Abstract
Background
The worldwide SARS-CoV-2 pandemic represents the most recent global healthcare crisis. While all healthcare systems suffered facing the immense burden of critically-ill COVID-19 patients, the levels of preparedness and adaptability differed highly between countries. Aim: to describe resource mobilization throughout the COVID-19 waves in Tunisian University Medical Intensive Care Units (MICUs) and to identify discrepancies in preparedness between the provided and required resource.
Methods
This is a longitudinal retrospective multicentre observational study conducted between March 2020 and May 2022 analyzing data from eight University MICUs. Data were collected at baseline and at each bed expansion period in relation to the nation’s four COVID-19 waves. Data collected included epidemiological, organizational and management trends and outcomes of COVID-19 and non-COVID-19 admissions.
Results
MICU-beds increased from 66 to a maximum of 117 beds. This was possible thanks to equipping pre-existing non-functional MICU beds (n = 20) and creating surge ICU-beds in medical wards (n = 24). MICU nurses increased from 53 to 200 of which 99 non-ICU nurses, by deployment from other departments and temporary recruitment. The nurse-to-MICU-bed ratio increased from 1:1 to around 1·8:1. Only 55% of beds were single rooms, 80% were equipped with ICU ventilators. These MICUs managed to admit a total of 3368 critically-ill patients (15% of hospital admissions). 33·2% of COVID-19-related intra-hospital deaths occurred within the MICUs.
Conclusion
Despite a substantial increase in resource mobilization during the COVID-19 pandemic, the current study identified significant persisting discrepancies between supplied and required resource, at least partially explaining the poor overall prognosis of critically-ill COVID-19 patients.
Keywords: COVID-19, Preparedness, Public health, Intensive care unit, Healthcare workers
Introduction
The Coronavirus SARS-CoV-2 spread rapidly, reaching almost every part of the world. The pandemic struck healthcare systems worldwide, unmasking many deficiencies. Developed countries such as Italy and the United States of America were overwhelmed by the pandemic [1], [2] . In Tunisia, these deficiencies existed prior to the pandemic, especially since the revolution, where hospitals suffered from poor infrastructure and lack of materials. In addition, the high rate of total payroll at 18%, of the gross domestic product, led to the absence of new personnel recruitment which resulted in healthcare workers (HCW) shortage [3], [4] . The expenses for health represent 6% of the gross domestic product which is rather modest compared to other countries such as France where health expenses attain 11·1% [5], [6] . In response to the pandemic, hospitals in Tunisia were constrained to perform changes in their infrastructures and reorganize resource such as HCW, materials, and, mostly the creation of surge intensive care unit (ICU)-beds [7]. This endeavor was revealed to be difficult and was gradual over the several waves of the pandemic. First of all, the deployment of personnel was initially influenced by fear of contamination [8], once deployed in the ICUs, the nurse-to-patient ratio was at 1:3–1:4. As for ICU-beds, the majority did not respond to certain standards such as the implementation of individual rooms and negative pressure rooms [7].
The aim of the present study is to describe resource mobilization throughout respective waves of the COVID-19 pandemic in Tunisian university medical intensive care units (MICU) and identify discrepancies in preparedness between resource supply and demand.
Methods
Study design and settings
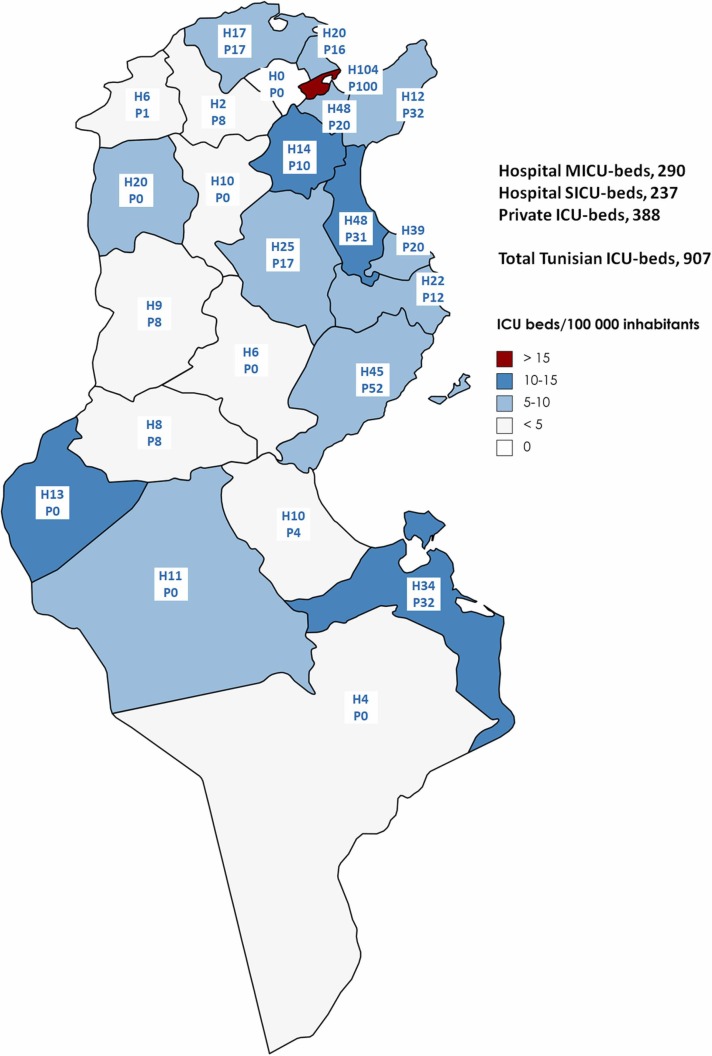
This is a longitudinal retrospective multicentre observational study conducted between March 2020 and May 2022 analyzing data from eight MICUs out of the 12 University MICUs that dealt with COVID-19 patients in Tunisia. Tunisia is a country located in North-Africa with a population of 11·8 million individuals and a total of 24 governorates or states. University MICUs are located in only ten governorates in which just over half (54·54%) of the population lives. Eight MICUs from six different governorates have participated in the current study ( Table 1). Fig. 1 was the result of a phone query we performed within the 24 governorates to describe the respective medical and surgical ICUs, and their affiliation to public or private hospitals.
