Abstract
Background
Stroke is a leading cause of mortality and morbidity. Thus, identifying associated risk factors may lead to earlier interventions aimed at reducing the risk of stroke development. Since cardiovascular disease simultaneously increases the risk of stroke and retinal vein occlusion (RVO), we sought to determine whether RVO is associated with the risk of stroke independent of underlying cardiovascular co-morbidities.
Methods
In this cross-sectional study, we reviewed the records of 80,754 individuals who were evaluated by an ophthalmologist over a 6-year period. We identified individuals with RVO, stroke and cardiovascular diseases including hypertension, diabetes mellitus, carotid disease, coronary artery disease and atrial fibrillation. Multivariable logistic regression models were used to analyze odds ratios for RVO and stroke.
Results
After adjusting for age, sex, cardiovascular disease and other risk factors, we found that the presence of RVO was associated with an odds ratio for stroke of 1.73 (CI, 1.40–2.12, p < 0.001). The association between RVO and stroke, after adjusting for sex and cardiovascular co-morbidities, was significantly stronger in individuals younger than 50 years of age, with an odds ratio of having a stroke of 3.06 (1.34–6.25, p < 0.001), while the presence of RVO in individuals older than 85 years was not significantly associated with stroke 1.19 (0.77–1.79, p = 0.41).
Conclusions
Our findings demonstrate that RVO is significantly associated with stroke, even after adjusting for underlying cardiovascular co-morbidities. This association was highly significant in younger subjects, while not significant in older individuals.
Subject terms: Retinal diseases, Risk factors, Epidemiology
Introduction
Stroke is one of the leading causes of mortality and morbidity in the world [1]. Consequently, identifying associated risk factors can lead to medical interventions aimed at reducing the risk of stroke development. Cardiovascular disease and its associated risk factors are the most common etiologies inciting strokes [1]. Besides stroke, cardiovascular disease is also associated with the development of vascular occlusions in the retina, including retinal artery or vein occlusions [2–6]. While a significant association between retinal artery occlusions and stroke has been documented [7–9], a similar link between stroke and retinal vein occlusion (RVO) is less well established [10–15]. Since cardiovascular co-morbidities simultaneously increase the risk of stroke and RVO [16], we examined whether RVO is associated with the presence of stroke independent of underlying cardiovascular co-morbidities. An independent association between RVO and stroke would underscore the importance of medical optimization and referral for further workup and evaluation in individuals with RVO, regardless of their underlying cardiovascular co-morbidities.
Materials/subjects and methods
This is a retrospective, cross-sectional study in which we reviewed the records of individuals who were evaluated by an ophthalmologist within our institution between January 2015 and December 2020. We excluded subjects who did not have a documented basic medical evaluation at our institution during this time frame. With these criteria, we identified a total of 80,754 individuals using the University of California San Diego (UCSD) Health’s Epic SlicerDicer, a self-service cohort discovery tool. Utilizing ICD-10 diagnostic codes, we then identified those individuals with a diagnosis of central and branch RVO (ICD-10, H34.81 and H34.83), stroke (I63), cardiovascular disease including coronary artery disease (CAD) (I25), carotid artery stenosis (I65.21, I65.22, I65.23 and I65.29), atrial fibrillation or atrial flutter (AF) (I48), and cardiovascular risk factors including essential hypertension (HTN) (I10), type 2 diabetes mellitus (DM) (E11) and hyperlipidaemia (HLD) (E78). We recorded additional variables including age, sex, and race through chart review.
All statistical analyses were performed using R version 4.0.3 (Vienna, Austria). Multivariable logistic regression models were used to analyze odds ratios for RVO and stroke with 95% confidence intervals. Differences between groups were analyzed with Pearson’s χ2 test for categorical variables and independent t-test for continuous variables. The study adhered to the tenets of the Declaration of Helsinki and was conducted in accordance with the regulations of the Health Insurance Portability and Accountability Act. Institutional Review Board approval was obtained from UCSD.
