Abstract
Aims
Family carers supporting an individual with psychosis often experience poorer mental health, however, little is known about specific risk factors among these carers. We investigated the associations between demographic, caregiving characteristics and mental health outcomes in family carers supporting an individual with psychosis and compared carers’ outcomes with general population norms.
Methods
We analysed baseline data from the COPe-support randomised controlled trial of online psychoeducation and peer support for adult carers supporting an individual with psychosis between 2018 and 2020. We collected carers’ demographic and health outcome data, including wellbeing using Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS as primary outcome), quality of life using EQ-5D-5L and caregiving experience assessed with Experience of Caregiving Inventory. We tested associations between carers’ demographic and caregiving characteristics for each outcome in turn and meta-analysed carers’ WEMWBS and EQ-5D-5L with Health Survey England (HSE) general population data from 2016 and 2017, respectively.
Results
The 407 carers of people with psychosis had a mean WEMWBS score of 42.2 (s.d. 9.21) and their overall weighted pooled WEMWBS score was 7.3 (95% confidence interval (CI) –8.6 to –6.0, p < 0.01) lower than the HSE general population sample, indicating carers have poorer mental wellbeing by more than double the minimum clinically important difference of 3 points on WEMWBS. Among all caring relationships, partners had poorer wellbeing compared to parents with lower WEMWBS score (–6.8, –16.9 to 3.3, p = 0.03). Single carers had significantly poorer wellbeing (–3.6, –5.6 to –1.5, p < 0.01) and a more negative caregiving experience than those who were cohabiting. Spending more than 35 h per week caregiving increased carers’ negative experience significantly (p = 0.01).
Conclusion
Carers of people with psychosis have poorer mental health than non-carers. Partners, lone carers and those spending more than 35 h per week on caring were found to be most at risk of poor mental health. Based on the results, we advocate that the details of carers for individuals with psychosis should be added to the existing carers or severe mental illness registers at all general practitioner surgeries and for their wellbeing screened routinely. Future large-scale prospective studies are needed to develop a predictive model to determine risk factors, hence to aid early identification of carers’ support needs. Such understandings are also useful to inform tailored intervention development.
Keywords: Caregiving, family carers, psychosis, public mental health, quality of life, wellbeing
Introduction
It is estimated that approximately 1.5 million people in the UK are caring for a family member or friend with a mental illness (The Schizophrenia Commission, 2012; NICE, 2014; Carers Trust, 2019). Psychotic disorders or psychosis are recognised as among the most common severe mental illness (SMI), often with worst outcomes (The Schizophrenia Commission, 2012; NICE, 2014). ‘Psychosis’ could be regarded as a broad category of major mental health conditions (such as schizophrenia, schizoaffective disorder and delusional disorder) that have psychotic symptoms as its hallmarks. Psychotic symptoms can cause significant distress in an individual and far-reaching impacts on their perception, thoughts, mood, behaviour and functioning. Often, people with psychosis require long-term treatment and support across a range of life domains, including emotional support, and financial and practical assistance for daily living activities (The Schizophrenia Commission, 2012; Sin and Norman, 2013; NICE, 2014; Sin et al., 2017). The importance of relatives and friends providing a supportive role – commonly referred to as family carers (or carers as referred to thereafter) – is well established. Individuals who receive support and care from their familial networks have a better prognosis and enhanced quality of life (QoL) (Pharoah et al., 2010; Sin et al., 2016).
The load and responsibility of caregiving can cause high levels of distress affecting the mental health of the carers themselves (Singleton et al., 2002; Smith et al., 2014; Stansfeld et al., 2014). Over the last decade, Health Survey England (HSE) (Bridges, 2012) and Adult Psychiatric Morbidity Surveys (APMS) (Smith et al., 2014; Stansfeld et al., 2014) have published some reports focusing on carers’ mental health, among their regular English adult population survey reports (e.g. McManus et al., 2016; NHS Digital HSE, 2016, 2017). These repeatedly reported that carers of individuals with ill health, disability or frailty (i.e. general carers) have poorer wellbeing than non-carers in the general population. A HSE 2012 report investigating carers’ mental wellbeing identified that general carers who provided caregiving for 10 or more hours per week (hpw) (n = 227) had the lowest mental wellbeing scores, compared to those providing up to 9 h (n = 560) or no care (n = 137), respectively (Bridges, 2012). Furthermore, carers’ mental health morbidities are known to be correlated with the amount of care they provide. In an analysis of APMS 2007 general population survey data, 25% (n = 1883) of participants, out of the total 7304 people, identified themselves as regular general carers supporting a family member or friend (Smith et al., 2014). The carers were found to have poorer mental health than non-carers and those caregiving more than 20 hpw had a twofold increase in mental distress symptomatology (Smith et al., 2014).
Comparing with caring for a loved one with a physical illness, supporting an individual with psychosis where comorbid physical health problems are common, is known to be much more demanding and stressful (Singleton et al., 2002; The Schizophrenia Commission, 2012; NICE, 2014; Steptoe et al., 2015). Research evidence further suggests that poor mental health in carers can negatively impact their caregiving capacity (Bebbington and Kuipers, 1994; Szmukler et al., 1996; Steptoe et al., 2015), rendering them less likely to engage in caring for their loved ones or more likely to exhibit critical or hostile behaviour towards the cared-for persons (CfP) (Szmukler et al., 1996; Cooper et al., 2010). In turn, high expressed emotion (EE), i.e. critical attitude or over-involvement within the family environment, has long been shown to increase risk of relapses in patients by three to fourfold (Bebbington and Kuipers, 1994), potentially leading to a vicious cycle of poor health and QoL for all concerned. Hence in the last decade, the UK government has published multiple policies and strategies aimed at identifying carers to provide them with support and intervention as early as possible (DOH, 2008, 2014; NICE, 2014; Yesufu-Udechuku et al., 2015). Although healthcare practitioners in primary and mental health services are best placed to identify and provide support for the carer population, in particular for those supporting an individual with psychosis, research evidence identifies an ongoing implementation gap (Sin et al., 2018; HQIP & Royal College of Psychiatrists, 2016).
