessed: 11 August 2022.
- 2.Snow KJ, Sismanidis C, Denholm J, et al. . The incidence of tuberculosis among adolescents and young adults: a global estimate. Eur Respir J 2018; 51: 1702352. doi: 10.1183/13993003.02352-2017 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization . Roadmap towards ending TB in children and adolescents, 2nd ed. 2018. https://apps.who.int/iris/handle/10665/275422 Date last accessed: 11 August 2022.
- 4.Swaminathan S, Pasipanodya JG, Ramachandran G, et al. Drug concentration thresholds predictive of therapy failure and death in children with tuberculosis: bread crumb trails in random forests. Clin Infect Dis 2016; 63: S63–S74. doi: 10.1093/cid/ciw471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pasipanodya JG, Srivastava S, Gumbo T. Meta-analysis of clinical studies supports the pharmacokinetic variability hypothesis for acquired drug resistance and failure of antituberculosis therapy. Clin Infect Dis 2012; 55: 169–177. doi: 10.1093/cid/cis353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schaaf HS, Garcia-Prats AJ, Donald PR. Antituberculosis drugs in children. Clin Pharmacol Ther 2015; 98: 252–265. doi: 10.1002/cpt.164 [DOI] [PubMed] [Google Scholar]
- 7.Fernandez E, Perez R, Hernandez A, et al. . Factors and mechanisms for pharmacokinetic differences between pediatric population and adults. Pharmaceutics 2011; 3: 53–72. doi: 10.3390/pharmaceutics3010053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stewart LA, Clarke M, Rovers M, et al. . Preferred reporting items for a systematic review and meta-analysis of individual participant data: the PRISMA-IPD statement. JAMA 2015; 313: 1657–1665. doi: 10.1001/jama.2015.3656 [DOI] [PubMed] [Google Scholar]
- 9.Roberts JA, Taccone FS, Lipman J. Understanding PK/PD. Intensive Care Med 2016; 42: 1797–1800. doi: 10.1007/s00134-015-4032-6 [DOI] [PubMed] [Google Scholar]
- 10.Ouzzani M, Hammady H, Fedorowicz Z, et al. . Rayyan – a web and mobile app for systematic reviews. Syst Rev 2016; 5: 210. doi: 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sterne JAC, Hernán MA, Reeves BC, et al. . ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016; 355: i4919. doi: 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Soliman ABE, Pawluk SA, Wilby KJ, et al. . The use of a modified Delphi technique to develop a critical appraisal tool for clinical pharmacokinetic studies. Int J Clin Pharm 2022; 44: 894–903. doi: 10.1007/s11096-022-01390-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Onis M, Onyango AW, Borghi E, et al. . Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 2007; 85: 660–667. doi: 10.2471/BLT.07.043497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alffenaar JWC, Gumbo T, Dooley KE, et al. . Integrating pharmacokinetics and pharmacodynamics in operational research to end tuberculosis. Clin Infect Dis 2020; 70: 1774–1780. doi: 10.1093/cid/ciz942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization . WHO consolidated guidelines on tuberculosis. Module 5: management of tuberculosis in children and adolescents. 2022. www.who.int/publications/i/item/9789240046764 Date last accessed: 11 August 2022.
