Abstract
Introduction
The rapid spread of COVID-19 poses a significant threat to nurses’ lives and health, resulting in varying degrees of mental distress. Nurses may experience compassion fatigue, and their professional quality of life and satisfaction may suffer as a result. Their coping mechanisms may vary as well, influencing their compassionate and safe care.
Objectives
The study's objectives are to explore levels of compassion satisfaction and fatigue among nurses and identify their coping strategies. Further, to investigate the relationship between coping strategies, compassion satisfaction, and compassion fatigue during the COVID-19 pandemic.
Methods
Using a descriptive correlational design, this study was conducted with a convenience sample of 443 nurses working in an Egyptian university hospital. Nurses completed the coping strategy indicator scale and the professional quality of life (compassion satisfaction and compassion fatigue) scale. The data were analyzed using descriptive statistics, Pearson correlation, and regression analysis.
Results
Nurses’ professional quality of life was average in terms of compassion satisfaction (2.95 ± 0.92) and compassion fatigue (2.38 ± 0.35). Nurses have a moderate use of coping strategies (2.13 ± 0.35). Problem-solving was rated as the highest coping strategy, while avoidance was rated as the lowest. Coping strategies showed a positive correlation with compassion satisfaction (r = 0.503, p < .001) and a negative correlation with compassion fatigue (r = −0.352, p < .001). In addition, coping strategies could predict 25.4% and 12.4% of compassion satisfaction and compassion fatigue, respectively (p < .001).
Conclusion
Compassion satisfaction and fatigue are key determinants of nurses’ quality of work life. Coping strategies, especially problem-solving and support systems, are vital to increase compassion satisfaction and mitigate burnout and secondary stress syndrome. Nurse managers should establish supportive work environments that promote nurses’ well-being. Resilience-building programs and coping strategies’ training are recommended to enhance the nurses’ quality of work life and positive work attitudes.
Keywords: burnout, coping strategies, COVID-19, compassion satisfaction, compassion fatigue, nurses, quality of life, secondary traumatic stress
Introduction
Nursing is a discipline marked by its humanistic aspect and distinctive caring services. Uniquely and therapeutically, nurses interact with their patients and their families. Nonetheless, the closer nurses become to their patients while providing care, the more things change when an unexpected event takes place. Nurses’ emotional and cognitive reactions to unexpected health events could be affected (Al Barmawi et al., 2019; Duarte et al., 2016). Recently, the coronavirus pandemic (COVID-19) emerged as the world's most important public health issue in 2019 (Rothan & Byrareddy, 2020). This unique viral virus does not discriminate between countries, socioeconomic status, or race and has spread to nearly every country globally, affecting the general population's quality of life (Lai, Wang, et al., 2020). The disease's severity and high fatality rates cause patients to suffer indefinitely, demanding hospitalization and comprehensive care (Baud et al., 2020). In such circumstances, healthcare workers, particularly nurses, play a critical role in public health and must continue working directly with the virus, becoming among the most vulnerable groups to the pandemic.
The psychological charge of uncertainty about the magnitude of the epidemic, the lack of proven therapies or a vaccine, and a paucity of healthcare supplies, particularly personal protective equipment, puts nurses at high risk of infection (Liu, Luo, et al., 2020). As a result, nurses manage limited resources while putting their physical and emotional health at risk and balancing the needs of patients with those of their own families (Lai, Ma, et al., 2020; Wu et al., 2020). They have been recognized as a high-risk group for altering their Professional Quality of Life (ProQOL; Zhang et al., 2018; Kang et al., 2020). Because nurses are exposed to these stressful events, they might develop compassion fatigue (CF), which could make their work life worse (Cieslak et al., 2014; Li et al., 2022). Therefore, it is critical to explore the level of nurses’ compassion satisfaction (CS) and CF and identify how they relate to their coping strategies. This investigation might help in the identification of the strategies needed for increasing nurses’ well-being and productivity, retaining positions within nursing, and, most importantly, promoting the provision of safe and quality care.
Review of Literature
Conceptual Framework and Theoretical Premises
This study was guided by two conceptualizations: ProQOL (Stamm, 2012) and coping strategies (Amirkhan, 1990). According to Stamm's theoretical model of ProQOL (Stamm, 2012), ProQOL refers to how individuals feel about their work as assistants and helpers. Individuals working in the helping professions, such as nurses, may be called upon to respond to personal, public, national, and even international emergencies. The overall concept of ProQOL includes two aspects: CS is a positive aspect, whereas CF is a negative aspect. Both these positive and destructive features of the job influence the ProQOL, and both might be facilitated or inhibited by an individual's personal characteristics, work-related factors, and multiple psychosocial factors (Lai, Wang, et al., 2022).
Specifically, CS is a state of pleasure and the feeling of self-appreciation from one's employment. Compassion satisfaction is considered a protective element and a beneficial aspect of being a nurse, as it is linked to a proclivity to give attention and care to suffer patients (Stamm, 2012; Zhang et al., 2018). While CF describes the charge of caring for others or their emotional distress, which arises from a wish to ignore others’ suffering. Compassion fatigue is a consequence of the emotional demands of constant exposure to human suffering, and it includes two aspects: burnout and secondary traumatic stress, which can occur concurrently or separately (Stamm, 2012). Burnout is characterized by emotional weariness, depersonalization, and a lack of personal fulfillment at work because of prolonged exposure to professional pressures. Burnout stems from a work environment, not a patient care episode, and causes exhaustion, frustration, and anger. While secondary traumatic stress is a bad emotion that is fueled by fear and work-related trauma (Stamm, 2012; Ruiz-Fernández et al., 2020). Stamm used these conceptual definitions as the basis for the development of the ProQOL tool, one of the most used tools for measuring CS and CF, especially among nurses. Previous research discovered that CS was a protective factor against CF, and nurses reported that high CS was associated with low CF (Ruiz-Fernández et al., 2020; Al Barmawi et al., 2019).
The second conceptualization in the current study is related to coping strategies (Amirkhan, 1990). In his model, Amirkhan (1990) combines the best of deductive and inductive approaches to the study of coping to isolate a few fundamental strategies with wide applicability. His middle-ground approach succeeded in identifying three strategies that seem to correspond to the most basic of human reactions to threat and stress: problem-solving, social support, and avoidance.