Most prior studies on carers’ mental wellbeing and other health outcomes have focused on those who support a loved one with a long-term illness or dementia, but not specific to psychosis. Systematic reviews on carers of people with psychosis report approximately 80% of the study participants were females, especially mothers for their adult child suffering from psychosis (Sin and Norman, 2013; Yesufu-Udechuku et al., 2015; Sin et al., 2017). Nearly half of these carers were provided over 32 hpw caregiving (Roick et al., 2007), potentially increasing their health morbidities. To date, little is known about other carers with a different relationship to the CfP, such as partners, children or siblings. Similarly, beyond time spent on caregiving, few studies have investigated other factors affecting carers’ mental health outcomes. The paucity of high-quality research translates into a lack of routine identification of carers and monitoring of their health outcomes. In order to establish how carers of people with psychosis fare in terms of mental wellbeing and QoL, we compared their outcomes with those of their counterparts in the general population. To further understand plausible risk factors associated with carers’ mental health outcomes for timely identification and provision of tailored interventions, we investigated a range of demographic and caregiving factors among carers.
Methods
Study population and design
We conducted analyses of baseline data from an online randomised controlled trial (RCT) targeting psychosis carers. The RCT was designed to evaluate a multi-component eHealth intervention, called COPe-support (Sin et al., 2019), for carers of individuals with psychosis and took place between 2018 and 2020, as described elsewhere (Sin et al., 2020). We recruited carers who have a significant emotional bond with the CfP (as defined by the NICE guideline) (NICE, 2014) and have at least weekly contact in any format including face-to-face meetings and remote interactions. The RCT recruitment activities took place across 30 NHS mental healthcare trusts and various voluntary carer services in England. Both the carers and their CfP were required to be residing in England during the study period (Sin et al., 2020). All eligible carers were accepted into the RCT regardless of any support or services they received. The baseline data collected from the RCT participants were utilised in this study.
We extracted data from HSE samples on general population mental wellbeing (NHS Digital HSE, 2016) and QoL data (NHS Digital HSE, 2017), to compare to the carers in the study. HSE is a series of annual, household surveys that gather cross-sectional data at the household and individual level. It uses a multi-stage stratified random probability sampling method to obtain a sample representative of the general population living in private households in England, based on postcode sector (see Craig et al., 2014 for further details of HSE sampling and data collection procedures). Each annual survey includes core questions and measurements concerning health conditions which are the same each year, in addition to year-specific questions that focus on particular health outcomes (Craig et al., 2014). These include the measurement of mental wellbeing in HSE 2016 and QoL in HSE 2017 (NHS Digital HSE, 2016, 2017).
Data collection
We collected baseline data from the participants through our online platform. These included carers’ demographic and 12 caregiving-related characteristics: age of carers and CfP; gender of the carers and their CfP; carer’s ethnicity as White or Black, Asian and minority ethnic (BAME); carers’ relationship with the CfP (parent, partner, child or sibling, or other relatives/close friend); carers’ employment status; highest education level achieved; marital status; the specific type of psychotic disorder the CfP suffered; time since illness onset in the CfP; living with the CfP or not; and hours spent caregiving per week.
Outcomes for population comparison
The primary health outcome was the carers’ mental wellbeing, measured with the Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS) (Tennant et al., 2007). WEMWBS scores range from 14 (minimum) to 70 (maximum); the higher the score the better the individual’s mental wellbeing and a change of 3 points in WEMWBS represents the minimum clinically important difference (MCID) (Maheswaran et al., 2012). We also examined carers’ QoL measured by EQ-5D-5L (Szende et al., 2014). EQ-5D-5L includes two parts: the visual analogue scale (VAS) which ranges from 0 (the worst health) to 100 (the best health) reflecting the individual’s own judgement and the index value of overall health-related QoL (Szende et al., 2014). The single index value ranges from 0 (dead) to 1 (full health) reflecting how good or bad the individual’s health state is according to the preferences of the general population of that country (van Hout et al., 2012). Both WEMWBS and EQ-5D-5L have been widely used in epidemiological studies, including the Health Surveys in England in 2016 and 2017 (NHS Digital HSE, 2016, 2017) from which we drew our comparison data as published population-level data.
Health outcomes in the carer sample only
We investigated other caregiving-related health outcomes which are known to be associated with carers’ mental wellbeing, including carers’ knowledge of mental health, appraisal of caregiving experience, carer-specific wellbeing and perceived support and EE (Bebbington and Kuipers, 1994; Szmukler et al., 1996; Singleton et al., 2002; Bridges, 2012; Smith et al., 2014; Sin et al., 2017). We assessed carers’ mental health knowledge with the Mental Health Knowledge Schedule (MAKS) (Evans-Lacko et al., 2010). MAKS scores range from 6 to 30; higher score indicates better knowledge of mental health (Evans-Lacko et al., 2010; Henderson and Thornicroft, 2013). We measured carers’ wellbeing and perceived support using Carer Wellbeing and Support scale (CWS), which was specifically designed for the carer populations (Quirk et al., 2012). Higher wellbeing scale total (range: 0–128) indicates better carer wellbeing; while higher support scores (reverse scoring used and total range: 0–51) indicates lower satisfaction with support received. Appraisal of caregiving was assessed using the Experience of Caregiving Inventory (ECI) (Szmukler et al., 1996) which produces two subscale scores: a negative subtotal ranging from 0 to 208 (higher scores indicate poorer negative appraisal of the caring situation, covering problems with services, stigma and dependency); and a positive subtotal from 0 to 56 (higher scores indicate better positive experience) (Szmukler et al., 1996; Joyce et al., 2000). Lastly, we assessed carers’ EE with Family Questionnaire (FQ), with higher scores indicating worse EE (range: 10–80) (Wiedemann et al., 2002).
