Abstract
Background
Several studies have shown that the impact of maternal mental health disorders on newborns’ well-being in low and middle-income countries (LMIC) are underreported, multi-dimensional and varies over time and differs from what is reported in high-income countries. We present the prevalence and risk factors associated with common mental disorders (CMDs) among breastfeeding mothers whose infants were admitted to Nigerian tertiary care facilities.
Methods
This was a national cross-sectional study involving mothers of hospitalised babies from eleven Nigerian tertiary hospitals. We used the WHO self-reporting Questionnaire 20 and an adapted WHO/UNICEF ten-step breastfeeding support package to assess mothers’ mental health and breastfeeding support.
Results
Only 895 of the 1,120 mothers recruited from eleven tertiary healthcare nurseries in six geopolitical zones of Nigeria had complete datasets for analysis. The participants’ mean age was 29.9 ± 6.2 years. One in four had CMDs; 24.0% (95% CI: 21.235, 26.937%). The ages of mothers, parity, gestational age at delivery, and length of hospital stay were comparable between mothers with and those without CMDs. Antenatal care at primary healthcare facilities (adjusted odds ratio [aOR:13], primary education [aOR:3.255] living in the south-southern region of the country [aOR 2.207], poor breastfeeding support [aOR:1.467], polygamous family settings [aOR:2.182], and a previous history of mental health disorders [aOR:4.684] were significantly associated with CMDs. In contrast, those from the middle and lower socioeconomic classes were less likely to develop CMDs, with [aOR:0.532] and [aOR:0.493], respectively.
Conclusion
In Nigeria, the prevalence of CMDs is relatively high among breastfeeding mothers with infants admitted to a tertiary care facility. Prior history of mental illness, polygamous households, mothers living in the southern region and low or no educational attainment have a greater risk of developing CMDs. This study provides evidence for assessing and tailoring interventions to CMDs among breastfeeding mothers in neonatal nurseries in LMIC.
Introduction
The World Health Organisation defines a mental disorder as a clinically substantial impairment in an individual’s cognitive, emotional control, or behaviour [1]. Common mental disorders (CMDs) include depression, generalised anxiety disorder, panic disorder, phobias, social anxiety disorder, obsessive-compulsive disorder, and posttraumatic stress disorder. The presence of CMD is linked to discomfort or impairment in key areas of function [1–4].
Recent years have seen an increase in the importance of mental health diseases, particularly CMD [5, 6]. In the global disease burden report, mental health disorders were included as one of the top 10 major causes of morbidity and mortality [6, 7]. The COVID-19 pandemic has been observed to exacerbate trends because of its influence on rising social isolation and other socioeconomic concerns [7–9]. According to a WHO report, approximately 1 billion people suffer from mental disorders, costing the global economy $2.5 billion per year. The global distribution of mental health disorders disproportionately affects low-middle income settings, which bear a greater burden [6, 10, 11] Unfortunately, the female gender, which appears to be more vulnerable in low-resource settings, is the most affected [6, 10, 11]. The perinatal period (pregnancy and postnatal) has a greater mental disease burden, with the highest incidence occurring in the immediate postpartum period of a woman’s life [7]. This becomes more concerning if the mother is faced with the additional task of caring for her newborn in a level 2–4 facility [10, 12–14].
A mother’s poor mental health can limit her ability to care for her child [10, 13, 14]. The consequences of a mother’s mental illness will affect her ability to support the family not only in terms of food supply but also in terms of acceptable and hygienic food provision, as well as her ability to use existing resources to meet a child’s nutritional needs [10, 13, 14] Common maternal mental health problems have been connected to 21–49% of childhood malnutrition and neonatal failure to thrive [13, 14]. Malnutrition results from poor mental health because it affects the child’s diet [14]. In addition, a mother needs to be mentally fit to produce adequate amounts of breastmilk, achieve appropriate positioning and attachment and establish effective bonding [15, 16]. Therefore, maternal mental illness often results in short- and long-term effects on growth and cognitive development [11].
It is worth noting that the relationship between a mother’s mental health and breastfeeding practice appears to be bidirectional [15, 16]. Breastfeeding has been documented as a stressor for some mothers who struggle with establishing adequate lactation or are asked to exclusively breastfeed their babies [17]. In a retrospective study, some mothers in remission from mental disorders reported a relapse as a result of the demand for exclusive breastfeeding [18]. In contrast, many prospective studies and pooled summary effects from meta-analyses show that adequate and well-supported breastfeeding is protective against mental illnesses with fewer relapses of mental breakdown in individuals with preexisting mental disorders [18].
Given the higher prevalence of mental disorders, it is critical to identify risk factors for CMD in nursing mothers [8, 9]. Identifying CMD risk factors in the context of a specific setting will allow for targeted evidence-based mental health promotion, especially in a country such as Nigeria, with a paucity of data on CMD among nursing mothers. Thus, we aimed to determine the prevalence of CMD and associated factors in mothers whose infants were admitted to Nigerian tertiary health nurseries.
Methods
Study design and settings
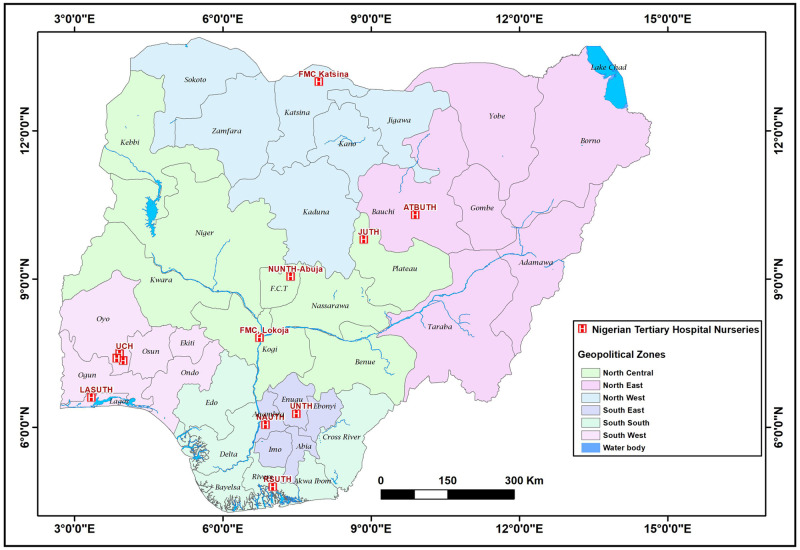
This study is part of a larger prospective, cross-sectional study conducted between May and August 2022 in twelve tertiary hospitals across Nigeria’s six geopolitical zones, including at least one hospital from each zone (Fig 1). In Nigeria, the nursery units of public tertiary hospitals have the highest bed capacity and staff strength, and they often account for the highest number of newborn hospitalizations in each state.