Problem-solving as a strategy seems derivative of “fight” tendencies. As a result of engaging in problem-focused coping activities, people regard challenges as chances for advantage or gain, believe that problems can be handled, and believe that they could successfully deal with them (Maghan, 2017). So, it involves an instrumental, problem-oriented approach to the active management of stressors. The strategy of seeking social support seems to tap a primal need for human contact in times of duress and manifests through a process of actively turning to others for comfort, help, and advice. Individuals can obtain various social support measures through their social relations with other people, groups, and the greater community (Huang et al., 2020). Avoidance comprising escape responses seems derivative of “flight” tendencies involving physical and/or psychological withdrawal, for example, through distraction or fantasy. Avoidant coping is a defensive strategy that involves ignoring, misrepresenting, or retreating from potentially dangerous stimuli. Because of concerns about COVID-19, nurses might delay or forgo critical emergency and routine medical care (Czeisler et al., 2020). Based on Amirkhan's (1990) conceptualization, one of the study's aims is to investigate coping strategies among nurses.
The Relationship Between Coping Strategies, CS, and CF
COVID-19 has not only changed how nurses feel but it has also changed how they cope with stressors around them. Previous studies pointed to the relationship that could exist between different coping strategies and nurses’ professional quality and reported on how these coping strategies can reduce CF and increase CS directly or indirectly among nurses. For instance, Al Barmawi et al. (2019) found that problem-solving, social support, and avoidance coping strategies enable nurses to deal with CF and reduce their secondary stress syndrome. Also, Upton (2018) referred to problem-solving and social support as effective coping mechanisms against nurses’ CF. Likewise, in a systematic review done by Ames et al. (2017), they reported that positive nurses’ social connections and support, self-regulation, mindfulness, problem-solving, and practicing resilience are among the effective strategies that reduce CF. Recently, Li et al. (2022) found that coping strategies are among the factors that can affect CS and CF during COVID-19. Therefore, there is a continuous need for research investigating and suggesting interventions and coping strategies that mitigate or prevent the effect of CF and stressors that repetitively challenge nurses in all settings (Kelly et al., 2015).
Research Hypotheses
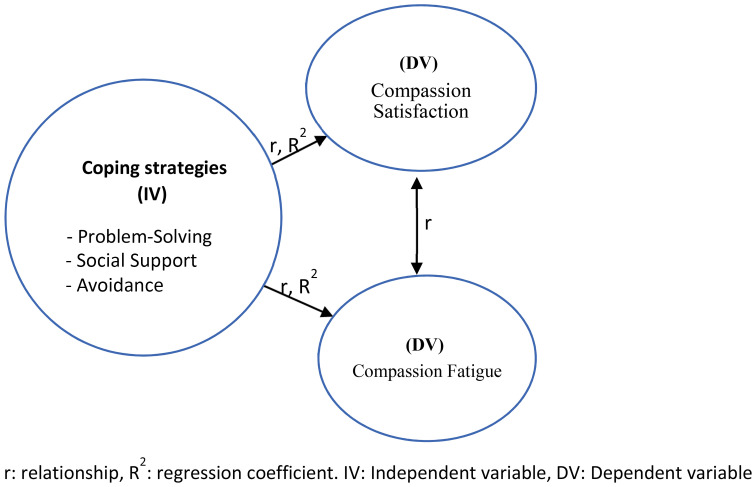
Based on previous conceptualizations, the researchers are interested in investigating CS, CF, and coping strategies among nurses and how they relate to each other. Thus, the following hypotheses were postulated: (see Figure 1).
H1 (1): Nurses have an average perception of their compassion satisfaction, compassion fatigue and coping strategies during the COVID-19 pandemic.
Figure 1.
Conceptual model of the study.
H1 (2): There is a significant relationship between coping strategies and each of compassion satisfaction and compassion fatigue. Coping strategies have a predictive power in this relationship.
Significance of the Study
Compared to other healthcare providers, nurses are often at the frontlines of patient care and witness the pain and suffering of patients in their daily work, in addition to the excessive workload, shift rotation, and work setting (Ruiz-Fernández et al., 2020; Sinclair et al., 2017). Thus, they are more vulnerable to CF than other healthcare workers. The levels of CS and CF have been measured in previous studies, either individually or in relation to other variables among nurses, which revealed spread and variability in the reported level according to working units, nurses’ characteristics, and work environment (Ruiz-Fernández et al., 2020; Salimi et al., 2020; Alharbi et al., 2020; Zhang et al., 2018; Flarity et al., 2016; Hunsaker et al., 2015; Kelly et al., 2015; Kim & Yom, 2014). As nurses develop CF, it is expected that their lives, decisions, and inappropriate responses will be influenced, potentially resulting in more sick leave, putting patient safety at risk, increasing adverse events, poor caring relationships, decreasing quality of care, and increasing job dissatisfaction (Fernandez et al., 2020). Moreover, nurses who are currently caring for COVID-19 patients or might care for them in the future are more likely to have poor mental health and need effective ways to deal with their situation (Lai, Ma, et al., 2020) and improve or maintain their ProQOL (Ruiz-Fernández et al., 2020).
Therefore, increased attention to nurses’ CS and fatigue and how they cope with CF is required to avoid such negative outcomes. Individuals with practical coping abilities and methods will be better able to manage stressful situations and reduce negative sentiments. However, the link between emotional responses and coping strategies is not always clear or consistent (Huang et al., 2020). Limited studies were conducted to examine the direct relationship between CS and CF in relation to coping strategies (Al Barmawi et al., 2019; Alharbi et al., 2020), especially during the COVID-19 pandemic. More research is needed to understand the association between nurses’ coping methods and emotional responses during a serious infectious epidemic like COVID-19.
With these premises in mind, researchers believe it is critical to measure nurses’ ProQOL in the contemporary emergency environment. To the best of the researchers’ knowledge, no study has examined CS and CF in relation to coping strategies among Egyptian nurses. Understanding CS and CF as experienced by nurses will provide insights for nurse leaders to identify and respond to nurses at risk of or experiencing CF. The aim of this study is to fill in the gaps in research and shed light on coping strategies that reducing CF and increasing CS among nurses and provide structure for best practice guidelines for nurse leaders in a variety of practice areas. Nurses will be better supported if leaders and decision-makers are made aware of these concerns and given guidance and implications when needed.
