Abstract
Background
Whilst the 99th percentile is the recommended diagnostic threshold for myocardial infarction, some guidelines also advocate the use of higher troponin thresholds to rule-in myocardial infarction at presentation. It is unclear whether the magnitude or change in troponin concentration can differentiate causes of myocardial injury and infarction in practice.
Methods
In a secondary analysis of a multi-centre randomized controlled trial, we identified 46,092 consecutive patients presenting with suspected acute coronary syndrome without ST-segment elevation myocardial infarction. High-sensitivity cardiac troponin I concentrations at presentation and on serial testing were compared between patients with myocardial injury and infarction. The positive predictive value (PPV) and specificity were determined at the sexspecific 99th percentile upper reference limit (URL), and rule-in thresholds of 64 ng/L and 5-fold of the URL for a diagnosis of type 1 myocardial infarction.
Results
Troponin was above the 99th percentile in 8,188 (18%) patients. The diagnosis was type 1 or type 2 myocardial infarction in 50% and 14%, and acute or chronic myocardial injury in 20% and 16%, respectively. Troponin concentrations were similar at presentation in type 1 (median [25th percentile - 75th percentile] 91 [30-493] ng/L) and type 2 (50 [22-147] ng/L) myocardial infarction, and in acute (50 [26-134] ng/L) and chronic (51 [31-130] ng/L) myocardial injury. The 99th percentile and rule-in thresholds of 64 ng/L and 5-fold URL gave a PPV of 57% (95% confidence interval [CI] 56-58%), 59% (58-61%) and 62% (60-64%), and a specificity of 96% (96-96%), 96% (96-96%) and 98% (97-98%), respectively. The absolute, relative and rate of change in troponin concentration was highest in patients with type 1 myocardial infarction (P<0.001 for all). Discrimination improved when troponin concentration and change in troponin were combined compared to troponin concentration at presentation alone (area under curve, 0.661 [0.642-0.680] versus 0.613 [0.594-0.633]).
Conclusion
Although we observed important differences in the kinetics, cardiac troponin concentrations at presentation are insufficient to distinguish type 1 myocardial infarction from other causes of myocardial injury or infarction in practice and should not guide management decisions in isolation.
Clinical Trial Registration
URL: https://www.clinicaltrials.gov. Unique identifier: NCT01852123
Keywords: Troponin, myocardial infarction, thresholds, PPV, rule-in, kinetics, pathways
Introduction
To promote adoption of common standards, the Universal Definition of Myocardial Infarction recommends cardiac troponin testing and the 99th percentile upper reference limit (URL) as the diagnostic threshold for myocardial infarction.1 In practice, there are many causes of troponin elevation, with around half of all increases due to conditions other than type 1 myocardial infarction.2–9 Nonetheless, the early differentiation between types of myocardial infarction and acute or chronic non-ischemic myocardial injury is important as the immediate management of these conditions differs.1,10,11 Prompt treatment with anti-platelet agents, anti-coagulation and coronary revascularisation is recommended in type 1 myocardial infarction, where these may not be indicated in type 2 myocardial infarction or myocardial injury, and indeed may be contraindicated.8,12
Alternative thresholds above the 99th percentile have been proposed to improve the positive predictive value (PPV) and specificity of troponin for type 1 myocardial infarction.11,13–16 The European Society of Cardiology guidelines propose the use of rule-in thresholds above the 99th percentile to guide admission to cardiology and coronary angiography.11 These rule-in thresholds and those five-times the URL are purported to give a PPV of at least 70% and 90%, resepectively.11 They were derived in selected patients with chest pain, but in practice troponin testing is applied more widely to evaluate patients with suspected acute coronary syndrome presenting with a broader range of symptoms.3,17 Guidelines also recommend serial testing with a rise or fall in cardiac troponin needed to confirm the diagnosis of myocardial infarction.1,10,11,18 However, patients with type 2 myocardial infarction and acute non-ischemic myocardial injury also have dynamic changes in troponin concentration on serial testing.19–21 It is unclear whether rule-in thresholds or troponin kinetics can reliably differentiate between types of myocardial infarction or between myocardial injury and infarction in clinical practice.22
Our aim was to evaluate the performance of recommended cardiac troponin thresholds to rule-in the diagnosis of type 1 myocardial infarction at presentation. We also sought to determine whether the kinetics of cardiac troponin differs sufficiently to discriminate between myocardial injury and infarction.23
Methods
Transparency and openness promotion
The High-Sensitivity Troponin in the Evaluation of Patients with Suspected Acute Coronary Syndrome (High-STEACS) trial makes use of multiple routine electronic health care data sources that are linked, deidentified, and held in a national safe haven, which is accessible by approved individuals who have undertaken the necessary governance training. Summary data and the analysis code can be made available upon request from the corresponding author.
Study population and trial design
High-STEACS is a stepped-wedge cluster randomized, controlled trial that evaluated the implementation of a high-sensitivity cardiac troponin I assay in consecutive patients with suspected acute coronary syndrome across 10 secondary and tertiary care hospitals in Scotland. A detailed description of this trial has been reported elsewhere,2 but in summary, all patients attending the Emergency Department were screened for suspected acute coronary syndrome by the attending clinician at the time cardiac troponin was requested, using an electronic form integrated into the clinical care pathway. Patients were eligible for inclusion if they presented with suspected acute coronary syndrome and had paired cardiac troponin measurements from the standard care and trial assay. Patients were excluded if they had been admitted previously during the trial period or were not resident in Scotland. In this analysis, we excluded patients with ST-segment elevation myocardial infarction,24 where troponin concentration at presentation was missing, or where the adjudicators were unable to arrive at a consensus for the final diagnosis.
Measurement of cardiac troponin
Cardiac troponin testing was performed at presentation to hospital and was repeated 6 or 12 hours after the onset of symptoms at the discretion of the attending physician in accordance with national guidelines.25,26 All patients had troponin measured using a high-sensitivity cardiac troponin I assay (ARCI UTECTSTAT high-sensitive troponin I assay; Abbott Laboratories, Abbott Park, IL, USA). This assay has an inter-assay coefficient of variation of less than 10% at 4.7 ng/L, and limit of detection of 1.2 ng/L and 1.9 ng/L. For consistency with prior studies, we defined the limit of detection as any concentration <2 ng/L and for the purpose of this analysis assigned concentrations below the limit of detection a value of 1.0 ng/L.27,28 The assay has a 99 percentile URL of 26 ng/L, with sex-specific thresholds of 34 ng/L and 16 ng/L in men and women, respectively.29,30
Diagnostic adjudication
All patients with any high-sensitivity cardiac troponin I concentration above the sex-specific 99th percentile were adjudicated and classified according to the Fourth Universal Definition of Myocardial Infarction.1 Two physicians independently reviewed all clinical information, with discordant diagnoses resolved by a third physician. Type 1 myocardial infarction was defined as myocardial necrosis (any high-sensitivity cardiac troponin I concentration above the sex-specific 99th percentile with a rise or fall in troponin where serial testing was performed) in the context of a presentation with suspected acute coronary syndrome and symptoms or signs of myocardial ischemia on the electrocardiogram. Patients with myocardial necrosis, symptoms or signs of myocardial ischemia, and evidence of myocardial oxygen supply-demand imbalance secondary to an alternative condition without evidence of acute atherothrombosis were classified as type 2 myocardial infarction.21 Patients with elevated troponin concentrations without symptoms or signs of myocardial ischemia were classified as having non-ischemic myocardial injury. All nonischemic myocardial injury was classified as acute, unless troponin concentrations changed ≤20% on serial testing in accordance with the Universal Definition, or if the adjudicated diagnosis was chronic heart failure or chronic renal failure, where the classification was chronic myocardial injury. A detailed summary of the adjudication procedures is provided in the Supplemental Material.