Ethics statement
Participants provided informed consent on our online platform for participation in the RCT of COPe-support. Participants received a goodwill payment (an online voucher) for their participation and provision of baseline data. The RCT has been reviewed and approved by South Central – Oxford C Research Ethics Committee (Reference: 18/SC/0104) and Health Research Authority (Reference: IRAS 240005).
Statistical analysis
The analysis began with computing the demographic and outcome measures (as aforementioned) using appropriate measures to describe central tendency and spread for continuous variables, and contingency tables for categorical variables. We examined associations and relationships between health outcomes through graphical displays, using Pearson’s correlation statistic, 95% confidence interval (CI) and p value to assess the direction and strength of the correlation. We explored the relationships between demographic characteristics for each outcome, in turn, using linear regression. The intention of the analysis was to explore the association between demographic and caregiving variables so all 12 covariates were included regardless of significance. The functional forms of covariates in the regression models were determined using external literature and visual plots. Interactions between carer characteristics and outcomes were pre-specified using data from published literature (on carers in general) and were: gender and age; relationship type and age of CfP; gender and time spent on care; and the relationship between carer and CfP with time spent on care (Bebbington and Kuipers, 1994; Szmukler et al., 1996; Singleton et al., 2002; Cooper et al., 2010; Bridges, 2012; Smith et al., 2014; Sin et al., 2017). We included these interactions if there was evidence of their importance p < 0.20. We evaluated the model assumptions using residual analysis. We used STATA version 15 (StataCorp., 2017).
To evaluate the difference in WEMWBS scores between our carer sample and the HSE 2016 general population data (NHS Digital HSE, 2016) we conducted a random-effects meta-analysis pooling the mean and standard deviations from each age category across the two populations. For this comparison, HSE wellbeing data were restricted to age ranges that matched those of our carer sample of this study. Standard deviations were estimated using the weighted sample and standard errors available in published reports. Weighted mean difference (WMD) was chosen instead of standardised mean difference (SMD) for interpretability. We used the same method to compare data on EQ-5D index value score for the carer sample with general population data from HSE 2017 survey data, grouped into corresponding age ranges (NHS Digital HSE, 2017).
Results
Carer sample characteristics
The RCT comprised 407 carers, out of 464 who gave informed consent and also provided baseline data. Table 1 summarises the demographic data of the carers. The mean age of carers was 53 years and the mean age of the CfP was 35 years. The majority of the carers were White, while 48 (11.8%) self-identifying as BAME, of which one-third (4.2%) described themselves as Black. A majority of participants were female and of these, a further majority cared for a male person. Parents comprised the majority of the participants, followed by partners, while children/siblings or other relatives/close friends formed the remainder (15.2%). Just over half of the participants were in work oreducation; while nearly a quarter were retired and one-fifth were not currently in work. Most carers described themselves as married or cohabiting, while one-third were single. About half of the participants lived with the CfP. About 40% of carers spent >35 hpw on caregiving; equivalent to a full-time vocational commitment.
Table 1. Summary of demographics and caregiving-related characteristics of carers.
| Carer characteristics (N = 407) | ||
| Age, Mean (s.d.) | 53.1 | (13.2) |
| Gender | n | % |
| Male | 77 | 18.9 |
| Female | 330 | 81.1 |
| Ethnicity | ||
| White | 359 | 88.2 |
| BAME | 48 | 11.8 |
| Employment status | ||
| Work/Education | 224 | 55.1 |
| Unemployed/Not working | 88 | 21.6 |
| Retired | 95 | 23.3 |
| Highest education level achieved | ||
| Pre-university | 127 | 31.2 |
| Undergraduate/Profession qualification | 153 | 37.6 |
| Postgraduate | 87 | 21.4 |
| Apprenticeship | 40 | 9.8 |
| Marital status | ||
| Married/cohabiting | 278 | 68.3 |
| Single/Divorced/Other | 129 | 31.7 |
| Relationship with CfP | ||
| Parent | 258 | 63.4 |
| Spouse/Partner | 87 | 21.4 |
| Child/Sibling | 44 | 10.8 |
| Friend/Other relatives | 18 | 4.4 |
| Living arrangement | ||
| With CfP | 227 | 55.8 |
| Not with CfP | 180 | 44.2 |
| Duration of care (hours/week) | ||
| 1-9 h/week | 110 | 27.0 |
| 10-19 h/week | 77 | 18.9 |
| 20-34 h/week | 57 | 14.0 |
| 35-49 h/week | 41 | 10.1 |
| 50 + hours/week | 122 | 30.0 |
| Cared-for persons’ characteristics | ||
| Age of CfP, Mean (s.d.) | 35.0 | (13.9) |
| Gender of CfP | n | % |
| Male | 255 | 62.7 |
| Female | 152 | 37.3 |
| Primary diagnosis of CfP | ||
| Schizophrenia | 170 | 41.8 |
| Psychosis | 202 | 49.6 |
| Type 1 Bipolar disorder | 35 | 8.6 |
| Time since CfP illness onset | ||
| 0-5 years | 197 | 48.4 |
| >5-10 years | 64 | 15.7 |
| >10 years | 146 | 35.9 |
Health outcomes of carers
Carers had a mean score of 42.2 (s.d. 9.2) on WEMWBS which ranged between 17 and 68 across the study population. Partners of the CfP had the lowest WEMWBS score (38.9, s.d. 9.5), while carers who were friends or other relatives scored the highest with WEMWBS (47.3, s.d. 9.3). The WEMWBS score was also higher for carers from a BAME ethnicity (45.9, S.D. 9.4) compared to those of White ethnicity (41.7, S.D. 9.1). The mean MAKS score was 23.7 (s.d. 2.9), with the maximum score being 30 this indicated that carers had good mental health knowledge (Evans-Lacko et al., 2010). The mean EQ-5D VAS score was 67.6 (s.d. 19.2), where 100 is perfect health, this mean is lower compared to the general population (82.8 s.d. 23.3) for the UK (Szende and Williams, 2004). See Table 2 for a summary of carers’ health outcome variables and HSE general population’s WEMWBS and EQ-5D index value data.