Objectives of the Study
The study's objectives are two-fold:
To explore levels of CS and fatigue among nurses and identify their coping strategies.
To investigate the relationship between coping strategies, CS, and CF during the Covid-19 pandemic.
Methods
Research Design and Setting
A descriptive correlational study design was conducted in all inpatient medical, surgical, and critical care units at a large, urban Egyptian University Hospital. It serves as a general and teaching hospital, furnished with 1825 inpatient beds and providing multispecialty health services.
Research Questions
To achieve the study's objectives, the following research questions are suggested:
What is the level of nurses’ CS, CF, and coping strategies during the COVID-19 pandemic?
What is the relationship between nurses’ coping strategies and each of CS and CF?
Sample and Inclusion/Exclusion Criteria
The study participants included a convenience sample of all staff nurses working in the previously mentioned units. Inclusion criteria for participation are working at least 8 h per week in an acute medical care hospital ward and having at least six months of working experience (N = 443). Exclusion criteria include newly hired nurses, intern nurses, and nursing students, as well as those who are unwilling to respond to the questionnaires. The Epi-Info program was used to determine the sample, which was based on the following parameters: total population of staff nurses (N = 724), acceptable error = 5%, expected frequency 50%, confidence coefficient at 95%, and significance level of 0.05. Thus, the minimum recommended sample size is 252, which is reached and exceeded in the current study (N = 443). There were 171 nurses in surgical care units, 141 in medical care units, and 131 in critical care units.
Study Instruments
Demographic Questionnaire
The researchers created a form that asks about nurses’ demographics and occupational characteristics, such as (gender, age, working unit, educational level, work experience, working shift, and shift hours).
Professional Quality of Life (ProQol) Scale
The ProQol Scale, version 5 (Stamm, 2012), a 30-item scale, was used to assess nurses’ ProQOL in terms of CS and CF. It is divided into three dimensions: CS, burnout, and secondary traumatic stress The two later dimensions measured CF. Each dimension is made up of 10 items. The responses were scored on a five-point Likert scale, with “1” being strongly disagree and “5” being strongly agree. Negative statements received a reversed score. The overall score ranged from 30 to 150, with low (a score of 22 or less), moderate (between 23 and 41), and high (a score of more than 42).
Coping Strategy Indicator
The coping strategy indicator (CSI) questionnaire, developed by Amirkhan (1990), was used to assess the coping methods of registered nurses. It included three subcategories: social support, problem-solving, and avoidance, with 11 items included in each method. Responses ranged from “not at all” to “a little” to “a lot” on a subscales of 1–3. The overall scorer has a range of 33–99, and the three subscales have a range of 11–33.
For Validity and Reliability, an expert panel of five academics from Alexandria University's Faculty of Nursing was tasked with reviewing and testing the content validity of the two adapted and translated tools. To ensure the study's validity, their recommendations are considered. The Cronbach's alpha coefficient test was also used to determine the internal consistency of study instruments. The ProQOL and the CSI measures were both reliable at a statistical significance level of p = .05, with the ProQOL scale = 0.89 and the CSI = 0.992. A pilot study with 45 nurses was conducted by the researchers that require simple clarification from researchers, but no changes were required in the items.
Approvals, Informed Consent, and Data Collection
The ethics committee at Alexandria University's Faculty of Nursing approved the study (June 2021). The researchers distributed the questionnaire to nurses who agreed to participate in the study after receiving official approval from the Faculty of Nursing and the hospital and nursing directors at Alexandria Main university hospital. The researchers informed all participants about the study's objectives and made it clear to the participants that they had the option of withdrawing from the study at any time. Participants were given their signed informed consent to participate in the study, and the researchers ensured data privacy and confidentiality. Data were collected with the permission of units’ nurse managers during the agreed-upon break time. Each nurse spent 30 min completing the questionnaire after obtaining detailed instructions. The data were gathered over three months, from December 2021 to February 2022.
Data Analysis
The data were coded and imported into IBM SPSS version 25. The normality of the data was checked. To describe the demographic variables, the researchers utilized frequencies and percentages, descriptive statistics (means and standard deviation) to summarize the findings, and Pearson correlation coefficient analysis (r) to examine the association between the study variables. The researchers also used regression analysis (R2) to assess whether the independent variable (coping strategies) might predict the dependent variables (CS and CF). With an alpha of 0.05, all statistical analyses were conducted.
Results
Nurses’ Characteristics
There were 443 nurses involved in the research. More than 80% of the participants were female, with an average age of 35.42 (SD = 9.81) and a range of 20 to 55 years old. Surgical units accounted for 38.6% of the total nurses, medical units 31.8%, and acute care units accounted for 29.6%. About 40.0% of nurses (39.7%) had a high school diploma, while 35.4% had a bachelor's degree in nursing. Nurses had an average of 11.40 (SD = 9.78) years of experience, and slightly more than half (51.7%) worked rotating shifts for 38.12 (SD = 2.76) hours per week. More demographic data can be found in Table 1.
Table 1.
Nurses’ Demographic Characteristics (N = 443).
| Demographics | No. | % |
|---|---|---|
| Gender | ||
| Male | 88 | 19.9 |
| Female | 355 | 80.1 |
| Age (years) | ||
| Less than 30 years | 199 | 44.9 |
| From 30–40 years | 110 | 24.8 |
| From 40–50 years | 90 | 20.3 |
| More than 50 years | 44 | 9.9 |
| Mean ± SD. | 35.42 ± 9.81 | |
| Unit | ||
| Medical | 141 | 31.8 |
| Surgical | 171 | 38.6 |
| ICU | 131 | 29.6 |
| Education level | ||
| Bachelor's degree of Nursing | 157 | 35.4 |
| Diploma of Technical Institute | 110 | 24.8 |
| Diploma of Secondary Nursing School | 176 | 39.7 |
| Years of experience in nursing | ||
| Less than 5 years | 200 | 45.1 |
| From 5–10 years | 44 | 9.9 |
| From 11–20 years | 89 | 20.1 |
| More than 20 years | 110 | 24.8 |
| Mean ± SD. | 11.40 ± 9.78 | |
| Working shift | ||
| Morning | 112 | 25.3 |
| Rotating | 229 | 51.7 |
| Night | 102 | 23.0 |
| Working hours/ week | ||
| <36 | 66 | 14.9 |
| 36–40 | 243 | 54.9 |
| ≥40 | 134 | 30.2 |
| Mean ± SD. | 38.12 ± 2.76 | |
SD = standard deviation.