Fig 1. Map of Nigeria showing selected Nigerian tertiary hospital nurseries in the six geopolitical zones [UCH-University College Hospital, UITH- FMC-Katsina: Federal Medical Centre, Kastina, JUTH- Jos University Teaching Hospital, RSUTH-Rivers State University Teaching Hospital, ATBUTH-Abubakar Tafawa Balewa Teaching Hospital, Bauchi, UNTH-University of Nigeria Teaching Hospital, FMC-Lokoja; Federal Medical Centre, Lokoja, NUTH-Nile University Teaching Hospital Abuja; (formerly Asokoro District Hospital), LASUTH-, Lagos State University Teaching Hospital, NAUTH-Nnamdi Azikiwe University Teaching Hospital].
Study participants
This study included suitable mother-baby dyads whose infants were hospitalised in selected Nigerian tertiary hospitals. We excluded mothers who did not provide informed consent, mothers whose babies were only fed infant formula for medical reasons, mothers who were critically ill and needed hospitalisation, mothers whose babies were admitted for less than 24 hours, and babies with multiple congenital abnormalities, surgical abdomen, or any other contraindication for oral feeds.
Sample size determination
The minimum sample size required for this study was calculated using the ‘Raosoft software’ (http://www.raosoft.com/samplesize.html). Using a previously determined estimated 24.3% prevalence of common mental disorder among breastfeeding mothers at 95% confidence level, 3% (0.03) tolerable margin of error, and a 10% non-response rate, a sample size of 832 was obtained [19]. Due to the multisite nature of this study, the total sample size was divided by six to give a target of 80–140 mothers-dyad per geopolitical zone to the proportion of neonatal admissions.
Subjects’ enrolment and conduct of the research
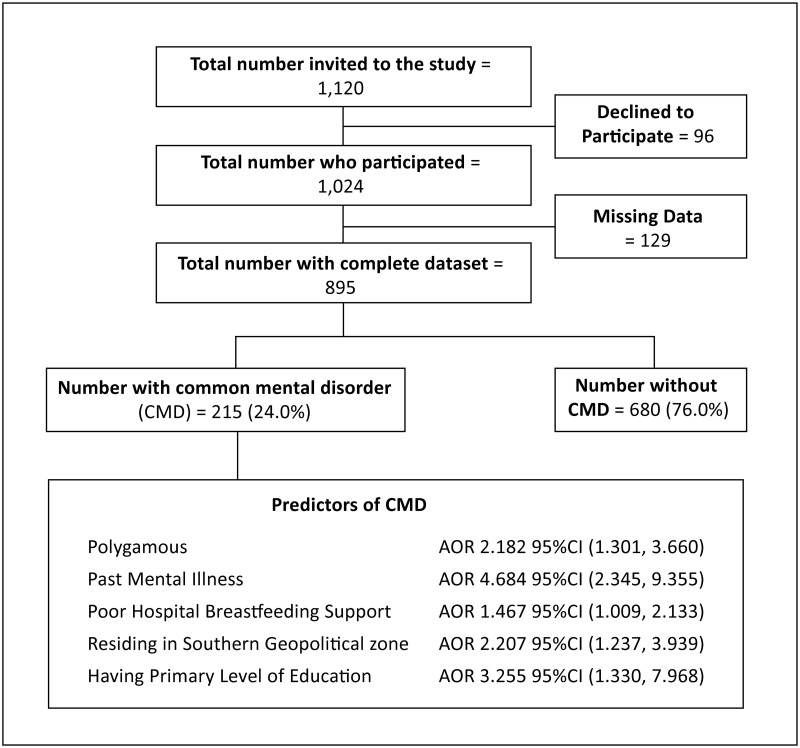
Eleven of 42 hospitals were selected as study sites utilising a multistage sample technique and GraphPad Prism 9 (GraphPad Software, 2365 Northside Dr Suite San Diego, CA 92108), (Fig 1.) Map of Nigeria showing selected Nigerian tertiary hospital nurseries in the six geopolitical zones; [UCH-University College Hospital, JUTH- Jos University Teaching Hospital, RSUTH-Rivers State University Teaching Hospital, FMC-Katsina: Federal Medical Centre, Kastina. ATBUTH-Abubakar Tafawa Balewa Teaching Hospital, Bauchi, UNTH-University of Nigeria Teaching Hospital, FMC-Lokoja; Federal Medical Centre, Lokoja, NUTH-Nile University Teaching Hospital Abuja; (formerly Asokoro District Hospital), LASUTH-, Lagos State University Teaching Hospital, NAUTH-Nnamdi Azikiwe University Teaching Hospital]. (Fig 2. Participants flow chart study on common mental disorders among breastfeeding mothers in Nigerian tertiary hospital nurseries).
Fig 2. Participants flow chart study on common mental disorders among breastfeeding mothers in Nigerian tertiary hospital nurseries (The flow chart describes the participants’ enrollment and the predictors of common mental disorders among breastfeeding mothers whose babies were admitted to tertiary nurseries).
Using stratified lists of hospitals per geopolitical zone, we selected one tertiary health centre per zone, for a total of six, using simple random sampling. In the second stage, we utilised a simple random procedure to select five additional tertiary health institutions from the pooled lists of tertiary health facilities across the country, bringing the total number of research sites to eleven. Using the approach of convenience sampling, study participants at each site were selected by picking all eligible consecutive admissions. At each study site, the co-investigator or a trained research assistant administered the Google Form to pairs of eligible mothers and infants in person. However, one of the centres in Northwestern Nigeria was inactive and was therefore excluded from the final data analysis. An inactive centre in Northwestern Nigeria was however, excluded from the data analysis.
Study tools
The self-reporting questionnaire (SRQ)-20 of the World Health Organization (WHO) was used to evaluate maternal mental health. It is a 20-item questionnaire that inquires about depressive, anxious, panic, and somatic symptoms in the four weeks prior. Each of the twenty items received a score of 1 or 0 to indicate the presence or absence of symptoms. The measure ranged from 0 to 20, with higher scores indicating poor mental health and lower values indicating good mental health [20]. As suggested by many studies, a cut-off of 7 was used to classify women as having common mental disorders (CMD)’ or no CMD [3, 20–22]. The scale was administered in English. Collaborating investigators from the geopolitical zone translated the questionnaire into the major local dialects, face-validated it, and requested that it be reviewed by Psychometricians in regions with low levels of illiteracy. This instrument’s reliability and validity are well established, and it has been used in local studies in Nigeria [11].