Table 2. Summary of carers’ and HSE sample’s health outcome variables.
| Health outcome measures | Score range and indication | Carer sample (n = 407) | HSE samples Mean (s.d.) |
||
|---|---|---|---|---|---|
| Mean (s.d.) | IQR | Median | |||
| WEMWBS | 14–70 (best) | 42.2 (9.2) | 36–49 | 42 | 49.9 (10.8)* |
| MAKS | 6–30 (best) | 23.7 (2.9) | 22–26 | 24 | NA |
| ECI – Negative subscale | 0–208 (worst) | 108.5 (32.4) | 89–132 | 110 | NA |
| ECI – Positive subscale | 0-56 (best) | 30.3 (7.4) | 25–35 | 31 | NA |
| FQ | 10–80 (worst) | 50.9 (10.4) | 44–57 | 51 | NA |
| CWS – Wellbeing subscale | 0 = 128 (best) | 73.5 (28.2) | 53–97 | 76 | NA |
| CWS – Support subscale | 0-51 (worst) | 22.4 (12.0) | 14–31 | 22 | NA |
| EQ-5D-5L visual analogue scale | 0-100 (best) | 67.6 (19.2) | 52–82 | 70 | NA |
| EQ-5D-5L index value score | 0–1 (best) | 0.73 (0.23) | 0.69–0.88 | 0.77 | 0.88 (0.25)** |
IQR, interquartile range; WEMWBS, Warwick-Edinburgh Mental Wellbeing Scale; MAKS, Mental Health Knowledge Schedule; ECI, Experience of Caregiving Index; FQ, Family Questionnaire; CWS, Carer Wellbeing and Support Scale; NA, not applicable;
n = 6799 from HSE 2016,
n = 7136 from HSE 2017.
Comparing carers’ mental wellbeing and QoL with HSE samples
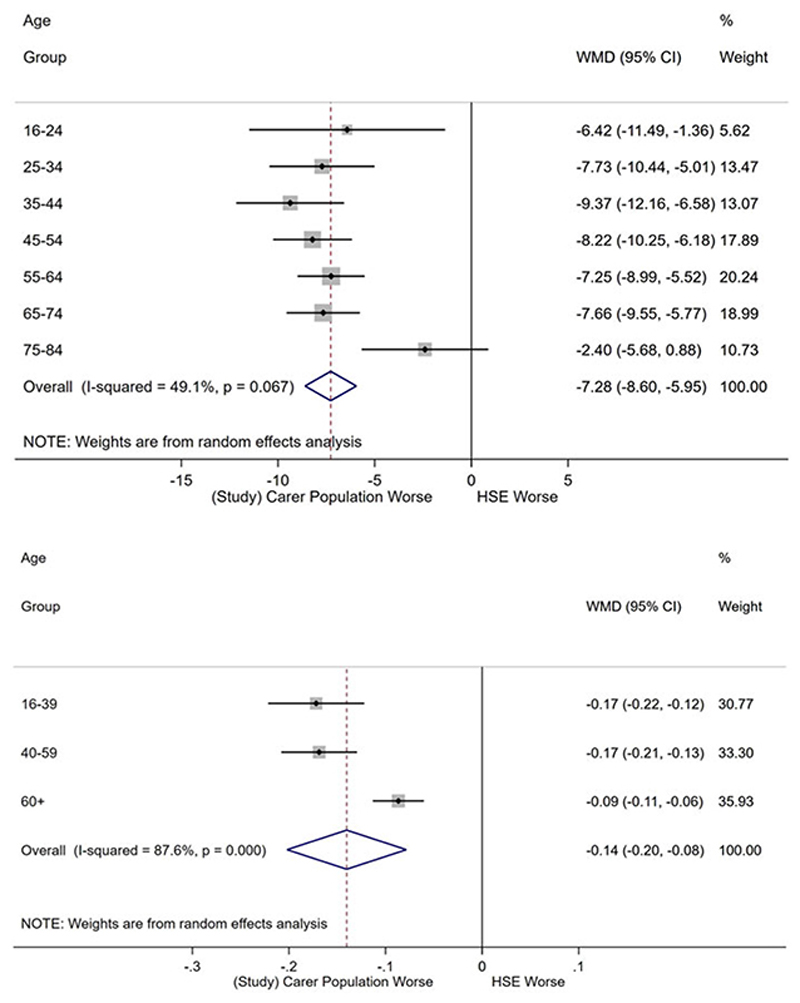
Figure 1a depicts the difference in WEMWBS score for carers in this study compared to the general population of the same age range from the most recent HSE data (n = 6,799, 51.3% women) (NHS Digital HSE, 2016). The overall weighted pooled WEMWBS score for carers was lower than the HSE sample by -7.3 (95% CI -8.6 to -6.0, p <0.01). These differences are two to three times the MCID of 3 points on WEMWBS (Maheswaran et al., 2012). A comparison of EQ-5D index value scores between carers and the HSE general population (n = 7136, 51.8% women) (NHS Digital HSE, 2017), estimated a pooled mean difference of –0.14 (–0.2 to –0.1, p < 0.01), indicating carers had poorer QoL (see Fig. 1b). Index value score differences were largest in the 16-39 age group, –0.17 (–0.2 to –0.1) and smallest for those older than 60, –0.14 (–0.2 to –0.1).
Fig. 1.
(a) Meta-analysis of WEMWBS score between study carer and HSE samples, (b) meta-analysis of EQ-5D index value score between study carer and HSE samples.
