Abstract
Objective: Numerous studies have been conducted to predict the prognosis of breast cancers. The effect of glucose transporter protein 1 (GLUT-1), the main carrier protein responsible for glucose transport, was investigated in breast cancer patients.
Material and Method: 170 patients operated for breast carcinoma were included in this study. We analysed the prognostic significance of GLUT-1 immune-expression in 149 patients without neoadjuvant therapy, and in 21 patients with neoadjuvant therapy.
Results: GLUT-1 expression was correlated with poor prognostic factors such as estrogen receptor and progesterone receptor negativity, high Ki-67 proliferation index, and high histological and nuclear grade (p<0.001). GLUT-1 was expressed at a statistically higher rate in invasive ductal carcinomas, compared to invasive lobular carcinomas (p <0.001), and was expressed at a higher rate in luminal B, human epidermal growth factor receptor 2 and triple-negative molecular subtypes compared to luminal A subtype tumors (p <0.001). There was no statistically significant difference between GLUT-1 expression and presence of neoadjuvant therapy. Univariate survival analysis showed high GLUT1 expression was associated with low disease-free survival.
Conclusion: GLUT-1 expression was found to be associated with poor pathological prognostic factors in breast carcinoma patients. The results suggest that GLUT-1 expression can be considered as a prognostic marker in breast cancers, and it may be used as a target molecule in personalized treatment approaches.
Keywords: Breast cancer, Immunohistochemistry, GLUT-1
INTRODUCTION
According to the Globocon 2018 data, breast cancers are the most common cancer in 11 regions worldwide and the first cause of cancer-related deaths in women. Around 2 million new patients and 600,000 deaths were recorded worldwide in 2018 (1).
The most important prognostic factors used in the treatment planning of patients are the TNM staging system and hormone receptor expression profiles (2). A very different prognosis is observed among patients of a similar stage. Therefore, different markers remain the subject of research to identify patients with poor prognosis and to develop new individualized treatment modalities.
Glucose transporter protein 1 (GLUT-1) is the main carrier protein responsible for physiological and pathological glucose transport. The expression of GLUT-1 increases with the effect of hypoxia and decreased oxidative phosphorylation to meet the increasing energy need of tumor cells for proliferation, invasion, and metastasis (3–5).
In our study, we aimed to determine the prognostic significance of GLUT-1 expression in breast cancer patients, the relationship between GLUT-1 expression level and clinicopathological prognostic parameters, and the effect of neoadjuvant therapy on GLUT-1 expression.
MATERIALS and METHODS
Study Design and Case Selection
Patients treated with invasive breast carcinoma with mastectomy +/- axillary lymph node materials operated in our center between January 2017 and April 2020 were retrospectively scanned from the departmental databases. Paraffin blocks, hematoxylin-eosin slides, and immunohistochemical slides (estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER 2), Ki-67) were retrieved from the pathology archives. Patients whose materials could not be found, and whose clinical data could not be reached were excluded from the study. A total of 170 female patients were included in the study.
Mastectomy + axillary lymph node dissection was performed in 154 patients, and simple mastectomy in 16 patients. Neoadjuvant chemotherapy treatment was applied in 21 of the patients.
Two different study groups were formed according to neoadjuvant treatments. The prognostic significance of GLUT-1 expression and its relationship with clinicopathological parameters were evaluated in the main study group of 149 patients who did not receive neoadjuvant therapy. The effect of neoadjuvant therapy on GLUT-1 expression was evaluated in the second study group consisting of 21 patients who received neoadjuvant therapy.
Slides stained with Hematoxylin-eosin and with immu-nohistochemical markers for ER (SP1, Ventana), PR (1E2, Ventana), HER2 (4B5, Ventana), and Ki-67 (30-9, Ventana) were re-evaluated and re-scored by 2 pathologists (O.O., Ç.Ö.). For each case, a paraffin block containing sufficient tumor area was determined to apply GLUT-1 immunohistochemical antibody.
Patient Data
Gender, age, survival time, development of metastasis, and data of recurrence were obtained from the hospital and national electronic databases. In addition, pathological data such as tumor diameter, pathological stage, nuclear grade, histological grade, axillary lymph node metastasis were obtained from the pathology reports.
Outcomes
Disease-free survival is defined as the time to clinical, radiological, or pathological metastasis/recurrence after major surgery or the time to the last follow-up. Unfortunately, we could not analyze overall survival due to the short follow-up period.
Histopathological and Immunohistochemical Staining
A 4 μm section from each formalin-fixed, paraffin-embedded tumor tissue block containing all morphological features of the tumor was selected for the study. Colon carcinoma tissue was added as the positive control, and benign breast parenchyma was designated as the negative control. The Ventana Medical System (SN: 714592, Ref: 750-700 Arizona, USA) automated immunohistochemistry device was used. Immunohistochemical staining was performed using UltraView Universal DAB Detection Kit (REF: 760-500, Ventana), and GLUT1 antibody (PA1-46152, 1/200 diluted, GLUT1 Rabbit Polyclonal Antibody).
