Objective:
We aimed to systematically review and quantify the association between acupuncture and pelvic floor muscle exercise and bladder dysfunction rehabilitation in individuals with spinal nerve injury.
Methods:
A meta-analysis was conducted using an evidence-based nursing analysis method based on clinical evidence. China National Knowledge Infrastructure, PubMed, VIP database, Wan Fang database, Cochrane Library, and other databases were searched by computer from January 1, 2000 to January 1, 2021. The literature was searched for clinical randomized controlled trials on acupuncture stimulation, pelvic floor muscle function training, and bladder function recovery training after spinal cord nerve injury. Two reviewers independently used The Cochrane Collaboration recommended randomized controlled trial risk of bias assessment tool to evaluate the quality of the literature. Then, the meta-analysis was performed using RevMan 5.3 software.
Results:
A total of 20 studies were included, with a total sample size of 1468 cases, including 734 patients in the control group and 734 patients in the experimental group. The results of our meta-analysis showed that acupuncture treatment [OR = 3.98, 95% CI (2.77, 5.72), Z = 7.49, P < .001] and pelvic floor muscle treatment [OR = 7.63, 95% CI (4.47, 13.04), Z = 7.45, P < .001] was statistically significant.
Conclusion:
Acupuncture and pelvic floor muscle exercise are effective intervention and treatment methods, which have obvious effects on rehabilitation treatment of bladder dysfunction after spinal nerve injury.
Keywords: acupuncture, bladder dysfunction, neurogenic bladder, pelvic floor muscles, spinal cord injury
1. Introduction
Bladder dysfunction (BD), also known as neurogenic bladder, is a common complication after spinal cord injury (SCI), mainly characterized by difficulty in urine storage, urination, or both.[1] Complications such as urinary tract infection, urinary calculi, hydronephrosis, and even renal failure are the main causes of death in patients with SCI in the middle and late stages.[2] This seriously endangers the health and quality of life of patients. Acupuncture, as a traditional Chinese medicine technique that can stimulate healthy qi and regulate oneself, plays a bidirectional, benign and holistic regulating effect of excitation and inhibition on central and peripheral nerve injury, so as to promote organ function recovery. In 1979, the World Health Organization drew up a list of 47 diseases that could be treated with acupuncture, including SCI and neurogenic bladder.[3] As a low-risk, noninvasive and interactive rehabilitation method, pelvic floor muscle training can effectively improve pelvic floor muscle tension, enhance patients’ ability to control urine and feces, and improve urinary retention and urinary incontinence.[4] Acupuncture and pelvic floor muscle training, as “green therapies,” have the advantages of quick efficacy, fewer side effects, and high safety.[5] Therefore, relevant studies have shown an upward trend in recent years. However, for a single study, the sample size observed is small and relevant evaluation indicators are scattered. This study aims to systematically evaluate and analyze multiple independent randomized clinical trials with the same research purpose through meta-analysis. This study hopes to further summarize and demonstrate the important role of acupuncture and pelvic floor muscle training in BD after SCI and explore whether they can achieve the purpose of clinical nursing: Avoid infection, reduce urinary retention, protect renal function and improve patients’ quality of life. Our aim is to provide a basis for clinical nursing of neurogenic bladder.
2. Methods
2.1. Data sources and search strategy
The Cochrane Library, PubMed, China National Knowledge Infrastructure, Wan Fang Data, VIP data and other databases were searched from January 1, 2000 to January 1, 2021 to find relevant studies on the effects of acupuncture and pelvic floor muscle training on BD after SCI. The Chinese and English search terms were SCI/neurogenic bladder/BD; Acupuncture/pelvic floor muscle.
2.2. Study selection and eligibility criteria
In brief, studies were eligible for inclusion if they: Study type: clinical controlled trial, randomized controlled trial; Subjects: patients with BD caused by SCI; Intervention measures: the experimental group was treated with acupuncture or pelvic floor muscle training combined with basic treatment, and the control group was treated with basic treatment.
2.2.1. Outcome indicators.
-
(i)
Total effective rate.
-
(ii)
Residual urine volume of bladder.
-
(iii)
Maximum bladder capacity.
-
(iv)
Bladder function score.
-
(v)
Urination times.
-
(vi)
Urodynamics.
-
(vii)
Daily urine leakage times.
-
(viii)
Urine output (max).
-
(ix)
TCM syndrome score.
-
(x)
Bladder pressure.
2.2.2. Exclusion criteria.
-
(i)
Comparison of different intervention schemes of the same intervention measure.
-
(ii)
The same study published by the same author.
