Abstract
BACKGROUND:
We aimed to explore the impact of the emergency department length of stay (EDLOS) on the outcome of trauma patients.
METHODS:
A retrospective study was conducted on all trauma patients requiring hospitalization between 2015 and 2019. Patients were categorized into 4 groups based on the EDLOS (<4 h, 4–12 h,12–24 h, and >24 h). Data were analyzed using Chi-square test (categorical variables), Student’s t-test (continuous variables), correlation coefficient, analysis of variance and multivariate logistic regression analysis for identifying predictors of short EDLOS and hospital mortality.
RESULTS:
The study involved 7,026 patients with a mean age of 32.1±15.6 years. One-fifth of patients had a short EDLOS (<4 h) and had higher level trauma team T1 activation (TTA-1), higher Injury Severity Score (ISS), higher shock index (SI), and more head injuries than the other groups (P=0.001). Patients with an EDLOS >24 h were older (P=0.001) and had more comorbidities (P=0.001) and fewer deaths (P=0.001). Multivariate regression analysis showed that the predictors of short EDLOS were female gender, GCS, SI, hemoglobin level, ISS, and blood transfusion. The predictors of mortality were TTA-1 (odds ratio [OR]=4.081, 95%CI: 2.364–7.045), head injury (OR=3.920, 95%CI: 2.413–6.368), blood transfusion (OR=2.773, 95%CI: 1.668–4.609), SI (OR=2.132, 95%CI: 1.364–3.332), ISS (OR=1.077, 95%CI: 1.057–1.096), and age (OR=1.040, 95%CI: 1.026–1.054).
CONCLUSIONS:
Patients with shorter EDLOS had different baseline characteristics and hospital outcomes compared with patients with longer EDLOS. Patients with prolonged EDLOS had better outcomes; however, the burden of prolonged boarding in the ED needs further elaboration.
Keywords: Emergency department, Length of stay, Trauma, Management, Outcomes, Trauma activation criteria
INTRODUCTION
Emergency department (ED) crowding is a global healthcare service issue, because of the imbalance between patient load, ED capacity and availability of in-hospital beds. Notably, the need for patient triage, radiological imaging, laboratory analysis, and multispecialty consultations for polytrauma patients often affects the patient flow in the ED.[1] In addition, a shortage of inpatient as well as intensive care unit (ICU) beds may burden the emergency services with longer ED waiting time before inpatient bed placement, which is referred to as ED boarding.[2] Over the past decade, there has been much concern regarding the ED length of stay (EDLOS) owing to the patient and family satisfaction and, more importantly, the potential impact on patient clinical outcomes.[3-5] Therefore, the EDLOS has been anticipated as a quality indicator and benchmark for emergency healthcare services. Earlier studies have identified detrimental effects of prolonged EDLOS, including higher mortality, prolonged hospital length of stay (HLOS), delayed ED interventions due to limited staffing, medication errors, and higher rates of infection among both trauma and non-trauma patients.[3,4,6-8] The damage control principles described as early identification of life-threatening injuries and prompt treatment should be a priority to improve outcomes in patients with trauma visiting busy EDs. Therefore, the concept of the “golden hour’’ where severely injured patients are transferred and resuscitated in specialized trauma centers, has become an essential part of any robust trauma system. It initiates at the first patient encounter in the field, triage, and resuscitation until arrival in the trauma center/ED for management.[9] The golden hour refers to the initial 60 min post-trauma which is crucial for transferring patients to a trauma center and initiating resuscitation (the 60-minute window to deliver the patient from the point of injury to a hospital capable of managing severe trauma).[10]
The available literature regarding the association of EDLOS and outcomes in trauma patients remains inconsistent and appears to contradict usual expectations of shorter EDLOS being associated with better survival. Some researchers have shown worse outcomes with prolonged EDLOS trauma patients,[6] while others have identified no significant difference in mortality by EDLOS.[5] Many major emergency and level 1 trauma centers have dedicated trauma resuscitation bays within the ED to provide protocol-driven critical care for severely injured patients.[11] However, standardized trauma resuscitation protocols followed in the trauma ICU may not always be instituted in the ED setting. This has been considered a possible explanation for more adverse outcomes in patients with prolonged EDLOS.[6] To our knowledge, only a few investigators have addressed the impact of EDLOS on outcomes in trauma patients. Therefore, the present study aims to explore the clinical characteristics and management based on the EDLOS and to assess the impact of EDLOS on the hospital course and outcomes in a level 1 trauma center. We hypothesized that EDLOS has a substantial impact on patient outcomes following traumatic injury.