Ethical approval
The study was approved by the Scotland A Research Ethics Committee, the Public Benefit and Privacy Panel for Health and Social Care, and by each National Health Service Health Board. Individual patient consent was not required and data from consecutive patients was collected prospectively from the electronic record, deidentified and linked within secure National Health Service Safe Havens.
Patient and public involvement
Patients and lay representatives were members of the steering committee for the trial and all related studies and were involved in the design, conduct and approval of the High-STEACS study.
Statistical Analysis
Baseline characteristics were summarized for the study population and in groups according to the diagnostic classification: type 1 myocardial infarction, type 2 myocardial infarction, acute myocardial injury, chronic myocardial injury and no myocardial injury. Group wise comparisons were performed using χ2, Kruskal-Wallis or one-way analysis of variance (one-way ANOVA) tests as appropriate. We constructed confusion matrices and calculated the PPV and specificity for type 1 myocardial infarction of a high-sensitivity cardiac troponin I concentration at presentation above the uniform 99th percentile (26 ng/L), sex-specific 99th percentile (16 ng/L in women, 34 ng/L in men), guideline recommended rule-in threshold of 64 ng/L, and 3-fold and 5-fold URL thresholds (78 and 130 ng/L, respectively). Based on prior literature we also determined the cardiac troponin concentration at presentation that met a pre-specified PPV of 75%.31 We calculated the 95% confidence interval (CI) using a Bayesian approach by sampling from a binomial likelihood with noninformative Jeffreys prior (ß-distribution shape parameters both equal to 0.5). In a sensitivity analysis, we evaluated the PPV and specificity in patients where the primary presenting symptom recorded by the attending clinician was chest pain.
In patients with serial sampling within 12 hours of presentation we used linear mixed-effects modelling with random slopes and intercepts to evaluate the relationship between symptom onset, troponin and change in troponin concentration. Non-linear associations were evaluated by adding a second-order polynomial term for time to the model. We have compared the models with and without a quadratic term for time, and the final model was chosen based on the lowest Akaike Information Criteria. To illustrate the kinetics of cardiac troponin across the groups we developed additional models for each diagnostic classification. Within each of these models we included type 2 myocardial infarction or acute or chronic myocardial injury, as a fixed effect, with type 1 myocardial infarction as the reference group. To evaluate whether relative or absolute change in troponin on serial testing improves discrimination for type 1 myocardial infarction over troponin concentration at presentation alone we used logistic regression and compared the area under the receiver operating characteristic curve (AUC). We evaluated models that incorporated relative and absolute change as continuous measure, and absolute and relative delta values of 15 ng/L and 20% as recommended in international guidelines.10,11 All analyses were performed in R (Version 3.5.1).
Results
The analysis population comprised 46,092 of the 48,242 patients enrolled in the trial after excluding those with ST-segment elevation myocardial infarction (n=925), those where the diagnosis could not be adjudicated (n=1,241), or those with missing troponin concentrations at presentation (n=24), Figure I in the Supplement).
Cardiac troponin concentrations were above the sex-specific 99th percentile URL in 8,188 (18%) patients. The adjudicated diagnosis was type 1 myocardial infarction in 50% (n=4,064), type 2 myocardial infarction in 14% (n=1,116), acute myocardial injury in 20% (n=1,676), and chronic myocardial injury in 16% (n=1,287) of patients (Table 1). Patients with type 1 myocardial infarction were younger and more likely to be men than those with type 2 myocardial infarction or acute and chronic myocardial injury. Chest pain was the primary presenting symptom in 90% of patients with type 1 myocardial infarction (3,315/3,692) and 73% in type 2 (744/1,026) myocardial infarction, but was less common in patients with acute (38%, 569/1,495) or chronic (49%, 559/1,131) myocardial injury.
Table 1. Baseline characteristics of study population stratified by adjudicated diagnosis of myocardial injury or infarction.
| All participants | Type 1 myocardial infarction | Type 2 myocardial infarction | Acute myocardial injury | Chronic myocardial injury | No myocardial injury | |
|---|---|---|---|---|---|---|
| No. of participants | 46,092 | 4,064 | 1,116 | 1,676 | 1,287 | 37,904 |
| Age (years) | 61.0 (49.0 - 75.0) | 69.0 (58.0 - 80.0) | 77.0 (67.0 - 84.0) | 78.0 (68.0 - 86.0) | 78.0 (65.5 - 85.0) | 58.0 (47.0 - 71.0) |
| Sex (Male) | 24,433 (53.0) | 2,371 (58.3) | 500 (44.8) | 664 (39.6) | 536 (41.6) | 20,341 (53.7) |
| Presenting symptoms * | ||||||
| Chest pain | 33,319 (81.6) | 3,315 (89.8) | 744 (72.5) | 569 (38.1) | 559 (49.4) | 28,091 (84.0) |
| Dyspnoea | 1,977 (4.8) | 146 (4.0) | 116 (11.3) | 372 (24.9) | 235 (20.8) | 1,107 (3.3) |
| Other | 2,003 (4.9) | 151 (4.1) | 61 (5.9) | 217 (14.5) | 116 (10.3) | 1,458 (4.4) |
| Palpitation | 1,213 (3.0) | 15 (0.4) | 67 (6.5) | 97 (6.5) | 42 (3.7) | 991 (3.0) |
| Syncope | 2,332 (5.7) | 65 (1.8) | 38 (3.7) | 240 (16.1) | 179 (15.8) | 1,808 (5.4) |
| Past medical history | ||||||
| Coronary artery disease | 11,349 (24.6) | 1,408 (34.6) | 454 (40.7) | 509 (30.4) | 492 (38.2) | 8,444 (22.3) |
| Myocardial infarction | 4,003 (8.7) | 619 (15.2) | 163 (14.6) | 161 (9.6) | 205 (15.9) | 2,832 (7.5) |
| Diabetes mellitus | 3,274 (7.1) | 708 (17.4) | 147 (13.2) | 208 (12.4) | 164 (12.7) | 2,039 (5.4) |
| Cerebrovascular disease | 2,732 (5.9) | 323 (8.0) | 135 (12.1) | 192 (11.5) | 167 (13.0) | 1,914 (5.1) |
| Hypercholesterolaemia | 18,412 (39.9) | 2,1056 (51.8) | 631 (56.5) | 852 (50.8) | 686 (53.3) | 14,0926 (37.2) |
| Heart failure | 3,908 (8.5) | 682 (16.8) | 291 (26.1) | 410 (24.5) | 363 (28.2) | 2,155(5.7) |
| Abnormal renal function | 8,398 (18.7) | 1,246 (31.2) | 536 (49.0) | 855 (52.6) | 642 (51.6) | 5,112 (13.9) |
| Previous revascularisation | ||||||
| PCI | 3,543 (7.7) | 446 (11.0) | 97 (8.7) | 94 (5.6) | 128 (9.9) | 2,743 (7.2) |
| CABG | 747 (1.6) | 101 (2.5) | 32 (2.9) | 45 (2.7) | 34 (2.6) | 534 (1.4) |
| Electrocardiogram † | ||||||
| Normal | 2,522 (37.3) | 1,519 (43.2) | 201 (19.6) | 400 (34.3) | 363 (36.8) | - |
| Myocardial ischemia | 1,740 (25.7) | 1,152 (32.8) | 379 (36.9) | 112 (9.6) | 75 (7.6) | - |
| ST depression | 1,185 (17.5) | 752 (21.4) | 278 (27.0) | 87 (7.5) | 56 (5.7) | - |
| ST elevation | 243 (3.6) | 129 (3.7) | 31 (3.0) | 38 (3.3) | 40 (4.1) | - |
| T-wave inversion | 1,191 (17.6) | 733 (20.8) | 166 (16.1) | 128 (11.0) | 148 (15.0) | - |
| Observations, haematology, and clinical chemistry | ||||||
| Systolic blood pressure, mmHg | 139.4 (28.9) | 143.3 (27.3) | 132.4 (29.9) | 135.7 (31.2) | 137.4 (28.6) | 137.5 (23.3) |
| Heart rate, bpm | 85.9 (26.4) | 78.3 (18.9) | 104.8 (35.1) | 94.2 (29.2) | 84.6 (23.9) | 77.2 (25.3) |
| Haemoglobin, g/L | 137.2 (18.2) | 135.5 (19.7) | 127.8 (25.3) | 129.7 (21.6) | 128.5 (20.6) | 138.2 (17.2) |
| Presentation troponin, ng/L | 3.0 (1.2 - 10.6) | 91.0 (30.2 - 492.5) | 49.5 (22.0 - 147.2) | 50.0 (25.5 - 134.2) | 51.1 (30.5 - 130.3) | 2.2 (1.0 - 5.1) |
| Peak troponin, ng/L | 3.6 (1.4 - 12.4) | 538.4 (85.0 - 3584.9) | 123.8 (48.1 - 599.7) | 74.0 (37.1 - 307.1) | 55.2 (34.1 - 144.7) | 2.6 (1.0 - 6.0) |
Presented as No. (%), mean±SD or median [25th percentile - 75th percentile]. Abbreviations: CABG = coronary artery bypass grafting; PCI = percutaneous coronary intervention. *Presenting symptoms are reported for the 87% (40,844/46,092) of patients where primary symptom data was available. † Electrocardiographic data reported for the 82% (6,739/8,188) patients with myocardial infarction or myocardial injury who had electrocardiographic data available. ‡ Serial testing was defined as two or more tests within 12 hours of presentation.