Question 1: What is the Level of Nurses’ CS, CF, and Coping Strategies During the COVID-19 Pandemic?
Regarding nurses’ responses on ProQol Scale, Table 2 showed that the mean score of CS was average (2.95 ± 0.92). Nearly half of the nurses (48.5%) had a moderate level of CS. For CF, the mean score was (2.38 ± 0.35). The highest percentage of nurses (68.8%) scored as having a moderate level (23–41) on the burnout score (2.59 ± 0.36), suggestive of actual or high risk of burnout, whereas most nurses (77.2%) reported having a low level of secondary stress syndrome (2.18 ± 0.39).
Table 2.
Mean Score and Level of Compassion Satisfaction and Compassion Fatigue as Determinants of Nurses’ Professional Quality of Life (N = 443).
| Variables | Mean score* | Score level | |||||
|---|---|---|---|---|---|---|---|
| Low (<23) |
Moderate (23–41) |
High (≥42) |
|||||
| Mean ± SD. | No. | % | No. | % | No. | % | |
| Compassion Satisfaction | 2.95 ± 0.92 | 184 | 41.5 | 215 | 48.5 | 44 | 9.9 |
| Overall Compassion Fatigue | 2.38 ± 0.35 | 178 | 40.2 | 252 | 56.9 | 13 | 2.9 |
| a. Burnout | 2.59 ± 0.36 | 123 | 27.8 | 305 | 68.8 | 15 | 3.4 |
| b. Secondary traumatic stress | 2.18 ± 0.39 | 342 | 77.2 | 88 | 19.9 | 13 | 2.9 |
SD = standard deviation.
*Five-point Likert scale.
For coping strategies, Table 3 revealed that the mean score of coping strategies was on average (2.13 ± 0.35). Nurses reported moderate use of the various strategies of social support (74.5%), problem-solving (79.2%), and avoidance (74.3%). However, the mean scores of problem-solving strategies (2.16 ± 0.42) and social support (2.14 ± 0.39) were slightly higher than the avoidance strategy (2.09 ± 0.34).
Table 3.
Mean Score and Level of Nurses’ Coping Strategies (N = 443).
| Coping strategies* | Mean score out of 3 | Score level | |||||
|---|---|---|---|---|---|---|---|
| Low (<33.3%) |
Moderate (33.3–66.6%) |
High (≥66.6%) |
|||||
| Mean ± SD | No. | % | No. | % | No. | % | |
| Social Support | 2.14 ± 0.39 | 27 | 6.1 | 330 | 74.5 | 86 | 19.4 |
| Problem Solving | 2.16 ± 0.42 | 29 | 6.5 | 351 | 79.2 | 64 | 14.3 |
| Avoidance | 2.09 ± 0.34 | 26 | 5.9 | 329 | 74.3 | 66 | 14.9 |
| Overall Coping Strategies | 2.13 ± 0.35 | 24 | 5.4 | 330 | 74.5 | 89 | 20.1 |
SD = standard deviation.
*Three-point Likert scale.
Question 2: What is the Relationship Between Nurses’ Coping Strategies and Each of CS and CF?
The result showed a significant positive correlation between overall coping strategies and CS (r = 0.503, p = .001). All coping strategies, including problem-solving, social support, and avoidance, showed significant positive correlations with CS (p < .001). On the other hand, the overall coping strategies score was negatively correlated with CF in terms of the overall score (r = −0.352, p = .001), burnout (r = −0.281, p < .001), and secondary traumatic stress (r = −0.368, p < .001). All coping strategies, including problem-solving, social support, and avoidance, showed significant negative correlations with CF and its dimensions of burnout and secondary traumatic stress (p < .001). For the correlation values, see Supplementary Table 1.
In addition, the regression coefficient revealed that overall coping strategies and their related dimensions as independent variables could predict about 25.6% of the positive variance of CS and 12.4% of the negative variance of CF as dependent variables where the regression model is significant (F = 50.264, F = 62.551, p < .001; Table 4).
Table 4.
Multivariate Regression Analysis Among Compassion Satisfaction, Compassion Fatigue, and Coping Strategies.
| Coping strategies with: | B | Beta | t | p | 95% CI | |
|---|---|---|---|---|---|---|
| LL | UL | |||||
| Compassion Satisfaction | 0.654 | 0.503 | 12.238 | <.001* | 0.549 | 0.759 |
| r = 0.503, R2 = 0.256, F = 50.264, p < .001* | ||||||
| Compassion Fatigue | −0.173 | −0.352 | 7.909 | <0.001* | −0.216 | −0.130 |
| r = −0.352, R2 = 0.124, F = 62.551, p < 0.001* | ||||||
B = the coefficient estimates; SE = standard error; t = t-test value; F = F-test; CI = confidence interval; LL = lower limit; UL = upper limit.
r: Pearson correlation coefficient; R2: regression coefficient.
*Statistically significant at p ≤ .5.
Moreover, the result revealed that CS was negatively correlated with CF in terms of the overall score (r = −0.139, p = 0.003), burnout (r = −0.157, p = .001), and secondary traumatic stress (r = −0.103, p = .030). That means that a higher level of CS was related to reduced burnout and secondary traumatic stress. For the correlation values, see Supplementary Table 1.
Discussion
To answer the first research question, this study found that in terms of ProQOL, nurses had an average perception of CS and CF, and they also had an average use of coping strategies. This finding supports the first hypothesis, H.1. Although the average level of CS and CF, most nurses reported having a lower level of secondary stress syndrome. From the researchers’ point of view, this result could be related to nurses’ internal feelings and conflict regarding their perceived important role during the COVID-19 epidemic, yet they could firmly attach to their intrinsic motivation and responsibility to provide nursing care and obtain compassion pleasure by actively connecting with patients, resulting in feeling less stressed. Nurses’ compassion comprises understanding, recognition, emotional timbre, empathy, and tolerance for the suffering of patients and other healthcare professionals, along with motivation and interactive action to cope with stress (Sinclair et al., 2017). Similarly, Chinese nurses and physicians described their COVID-19 experiences as a feeling of obligation to alleviate patients’ pain and a need to work together to defend the country against the virus, according to Liu, Luo, et al. (2020). Our result concurs with Li et al. (2022), who reported that the levels of CS, burnout, and secondary traumatic stress, were moderate to high among Chinese nurses. Also, Ruiz-Fernández et al. (2020) revealed that nurses had high CS scores during the COVID-19 health crisis in Spain. On the other hand, Salimi et al. (2020) found that most respondents who cared for critically ill patients had a moderate or high level of secondary traumatic stress.