Other components of the questionnaire
The other components of the questionnaire included sociodemographic information, antenatal care, and questions about breastfeeding support. (hospital and family). The questions on breastfeeding support were derived following proper appraisal of relevant literature, WHO and UNICEF packages on successful breastfeeding [23]. Experts and members of the research team evaluated the derived breastfeeding questions and made additional modifications. Before the study commenced, we pilot-tested and validated the questionnaire with 90 mothers-dyads in one of the tertiary nurseries in southwestern Nigeria. The mother-baby pairs who took part in the pilot study were excluded from the final study. The pilot testing feedback was incorporated into the study’s final questionnaire. The details in the questionnaire can be accessed using the link: https://forms.gle/BJmWKdjkzDdt47oXA.
Data management and analysis
The data were collected via Google form, extracted and exported into the Statistical Package for Social Sciences (S.P.S. S) version 23 for analysis. Sociodemographic factors, parity, and details of ANC, including gestational age at delivery, are summarised in the frequency table. Using a cut-off of 7, the SR1-20 was used to classify the mothers into CMDs and no CMDs groups. The mean score of the response was used to classify breastfeeding support as good (values corresponding to a mean score of 11.5 ± 5.2 and above) or poor (values below the mean score of 6.3). Pearson’s chi-squared test was used to examine associations between CMD and sociodemographics, gestational age at delivery, parity, baby’s duration on admission, and breastfeeding support while Fischer’s exact test was used to test for association between CMDs and antenatal factors (ANC attendance and place). For the Oyedeji social class, the education and occupation/business engagement of both parents were stratified into five categories. Parental occupations range from unemployed to senior public servants, professionals, managers, large-scale traders, businessmen, and contractors, while educational attainment ranges from no formal education to a graduate degree. The mean score of both parents at each stratum was estimated to the nearest integer, and a score was assigned. Furthermore, the five grades are reclassified into three social classes (upper: social classes I & II, middle: social classes III, and low: classes IV & V) [24]. We defined a monogamous family as a mother in an exclusive conjugal relationship with her partner, as do single mothers’ perceptions of being in an exclusive relationship with her partner before separation.
A mother is considered to have a polygamous marital status if she is in a relationship with a man who has or is having concurrent conjugal relationships with other women. Multivariable analysis was used to determine and report the adjusted odds ratio (AOR) with a 95% confidence interval for predictor variables that were statistically associated with CMDs on bivariable analysis. The predictor variables include geopolitical zones, educational level, location of ANC, marital status, family settings, and past mental illness. The significance level was set at p < 0.05.
Ethical considerations
The National Health Research Ethics Committee of Nigeria granted ethical permission (NHREC/01/01/2007-31/03/2022) (NHREC) for the study. This study was conducted in accordance with the Helsinki Declaration. Before enrollment, voluntary participation was required of invited study participants. The details of the study were explained to the respondents, who were then asked to describe the study, and their comprehension was assessed. The respondent then voluntarily provided electronic consent by selecting yes to continue the questionnaire or no to decline participation. The data was redacted and password-protected to ensure privacy. Mothers found to have common mental disorders were referred to a psychiatrist and/or a psychologist for intervention.
Results
Of the 1,120 mothers-dyads recruited for the study, at the tertiary healthcare nurseries in the six geopolitical zones in Nigeria, 895 (79.9%) had a complete dataset for analysis. Fig 2 shows the flow diagram of the study participant. The mean age of the study participants was 29.9 ± 6.2 years, and 76.2% of them were between the ages of 25 and 40. The majority of the mothers 835 (93.3%) received antenatal care, and approximately half were para 2 to 4 (48.5%). Nearly two-thirds (547, 61.1%) of the infants were born at term. Even though only 9.8% of participants lacked formal education, more than half, 490 (54.7%) belonged to a lower socioeconomic class. The socio-demographic data in Table 1 provide the details.
Table 1. General characteristics of the study population.
| Variables | Subcategory | Frequency | Percent |
|---|---|---|---|
| n = 895 | |||
| Age group (years) | 15–20 | 69 | 7.7 |
| >21–<34 | 597 | 66.7 | |
| ≥35 | 229 | 25.6 | |
| Parity | 1 | 339 | 37.9 |
| 2–4 | 434 | 48.5 | |
| ≥5 | 122 | 13.6 | |
| ANC | No | 60 | 6.7 |
| Yes | 835 | 93.3 | |
| Place of ANC | Maternity home | 14 | 1.7 |
| Private hospital | 44 | 5.3 | |
| Primary health facility | 267 | 32.0 | |
| Secondary health facility | 221 | 26.5 | |
| Tertiary health facility | 289 | 34.5 | |
| Gestational age at delivery | |||
| Preterm | 304 | 34.0 | |
| Term | 591 | 66.0 | |
| Baby’s duration on admission (days) | 1–3 | 208 | 23.2 |
| 4–7 | 386 | 43.1 | |
| >7 | 301 | 33.6 | |
| Educational level | No formal education | 88 | 9.8 |
| Primary | 44 | 4.9 | |
| Secondary | 314 | 35.1 | |
| Tertiary | 449 | 50.2 | |
| SEC | Upper | 127 | 14.2 |
| Middle | 278 | 31.1 | |
| Lower | 490 | 54.7 | |
| Geopolitical zones | North-west | 124 | 13.9 |
| North-east | 75 | 8.4 | |
| North-central | 281 | 31.4 | |
| South-east | 93 | 10.4 | |
| South-south | 103 | 11.5 | |
| South-west | 219 | 24.5 | |
| Marital status | Married | 854 | 95.4 |
| Single | 41 | 4.6 | |
| Family settings | Monogamous | 779 | 87.0 |
| Polygamous | 116 | 13.0 |
ANC-antenatal clinic attendance, SEC-Socioeconomic class Mean age 29.9 ± 6.2
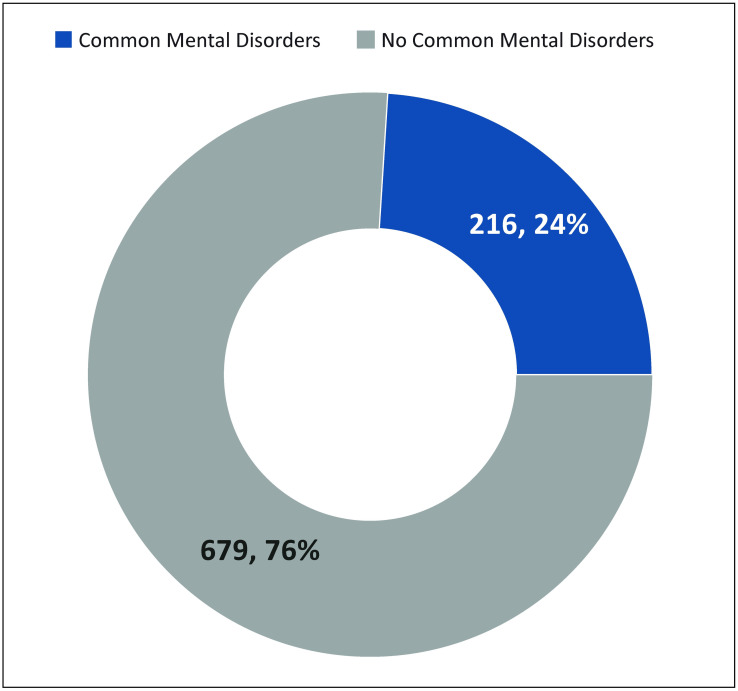
Common mental disorders were present in one in four; 24.0% (95% CI: 21.235, 26.937%) of breastfeeding mothers in tertiary hospital nurseries (Fig 3. Prevalence of Common Mental Disorders (CMDs)).