Troponin concentrations at presentation in myocardial injury and infarction
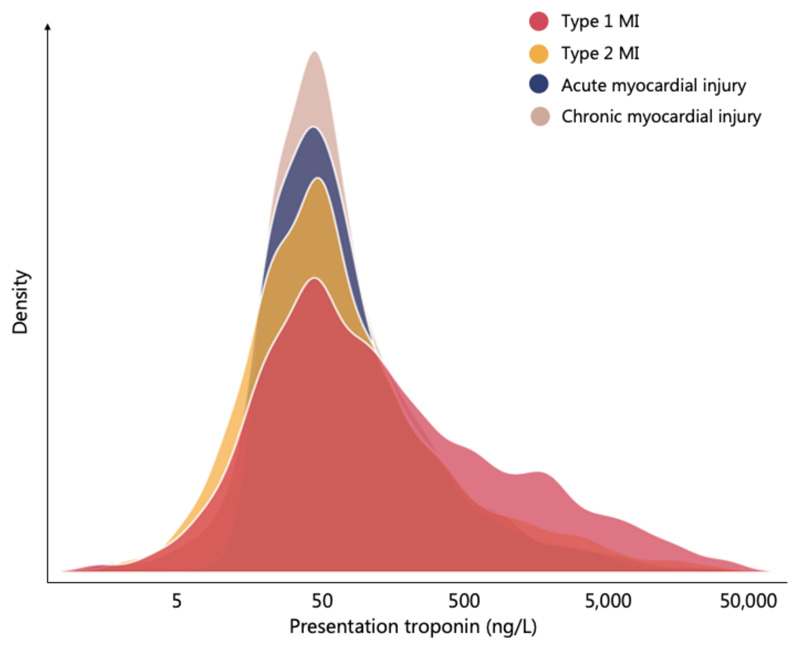
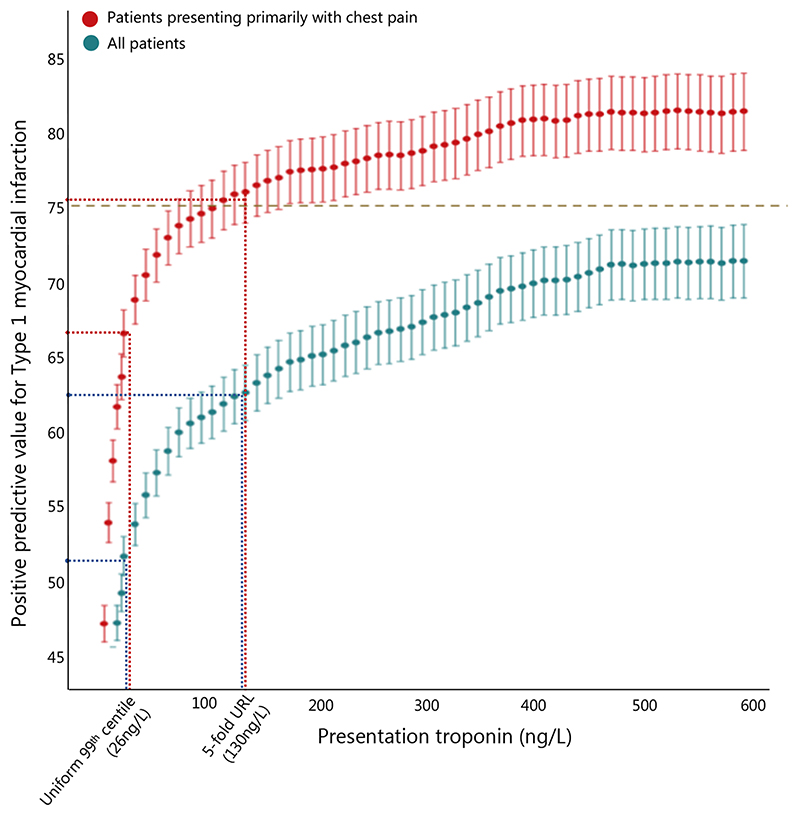
At presentation, troponin concentrations were similar in type 1 (median [25th percentile to 75th percentile] 91 [30 to 493] ng/L) and type 2 (50 [22 to 147] ng/L) myocardial infarction, and in acute (50 [26 to 134] ng/L) and chronic (51 [31 to 130] ng/L) myocardial injury (Figure 1, Table 1). A troponin concentration above the uniform 99th percentile at presentation gave a PPV of 48% and specificity of 92% for type 1 myocardial infarction (Table 2). The sex-specific 99th percentile of 16 ng/L in women gave a PPV and specificity of 39% and 89%, whereas the sexspecific 99th percentile of 34 ng/L in men gave a PPV and specificity of 56% and 93%, respectively. The rule-in threshold of 64 ng/L and 5-fold URL threshold gave PPVs of 57% and 62% respectively, with specificities of 96% and 97% (Figure 2). To achieve a PPV of 75% a rule-in threshold of 1,303 ng/L was required, whereas no threshold gave a PPV of 90% or above.
Figure 1. High-Sensitivity Cardiac Troponin I Concentrations at Presentation in Patients with Myocardial Injury and Infarction.
Kernel density plot of presentation troponin concentration stratified by the adjudicated diagnosis: type 1 myocardial infarction (red), type 2 myocardial infarction (yellow), acute myocardial injury (blue) and chronic myocardial injury (grey).