- 16.Garcia-Prats AJ, Svensson EM, Winckler J, et al. . Pharmacokinetics and safety of high-dose rifampicin in children with TB: the Opti-Rif trial. J Antimicrob Chemother 2021; 76: 3237–3246. doi: 10.1093/jac/dkab336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Antwi S, Yang H, Enimil A, et al. . Pharmacokinetics of the first-line antituberculosis drugs in Ghanaian children with tuberculosis with or without HIV coinfection. Antimicrob Agents Chemother 2017; 61: e01701-16. doi: 10.1128/AAC.01701-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martial LC, Kerkhoff J, Martinez N, et al. . Evaluation of dried blood spot sampling for pharmacokinetic research and therapeutic drug monitoring of anti-tuberculosis drugs in children. Int J Antimicrob Agents 2018; 52: 109–113. doi: 10.1016/j.ijantimicag.2018.04.020 [DOI] [PubMed] [Google Scholar]
- 19.Mave V, Kinikar A, Kagal A, et al. . Isoniazid concentrations in hair and plasma area-under-the-curve exposure among children with tuberculosis. PLoS One 2017; 12: e0189101. doi: 10.1371/journal.pone.0189101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McIlleron H, Willemse M, Werely CJJ, et al. . Isoniazid plasma concentrations in a cohort of South African children with tuberculosis: implications for international pediatric dosing guidelines. Clin Infect Dis 2009; 48: 1547–1553. doi: 10.1086/598192 [DOI] [PubMed] [Google Scholar]
- 21.McIlleron H, Willemse M, Schaaf HS, et al. . Pyrazinamide plasma concentrations in young children with tuberculosis. Pediatr Infect Dis J 2011; 30: 262–265. doi: 10.1097/INF.0b013e3181fbefe1 [DOI] [PubMed] [Google Scholar]
- 22.Mlotha R, Waterhouse D, Dzinjalamala F, et al. . Pharmacokinetics of anti-TB drugs in Malawian children: reconsidering the role of ethambutol. J Antimicrob Chemother 2015; 70: 1798–1803. doi: 10.1093/jac/dkv039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mukherjee A, Velpandian T, Singla M, et al. . Pharmacokinetics of isoniazid, rifampicin, pyrazinamide and ethambutol in Indian children. BMC Infect Dis 2015; 15: 126. doi: 10.1186/s12879-015-0862-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mukherjee A, Velpandian T, Singla M, et al. . Pharmacokinetics of isoniazid, rifampicin, pyrazinamide and ethambutol in HIV-infected Indian children. Int J Tuberc Lung Dis 2016; 20: 666–672. doi: 10.5588/ijtld.15.0288 [DOI] [PubMed] [Google Scholar]
- 25.Pouplin T, Bang ND, Toi PV, et al. . Naïve-pooled pharmacokinetic analysis of pyrazinamide, isoniazid and rifampicin in plasma and cerebrospinal fluid of Vietnamese children with tuberculous meningitis. BMC Infect Dis 2016; 16: 114. doi: 10.1186/s12879-016-1470-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ramachandran G, Hemanth Kumar AK, Bhavani PK, et al. . Age, nutritional status and INH acetylator status affect pharmacokinetics of anti-tuberculosis drugs in children. Int J Tuberc Lung Dis 2013; 17: 800–806. doi: 10.5588/ijtld.12.0628 [DOI] [PubMed] [Google Scholar]
- 27.Arya A, Roy V, Lomash A, et al. . Rifampicin pharmacokinetics in children under the Revised National Tuberculosis Control Programme, India, 2009. Int J Tuberc Lung Dis 2015; 19: 440–445. doi: 10.5588/ijtld.13.0819 [DOI] [PubMed] [Google Scholar]
- 28.Ramachandran G, Hemanth Kumar AK, Bhavani PK, et al. . Pharmacokinetics of first-line antituberculosis drugs in HIV-infected children with tuberculosis treated with intermittent regimens in India. Antimicrob Agents Chemother 2015; 59: 1162–1167. doi: 10.1128/AAC.04338-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rangari GM, Roy V, Sethi GR, et al. . Blood levels of isoniazid in Indian children with tuberculosis. Indian J Tuberc 2015; 62: 80–85. doi: 10.1016/j.ijtb.2015.04.006 [DOI] [PubMed] [Google Scholar]
- 30.Ranjalkar J, Mathew SK, Philip V, et al. . Isoniazid and rifampicin concentrations in children with tuberculosis with either a daily or intermittent regimen: implications for the revised RNTCP 2012 doses in India. Int J Antimicrob Agents 2018; 51: 663–669. doi: 10.1016/j.ijantimicag.2017.12.004 [DOI] [PubMed] [Google Scholar]
- 31.Roy V, Tekur U, Chopra K. Pharmacokinetics of isoniazid in pulmonary tuberculosis – a comparative study at two dose levels. Indian Pediatr 1996; 33: 287–291. [PubMed] [Google Scholar]