Results
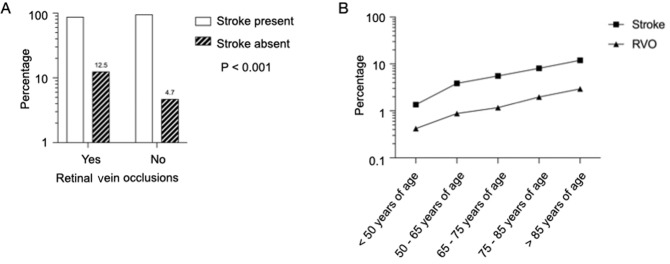
There were 46,506 individuals with at least one cardiovascular disease or cardiovascular disease risk factor, including: HTN (n = 34,354), HLD (n = 32,636), DM (n = 16,943), CAD (n = 12,157), AF (n = 6584), and carotid artery disease (n = 3241). We identified 925 and 3893 individuals with RVO and stroke, respectively. Baseline characteristics of the study population are shown in Table 1. Individuals with RVO were older than those without (71 vs. 59 years of age, p < 0.001), and had higher prevalence of cardiovascular disease (36.2% vs. 20.1%, p < 0.001), cardiovascular risk factors (83.0% vs. 55.5%, p < 0.001) and stroke (12.5% vs. 4.7%, p < 0.001) (Fig. 1A). The percentage of females was higher among individuals without RVO (57.0 vs. 51.1, p < 0.001) (Table 1). The overall prevalence of RVO and stroke was 1.15% and 4.82%, respectively, and increased with age for RVO and stroke as shown in Fig. 1B.
Table 1.
Baseline characteristics of the study cohort.
| RVO present | RVO absent | p value | |
|---|---|---|---|
| N = 925 | N = 79,829 | ||
| Age, years | 71 (16) | 59 (21) | <0.001 |
| Females | 473 (51.1) | 45,519 (57.0) | <0.001 |
| Race | 0.80 | ||
| White | 569 (61.5) | 49,064 (61.5) | |
| Asian | 125 (13.5) | 11,809 (14.8) | |
| Black or African American | 40 (4.3) | 3077 (3.9) | |
| Native Hawaiian or Pacific Islander | 6 (0.6) | 422 (0.5) | |
| American Indian or Alaska Native | 4 (0.4) | 356 (0.4) | |
| Other races | 170 (18.4) | 13,627 (17.1) | |
| Unknown | 35 (3.8) | 3346 (4.2) | |
| Cardiovascular disease | 335 (36.2) | 16,083 (20.1) | <0.001 |
| CAD (12,157) | 241 (26.1) | 11,916 (14.9) | |
| AF (6584) | 149 (16.1) | 6435 (8.1) | |
| Carotid artery disease (3241) | 110 (11.9) | 3131 (3.9) | |
| HTN and cardiovascular risk factors | 768 (83.0) | 44,336 (55.5) | <0.001 |
| HTN (34,354) | 655 (70.8) | 33,699 (42.2) | |
| HLD (32,636) | 543 (58.7) | 32,093 (40.2) | |
| DM (16,943) | 344 (37.2) | 16,599 (20.8) | |
| Stroke | 116 (12.5) | 3777 (4.7) | <0.001 |
Statistically significant p-values are in bold.
Mean and standard deviation reported for age. Frequency and percentage reported for other variables.
CAD coronary artery disease, AF atrial fibrillation, HTN hypertension, HLD hyperlipidaemia, DM diabetes mellitus.
Fig. 1. Frequencies of retinal vein occlusions and stroke.
A Percentage of individuals with stroke in those with and without RVO. Statistical significance tested using χ2. B Percentage of individuals with stroke and RVO across different age groups. RVO retinal vein occlusions.