-
(iii)
The number of study cases is <10, and the total number of cases is <30.
-
(iv)
The reported data are incomplete.
-
(v)
The outcome indicators are significantly different and cannot be combined with other data.
2.3. Study screening and data extraction
To set up the medical evidence-based clinical nursing technical team, the team members included: 1 head nurse of rehabilitation department as the team leader, 1 rehabilitation doctor as the deputy team leader, 2 graduate students and 1 undergraduate as the team members. The education requirements were a bachelor’s degree or above and proficient in professional knowledge related to medical evidence-based clinical nursing techniques.
In the evidence-based nursing group, 2 group members read the full text independently, and extracted the basic data in the study according to a unified format, such as the author, the total number of cases, the number of cases in the experimental group and the control group, the way of randomization, the balance between groups, curative effect, outcome indicators and so on, and sorted out the data in a list. In case of any disagreement during data extraction, it can be resolved through discussion or by the ruling of the third researcher.
2.4. Quality of evidence assessment
Two researchers independently and strictly followed the Cochrane systematic Review manual, used the criteria of clinical randomized controlled study bias evaluation, extracted the study objects, and protocols from the selected study, carried out rigorous quality assessment and bias risk assessment, and finally summarized the results. The main elements of the evaluation include randomness, whether the allocation plan is hidden, blinded, outcome, and comprehensive data collection, selective reporting of research results, and other potential benefit bias. If the selected study content met the evaluation criteria, the risk of bias of the study was small; If the risk of partial content bias was unclear and there were no high-risk items, the risk of study bias was moderate; If all the contents did not meet the evaluation criteria, the risk of bias was high. In case of disagreement, it was resolved through discussion or by the decision of the third researcher.
2.5. Data analysis
RevMan 5.3 software was used for statistical analysis of the included studies. χ2 test was used for heterogeneity analysis. Summary estimates were obtained with the random-effects-models if I2 statistics >50%. If I2 < 50%, and the fixed effects model was selected. Sensitivity analyses or subgroup analyses were performed using RevMan 5.3 software when necessary. In this study, the odds ratio data (or value) were selected to analyze the correlation strength between disease and exposure. At the same time, the 95% confidence interval was calculated, and the “forest map” was drawn by data and statistical software to describe the results. All tests carried out were 2 tailed taking the P value <0.05 as significant.
3. Results
3.1. Study retrieval results
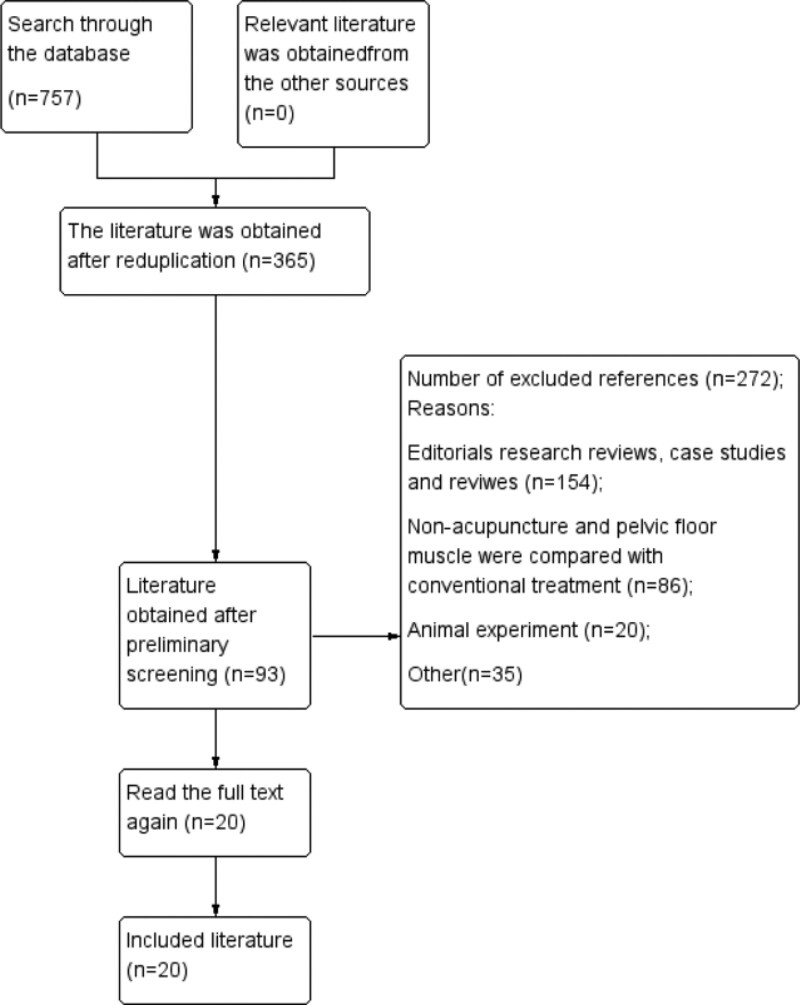
Of 757 citations retrieved by 2 reviewers based on the search strategy, 365 valid studies were obtained after reduplicating, 93 valid studies were reviewed in title and abstract, 73 studies were eliminated after detailed reading, and finally 20 qualified studies were selected for the study.[6–25] (Fig. 1). The selected studies were randomized and controlled. Among the included studies, 12 involved acupuncture therapy and treatment, and 8 involved pelvic floor muscle treatment.