Correlations between health and caregiving-related outcomes
We proceeded to explore correlations between carers’ wellbeing and QoL and other health and caregiving-related outcomes. There were strong negative correlations between mental wellbeing and negative caregiving experience, –0.47 (95% CI –0.5 to –0.4, p < 0.01); that is, carers’ mental wellbeing was better among those who had a lower ECI negative subscale score. Similarly, carers’ mental wellbeing was found to be negatively correlated with EE (-0.55. -0.6 to -0.5, p <0.01); i.e. better wellbeing in those with lower EE scores. Conversely, carers’ mental wellbeing was positively correlated with positive caregiving experience, 0.31 (0.2-0.4, p < 0.01). Strong positive correlations occurred between mental wellbeing and carer wellbeing, 0.65 (0.6–0.7, p< 0.01). Carers’ wellbeing, in turn, had strong negative correlations with negative caregiving experience (–0.77, –0.8 to –0.7, p < 0.01) and EE (–0.79, –0.8 to –0.7, p < 0.01), respectively. Between other health outcomes, strong positive correlations were identified between negative caregiving experience and EE, 0.76 (0.7–0.8, p < 0.01).
Association between carers’ characteristics and health outcomes
Wellbeing
Mental wellbeing differed between White and BAME carers, with the latter having a higher adjusted WEMWBS score, as reported in Table 3. The relationship with CfP was found to be associated with wellbeing, with partners and friends/other relatives having poorer wellbeing compared to parents. Table 3 depicts that compared with the reference group (carers who were cohabiting), single carers had significantly poorer wellbeing. There was evidence for an interaction between the age of CfP and the relationship with the carer (p < 0.01). With the interaction, a year’s increase in age of CfP corresponds to an increase in wellbeing for parents (0.3, 0.1–0.5), partners (0.2, 0.0–0.4), and friend/other relatives (0.4, 0.1–0.6), but a decrease (–0.1, –0.3 to 0.1) for children/siblings.
Table 3. Selected covariates from multi-variable regression analyses for WEMWBS.
| Partial WEMWBS regression results | |||
|---|---|---|---|
| Regression coefficient | Estimate | 95% confidence interval | p value* |
| Age of CfP | 0.29 | (0.1–0.5) | p <0.01 |
| Ethnicity | |||
| White | Ref. | – | p <0.01 |
| BAME | 4.50 | (1.8–7.2) | |
| Relationship with CfP | |||
| Parent | Ref. | – | p = 0.03 |
| Spouse/Partner | –6.83 | (–16.9 to 3.3) | |
| Child/Sibling | 10.32 | (–1.2 to 21.9) | |
| Friend/Other relatives | –3.23 | (–17.2 to 10.7) | |
| Marital status | |||
| Married | Ref. | – | p <0.01 |
| Single/Other | –3.56 | (–5.6 to –1.5) | |
| Duration of Care (hours/week) | |||
| 1–9 | Ref. | – | p = 0.07 |
| 10–19 | –1.25 | (–3.8 to 1.3) | |
| 20–34 | –2.27 | (–5.2 to 0.7) | |
| 35-49 | –3.13 | (–6.5 to 0.3) | |
| 50 + | –4.29 | (–7.2 to –1.3) | |
| Interaction | |||
| Age of CfP×Spouse/Partner | –0.06 | (–0.3 to 0.2) | p <0.01 |
| Age of CfP × Child/Sibling | –0.36 | (–0.6 to –0.1) | |
| Age of CfP × Friend/Other | 0.08 | (–0.2 to 0.4) | |
p values shown for categorical coefficients are from a Wald test for statistical significance for all levels of coefficient.
These estimates are taken from the full regression model which can be seen in online Supplementary Table 1 with the full models from all outcomes.
Online Supplementary Table 1 shows the multi-variable regression analyses for all health outcomes with 12 covariates in the model. We focused on reporting the associations and interactions with significant results herewith. Focusing on carer-specific wellbeing (i.e. CWS wellbeing scores), we found that time spent caring (p = 0.01) has strong negative associations with carer wellbeing. As time spent caring increased, carer’s wellbeing deteriorated; compared to those providing 9 or less hpw on caring, those who spent 10–19 hpw and ⩾50 hpw caring had a decrease of –6.0 (–14.0 to 2.0, p = 0.14) and –16.6 (–25.8 to –7.5, p < 0.01) in CWS wellbeing scores, respectively.
Negative caregiving experience and EE
The adjusted ECI negative subscale for the carers reduced by -0.5 (-1.0 to -0.1, p = 0.02) for each year increase in age of the CfP. Carers’ FQ score also reduced with increasing age of CfP, with a mean decrease of -0.1 (-0.2 to 0.0, p = 0.19) for each year, as reported in online Supplementary Table 1. These translate into a reduction in the carers’ negative caregiving experience and EE when the CfP was older in age. Compared to parents who spent the same time caring, carers who were partners (3.6, –5.3 to 12.5), siblings/children (3.4, –3.7 to 10.5) had poorer EE (group p = 0.03). Those who were single had poorer experience compared to those who were in an intimate relationship, with higher estimated mean ECI-negative scores of 7.3 (0.0–14.6, p = 0.05). Spending more than 35 hpw caregiving increased carers’ negative caregiving experience significantly; with those caring for 35–49 hpw having the highest ECI negative score increase of 37.8 (8.5–67.1, p <0.01), compared to those caring for <10hpw, of the same gender and same relationship.
Other health and caregiving-related outcomes
No demographic or caregiving characteristics, other than the carer’s marital status, showed any strong association with mental health knowledge. Those who were single had an estimated mean reduction in MAKs score of -0.8 (95% CI -1.5 to -0.1, p = 0.03). The model for the ECI positive subscale showed that female carers had a score that was 6.7 (3.1–10.3, p <0.01) higher than male carers spending the same time caring. The score was also higher for BAME carers, with an estimated mean increase of 6.0 (3.7–8.3, p <0.01) compared to carers of White ethnicity. Relative to parents who spent the same time caring, children/siblings and friends/other relatives had an increase of 12.0 (95% CI 4.0–20.2, p <0.01) and 12.3 (95% CI 1.7–22.8, p = 0.02) in CWS Support score respectively, i.e. less satisfied with the support received. Strong statistical associations were identified between EQ-5D VAS and the following demographics showing: a higher score for those married (p < 0.01), higher for retired (p< 0.01) and lower for those unemployed compared to those working or in education (p < 0.01) (see online Supplementary Table 1).