Fig 3. Prevalence of common mental disorders.
Overall, less than half (427; 47.7%) of the mother received optimal breastfeeding support in the hospital. Only 198 (22.1%) breastfeeding mothers received family support for breastfeeding while nursing babies in the hospital nursery. Of the 895 respondents, 41 (4.6%) disclosed having been diagnosed with mental health disorders.
The ages of mothers with CMDs and mothers without CMDs were comparable. Similarly, parity, gestational age at delivery, length of hospital stay, socioeconomic status, hospital breastfeeding support, and family support were comparable between the two groups (Table 2). In contrast, there were significant differences in the place of antenatal care attendance, educational levels, geopolitical zones within the country, marital status, family settings, and background history of mental disorders between mothers with CMD and those without CMD. (Table 2).
Table 2. Factors associated with common mental disorders (CMDs).
| Variables | Subcategory | CMDs | No CMDs | χ2 | P |
|---|---|---|---|---|---|
| n = 895 | n = 216 | n = 679 | |||
| Age group | 15–20 (69) | 17(24.6) | 52(75.4) | 0.056 | 0.967 |
| >20–<35 (597) | 145(24.3) | 452(75.7) | |||
| ≥35(229) | 54(23.6) | 175(76.4) | |||
| Parity | 1 (339) | 77 (22.7) | 262 (77.3) | 0.615 | 0.735 |
| 2–4 (434) | 109 (25.1) | 325 (74.9) | |||
| >4 (122) | 30 (24.6) | 92 (75.4) | |||
| ANC | None (60) | 20 (33.3) | 40 (66.7) | 22.225f | <0.001 |
| Maternity home (14) | 5 (35.7) | 9 (64.3) | |||
| Private hospital (44) | 12 (27.3) | 32 (72.7) | |||
| Primary (267) | 79 (29.6) | 188 (70.4) | |||
| Secondary (221) | 57 (25.8) | 164 (74.2) | |||
| Tertiary (289) | 43 (14.9) | 246 (85.1) | |||
| Gestational age | Preterm (304) | 226(74.3) | 78(25.7) | 0.586 | 0.459 |
| Term (591) | 453(76.6) | 138(23.4) | |||
| Baby’s admission duration | < 3 (208) | 61 (29.30 | 147 (70.7) | 4.029 | 0.133 |
| 3–7 (386) | 86 (22.3) | 300 (77.7) | |||
| >7 (301) | 69 (22.9) | 232 (77.1) | |||
| Educational level | No formal education (88) | 18 (20.5) | 70 (79.5) | 13.618 | 0.003 |
| Primary (44) | 20 (45.50 | 24 (54.5) | |||
| Secondary (314) | 81 (25.8) | 233 (74.2) | |||
| Tertiary (449) | 97 (21.6) | 352 (78.4) | |||
| Socioeconomic class | Upper (127) | 37 (29.1) | 90 (70.90 | 3.891 | 0.143 |
| Middle (278) | 57 (20.5) | 221 (79.5) | |||
| Lower (490) | 122 (24.9( | 368 (75.1) | |||
| Geopolitical zones | Northwest (124) | 18 (14.5) | 106 (85.5) | 17.840 | 0.003 |
| Northeast (75) | 21 (28.0) | 54 (72.0) | |||
| Northcentral (281) | 62 (22.1) | 219 (77.9) | |||
| Southeast (93) | 30 (32.3) | 63 (67.7) | |||
| Southsouth (103) | 36 (35.0) | 67 (65.0) | |||
| Southwest (219) | 49 (22.4) | 170 (77.6) | |||
| Marital status | Married (854) | 198 (23.2) | 656 (76.8) | 9.171 | 0.002 |
| Single parent (41) | 18 (43.9) | 23 (56.1) | |||
| Family settings | Monogamous (779) | 178 (22.8) | 601 (77.2) | 5.414 | 0.020 |
| Polygamous (116) | 38 (32.8) | 78 (67.2) | |||
| Hospital Breastfeeding support | Poor (435) | 112 (25.7) | 323 (74.3) | 1.203 | 0.273 |
| Good (460) | 104 (22.6) | 356 (77.4) | |||
| Family Breastfeeding support | Yes (198) | 55 (27.8) | 143 (72.20 | 1.844 | 0.175 |
| No (697) | 161 (23.1) | 536 (76.9) | |||
| Past Mental illness | Yes (41) | 24 (58.5) | 17 (41.5) | 27.775 | <0.0001 |
| No (854) | 192 (22.5) | 662 (77.5) |
ANC-antenatal care; f Fischer’s exact test
In the multivariable analysis, factors that were significantly associated with CMDs included the place of ANC attendance, with primary healthcare facilities having up to 13 times the odds for CMDS. The primary level of education (adjusted odds ratio [aOR] 3.255, 95% CI 1.330, 7.968), living in the south-southern region of the country [aOR 2.207, 95% CI: 1.237, 3.939], poor breastfeeding support [aOR 1.467, 95% CI 1.009, 2.133], polygamous family settings [aOR 2.182, 95% CI 1.301, 3.660], and a previous history of mental health disorders [aOR 4.684, 95% CI 1.301, 9.355]. In contrast, those from the middle and lower socioeconomic classes were less likely to develop CMDs, with [aOR 0.532] and [aOR 0.493] respectively (Table 3).