Table 1.
Distribution of the bed capacity and healthcare workers’ in the included Medical Intensive Care Units (MICUs) according to the related region and hospital.
| MICUs, Governorate | Governorate Population | Hospital beds | MICU beds | Hospital Adult total ICU beds | Hospital nurses |
|---|---|---|---|---|---|
| Hached, Sousse | 737 027 | 704 | 10(0.014) | 14 | 1384(1.96) |
| Mami, Ariana | 655 455 | 375 | 20(0.053) | 20 | 575(1.53) |
| Sfar, Mahdia | 439 824 | 535 | 14(0.026) | 18 | 441(0.824) |
| Zaghouan | 187 990 | 163 | 11(0.067) | 13 | 210(1.28) |
| La Rabta, Tunis | 1 073 110 | 980 | 6(0.006) | 11 | 2018(2.06) |
| Thameur, Tunis | 1 073 110 | 348 | 7(0.020) | 17 | 499(1.43) |
| Yasminet, Ben Arous | 703 206 | 154 | 8(0.052) | 8 | 195(1.26) |
| CAMU, Tunis | 1 073 110 | 22 | 9(0.409) | 9 | 85(3.86) |
Fig. 1.
Visual presentation of regional indexed distribution of ICU beds within the public and private hospitals in Tunisia within the COVID-19 pandemic. *H, hospital-ICU beds; *P, private-ICU beds; MICU, Medical Intensive Care Unit; SICU, surgical Intensive Care Unit; ICU, Intensive Care Unit.
This study is in compliance with the STROBE criteria for observational studies (supplementary material S1).
Definitions and variables
All of the ICUs participating in this study possess required criteria to be classed as a level three ICU according to the task force of the world federation of societies of intensive and critical care medicine [9].
The four COVID-19 waves were defined as first, second, third, and fourth waves from, respectively, March 2020 to April 2020, from August 2020 to May 2021, June 2021 to September 2021, and December 2021 to May 2022.
SARS-CoV-2 infection was defined as either a positive Real-Time Reverse Transcriptase-Polymerase Chain Reaction assay of nasal swabs or a positive coronavirus-19 rapid antigen test device [10], along with a high pre-test clinical probability.
COVID-19-related Acute Respiratory Distress Syndrome (ARDS) management protocol: Therapeutic protocols complied with national and international guidelines, which recommend systematic corticosteroids and preventive anticoagulation to all patients, and elective antibiotherapy and anti-IL-6 in specific indications [11]. The main concern in the management of ARDS related Acute Hypoxemic Respiratory Failure is to improve oxygenation and reduce muscle use [12], [13] and promote lung recruitment while preventing Patient Self-Inflicted Lung Injury (P-SILI) [14], [15] and not delay intubation while promoting protective ventilation and preventing Ventilator Induced Lung Injury (VILI) and heart/lung interaction [16]. Diagnostic and therapeutic procedures were protocolized. Based on that, a goal-directed bundle associating Non-Invasive Respiratory Support (NIRS), bed rest, awake proning, and ICU delirium prevention and management was implemented in spontaneous breathing patients [16].
Data collection
Most data were collected prospectively through pre-existing registers for each hospital and ICU. Data not already collected in registers were recorded retrospectively following a consensus describing each variable that was shared via email. The principal investigator visited each site before and during data collection to ensure that the respective ICUs' report forms were consistently filled out, thus controlling for any information bias. A single senior intensivist trained in data collection and handling from each site was responsible for recording and providing data from his center to control for potential interobserver and intraobserver bias. Each hospital and its corresponding ICU recorded their data on a specific case record form. Data were collected at baseline and at each bed expansion period in relation with the nation’s four COVID-19 waves. There were no missing data.
For the current study, epidemiological data recorded in each evolution period consisted of total COVID-19 admissions, deaths, and non-COVID admissions to the corresponding regular ward and ICU. Furthermore, the need for invasive mechanical ventilation (IMV) in ICU patients was recorded. Organizational data in each ICU were also recorded for each evolution period: number of beds and surge beds, critical care and non-critical care nurses, critical care and non-critical care residents, and senior critical care doctors. To evaluate the impact of resource mobilization, mortality rates were compared between the two periods, before and after the maximum reached resource mobilization. Early reports from northern Italy and China pointed to a high burden of ICU as well as poor outcomes [17], [18], [19]. On the other hand, adequate preparedness for the COVID-19 pandemic was associated with better outcomes in Nordic countries [20].
Statistical analyses
Characteristics were described as frequencies and percentages for categorical variables. Where appropriate, data are presented normalized to the population (per 100 000 inhabitants). Statistical analyses were performed with SPSS software. Epi Info statistics software was used to compare the between periods mortality proportions.
Results
Resource mobilization
MICUs’ beds and response in surge bed capacities
During the course of the pandemic, there were four different evolutions within all ICUs; the first as a preparation for the 2nd COVID-19 wave, the second within the course of the 2nd wave, the third at the beginning of the 3rd wave, and the last evolution during the 4th spike.
The total number of beds within the eight ICUs increased exponentially from 66 beds at baseline, of which only 14 were dedicated to COVID-19 patients, to 117 beds of which all can be dedicated to COVID-19 patients if required. The maximum bed capacity was reached during the 3rd wave which was the deadliest. Table 2 displays all MICUs bed capacities and their evolution periods within the different waves. To reach these numbers different hospitals applied different means: equipping pre-existing non-functional ICU beds and creating dedicated surge beds in medical wards.