Table 2. Diagnostic performance of cardiac troponin concentration at presentation in all patients with suspected acute coronary syndrome and in those with a primary symptom of chest pain.
| Threshold | True positives | False positives | True negatives | False negatives | PPV (95% CI) | NPV (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|
| All suspected acute coronary syndrome (n=46,068) | |||||||||
| Uniform 99th percentile | 26 ng/L | 3,191 | 3,466 | 38,562 | 873 | 47.9 (46.7 to 49.1) | 97.8 (97.6 to 97.9) | 78.5 (77.2 to 79.8) | 91.8 (91.5 to 92.0) |
| Sex-specific 99th percentile | 34 ng/L (men) | 1,876 | 1,500 | 20,569 | 492 | 55.6 (53.9 to 57.3) | 97.7 (97.4 to 97.9) | 79.2 (77.6 to 80.9) | 93.2 (92.9 −93.5) |
| 16 ng/L (women) | 1,463 | 2,256 | 17,703 | 230 | 39.3 (37.8 to 40.9) | 98.7 (98.5 to 98.9) | 86.5 (84.87 to 88.0) | 88.7 (88.3 −89.1) | |
| Rule-in* | 64 ng/L | 2,308 | 1,734 | 40,294 | 1,756 | 57.1 (55.6 to 58.6) | 95.8 (95.6 to 96.0) | 56.8 (55.3 to 58.3) | 95.9 (95.7 to 96.1) |
| 3-times URL | 78 ng/L | 2,161 | 1,494 | 40,534 | 1,903 | 59.1 (57.5 to 60.7) | 95.5 (95.3 to 95.7) | 53.2 (51.6 to 54.7) | 96.4 (96.3 to 96.6) |
| 5-times URL | 130 ng/L | 1,760 | 1,073 | 40,955 | 2,304 | 62.1 (60.3 to 63.9) | 94.7 (94.5 to 94.9) | 43.3 (41.8 – 44.8) | 97.5 (97.3 to 97.6) |
| Primary symptom of chest pain (n=33,308) | |||||||||
| Uniform 99th percentile | 26 ng/L | 2,577 | 1,562 | 28,442 | 738 | 62.3 (60.8 to 63.7) | 97.5 (97.3 to 97.7) | 77.7 (76.3 to 79.1) | 94.8 (94.5 to 95.0) |
| Sex-specific 99th percentile | 34 ng/L (men) | 1,531 | 698 | 15,323 | 416 | 68.7 (66.7 to 70.6) | 97.4 (97.1 to 97.6) | 78.6 (76.8 to 80.4) | 95.7 (95.3 −96.0) |
| 16 ng/L (women) | 1,172 | 993 | 12,990 | 195 | 54.1 (52.0 to 56.2) | 98.5 (98.3 to 98.7) | 85.7 (83.8 to 87.5) | 92.9 (92.5 −93.3) | |
| Rule-in* | 64 ng/L | 1,847 | 733 | 29,271 | 1,468 | 71.6 (69.8 to 73.3) | 95.2 (95.0 to 95.5) | 55.7 (54.0 to 57.4) | 97.6 (97.4 to 97.7) |
| 3-times URL | 78 ng/L | 1,727 | 632 | 29,372 | 1,588 | 73.2 (71.4 to 75.0) | 94.9 (94.6 to 95.1) | 52.1 (50.4 to 53.8) | 97.9 (97.7 to 98.1) |
| 5-times URL | 130 ng/L | 1,388 | 447 | 29,557 | 1,927 | 75.6 (73.6 to 77.6) | 93.9 (93.6 to 94.1) | 41.9 (40.2 to 43.6) | 98.5 (98.4 to 98.6) |
Presented as number or % (95% confidence intervals) as appropriate. * rule-in threshold recommended in the ESC 0/1 hour and 0/2 early rule-out and rule-in algorithms 11 Abbreviations: PPV = positive predictive value, NPV = negative predictive value, URL = upper reference limit
Figure 2. Positive Predictive Value of High-Sensitivity Cardiac Troponin I Concentration at Presentation for a Diagnosis of Type 1 Myocardial Infarction.
Positive predictive value and 95% confidence intervals of high-sensitivity cardiac troponin I concentration at presentation for type 1 myocardial infarction in all patients with suspected acute coronary syndrome (blue) and in those with a primary symptom of chest pain (red). The dotted lines illustrate the positive predictive value of the uniform 99th percentile and 5-fold upper reference limit (URL).
In a sensitivity analysis restricted to 82% (33,319/40,844) of patients in whom the primary presenting symptom was chest pain (Table I in the Supplement), the PPV and specificity for type 1 myocardial infarction at the rule-in threshold of 64 ng/L was 72% and 98%, respectively (Table 2). The 5-fold URL threshold gave a PPV of 75% and a specificity of 99%. A rule-in threshold of 119 ng/L gave a PPV of 75%, but no threshold achieved a PPV of 90% in this population (Figure 2).
Troponin kinetics in myocardial injury and infarction
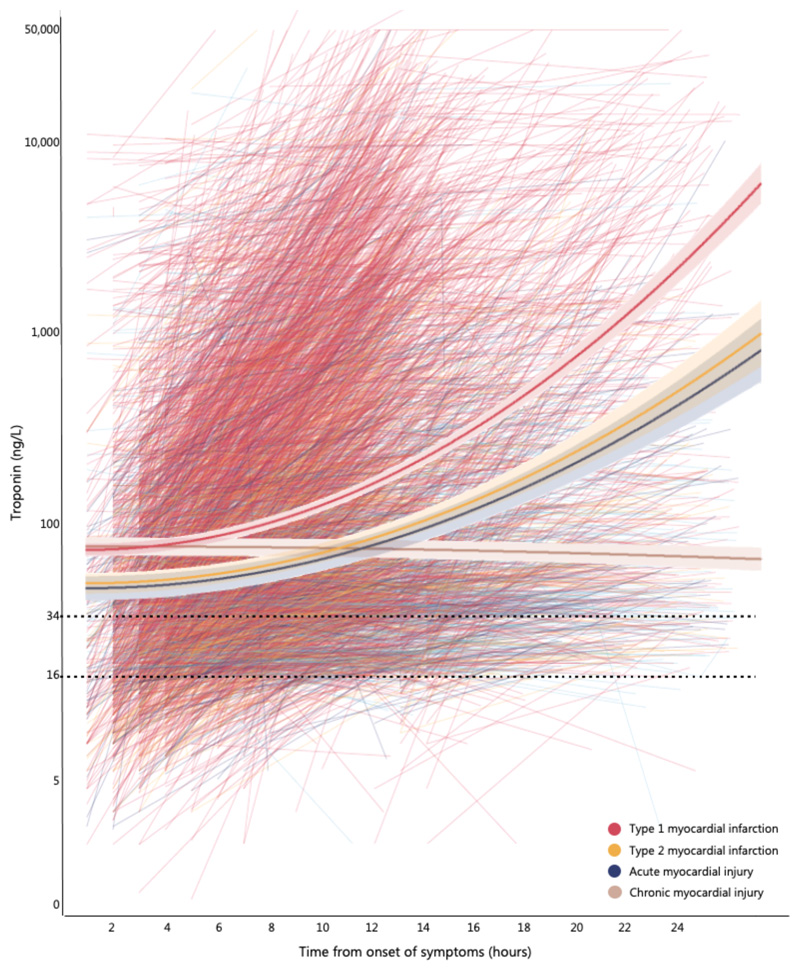
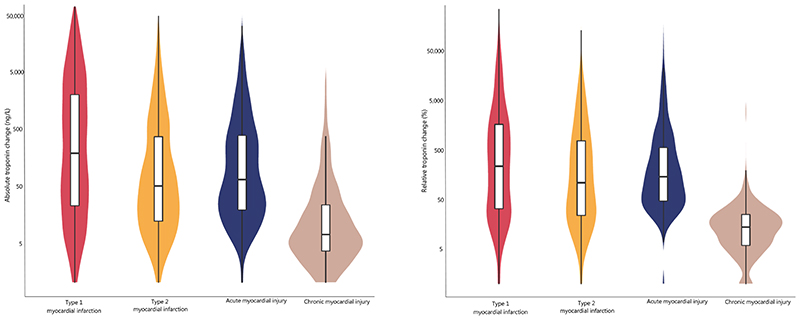
Serial troponin testing within 12 hours of presentation was performed in 4,187 (51%) patients with concentrations above the sex-specific 99th percentile. The time from symptom onset to initial troponin sampling was similar in patients with type 1 and type 2 myocardial infarction and acute myocardial injury (240 [180 to 420] minutes), but was longer in patients with chronic myocardial injury (300 [180 to 780] minutes). The rate of change in troponin within 12 hours of presentation was highest in patients with type 1 myocardial infarction, as compared to type 2 myocardial infarction and acute or chronic myocardial injury (P<0.001 for all, Figure 3). The absolute change in troponin concentration differed in patients with type 1 myocardial infarction (177 [21 to 1,929] ng/L), as compared to type 2 myocardial infarction (46 [10 to 365] ng/L), acute non-ischemic myocardial injury (57 [17 to 384] ng/L) and chronic myocardial injury (6 [2 to 22] ng/L) (P<0.001 for all Figure 4). The relative change in troponin concentration also differed between patients with type 1 myocardial infarction (231 [31 to 1,602] %), as compared to as compared to type 2 myocardial infarction (105 [22 to 656] %), acute non-ischemic myocardial injury (129 [45 to 534] %), and chronic myocardial injury (12 [5 to 24] %)(P<0.001 for all).