Discussion
Our study results identified that psychosis carers have significantly poorer mental wellbeing and QoL than their peers in the wider general population in England of a similar age range. Carers of people with psychosis seemed to have much poorer mental wellbeing than those general carers in the HSE sample who spent more than 10 hpw caring (Bridges, 2012). Partners of the CfP and single carers were found to have the poorest mental wellbeing. Partners were also found to have the lowest carer’s wellbeing, worst negative caregiving experience, higher EE and lower satisfaction with support received. Spending over 35 hpw on caring was associated with a significantly poorer negative experience. Increased caregiving over this threshold was also associated with higher EE, indicating that carers were more likely to exhibit critical attitude towards their CfP. All carers, apart from siblings and children, had higher wellbeing, when the individual they cared for was older.
Our study confirms that associations found between carers’ characteristics in general and outcomes (Singleton et al., 2002; Cooper et al., 2010; Bridges, 2012; Smith et al., 2014) also apply in the context of psychosis caregiving. Firstly, other researchers suggested that while siblings and children ‘inherit’ the key-carer role from the original carers (most likely their parents who can no longer provide care) (Bowman et al., 2014; Sin et al., 2016), they tend to step into the dual caring role for the older generation as well as for dependent children. These ‘sandwich carers’ are not widely-recognised in psychosis literature or clinical practice (Ben-Galim and Silim, 2013; Centre for Policy on Ageing, 2015). Secondly, carers who are not in a relationship are likely to be those described as a lone carer having no relief to share the caregiving load while also bearing more socio-economic challenges (Singleton et al., 2002; The Schizophrenia Commission, 2012; Sin et al., 2017; Carers Trust, 2019). Thirdly, our results showed that partners had worse health outcomes than other carers of individuals with psychosis. The current study might well be the first which has a high proportion of partners as the key carers, contrary to general beliefs that people with psychosis are less likely to have an intimate partner (Office for National Statistics, 2001). The results may also suggest that partners are often the ones who shoulder most of the emotional burden as well as practical caring responsibilities.
In our analysis, BAME carers were found to have better mental wellbeing and a more positive experience of caregiving than those with a White background. However, these results should be interpreted with caution due to the relatively small proportion of BAME in our overall sample. Another salient finding concerns the poorer satisfaction with support received in carers who did not live with the CfP. While these carers provide immense support to their CfP from a distance, they might be less well-recognised by services and professionals as a carer.
Strengths and limitations
To our knowledge, this study is the first examining wellbeing and QoL of carers supporting individuals with psychosis. Our study sample comes from an England-wide digital intervention trial which prospectively collected high-quality baseline data. A principled modelling approach was used, i.e. models were not fitted to the data but rather pre-specified covariates and interactions were examined. This study was one of the first online trials of a digital intervention targeting carers and its participants may differ systematically from the wider population of carers for people with psychosis. Because of the gender imbalance, the representativeness of our sample cannot be definitely established and caution should be given to the comparison of carers’ wellbeing and QoL with HSE general population data. Most carers were recruited through 30 mental health trusts across England indicating their CfP was receiving care at the time of enrolling into the trial. These carers might have increased needs for support, hence were actively seeking help. Only carers gave consent to join the study; the data we collected on their CfP were limited. Our sample only included a small proportion of Black carers, contrary to the well-documented over-representation of people of Black African and Caribbean backgrounds diagnosed with psychosis and having poorer outcomes, yet the least likely to access carer-focused or family-based intervention (The Schizophrenia Commission, 2012; NICE, 2014). This study used a cross-sectional design and thus results imply no causal effects.
Future research and implications for clinicians and policy makers
All carers of people with psychosis should be under the care of a general practitioner (GP) and in some cases may also be in contact with mental health services and clinicians due to their caring role for their loved ones. We advocate for an increased awareness of carers’ needs across healthcare settings. We suggest that all GP practices add the details of carers for individuals with psychosis to the existing carers or SMI register (DOH, 2008, 2014) and screen for their wellbeing to aid early identification of support needs. Further large-scale prospective studies are needed to investigate and confirm associations between carers’ health and various demographic and caregiving-related outcomes including negative caregiving experience and EE. These will inform the development of a predictive model to determine risk factors and potential interventions for healthcare professionals to use as a tool. Meanwhile, our study results indicate that there are potential risk factors among carers that clinicians may benefit from paying particular attention to, including partners, lone carers and those providing more than 35 hpw caregiving. These factors identify carers most at risk of poor wellbeing and other health outcomes and also signal their diminishing coping capacity and an increased risk in them being critical to the CfP (Szmukler et al., 1996; Cooper et al., 2010; Sin et al., 2017). Our learning from this study may also be useful to other researchers in devising effective interventions which are easily accessible for carers. Using corroborating evidence from future prospective studies, design and development of future interventions should target the risk factors (e.g. lone carers) and needs (e.g. communication with the CfP) identified in the carers.
Supplementary Material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796020001067.
Acknowledgements
The authors thank all the input and contributions from the members of the Project Reference Group. They are Ellen Harris; Jacqueline Marks; Angela Ryan; Storm Ryan; Lana Samuels; Dr Clive Travis; Leigh Wallbank; and Dr Elen Williams (see http://cope-support.org/team/). We thank all the carers who joined the study.
For recruiting participants into the study, the project team acknowledges the support of the National Institute for Health Research, through the Clinical Research Network (Division 4).