On the other hand, the study indicated that the highest percentage of nurses scored moderately on CF and burnout, suggestive of the actual or potential risk of burnout. This score might be related to the great personal suffering and associated personal fear of caring for difficult patients’ cases, fruitless care, work environment pressures, personal experience, isolation measures, families’ worry, and ambiguity during the COVID-19 crisis. All these factors contribute to nurses’ CF (Liu, Luo, et al., 2020). Our finding is consistent with that of Lai, Ma, et al. (2020), who reported greater stress levels, anxiety, depression, and stress among healthcare workers in Wuhan, China's COVID-19 hub. They reported that nurses were worried about the spread of infection to themselves and their families, the increased need for safe treatment, and the possibility of a shortage of critical personal protective equipment. Also, Liu, Yang, et al. (2020) and Trumello et al. (2020) found considerably greater stress levels, burnout, secondary trauma, anxiety, and depression among professionals working with COVID-19 patients.
Concerning the perceived coping strategies during the COVID-19 pandemic, the results of this study showed that nurses used social support, problem-solving, and avoidance of stress approaches in a moderate way. Nonetheless, nurses relied on problem-solving and social support strategies more than avoidance strategy. One reason could be that nurses believe they are advocates for their patients’ problems and needs, and they must be willing to deal with these problems even if it means giving up their own lives to do their jobs. Also, they might ask their friends and family for social support to help them deal with the stress of caring for sick people, staying in touch with their families, and dealing with the effects of a community inquiry. They have no choice but to deal with these stressful things, and to get through this terrible disaster, they must be able to solve problems and make decisions when they are stressed. Congruently, Al Thobaity and Alshammari (2020) stressed the significance of nurses’ multifaceted roles on the frontlines of the COVID-19 struggle and the importance of their problem-solving skills. Similarly, Man et al. (2020) discovered that problem-focused coping tactics were more effective than emotion-focused strategies in controlling the COVID-19 disease, lending support to the current finding. According to Liu, Luo, et al. (2020), in the face of this new disease and its unanticipated repercussions, healthcare personnel tend to prioritize their tasks, stay focused on their jobs, and demonstrate a sense of unity and professional dedication. Likewise, this study underlined the importance of a social support system in the workplace, an additional factor that influences nurses’ ability to deal with stressful situations (Al Barmawi et al., 2019). Moreover, Liu, Luo, et al. (2020) emphasized the need for providing nurses with adequate emotional and social support to enable them to consciously cope with their emotional duties and incorporate passionate care for the patients and their families.
On the other hand, the avoidance approach was reported as having the lowest score among coping strategies. This result could be related to the nature of this approach as a passive coping style. Nurses may rely less on avoidance to manage their work coping because it may lead to increased feelings of stress and anger that could be associated with a failure to manage workload, resulting in burnout. A similar justification was reported by Al Barmawi et al. (2019). Therefore, education and training and organizational support must be ongoing for improving nurses’ resilience and problem-solving strategies to manage stressful issues and increasing their readiness to handle disasters and public health emergencies (Abou Hashish & Banoona, 2022; Abd-El Aliem & Abou Hashish, 2021; Al Thobaity & Alshammari, 2020).
To answer the second question, this study found that coping strategies (overall and dimensions), including problem-solving, social support, and avoidance, showed significant positive correlations with CS. On the other hand, coping strategies (overall and dimensions) showed significant negative correlations with CF and its dimensions of burnout and secondary traumatic stress. These significant associations were supported by the result of regression analysis, where the regression coefficient values revealed that coping strategies as independent variables played a significant role in the positive prediction of CS (25.6%) and the negative prediction of CF (12.4%) as dependent variables. Our result supports Hypothesis 2 and implies that nurses with effective coping strategies might report higher levels of CS and experience less CF. These findings might be justified in that nurses who perceive more support from families, friends, and colleagues might be able to fully concentrate on their work, become confident in addressing their work-related problems and stress, and appropriately release negative emotions, which lead to decreased CF among nurses. This justification aligns with previous studies (Li et al., 2022; Ruiz-Fernández et al., 2021).
In support of these findings, Al Barmawi et al. (2019) found that effective coping strategies were associated with higher levels of CS and the ability to deal with higher levels of CF, burnout, and secondary traumatic stress. They found that high scores on problem-solving, social support avoidance, and coping subscales were also associated with lower CF, burnout, and secondary stress syndrome scores. Also, Shin et al. (2014) did another study that showed that nurses who used both problem-focused and emotion-focused coping strategies felt less emotional fatigue. Hunsaker et al. (2015) found that positive nurse social connections and support may reduce CF and promote CS. Moreover, Li et al. (2022) found a significant negative association between nurses’ coping styles, CF, and both burnout and secondary traumatic stress. They emphasized effective positive coping strategies and concluded that with continued close contact with critically ill and difficult patients, nurses who use passive coping styles may have more stress-related thoughts and feelings, which can hinder effective coping behaviors in their overloaded nursing work. They are also more likely to get tired of helping other people and need more support and attention at work.
Furthermore, in a mixed-methods study, Upton (2018) asked the interviewed nurses about the coping strategies that enable hospital nurses to mitigate the prevalence and levels of CF. Nurses acknowledged that having a realistically helpful thinking style about the quality of nursing care and how to solve related problems were useful coping strategies for the role of the nurse. They also stated that staff support at all levels, particularly for those who have experienced CF, was viewed as a very helpful coping strategy, as well as organizational skills to control stress and CF levels. Likewise, Ames et al. (2017) emphasized on social connections, problem-solving, and practicing resilience as strategies that reduce CF and increase CS in nurses.