The cytoplasmic and membranous staining pattern was accepted as positive staining for the GLUT-1 antibody. Specimens were scored according to the intensity of staining (0- no staining; 1- weak; 2- moderate; 3- strong), and the extent of tumor cells stained (<10% were scored as 0; 10-25% as 1 point; 26-50% as 2 points; and > 50% as 3 points).
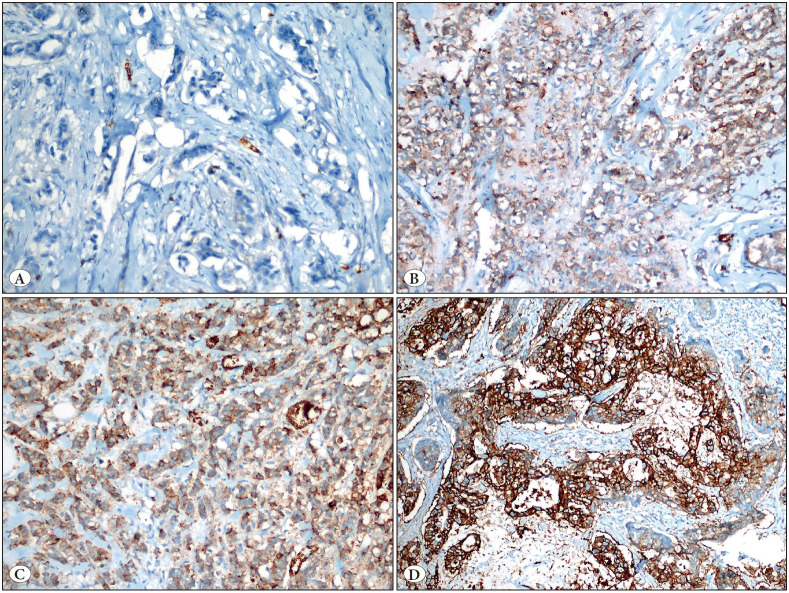
After the evaluation, intensity and extensity scores were summed up for statistical analysis, and > 2 points were accepted as positive while ≤ 2 points were considered as negative GLUT-1 final scores (6) (Figure 1A-D).
Figure 1.
A) No staining with GLUT-1 antibody (GLUT x400), B) Weak intensity of GLUT-1 immunoreactivity (GLUT x200), C) Moderate intensity of GLUT-1 immunoreactivity (GLUT x200), D) Strong intensity of GLUT-1 immunoreactivity in tumor (GLUT x200).
Patients with a staining prevalence of more than 1% for ER and PR were accepted as positive. Patients with complete membranous staining in more than 10% tumor cells for HER 2 were accepted as score 3 (positive), weak to moderate complete membrane staining in more than 10% of tumor cells, or complete membrane staining in less than 10% of tumor cells were accepted as score 2. More than 10% incomplete weak membranous staining and no staining were considered negative (7,8). Since additional studies such as SISH and FISH could not be performed at our center, cases with a HER2 score of 2 were classified as HER2 status unknown. The Ki-67 proliferation index was evaluated in the area where the hot spot staining was observed. A Ki-67 proliferation index ≥14% were considered as high, and <14% were considered as low Ki-67 proliferation index (9).
The patients were divided into surrogate subtypes (luminal A (LA)(ER+, PR+/-, HER2 -, low Ki-67), luminal B (LB)( ER+, PR+/-, HER2+ or ER+, PR+/-, HER2-, high Ki-67) , HER2 (ER-,PR-, HER2+), and triple-negative (TN)( ER-, PR-, HER2-)) according to the ER, PR, HER2, and Ki-67 immunohistochemical marker staining patterns (10,11). All patients were divided into histological types according to the World Health Organization breast cancer classification (11), and graded according to the Nottingham histological grade scoring system (12).
Statistical Analysis
Statistical analysis was performed using SPSS version 21 software. The compliance of numerical variables to a normal distribution was evaluated using the Kolmogorov-Smirnov test and histogram graphics. Continuous variables not conforming to a normal distribution were compared between groups using the Mann-Whitney U test. Whether there was a difference between the groups in terms of categorical variables was evaluated using the Chi-square (Pearson Chi-square, Linear-by-linear association) and Fisher’s Exact tests. Clinicopathological variables predicting disease-free survival was investigated by univariate analyzes using the Log-rank test and Cox regression analysis. Variables with p<0.2 as determined by univariate analyses were selected as covariates, and independent risk factors predicting disease-free survival were analyzed using the backward method Cox regression analysis. Survival rates were calculated by Kaplan-Meier survival analysis. For statistical significance, the p value was set as <0.05.
RESULTS
General Characteristics
The mean age of the 149 patients was 59.4 (range, 31-91). The tumor size was 0.5-14 cm, and the mean tumor diameter was 2.72 cm. 116 of the patients were invasive ductal carcinomas (IDC), 9 were invasive lobular carcinomas (ILC), 5 were mixed (ductal and lobular), and 19 were other types (tubular, mucinous, micropapillary, metaplastic carcinomas) of invasive breast carcinomas. The clinicopathological features of the patients are shown in Table 1.