Figure 1.
Flow chart of literature screening.
3.2. Basic information and study characteristics
A total of 20 relevant studies were included in the study, and all 20 studies reported the effective rate of acupuncture treatment and pelvic floor muscle treatment. A total of 1468 patients with BD caused by spinal cord nerve injury were included. The number of patients in the observation group was the same as that in the control group. The basic information of the study is shown in Table 1.
Table 1.
Characteristics of clinical trials included in current meta analysis.
| Study | Sample (cases) | Randomization | Balance between groups | Included in the index | Interventions | Period of treatment (wk) | Outcome indicators | ||
|---|---|---|---|---|---|---|---|---|---|
| T | C | T | C | ||||||
| Huang 2002[6] | 32 | 32 | Random | Good | Efficient | Acupuncture | Intramuscular injection of neostigmine methyl- sulfate | 4 | ① |
| Hu 2018[7] | 27 | 27 | Random | Good | Efficient | Rehabilitation nursing combined with acupuncture | Rehabilitation nursing | 8 | ①②③ |
| Gu 2005[8] | 32 | 32 | Random | Good | Efficient | Acupuncture at babao point combined with intermittent catheterization | Intermittent catheterization | 8 | ①② |
| Hou 2019[9] | 32 | 32 | Table of random number | Good | Efficient | Acupuncture at Dong Qi point combined with salt separated moxibustion at Shenque point | Intermittent catheterization | 4 | ①③④⑤ |
| Liu 2020[10] | 34 | 34 | Random | Good | Efficient | Rehabilitation training combined with acupuncture | Rehabilitation training | 8 | ①④⑥ |
| Hu 2015[11] | 30 | 30 | Table of random numbers | Good | Efficient | Routine acupuncture with bladder trigone intensive acupuncture | Routine acupuncture | 4 | ①②③⑦⑧ |
| Xie 2017[12] | 28 | 28 | Random | Good | Efficient | Routine bladder function training combined with acupuncture | Routine acupuncture | 4 | ①②④⑦⑧ |
| Luo 2020[13] | 30 | 30 | Table of random numbers | Good | Efficient | Intermittent catheterization combined with acupuncture | Intermittent catheterization | 4 | ①②④ |
| Yang 2020[14] | 38 | 37 | Random | Good | Efficient | Bladder function training combined with acupuncture | Bladder function training | 8 | ①②⑤⑩ |
| Cui 2016[15] | 43 | 43 | Table of random numbers | Good | Efficient | Rehabilitation nursing combined with acupuncture | Rehabilitation nursing | 8 | ①②③ |
| Chen 2017[16] | 80 | 80 | Random | Good | Efficient | Bladder function training combined with acupuncture | Bladder function training | 8 | ①⑤⑨⑩ |
| Qiao 2019[17] | 40 | 40 | Random | Good | Efficient | Rehabilitation training combined with acupuncture | Rehabilitation training | 2 | ①②⑤⑥⑨⑩ |
| Liu 2017[18] | 35 | 38 | Table of random numbers | Good | Efficient | Pelvic floor myoelectric stimulation | Bladder function training | 2 | ①③⑥ |
| Pan 2016[19] | 43 | 43 | Table of random numbers | Good | Efficient | Intermittent catheterization combined with pelvic floor myoelectric stimulation | Intermittent catheterization | 8 | ①②⑥ |
| Wang 2017[20] | 30 | 26 | Random | Good | Efficient | Pelvic floor muscle training combined with intermittent catheterization | Intermittent catheterization | 3 | ①②⑧ |
| Guan 2018[21] | 30 | 30 | Random | Good | Efficient | Pelvic floor muscle training combined with intermittent catheterization | Intermittent catheterization | 4 | ①⑥ |
| Li 2019[22] | 32 | 32 | Random | Good | Efficient | Intermittent catheterization combined with pelvic floor myoelectric stimulation | Intermittent catheterization | 4 | ①②③⑥ |
| Zhou 2020[23] | 42 | 42 | Random | Good | Efficient | Pelvic floor myoelectric stimulation combined with bladder function training | Bladder function training | 8 | ①②⑥ |
| Liu 2015[24] | 40 | 42 | Systematic sampling | Good | Efficient | Pelvic floor myoelectric stimulation combined with routine indwelling catheterization | Routine indwelling catheterization | 4 | ①②⑥ |
| Zhou 2015[25] | 36 | 36 | Random | Good | Efficient | Pelvic floor muscle training combined with routine rehabilitation | Rehabilitation training | 4 | ①② |
Note: T is the experimental group and C is the control group. Outcome indicators: ① total effective rate; ② residual urine volume of bladder (RUV); ③ maximum bladder capacity (MBC); ④ bladder function score; ⑤ urination times; ⑥ urodynamics; ⑦ daily urine leakage times; ⑧ urine output (max); ⑨ TCM syndrome score; ⑩ bladder pressure.