METHODS
Study design
We performed a retrospective observational study to analyze all trauma patients who were admitted to the level 1 trauma center at Hamad General Hospital (HGH) from January 2015 to January 2019. All trauma patients (>13 years old) who presented at the ED and required hospitalization were included in the study. Patients who died en-route to the hospital and those who were not admitted were excluded. Also, the study did not include deaths that occurred on arrival at the ED. Data for the relevant study variables were extracted from the Qatar Trauma Registry (QTR) maintained by the HGH Trauma Surgery Section. This database comprised uniform data elements of the prehospital information, details of the injury, demographic and clinical characteristics, diagnoses, and outcomes of all trauma patients. The QTR has internal and external regular validation and is linked to the National Trauma Data Bank (NTDB) and is compliant with the standards of the American College of Surgeons Trauma Quality Improvement Program (ACS-TQIP).
Study settings
The HGH Hamad Trauma Center (HTC) is the only level 1 trauma center for the entire population of Qatar (approximately 2.7 million), with up to 1,800 trauma admissions per year.[11] It is committed to advancing trauma care with the delivery of immediate prehospital care by emergency medical services (EMS) to subsequent in-hospital trauma care. The HTC is located within the ED, which comprises 6 resuscitation bays covered by 19 trauma ICU beds, 7 step-down ICU beds and a 25-bed capacity inpatient trauma ward. Radiology services, including computed tomography (CT) scan imaging, are available within proximity, with portable radiographs available within minutes. The trauma bays are well connected with the trauma ICU and operating rooms to facilitate minimal transfer time. The study included all patients who arrived alive at the trauma unit (TRU), which is a part of the ED that deals with trauma patients who only require hospitalization.
Trauma activation criteria
Figure 1 shows the criteria for trauma triage at our institution. Based on these activation code criteria, trauma patients are classified as trauma team T1 activation (TTA-1), TTA-2, or TTA-3 depending on various clinical and anatomic parameters. In the TTA-1 and TTA-2 categories, patients are managed at the trauma resuscitation bays by the trauma surgeons, while the patients in the TTA-3 category are treated by emergency physicians in the ED or can be in the trauma resuscitation bays. Therefore, the EDLOS for TTA-1 and TTA-2 category patients refers to the time when the patient first presented and managed at the trauma resuscitation bays by the trauma surgeons. On the other hand, EDLOS for TTA-3 category patients is considered from the initial trauma activation or consultation as they are often treated by emergency physicians in the ED and then transferred to the trauma service. The EDLOS mainly depends upon four factors: initial resuscitation, radiological imaging, consultation with other subspecialties, and time spent in transit to the area of disposition (ED boarding). The time in the ED was mostly dependent on the patient’s condition, time for resuscitation and radiological diagnosis. The benchmark time for trauma consultants to attend the TTA-1 is 15 min, with a compliance rate of 88% based on our recent records.
Figure 1.
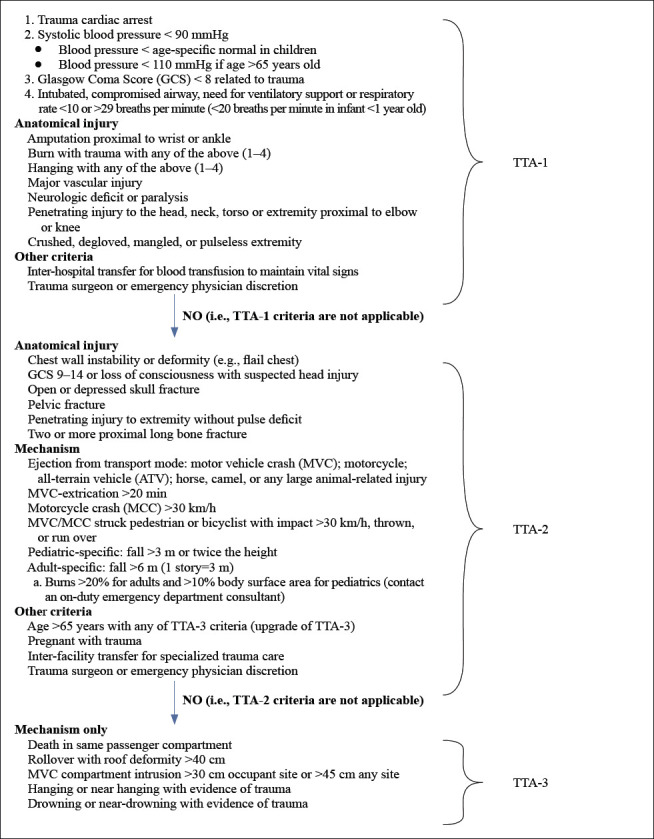
Trauma team activation (TTA) criteria at Hamad medical corporation.
Data collection
Data included demographics (age, gender, nationality), mode of transportation, trauma activation criteria (TTA1–3), EDLOS, disposition, initial vital signs at the scene and upon arrival to the ED, shock index, laboratory and radiological findings, comorbidities, alcohol consumption, Injury Severity Scores (ISS), Trauma Injury Severity Score (TRISS), Revised Trauma Score (RTS), Glasgow Come Score (GCS), Abbreviated Injury Scores (AIS), associated injuries, blood transfusion, ICU and HLOS, ventilatory days, in-hospital complications and mortality. EDLOS includes the time from ED arrival to disposition (admission to ICU, trauma ward, operating room, or discharge). EDLOS was considered “short” if the ED stay was <4 h, in accordance with prior studies.[5]
Outcomes
The primary outcome was all-cause in-hospital mortality, while secondary outcome measures were ICU LOS, hospital LOS, ventilatory days and in-hospital complications.