Table 1.
Association of glucose transporter protein 1 (GLUT-1) expression with clinicopathological parameters in 149 patients who did not receive neoadjuvant therapy.
|
Variables |
GLUT-1 |
|||
|---|---|---|---|---|
|
|
Negative |
Positive |
|
|
|
|
Count (%) |
Count (%) |
p value* |
|
|
Diameter |
<2 cm |
29 (41.4) |
21 (26.6) |
0.13 |
|
2-5 cm |
35 (50) |
52 (65.8) |
|
|
|
> 5 cm |
6 (8.6) |
6 (7.6) |
|
|
|
Molecular surrogate subtypes** |
LA |
48 (70.6) |
17 (21.5) |
<0.001 |
|
LB |
19 (27.9) |
47 (59.5) |
|
|
|
HER 2 |
1 (1.5) |
7 (8.9) |
|
|
|
TN |
0 (0) |
8 (10.1) |
|
|
|
Histologic type |
IDC |
46 (65.7) |
70 (88.6) |
0.005 |
|
ILC |
8 (11.4) |
1 (1.3) |
|
|
|
Mixed |
3 (4.3) |
2 (2.5) |
|
|
|
Others |
13 (18.6) |
6 (7.6) |
|
|
|
Estrogen Receptor |
Negative |
1 (1.4) |
16 (20.3) |
<0.001 |
|
Positive |
69 (98.6) |
63 (79.7) |
|
|
|
Progesterone Receptor |
Negative |
3 (4.3) |
29 (36.7) |
<0.001 |
|
Positive |
67 (95.7) |
50 (63.3) |
|
|
|
Ki-67** |
Low |
53 (75.7) |
16 (21.1) |
<0.001 |
|
High |
17 (24.3) |
60 (78.9) |
|
|
|
HER 2 |
Negative |
59 (84.3)) |
54 (68.4) |
0.004 |
|
Positive |
6 (8.6) |
23 (29.1) |
|
|
|
Unknown |
5 (7.1) |
2 (2.5) |
|
|
|
Nuclear Grade |
1 |
9 (12.9) |
1 (1.3) |
<0.001 |
|
2 |
58 (82.9) |
58 (73.4) |
|
|
|
3 |
3 (4.3) |
20 (25.3) |
|
|
|
Histological Grade |
1 |
12 (17.1) |
1 (1.3) |
<0.001 |
|
2 |
55 (78.6) |
59 (74.7) |
|
|
|
3 |
3 (4.3) |
19 (24.1) |
|
|
|
Angiolymphatic Invasion |
No |
40 (57.1) |
42 (53.2) |
0.626 |
|
Yes |
30 (42.9) |
37 (46.8) |
|
|
|
Perineural Invasion |
No |
47 (67.1) |
56 (70.9) |
0.622 |
|
Yes |
23 (32.9) |
23 (29.1) |
|
|
|
Multicentricity |
No |
54 (77.1) |
70 (88.6) |
0.062 |
|
Yes |
16 (22.9) |
9 (11.4) |
|
|
|
Lymph node metastasis |
No |
36 (57.1) |
35 (47.3) |
0.25 |
|
Yes |
27 (42.9) |
39 (52.7) |
|
|
|
Metastasis |
No |
68 (97.1) |
69 (87.3) |
0.035 |
|
Yes |
2 (2.9) |
10 (12.7) |
|
|
|
Death |
No |
69 (98.6) |
77 (97.5) |
1.000 |
|
Yes |
1 (1.4) |
2 (2.5) |
|
|
* P value below 0.05 is statistically significant
** We had missing data for some variables (3 patients for Ki-67 immunohistochemistry and 2 patients for molecular surrogate subtypes)
*** LA: Luminal A, LB: Luminal B, HER 2: Human epidermal growth factor receptor 2, IDC: Invasive ductal carcinomas, ILC: Invasive lobular carcinoma
GLUT-1 Expression and Clinicopathological Features
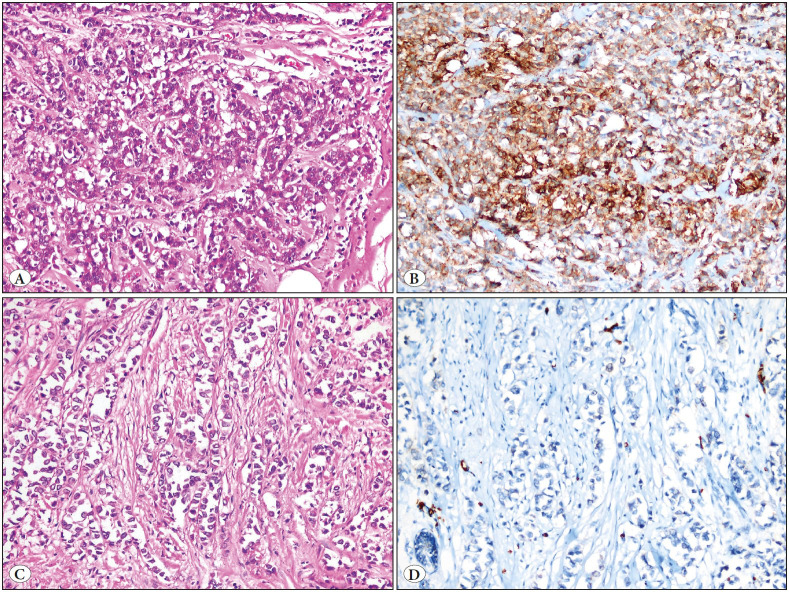
GLUT-1 expression was positive in 53% (79/149) of the patients. According to histological types and molecular surrogate subtypes, GLUT-1 was expressed at a statistically higher rate in IDC patients compared to ILC (p <0.001) (Figure 2A-D). GLUT1 was expressed at a higher rate in Luminal B, HER 2 and triple negative subtypes, compared to the Luminal A subtype cases (p <0.001).