- 32.Roy V, Tekur U, Chopra K. Pharmacokinetics of pyrazinamide in children suffering from pulmonary tuberculosis. Int J Tuberc Lung Dis 1999; 3: 133–137. [PubMed] [Google Scholar]
- 33.Roy V, Gupta D, Gupta P, et al. . Pharmacokinetics of isoniazid in moderately malnourished children with tuberculosis. Int J Tuberc Lung Dis 2010; 14: 374–376. [PubMed] [Google Scholar]
- 34.Roy V, Sahni P, Gupta P, et al. . Blood levels of pyrazinamide in children at doses administered under the revised national tuberculosis control program. Indian Pediatr 2012; 49: 721–725. doi: 10.1007/s13312-012-0164-8 [DOI] [PubMed] [Google Scholar]
- 35.Ruslami R, Gafar F, Yunivita V, et al. . Pharmacokinetics and safety/tolerability of isoniazid, rifampicin and pyrazinamide in children and adolescents treated for tuberculous meningitis. Arch Dis Child 2022; 107: 70–77. doi: 10.1136/archdischild-2020-321426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schaaf HS, Parkin DP, Seifart HI, et al. . Isoniazid pharmacokinetics in children treated for respiratory tuberculosis. Arch Dis Child 2005; 90: 614–618. doi: 10.1136/adc.2004.052175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schaaf HS, Willemse M, Cilliers K, et al. . Rifampin pharmacokinetics in children, with and without human immunodeficiency virus infection, hospitalized for the management of severe forms of tuberculosis. BMC Med 2009; 7: 19. doi: 10.1186/1741-7015-7-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chabala C, Turkova A, Hesseling AC, et al. . Pharmacokinetics of first-line drugs in children with tuberculosis, using World Health Organization-recommended weight band doses and formulations. Clin Infect Dis 2022; 74: 1767–1775. doi: 10.1093/cid/ciab725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schipani A, Pertinez H, Mlota R, et al. . A simultaneous population pharmacokinetic analysis of rifampicin in Malawian adults and children. Br J Clin Pharmacol 2016; 81: 679–687. doi: 10.1111/bcp.12848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shah I, Jadhao N, Deshpande S, et al. . Pharmacokinetics of isoniazid in Indian children with tuberculosis on daily treatment. Int J Tuberc Lung Dis 2019; 23: 52–57. doi: 10.5588/ijtld.18.0463 [DOI] [PubMed] [Google Scholar]
- 41.Shah I, Kumar Das S, Shetty NS, et al. . Pharmacokinetics of isoniazid in children with tuberculosis – a comparative study at two doses. Pediatr Pulmonol 2020; 55: 660–665. doi: 10.1002/ppul.24624 [DOI] [PubMed] [Google Scholar]
- 42.Thee S, Seddon JA, Donald PR, et al. . Pharmacokinetics of isoniazid, rifampin, and pyrazinamide in children younger than two years of age with tuberculosis: evidence for implementation of revised World Health Organization recommendations. Antimicrob Agents Chemother 2011; 55: 5560–5567. doi: 10.1128/AAC.05429-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Van Aartsen D, Justine M, Mduma E, et al. . Enteropathogen spectrum and effect on antimycobacterial pharmacokinetics among children with tuberculosis in rural Tanzania: a prospective cohort study. Lancet Microbe 2022; 3: e408–e416. doi: 10.1016/S2666-5247(21)00308-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Verhagen LM, Lopez D, Hermans PWM, et al. . Pharmacokinetics of anti-tuberculosis drugs in Venezuelan children younger than 16 years of age: supportive evidence for the implementation of revised WHO dosing recommendations. Trop Med Int Health 2012; 17: 1449–1456. doi: 10.1111/tmi.12003 [DOI] [PubMed] [Google Scholar]
- 45.Zhu M, Starke JR, Burman WJ, et al. . Population pharmacokinetic modeling of pyrazinamide in children and adults with tuberculosis. Pharmacotherapy 2002; 22: 686–695. doi: 10.1592/phco.22.9.686.34067 [DOI] [PubMed] [Google Scholar]
- 46.Zhu M, Burman WJ, Starke JR, et al. . Pharmacokinetics of ethambutol in children and adults with tuberculosis. Int J Tuberc Lung Dis 2004; 8: 1360–1367. [PubMed] [Google Scholar]