Table 2.
Compared Medical Intensive Care Units (MICUs) beds’ capacities and their evolution within the different pandemic waves.
| MICUs | Baseline | Wave 1 March 20-April 20 | Wave 2 August 20- May 21 | Wave 3 June 21- Sep 21 | Wave 4 Dec 21-May 22 | Surge beds n (%) | Means |
|---|---|---|---|---|---|---|---|
| Hached, Sousse | 10 | 4 | 12 | 23 | 12 | 13 (130) | A, 5 B, 8 |
| Mami, Ariana | 20 | 10 | 10 | 20 | 20 | 0 (0) | - |
| Sfar, Mahdia | 10 | - | 4 | 14 | 10 | 4 (40) | A, 4 |
| Régional, Zaghouan | 6 | - | 6 | 10 | 11 | 5 (83·3) | A, 3 B, 2 |
| La Rabta, Tunis | 6 | - | 6 | 8 | 8 | 2 (33·3) | A, 2 |
| Thameur, Tunis | 7 | - | 6 | 21 | 20 | 14 (200) | B, 14 |
| Yasminet, Ben Arous | 8 | - | 8 | 10 | 12 | 4 (50) | A, 4 |
| CAMU, Tunis | 9 | - | 5 | 11 | 11 | 2 (22·2) | A, 2 |
| Totals | 76 | 14 | 57 | 117 | 104 | 44 (57·9) |
A, equipping pre-existing non-functional ICU beds; B, creating dedicated surge beds in medical wards.
Data were expressed as n (%) for categorical variables.
Nurses’ mobilization and trends throughout the COVID-19 pandemic
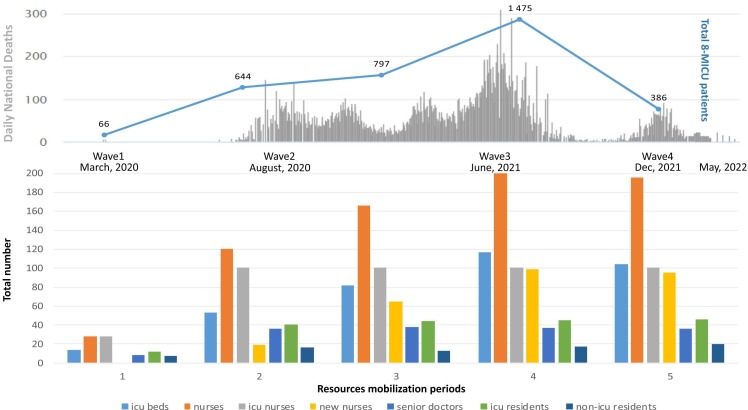
Fig. 2 displays trends of MICU-beds, HCW, and doctors (colored bar chart) and managed patients (blue curve) within the eight MICUs according to the respective pandemic waves referred to by the spikes of national COVID-19 mortality incidence (gray bar chart).
Fig. 2.
MICU-beds and healthcare workers’ mobilization across respective COVID-19 pandemic waves in Tunisian University MICUs. Fig. 2 displays trends of MICU-beds, healthcare workers, and doctors (colored bar chart) and managed patients (blue curve) within the eight MICUs according to the respective pandemic waves referred to by the spikes of national COVID-19 mortality incidence (gray bar chart).
During the start (period 1, Fig. 2) of the pandemic COVID-19 patients were only admitted to two MICUs (Hached, Sousse and Mami, Ariana), in the two hospitals initially considered as referral hospitals, n = 14 MICU-beds having managed the only first 66 COVID-19 patients. The remaining hospitals started progressively admitting COVID-19 patients during the course of the pandemic. It was only at the 3rd bed-expansion period within the second wave of the pandemic, that all eight hospitals, thus all eight MIUCs, were obliged to admit COVID-19 patients. The maximum number of patients managed within the eight MICUs was recorded during the 4th period (corresponding to the 3rd wave) at 1475 patients managed within 117 MICU-beds by 200 nurses (101 ICU nurses + 99 non-ICU deployed nurses).
The number of nurses increased along with the increase in bed capacity. Surge nurses were either recruited in form of temporary work contracts or deployed from other departments that decreased or stopped their activity during the waves. Through the different waves of the pandemic, despite the continuous increase in recruited nurses, the nurse-to-MICU-bed ratio never exceeded 2·26:1. Half of the deployed nurses were non-ICU ones.
Organization of doctors within the different MICUs
Deploying both senior doctors and residents was difficult due to the limited number of intensivists available. The number of senior doctors remained constant within all four pandemic waves whereas the number of residents only slightly increased from 57 to 66. (Fig. 2).
General outcomes of patients admitted to hospitals and related MICUs during the COVID-19 pandemic
Throughout the pandemic, the MICUs managed to absorb 3368 critical COVID-19 patients, corresponding to 15% of all COVID-19 patients admitted to the respective hospitals (ranging between 5·4% and 65·9%). Forty-six percent required IMV, ranging from 16·9% to 56·3%. Mortality was rather high at 43·4% ranging from 25·7% to 54·5%. As the maximum of MICU beds and nurses was mobilized within the year 2021, respective compared mortality rates between 2020 and 2021–2022 were 50·70% vs 45·14%, p = 0·012.
Only six MICUs continued admitting both COVID-19 and non-COVID-19 patients. In those ICUs, 2301 non-COVID-19 patients were admitted ranging between 47 (Yasminet, Ben Arous) and 1043 (CAMU Toxicology-MICU, Tunis).
Patient admissions, IMV management, and deaths in each MICU and its corresponding hospital are summarized in Table 3.
Table 3.