Figure 2.
A) Invasive ductal carcinoma, intermediate nuclear grade (HE x200), B) Strong intensity of GLUT-1 immunoreactivity in invasive ductal carcinoma (GLUT x200), C) Invasive lobular carcinoma (HE x200), D) No staining with GLUT-1 in invasive lobular carcinoma (GLUT x200).
GLUT-1 expression was positively correlated with poor prognostic factors such as ER and PR negativity, high Ki-67 proliferation index, and high histological and nuclear grade (p <0.001) (Table 1).
No statistically significant difference was found between GLUT-1 expression, and presence of neoadjuvant chemotherapy (Table 2).
Table 2.
Glucose transporter protein 1 (GLUT-1) expression rates by neoadjuvant treatment status.
|
|
|
GLUT-1 |
|
|
|
|---|---|---|---|---|---|
|
|
|
Negative |
Positive |
Total |
p value* |
|
Neoadjuvant chemotherapy |
No, n (%) |
70 (47) |
79 (53) |
149 |
0.112 |
|
Yes, n (%) |
6 (28.6) |
15 (71.4) |
21 |
|
|
* P value below 0.05 is statistically significant
GLUT-1 Expression and Survival Analysis
The follow-up periods of the patients varied between 8 to 47 months (median 26 months). In the survival analysis, disease-free survival (DFS) durations were found to be significantly shorter in patients with GLUT-1 expression compared to patients without GLUT-1 expression (40,65 months (95% CI: 37.57-43.79) vs. 45.86 months (95% CI 44.26-47.42) (log-rank p: 0.027) (Figure 3). Although DFS was shorter in patients with GLUT-1 positivity in univariate analysis; multivariant analysis revealed only size (>5 cm vs <2 cm) (HR: 31.376; 95% CI: 3.36- 292.968), and Ki-67 level (HR: 7.61; 95% CI: 1.478- 39.192) to predict low DFS (Table 3, Table 4).
Figure 3.
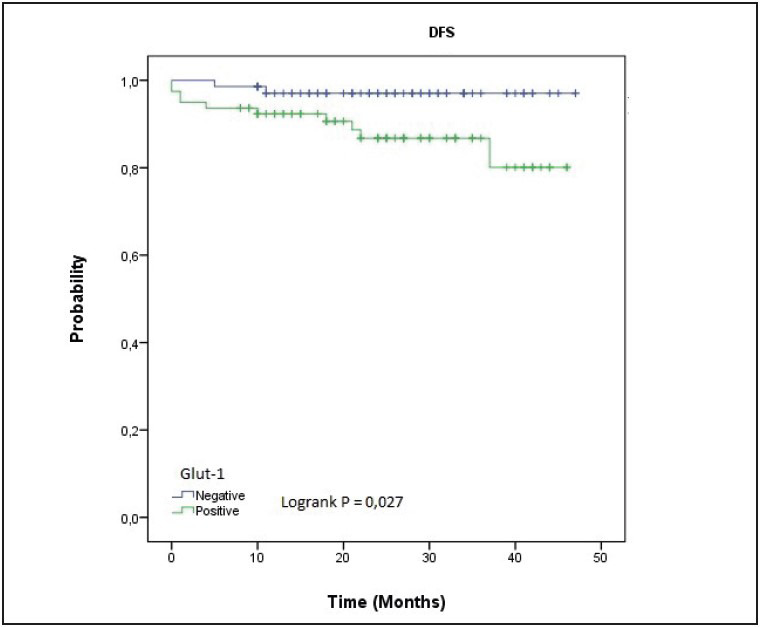
Kaplan-Meier disease free survival by GLUT-1 expression.
Table 3.