Additionally, this study found that CS was negatively correlated with CF, as measured by the total score, burnout, and secondary traumatic stress. The logical assumption that could explain this finding is that CS has been identified as a feature that protects nurses from CF and stressful feelings. Nurses who are compassionately satisfied are better able to provide competent and compassionate care. This result means that higher satisfaction levels suggest a lower risk of CF, burnout, and secondary traumatic stress. This finding aligns with those of Ruiz-Fernández et al. (2020) and Al Barmawi et al. (2019), who found a negative correlation between CS and CF, including burnout and secondary traumatic stress. Also, Pérez-Chacón et al. (2021) showed that nurses’ CS was negatively related to the overall score of CF and its related factors of burnout and secondary traumatic stress.
In summary, to promote their professional quality of work life, increase their CS, and decrease their CF, nurses require continuous training in coping methods and resilience-building to deal effectively with the stressors and challenges they are exposed to. Like previous studies, we emphasize that resilience is another key factor for helping individuals cope with stress or adversity effectively and develop problem-solving skills to recover from negative events (Li et al., 2022). Further investigation is needed in this area. Nurses with an adequate level of resilience usually remain positive and think of work-related traumatic experiences as a normal part of life, which helps them reduce emotional exhaustion, increase job satisfaction, and cope with compassion distress more successfully (Zheng et al., 2021). In the same way, Abd-El Aliem and Abou Hashish (2021) and Abou Hashish (2020) suggested that hospital and nurse managers create and keep a supportive work environment where work climate and leadership styles are factors that make nurses more resilient and committed. Moreover, Al Thobaity and Alshammari (2020) emphasized that nurses must be skilled in problem-solving, decision-making, and crisis management to satisfy patients and their families. This includes medical care, decontamination, isolation, communication, triage, emotional support, and, if needed, palliative care.
Strengths and Limitations
To the best of the author's knowledge, this is the first study to investigate coping strategies in relationship to CS and CF among Egyptian nurses during the COVID-19 pandemic which could pave the way for more future research. Managers, policymakers, and the nursing syndicate could all benefit from the findings in the future. Certain limitations, however, should be addressed in this investigation in relation to sampling and design. The cross-sectional survey makes it difficult to identify the causal relationships between the variables. Another limitation was the data's reliance on self-reports of their perceptions, which may have biased the results. Also, the sample drawn from a single large university hospital is not representative of all Egyptian nurses or the healthcare business and restricts the findings’ generalizability. To overcome this limitation, many implications for future studies are recommended in the implication section.
Implications of the study
Implications for Nursing Practice
In order to deal with the demanding circumstances of COVID-19, managers could make use of these findings to develop an empowering work environment. We recommend focusing on activities that encourage healthier coping mechanisms and implementing a psychological intervention plan with two pillars: (a) resource support, which entails giving nurses the necessary knowledge, supervision, and personal protective equipment; and (b) social and emotional support, which entails improving nurses’ emotional capability to manage stress and burnout.
Effective retention strategies and targeted interventions are needed to decrease CF and promote CS among nurses. Therefore, nurse managers should foster healthy work environments, implement evidence-based programs (such as effective coping strategies, resilience-building, and mindfulness initiatives, as well as gratitude boards), and provide educational opportunities for their staff to help them become more resilient and confident in their work. Increasing the quality of work–life and promoting positive work attitudes among Egyptian nurses is a common recommendation in previous Egyptian studies (Abd-El Aliem & Abou Hashish, 2021; Abou Hashish, 2020; Abou Hashish & Ashour, 2020).
Future Research Implications
Large-scale quantitative studies of nurses’ work–life quality are needed in Egypt and around the world. To better understand the nursing population, future research should include a larger sample of recruited administrators and nurses with probability across different health sectors, which could assist in reducing potential bias from various health sectors. Qualitative studies with in-depth interviews and focus group discussions with nurse managers and nurses from various settings could yield thorough information about their lived experience caring for COVID-19 patients, as well as the underlying challenges and causes of CF. Future research should be conducted to investigate the relationship between resilience and coping strategies of nurses, utilizing a measurable multi-rating evaluation approach such as 360° (peer, subordinate, and boss) and providing diverse samples to confirm the findings of this study. In addition, professional interventions, such as workshops and training programs, are essential for strengthening nurses’ autonomy, support, leadership, and resilience, and they should be supported with evaluations to determine their impact. Likewise, future studies could focus on the work environment and other contextual factors, including leadership, job commitment, and personality characteristics of nurses, as other predictors or variables that could affect nurses’ ProQOL and coping strategies. Finally, further research is needed to assess nurses’ levels of awareness, readiness, and risk perception, as these are significant considerations in the context of epidemics with unknown causes.
Conclusion
Our study provides the baseline assessment knowledge that nurse managers and leaders might need to develop tailored and targeted interventions toward reducing CF and burnout and promoting effective coping strategies in such traumatic events. According to the findings of this study, nurses’ ProQOL was average in terms of CS and CF. Despite this, the majority of nurses reported having a low level of secondary stress syndrome. Nurses also employ moderate coping strategies, which demonstrated considerable predictive value and were linked to higher levels of CS and lower levels of CF. Coping strategies, particularly problem-solving and social support strategies, influence nurses’ CS and CF.
In conclusion, this study disclosed that the participating nurses valued and adhered to their obligations and roles as frontline providers and advocates for passionate patient care, especially during COVID-19. They experience CF if their desire to alleviate suffering exceeds their ability to care for patients. The Egyptian nurses showed a high level of professional dedication and acceptance of the necessity to solve problems, seek social support, and overwork with compassion when caring for COVID-19 patients, despite CF and burnout. Hence, it is vital to provide nurses with comprehensive support to improve their well-being, resilience, preparedness, and crisis management efficacy as recommended in our implications.
Supplemental Material
Supplemental material, sj-docx-1-son-10.1177_23779608231160463 for The Relationship Between Coping Strategies, Compassion Satisfaction, and Compassion Fatigue During the COVID-19 Pandemic by Ebtsam Aly Abou Hashish and Amal Diab Ghanem Atalla in SAGE Open Nursing
Acknowledgments
The authors thank all the nurses who agreed to and completed our questionnaires.