Statistical analysis
Data are presented as proportions, medians (interquartile range [IQR]), or mean ± standard deviation (SD) as appropriate. Patients were divided into 4 groups based on the EDLOS <4 h, 4–12 h, 12–24 h, and >24 h. Differences in categorical variables were analyzed using the Chi-square test, as appropriate. Yates’ corrected Chi-square test was used for categorical variables if the expected cell frequencies were below 5. The normality of continuous variables was checked using the Kolmogorov-Smirnov test. Continuous variables were compared using Student’s t-test for two groups or ANOVA for more than two groups for parametric data (using Bonferroni correction). The Mann-Whitney U test and Kruskal-Wallis test were used for nonparametric data, as appropriate. The Pearson correlation coefficient (r) was calculated to identify the linear relationship between the EDLOS and other relevant covariates. Multivariate logistic regression analysis was performed for the predictors of mortality using the most relevant covariates such as age, gender, ISS, EMS transportation time, head injury, blood transfusion (any), TTA code, shock index and EDLOS. In another regression analysis model to predict a short EDLOS, we used the following variables: age, gender, ISS, GCS, shock index, blood transfusion, on-admission blood hemoglobin, serum lactate and base deficit. Data were expressed using odds ratios (ORs) and 95% confidence intervals (CIs), A two-tailed P-value <0.05 was considered statistically significant. Data analysis was carried out using the Statistical Package for Social Sciences version 21 (SPSS Inc., USA).
RESULTS
Patient characteristics and disposition
During the study period, 7,438 patients were transported to the trauma unit through the EMS of whom 412 died en-route to the hospital, resulting in 7,026 patients enrolled in the present analysis (Figure 2). The age of the patients was 32.1±15.6 years, and the majority were males (90.3%). Table 1 analyzes the demographics, clinical characteristics and injury severity based on the EDLOS. The overall EDLOS was 10.9±15.4 h, and most (78.3%) had TTA-2 activation. The trauma patients frequently stayed in the ED for 4–12 h (50.7%), followed by <4 h (23.2%), 12–24 h (17.2%) and >24 h (9.0%). The most frequent ED disposition was in the inpatient ward (57.5%), followed by ICU admission (21.7%), operating room (18.6%) and discharged home (2.0%). Fifteen patients (0.2%) were transferred from the ED to the other facilities. Ground ambulance (84.4%) was the most common transportation mode; 9.1% were brought to the ED by helicopter and 6.5% by private vehicle. Those who had shorter EDLOS (<4 h) were significantly younger, primarily males, rapidly transported to the ED with shorter EMS time and were more likely to have TTA-1 compared to the other groups (P=0.001 for all). On the other hand, trauma patients with a TTA-2 were more likely to stay in the ED for 4–12 h and 12–24 h (P=0.001). Also, those with shorter EDLOS (<4 h) were frequently transferred to the operating room (36.5%) or the ICU (32.3%) whereas those who spent more than 4 h were more likely to be transferred to the inpatient trauma wards (P=0.001). Only 2% of the patients were deemed fit to be discharged home from the ED and such patients were more likely to have longer EDLOS (12–24 h and ≥24 h).
Figure 2.
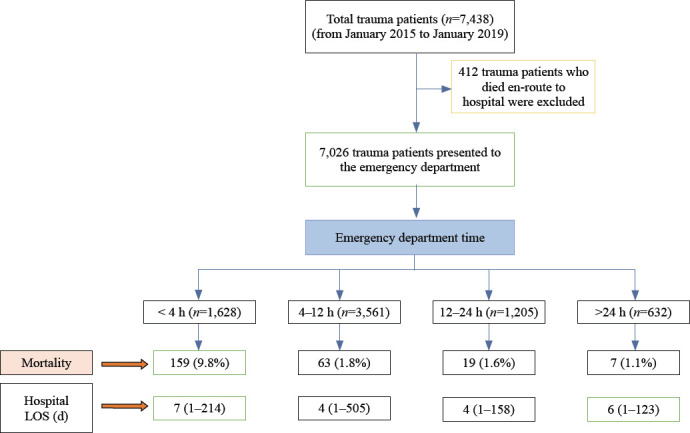
Flow diagram for study design. LOS: hospital length of stay, given as median and interquartile range (IQR).
Table 1.