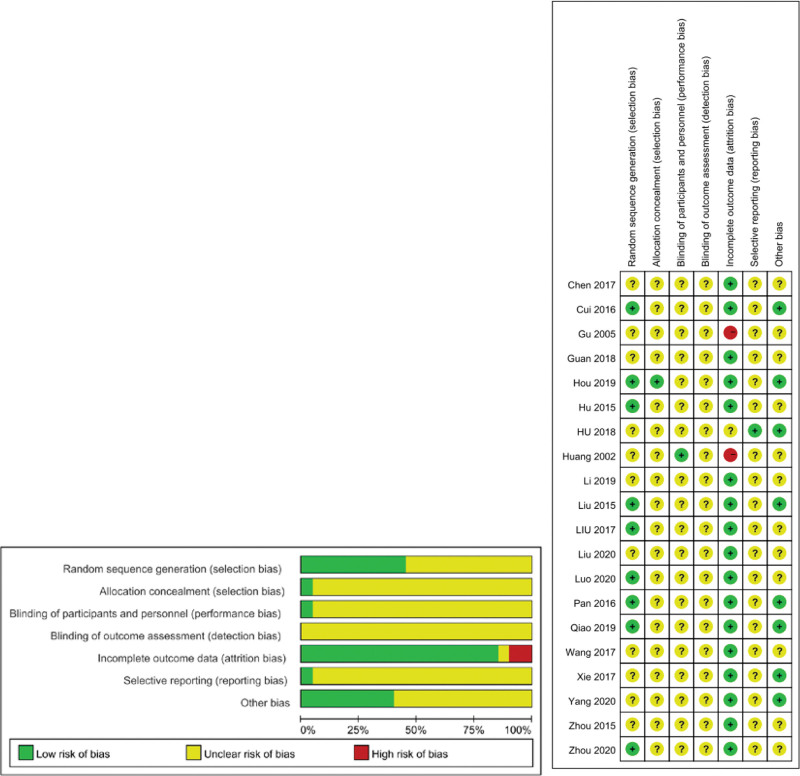
3.3. Bias risk of included studies
A total of 20 studies were included in this review, and all the research methods met the inclusion criteria. Among them, 13 did not report the specific method of random allocation, and only 1 of all the studies reported the relevant information hidden in allocation. There were 2 reports that did not report the initial experimental data, indicating incomplete data with high risk. See Figure 2.
Figure 2.
Summary of bias risk. “-” indicates that the possibility of bias is the highest, “?” indicates that the risk of bias is unclear, and “+” indicates that the possibility of bias is the lowest. Red represents high risk of bias, yellow represents unclear risk of bias, and green represents low risk of bias.