Footnotes
Authors’ Note: All authors have approved the manuscript for submission. We confirm that the content of the manuscript has not been published or submitted for publication elsewhere. The ethics committee at Alexandria University's Faculty of Nursing approved the study (June 2021). The researchers made it clear to the participants that they had the option of withdrawing from the study at any time. Participants given their signed informed consent to participate in the study, and the researchers ensured data privacy and confidentiality. All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Authors’ Contribution: Both authors (Abou Hashish E & Atalla A) have substantial contributions to Conceptualization, Methodology, design; acquisition of data; Software, Data curation, technical, or material support; analysis and interpretation of data; drafting of the manuscript. Abou Hashish, the final manuscript draft and the correspondence. The authors read and approved the final manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ebtsam Aly Abou Hashish https://orcid.org/0000-0003-0492-7615
Supplemental Material: Supplemental material for this article is available online.
References
- Abd-El Aliem S. M. F., Abou Hashish E. A. (2021). The relationship between transformational leadership practices of first-line nurse managers and Nurses’ organizational resilience and job involvement: A structural equation model. Worldviews on Evidence-Based Nursing, 18(5), 273–282. 10.1111/wvn.12535 [DOI] [PubMed] [Google Scholar]
- Abou Hashish E., Banoona R. (2022). Disaster nursing and disaster preparedness: An investigation of nursing students’ knowledge, competence and attitudes. Nursing Management, 30(4), 25–31. 10.7748/nm.2022.e2058 [DOI] [PubMed] [Google Scholar]
- Abou Hashish E. A. (2020). Nurses’ perception of organizational justice and its relationship to their workplace deviance. Nursing Ethics, 27(1), 273–288. 10.1177/0969733019834978 [DOI] [PubMed] [Google Scholar]
- Abou Hashish E. A., Ashour H. (2020). Determinants and mitigating factors of the brain drain among Egyptian nurses: A mixed-methods study. Journal of Research in Nursing, 25(8), 699–719. 10.1177/1744987120940381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Barmawi M. A., Subih M., Salameh O., Sayyah Yousef Sayyah N., Shoqirat N., Abdel-Azeez Eid Abu Jebbeh R. (2019). Coping strategies as moderating factors to compassion fatigue among critical care nurses. Brain and Behavior, 9(4), 1–8. 10.1002/brb3.1264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alharbi J., Jackson D., Usher K. (2020). Personal characteristics, coping strategies, and resilience impact on compassion fatigue in critical care nurses: A cross-sectional study. Nursing & Health Sciences, 22(1), 20–27. 10.1111/nhs.12650 [DOI] [PubMed] [Google Scholar]
- Al Thobaity A., Alshammari F. (2020). Nurses on the frontline against the COVID-19 pandemic: An integrative review. Dubai Medical Journal, 3(3), 87–92. 10.1159/000509361 [DOI] [Google Scholar]
- Ames M., Salmond E., Holly C., Kamienski M. (2017). Strategies that reduce compassion fatigue and increase compassion satisfaction in nurses: A systematic review protocol. JBI Database of Systematic Reviews and Implementation Reports, 15(7), 1800–1804. 10.11124/JBISRIR-2016-003142 [DOI] [PubMed] [Google Scholar]
- Amirkhan J. H. (1990). A factor analytically derived measure of coping: The coping strategy indicator. Journal of Personality and Social Psychology, 59(5), 1066–1074. 10.1037/0022-3514.59.5.1066 [DOI] [Google Scholar]
- Baud D., Qi X., Nielsen-Saines K., Musso D., Pomar L., Favre G. (2020). Real estimates of mortality following COVID-19 infection. The Lancet Infectious Diseases, 20(7), 773. 10.1016/S1473-3099(20)30195-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cieslak R., Shoji K., Douglas A., Melville E., Luszczynska A., Benight C. C. (2014). A meta-analysis of the relationship between job burnout and secondary traumatic stress among workers with indirect exposure to trauma. Psychological Services, 11(1), 75–86. 10.1037/a0033798 [DOI] [PubMed] [Google Scholar]
- Czeisler MÉ, Marynak K., Clarke K. E., Salah Z., Shakya I., Thierry J. M., Howard M. E. (2020). Delay or avoidance of medical care because of COVID-19-related concerns—United States, June 2020. Morbidity and Mortality Weekly Report, 69(36), 1250–1257. 10.15585/mmwr.mm6936a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duarte J., Pinto-Gouveia J., Cruz B. (2016). Relationships between nurses’ empathy, self-compassion and dimensions of professional quality of life: A cross-sectional study. International Journal of Nursing Studies, 60(Aug), 1–11. 10.1016/j.ijnurstu.2016.02.015 [DOI] [PubMed] [Google Scholar]
- Fernandez R., Lord H., Halcomb E., Moxham L., Middleton R., Alananzeh I., Ellwood L. (2020). Implications for COVID-19: A systematic review of nurses’ experiences of working in acute care hospital settings during a respiratory pandemic. International Journal of Nursing Studies, 111(103637), 1–8. 10.1016/j.ijnurstu.2020.103637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flarity K., Nash K., Jones W., Steinbruner D. (2016). Intervening to improve compassion fatigue resiliency in forensic nurses. Advanced Emergency Nursing Journal, 38(2), 147–156. 10.1097/TME.0000000000000101 [DOI] [PubMed] [Google Scholar]
- Huang L., Lei W., Xu F., Liu H., Yu L. (2020). Emotional responses and coping strategies in nurses and nursing students during COVID-19 outbreak: A comparative study. PLoS One, 15(8), 1–12. 10.1371/journal.pone.0237303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunsaker S., Chen H., Maughan D., Heaston S. (2015). Factors that influence the development of compassion fatigue, burnout, and compassion satisfaction in emergency department nurses. Journal of Nursing Scholarship, 47(2), 186–194. 10.1111/jnu.12122 [DOI] [PubMed] [Google Scholar]
- Kang L., Ma S., Chen M., Yang J., Wang Y., Li R., Yao L., Bai H., Cai Z., Xiang Yang B., Hu S., Zhang K., Wang G., Ma C., Liu Z. (2020). Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain, Behavior, and Immunity, 87(2020), 11–17. 10.1016/j.bbi.2020.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly L., Runge J., Spencer C. (2015). Predictors of compassion fatigue and compassion satisfaction in acute care nurses. Journal of Nursing Scholarship, 47(6), 522–528. 10.1111/jnu.12162 [DOI] [PubMed] [Google Scholar]