Univariate analysis results of clinicopathological variables associated with disease-free survival.
|
Variables |
B |
SE |
Wald |
p |
HR |
95.0% CI for HR |
|
|---|---|---|---|---|---|---|---|
|
Lower |
Upper |
||||||
|
Age |
0.017 |
0.022 |
0.636 |
0.425 |
1.018 |
0.975 |
1.062 |
|
GLUT-1 |
1.551 |
0.775 |
4.007 |
0.045 |
4.715 |
1.033 |
21.523 |
|
Estrogen Receptor |
-1.526 |
0.615 |
6.152 |
0.013 |
0.217 |
0.065 |
0.726 |
|
Progesterone Receptor |
1.425 |
0.578 |
6.072 |
0.014 |
4.159 |
1.339 |
12.923 |
|
Ki-67 |
1.658 |
0.776 |
4.564 |
0.033 |
5.251 |
1.147 |
24.043 |
|
Diameter ( > 5 cm vs. <2 cm) |
3.109 |
1.122 |
7.684 |
0.006 |
22.399 |
2.486 |
201.814 |
|
HER 2 |
-0.993 |
1.045 |
0.904 |
0.342 |
0.37 |
0.048 |
2.87 |
|
Angiolymphatic Invasion |
0.598 |
0.588 |
1.037 |
0.309 |
1.819 |
0.575 |
5.756 |
|
Perineural Invasion |
0.935 |
0.578 |
2.615 |
0.106 |
2.547 |
0.82 |
7.91 |
|
Lymph Node Metastasis |
0.68 |
0.63 |
1.165 |
0.28 |
1.974 |
0.574 |
6.792 |
|
Multicentricity |
-0.76 |
1.045 |
0.53 |
0.467 |
0.467 |
0.06 |
3.625 |
* Cox regression analysis
Table 4.
Independent risk factors associated with disease-free survival (Multivariate analysis).
|
|
B |
SE |
Wald |
p |
HR |
95.0% CI for HR |
|
|---|---|---|---|---|---|---|---|
|
Lower |
Upper |
||||||
|
Diameter |
|
|
15.772 |
0 |
|
|
|
|
2-5 cm vs <2 cm |
0.969 |
1.086 |
0.795 |
0.372 |
2.635 |
0.313 |
22.152 |
|
>5 cm vs <2 cm |
3.446 |
1.14 |
9.14 |
0.003 |
31.376 |
3.36 |
292.968 |
|
Ki 67 |
2.029 |
0.836 |
5.889 |
0.015 |
7.61 |
1.478 |
39.192 |
* Cox regression model
DISCUSSION
Glucose metabolism is one of the most significant steps in regulating cellular and systemic homeostasis and tumor carcinogenesis. Glucose transporter protein families provide glucose uptake from the systemic circulation into the cell (5,13,14). GLUT-1 is the main carrier protein found in many cells responsible for physiological and pathological glucose uptake. Their values in these cells change under physiological and pathological conditions. Especially the inhibition and activation of RAS, SRC, c-MYC and P53 genes were associated with GLUT-1 expression levels (15,16). In non-neoplastic cells, the p53 gene has been reported to inhibit GLUT-1 and GLUT-4, and the mutation in the p53 gene has been reported to accelerate glucose transport for tumor cells by increasing the function of GLUT (17,18).
Various studies have shown that the use of GLUT-1 antibodies provides a reduction in tumor size as a result of apoptosis, and some molecules have an antiproliferative effect on tumor cells by causing GLUT-1 inhibition (19–21). This situation reveals the close connection between carcinogenesis and glucose metabolism of tumoral cells via glucose transporter proteins, and shows that glucose transporter proteins may be target molecules in cancer therapy. Targeting this pathway may lead to significant results in cancer treatment. In addition to these promising findings of GLUT-1 expression in cancer treatment, it has been also reported that GLUT-1 expression can be used diagnostically to differentiate benign and malignant urothelial tumors (22).
The prognostic significance of GLUT-1 expression in different cancer types such as osteosarcoma, gastric adenocarcinoma, esophagus adenocarcinoma, pancreatic carcinoma, lung carcinoma, oral squamous cell carcinoma, endometrial adenocarcinoma has been reported in numerous studies (23–30).
In the meta-analysis of Deng et al. (31), consisting of 1861 breast cancer patients, high GLUT-1 expression levels correlated with high histological grade, negative ER and PR, and low survival times. In addition, Krzeslak et al. (32) reported that GLUT-1 expression was observed in 50% of breast carcinoma patients and that GLUT-1 expression was detected at a higher rate in poorly differentiated tumors than well-differentiated tumors. Kang et al. (33) reported that GLUT-1 expression was associated with negative ER, PR, and high nuclear grade and poor prognosis in breast carcinoma patients. Hussein et al. (34) found higher GLUT-1 expression levels in IDC patients compared to ILC and mixed ductal and lobular carcinoma patients. In the same study, GLUT-1 expression was found to be associated with basal phenotype breast carcinoma with high histological grade, negative ER and PR, and high p53 expression level.