Compared in-hospital and Medical Intensive Care Units’ (MICUs) admissions, invasive mechanical ventilation (IMV) and deaths within the pandemic.
| MICUs | COVID-19 Hospital-admissions n |
COVID-19 MICU/hospital-admissions n (%) |
Non-COVID-19 MICU-admissions n |
COVID-19 IMV-MICU n (%) |
COVID-19 MICU-deaths n (%) | COVID-19 Hospital-deaths n |
COVID-19 MICU/Hospital-deaths % |
|---|---|---|---|---|---|---|---|
| Hached, Sousse | 3714 | 534 (14·4) | 378 | 280 (52·4) | 246 (46·1) | 759 | 32·4 |
| Mami, Ariana | 4880 | 674 (13·8) | 244 | 371 (55·0) | 362 (53·7) | 701 | 51·6 |
| Sfar, Mahdia | 1784 | 472 (26·5) | 0 | 230 (48·7) | 188 (39·8) | 431 | 43·6 |
| Zaghouan | 1 551 | 368 (23·7) | 235 | 154 (41·4) | 158 (42·9) | 342 | 46·2 |
| La Rabta, Tunis | 5071 | 343 (6·8) | 0 | 193 (56·3) | 187 (54·5) | 1057 | 17·7 |
| Thameur, Tunis | 892 | 538 (60·3) | 354 | 91 (16·9) | 138 (25·7) | 493 | 28·0 |
| Yasminet, Ben Arous | 4260 | 230 (5·4) | 47 | 128 (55·7) | 110 (47·8) | 552 | 19·9 |
| CAMU, Tunis | 317 | 209 (65·9) | 1043 | 103 (49·3) | 74 (35·4) | 74 | 100 |
| Totals | 22,469 | 3368 (15·0) | 2301 | 1550 (46·0) | 1463 (43·4) | 4409 | 33·2 |
Discrepancies in preparedness between resource supply and demand
MICUs’ infrastructures prior to the pandemic discrepancies
Within the eight MICUs participating in the present study, none had “cleanrooms” modern standard infrastructure (which are well isolated, well-controlled from contamination, and actively cleansed). Out of the existing 76 MICU-beds prior to the pandemic, only 55% were individual beds in individual rooms. All individual rooms had a surface of over 25 square meters. None of the MICUs had pre-existing airlocks at the entrance of the rooms and only eight negative-pressure rooms within one MICU (Yasminet, Ben Arous) were available at the start of the pandemic. Two MICUs were able to install airlocks during the first wave (Hached, Sousse and Mami, Ariana).
Material supply discrepancies
Eighty percent of pre-existing beds were equipped with ICU ventilators. However, these ventilators were predominantly old models and unable to perform High Flow Nasal Oxygen function. Most recent ventilators lacked heated humidification systems. The absence of humidification also impeded the use of Continuous Positive Airway Pressure (CPAP) via ICU ventilators. Impedance valves used to produce CPAP via facial masks were inexistent.
Immediately before the first COVID-19 wave many parties, including the government and donors from the society, attempted but failed to provide ventilators for the MICUs due to their unavailability in the local market along with COVID-19 related international restrictions complicating import.
Healthcare workers’ mobilization discrepancies
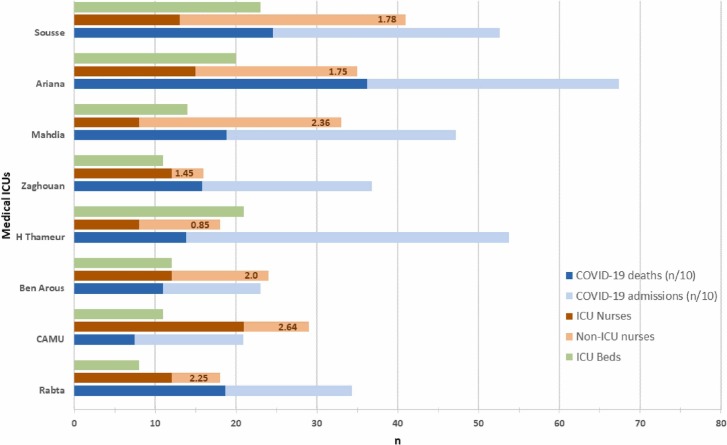
Healthcare worker’s shortage during the pandemic has been described by the discrepancies between the observed nurse: ICU-bed ratio and a calculated ratio of 3:1, estimated to provide a nurse-to-patient ratio of 1:2 per shift [21], [22], [23], ensuring at least four shifts. Fig. 3.
Fig. 3.
Compared maximum bed capacity, ICU-nurses and deployed-nurses, admitted COVID-19 patients and deaths within respective eight Tunisian University Medical-ICUs. * 1·78, nurse-to-ICU-bed ratio. ICU, Intensive Care Unit.
For all, the 117 beds (54 invasive beds, 63 noninvasive beds) and given the respective nurse:patient ratios at 1:1 for invasive and 1:2 for noninvasive, the total required nurses number is estimated at 304 ICU nurses, while in the present study, there were only 200 nurses (101 ICU nurses and 99 deployed non-ICU nurses).
The 99 deployed non-ICU nurses are largely insufficient, as in hospital-1 that mobilized the largest number of non-ICU nurses (n = 41), there were only 28 deployed non-ICU nurses from the nurses already working in the hospital’s regular wards (n = 1384), and 13 non-ICU short employment contract nurses. Within this large reserve of the already employed 1384 nurses, only 200 were dispatched to the COVID-19 oxygen wards, the remaining were evolving either in medical wards with restricted non-COVID-19 activity or surgical wards with delayed elective surgery. Meanwhile, the gap in ICU nurses’ recruitment and the real workload was absorbed by the already understaffed residents.
Organization discrepancies
A surrogate of this discrepancy could be the number of intra-hospital patients potentially denied for ICU admission. As this information was missing, intra-hospital deaths could be assumed as potentially severe to critical patients denied for ICU admission. Indeed, the low ICU / intra-hospital deaths ratio at 33·2% means clearly that 66% of deaths occurred out of the MICUs demonstrating that the system is largely overwhelmed.