Patients demographics, clinical characteristics and injury severity based on emergency department length of stay (n=7,026)
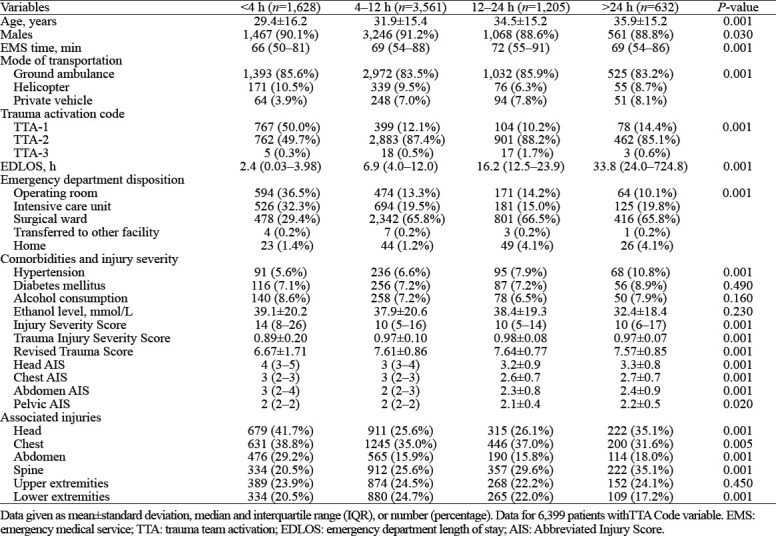
Comorbidities and injury severity
As described in Table 1, the study groups were comparable for the frequency of comorbidities and alcohol consumption except for hypertension, which was significantly higher in the ≥24 h group.
Patients with shorter EDLOS (<4 h) were found to have significantly higher ISS 14 (8–26), head AIS 4 (3–5), chest AIS 3 (2–3), abdominal AIS 3 (2–4), pelvis AIS 2 (2–2) and lower TRISS (0.89±0.20) and RTS scores (6.67±1.71) than the other groups with longer EDLOS. The frequency of head, chest and abdominal injuries was also significantly higher in patients with shorter EDLOS (<4 h), while spinal (>24 h) and lower extremity injuries (4–12 h) were more common in the longer EDLOS group.
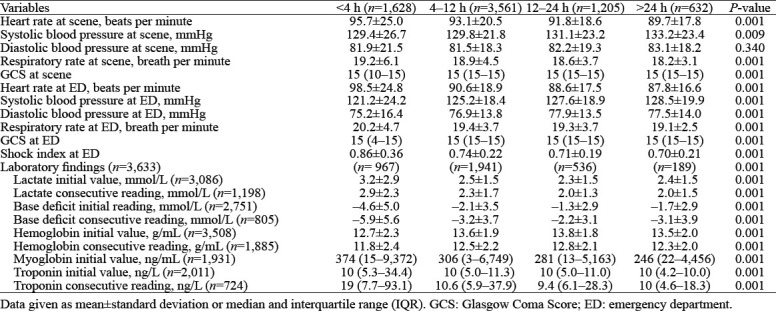
Prehospital and on-admission vital signs and laboratory findings
Table 2 shows the analysis of the initial vital signs and laboratory findings based on EDLOS. The group with shorter EDLOS (<4 h) had higher heart and respiratory rates and lower systolic blood pressure at the scene as well as upon ED admission than the other groups (P=0.001 for all). Also, the shock index at ED was significantly higher in the <4 h group than in the other groups. The laboratory findings revealed significantly elevated levels of serum lactate, base deficit, myoglobin and troponin levels, and lower hemoglobin levels both on initial and follow-up measurements in patients who stayed <4 h in the ED (P=0.001).
Table 2.
Prehospital and on-admission vital signs and laboratory findings based on emergency department length of stay
Hospital complications and mortality
Table 3 demonstrates the complications and outcomes based on the EDLOS. Patients who stayed longer in the ED (>24 h) were more likely to have frequent CT scanning (P=0.001) than those who stayed for a shorter duration. On the other hand, the short-stay group (<4 h) received more blood transfusions with higher median blood units transfused and were more likely to develop pneumonia, sepsis, and ARDS and to have prolonged ICU and hospital LOS (P=0.001 for all). Patients in the 4–12 h and 12–24 h groups required prolonged mechanical ventilation more than the other groups (P=0.04). The overall in-hospital mortality rate was 3.5% (n=248) and this was significantly higher in those who had shorter EDLOS (<4 h) in comparison to other groups (P=0.001). The rate of ICU mortality was significantly higher in the 4–12 h group, whereas mortality in the operating room was more common in the <4 h group (P=0.01).
Table 3.
Complications and outcomes based on emergency department length of stay
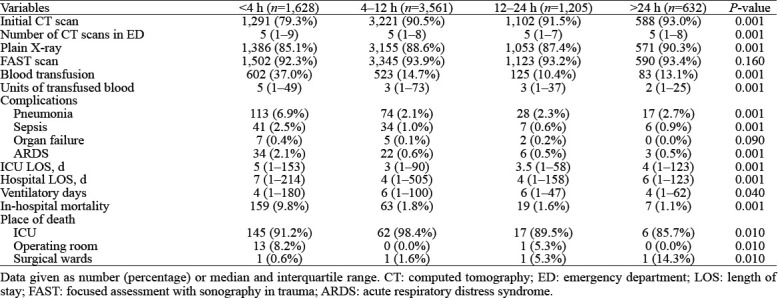
Figure 3 shows that in the first 4 hours, the rate of mortality directly proportionated with the number of hours the patients stayed at the ED, after which the relationship reversed.