Figure 3. Kinetics of High-Sensitivity Cardiac Troponin I Concentration from Symptom Onset in Patients with Myocardial Injury and Infarction.
Spaghetti plot illustrating high-sensitivity cardiac troponin I concentrations in relation to the time of symptom onset in individual patients stratified by the adjudicated diagnosis: type 1 myocardial infarction (red), type 2 myocardial infarction (yellow), acute myocardial injury (blue) and chronic myocardial injury (grey). The plot is restricted to those patients where any troponin concentration was above the sex-specific 99th percentile concentration during serial testing within 12 hours of presentation, and where the time of symptom onset was known (n=3,845). Linear mixed-effects modeling was done using random intercepts and random slopes, including quadratic terms for time, with cardiac troponin I as outcome. The output from a linear mixed-effects model incorporating time from symptom onset, troponin and change in troponin concentration is overlaid for each condition. For each condition, the final model to estimate the trajectory of cardiac troponin I was chosen based on the Akaike Information Criteria.
Figure 4. Absolute and Relative Change in High-Sensitivity Cardiac Troponin I Concentration on Serial Testing in Patients with Myocardial Injury and Infarction.
Violin-density and box and whisker plots illustrating the absolute and relative change in high-sensitivity cardiac troponin I concentration on serial testing in patients stratified by the adjudicated diagnosis: type 1 myocardial infarction (red), type 2 myocardial infarction (yellow), acute myocardial injury (blue) and chronic myocardial injury (grey)
Combining troponin concentration at presentation with an absolute change in troponin on serial testing of ≥15 ng/L, or relative change of ≥20% improved discrimination for type 1 myocardial infarction compared to troponin concentration at presentation alone (0.646 [0.627 to 0.666] and AUC 0.661 [0.642 to 0.680] respectively, versus 0.613 [0.594 to 0.633], Figure II in the Supplement).
Discussion
In consecutive patients with suspected acute coronary syndrome we evaluated whether troponin concentrations at presentation or their kinetics differed sufficiently to discriminate between myocardial injury and infarction. We report a number of observations that are relevant to practice. First, troponin concentrations at presentation are similar in patients with myocardial injury or infarction regardless of the diagnostic classification. Second, the use of recommended rule-in thresholds above the 99th percentile provide only marginal improvements in the PPV and specificity for type 1 myocardial infarction. Troponin thresholds >1,000 ng/L would be required to achieve a PPV of 75% or more. Third, the magnitude and rate of change of troponin can help differentiate type 1 from type 2 myocardial infarction, and acute or chronic myocardial injury. Whilst we observed important differences in troponin kinetics, the troponin concentration at presentation provides only limited discrimination between type 1 myocardial infarction and other causes of myocardial injury or infarction. Clinical context may be more helpful than any given rule-in threshold to guide the triage and initial management of patients with suspected acute coronary syndrome in practice.
In contrast to the previous generation of cardiac troponin assays, high-sensitivity assays are able to precisely measure troponin at very low concentrations. Accelerated diagnostic pathways that harness this enhanced precision to enable earlier decisions to rule-out and rule-in myocardial infarction are now used widely around the world and have been recommended by international guidelines.1,11,32,33 The diagnostic performance of these pathways has been validated in multiple observational studies,16,34–38 and the effectiveness and safety of ruling out myocardial infarction earlier demonstrated in randomized controlled trials.39,40 However, the only prior randomized trial to evaluate the effectiveness of applying the 99th percentile to rule-in myocardial infarction did not demonstrate better outcomes.41
The major advantage of accelerated diagnostic pathways using high-sensitivity cardiac troponin testing is that they improve confidence to rule out myocardial infarction and reduce the need for admission to hospital.24,39,40 However, the use of lower thresholds to diagnose myocardial infarction has identified more patients with elevated cardiac troponin concentrations due to other conditions.2,3,9 As such, thresholds above the 99th percentile have been proposed to improve the specificity and positive predictive value and to accelerate the rule-in of myocardial infarction. Assay specific rule-in thresholds are recommended by the European Society of Cardiology practice guidelines, which also advocate that patients with troponin concentrations above these thresholds at presentation are triaged to a coronary care unit and undergo coronary angiography.11 However, the performance of these rule-in thresholds has not been evaluated in clinical practice, where testing is often performed in a broader group of patients. Our findings are consistent with the concept that underpins these recommendations - the higher the troponin concentration at presentation, the higher the likelihood of type 1 myocardial infarction. However, the PPV of the rule-in threshold was 57%, and was considerably lower than the 77% and 70% reported in the derivation and validation of this rule-in threshold.42 Our observations are consistent with a recent study level meta-analysis, which reported that the PPV of the rule-in component of a multi-threshold 0/1 hour pathway using a high-sensitivity cardiac troponin T assay was 51%.43 However, this was not a patient level analysis, and the performance of the rulein threshold in isolation was not reported. Interestingly, when our patient population was restricted to the 33,308 patients presenting with a primary symptoms of chest pain to enable direct comparison with those studies in which the rule-in threshold was defined, we observed a substantial improvement in the PPV to 72%. Taken together these observations highlight the importance of interpreting cardiac troponin in context and the merits of evaluating the performance of diagnostic tests in the population in which they are applied in practice.
In consecutive patients with suspected acute coronary syndrome half of all patients with elevated cardiac troponin concentrations had a diagnosis of type 2 myocardial infarction or acute and and chronic non-ischemic myocardial injury. Our findings are consistent with those from the Biomarkers in Acute Cardiac Care (BACC) study where just 29% of patients with an elevated cardiac troponin T concentration had a diagnosis of type 1 myocardial infarction.44 Whilst we observed that troponin concentrations were higher in type 1 myocardial infarction there was substantial overlap with type 2 myocardial infarction and myocardial injury suggesting troponin alone at any threshold cannot reliably discriminate between these conditions. Even at a threshold 5-times the URL, purported to have a PPV of over 90%,11 we observed that the PPV was just 62% for type 1 myocardial infarction. A threshold more than 50-times the URL would be required to achieve a PPV of 75% when applied to all patients with suspected acute coronary syndrome.
Whilst our observations highlight the limitations of using single troponin measurements to triage patients, confirmation of the diagnosis of myocardial infarction requires serial testing and a rise or fall in cardiac troponin.1 We observed differences in the rate of troponin release with a higher rate of change, as well as larger absolute and relative changes on serial sampling, in patients with type 1 myocardial infarction compared to type 2 myocardial infarction or acute and chronic myocardial injury. Despite these differences, the use of relative or absolute delta change criteria only marginally improved discrimination compared with the troponin concentration alone. This is perhaps not surprising given the observed changes in troponin concentration on serial testing in both type 2 myocardial infarction and in acute myocardial injury. Whilst previous studies using a contemporary sensitive troponin assay in a small cohort of 66 and 188 patients with type 1 and type 2 myocardial infarction, respectively, suggested no improvement in discrimination when change in troponin at 3 or 6 hours was combined with the absolute concentration,45 we observed a modest improvement. It would seem unlikely that the shorter time intervals between serial testing would improve discrimination, but this should be evaluated in future studies.