Discussion
Pandemics generally exhibit a critical challenge and a unique threat to the country’s health care system. Many healthcare systems worldwide were overwhelmed by the substantial increase in the demand and supply of health services. Therefore, pandemic preparedness necessitates adapted scalable infrastructure and capacity as a critical aspect of a country’s emergency response.
Albeit huge efforts were deployed to increase MICU bed surge capacity, ventilators, HCW, and organization, Tunisian ICUs failed to accommodate and ingest the overwhelming demand for healthcare services, one of the most critical issues during the healthcare system response to epidemics. This was demonstrated by the huge proportion of ICU mortality, a consequence of the discrepancy between supply and demand, slow supply, and supply quality. Furthermore, relatively high intra-hospital COVID-19 deaths within the oxygen wards (a surrogate for the patients denied for ICU admission) demonstrate an overwhelming system.
Study limitations
Several limitations could be addressed in the present study. First, the retrospective design was an impediment to exactly appreciate the proportion of patients necessitating ICU admission, thus an exact measurement of the supply/demand discrepancies. This was addressed by the use of pre-defined surrogates such as in-hospital COVID-19 mortality. Second, the present study included only eight over 12 University MICUs, but this is quite representative of the real response to the epidemic as these MICUs’ respective hospitals drained the quasi-majority of the severe to critical COVID-19 patients nationwide. Other ICUs were secondarily involved in the management of the third wave of the pandemic mainly surgical ICUs, non-University MICUs, or the several field hospitals. Finally, the relatively poor outcomes should be balanced with the poor structural, material, HCW, and organizational resource prior to the pandemic in a low-middle-income country experiencing difficulties in a continuing process of a post-revolution political transition.
Strengths of the study
First, this is the first multicentre study addressing the issue of preparedness in Tunisian University MICUs, relating 66% of the MICUs involved in the pandemic. Second, it unveiled difficulties faced by a North-African low-middle income country displaying different geopolitics, cultural and social singularities, low resource and infrastructure, and organizational issues. This could be used as a valuable benchmark to adapt the response to future pandemics. Finally, the present study sheds light on the different management aspects of severe to critical COVID-19, thus giving great lessons and messages when facing future pandemics.
Human and material resource mobilization through the different COVID-19 waves
The current study demonstrated a sharp rise in the number of MICU beds available for COVID-19 patients throughout the pandemic. Despite substantial achievements, a delay was noted in coordinating efforts between the MICUs.
Although MICUs failed to accommodate and ingest the overwhelming demand for healthcare services, as they managed only 15% of the respective hospital admitted patients, this is largely discrepant with initial worldwide reports within the pandemic relating over 35% [24], [25], they were able to achieve a significant decrease of ICU mortality within the second year of the pandemic after they have reached the maximum of resource mobilization. This gain could also be explained by the improvement of the evolving knowledge [26], [27], and the ICU management quality [28] but not the vaccination as it started very late in the course of the pandemic or the greater flux and severity of the patients within the second period.
Within the study, we noted a first increase between the 1st and 2nd waves, on account of six MICUs joining in managing COVID-19 patients. In fact, at the very start of the pandemic only two hospitals, considered as referral hospitals, admitted patients from all around the country. This sectorization was mainly the result of a poor appreciation of the pandemic’s severity by officials along with considerable fear striking both HCW and administrates. As a result of efforts deployed throughout the study period, all eight MICUs combined, managed to provide a maximum of 117 MICU-beds, generating a maximum total surge capacity of 44/76 MICU-beds (57·9%). Overwhelmed by a never-ending increase in critically-ill patients requiring life-sustaining management, ICUs around the world adopted different strategies for the sole purpose of increasing bed capacity [29], [30], [31]. The response to the overflow of critically-ill patients varied depending on public health policies. As a matter of fact, various reports demonstrated that ICUs in different demographic settings and political environments managed to produce different rates of increase in surge bed capacity. Nordic countries displayed a variable increase in ICU beds between March 2020 and May 2020 ranging from 30·3% to 143·75% [20] while a tertiary teaching hospital in Saudi Arabia of over 1100 beds managed to obtain a 117·24% increase in the number of ICU beds between March 1st and July 31st [32]. The recent UNITE-COVID study including 280 ICUs from 46 countries showed a global increase between February and May 2020 by 54·74%, which is comparable to the findings in the current study [33]. In certain cases however, healthcare systems failed to adapt such as in a recent Brazilian survey reporting that ICU beds, nurses, and ventilators were significantly less available during the second national surge [34], an assessment of the surge capacity in the Kenyan health system unveiled a major shortage in hospital accommodation capacities [35].
Discrepancies between what we have done and what we should have done better
Managing critically-ill COVID-19 patients comes down to much more than a mere physical ICU bed [9]. Although vital, continuous monitoring technology as well as organ support therapy require trained and qualified HCWs. It has already been established that higher nursing staff-to-patient ratio is associated with better safety and patient outcomes [21]. Many teams have already stated that the main limit to further increasing bed capacity despite abundant physical beds and ventilators is available nursing staff [29], [36]. In the present study, diverse strategies were adopted to provide sufficient nursing staff for functioning ICU beds, resulting in a two-fold increase in the nurse-to-patient ratio which remains very insufficient compared to recommendations [22], [37].
The main difficulty at the beginning of the pandemic was overcoming the disproportional fear of infection transmission [8], potentially explaining the delay in deployment of nurses working in other departments with decreased activity (surgical wards, post-operative units, surgical ICUs…). Over the course of the evolution, there was an increase in both the number and competence of deployed nurses. The more effective way of increasing the nursing staff was secondarily exerted by the government which consisted in providing short-term employment contracts to recently-graduated and unemployed nurses. The recruitment of these young volunteer nurses provided an important number of HCWs, but with insufficient experience relating to critical care, and required intensive training within the ICUs and they ought to be accompanied by trained nurses already evolving in the respective ICUs.