Similar to the studies reported in the literature, GLUT-1 expression was higher in Luminal B, HER2 and, triple negative subtypes compared to Luminal A subtype cases in our study. Additionally, GLUT-1 expression was found to be statistically correlated with poor prognostic parameters such as high histological and nuclear grade, negative ER and PR expression, and high Ki-67 proliferation index. In the survival analysis, disease-free survival (DFS) durations were found to be significantly shorter in patients with GLUT-1 expression. GLUT-1 expression was not associated with tumor size, axillary lymph node metastasis, angiolymphatic invasion, perineural invasion, and multicentricity variables.
These findings suggest that the evaluation of GLUT-1 expression in breast cancers may be a promising parameter. However, studies with larger cohorts and longer follow-up periods are necessary in order to bring GLUT1 expression analysis to daily practice.
In our study, GLUT-1 expression was found to be statistically significantly lower in ILC patients compared to IDC patients. The reasons for this result might be the energy metabolism mediated by a different glucose transporter protein in the development of ILC or low GLUT-1 levels that cannot be evaluated immunohistochemically in ILC cases.
To our knowledge, there is no study investigating the relationship between GLUT-1 expression and neoadjuvant therapy in breast cancer patients. In our study, GLUT-1 expression was compared in two groups; patients with or without neoadjuvant therapy. Although GLUT-1 expression was higher in patients receiving neoadjuvant therapy (71.4% vs. 54%), no significant difference was observed between these two groups. The reason might be that current neoadjuvant therapy applications have no affect over GLUT-1, or the small number of patients with neoadjuvant therapy in our study.
However, there are limitations in our study in this regard. In order to determine the relationship between GLUT-1 expression and neoadjuvant therapy, the comparison of GLUT-1 expression between the pretreatment core biopsy and post-treatment surgical materials may be more decisive. This was not in the design of our study.
CONCLUSION
In our study, GLUT-1 expression was associated with pathological poor prognostic factors such as high histological and nuclear grade, ER and PR negativity, and low disease-free survival in breast carcinoma patients. These results suggest that GLUT-1 expression can be considered as a prognostic marker in breast cancers. It can be a promising target molecule for personalized treatment approaches. However, for the GLUT-1 molecule to be used in daily practice as a prognostic marker, our results should be supported by studies with longer follow-up periods and larger cohorts.
Conflict of Interest
Authors declare no conflict of interest.
References
- Ferlay J., Colombet M., Soerjomataram I., Mathers C., Parkin D. M., Piñeros M., Znaor A., Bray F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Apr;2019 Int J Cancer. 144(8):1941. doi: 10.1002/ijc.31937. [DOI] [PubMed] [Google Scholar]
- Li Jiehua, Chen Zhibai, Su Ka, Zeng Jian. Clinicopathological classification and traditional prognostic indicators of breast cancer. 2015Int J Clin Exp Pathol. 8(7):8500. [PMC free article] [PubMed] [Google Scholar]
- Chiche Johanna, Brahimi-Horn M. Christiane, Pouysségur Jacques. Tumour hypoxia induces a metabolic shift causing acidosis: a common feature in cancer. Apr;2010 J Cell Mol Med. 14(4):771. doi: 10.1111/j.1582-4934.2009.00994.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ancey Pierre-Benoit, Contat Caroline, Meylan Etienne. Glucose transporters in cancer - from tumor cells to the tumor microenvironment. Aug;2018 FEBS J. 285(16):2926. doi: 10.1111/febs.14577. [DOI] [PubMed] [Google Scholar]
- Pragallapati Sindhuri, Manyam Ravikanth. Glucose transporter 1 in health and disease. Dec;2019 J Oral Maxillofac Pathol. 23(3):443. doi: 10.4103/jomfp.JOMFP_22_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J.-C., Zhang J.-J., Zhang W., Ke Z.-Y., Ma L.-G., Liu M. Expression of GLUT-1 in nasopharyngeal carcinoma and its clinical significance. Nov;2017 Eur Rev Med Pharmacol Sci. 21(21):4891. [PubMed] [Google Scholar]