In recent years a number of approaches have been proposed that could enable clinicians to use cardiac troponin more flexibly.31,46,47 These approaches recognize the limitations of applying fixed thresholds to triage a heterogenous population of patients and the challenge of performing serial testing at precise intervals in clinical practice. The Troponin only-Manchester Acute Coronary Syndrome (T-MACS) rule uses logistic regression to provide individual patient risk estimates for non-ST-segment elevation myocardial infarction, by incorporating age, sex, clinical variables, and a measure of high-sensitivity cardiac troponin T at presentation. The T-MACS rule performs well, but does not discriminate type 1 myocardial infarction from other causes of troponin elevation or take into account serial testing.47 In a collaborative analysis that pooled data from multiple cohorts, the Calculation of Myocardial Infarction Risk Probabilities to Manage Patients With Suspicion of Myocardial Infarction (COMPASS-MI) investigators highlight that a more flexible approach is required and demonstrate proof of concept that the negative and positive predictive values for type 1 myocardial infarction vary across a range of thresholds and delta change in troponin values.46 Finally, the myocardial-ischemic-injury-index (MI3) uses a gradient boosting machine learning algorithm to combine age, sex and paired high-sensitivity cardiac troponin I values to compute a value (0-100) that reflects the likelihood of type 1 myocardial infarction for an individual patient.31 Serial testing can be performed at any time point and the algorithm incorporates a measure of rate of change in troponin. Whilst each of these approaches show considerable promise it is unclear at present whether the use of these probabilistic scores in practice improves clinical decisions compared to existing guideline recommended pathways using fixed thresholds.
We recognize some strengths and limitations of this study. First, we enrolled consecutive patients in whom the attending clinician suspected acute coronary syndrome by embedding our screening tool into the electronic health care system. This avoided selection bias and ensured that our study population was representative. Second, all diagnoses were adjudicated according to the Fourth Universal Definition of Myocardial Infarction ensuring our findings are relevant to contemporary practice. Whilst few patients had missing troponin values for the evaluation of rule-in thresholds (0.1%), serial testing was performed at the discretion of the attending clinician and was only performed in 53% of patients with myocardial injury or infarction. It is likely that those patients undergoing serial testing differed from those who had a single test performed, however our comparison between patients with type 1 and type 2 myocardial infarction and those with myocardial injury was limited to the subgroup of patients with 2 or more tests performed within 12-hours of presentation. Importantly cardiac troponin was measured using a single high-sensitivity cardiac troponin I assay, and we recognize that the performance of rule-in thresholds for myocardial infarction are likely to differ for other assays. Finally, the approach to patient selection for cardiac troponin testing will vary across healthcare systems, and we would recommend some caution in extrapolating the performance of rule-in thresholds to sites where testing is performed more widely.
In conclusion, although we observed important differences in the kinetics, cardiac troponin concentrations at presentation are insufficient to distinguish type 1 myocardial infarction from other causes of myocardial injury or infarction in practice. Clinical context may be more helpful than any rule-in threshold when guiding initial triage and management decisions.
Supplementary Material
Clinical perspective.
What is new?
In 46,092 consecutive patients with suspected acute coronary syndrome we evaluated the performance of the 99th percentile rule-in threshold, and thresholds of 64 ng/L and 5-times the upper reference limit, for the diagnosis of type 1 myocardial infarction.
Troponin concentrations at presentation have a low positive predictive value for type 1 myocardial infarction, and a threshold 50-times the upper reference limit is required to achieve a positive predictive value ≥70%.
Change in troponin on serial testing only marginally improves positive predictive value for type 1 myocardial infarction over presenting troponin alone (area under curve, 0.661 [0.642 to 0.680] versus 0.613 [0.594 to 0.633])
What Are the Clinical Implications?
Troponin concentrations at presentation are insufficient to distinguish type 1 myocardial infarction from other causes of myocardial injury or infarction and should not be used in isolation to guide management decisions in patients with suspected acute coronary syndrome.
Consideration of other important clinical factors may be more helpful than any rule-in threshold to guide initial triage and management.
Aknowledgments
RW, FSA, POC, DK, ARC and NLM conceived the study and its design. RW, DK and ARC had access to the data and performed the analysis. RW, DK, ARC and NLM interpreted the data and drafted the manuscript. All authors revised the manuscript critically for important intellectual content and provided their final approval of the version to be published. All authors are accountable for the work. We thank the High-STEACS Investigators for their contributions to the conception or design of the work, or the acquisition, analysis, or interpretation of data for the work.
Funding sources
The High-STEACS trial was funded by a Special Project Grant from the British Heart Foundation (SP/12/10/29922). RW, AB and DD are supported by Clinical Research Training Fellowships (MR/V007017/1, MR/V007254/1) and a PhD studentship (MR/N013166/1) from the Medical Research Council. KL is supported by a Clinical Research Training Fellowship (FS/18/25/33454) from the British Heart Foundation. DMK is supported by a grant from Health Data Research UK, which receives its funding from Health Data ResearchUK Ltd (HDR-5012) funded by the UK Medical Research Council, Engineering and Physical Sciences Research Council, Economic and Social Research Council, Department of Health and Social Care (England), Chief Scientist Office of the Scottish Government Health and Social Care Directorates, Health and Social Care Research and Development Division (Welsh Government), Public Health Agency (Northern Ireland), British Heart Foundation and the Wellcome Trust. ARC receives support from a Starter Grant for Clinical Lecturers by the Academy of Medical Sciences (SGL021/1075). NLM is supported by the Butler British Heart Foundation Senior Clinical Research Fellowship (FS/16/14/32023), a Programme Grant (RG/20/10/34966) and a Research Excellence Award (RE/18/5/34216) from the British Heart Foundation. Abbott Laboratories provided cardiac troponin assay reagents, calibrators, and controls without charge.
Non-standard abbreviaitons and acronyms:
- PPV
positive predictive value
- NPV
negative predictive value
- ESC
European Society of Cardiology
- URL
upper reference limit
- ng/L
nanograms per litre
- g/L
grams per litre
- CABG
coronary artery bypass grafting
- PCI
percutaneous coronary intervention
Footnotes
Disclosures
NLM has received honoraria from Abbott Diagnostics, Siemens Healthineers, Roche Diagnostics and LumiraDx and the University of Edinburgh has received research grants from Abbott Diagnostics and Siemens Healthineers.