Despite a substantial increase in ICU beds, equipment, and nurses, there was little to no addition to the number of senior doctors or medical residents. In fact, a major drawback in the current study’s healthcare system is that Anesthesiology and Intensive care are two separate specialties meaning that there was a limited pool of qualified intensivists available. In certain healthcare systems such as during the first wave in France, despite also being different specialties, there was a 65% increase in critical care medical manpower by mobilizing anesthesiology physicians and residents with complete intensive care training [30].
In the present study, the eight MICUs tackled organizational issues by equipping pre-existing non-functional ICU beds, creating dedicated surge beds, stopping all non-urgent surgical activities, and using postoperative beds for COVID-19 patients. Meanwhile, some studies offered an alternative to ICU organization such as the study of Oakley et al. where the configuration of the ICU followed an " assembly line " approach, where ICU care of the COVID-19 disease was deconstructed into its constituent’s parts allowing several teams, that each had a particular set of skills, to work in a sequential manner [38]. In contrast, another strategy was conducted in a French hospital where one building with its three floors was restructured to englobe all the aspects of dealing with the disease, namely, an intensive care unit, an acute care unit, a physical medicine and rehabilitation, and a COVID-19 screening area. Another interesting fact is that the pavilion had autonomy regarding dedicated patients’ pathway and the logistical organization such as materials and workforce. This type of organization facilitates transfer of patients between the different units [39]. Some hospitals, chose other strategies such as canceling elective surgeries and suspension of most deferrable activities to improve hospital capacity [31], [40].
Messages learned from the pandemic
Several lessons can be drawn from the results of the present study assessing preparedness and impact during the COVID-19 pandemic.
Act early and widely
It is never to underestimate a crisis and to act as early as possible. A common theme in our countries is that we designated certain hospitals to care for COVID-19 patients at the start of the crisis. Little did we know that all the hospitals in the country would be overwhelmed by the sheer number of critical cases. The point here is never to underestimate a crisis, always be vigilant and prepared for the worse.
Engagement with social accountability partners
This is the cornerstone of the management of a pandemic [41]. Being inspired from similar projects facilitated elsewhere could be a valuable behavior to start with.
Healthcare systems organizational aspects
In a public health crisis such as the COVID-19 pandemic, prompt priority should be given to the creation of large-scale ICUs “Mega-ICUs” in hospitals dedicated to treating the same disease with its myriad of severity presentations. Protocolization and deconstruction of tasks creating devoted teams of doctors, nurses, and caregivers managing tasks within their respective area of expertize could help improve outcome, increase commitment, and reduce psychological impact (teams dedicated to triage, delirium management, family-needs, ventilatory management, renal replacement therapy, interventional procedures). These hospitals should be kept up-to-date with emerging guidelines and recommendations, being flexible and following trends while ensuring continuous commitment with authorities, stakeholders and the civil society. Simplicity and flexibility, rather that rigidity and fear, seem to have favorably impacted outcomes.
Team building and efficiency
Designate a team of professionals with the specific tasks of i) managing staff members within hospitals ensuring equitable and customized deployment, ii) ensuring minimal required training prior to deployment, iii) anticipate and provide psychological support, promoting transparency between administration and frontline staff, detecting early signs of burnout and managing fear, iv) ensure the provision of necessary staff protection. The creation of airlocks for disinfection or even areas for donning and doffing personal protective equipment can reduce fear and the psychological impact on caregivers.
Simplicity, pragmatism, frugality and adherence to basic principles
Striving for excellence in face of adversity as doing more with less or promoting creativity and innovation. The art to do simple things well, is encouraged, aiming toward clinical acumen and less invasive critical care.
Bed capacity to be substantially increased
There is a high need to upgrade and standardize existing ICUs and create new ones.
This pandemic has finally taught us to move from the ventilator to the staff, to pay attention to equity, to accept the uncertainty, to have faith in science, in data, in ourselves and in our colleagues. We have to manage fear and misinformation and develop leadership.
Conclusion
Albeit respectable deployed efforts to mobilize resources throughout respective waves of COVID-19 pandemic in Tunisian University MICUs, the present study identified significant discrepancies in preparedness between resources’ supply and demand. This may explain in part the poor prognosis of COVID-19 especially in mechanically ventilated patients.
Humans Ethics Statement
All procedures performed in the present retrospective study, involving human participants, were in accordance with the ethical standards of the Institutional Research and Ethics Committee of the University Hospital Farhat Hached, Sousse and National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Authorship
(1) Literature search, (2) Data collection, (3) Study design, (4) Analysis of data, (5) Manuscript preparation, (6) Review of manuscript.
| MB, | MD, Professor, | (1, 2, 3, 4, 5, 6) |
| KM, | MD, Associate-Professor, | (1, 2, 3, 4, 5, 6) |
| RT, | MD, Resident, | (1, 2, 3, 4, 5, 6) |
| EE, | MD, Associate-Professor, | (1, 2, 3, 4, 5, 6) |
| SA, | MD, Professor, | (2, 3, 6) |
| FJ, | MD, Associate-Professor, | (2, 3, 6) |
| JBK, | MD, Professor, | (2, 3, 6) |
| OJ, | MD, Associate-Professor, | (2, 3, 6) |
| HN, | MD, Associate-Professor, | (2, 3, 6) |
| SE, | MD, Professor, | (2, 3, 6) |
| FE, | MD, Associate-Professor, | (2, 3, 6) |
| IT, | MD, Associate-Professor, | (2, 3, 6) |
| TM, | MD, Professor, | (2, 3, 6) |
| AT, | MD, Professor, | (2, 3, 6) |
| ES, | MD, Resident, | (2, 3, 6) |
| SA, | MD, Professor, | (2, 3, 6) |
| HD, | MD, Associate-Professor, | (2, 3, 6) |
| BB, | MD, Associate-Professor, | (2, 3, 6) |
| NB, | MD, Professor, | (2, 3, 6) |
| IF, | MD, Professor, | (2, 3, 6) |
| MK, | MD, Associate-Professor, | (2, 3, 6) |
| NK, | MD, Professor, | (2, 3, 6) |
| ABJ, | MD, Associate-Professor, | (2, 3, 6) |
| HBG, | MD, Professor, | (2, 3, 6) |
| NB, | MD, Professor, | (2, 3, 6) |
Adult Consent To Participate Written
This study received approval from the Institutional Research and Ethics Committee of the University Hospital Farhat Hached, Sousse. The need for a written informed consent was waived, as the study was a retrospective one.