- 47.Tikiso T, Mcilleron H, Abdelwahab MT, et al. . Population pharmacokinetics of ethambutol in African children: a pooled analysis. J Antimicrob Chemother 2022; 77: 1949–1959. doi: 10.1093/jac/dkac127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dayal R, Singh Y, Agarwal D, et al. . Pharmacokinetic study of isoniazid and pyrazinamide in children: impact of age and nutritional status. Arch Dis Child 2018; 103: 1150–1154. doi: 10.1136/archdischild-2017-313910 [DOI] [PubMed] [Google Scholar]
- 49.Denti P, Wasmann RE, van Rie A, et al. . Optimizing dosing and fixed-dose combinations of rifampicin, isoniazid, and pyrazinamide in pediatric patients with tuberculosis: a prospective population pharmacokinetic study. Clin Infect Dis 2022; 75: 141–151. doi: 10.1093/cid/ciab908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Graham SM, Bell DJ, Nyirongo S, et al. . Low levels of pyrazinamide and ethambutol in children with tuberculosis and impact of age, nutritional status, and human immunodeficiency virus infection. Antimicrob Agents Chemother 2006; 50: 407–413. doi: 10.1128/AAC.50.2.407-413.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gupta P, Roy V, Sethi GR, et al. . Pyrazinamide blood concentrations in children suffering from tuberculosis: a comparative study at two doses. Br J Clin Pharmacol 2008; 65: 423–427. doi: 10.1111/j.1365-2125.2007.03069.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ibrahim M, Engidawork E, Yimer G, et al. . Pharmacokinetics of isoniazid in Ethiopian children with tuberculosis in relation to the N-acetyltransferase 2 (NAT2) genotype. Afr J Pharm Pharmacol 2013; 7: 1124–1130. doi: 10.5897/AJPP2012.0040 [DOI] [Google Scholar]
- 53.Justine M, Yeconia A, Nicodemu I, et al. . Pharmacokinetics of first-line drugs among children with tuberculosis in rural Tanzania. J Pediatric Infect Dis Soc 2020; 9: 14–20. doi: 10.1093/jpids/piy106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.McIlleron H, Hundt H, Smythe W, et al. . Bioavailability of two licensed paediatric rifampicin suspensions: implications for quality control programmes. Int J Tuberc Lung Dis 2016; 20: 915–919. doi: 10.5588/ijtld.15.0833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Daskapan A, Idrus LR, Postma MJ, et al. . A systematic review on the effect of HIV infection on the pharmacokinetics of first-line tuberculosis drugs. Clin Pharmacokinet 2019; 58: 747–766. doi: 10.1007/s40262-018-0716-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Stott KE, Pertinez H, Sturkenboom MGG, et al. . Pharmacokinetics of rifampicin in adult TB patients and healthy volunteers: a systematic review and meta-analysis. J Antimicrob Chemother 2018; 73: 2305–2313. doi: 10.1093/jac/dky152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gafar F, van't Boveneind-Vrubleuskaya N, Akkerman OW, et al. . Nationwide analysis of treatment outcomes in children and adolescents routinely treated for tuberculosis in the Netherlands. Eur Respir J 2019; 54: 1901402. doi: 10.1183/13993003.01402-2019 [DOI] [PubMed] [Google Scholar]
- 58.Turkova A, Wills GH, Wobudeya E, et al. . Shorter treatment for nonsevere tuberculosis in African and Indian children. N Engl J Med 2022; 386: 911–922. doi: 10.1056/NEJMoa2104535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thee S, Roy RB, Blázquez-Gamero D, et al. . Treatment and outcome in children with tuberculous meningitis – a multi-centre Paediatric Tuberculosis Network European Trials Group study. Clin Infect Dis 2022; 75: 372–381. doi: 10.1093/cid/ciab982 [DOI] [PubMed] [Google Scholar]
- 60.Nataprawira HM, Gafar F, Risan NA, et al. . Treatment outcomes of childhood tuberculous meningitis in a real-world retrospective cohort, Bandung, Indonesia. Emerg Infect Dis 2022; 28: 660–671. doi: 10.3201/eid2803.212230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chiang SS, Khan FA, Milstein MB, et al. . Treatment outcomes of childhood tuberculous meningitis: a systematic review and meta-analysis. Lancet Infect Dis 2014; 14: 947–957. doi: 10.1016/S1473-3099(14)70852-7 [DOI] [PubMed] [Google Scholar]
- 62.Alffenaar JWC, Stocker SL, Forsman LD, et al. . Clinical standards for the dosing and management of TB drugs. Int J Tuberc Lung Dis 2022; 26: 483–499. doi: 10.5588/ijtld.22.0188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Denti P, Wasmann RE, Francis J, et al. . One dose does not fit all: revising the WHO paediatric dosing tool to include the non-linear effect of body size and maturation. Lancet Child Adolesc Health 2022; 6: 9–10. doi: 10.1016/S2352-4642(21)00302-3 [DOI] [PubMed] [Google Scholar]