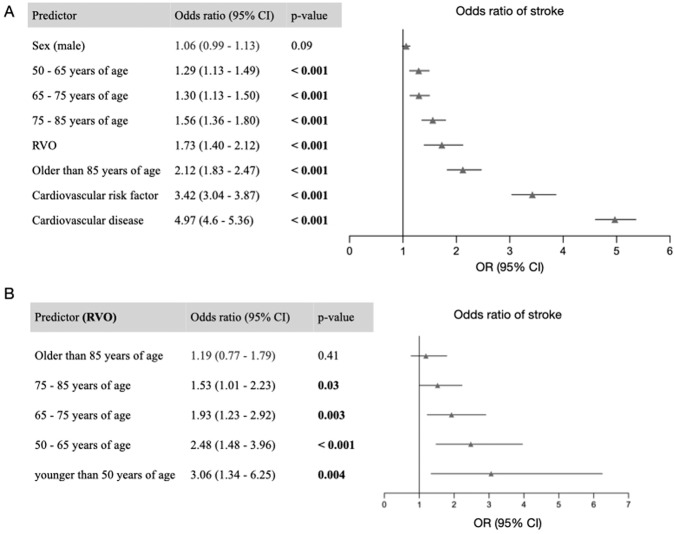
We then asked whether RVO is associated with stroke, independent of underlying cardiovascular disease or risk factors. After adjusting for age, sex, cardiovascular disease and risk factors, we found that the presence of RVO was associated with an odds ratio for stroke of 1.73 (CI, 1.40–2.12, p < 0.001) (Fig. 2A). Because age is known to be an independent risk factor both for RVO and for cardiovascular disease [17, 18], we tested whether age modified the association of RVO with stroke. We identified that there was a significant interaction between age >85 years and RVO (p = 0.01). We then conducted a subgroup analysis in which we evaluated the relationship between RVO and stroke within each age category. The association between RVO and stroke, after adjusting for sex and cardiovascular co-morbidities, was significantly stronger in individuals younger than 50 years of age, with an odds ratio of having a stroke of 3.06 (1.34–6.25, p < 0.001) (Fig. 2B). On the contrary, the presence of RVO among individuals older than 85 years of age was not significantly associated with stroke, with an odds ratio of 1.19 (0.77–1.79, p = 0.41) (Fig. 2B).
Fig. 2. Odds ratio for stroke.
A A multivariable logistic regression model for the presence of stroke. Covariates include RVO, cardiovascular disease, cardiovascular risk factors, age and sex. Reference age group is individuals less than 50 years of age. B Multivariable logistic regression models for the presence of stroke in each age group, using RVO as a predictor, and after adjusting for the same covariates. Error bars represent 95% confidence intervals. RVO retinal vein occlusions.
Discussion
We examined the association between RVO and stroke in a large cross-sectional analysis of individuals who underwent ocular examination over a period of 6 years. The major findings of our study were (1) RVO was significantly associated with stroke independent of underlying cardiovascular co-morbidities, and (2) this association was highly significant in younger individuals, while not significant in those over 85 years of age, after adjusting for confounding variables.
The association between RVO and cardiovascular disease has been examined in different clinical settings, with conflicting findings [10–15]. Ho et al. examined the association between RVO and stroke, in a population-based Taiwanese database, and found no association between RVO and stroke except for in those between 60 and 69 years of age [11]. Similarly, Tsaloumas et al. examined the incidence of stroke in a cohort of 588 individuals who presented with RVO and found no increased incidence of stroke in their RVO cohort compared to the general population [10]. On the other hand, Park et al. found an increased risk of stroke in subjects that presented with incident RVO, which was highest in the 30 days following the event [19]. In addition, a significant association between RVO and stroke was found in large case–control studies identified from national registries (the Korean National Health Insurance Research Database [12], the Taiwanese National Health Insurance Research Database [13], and the Danish national registries [14]), as well as in a systematic review by Woo et al. [20]. These studies had large sample sizes and long follow-up periods, and their results were consistent with ours. However, they did not consistently adjust for all cardiovascular diseases including CAD, AF, and carotid artery disease. Werther et al. examined the association between RVO and stroke, based on the US health care claims database, and found an increased risk of stroke in individuals with RVO, after adjusting for cardiovascular co-morbidities [15]. The odds ratio was 1.72 (1.27–2.34), which is strikingly similar to the results we present here (odds ratio 1.73, 95% CI 1.40–2.12).