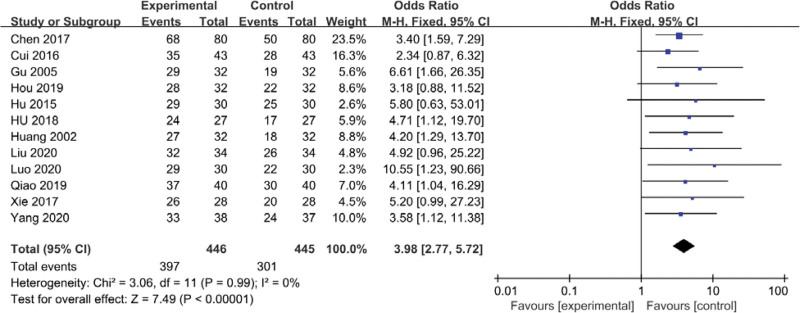
3.4. Analysis results of rehabilitation effect of acupuncture stimulation on patients with bladder function after SCI
Twelve studies on acupuncture treatment and BD caused by SCI (n = 891) were included to analyze whether acupuncture treatment is an effective intervention method for patients with BD after SCI. Heterogeneity test showed χ2 = 3.06, I2 = 0% (P < .001). The fixed effect model was selected according to chi-square test and odds ratio results. Sensitivity analysis showed that there was little difference before and after analysis, and the difference between the 2 groups was statistically significant. Odds ratio OR = 3.98, 95% confidence interval [2.77, 5.72], combined effect size Z = 7.49. Meta-analysis showed that acupuncture had a positive effect on rehabilitation of BD after SCI, as shown in Figure 3.
Figure 3.
Forest map of bladder dysfunction after spinal cord injury treated by acupuncture.
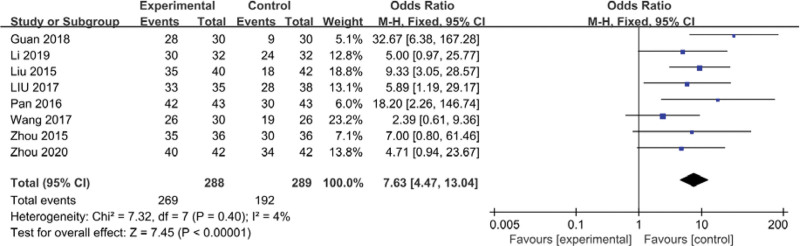
3.5. Analysis of rehabilitation effect of pelvic floor muscle therapy on patients with BD after SCI
Eight studies on pelvic floor muscle therapy and BD caused by SCI (N = 577) were included to analyze whether pelvic floor muscle therapy was an effective intervention for patients with BD after SCI. Heterogeneity test2 = 3.06, I2 = 4% (P < .001). The fixed effect model was selected according to the results of chi square test and odds ratio. Sensitivity analysis showed that there was little difference before and after this study, and the difference between the 2 groups was statistically significant. Odds ratio, OR = 7.63, 95% confidence interval [4.47, 13.04], combined effect Z = 7.45. Meta-analysis showed that pelvic floor muscle therapy had a positive effect on rehabilitation of BD after SCI, as shown in Figure 4.
Figure 4.
Forest plot of bladder dysfunction after pelvic floor muscle treatment of spinal cord injury.
4. Discussion
4.1. Analysis of the research results of acupuncture treatment on BD after SCI
Based on limited evidence, this analysis showed that the overall trend in the treatment of BD after SCI was significantly better in the experimental group than in the control group. BD after SCI, belongs to the categories of “uroschesisn” and “enuresis” in the discussion of traditional Chinese medicine. It emerged from Suwen xuan Ming Wu Qi, which revolves around the urological disease of bladder.[26] The lesion is located in the bladder. The upper part of the bladder is connected with the spleen and lung, and the middle part of the triple energizer is closely connected. If the bladder gasification is unbalanced, the kidney is evil, causing qi stagnation, blocked Qi and blood, and unable to camp Yin and Yang. The use of acupuncture in traditional Chinese medicine can dredge and close Qi, regulate bladder, benefit kidney and consolidate foundation, ameliorate patients’ lower urinary tract function and improve patients’ health quality.
Acupuncture is one of the oldest medical practices in traditional Chinese medicine. At present, acupuncture has been more and more widely used in China to treat neurogenic bladder after SCI, because it is a “green treatment plan” with fewer complications.[27] Acupuncture treatment still follows the traditional acupoint selection principle, which mainly combines remote acupoints with local acupoints, and the main acupuncture points such as bladder Shu, Yin ling quan, San yin jiao, and Zhong ji play a major role. Acupuncture at the above commonly used main points can help regulate the viscera, qi, blood, and body fluid, strengthen qi mechanism and dredge waterways, so as to achieve bladder vaporization and ultimately achieve the therapeutic purpose of bladder and urine self-passage.[28] Meanwhile, during the development and research process, the special way of acupuncture and moxibustion also shows its advanced nature. Like the matrix selection: The structure of acupuncture points, meridians and meridians distribution is 3-dimensional space, which accumulates the lesions in the 3-dimensional center, and implements targeted, efficient and reasonable treatment according to the matrix rules.[29]
In this study, 12 studies and 891 individual cases were included on the efficacy of acupuncture on BD after SCI. Through the key observation of the experimental group of cases, it was found that acupuncture at these points could strengthen the bladder muscle strength, promote the relaxation of the bladder detrusor muscle, and thus adjust the bladder muscles. In modern medical studies, acupuncture at these sympathetic acupoints can promote the metabolism of bladder damaged tissues, promote microcirculation, relieve local retention, reflexively regulate the spinal cord, and promote the recovery of spinal segmental control sensitivity, so as to restore urodynamics.[30] At the same time, it can also activate the excitability of cerebral cortex, promote the generation of metabolites of cerebral cortex, and promote the recovery of bladder function. This analysis showed that acupuncture treatment in the observation group had a strong advantage over conventional rehabilitation training. Acupuncture treatment of this kind of patients can stimulate internal self-repair and bladder function reconstruction, and achieve relatively normal urination function, which is a meaningful treatment plan for BD after SCI.