Human Accordance Statement
Not Applicable, retrospective design.
Funding
This research did not receive any specific grant from funding agencies.
Conflict of interest
All the authors certify that they have no affiliations with/or involvement in any organization or entity with any financial interest in the subject matter or materials discussed in this manuscript.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.jiph.2023.02.022.
Appendix A. Supplementary material
Supplementary material
.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to limitations of ethical approval involving the participants’ data and anonymity but are available from the corresponding author on reasonable request.
References
- 1.Fagiuoli S., Lorini F.L., Remuzzi G. Covid-19 Bergamo Hospital Crisis Unit. Adaptations and lessons in the Province of Bergamo. N Engl J Med. 2020;382 doi: 10.1056/NEJMc2011599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harris G., Adalja A. ICU preparedness in pandemics: lessons learned from the coronavirus disease-2019 outbreak. Curr Opin Pulm Med. 2021;27:73–78. doi: 10.1097/MCP.0000000000000749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soudani S.F.M.I.: La Tunisie doit contenir la masse salariale à 15% du PIB en 2022. lecourrierdelatlas 2021. https://www.lecourrierdelatlas.com/fmi-la-tunisie-doit-contenir-la-masse-salariale-a-15-du-pib-en-2022/ (accessed September 27, 2022).
- 4.Réduction de la masse salariale: Ce qu’a proposé le gouvernement Bouden au FMI | Webmanagercenter n.d. https://www.webmanagercenter.com/2021/12/27/478129/reduction-de-la-masse-salariale-ce-qua-propose-le-gouvernement-bouden-au-fmi/ (accessed September 27, 2022).
- 5.Tunisia. Principales statistiques sanitaires. World Health Organ - Reg Off East Mediterr n.d. http://www.emro.who.int/fr/right-teasers/tunisia/principales-statistiques-sanitaires.html (accessed September 27, 2022).
- 6.Dépenses de santé en proportion du PIB | Panorama de la santé 2021: Les indicateurs de l′OCDE | OECD iLibrary n.d. https://www.oecd-ilibrary.org/sites/abdeea0e-fr/index.html?itemId=/content/component/abdeea0e-fr#indicator-d1e33231 (accessed September 27, 2022).
- 7.Meddeb K., Toumi R., Boussarsar M. Lessons learned from the COVID-19 pandemic in a North-African country (Tunisia) Tunis Med. 2022;100:568–571. [PMC free article] [PubMed] [Google Scholar]
- 8.Meddeb K., Chelbi H., Boussarsar M. Fear, preparedness and Covid-19. Tunis Med. 2020;98:321–323. [PubMed] [Google Scholar]
- 9.Marshall J.C., Bosco L., Adhikari N.K., Connolly B., Diaz J.V., Dorman T., et al. What is an intensive care unit? A report of the task force of the World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care. 2017;37:270–276. doi: 10.1016/j.jcrc.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 10.Organization W.H. Clinical management of severe acute respiratory infection when novel coronavirus (nCoV) infection is suspected, Interim guidance, 13 March 2020 2020.
- 11.Direction Qualité des Soins et Sécurité des Patients. GUIDE PARCOURS DU PATIENT SUSPECT OU CONFIRME COVID-19 REPONSE RAPIDE. vol. VERSION NOVEMBRE 2020. https://www.ineas.tn/sites/default/files/gps_covid-19_mise_a_jour.pdf, 2020.
- 12.Sklar M.C., Munshi L. Advances in ventilator management for patients with acute respiratory distress syndrome. Clin Chest Med. 2022;43:499–509. doi: 10.1016/j.ccm.2022.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Esnault P., Cardinale M., Hraiech S., Goutorbe P., Baumstrack K., Prud’homme E., et al. High respiratory drive and excessive respiratory efforts predict relapse of respiratory failure in critically Ill patients with COVID-19. Am J Respir Crit Care Med. 2020;202:1173–1178. doi: 10.1164/rccm.202005-1582LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Battaglini D., Robba C., Ball L., Silva P.L., Cruz F.F., Pelosi P., et al. Noninvasive respiratory support and patient self-inflicted lung injury in COVID-19: a narrative review. Br J Anaesth. 2021;127:353–364. doi: 10.1016/j.bja.2021.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grieco D.L., Menga L.S., Eleuteri D., Antonelli M. Patient self-inflicted lung injury: implications for acute hypoxemic respiratory failure and ARDS patients on non-invasive support. Minerva Anestesiol. 2019;85:1014–1023. doi: 10.23736/S0375-9393.19.13418-9. [DOI] [PubMed] [Google Scholar]
- 16.Meyer N.J., Gattinoni L., Calfee C.S. Acute respiratory distress syndrome. Lancet Lond Engl. 2021;398:622–637. doi: 10.1016/S0140-6736(21)00439-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet Lond Engl. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H., et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A., et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chew M.S., Kattainen S., Haase N., Buanes E.A., Kristinsdottir L.B., Hofsø K., et al. A descriptive study of the surge response and outcomes of ICU patients with COVID-19 during first wave in Nordic countries. Acta Anaesthesiol Scand. 2022;66:56–64. doi: 10.1111/aas.13983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bray K., Wren I., Baldwin A., St Ledger U., Gibson V., Goodman S., et al. Standards for nurse staffing in critical care units determined by: the British Association of Critical Care Nurses, The Critical Care Networks National Nurse Leads, Royal College of Nursing Critical Care and In-flight Forum. Nurs Crit Care. 2010;15:109–111. doi: 10.1111/j.1478-5153.2010.00392.x. [DOI] [PubMed] [Google Scholar]
- 22.Sharma S.K., Rani R. Nurse-to-patient ratio and nurse staffing norms for hospitals in India: a critical analysis of national benchmarks. J Fam Med Prim Care. 2020;9:2631–2637. doi: 10.4103/jfmpc.jfmpc_248_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The Importance of the Optimal Nurse-to-Patient Ratio n.d. https://www.wolterskluwer.com/en/expert-insights/the-importance-of-the-optimal-nursetopatient-ratio (accessed September 29, 2022).