Figure 3.
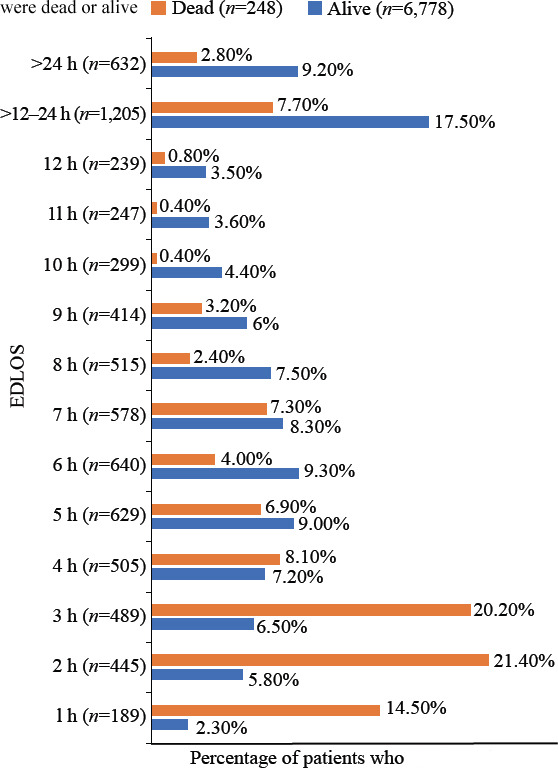
Hospital deaths versus alive in relation to EDLOS (P=0.001). EDLOS: emergency department length of stay.
Bivariate correlation coefficient (supplementary Table 1) demonstrates the significant positive and negative correlations between EDLOS and other relevant parameters. The EDLOS was significantly correlated with patient age (r=0.091), ISS (r=-0.047), GCS at ED (r=0.087), TRISS (r=0.089), RTS (r=0.102), amount of blood transfused (r=-0.137), TTA (r=0.12) and hospital LOS (r=-0.040), P=0.001 for all.
Multivariate logistic regression analysis
Table 4 shows the multivariate analysis for the predictors of shorter EDLOS (<4 h). Female gender (OR=1.670, 95%CI: 1.135–2.463), initial ED GCS (OR=0.853, 95%CI: 0.831–0.876), shock index (OR=1.546, 95%CI: 1.004–2.379), initial hemoglobin (OR=0.922, 95%CI: 0.874–0.973), ISS (OR=1.018, 95%CI: 1.006–1.030), and blood transfusion (OR=1.477, 95%CI: 1.118–1.952), were predictors for short EDLOS.
Table 4.
Predictors of short emergency length of stay (EDLOS <4 h)
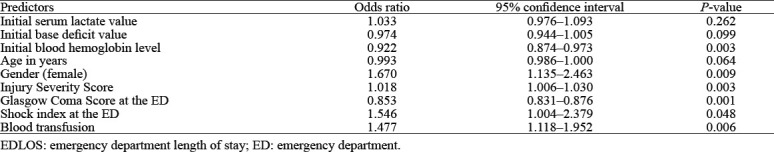
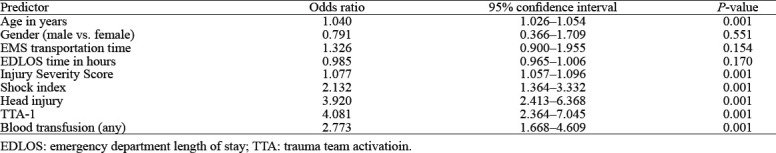
Table 5 shows the multivariate logistic regression analysis for the predictors of mortality after adjusting for the relevant covariates. TTA-1 (OR=4.081, 95%CI: 2.364–7.045; P=0.001), head injury (OR=3.920, 95%CI: 2.413–6.368; P=0.001), blood transfusion (OR=2.773, 95%CI: 1.668–4.609; P=0.001), shock index (OR=2.132, 95%CI: 1.364–3.332; P=0.001), ISS (OR=1.077, 95%CI: 1.057–1.096; P=0.001), and age (OR=1.040, 95%CI: 1.026–1.054; P=0.001) were predictors of hospital mortality. However, gender, EMS transportation time, and EDLOS were not predictors of mortality.
Table 5.
Multivariate regression analysis for the predictors of mortality
DISCUSSION
The present study highlighted the fact that trauma patients with shorter EDLOS (<4 h) had significantly higher ISS and in-hospital complications. Additionally, positive correlations were found between EDLOS and age, GCS, TRISS and RTS, whereas; the amount of blood transfused, and hospital LOS showed a negative correlation. The study identified that a short EDLOS was not an independent predictor of mortality; however, patients with a shorter EDLOS were different at baseline from patients with a long EDLOS. The predictors of a short stay in the ED included female gender, GCS, shock index, blood hemoglobin, ISS, and blood transfusion. Moreover, the rate of mortality directly proportionated with the number of hours the patients stayed at the ED in the first 4 hours, after which an inverse relationship was noted.