Financial support
This study, as part of a bigger research programme entitled EFFIP (E-support for Families and Friends of Individuals affected by Psychosis) is funded by the National Institute for Health Research under its Post-Doctoral Research Fellowship (awarded to Dr Jacqueline Sin, reference: PDF-2015-08-035). The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health and Social Care. NIHR had no involvement in study design, collection, analysis or interpretation of data, writing the manuscript and decision to submit the manuscript for publication.
Imperial College London Open Access Fund supports the open access publication for this paper.
Footnotes
Author contributions. JS conceived the study and initiated the study design with supervision from VC. JS is the grant holder. JS, JE, RB, CH, SG, LW, TC, and VC further developed the study design and its implementation. VC and JE acted as trial statisticians and led the statistical analysis and interpretation of results. RB and AA provided input to support study conduct and data management. All authors read and approved the final manuscript. JS and VC are the guarantors.
Conflict of interest. All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf. All authors declare no conflict of interest.
Ethical standards. This study has been reviewed and approved by South Central - Oxford C Research Ethics Committee (Reference: 18/SC/0104) and Health Research Authority (Reference: IRAS 240005). Prior to study participation, all participants viewed and consented to the information that was provided in the Participant Information Sheet.
Data. The datasets generated during and/or analysed during the current study are not publicly available due to conditions on participant consent and other ethical restrictions.
References
- Bebbington PE, Kuipers E. The predictive utility of expressed emotion in schizophrenia. Psychological Medicine. 1994;24:707–718. doi: 10.1017/s0033291700027860. [DOI] [PubMed] [Google Scholar]
- Ben-Galim D, Silim A. The Sandwich Generation: Older Women Balancing Work and Care. London: Institute for Public Policy Research; 2013. [Google Scholar]
- Bowman S, Alvarez-Jimenez M, Wade D, McGorry P, Howie L. Forgotten family members: the importance of siblings in early psychosis. Early Intervention in Psychiatry. 2014;8:269–275. doi: 10.1111/eip.12068. [DOI] [PubMed] [Google Scholar]
- Bridges S. Wellbeing (Chapter 5) - Health Survey England 2012. Vol. 1 London: The Health and Social Information Centre; 2012. [Google Scholar]
- Carers Trust Key facts sbout carers. [accessed on 20 April 2020];2019 Available at https://www.carersuk.org/images/Facts_about_Carers_2019.pdf.
- Centre for Policy on Ageing. Older and Sandwich Generation Carers and the Impact of Caring. London: Centre for Policy on Ageing; 2015. [Google Scholar]
- Cooper C, Blanchard M, Selwood A, Walker Z, Livingston G. Family carers’ distress and abusive behaviour: longitudinal study. British Journal of Psychiatry. 2010;196:480–485. doi: 10.1192/bjp.bp.109.071811. [DOI] [PubMed] [Google Scholar]
- Craig R, Fuller E, Mindell J, editors. Health Survey for England 2014 - Volume 2 Methods and documentation. [Accessed on 20 April 2020];2014 Available at https://files.digital.nhs.uk/publicationimport/pub19xxx/pub19295/hse2014-methods-and-docs.pdf. [Google Scholar]
- Department of Health. Carers at the Heart of 21st-Century Families and Communities. London: DOH; 2008. [Google Scholar]
- Department of Health. The Care Act and Whole-Family Approaches. London: DoH; 2014. [Google Scholar]
- Evans-Lacko S, Little K, Meltzer H, Rose D, Rhydderch D, Henderson C, Thornicroft G. Development and psychometric properties of the Mental Health Knowledge Schedule (MAKS) Canadian Journal of Psychiatry. 2010;55:440–448. doi: 10.1177/070674371005500707. [DOI] [PubMed] [Google Scholar]
- Report of the Early Intervention in Psychosis Audit. London: NHS England; 2016. Healthcare Quality Improvement Partnership (HQIP) & Royal College of Psychiatrists. [Google Scholar]
- Henderson C, Thornicroft G. Evaluation of the time to change programme in England 2008-2011. British Journal of Psychiatry. 2013;202(Supplement 55):s45–s48. doi: 10.1192/bjp.bp.112.112896. [DOI] [PubMed] [Google Scholar]
- Joyce J, Leese M, Szmukler G. The experience of caregiving inventory: further evidence. Social Psychiatry & Psychiatric Epidemiology. 2000;35:185–189. doi: 10.1007/s001270050202. [DOI] [PubMed] [Google Scholar]
- Maheswaran H, Weich S, Powell J, Stewart-Brown S. Evaluating the responsiveness of the Warwick Edinburgh Mental Well-Being Scale (WEMWBS): group and individual level analysis. Health and Quality of Life Outcomes. 2012;10:156. doi: 10.1186/1477-7525-10-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McManus S, Bebbington P, Jenkins R, Brugha T, editors. Mental Health and Wellbeing in England: Adult Psychiatric Morbidity Survey 2014. Leeds, NHS Digital; 2016. [Google Scholar]
- National Institute for Clinical Excellence (NICE) Psychosis and Schizophrenia in Adults: Treatment and Management (National Clinical Guideline No 178) London: National Collaboration Centre for Mental Health; 2014. [Google Scholar]
- NHS Digital Health Survey for England (HSE) Adult wellbeing - Tables (version 2) [accessed on 20 April 2020];2016 Available at https://digital.nhs.uk/data-and-informa-tion/publications/statistical/health-survey-for-england/health-survey-for-england-2016.
- NHS Digital Health Survey for England (HSE) EQ-5D Dimensions. [accessed on 20 April 2020];2017 Available at https://digital.nhs.uk/data-and-information/find-data-and-pub-lications/supplementary-information/2019-supplementary-information-files/health-survey-for-england-hse-2017.