- Fitzgibbons Patrick L., Dillon Deborah A., Alsabeh Randa, Berman Michael A., Hayes Daniel F., Hicks David G., Hughes Kevin S., Nofech-Mozes Sharon. Template for reporting results of biomarker testing of specimens from patients with carcinoma of the breast. May;2014 Arch Pathol Lab Med. 138(5):595. doi: 10.5858/arpa.2013-0566-CP. [DOI] [PubMed] [Google Scholar]
- Allison Kimberly H., Hammond M. Elizabeth H., Dowsett Mitchell, McKernin Shannon E., Carey Lisa A., Fitzgibbons Patrick L., Hayes Daniel F., Lakhani Sunil R., Chavez-MacGregor Mariana, Perlmutter Jane, Perou Charles M., Regan Meredith M., Rimm David L., Symmans W. Fraser, Torlakovic Emina E., Varella Leticia, Viale Giuseppe, Weisberg Tracey F., McShane Lisa M., Wolff Antonio C. Estrogen and Progesterone Receptor Testing in Breast Cancer: ASCO/CAP Guideline Update. Apr;2020 J Clin Oncol. 38(12):1346. doi: 10.1200/JCO.19.02309. [DOI] [PubMed] [Google Scholar]
- Cirqueira Magno Belém, Moreira Marise Amaral Rebouças, Soares Leonardo Ribeiro, Cysneiros Maria-Auxiliadora de Paula Carneiro, Vilela Maria-Helena Tavares, Freitas-Junior Ruffo. Effect of Ki-67 on Immunohistochemical Classification of Luminal A to Luminal B Subtypes of Breast Carcinoma. Oct;2015 Breast J. 21(5):465. doi: 10.1111/tbj.12441. [DOI] [PubMed] [Google Scholar]
- Bandyopadhyay Sudeshna, Bluth Martin H., Ali-Fehmi Rouba. Breast Carcinoma: Updates in Molecular Profiling 2018. Jun;2018 Clin Lab Med. 38(2):401. doi: 10.1016/j.cll.2018.02.006. [DOI] [PubMed] [Google Scholar]
- Rakha EA, Allison KH, Ellis IO, Horii R, Masuda S, Penault-Llorca F. Invasive breast carcinoma: General overview. In: Lokuhetty D, , White VA, , Watanabe R, , Cree IA, , editors. Breast Tumours, WHO Classification of Tumours. IARC; Lyon: [ Sep 15; 2022 ]. p. 82. [Google Scholar]
- Elston C. W., Ellis I. O. Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Nov;1991 Histopathology. 19(5):403. doi: 10.1111/j.1365-2559.1991.tb00229.x. [DOI] [PubMed] [Google Scholar]
- Rastogi Kanika, Singh Lavleen, Khan Niyaz A., Goyal Surbhi, Khatri Arti, Gupta Natasha. Benign vascular anomalies: A transition from morphological to etiological classification. Jun;2020 Ann Diagn Pathol. 46:151506. doi: 10.1016/j.anndiagpath.2020.151506. [DOI] [PubMed] [Google Scholar]
- Thorens Bernard, Mueckler Mike. Glucose transporters in the 21st Century. Feb;2010 Am J Physiol Endocrinol Metab. 298(2):E141. doi: 10.1152/ajpendo.00712.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Mutong, Zhang Zhenyu. Glucose Transporter Regulation in Cancer: A Profile and the Loops. 2016Crit Rev Eukaryot Gene Expr. 26(3):223. doi: 10.1615/CritRevEukaryotGeneExpr.2016016531. [DOI] [PubMed] [Google Scholar]
- Macheda Maria L., Rogers Suzanne, Best James D. Molecular and cellular regulation of glucose transporter (GLUT) proteins in cancer. Mar;2005 J Cell Physiol. 202(3):654. doi: 10.1002/jcp.20166. [DOI] [PubMed] [Google Scholar]
- Ramos Helena, Calheiros Juliana, Almeida Joana, Barcherini Valentina, Santos Sónia, Carvalho Alexandra T. P., Santos Maria M. M., Saraiva Lucília. SLMP53-1 Inhibits Tumor Cell Growth through Regulation of Glucose Metabolism and Angiogenesis in a P53-Dependent Manner. Jan;2020 Int J Mol Sci. 21(2):E596. doi: 10.3390/ijms21020596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torre Alejandro J. De la, Rogoff Daniela, White Perrin C. P53 and cellular glucose uptake. 2013Endocr Res. 38(1):32. doi: 10.3109/07435800.2012.710883. [DOI] [PubMed] [Google Scholar]
- Rastogi Shipra, Banerjee Sarmistha, Chellappan Srikumar, Simon George R. Glut-1 antibodies induce growth arrest and apoptosis in human cancer cell lines. Nov;2007 Cancer Lett. 257(2):244. doi: 10.1016/j.canlet.2007.07.021. [DOI] [PubMed] [Google Scholar]
- Wu Qin, Ba-Alawi Wail, Deblois Genevieve, Cruickshank Jennifer, Duan Shili, Lima-Fernandes Evelyne, Haight Jillian, Tonekaboni Seyed Ali Madani, Fortier Anne-Marie, Kuasne Hellen, McKee Trevor D., Mahmoud Hassan, Kushida Michelle, Cameron Sarina, Dogan-Artun Nergiz, Chen WenJun, Nie Yan, Zhang Lan Xin, Vellanki Ravi N., Zhou Stanley, Prinos Panagiotis, Wouters Bradly G., Dirks Peter B., Done Susan J., Park Morag, Cescon David W., Haibe-Kains Benjamin, Lupien Mathieu, Arrowsmith Cheryl H. GLUT1 inhibition blocks growth of RB1-positive triple negative breast cancer. Aug;2020 Nat Commun. 11(1):4205. doi: 10.1038/s41467-020-18020-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zambrano Angara, Molt Matías, Uribe Elena, Salas Mónica. Glut 1 in Cancer Cells and the Inhibitory Action of Resveratrol as A Potential Therapeutic Strategy. Jul;2019 Int J Mol Sci. 20(13):E3374. doi: 10.3390/ijms20133374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyaci Ceren, Behzatoğlu Kemal. Diagnostic Value of Glucose Transporter 1 (GLUT-1) Expression in Nested Variant of Urothelial Carcinoma. 2019Turk Patoloji Derg. 35(1):22. doi: 10.5146/tjpath.2018.01435. [DOI] [PubMed] [Google Scholar]