With the rising demand for medical services and the parallel development of hospital capacity, ED overcrowding has been a major problem for healthcare systems across the world, resulting in a bottleneck scenario in EDs.[12] Such a situation could potentially translate into poor patient outcomes and decreased physician efficiency.[13] A large retrospective study on 41,256 patients admitted to the ED, considered a short EDLOS to be 2 h and showed an increased risk of mortality from 2.5% to 4.5% and prolonged LOS from 5.6 to 8.7 d in patients with increased boarding time.[4]
Literature pertaining to the EDLOS in trauma patients is limited; however, studies based on ED data have used different cut-off values for a long EDLOS, which between 4 h and 48 h.[14] Other studies have varying cut-off values to define a short EDLOS, ranging from 2 h to 6 h.[3,5,6,15]
In our study, a higher proportion of in-hospital mortality occurred <4 h after ED admission (9.8%). This could be explained by the fact that most patients were severely injured and required blood transfusions, or urgent interventions in the operating room, interventional radiology suite or ICU, which mandated rapid transfer out of the ED resuscitation unit. On the other hand, a relatively smaller proportion of patients who stayed longer in the ED 12–24 h (1.6%) and >24 h (1.1%) died. This could be attributed to the fact that healthcare in the ED is performed by a highly trained and dedicated trauma team. However, this may not be the case in every trauma center, as protocolized intensive care does not always extend to the ED setting (due to the volume of patients and ED logistics) and the monitoring capabilities may also vary. Prolonged EDLOS was not related to worse outcomes, but it would influence the therapy course and resources. Contrary to our findings, an earlier study demonstrated an association between longer EDLOS and higher in-hospital mortality among trauma patients.[6] The authors have analyzed the outcome of 3,973 trauma patients with respect to EDLOS (short EDLOS < 2 h). It was found that patients with a shorter EDLOS had significantly better outcomes in terms of mortality, HLOS and ICU stay. Moreover, in our study, the three groups with an EDLOS > 4 h showed similar rates of mortality with more time spent in the ED as opposed to the findings by Mowery et al,[6] which reported an increase in hospital mortality for each additional hour a trauma patient spends in the ED. Notably, in Mowery’s study[6], the authors excluded patients who required surgical intervention within the first two hours and those who had an EDLOS longer than 5 h. Similar to our findings, Richardson et al[3] demonstrated that patients in the non-delayed group (17%) had a significantly higher mortality rate than those in the delayed group (5.3%). Furthermore, hourly interval assessments revealed no corresponding increase in the mortality rate, supporting our findings. Unlike what we found, Kinney et al[5] studied 1,207 trauma patients and reported no difference in mortality or HLOS between short and long EDLOS. A previous study reported an independent association of older age, high ISS, lower GCS, positive head, chest, and abdominal CT scan and short EDLOS with the worst outcomes.[3] Of note, the older population (≥65 years) in our study represented only 3.5% of the cohort, with a median EDLOS of 8.5 h (IQR 5–17 h). Several studies reported a median EDLOS between 4.7 and 7 h among older populations; however, these studies did not target trauma populations.[16-17]
In our study, patients in the short EDLOS group were more likely to have prolonged ICU and hospital stays, but the duration of mechanical ventilation was longer in those with an EDLOS >12 h. In line with our results, Richardson et al[3] demonstrated a significant increase in the HLOS, and ICU stay among trauma patients with a short EDLOS of approximately three extra days. In contradiction to our findings, Kinney et al[5] showed no association between HLOS and EDLOS. However, there was a significant correlation between HLOS and TRISS; lower TRISS was associated with 2.7 times longer HLOS. This suggests that severely injured patients had a longer HLOS regardless of EDLOS. Also, Becker et al[18] showed no difference in HLOS between the short- and long-EDLOS groups. However, Mowery et al[6] reported significantly shorter HLOS and ICU days in the short EDLOS group. A systematic review of strategies to measure and improve ED performance showed an association between ED performance, types of ED interventions and the measures used to assess the effectiveness of those interventions.[19] The improvement of ED performance could be achieved through the implementation of tailored approaches in a protocolized manner.
In our study, the laboratory findings revealed significantly elevated levels of serum lactate and troponin and lower hemoglobin and base deficit levels in patients with a short EDLOS, indicating the severity of injury and critical status of the patients. A prior study showed that correction of serum lactate can be achieved faster in the trauma unit than in the ED, which reflects more effective resuscitation.[6]
Our findings showed that patients with a short EDLOS were more likely to have abdominal injuries. Based on these findings, definitive care measures should be instituted earlier, resulting in a shorter EDLOS.[18] This highlights the need for a robust triaging system to identify patients who would require more vigorous critical care in an ICU setting or operative intervention and thus facilitate earlier transfer out of the ED.[3,6,20] Also, a well-trained EMS team could rely on the initial vitals at the scene, which could help in the timely triage of patients to either dedicated trauma bays or other areas of the ED.[21] Notably, the HTC has six dedicated trauma bays run by trauma surgeons with easy access to ICUs and operating rooms placed within proximity, which could facilitate early appropriate resuscitation and emergency care.