- 64.Paradkar MS, Devaleenal DB, Mvalo T, et al. . Randomized clinical trial of high-dose rifampicin with or without levofloxacin versus standard of care for pediatric tuberculous meningitis: the TBM-KIDS trial. Clin Infect Dis 2022; 75: 1594–1601. doi: 10.1093/cid/ciac208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Donald PR, Maher D, Maritz JS, et al. . Ethambutol dosage for the treatment of children: literature review and recommendations. Int J Tuberc Lung Dis 2006; 10: 1318–1330. [PubMed] [Google Scholar]
- 66.Jacobs TG, Svensson EM, Musiime V, et al. . Pharmacokinetics of antiretroviral and tuberculosis drugs in children with HIV/TB co-infection: a systematic review. J Antimicrob Chemother 2020; 75: 3433–3457. doi: 10.1093/jac/dkaa328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gurumurthy P, Ramachandran G, Hemanth Kumar AK, et al. . Malabsorption of rifampin and isoniazid in HIV-infected patients with and without tuberculosis. Clin Infect Dis 2004; 38: 280–283. doi: 10.1086/380795 [DOI] [PubMed] [Google Scholar]
- 68.Alghamdi WA, Al-Shaer MH, Peloquin CA. Protein binding of first-line antituberculosis drugs. Antimicrob Agents Chemother 2018; 62: 00641-18. doi: 10.1128/AAC.00641-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Te Brake LHM, Ruslami R, Later-Nijland H, et al. . Exposure to total and protein-unbound rifampin is not affected by malnutrition in Indonesian tuberculosis patients. Antimicrob Agents Chemother 2015; 59: 3233–3239. doi: 10.1128/AAC.03485-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Oshikoya KA, Sammons HM, Choonara I. A systematic review of pharmacokinetics studies in children with protein-energy malnutrition. Eur J Clin Pharmacol 2010; 66: 1025–1035. doi: 10.1007/s00228-010-0851-0 [DOI] [PubMed] [Google Scholar]
- 71.Azuma J, Ohno M, Kubota R, et al. . NAT2 genotype guided regimen reduces isoniazid-induced liver injury and early treatment failure in the 6-month four-drug standard treatment of tuberculosis: a randomized controlled trial for pharmacogenetics-based therapy. Eur J Clin Pharmacol 2013; 69: 1091–1101. doi: 10.1007/s00228-012-1429-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Verma R, Patil S, Zhang N, et al. . A rapid pharmacogenomic assay to detect NAT2 polymorphisms and guide isoniazid dosing for tuberculosis treatment. Am J Respir Crit Care Med 2021; 204: 1317–1326. doi: 10.1164/rccm.202103-0564OC [DOI] [PubMed] [Google Scholar]
- 73.Weiner M, Peloquin C, Burman W, et al. . Effects of tuberculosis, race, and human gene SLCO1B1 polymorphisms on rifampin concentrations. Antimicrob Agents Chemother 2010; 54: 4192–4200. doi: 10.1128/AAC.00353-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dorman SE, Nahid P, Kurbatova EV, et al. . Four-month rifapentine regimens with or without moxifloxacin for tuberculosis. N Engl J Med 2021; 384: 1705–1718. doi: 10.1056/NEJMoa2033400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Imperial MZ, Nahid P, Phillips PPJ, et al. . A patient-level pooled analysis of treatment-shortening regimens for drug-susceptible pulmonary tuberculosis. Nat Med 2018; 24: 1708–1715. doi: 10.1038/s41591-018-0224-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kim HY, Byashalira KC, Heysell SK, et al. . Therapeutic drug monitoring of anti-infective drugs: implementation strategies for 3 different scenarios. Ther Drug Monit 2022; 44: 3–10. doi: 10.1097/FTD.0000000000000936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Litjens CHC, Aarnoutse RE, van Ewijk-Beneken Kolmer EWJ, et al. . Protein binding of rifampicin is not saturated when using high-dose rifampicin. J Antimicrob Chemother 2019; 74: 986–990. doi: 10.1093/jac/dky527 [DOI] [PubMed] [Google Scholar]
- 78.Snow KJ, Cruz AT, Seddon JA, et al. . Adolescent tuberculosis. Lancet Child Adolesc Health 2020; 4: 68–79. doi: 10.1016/S2352-4642(19)30337-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplementary material ERJ-01596-2022.Supplement (6MB, pdf)
This one-page PDF can be shared freely online.
Shareable PDF ERJ-01596-2022.Shareable (799.4KB, pdf)