A 50-year-old female presented to the outpatient department with a history of gradually progressive painless swelling over both upper eyelids for the past two and half years. The patient also had a history of dryness of the mouth and difficulty in swallowing food for the past four months. There was no history of pain or redness of eyes or oral mucosa, fever, weight loss, joint pains, cough, shortness of breath, drug intake, and diabetes mellitus. She had stable vitals and systemic examination was unremarkable. On local examination, it was found that there were swellings involving the lateral part of both upper eyelids over the area of lacrimal glands as shown in Figure 1. These swellings were 2 x 1 cm in size, firm, non-fluctuating, and non-tender. There was no enlargement of the parotid and submandibular glands. Because of suspicion of keratoconjunctivitis sicca, the Schirmer test was performed. It showed 4 mm moistened area in 5 minutes thus positive for dry eyes.[1] Fluorescein staining of the cornea was performed. The cornea was divided into the superior, central, and inferior areas. Each area was given a score of 0 (for no staining) to 3 (for continuous epithelial defect), the maximum score being 9. The right and left cornea had scores of 6 and 3, respectively.[2] The patient's HBsAg, anti-hepatitis C, and HIV antibody titers were normal. HbA1c, lipid, and thyroid profiles were unremarkable. Erythrocyte sedimentation rate and C-reactive protein were elevated suggestive of inflammatory etiology. Anti-nuclear antibodies (ANA), rheumatoid factor (RF), and anti-cyclic citrullinated peptides were negative. Autoimmune markers for Sjögren's syndrome anti-Ro (SS-A) and anti-La (SS-B) were negative. ANA was performed using an indirect immunofluorescence assay (IIF) and the rest of the autoimmune markers were measured using enzyme-linked immunosorbent assays (ELISA).
Figure 1.
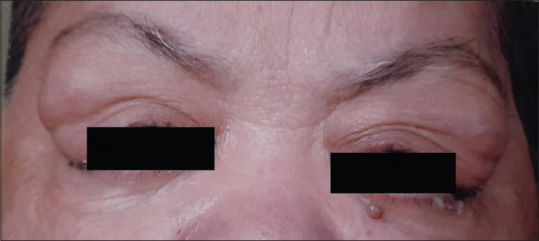
Bilateral lacrimal gland enlargement
As anti-Ro and anti-La antibodies turned out to be negative, the possibility of IgG4-related disorder was entertained and serum IgG4 levels were sent; which also turned out to be normal (less than 140 mg/dL). Computed tomography scan was suggestive of well-defined homogeneously enhancing symmetrical lesions in the superolateral aspect of bilateral orbits, likely of lacrimal gland origin, and the parotid glands were unremarkable. Biopsy was suggestive of highly cellular benign lymphoepithelial lesions involving the lacrimal gland as shown in Figure 2; there was no evidence of spindle-shaped fibroblasts of IgG4-positive plasma cells. Biopsy findings were strongly in favor of Sjögren's syndrome. The patient was started on prednisolone and artificial tears. She improved within a few weeks of follow-up.
Figure 2.
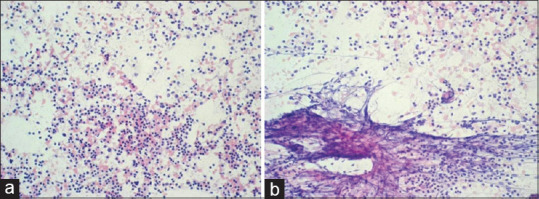
(a and b) FNAB of lacrimal gland showing large number of lympoepithelial cells with epitheloid cells suggestive of Sjögren's syndrome. (HE stain, magn. 200x)
Although keratoconjunctivitis sicca and xerostomia are common features of Sjögren's syndrome, the lacrimal gland enlargement is considered to be unusual. Causes of the lacrimal gland enlargement are broadly divided into two categories: neoplastic (epithelial/lymphoid tumors) and inflammatory (infectious/non-infectious). Infectious etiologies represent acute dacryoadenitis with painful, tender enlargement of glands, and erythema with discharge, which includes mainly viral and bacterial causes. Inflammatory non-infectious etiologies result in subacute to chronic painless enlargement of glands and these include orbital pseudotumor and Mikulicz's disease (as a part of IgG4-related disorder), sarcoidosis, and Sjögren's syndrome.[3,4] Mikulicz's disease is an IgG4-related disorder characterized by the combination of the bilateral lacrimal gland as well as parotid and submandibular gland enlargement. It has lymphoplasmacytic infiltration with IgG4 positive cells, storiform fibrosis, and obliterative phlebitis on biopsy, while sarcoidosis will have non-necrotizing granulomatous inflammation.[4] Autoimmune antibodies anti-Ro/La are present in 60-80% of primary Sjögren's syndrome cases.[3,4] Around 15% of cases of primary Sjögren's syndrome are seronegative for anti-Ro/La, ANA, and RF; these are diagnosed based on clinical features and lymphocytic infiltration on biopsy.[5] The present case had unusual characteristics in terms of lacrimal gland enlargement and negative autoimmune markers.
Declaration of patient consent
The authors certify that appropriate patient consent was obtained.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Stevens S. Schirmer's test. Community Eye Health. 2011;24:45. [PMC free article] [PubMed] [Google Scholar]
- 2.Usuba FS, de Medeiros-Ribeiro AC, Novaes P, Aikawa NE, Bonfiglioli K, Santo RM, et al. Dry eye in rheumatoid arthritis patients under TNF-inhibitors: Conjunctival goblet cell as an early ocular biomarker. Sci Rep. 2020;10:14054. doi: 10.1038/s41598-020-70944-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel R, Patel BC. Dacryoadenitis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535384/#_NBK535384_pubdet_ . [Google Scholar]
- 4.Baer AN. Diagnosis and classification of Sjögren's syndrome. In: UpToDate, Post, TW (Ed), UpToDate, Waltham, MA. 2022. Available from: https://www.uptodate.com/contents/diagnosis-and-classification-of-sjogrens-syndrome#H57368768 .
- 5.Yazisiz V, Aslan B, Erbasan F, Uçar İ, Öğüt TS, Terzioğlu ME. Clinical and serological characteristics of seronegative primary Sjögren's syndrome: A comparative study. Clin Rheumatol. 2021;40:221–9. doi: 10.1007/s10067-020-05154-9. [DOI] [PubMed] [Google Scholar]