4.2. Analysis of research results on pelvic floor muscle therapy for neurogenic bladder after SCI
The analysis of this study shows that pelvic floor muscle therapy has significant advantages over conventional therapy in the treatment and rehabilitation of BD after SCI. Pelvic floor muscle is the main muscle group distributed around the lower urinary tract. SCI leads to the weakening or deficiency of pelvic floor muscle strength, which directly leads to the dysfunction of neurogenic organs. Therefore, the training and recovery of pelvic floor muscle can effectively improve BD.
Pelvic floor muscle training, also known as “Kegel exercise,” belongs to positive reinforcement behavior correction, which mobilizes and adjusts patients’ subjective initiative and constructs new healthy behaviors for patients.[31] This training conforms to the principle of “balancing the bladder” in the treatment of BD, which is to protect the balance of the upper urinary tract as the focus of treatment, and establish and maintain the treatment mode that does not damage or threaten the upper urinary tract. In recent years, pelvic floor muscle electrical stimulation has been widely used in the treatment of this disease due to its advantages of low cost and high efficiency.[32] Among them, biofeedback electrical stimulation makes patients intuitively feel the rhythmic contraction of pelvic floor muscle, which is a better pelvic floor muscle treatment in clinical application.[33]
In this study, 8 studies and 577 individual cases were included on the efficacy of pelvic floor muscle training for BD after SCI. The results of data calculation can fully prove that the therapeutic effect of pelvic floor muscle is significantly better than that of the control group. Patients with BD caused by SCI can directly take the pelvic floor muscle electrical stimulation treatment of the observation group clinically. As a noninvasive form, the pelvic floor muscle treatment of the observation group has low possibility of adverse events and high degree of cooperation of patients. Moreover, biofeedback electrical stimulation reduces the monotony and dryness of rehabilitation training and mobilizes the subjective initiative of patients. At present, pelvic floor muscle training is considered to be a very important and promising treatment method, which has a significant effect on the treatment of BD.[34]
5. Limitations
First, there are few studies on urinary control treatment for BD after SCI, and the medical research on this treatment is not extensive enough. Medical personnel need to make discoveries and innovations, and carry out large-sample, high-level, multi-center research experiments. Second, the scientific of guiding theory, the preciseness of clinical experiments and the standardization of operation methods still need to be improved. Third, only Chinese and English studies were retrieved, and other language studies were not involved, so the results may not be comprehensive.
6. Conclusion
Meta-analysis is a comprehensive analysis method that integrates similar independent research, improves the reliability of data results, and evaluates the results. Its advantage is to increase the efficiency of statistical test through accurate homogeneous data analysis, which can help similar studies find differences, summarize the reasons, get more scientific and effective results, and provide direction and support for clinical nursing.[35] As a common complication of SCI, BD has a great impact on physiology, psychology, and social survival. A series of complications such as urinary tract infection, urinary calculus, hydronephrosis, and even renal failure have become the main causes of patients’ late death.[36] This study shows that acupuncture and pelvic floor muscle training is an effective treatment for patients with BD after SCI, which is the same as the results of independent studies. These 2 treatments can improve patients’ bladder state and quality of life. They can be widely used in the clinical treatment of the disease. Meanwhile, it is hoped that acupuncture and pelvic floor muscle training can be combined for the treatment of BD after SCI in the next research process, so as to achieve the best treatment plan.
Author contributions
Formal analysis: Bai Mengjiao, Wang Lu.
Project administration: Li Li.
Resources: Zhang Meixia.
Writing – original draft: Zang Yuantong.