- Office for National Statistics (ONS) Socio-demographic Differences in General Practice Consultation Rates for Psychiatric Disorders among Patients Aged 16-64. London: 2001. [Google Scholar]
- Pharoah F, Mari JJ, Rathbone J, Wong W. Family intervention for schizophrenia. Cochrane Database of Systematic Reviews 2010. 2010;(12) doi: 10.1002/14651858.CD000088.pub3. Art. No.: CD000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quirk A, Smith S, Hamilton S, Lamping D, Lelliott P, Stahl D, Pinfold V, Andiappan M. Development of the Carer Well-Being and Support (CWS) Questionnaire. Mental Health Review. 2012;17:128–138. [Google Scholar]
- Roick C, Heider D, Bebbington PE, Angermeyer MC, Azorin JM, Brugha TS, Kilian R, Johnson S, Toumi M, Kornfeld A. Burden on caregivers of people with schizophrenia: comparison between Germany and Britain. British Journal of Psychiatry. 2007;190:333–338. doi: 10.1192/bjp.bp.106.025353. [DOI] [PubMed] [Google Scholar]
- Sin J, Norman I. Psychoeducational interventions for family members of people with schizophrenia: a mixed-method systematic review. Journal of Clinical Psychiatry. 2013;74:e1145–e1162. doi: 10.4088/JCP.12r08308. [DOI] [PubMed] [Google Scholar]
- Sin J, Murrells T, Spain D, Norman I, Henderson C. Wellbeing, mental health knowledge and caregiving experiences of siblings of people with psychosis, compared to their peers and parents: an exploratory study. Social Psychiatry and Psychiatric Epidemiology. 2016;51:1247–1255. doi: 10.1007/s00127-016-1222-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin J, Gillard S, Spain D, Cornelius V, Chen T, Henderson C. Effectiveness of psychoeducational interventions for family carers of people with psychosis: a systematic review and meta-analysis. Clinical Psychology Review. 2017;56:13–24. doi: 10.1016/j.cpr.2017.05.002. [DOI] [PubMed] [Google Scholar]
- Sin J, Henderson C, Spain D, Cornelius V, Chen T, Gillard S. eHealth interventions for family carers of people with long term illness: A promising approach? Clinical Psychology Review. 2018;60:109–125. doi: 10.1016/j.cpr.2018.01.008. [DOI] [PubMed] [Google Scholar]
- Sin J, Henderson C, Woodham LA, Sesé Hernández A, Gillard S. A multicomponent eHealth intervention for family carers for people affected by psychosis: a coproduced design and build study. Journal of Medical Internet Research. 2019;21:e14374. doi: 10.2196/14374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin J, Henderson C, Cornelius V, Chen T, Elkes J, Woodham LA, Sesé Hernández A, Spence-Polin D, Batchelor R, Gillard S. COPe-support - a multi-component digital intervention for family carers for people affected by psychosis: study protocol for a randomized controlled trial. BMC Psychiatry. 2020;20:129. doi: 10.1186/s12888-020-02528-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singleton N, Maung N, Cowie A, Sparks J, Bumpstead R, Meltzer H. Mental Health of Carers: The Report of A Survey Carried out by Social Survey Division of the Office for National Statistics on Behalf of the Department of Health. London: TSO; 2002. [Google Scholar]
- Smith L, Onwumere J, Craig T, McManus S, Bebbington P, Kuipers E. Mental and physical illness in caregivers: results from an English national survey sample. British Journal of Psychiatry. 2014;205:197–203. doi: 10.1192/bjp.bp.112.125369. [DOI] [PubMed] [Google Scholar]
- Stansfeld S, Smuk M, Onwumere J, Clark C, Pike C, Mcmanus S, Harris J, Bebbington P. Stressors and common mental disorder in informal carers - an analysis of the English Adult Psychiatric Morbidity Survey 2007. Social Science & Medicine. 2014;120:190–198. doi: 10.1016/j.socscimed.2014.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 15. StataCorp LLC; College Station, TX: 2017. [Google Scholar]
- Steptoe A, Deaton A, Stone AA. Psychological wellbeing, health and ageing. Lancet (London, England) 2015;385:640–648. doi: 10.1016/S0140-6736(13)61489-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szende A, Williams A, editors. Measuring Self-Reported Population Health: An International Perspective Based on EQ-5D. EuroQol Group; London: 2004. [PubMed] [Google Scholar]
- Szende A, Janssen B, Cabases J. Self-reported Population Health: An International Perspective Based on EQ-5D. Springer; Dordrecht: 2014. [PubMed] [Google Scholar]
- Szmukler G, Burgess P, Herrman H, Benson A, Colusa S, Bloch S. Caring for relatives with serious mental illness; the development of the experience of caregiving inventory. Social Psychiatry & Psychiatric Epidemiology. 1996;31:137–148. doi: 10.1007/BF00785760. [DOI] [PubMed] [Google Scholar]
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, Parkingson J, Secker J, Stewart-Brown S. The Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS): development and UK validation. Health & Quality of Life Outcome. 2007;5:63. doi: 10.1186/1477-7525-5-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Schizophrenia Commission. Rethink Mental Illness. London: 2012. The Abandoned Illness - A Report by the Schizophrenia Commission. [Google Scholar]
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, Lloyd A, Scalone L, Kind P, Pickard AS. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value in Health: The Journal of the International Society for Pharmacoeconomics and Outcomes Research. 2012;15:708–715. doi: 10.1016/j.jval.2012.02.008. [DOI] [PubMed] [Google Scholar]
- Wiedemann G, Rayki O, Feinstein E, Hahlweg K. The family questionnaire: development and validation of a new self-report scale for assessing expressed emotion. Psychiatry Research. 2002;109:265–279. doi: 10.1016/s0165-1781(02)00023-9. [DOI] [PubMed] [Google Scholar]
- Yesufu-Udechuku A, Harrison B, Mayo-Wilson E, Young N, Woodhams P, Shiers D, Kuipers E, Kendall T. Interventions to improve the experience of caring for people with severe mental illness: systematic review and meta-analysis. British Journal of Psychiatry. 2015;206:268–274. doi: 10.1192/bjp.bp.114.147561. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.