- Kim H. J., Yom Y. H. (2014). Structural equation modeling on burnout in clinical nurses based on CS-CF model. Journal of Korean Academy of Nursing, 44(3), 259–269. 10.4040/jkan.2014.44.3.259 [DOI] [PubMed] [Google Scholar]
- Lai C.-C., Wang C.-Y., Wang Y.-H., Hsueh S.-C., Ko W.-C., Hsueh P.-R. (2020). Global epidemiology of coronavirus disease 2019 (COVID- 19): Disease incidence, daily cumulative index, mortality, and their association with country healthcare resources and economic status. International Journal of Antimicrobial Agents, 55(4), 1–8. 10.1016/j.ijantimicag.2020.105946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Hu S. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open, 3(3), 1–12. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Wang Q., Guan C., Luo L., Hu X. (2022). Compassion fatigue and compassion satisfaction among Chinese palliative care nurses: A province-wide cross-sectional survey. Journal of Nursing Management, 30(7), 3060–3073. 10.1111/jonm.13708 [DOI] [PubMed] [Google Scholar]
- Liu Q., Luo D., Haase J. E., Guo Q., Wang X. Q., Liu S., Yang B. X. (2020). The experiences of health-care providers during the COVID-19 crisis in China: A qualitative study. The Lancet Global Health, 8(6), e790–e798. 10.1016/S2214-109X(20)30204-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Yang L., Zhang C., Xiang Y. T., Liu Z., Hu S., Zhang B. (2020). Online mental health services in China during the COVID-19 outbreak. The Lancet Psychiatry, 7(4), e17–e18. 10.1016/S2215-0366(20)30077-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maghan M. (2017). Problem solving style and coping strategies: Effects of perceived stress. Creative Education, 8(14), 2332–2351. 10.4236/ce.2017.814160 [DOI] [Google Scholar]
- Man M. A., Toma C., Motoc N. S., Necrelescu O. L., Bondor C. I., Chis A. F., Lesan A., Pop C. M., Todea D. A., Dantes E., Puiu R., Rajnoveanu R. M. (2020). Disease perception and coping with emotional distress during COVID-19 pandemic: A survey among medical staff. International Journal of Environmental Research and Public Health, 17(13), 1–12. 10.3390/ijerph17134899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Chacón M., Chacón A., Borda-Mas M., Avargues-Navarro M. L. (2021). Sensory processing sensitivity and compassion satisfaction as risk/protective factors from burnout and compassion fatigue in healthcare and education professionals. International Journal of Environmental Research and Public Health, 18(2), 611. 10.3390/ijerph18020611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothan H. A., Byrareddy S. N. (2020). The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. Journal of Autoimmunity, 109(102433), 1–5. 10.1016/j.jaut.2020.102433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz-Fernández M. D., Ramos-Pichardo J. D., Ibáñez-Masero O., Cabrera-Troya J., Carmona-Rega M. I., Ortega-Galán ÁM. (2020). Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. Journal of Clinical Nursing, 29(21-22), 4321–4330. 10.1111/jocn.15469 [DOI] [PubMed] [Google Scholar]
- Ruiz-Fernández M. D., Ramos-Pichardo J. D., Ibañez-Masero O., Sánchez-Ruiz M. J., Fernández-Leyva A., Ortega-Galán ÁM. (2021). Perceived health perceived social support an professional quality of life in hospital emergency nurses. International Emergency Nursing, 59(101079), 1–6. 10.1016/j.ienj.2021.101079 [DOI] [PubMed] [Google Scholar]
- Salimi S., Pakpour V., Rahmani A., Wilson M., Feizollahzadeh H. (2020). Compassion satisfaction, burnout, and secondary traumatic stress among critical care nurses in Iran. Journal of Transcultural Nursing, 31(1), 59–66. 10.1177/1043659619838876 [DOI] [PubMed] [Google Scholar]
- Shin H., Park Y. M., Ying J. Y., Kim B., Noh H., Lee S. M. (2014). Relationships between coping strategies and burnout symptoms: A meta-analytic approach. Professional Psychology Research and Practice, 45(1), 44–56. 10.1037/a0035220 [DOI] [Google Scholar]
- Sinclair S., Beamer K., Hack T. F., McClement S., Raffin Bouchal S., Chochinov H. M., Hagen N. A. (2017). Sympathy, empathy, and compassion: A grounded theory study of palliative care patients’ understandings, experiences, and preferences. Palliative Medicine, 31(5), 437–447. 10.1177/0269216316663499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stamm B. H. (2012). Professional quality of life elements theory and measurement. Retrieved November 2021 from https://proqol.org/
- Trumello C., Bramanti S. M., Ballarotto G., Candelori C., Cerniglia L., Cimino S., Babore A. (2020). Psychological adjustment of healthcare workers in Italy during the COVID-19 pandemic: Differences in stress, anxiety, depression, burnout, secondary trauma, and compassion satisfaction between frontline and non-frontline professionals. International Journal of Environmental Research and Public Health, 17(22), 1–13. 10.3390/ijerph17228358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Upton K. V. (2018). An investigation into compassion fatigue and self-compassion in acute medical care hospital nurses: A mixed methods study. Journal of Compassionate Health Care, 5(1), 1–27. https://doi.org/10.1186/s40639-018-0050-x [Google Scholar]
- Wu P. E., Styra R., Gold W. L. (2020). Mitigating the psychological effects of COVID-19 on health care workers. CMAJ : Canadian Medical Association Journal, 192(17), E459–E460. 10.1503/cmaj.200519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y. Y., Han W. L., Qin W., Yin H. X., Zhang C. F., Kong C., Wang Y. L. (2018). Extent of compassion satisfaction, compassion fatigue and burnout in nursing: A meta-analysis. Journal of Nursing Management, 26(7), 810–819. 10.1111/jonm.12589 [DOI] [PubMed] [Google Scholar]
- Zheng R., Guo Q., Chen Z., Ma L., McClement S. (2021). An exploration of the challenges for oncology nurses in providing hospice care in mainland China: A qualitative study. Asia-Pacific Journal of Oncology Nursing, 8(2), 139–146. 10.4103/apjon.apjon_62_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-son-10.1177_23779608231160463 for The Relationship Between Coping Strategies, Compassion Satisfaction, and Compassion Fatigue During the COVID-19 Pandemic by Ebtsam Aly Abou Hashish and Amal Diab Ghanem Atalla in SAGE Open Nursing