Table 3. Multivariable logistic regression of factors associated with CMDs.
| Variables | CMDs | OR | 95% CI | Adjusted OR | 95% CI | P |
|---|---|---|---|---|---|---|
| n = 216 | ||||||
| Place of ANC | ||||||
| Tertiary | 43 (19.9) | 1 | ||||
| Secondary | 57 (26.4) | 1.988 | 1.277, 3.095 | 4.664 | 2.200, 9.888 | <0.001 |
| Primary | 79 (36.6) | 2.404 | 1.584, 3.648 | 3.749 | 1.094, 12.848 | 0.035 |
| Private hospital | 12 (5.6) | 2.145 | 1.025, 4.489 | 2.372 | 1.061, 5.306 | 0.035 |
| Maternity home | 5 (2.3) | 3.178 | 1.016, 9.940 | 2.627 | 1.602, 4.306 | 0.001 |
| None | 20 (9.2) | 2.860 | 1.528. 5.354 | 2.201 | 1.364, 3.533 | 0.001 |
| Baby’s duration on admission (days) | ||||||
| < 3 | 61 (28.2) | 1 | ||||
| 3–7 | 86 (39.8) | 0.691 | 0.471, 1.013 | 0.776 | 0.501, 1.202 | 0.256 |
| >7 | 69 (32.0) | 0.717 | 0.480, 1.071 | 0.754 | 0.479, 1.187 | 0.223 |
| Educational level | ||||||
| No formal edu. | 18 (8.3) | 1 | ||||
| Primary | 20 (9.3) | 3.241 | 1.474, 7.124 | 3.255 | 1.330, 7.968 | 0.010 |
| Secondary | 81 (37.5) | 1.352 | 0.760, 2.406 | 1.538 | 0.743, 3.183 | 0.246 |
| Tertiary | 97 (44.9) | 1.072 | 0.609, 1.885 | 1.358 | 0.621, 2.970 | 0.443 |
| SEC | ||||||
| Upper | 37 (17.1) | 1 | ||||
| Middle | 57 (26.4) | 0.627 | 0.388, 1.015 | 0.532 | 0.316, 0.896 | 0.018 |
| Lower | 122 (56.5) | 0.806 | 0.522, 1.245 | 0.493 | 0.286, 0.849 | 0.011 |
| Geopolitical zones | ||||||
| Northcentral | 62 (28.7) | 1 | ||||
| Northeast | 21 (9.7) | 1.374 | 0.771, 2.447 | 0.972 | 0.493, 1.915 | 0.934 |
| Northwest | 18 (8.3) | 0.600 | 0.338, 1.065 | 0.497 | 0.257, 0.960 | 0.037 |
| Southeast | 30 (13.9) | 1.682 | 1.002, 2.824 | 1.372 | 0.760, 2.475 | 0.494 |
| Southsouth | 36 (16.7) | 1.898 | 1.159, 3.109 | 2.207 | 1.237, 3.939 | 0.007 |
| Southwest | 49 (22.7) | 1.018 | 0.666, 1.557 | 0.777 | 0.483, 1.249 | 0.297 |
| Hosp BF sup. | ||||||
| Good | 104 (48.1) | 1 | ||||
| Poor | 112 (51.9) | 1.187 | 0.874, 1.613 | 1.467 | 1.009, 2.133 | 0.045 |
| Marital status | ||||||
| Married | 198 (91.7) | 1 | ||||
| Single | 18 (8.3) | 2.593 | 1.371, 4.902 | 1.979 | 0.986, 3.971 | 0.055 |
| Family settings | ||||||
| Monogamous | 178 (82.4) | 1 | ||||
| Polygamous | 38 (17.6) | 1.645 | 1.078, 2.509 | 2.182 | 1.301, 3.660 | 0.003 |
| Family BF sup | ||||||
| No | 161 (74.5) | 1 | ||||
| Yes | 55 (25.5) | 1.280 | 0.896, 1.831 | 1.189 | 0.787, 1.796 | 0.412 |
| Past Mental illness | ||||||
| No | 192 (88.9) | 1 | 1 | |||
| Yes | 24 (11.1) | 4.868 | 2.562, 9.248 | 4.684 | 2.345, 9.355 | <0.001 |
CMDs-common mental disorders; OR-odds ratio; CI-Confidence intervals; ANC-Antenatal care; edu-education; SEC-socioeconomic class; BF sup-breastfeeding support
Discussion
Common mental disorders refer to a range of nonpsychotic mental health conditions, such as anxiety, depression and somatoform disorders. In this study, the prevalence of CMDs among breastfeeding mothers in tertiary hospital nurseries in Nigeria was 24%. This demonstrates that one in four of the women in this study had CMDs. The additional strain of having a child in the nursery may be the cause of this. Furthermore, several studies have suggested that the challenges of nursing may increase the frequency and/or severity of maternal psychological disorders [25, 26].
The prevalence of CMDs in the mothers in this study is low when compared to the prevalence of CMDs among other categories of mothers in other studies. Among pregnant women, a higher prevalence range of 35.8% to 39.5% has been documented [27–31], while the documented range among mothers of children under the age of five years was 36.6% to 46.2% [32–34]. The low prevalence of CMDs among BF mothers may be due to the wide range of psychological benefits of breastfeeding to the mother. It has been documented that the act of breastfeeding promotes hormonal processes that induce the release of oxytocin, an important hormone related to maternal bonding, and attenuates the cortisol response to stress, which when consistently high, is one of the strongest risk factors for the development of psychiatric disorders [35]. Moreover, breastfeeding supports the regulation of sleep and wake patterns for both mother and infant and sustains and improves maternal self-efficacy. Consequently, breastfeeding mothers are more likely to report positive mood, less anxiety, and increased calm compared to formula-feeding mothers [36, 37]. Furthermore, Yeun et al., [38] in a systematic review of 36 studies, concluded that breastfeeding was associated with improved maternal mental health outcomes.