Strengths of our study compared to other studies are (1) that we only included individuals who had an ophthalmological evaluation in addition to the general physical exam at a single institution over a 6-year period, (2) that we adjusted for common cardiovascular disease and risk factors in our models, and (3) that we separately analyzed the relationship between RVO and stroke in different age groups. Our findings demonstrate a significant association between RVO and stroke, independent of any underlying cardiovascular disease or cardiovascular risk factors, including CAD, AF, carotid disease, HTN, HLD and DM. Because of the cross-sectional nature of our study, we cannot determine if RVO precedes stroke; however, given the association, presence of RVO, even in the setting of already diagnosed cardiovascular disease, may warrant further evaluation, closer follow-up, and communication with primary care providers regarding optimizing management of existing cardiovascular conditions and risk factors. Interestingly, while the incidence of stroke and RVO was highest in individuals above 85 years of age, there was no significant association between RVO and stroke in this age group, after adjusting for coexisting cardiovascular co-morbidities. Hence, an extensive medical workup may not necessarily be indicated for those who develop RVO in this older age group. We hypothesize that the strength of the association between RVO and stroke may be attenuated in the older age group because older age is an independent risk factor for RVO, stroke and cardiovascular disease [17, 18, 21]. As such, RVO is much more prevalent in older age, and RVO then appears to be less strongly associated with stroke in this population.
Important limitations should be considered while interpreting our findings. This retrospective analysis is based on reported diagnostic ICD-10 codes, and a consistent workup of patients was not performed. It is also likely that the overall prevalence of RVO may have been underestimated, as individuals may have sought out medical care outside of our institution at any point during the 6-year interval. In addition, we only examined the contribution of the most common cardiovascular diseases and risk factors [1] to the development of stroke. Finally, while we demonstrate a strong association between RVO and stroke, because of the retrospective, cross-sectional study design, we cannot infer causality.
In summary, our findings demonstrate that RVO is significantly associated with stroke, and this association is strongest in younger subjects. Therefore, in patients without known cardiovascular disease, the presence of RVO should prompt a clinical workup to optimize medical management with the goal of reducing the subsequent risk of stroke. In patients with an established history of cardiovascular disease, the presence of RVO may indicate the need for stricter treatment goals as well as closer follow-up to mitigate risk for stroke.
Summary
What was known before
Cardiovascular disease is associated with the development of vascular occlusions in the retina, including retinal artery or vein occlusions. It is also associated with an increased risk of cerebrovascular stroke. Whether retinal vein occlusions are associated with stroke independent of underlying cardiovascular disease is unknown.
What this study adds
Our findings demonstrate a significant association between retinal vein occlusion and stroke, independent of underlying cardiovascular disease or cardiovascular risk factors. This association is strongest in younger individuals.
Author contributions
CYB and MFB designed the study. CYB, SM, SM, CKL, FA and MFB acquired and/or analyzed the data. CYB and MFB performed the statistical analysis. All authors participated in the writing and revision of the manuscript.
Funding
CYB is funded by AHA Award 857722 and NIDDK K23 DK129836. MFB is supported by NIH Research Grant P30CA016359 from the National Cancer Institute.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart Disease and Stroke Statistics-2019 Update: a report from the American Heart Association. Circulation. 2019;139:e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 2.Bakhoum MF, Freund KB, Dolz-Marco R, Leong BCS, Baumal CR, Duker JS, et al. Paracentral acute middle maculopathy and the ischemic cascade associated with retinal vascular occlusion. Am J Ophthalmol. 2018;195:143–53. doi: 10.1016/j.ajo.2018.07.031. [DOI] [PubMed] [Google Scholar]