Role of Funder
The funders played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- 1.Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD. Fourth universal definition of myocardial infarction (2018) European Heart Journal. 2019;40:237–269. doi: 10.1093/eurheartj/ehy462. [DOI] [PubMed] [Google Scholar]
- 2.Chapman AR, Adamson PD, Shah ASV, Anand A, Strachan FE, Ferry AV, Ken Lee K, Berry C, Findlay I, Cruikshank A, Reid A, et al. High-Sensitivity Cardiac Troponin and the Universal Definition of Myocardial Infarction. Circulation. 2020;141:161–171. doi: 10.1161/CIRCULATIONAHA.119.042960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shah ASV, Sandoval Y, Noaman A, Sexter A, Vaswani A, Smith SW, Gibbins M, Griffiths M, Chapman AR, Strachan FE, Anand A, et al. Patient selection for high sensitivity cardiac troponin testing and diagnosis of myocardial infarction: prospective cohort study. BMJ (Clinical research ed) 2017;359:j4788. doi: 10.1136/bmj.j4788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mills NL, Lee KK, McAllister DA, Churchhouse AMD, MacLeod M, Stoddart M, Walker S, Denvir MA, Fox KAA, Newby DE. Implications of lowering threshold of plasma troponin concentration in diagnosis of myocardial infarction: Cohort study. BMJ (Online) 2012;344 doi: 10.1136/bmj.e1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah ASV, McAllister DA, Mills R, Lee KK, Churchhouse AMD, Fleming KM, Layden E, Anand A, Fersia O, Joshi NV, Walker S, et al. Sensitive Troponin Assay and the Classification of Myocardial Infarction. American Journal of Medicine. 2015;128:493–501.:e3. doi: 10.1016/j.amjmed.2014.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sandoval Y, Jaffe AS. Type 2 Myocardial Infarction: JACC Review Topic of the Week. Journal of the American College of Cardiology. 2019;73:1846–1860. doi: 10.1016/j.jacc.2019.02.018. [DOI] [PubMed] [Google Scholar]
- 7.McCarthy CP, Vaduganathan M, Januzzi JL. Type 2 myocardial infarction — Diagnosis, prognosis, and treatment. JAMA - Journal of the American Medical Association. 2018;320:433–434. doi: 10.1001/jama.2018.7125. [DOI] [PubMed] [Google Scholar]
- 8.DeFilippis AP, Chapman AR, Mills NL, De Lemos JA, Arbab-Zadeh A, Newby LK, Morrow DA. Assessment and treatment of patients with type 2 myocardial infarction and acute nonischemic myocardial injury. Circulation. 2019;140:1661–1678. doi: 10.1161/CIRCULATIONAHA.119.040631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taggart C, Wereski R, Mills NL, Chapman AR. Diagnosis, Investigation and Management of Patients with Acute and Chronic Myocardial Injury. Journal of Clinical Medicine. 2021;10:2331. doi: 10.3390/jcm10112331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Ganiats TG, Holmes DR, Jaffe AS, Jneid H, Kelly RF, Kontos MC, Levine GN, et al. 2014 AHA/ACC Guideline for the Management of Patients With Non-ST-Elevation Acute Coronary Syndromes: Executive Summary. Circulation. 2014;130:2354–2394. doi: 10.1161/CIR.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 11.Collet J-P, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, Dendale P, Dorobantu M, Edvardsen T, Folliguet T, Gale CP, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. European Heart Journal. 2020:1–79. [Google Scholar]
- 12.Chapman AR, Sandoval Y. Type 2 Myocardial Infarction: Evolving Approaches to Diagnosis and Risk-Stratification. Clinical chemistry. 2021;67:61–69. doi: 10.1093/clinchem/hvaa189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boeddinghaus J, Twerenbold R, Nestelberger T, Koechlin L, Wussler D, Meier M, Troester V, Zimmermann T, Badertscher P, Wildi K, Giménez MR, et al. Clinical use of a new high-sensitivity cardiac troponin I assay in patients with suspected myocardial infarction. Clinical Chemistry. 2019;65:1426–1436. doi: 10.1373/clinchem.2019.304725. [DOI] [PubMed] [Google Scholar]
- 14.Boeddinghaus J, Nestelberger T, Twerenbold R, Neumann JT, Lindahl B, Giannitsis E, Sörensen NA, Badertscher P, Jann JE, Wussler D, Puelacher C, et al. Impact of age on the performance of the ESC 0/1h-algorithms for early diagnosis of myocardial infarction. European Heart Journal. 2018;39:3780–3794. doi: 10.1093/eurheartj/ehy514. [DOI] [PubMed] [Google Scholar]
- 15.Boeddinghaus J, Reichlin T, Cullen L, Greenslade JH, Parsonage WA, Hammett C, Pickering JW, Hawkins T, Aldous S, Twerenbold R, Wildi K, et al. Two-Hour Algorithm for Triage toward Rule-Out and Rule-In of Acute Myocardial Infarction by Use of High-Sensitivity Cardiac Troponin I. Clinical Chemistry. 2016;62:494–504. doi: 10.1373/clinchem.2015.249508. [DOI] [PubMed] [Google Scholar]
- 16.Twerenbold R, Neumann JT, Sörensen NA, Ojeda F, Karakas M, Boeddinghaus J, Nestelberger T, Badertscher P, Rubini Giménez M, Puelacher C, Wildi K, et al. Prospective Validation of the 0/1-h Algorithm for Early Diagnosis of Myocardial Infarction. Journal of the American College of Cardiology. 2018;72:620–632. doi: 10.1016/j.jacc.2018.05.040. [DOI] [PubMed] [Google Scholar]
- 17.Sandoval Y, Smith SW, Schulz K, Sexter A, Apple FS. Rapid Identification of Patients at High Risk for Acute Myocardial Infarction Using a Single High-Sensitivity Cardiac Troponin I Measurement. Clinical Chemistry. 2020;66:620–622. doi: 10.1093/clinchem/hvaa045. [DOI] [PubMed] [Google Scholar]
- 18.Cullen LA, Mills NL, Mahler S, Body R. Early rule-out and rule-in strategies for myocardial infarction. Clinical Chemistry. 2017;63:129–139. doi: 10.1373/clinchem.2016.254730. [DOI] [PubMed] [Google Scholar]
- 19.Felker GM, Mentz RJ, Teerlink JR, Voors AA, Pang PS, Ponikowski P, Greenberg BH, Filippatos G, Davison BA, Cotter G, Prescott MF, et al. Serial high sensitivity cardiac troponin T measurement in acute heart failure: Insights from the RELAX-AHF study. European Journal of Heart Failure. 2015;17:1262–1270. doi: 10.1002/ejhf.341. [DOI] [PubMed] [Google Scholar]
- 20.Thelin J, Melander O. Dynamic high-sensitivity troponin elevations in atrial fibrillation patients might not be associated with significant coronary artery disease. BMC Cardiovascular Disorders. 2017;17:1–9. doi: 10.1186/s12872-017-0601-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chapman AR, Adamson PD, Mills NL. Assessment and classification of patients with myocardial injury and infarction in clinical practice. Heart. 2017;103:10–18. doi: 10.1136/heartjnl-2016-309530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sandoval Y, Smith SW, Schulz KM, Murakami MM, Love SA, Nicholson J, Apple FS. Diagnosis of Type 1 and Type 2 Myocardial Infarction Using a High-Sensitivity Cardiac Troponin I Assay with Sex-Specific 99th Percentiles Based on the Third Universal Definition of Myocardial Infarction Classification System. Clinical Chemistry. 2015;61:657–663. doi: 10.1373/clinchem.2014.236638. [DOI] [PubMed] [Google Scholar]
- 23.Sandoval Y, Smith SW, Sexter A, Schulz K, Apple FS. Use of objective evidence of myocardial ischemia to facilitate the diagnostic and prognostic distinction between type 2 myocardial infarction and myocardial injury. European Heart Journal: Acute Cardiovascular Care. 2020;9:62–69. doi: 10.1177/2048872618787796. [DOI] [PubMed] [Google Scholar]
- 24.Wereski R, Chapman AR, Lee KK, Smith SW, Lowe DJ, Gray A, Mills NL. High-Sensitivity Cardiac Troponin Concentrations at Presentation in Patients with ST-Segment Elevation Myocardial Infarction. JAMA Cardiology. 2020;5:1302–1304. doi: 10.1001/jamacardio.2020.2867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Healthcare Improvment Scotland. Scottish Intercollegiate Guidelines Network (SIGN) 93 Acute coronary syndrome national clinical guideline. SIGN Guidelines. 2013 [Google Scholar]