Previous studies on maternal mental health in Nigeria and other low-income countries found a much lower prevalence [39–41]. This disparity may be due to differences in the morbidity spectrum targeted, as well as differences in the sensitivity of measuring instruments and their cut-off points for mental health disorders [41]. This disparity may also be explained by differences in the timing of assessments during pregnancy and postpartum. It was also suggested that lower CMDs observed among childbearing women in high-income countries could be attributed to better maternal support during pregnancy and the immediate postnatal period than women in low-income countries [41].
Regarding the associated factors, place of ANC, level of education, place of abode, poor breastfeeding support, polygamous family setting and history of mental illness were significantly associated with CMDs. Mothers who attended ANC in PHCs were 13 times more likely to develop CMDs than those who received ANC in other facilities. This could be traceable to the quality of care received and the level of competence of the health workers in PHC. According to Ntoimo et al., [42]. pregnant women were hesitant to attend ANC in PHC due to the mothers’ palpable stress caused by a poor road network, difficulty with transportation, long distances, and random facility openings. The use of abusive care by healthcare professionals, the severe shortage of healthcare professionals in these facilities, the lengthy wait times, and the discouragement of partner support are other reasons to mention a few [42]. These possible stressors could predispose pregnant women attending ANC in this facility to CMD. Attending antenatal clinics has also been linked to an increased understanding of pregnancy complications, including mental diseases, as well as increased chances of learning about pregnancy readiness and reducing risk factors [43, 44]. This highlights the need for the government and private individuals to restructure PHC with qualified personnel and improved infrastructure, as well as a shift in the attitudes of health workers toward pregnant women. In contrast, pregnant women at high risk of CMDs should make a secondary health facility their first point of contact. Women with poor or no educational attainment are susceptible to CMDs [14, 34]. In the current study, mothers with primary education were three times more likely to have CMDs. Therefore, the educational level has a major impact on maternal mental health as higher education was found to be protective against maternal mental disorders [41, 45]. According to this study, mothers who dwell in the south of the country are twice more likely to exhibit CMD symptoms than mothers who live in the north. The reason for the regional variation in CMDs in the present study is unclear and may necessitate further research. However, published literature suggests that the variation may be due to differences in obstetric care [41]. Regions with a low tolerance for mother-baby separation and early, close relative access to the mother after birth will have better coping with perinatal stress and, as a result, a lower prevalence of CMDs [46]. In addition, the disparity may be attributed to variations in neonatal intensive care settings. In settings where family members have limited access to mother-baby dyads, the enormous benefits of family-centred care including mental health support from several reports are undermined [41, 47, 48]. Again, the importance of regional sociocultural differences in influencing mothers’ mental health cannot be overstated. In a special WHO report on maternal mental health in low- and middle-income countries, sociocultural factors such as breastfeeding not being fashionable and, for cosmetic preservation of breast shape, the class perception of the feeding bottle, all of which may deprive the mother of the mood-enhancing effect of breastfeeding, are cited as risk factors for CMDs [41]. In addition, the cultural perception of a mother’s breastfeeding difficulties as a sign of weakness by family members increases the mother’s stress level and predisposes her to mental disorder.
Polygamous household settings were two times more likely to have CMDs in the current study similar to finding in northern Nigeria by Imam et al., [49] and A WHO report on CMDs in LMIC [41]. This might be because polygamy comes with additional pressures. In contrast, Abdullahi et al., [11] found no evidence of polygamy as a risk factor for CMDs because the practice was prevalent in the study settings and was regarded as the norm [11].
Notably, this study also found a correlation between a prior history of mental illness and CMDs among nursing mothers, with an odds ratio as high as 4.684. This finding supported the literature’s contention that past mental health issues increase the chance of developing postpartum mental illnesses in the future to as high as 22 folds [7, 45, 50, 51]. This highlights the importance of upscaling mental health services as a core component of antenatal and postnatal care, particularly in low-income countries where such services are limited. Our observation of no apparent relationship between maternal age and CMDs is in contrast to other research findings, which showed a substantial relationship between CMDs and higher maternal age [13, 14]. Perhaps the predominance of younger mothers in our study population helps to explain the lack of an association between age and maternal CMDs in the current study. In addition, the SRQ-20 was not designed to detect psychotic disorders which are linked to older age groups.
Study limitations
Although this study had a good sample size involving all of the major regions of Nigeria, the number of voluntary participants differed across geopolitical zones, with the southeastern region of Nigeria having the lowest number of individuals. This survey was also cross-sectional in design; a prospective study with adequate follow-up would have revealed more about the maternal level of CMD. However, we hope that this will serve as a basis for a more robust longitudinal study design utilising validated instruments to help define the specific mental disorders among breastfeeding mothers with infants admitted to tertiary facilities for targeted intervention. We hope that the second phase of this study will take a longitudinal design approach, assuming that funding will be available.
Conclusion
In Nigeria, the prevalence of common mental disorders is relatively high among breastfeeding mothers with infants admitted to a tertiary care facility. Populations with a history of mental illness, polygamous households, mothers living in the southern region of the country, and low or no educational attainment have a greater risk of developing common mental disorders. This study provides evidence for assessing and tailoring interventions to this specific population.
Supporting information
(SAV)
Acknowledgments
We appreciate all of the mother-baby pairs who participated in this study as well as the healthcare providers who took care of them.
Data Availability
The data have been uploaded with the paper.
Funding Statement
The author(s) received no financial support for the work.
References
- 1.World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. World Health Organization; 1992. https://scholar.google.com/scholar?hl=en&q=Organization+WH.+The+ICD-10+Classification+of+Mental+and+Behavioural+Disorders%3A+Clinical+Descriptions+and+Diagnostic+Guidelines.+Genova%3A+World+Health+Organisation%3B+1992 [Accessed:10 March 2022].