Abbreviations:
- BD
- bladder dysfunction
- SCI
- spinal cord injury
This meta-analysis was funded by Inner Mongolia Medical University Science and Technology Million Project (YKD2018KJBW(LH)050), and the Inner Mongolia Medical University “to the far” talent program project (ZY0301020).
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
The authors have no conflicts of interest to disclose.
This study has been reviewed by the hospital ethics committee.
How to cite this article: Zang Y, Bai M, Wang L, Zhang M, Li L. Effects of acupuncture and pelvic floor muscle training on bladder dysfunction after spinal cord injury: A meta-analysis. Medicine 2023;102:10(e33048).
References
- [1].Li LF, Leung GKT, Liu WM. Sacral nerve stimulation for neurogenic bladder. World Neurosurg. 2016;90:236–43. [DOI] [PubMed] [Google Scholar]
- [2].Li YY, Wang B, Liu Y, et al. System review and meta analysis of therapeutic effects of acupuncture on neurogenic bladder. World Chin Med. 2020;15:2076–84. [Google Scholar]
- [3].Lin QQ, Liu CM, Chen KW, et al. Review of acupuncture and moxibustion treatment of neurogenic bladder after spinal cord injury. J Fujian Univ Trad Chin Med. 2021;31:335–40. [Google Scholar]
- [4].Lawson S, Sacks A. Pelvic floor physical therapy and women’s health promotion. J Midwifery Womens Health. 2018;63:410–7. [DOI] [PubMed] [Google Scholar]
- [5].Zheng Y, Yang H, Yin X, et al. Acupoint injection combined with pelvic floor rehabilitation in the treatment of postpartum pelvic floor disorders: a protocol of randomized controlled trial. Medicine (Baltim). 2021;100:e25511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Huang ZG, You B. Acupuncture treatment on 32 cases of urinary retention after spinal cord injury. Shanhai Acupunct Moxibustion. 2002;21:31. [Google Scholar]
- [7].Hu ZJ, Zhang J, Chai Y, et al. Effect of acupuncture combined with rehabilitation nursing interventions on functional recovery of patients with neurogenic bladder after spinal cord injury. Nurs Int Trad Chin Western Med. 2018;4:67–9. [Google Scholar]
- [8].Gu XD, Fu JM, Yao YH. Clinical observation of electroacupuncture on eight-liao points in 64 bladder dysfunction patients with spinal cord injury. Clin Acupunct Moxibustion. 2005;21:47–8. [Google Scholar]
- [9].Hou Z, Luo KM, Qi TC, et al. Clinical observation on 32 cases of urinary retention after spinal cord injury treated with salt-separated moxibustion at Dong’s Qi and Shenque Point. Chin J Ethnomed Ethnopharm. 2019;28:95–8. [Google Scholar]
- [10].Liu WD. Clinical effect of rehabilitation training combined with acupuncture on neurogenic bladder patients with spinal cord injury. Reflexol Rehabil Med. 2020;29:33–4. [Google Scholar]
- [11].Hu QL, Zhao YC, Hu D, et al. Clinical observation of acupuncture at trigone of urinary bladder for urination dysfunction induced by spinal cord injury. Chin Acupunc Moxibustion. 2015;35:21–4. [PubMed] [Google Scholar]
- [12].Xie XL, Jing HL. Clinical study of acupuncture in treatment of bladder dysfunction after spinal cord injury. Cardiovasc Dis J Int Trad Chin Western Med (Electronic). 2017;5:163–4. [Google Scholar]
- [13].Luo J. Effect of acupuncture and intermittent catheterization on bladder function in patients with urinary retention after spinal cord injury. Chin For Med Res. 2020;18:130–2. [Google Scholar]
- [14].Yang Y, Xie N, Zhang JM. Observation on the effect of acupuncture combined with rehabilitation nursing to promote neurogenic bladder function recovery after spinal cord injury. J Sichuan Trad Chin Med. 2020;38:197–200. [Google Scholar]
- [15].Cui Y, Guo B. Acupuncture and moxibustion in combination with rehabilitation nursing to promote the effect of neurogenic bladder after spinal cord injury recovery. J Changchun Univ Chin Med. 2016;32:550–551554. [Google Scholar]
- [16].Chen YS, Kong XY, Jia JR. Clinical research of acupuncture for neurogenic bowel dysfunction due to spinal cord injury. J New Chin Med. 2017;49:148–50. [Google Scholar]
- [17].Qiao S, Zhang Z. Effect of acupuncture on neurogenic bladder after spinal cord injury. Mod J Int Trad Chin Western Med. 2019;28:1758–17601780. [Google Scholar]