Study limitations
This study has several limitations due to the retrospective study design and single trauma center experience, which may not be applicable to other ED settings. In addition, we lack breakdown information regarding the time spent in resuscitation, imaging, consultation with other specialties and time spent in transit to the area of disposition which may provide a clearer picture for identifying potential areas of delay. We did not analyze data on the causes of death, as we did not have a routine post-mortem examination. We are unable to comment on ED procedures, the amount of consulting services provided, or care-related issues that may have led to mortality or HLOS. These additional variables may have an impact on EDLOS and may be investigated in future research. Moreover, EDLOS can fluctuate based on temporal factors such as mass gathering events or infectious pandemics. The detailed mechanism of injury was not analyzed in this study; however, blunt trauma constitutes >80% of trauma in Qatar.[22,23] Last, there were inconsistencies among different studies in the definition of EDLOS, limiting the ability to compare and appropriately plan. Most patients in the present study were young and males which is a unique characteristic of trauma victims in our region in the Arab Middle East.[22]
CONCLUSION
This study highlights that those patients with shorter EDLOS have different baseline characteristics compared with those who have prolonged EDLOS and are associated with worse outcomes as such patients were seriously injured and required definitive emergency care. On the other hand, patients with prolonged ED time had better outcomes due to less severe injuries and hemodynamic stability. Therefore, there was no urgency to be transferred to the ICU or operating room, so they were more likely to be boarded in the ED until a bed was available in the wards. Notably, such patients have the potential to increase the burden on the ED in terms of bed availability and the workload on the ED staff. Further larger studies are warranted to establish the importance of rapid triage to facilitate patient disposition in a location that allows the implementation of early, goal-directed trauma resuscitation and management. Moreover, the burden of prolonged EDLOS needs further investigation.
ACKNOWLEDGMENT
We thank all the staff of the trauma registry database at the trauma surgery section and nursing staff (Haris Paikkattummel, Smijith Vadakkumpattu, Motasem Awwad, Ralph Villar, Lionel Tuazon and Muneer Poyil), Department of Surgery, Hamad General Hospital, Doha Qatar.
Footnotes
Funding: This research did not receive any specific grant from any funding agency.
Ethical approval: This study obtained ethical approval from the Research Ethics Committee, at the Medical Research Center, Hamad Medical Corporation (HMC), Doha, Qatar (MRC-01-18-131). Participants are not contacted directly and data were collected anonymously.
Conflicts of interest: This study was presented in part at the 2022 Academic Surgical Congress 1-3 February 2022, Orlando, FL, USA. The authors have no conflicts of interest and no financial issues to disclose.
Author contributions: All authors (AF, AE, MA, AK, KA, BD, SM, AKL, HA and SR) have substantial contributions to the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; and final approval of the version to be published.
All the supplementary files in this paper are available at http://wjem.com.cn.
REFERENCES
- 1.Yarmohammadian MH, Rezaei F, Haghshenas A, Tavakoli N. Overcrowding in emergency departments:a review of strategies to decrease future challenges. J Res Med Sci. 2017;22:23. doi: 10.4103/1735-1995.200277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morley C, Unwin M, Peterson GM, Stankovich J, Kinsman L. Emergency department crowding:a systematic review of causes, consequences and solutions. PLoS One. 2018;13(8):e0203316. doi: 10.1371/journal.pone.0203316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Richardson JD, Franklin G, Santos A, Harbrecht B, Danzl D, Coleman R, et al. Effective triage can ameliorate the deleterious effects of delayed transfer of trauma patients from the emergency department to the ICU. J Am Coll Surg. 2009;208(5):671–8. doi: 10.1016/j.jamcollsurg.2008.11.018. [DOI] [PubMed] [Google Scholar]
- 4.Singer AJ, Thode HC, Jr, Viccellio P, Pines JM. The association between length of emergency department boarding and mortality. Acad Emerg Med. 2011;18(12):1324–9. doi: 10.1111/j.1553-2712.2011.01236.x. [DOI] [PubMed] [Google Scholar]
- 5.Kinney PE, Gursahani K, Armbrecht E, Dalawari P. Does emergency medicine length of stay predict trauma outcomes at a Level 1 Trauma Center? J Hosp Adm. 2015;4(5):1. [Google Scholar]