- 24.Rahman S., Montero M.T.V., Rowe K., Kirton R., Kunik F. Epidemiology, pathogenesis, clinical presentations, diagnosis and treatment of COVID-19: a review of current evidence. Expert Rev Clin Pharmacol n.d.:1–21. https://doi.org/10.1080/17512433.2021.1902303. [DOI] [PMC free article] [PubMed]
- 25.Silva B.R.O., Rodrigues W.F., Abadia D.G.P., Alves da Silva D.A., Andrade E., Silva L.E., Desidério C.S., et al. Clinical-epidemiology aspect of inpatients with moderate or severe COVID-19 in a Brazilian Macroregion: disease and countermeasures. Front Cell Infect Microbiol. 2022;12 doi: 10.3389/fcimb.2022.899702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu Y., Peng Z., Yan Y., Hu J., Wang Y., Wang X., et al. Current knowledge of COVID-19: advances, challenges and future perspectives. Biosaf Health. 2021;3:202–209. doi: 10.1016/j.bsheal.2021.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Verspoor K. The evolution of clinical knowledge during COVID-19: towards a global learning health system. Yearb Med Inf. 2021;30:176. doi: 10.1055/s-0041-1726503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Salem A., Elamir H., Alfoudri H., Shamsah M., Abdelraheem S., Abdo I., et al. Improving management of hospitalised patients with COVID-19: algorithms and tools for implementation and measurement. BMJ Open Qual. 2020;9 doi: 10.1136/bmjoq-2020-001130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Litton E., Huckson S., Chavan S., Bucci T., Holley A., Everest E., et al. Increasing ICU capacity to accommodate higher demand during the COVID-19 pandemic. Med J Aust. 2021;215:513–517. doi: 10.5694/mja2.51318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Verdonk F., Zacharowski K., Ahmed A., Orliaguet G., Pottecher J. A multifaceted approach to intensive care unit capacity. Lancet Public Health. 2021;6 doi: 10.1016/S2468-2667(21)00131-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vranas K.C., Golden S.E., Mathews K.S., Schutz A., Valley T.S., Duggal A., et al. The influence of the COVID-19 pandemic on ICU organization, care processes, and frontline clinician experiences: a qualitative study. Chest. 2021;160:1714–1728. doi: 10.1016/j.chest.2021.05.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Al-Dorzi H.M., Aldawood A.S., Almatrood A., Burrows V., Naidu B., Alchin J.D., et al. Managing critical care during COVID-19 pandemic: the experience of an ICU of a tertiary care hospital. J Infect Public Health. 2021;14:1635–1641. doi: 10.1016/j.jiph.2021.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Greco M., De Corte T., Ercole A., Antonelli M., Azoulay E., Citerio G., et al. Clinical and organizational factors associated with mortality during the peak of first COVID-19 wave: the global UNITE-COVID study. Intensive Care Med. 2022;48:690–705. doi: 10.1007/s00134-022-06705-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lobo S.M., Creutzfeldt C.J., Maia I.S., Town J.A., Amorim E., Kross E.K., et al. Perceptions of critical care shortages, resource use, and provider well-being during the COVID-19 pandemic. Chest. 2022;161:1526–1542. doi: 10.1016/j.chest.2022.01.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barasa E.W., Ouma P.O., Okiro E.A. Assessing the hospital surge capacity of the Kenyan health system in the face of the COVID-19 pandemic. PLoS One. 2020;15 doi: 10.1371/journal.pone.0236308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Young P.J., Psirides A., Streat S. New Zealand’s staffed ICU bed capacity and COVID-19 surge capacity. N Z Med J. 2021;134:8–10. [PubMed] [Google Scholar]
- 37.Cribbin D. Critical Care Nursing Workforce Report 2018 n.d.:22.
- 38.Oakley C., Pascoe C., Balthazor D., Bennett D., Gautam N., Isaac J., et al. Assembly line ICU: what the Long Shops taught us about managing surge capacity for COVID-19. BMJ Open Qual. 2020;9 doi: 10.1136/bmjoq-2020-001117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bessis S., Dinh A., Gautier S., Davido B., Levy J., Lawrence C., et al. A restructured hospital into a one-building organization for COVID-19 patients: a resilient and effective response to the pandemic. Front Public Health. 2022 doi: 10.3389/fpubh.2022.709848. 709848–709848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Covid-19 pandemic: a frontline hospital reorganization to cope with therapeutic and diagnostic emergency - PubMed n.d. https://pubmed.ncbi.nlm.nih.gov/32810626/ (accessed September 28, 2022). [DOI] [PMC free article] [PubMed]
- 41.Faviero G.F., Stocking B.M., Hoffman S.J., Liu A., Bausch D.G., Galea S., et al. An effective pandemic treaty requires accountability. Lancet Public Health. 2022;7:e730–e731. doi: 10.1016/S2468-2667(22)00192-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to limitations of ethical approval involving the participants’ data and anonymity but are available from the corresponding author on reasonable request.