- [18].Liu LL, Dai MH, Liu M, et al. Postoperative treatment of urinary dysfunction in patients with incomplete spinal cord injury: electrical pelvic floor stimulation versus bladder training therapy. Zhejiang Med J. 2017;39:273–6. [Google Scholar]
- [19].Pan SG, Lu H, Liu WP, et al. Influence of intermittent catheterization combined with pelvic floor muscle training on neurogenic bladder in patients with spinal cord injury. Chin Nurs Res. 2016;30:453–5. [Google Scholar]
- [20].Wang F. Effect of different training methods on urination function of patients with neurogenic bladder. J Chengde Med College. 2017;34:252–3. [Google Scholar]
- [21].Guan ZC, Mo HP, Yu XM, et al. Observation on efficacy of intermittent catheterization combined with pelvic floor muscle training for the treatment of neurogenic bladder after spinal cord injury. China Pract Med. 2018;13:20–1. [Google Scholar]
- [22].Li X. Effect of pelvic floor myoelectric biofeedback on urination dysfunction after spinal cord injury. Electr J Clin Med Liter. 2019;6:15–6. [Google Scholar]
- [23].Zhou HQ, Liu YY, Ying Y. Effect of pelvic floor muscle stimulation combined with bladder function training on bladder function recovery in patients with neurogenic bladder after spinal cord injury. China Mod Doctor. 2020;58:6–9. [Google Scholar]
- [24].Liu LL, Dong YL, Dai MH. Effect of pelvic floor myoelectric biofeedback on urination dysfunction after spinal cord injury. Chin J Phys Med Rehabil. 2015;37:209–11. [Google Scholar]
- [25].Zhou B, Wang W, Liu CX. Effect of pelvic floor muscle training on bladder dysfunction in patients with spinal cord injury. Med Forum. 2015;19:1168–70. [Google Scholar]
- [26].Wang XF, Wei D. Research situation of neurogenic bladder after acupuncture and moxibustion treatment of SCI. //2017 World Acupuncture and Moxibustion Academic Conference and 2017 Chinese Acupuncture and Moxibustion Society Annual Conference Proceedings. 2017:1–4. [Google Scholar]
- [27].Ifrim Chen F, Antochi AD, Barbilian AG. Acupuncture and the retrospect of its modern research. Rom J Morphol Embryol. 2019;60:411–8. [PubMed] [Google Scholar]
- [28].Zhu TL, Zhang HJ, Lou JL, et al. Clinical application of acupuncture in the treatment of neurogenic bladder. J Emerg Trad Chin Med. 2020;29:735–8. [Google Scholar]
- [29].Xu XM, Xu YL. Clinical efficacy on neurogenic bladder after spinal cord injury treated with rehabilitation training and acupuncture-moxibustion. Chin Acupunc Moxibustion. 2015;35:670–3. [PubMed] [Google Scholar]
- [30].Shen J, Wang WY, Que ZH, et al. Clinical study on acupuncture-moxibustion plus intermittent catheterization in treating neurogenic bladder after spinal cord injury. Shanghai J Acupunc Moxibustion. 2018;37:1187–90. [Google Scholar]
- [31].Huang YC, Chang KV. Kegel exercises. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. [PubMed] [Google Scholar]
- [32].Jha S, Walters SJ, Bortolami O, et al. Impact of pelvic floor muscle training on sexual function of women with urinary incontinence and a comparison of electrical stimulation versus standard treatment (IPSU trial): a randomised controlled trial. Physiotherapy. 2018;104:91–7. [DOI] [PubMed] [Google Scholar]
- [33].Jiang W, Zhang MS, Tan BT, et al. Effects of pelvic biofeedback electrical stimulation on neurogenic bladder in patients with spinal cord injury. J Third Milit Med Univ. 2014;36:1725–8. [Google Scholar]
- [34].Wallace SL, Miller LD, Mishra K. Pelvic floor physical therapy in the treatment of pelvic floor dysfunction in women. Curr Opin Obstet Gynecol. 2019;31:485–93. [DOI] [PubMed] [Google Scholar]
- [35].Lee YH. An overview of meta-analysis for clinicians. Korean J Intern Med. 2018;33:277–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Milligan J, Goetz LL, Kennelly MJ. A Primary care provider’s guide to management of neurogenic lower urinary tract dysfunction and urinary tract infection after spinal cord injury. Top Spinal Cord Inj Rehabil. 2020;26:108–15. [DOI] [PMC free article] [PubMed] [Google Scholar]