- Fan Jian, Mei Jiong, Zhang Ming-Zhu, Yuan Feng, Li Shan-Zhu, Yu Guang-Rong, Chen Long-Hui, Tang Qian, Xian Cory J. Clinicopathological significance of glucose transporter protein-1 overexpression in human osteosarcoma. Aug;2017 Oncol Lett. 14(2):2439. doi: 10.3892/ol.2017.6437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berlth Felix, Mönig Stefan, Pinther Berit, Grimminger Peter, Maus Martin, Schlösser Hans, Plum Patrick, Warnecke-Eberz Ute, Harismendy Olivier, Drebber Uta, Bollschweiler Elfriede, Hölscher Arnulf, Alakus Hakan. Both GLUT-1 and GLUT-14 are Independent Prognostic Factors in Gastric Adenocarcinoma. Dec;2015 Ann Surg Oncol. 22 Suppl 3:S822. doi: 10.1245/s10434-015-4730-x. [DOI] [PubMed] [Google Scholar]
- Yin Chenqing, Gao Bin, Yang Ju, Wu Jingbo. Glucose Transporter-1 (GLUT-1) Expression is Associated with Tumor Size and Poor Prognosis in Locally Advanced Gastric Cancer. Mar;2020 Med Sci Monit Basic Res. 26:e920778. doi: 10.12659/MSMBR.920778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiba Itaru, Ogawa Kazuhiko, Morioka Takamitsu, Shimoji Hideaki, Sunagawa Nao, Iraha Shiro, Nishimaki Tadashi, Yoshimi Naomi, Murayama Sadayuki. Clinical significance of GLUT-1 expression in patients with esophageal cancer treated with concurrent chemoradiotherapy. Jan;2011 Oncol Lett. 2(1):21. doi: 10.3892/ol.2010.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basturk Olca, Singh Rajendra, Kaygusuz Ecmel, Balci Serdar, Dursun Nevra, Culhaci Nil, Adsay N. Volkan. GLUT-1 expression in pancreatic neoplasia: implications in pathogenesis, diagnosis, and prognosis. Mar;2011 Pancreas. 40(2):187. doi: 10.1097/MPA.0b013e318201c935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh Young Wha, Lee Su Jin, Park Seong Yong. Differential expression and prognostic significance of GLUT1 according to histologic type of non-small-cell lung cancer and its association with volume-dependent parameters. Feb;2017 Lung Cancer. 104:31. doi: 10.1016/j.lungcan.2016.12.003. [DOI] [PubMed] [Google Scholar]
- Harshani Jyotsna M., Yeluri Sivaranjani, Guttikonda Venkateswara Rao. Glut-1 as a prognostic biomarker in oral squamous cell carcinoma. Dec;2014 J Oral Maxillofac Pathol. 18(3):372. doi: 10.4103/0973-029X.151318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khabaz Mohamad Nidal, Qureshi Imtiaz Ahmad, Al-Maghrabi Jaudah Ahmad. GLUT 1 expression is a supportive mean in predicting prognosis and survival estimates of endometrial carcinoma. 2019Ginekol Pol. 90(10):582. doi: 10.5603/GP.2019.0102. [DOI] [PubMed] [Google Scholar]
- Deng Yu, Zou Jialing, Deng Ting, Liu Junying. Clinicopathological and prognostic significance of GLUT1 in breast cancer: A meta-analysis. Nov;2018 Medicine (Baltimore) 97(48):e12961. doi: 10.1097/MD.0000000000012961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krzeslak Anna, Wojcik-Krowiranda Katarzyna, Forma Ewa, Jozwiak Paweł, Romanowicz Hanna, Bienkiewicz Andrzej, Brys Magdalena. Expression of GLUT1 and GLUT3 glucose transporters in endometrial and breast cancers. Jul;2012 Pathol Oncol Res. 18(3):721. doi: 10.1007/s12253-012-9500-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang Sung Soo, Chun Yi Kyeong, Hur Min Hee, Lee Hae Kyung, Kim Yee Jeong, Hong Sung Ran, Lee Jee Hyun, Lee Sung Gong, Park Yong Koo. Clinical significance of glucose transporter 1 (GLUT1) expression in human breast carcinoma. Oct;2002 Jpn J Cancer Res. 93(10):1123. doi: 10.1111/j.1349-7006.2002.tb01214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussein Yaser R., Bandyopadhyay Sudeshna, Semaan Assaad, Ahmed Quratulain, Albashiti Bassam, Jazaerly Tarek, Nahleh Zeina, Ali-Fehmi Rouba. Glut-1 Expression Correlates with Basal-like Breast Cancer. Dec;2011 Transl Oncol. 4(6):321. doi: 10.1593/tlo.11256. [DOI] [PMC free article] [PubMed] [Google Scholar]