- 2.National Collaborating Centre for Mental Health (UK). Common Mental Health Disorders: Identification and Pathways to Care. Leicester (UK): British Psychological Society (UK); 2011. https://pubmed.ncbi.nlm.nih.gov/22536621/ [Accessed:13 June 2022]. [PubMed]
- 3.Beusenberg M, Orley JH, Health WHOD of M. A user’s guide to the Self-Reporting Questionnaire (SRQ). Geneva: Geneva: World Health Organization, 1994. http://apps.who.int/iris/handle/10665/61113 [Accessed 1 Oct 1, 2022]
- 4.Prescott SL, Greeson JM and El-Sherbini MS. No Health without Mental Health: Taking Action to Heal a World in Distress—With People, Places, and Planet ‘in Mind’. Challenges 2022; 13: 37. [Google Scholar]
- 5.Rehm J and Shield KD. Global burden of disease and the impact of mental and addictive disorders. Current psychiatry reports 2019; 21: 1–7. [DOI] [PubMed] [Google Scholar]
- 6.Global Burden of Disease 2019. Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022. Feb 1; 9(2):137–50. doi: 10.1016/S2215-0366(21)00395-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howard LM and Khalifeh H. Perinatal mental health: a review of progress and challenges. World Psychiatry 2020; 19: 313–327. doi: 10.1002/wps.20769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fond G, Nemani K, Etchecopar-Etchart D, Loundou A, Goff DC, Lee SW, et al. Association between mental health disorders and mortality among patients with COVID-19 in 7 countries: a systematic review and meta-analysis. JAMA psychiatry 2021; 78: 1208–1217. doi: 10.1001/jamapsychiatry.2021.2274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ueda M, Nordström R, Matsubayashi T. Suicide and mental health during the COVID-19 pandemic in Japan. J Public Health. 2022; 44(3):541–8. doi: 10.1093/pubmed/fdab113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ayele FM, Metekya WM, Tesfay K. Association of Maternal Common Mental Disorder and Young Children Acute Malnutrition among Mekelle Public Health Facilities, Northern Ethiopia, 2019-a Case-control Study. Open Public Health J. 2020; 13(1). [Google Scholar]
- 11.Abdullahi AT, Farouk ZL, Imam A. Common mental disorders in mothers of children attending out-patient malnutrition clinics in rural North-western Nigeria: a cross-sectional study. BMC Public Health 2021; 21(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bonacquisti A, Geller PA, Patterson CA. Maternal depression, anxiety, stress, and maternal-infant attachment in the neonatal intensive care unit. J Reprod Infant Psychol 2020;38(3):297–310. doi: 10.1080/02646838.2019.1695041 [DOI] [PubMed] [Google Scholar]
- 13.Harpham T, Huttly S, De Silva MJ, Abramsky T. Maternal mental health and child nutritional status in four developing countries. J. Epidemiol. Community Health 2005;59(12):1060–4. doi: 10.1136/jech.2005.039180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nguyen PH, Saha KK, Ali D, Menon P, Manohar S, Mai LT, et al. Maternal mental health is associated with child undernutrition and illness in Bangladesh, Vietnam and Ethiopia. Public Health Nutr. 2014;17(6):1318–27. doi: 10.1017/S1368980013001043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tanganhito DDS, Bick D, Chang Y-S. Breastfeeding experiences and perspectives among women with postnatal depression: a qualitative evidence synthesis. Women and Birth. 2020;33(3):231–9. doi: 10.1016/j.wombi.2019.05.012 [DOI] [PubMed] [Google Scholar]
- 16.Coo S, García MI, Mira A, Valdés V. The role of perinatal anxiety and depression in breastfeeding practices. Breastfeed Med. 2020; 15(8):495–500. doi: 10.1089/bfm.2020.0091 [DOI] [PubMed] [Google Scholar]
- 17.Okolie U. Problems encountered by breastfeeding mothers in their practice of exclusive breast feeding in tertiary hospitals in Enugu State, South-east Nigeria. J Nutr Metab.2012;4(8):107–13. [Google Scholar]
- 18.Pezley L, Cares K, Duffecy J, Koenig MD, Maki P, Odoms-Young A, et al. Efficacy of behavioral interventions to improve maternal mental health and breastfeeding outcomes: a systematic review. Int. Breastfeed. J. 2022;17(1):1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chrzan-Dętkoś M, Walczak-Kozłowska T, Lipowska M. The need for additional mental health support for women in the postpartum period in the times of epidemic crisis. BMC pregnancy and childbirth. 2021;21(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen S, Zhao G, Li L, Wang Y, Chiu H, Caine E. Psychometric properties of the Chinese version of the Self-Reporting Questionnaire 20 (SRQ-20) in community settings. Int. J. Soc. Psychiatry.2009;55(6):538–47. doi: 10.1177/0020764008095116 [DOI] [PubMed] [Google Scholar]
- 21.Giang KB, Allebeck P, Kullgren G, Van Tuan N. The Vietnamese version of the Self Reporting Questionnaire 20 (SRQ-20) in detecting mental disorders in rural Vietnam: a validation study. Int. J. Soc. Psychiatry. 2006; 52(2):175–84. doi: 10.1177/0020764006061251 [DOI] [PubMed] [Google Scholar]
- 22.van der Westhuizen C, Wyatt G, Williams JK, Stein DJ, Sorsdahl K. Validation of the self-reporting questionnaire 20-item (SRQ-20) for use in a low-and middle-income country emergency centre setting. Int J Ment Health Addict. 2016; 14(1):37–48. doi: 10.1007/s11469-015-9566-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Okolo S, Ogbonna C. Knowledge, attitude and practice of health workers in Keffi local government hospitals regarding Baby-Friendly Hospital Initiative (BFHI) practices. Eur. J. Clin. Nutr. 2002; 56(5):438–41. doi: 10.1038/sj.ejcn.1601331 [DOI] [PubMed] [Google Scholar]
- 24.Oyedeji G. Socio-economic and cultural background of hospitalized children in Ilesa. Niger J Paediatr. 1985; 12:111–7. [Google Scholar]
- 25.Chaput KH, Nettel-Aguirre A, Musto R, Adair CE, Tough SC. Breastfeeding difficulties and supports and risk of postpartum depression in a cohort of womenwho have given birth in Calgary: a prospective cohort study. Can. Med. Assoc. J. 2016;4(1):E103–E9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dias CC, Figueiredo B. Breastfeeding and depression: a systematic review of the literature. J. Affect. Disord.2015; 171:142–54. doi: 10.1016/j.jad.2014.09.022 [DOI] [PubMed] [Google Scholar]