- 3.Chan AX, Bakhoum CY, Bangen KJ, Bakhoum MF. The relationship between retinal vascular occlusions and cognitive dementia in a large cross-sectional cohort. Am J Ophthalmol. 2021;226:201–5. [DOI] [PMC free article] [PubMed]
- 4.Long CP, Chan AX, Bakhoum CY, Toomey CB, Madala S, Garg AK, et al. Prevalence of subclinical retinal ischemia in patients with cardiovascular disease – a hypothesis driven study. EClinicalMedicine. 2021;33:100775. doi: 10.1016/j.eclinm.2021.100775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu CY, Riangwiwat T, Limpruttidham N, Rattanawong P, Rosen RB, Deobhakta A. Association of retinal vein occlusion with cardiovascular events and mortality: a systematic review and meta-analysis. Retina. 2019;39:1635–45. doi: 10.1097/IAE.0000000000002472. [DOI] [PubMed] [Google Scholar]
- 6.Scott IU, Campochiaro PA, Newman NJ, Biousse V. Retinal vascular occlusions. Lancet. 2020;396:1927–40. doi: 10.1016/S0140-6736(20)31559-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mir TA, Arham AZ, Fang W, Alqahtani F, Alkhouli M, Gallo J, et al. Acute vascular ischemic events in patients with central retinal artery occlusion in the United States: a nationwide study 2003-2014. Am J Ophthalmol. 2019;200:179–86. doi: 10.1016/j.ajo.2019.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klein R, Klein BE, Jensen SC, Moss SE, Meuer SM. Retinal emboli and stroke: the Beaver Dam Eye Study. Arch Ophthalmol. 1999;117:1063–8. doi: 10.1001/archopht.117.8.1063. [DOI] [PubMed] [Google Scholar]
- 9.Rim TH, Han J, Choi YS, Hwang SS, Lee CS, Lee SC, et al. Retinal artery occlusion and the risk of stroke development: twelve-year nationwide cohort study. Stroke. 2016;47:376–82. doi: 10.1161/STROKEAHA.115.010828. [DOI] [PubMed] [Google Scholar]
- 10.Tsaloumas MD, Kirwan J, Vinall H, O’Leary MB, Prior P, Kritzinger EE, et al. Nine year follow-up study of morbidity and mortality in retinal vein occlusion. Eye (Lond) 2000;14(Pt6):821–7. doi: 10.1038/eye.2000.230. [DOI] [PubMed] [Google Scholar]
- 11.Ho JD, Liou SW, Lin HC. Retinal vein occlusion and the risk of stroke development: a five-year follow-up study. Am J Ophthalmol. 2009;147:283–90.e282. doi: 10.1016/j.ajo.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 12.Rim TH, Kim DW, Han JS, Chung EJ. Retinal vein occlusion and the risk of stroke development: a 9-year nationwide population-based study. Ophthalmology. 2015;122:1187–94. doi: 10.1016/j.ophtha.2015.01.020. [DOI] [PubMed] [Google Scholar]
- 13.Chen YY, Yen YF, Lin JX, Feng SC, Wei LC, Lai YJ, et al. Risk of ischemic stroke, hemorrhagic stroke, and all-cause mortality in retinal vein occlusion: a nationwide population-based cohort study. J Ophthalmol. 2018;2018:8629429. doi: 10.1155/2018/8629429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bertelsen M, Linneberg A, Rosenberg T, Christoffersen N, Vorum H, Gade E, et al. Comorbidity in patients with branch retinal vein occlusion: case-control study. BMJ. 2012;345:e7885. doi: 10.1136/bmj.e7885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Werther W, Chu L, Holekamp N, Do DV, Rubio RG. Myocardial infarction and cerebrovascular accident in patients with retinal vein occlusion. Arch Ophthalmol. 2011;129:326–31. doi: 10.1001/archophthalmol.2011.2. [DOI] [PubMed] [Google Scholar]
- 16.Ponto KA, Scharrer I, Binder H, Korb C, Rosner AK, Ehlers TO, et al. Hypertension and multiple cardiovascular risk factors increase the risk for retinal vein occlusions: results from the Gutenberg Retinal Vein Occlusion Study. J Hypertens. 2019;37:1372–83. doi: 10.1097/HJH.0000000000002057. [DOI] [PubMed] [Google Scholar]
- 17.Barnett EM, Fantin A, Wilson BS, Kass MA, Gordon MO. The incidence of retinal vein occlusion in the ocular hypertension treatment study. Ophthalmology. 2010;117:484–8. doi: 10.1016/j.ophtha.2009.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.North BJ, Sinclair DA. The intersection between aging and cardiovascular disease. Circ Res. 2012;110:1097–108. doi: 10.1161/CIRCRESAHA.111.246876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park SJ, Choi N-K, Yang BR, Park KH, Woo SJ. Risk of stroke in retinal vein occlusion. Neurology. 2015;85:1578–84. doi: 10.1212/WNL.0000000000002085. [DOI] [PubMed] [Google Scholar]
- 20.Woo SCY, Lip GYH, Lip PL. Associations of retinal artery occlusion and retinal vein occlusion to mortality, stroke, and myocardial infarction: a systematic review. Eye. 2016;30:1031–8. doi: 10.1038/eye.2016.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yousufuddin M, Young N. Aging and ischemic stroke. Aging (Albany NY) 2019;11:2542–4. doi: 10.18632/aging.101931. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.