- 6.Mowery NT, Dougherty SD, Hildreth AN, Holmes JH, 4th, Chang MC, Martin RS, et al. Emergency department length of stay is an independent predictor of hospital mortality in trauma activation patients. J Trauma. 2011;70(6):1317–25. doi: 10.1097/TA.0b013e3182175199. [DOI] [PubMed] [Google Scholar]
- 7.Zhang ZH, Bokhari F, Guo YZ, Goyal H. Prolonged length of stay in the emergency department and increased risk of hospital mortality in patients with sepsis requiring ICU admission. Emerg Med J. 2019;36(2):82–7. doi: 10.1136/emermed-2018-208032. [DOI] [PubMed] [Google Scholar]
- 8.Carr BG, Kaye AJ, Wiebe DJ, Gracias VH, Schwab CW, Reilly PM. Emergency department length of stay:a major risk factor for pneumonia in intubated blunt trauma patients. J Trauma. 2007;63(1):9–12. doi: 10.1097/TA.0b013e31805d8f6b. [DOI] [PubMed] [Google Scholar]
- 9.Sivanandan A, Abhilash KP. Early management of trauma:the golden hour. Curr Med Issues. 2020;18(1):36. [Google Scholar]
- 10.Alarhayem AQ, Myers JG, Dent D, Liao L, Muir M, Mueller D, et al. Time is the enemy:mortality in trauma patients with hemorrhage from torso injury occurs long before the “golden hour”. Am J Surg. 2016;212(6):1101–5. doi: 10.1016/j.amjsurg.2016.08.018. [DOI] [PubMed] [Google Scholar]
- 11.Al-Thani H, El-Menyar A, Asim M, Mollazehi M, Abdelrahman H, Parchani A, et al. Evolution of the Qatar trauma system:the journey from inception to verification. J Emerg Trauma Shock. 2019;12(3):209–17. doi: 10.4103/JETS.JETS_56_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Erenler AK, Akbulut S, Guzel M, Cetinkaya H, Karaca A, Turkoz B, et al. Reasons for overcrowding in the emergency department:experiences and suggestions of an education and research hospital. Turk J Emerg Med. 2016;14(2):59–63. doi: 10.5505/1304.7361.2014.48802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu S, Hobgood C, Brice JH. Impact of critical bed status on emergency department patient flow and overcrowding. Acad Emerg Med. 2003;10(4):382–5. doi: 10.1111/j.1553-2712.2003.tb01353.x. [DOI] [PubMed] [Google Scholar]
- 14.Andersson J, Nordgren L, Cheng I, Nilsson U, Kurland L. Long emergency department length of stay:a concept analysis. Int Emerg Nurs. 2020;53:100930. doi: 10.1016/j.ienj.2020.100930. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed AA, Ibro SA, Melkamu G, Seid SS, Tesfaye T. Length of stay in the emergency department and its associated factors at jimma medical center, southwest Ethiopia. Open Access Emerg Med. 2020;12:227–35. doi: 10.2147/OAEM.S254239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Street M, Considine J, Livingston P, Ottmann G, Kent B. In-reach nursing services improve older patient outcomes and access to emergency care. Australas J Ageing. 2015;34(2):115–20. doi: 10.1111/ajag.12137. [DOI] [PubMed] [Google Scholar]
- 17.Street M, Mohebbi M, Berry D, Cross A, Considine J. Influences on emergency department length of stay for older people. Eur J Emerg Med. 2018;25(4):242–9. doi: 10.1097/MEJ.0000000000000452. [DOI] [PubMed] [Google Scholar]
- 18.Becker A, Segal G, Berlin Y, Hershko D. The emergency department length of stay:is the time running out? Chin J Traumatol. 20191;22(3):125–8. doi: 10.1016/j.cjtee.2019.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Austin EE, Blakely B, Tufanaru C, Selwood A, Braithwaite J, Clay-Williams R. Strategies to measure and improve emergency department performance:a scoping review. Scand J Trauma Resusc Emerg Med. 2020;28(1):55. doi: 10.1186/s13049-020-00749-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen CH, Shin SD, Sun JT, Jamaluddin SF, Tanaka H, Song KJ, et al. Association between prehospital time and outcome of trauma patients in 4 Asian countries:a cross-national, multicenter cohort study. PLoS Med. 2020;17(10):e1003360. doi: 10.1371/journal.pmed.1003360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mermiri M, Mavrovounis G, Chatzis D, Mpoutsikos I, Tsaroucha A, Dova M, et al. Critical emergency medicine and the resuscitative care unit. Acute Crit Care. 2021;36(1):22–8. doi: 10.4266/acc.2020.00521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.El-Menyar A, Mekkodathil A, Asim M, Consunji R, Strandvik G, Peralta R, et al. Maturation process and international accreditation of trauma system in a rapidly developing country. PLoS One. 2020;15(12):e0243658. doi: 10.1371/journal.pone.0243658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Asim M, El-Menyar A, Al-Thani H, Abdelrahman H, Zarour A, Latifi R. Blunt traumatic injury in the Arab Middle Eastern populations. J Emerg Trauma Shock. 2014;7(2):88–96. doi: 10.4103/0974-2700.130878. [DOI] [PMC free article] [PubMed] [Google Scholar]