- 27.Woldetsadik AM, Ayele AN, Roba AE, Haile GF, Mubashir K. Prevalence of common mental disorder and associated factors among pregnant women in South-East Ethiopia, 2017: a community based cross-sectional study. Reprod. Health. 2019;16(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tamiru D, Misgana T, Tariku M, Tesfaye D, Alemu D, Weldesenbet AB, et al. Prevalence and associated factors of common mental disorders among pregnant mothers in rural eastern Ethiopia. Front. Psychiatry. 2022;13. doi: 10.3389/fpsyt.2022.843984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kaaya S, Mbwambo J, Kilonzo G, Van Den Borne H, Leshabari M, Fawzi MS, et al. Socio-economic and partner relationship factors associated with antenatal depressive morbidity among pregnant women in. Tanzan. J. Health Res. 2010;12 (1):23–35. [DOI] [PubMed] [Google Scholar]
- 30.Hartley M, Tomlinson M, Greco E, Comulada WS, Stewart J, Le Roux I, et al. Depressed mood in pregnancy: prevalence and correlates in two Cape Town peri-urban settlements. Reprod. Health. 2011;8(1):1–7. doi: 10.1186/1742-4755-8-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Niemi M, Falkenberg T, Petzold M, Chuc NTK, Patel V. Symptoms of antenatal common mental disorders, preterm birth and low birthweight: a prospective cohort study in a semi-rural district of Vietnam. Trop. Med. Int. Health. 2013; 18(6):687–95. doi: 10.1111/tmi.12101 [DOI] [PubMed] [Google Scholar]
- 32.Paffer ATd, Ferreira HdS, Cabral Júnior CR, Miranda CTd. Prevalence of common mental disorders in mothers in the semiarid region of Alagoas and its relationship with nutritional status. Sao Paulo Med. J. 2012; 130:84–91. doi: 10.1590/s1516-31802012000200003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shifa GT, Ahmed AA, Yalew AW. The relationship between under-five child death and maternal mental distress in Gamo Gofa Zone, Southern Ethiopia: a community based comparative cross-sectional study. BMC women’s health. 2018; 18(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khan AM, Flora MS. Maternal common mental disorders and associated factors: a cross-sectional study in an urban slum area of Dhaka, Bangladesh. Int. J. Ment. Health Syst. 2017;11(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Figueiredo B, Dias CC, Brandão S, Canário C, Nunes-Costa R. Breastfeeding and postpartum depression: state of the art review. Jornal de pediatria. 2013;89:332–8. doi: 10.1016/j.jped.2012.12.002 [DOI] [PubMed] [Google Scholar]
- 36.Hahn-Holbrook J, Haselton MG, Dunkel Schetter C, Glynn LM. Does breastfeeding offer protection against maternal depressive symptomatology? Arch Womens Ment Health. 2013;16(5):411–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mezzacappa ES, Katkin ES. Breast-feeding is associated with reduced perceived stress and negative mood in mothers. Health Psychol. 2002;21(2):187. [PubMed] [Google Scholar]
- 38.Yuen M, Hall OJ, Masters GA, Nephew BC, Carr C, Leung K, et al. The Effects of Breastfeeding on Maternal Mental Health: A Systematic Review. J. Women’s Health 2022. doi: 10.1089/jwh.2021.0504 [DOI] [PubMed] [Google Scholar]
- 39.Abiodun O, Adetoro O, Ogunbode O. Psychiatric morbidity in a pregnant population in Nigeria. Gen. Hosp. Psychiatry. 1993;15 (2):125–8. doi: 10.1016/0163-8343(93)90109-2 [DOI] [PubMed] [Google Scholar]
- 40.Mahenge B, Stöckl H, Likindikoki S, Kaaya S, Mbwambo J. The prevalence of mental health morbidity and its associated factors among women attending a prenatal clinic in Tanzania. Int. J. Gynecol. Obstet. 2015;130(3):261–5. doi: 10.1016/j.ijgo.2015.04.032 [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization. Maternal mental health and child health and development in low and middle income countries: report of the meeting, Geneva, Switzerland, 30 January-1 February, 2008. 2008.
- 42.Ntoimo LFC, Okonofua FE, Igboin B, Ekwo C, Imongan W, Yaya S. Why rural women do not use primary health centres for pregnancy care: evidence from a qualitative study in Nigeria. BMC Pregnancy and Childbirth. 2019;19(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dadras O, Nakayama T, Kihara M, Ono-Kihara M, Seyedalinaghi S, Dadras F. The prevalence and associated factors of adverse pregnancy outcomes among Afghan women in Iran; Findings from community-based survey. Plos one. 2021;16(1):e0245007. doi: 10.1371/journal.pone.0245007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tendean AF, Dewi A, Wirasto A. The Implementation of Antenatal Care with Telehealth Towards Pregnant Women’s Mental Health. J Medicoecological dan Manaj Rumah Sakit. 2021;10(2):103–18. [Google Scholar]
- 45.Fellmeth G, Fazel M, Plugge E. Migration and perinatal mental health in women from low- and middle-income countries: a systematic review and meta-analysis. Bjog. 2017;124(5):742–52. doi: 10.1111/1471-0528.14184 [DOI] [PubMed] [Google Scholar]
- 46.Hendrix CL, Werchan D, Lenniger C, Ablow JC, Amstadter AB, Austin A, et al. Geotemporal analysis of perinatal care changes and maternal mental health: an example from the COVID-19 pandemic. Arch Womens Ment. Health. 2022;25(5):943–56. doi: 10.1007/s00737-022-01252-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Treyvaud K, Spittle A, Anderson PJ, O’Brien K. A multilayered approach is needed in the NICU to support parents after the preterm birth of their infant. Early Hum. Dev. 2019; 139:104838. doi: 10.1016/j.earlhumdev.2019.104838 [DOI] [PubMed] [Google Scholar]
- 48.Franck LS, O’Brien K. The evolution of family-centered care: From supporting parent-delivered interventions to a model of family integrated care. Birth Defects Res. 2019;111(15):1044–59. doi: 10.1002/bdr2.1521 [DOI] [PubMed] [Google Scholar]
- 49.Imam A, Hassan-Hanga F, Sallahdeen A, Farouk ZL. Socio-demographic and household-level risk factors for severe acute malnutrition in pre-school children in north-western Nigeria. J. Trop. Pediatr. 2020;66(6):589–97. doi: 10.1093/tropej/fmaa018 [DOI] [PubMed] [Google Scholar]
- 50.Alvarenga P, Frizzo GB. Stressful Life Events and Women’s Mental Health During Pregnancy and Postpartum Period1. Paidéia (Ribeirão Preto). 2017;27:51–9. [Google Scholar]
- 51.O’hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu. Rev. Clin. Psychol. 2013;9:379–407. doi: 10.1146/annurev-clinpsy-050212-185612 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(SAV)
Data Availability Statement
The data have been uploaded with the paper.