- 26.Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, Caso P, Dudek D, Gielen S, Huber K, Ohman M, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. European Heart Journal. 2011;32:2999–3054. doi: 10.1093/eurheartj/ehr236. [DOI] [PubMed] [Google Scholar]
- 27.Bularga A, Lee KK, Stewart S, Ferry AV, Chapman AR, Marshall L, Strachan FE, Cruickshank A, Maguire D, Berry C, Findlay I, et al. High-Sensitivity Troponin and The Application of Risk Stratification Thresholds in Patients with Suspected Acute Coronary Syndrome. Circulation. 2019:1557–1568. doi: 10.1161/CIRCULATIONAHA.119.042866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sandoval Y, Smith SW, Shah ASV, Anand A, Chapman AR, Love SA, Schulz K, Cao J, Mills NL, Apple FS. Rapid rule-out of acute myocardial injury using a single high-sensitivity cardiac troponin i measurement. Clinical Chemistry. 2017;63:369–376. doi: 10.1373/clinchem.2016.264523. [DOI] [PubMed] [Google Scholar]
- 29.Chin CWL, Shah ASV, McAllister DA, Cowell SJ, Alam S, Langrish JP, Strachan FE, Hunter AL, Choy AM, Lang CC, Walker S, et al. High-sensitivity troponin i concentrations are a marker of an advanced hypertrophic response and adverse outcomes in patients with aortic stenosis. European Heart Journal. 2014;35:2312–2321. doi: 10.1093/eurheartj/ehu189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shah ASV, Griffiths M, Lee KK, McAllister DA, Hunter AL, Ferry AV, Cruikshank A, Reid A, Stoddart M, Strachan F, Walker S, et al. High sensitivity cardiac troponin and the under-diagnosis of myocardial infarction in women: prospective cohort study. BMJ. 2015;350:g7873. doi: 10.1136/bmj.g7873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Than MP, Pickering JW, Sandoval Y, Shah ASV, Tsanas A, Apple FS, Blankenberg S, Cullen L, Mueller C, Neumann JT, Twerenbold R, et al. Machine Learning to Predict the Likelihood of Acute Myocardial Infarction. Circulation. 2019:899–909. doi: 10.1161/CIRCULATIONAHA.119.041980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Institute of Clinical Excellence. Acute Coronary Syndromes. NICE Guidelines. 2020:NG185 [Google Scholar]
- 33.Apple FS, Collinson PO, Kavsak PA, Body R, Ordóñez-Llanos J, Saenger AK, Omland T, Hammarsten O, Jaffe AS. The IFCC Clinical Application of Cardiac Biomarkers Committee’s Appraisal of the 2020 ESC Guidelines for the Management of Acute Coronary Syndromes in Patients Presenting Without Persistent ST-segment Elevation: Getting Cardiac Troponin Right. Clinical Chemistry. 2021;67:730–735. doi: 10.1093/clinchem/hvaa337. [DOI] [PubMed] [Google Scholar]
- 34.Chapman AR, Anand A, Boeddinghaus J, Ferry AV, Sandeman D, Adamson PD, Andrews J, Tan S, Cheng SF, D’Souza M, Orme K, et al. Comparison of the efficacy and safety of early rule-out pathways for acute myocardial infarction. Circulation. 2017;135:1586–1596. doi: 10.1161/CIRCULATIONAHA.116.025021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haller PM, Boeddinghaus J, Neumann JT, Sörensen NA, Hartikainen TS, Goßling A, Nestelberger T, Twerenbold R, Lehmacher J, Keller T, Zeller T, et al. Performance of the ESC 0/1-h and 0/3-h algorithm for the rapid identification of myocardial infarction without ST-elevation in patients with diabetes. Diabetes Care. 2020;43:460–467. doi: 10.2337/dc19-1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Twerenbold R, Badertscher P, Boeddinghaus J, Nestelberger T, Wildi K, Puelacher C, Sabti Z, Rubini Gimenez M, Tschirky S, Du Fay De Lavallaz J, Kozhuharov N, et al. 0/1-Hour Triage Algorithm for Myocardial Infarction in Patients with Renal Dysfunction. Circulation. 2018;137:436–451. doi: 10.1161/CIRCULATIONAHA.117.028901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Twerenbold R, Costabel JP, Nestelberger T, Campos R, Wussler D, Arbucci R, Cortes M, Boeddinghaus J, Baumgartner B, Nickel CH, Bingisser R, et al. Outcome of Applying the ESC 0/1-hour Algorithm in Patients With Suspected Myocardial Infarction. Journal of the American College of Cardiology. 2019;74:483–494. doi: 10.1016/j.jacc.2019.05.046. [DOI] [PubMed] [Google Scholar]
- 38.Pickering JW, Greenslade JH, Cullen L, Flaws D, Parsonage W, Aldous S, George P, Worster A, Kavsak PA, Than MP. Assessment of the European Society of Cardiology 0-Hour/1-Hour Algorithm to Rule-Out and Rule-In Acute Myocardial Infarction. Circulation. 2016;134:1532–1541. doi: 10.1161/CIRCULATIONAHA.116.022677. [DOI] [PubMed] [Google Scholar]
- 39.Anand A, Lee KK, Chapman AR, Ferry AV, Adamson PD, Strachan FE, Berry C, Findlay I, Cruickshank A, Reid A, Collinson PO, et al. High-Sensitivity Cardiac Troponin on Presentation to Rule Out Myocardial Infarction: A Stepped-Wedge Cluster Randomized Controlled Trial. Circulation. 2021;143:2214–2224. doi: 10.1161/CIRCULATIONAHA.120.052380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chew DP, Papendick C, Blyth A, Seshadri A, Edmonds MJR, Briffa T, Cullen LA, Quinn S, Karnon J, Chuang A, Nelson AJ, et al. A randomized trial of a 1-hour troponin T protocol in suspected acute coronary syndromes: Design of the Rapid Assessment of Possible ACS In the emergency Department with high sensitivity Troponin T (RAPID-TnT) study. Circulation. 2019;140:1543–1556. doi: 10.1161/CIRCULATIONAHA.119.042891. [DOI] [PubMed] [Google Scholar]
- 41.Shah ASV, Anand A, Strachan FE, Ferry AV, Lee KK, Chapman AR, Sandeman D, Stables CL, Adamson PD, Andrews JPM, Anwar MS, et al. High-sensitivity troponin in the evaluation of patients with suspected acute coronary syndrome: a stepped-wedge, cluster-randomised controlled trial. The Lancet. 2018;392:919–928. doi: 10.1016/S0140-6736(18)31923-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jaeger C, Wildi K, Twerenbold R, Reichlin T, Rubini Gimenez M, Neuhaus JD, Grimm K, Boeddinghaus J, Hillinger P, Nestelberger T, Singeisen H, et al. One-hour rule-in and rule-out of acute myocardial infarction using high-sensitivity cardiac troponin I. American Heart Journal. 2016;171:92–102.:e5. doi: 10.1016/j.ahj.2015.07.022. [DOI] [PubMed] [Google Scholar]
- 43.Chiang C-H, Chiang C-H, Gi W-T, Wu Y-K, Huang S-S, Yeo YH, Lee C-C. Safety and efficacy of the European Society of Cardiology 0/1-Hour algorithm for diagnosis of myocardial infarction: systematic review and meta-analysis Coronary artery disease. doi: 10.1136/heartjnl-2019-316343. [DOI] [PubMed] [Google Scholar]
- 44.Hartikainen TS, Sorensen NA, Haller PM, Goßling A, Lehmacher J, Zeller T, Blankenberg S, Westermann D, Neumann JT. Clinical application of the 4th universal definition of myocardial infarction. European Heart Journal. 2020;41:2209–2216. doi: 10.1093/eurheartj/ehaa035. [DOI] [PubMed] [Google Scholar]
- 45.Sandoval Y, Thordsen SE, Smith SW, Schulz KM, Murakami maryann M, Pearce LA, Apple FS. Cardiac troponin changes to distinguish type 1 and type 2 myocardial infarction and 180-day mortality risk. European Heart Journal: Acute Cardiovascular Care. 2014;3:317–325. doi: 10.1177/2048872614538411. [DOI] [PubMed] [Google Scholar]
- 46.Neumann JT, Twerenbold R, Ojeda F, Sörensen NA, Chapman AR, Shah ASV, Anand A, Boeddinghaus J, Nestelberger T, Badertscher P, Mokhtari A, et al. Application of High-Sensitivity Troponin in Suspected Myocardial Infarction. New England Journal of Medicine. 2019;380:2529–2540. doi: 10.1056/NEJMoa1803377. [DOI] [PubMed] [Google Scholar]
- 47.Body R, Carlton E, Sperrin M, Lewis PS, Burrows G, Carley S, McDowell G, Buchan I, Greaves K, Mackway-Jones K. Troponin-only Manchester Acute Coronary Syndromes (T-MACS) decision aid: Single biomarker re-derivation and external validation in three cohorts. Emergency Medicine Journal. 2017;34:349–356. doi: 10.1136/emermed-2016-205983. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.