Abstract
Background
Despite the importance of reducing treatment burden for people with cystic fibrosis (CF), it has not been fully understood as a concept. This study aims to quantify the treatment burden perceived by CF adults and explore the association between different validated treatment burden measures.
Methods
This is a cross-sectional observational study of CF adults attending a single large UK adult center. Participants completed an online survey that contained three different treatment burden scales; CF Questionnaire-Revised (CFQ-R) subscale, CF Quality of Life (CFQoL) subscale, and the generic multimorbidity treatment burden questionnaire (MTBQ).
Results
Among 101 participants, the median reported treatment burden by the CFQ-R subscale was 55.5 (IQR 33.3 – 66.6), the CFQoL subscale was 66.6 (IQR 46.6 – 86.6), and the MTBQ reversed global score was 84.6 (IQR 73.1 – 92.3). No correlation was found between respondents’ demographic or clinical variables and treatment burden measured via any of the three measures. All treatment burden measures showed correlations against each other. More treatments were associated with high treatment burden as measured by the CFQ-R, CFQoL subscales, and the MTBQ. However, longer treatment time and more complex treatment plans were correlated with high treatment burden as measured by the CFQ-R and CFQoL subscales, but not with the MTBQ.
Conclusions
Treatment burden is a substantial issue in CF. Currently, the only available way to evaluate it is with the CF-specific quality of life measure treatment burden subscales (CFQ-R and CFQoL); both indicated that treatment burden increases with more treatments, longer treatment time, and more complex treatments.
Keywords: cystic fibrosis, treatment burden, patient-reported outcomes
Introduction
Survival for people with cystic fibrosis (pwCF) has increased over the years. According to the UK CF Registry in 2020, the median predicted survival for pwCF born today is 50.6 years1. This is due to multiple treatments and prevention therapies2. To maintain the health of pwCF, a complicated treatment regimen is needed daily. This includes nutritional management, inhalation therapies, sputum clearance using chest physiotherapy, antibiotic therapy, and cystic fibrosis transmembrane conductance regulator (CFTR) modulators3. It is estimated that adults with CF require two to three hours daily to complete their treatments resulting in a high burden for them or their caregivers3.
Treatment burden is a result of healthcare workload experienced by patients with chronic conditions and their caregivers that affects their lives and well-being4. This workload involves patient’s time and effort to complete the treatment in addition to other self-care tasks such as monitoring the condition, nutritional management, and exercise4. High treatment burden may be associated with low quality of life, low adherence to treatment, and inefficient use of medical resources if people cannot adhere to treatment plans5. Treatment burden is considered an important issue and ranked as the top research question for pwCF, caregivers, and clinicians according to James Lind Alliance’s top CF questions list6.
Treatment burden could be induced by the treatment type, amount, frequency, duration, learning and remembering how to manage treatments, sterilization of medical equipment, or the constant monitoring of the condition at home7,8. Also, the complexity of administration for some treatments could contribute to increasing the perceived treatment burden7. Nonetheless, these factors may not necessarily equate to the burden perceived by a person with CF as they are objective aspects of treatment burden. Each person perceives treatment burden differently; it is subjective to the person with CF9.
Currently, the only available instruments to capture perceived treatment burden for pwCF are the treatment burden subscales of the CF-specific quality of life measures; the CF questionnaire revised (CFQ-R) and the CF quality of life (CFQoL) instruments10,11. Both subscales cover some concepts of treatment burden such as time spent on treatment, difficulties caused by the treatments, and interference with life and happiness. However, these subscales only focus on specific aspects of treatment burden and neglect other areas such as the burden of financial and managerial requirements associated with treatment. Despite the lack of complete CF-specific instruments, there are generic treatment burden instruments that are used with different conditions. These instruments include the Multimorbidity Treatment Burden Questionnaire (MTBQ) developed for a UK population and the Treatment Burden Questionnaire (TBQ)12,13. However, these generic instruments have not been evaluated in pwCF. There are no available studies that have compared the performance of different treatment burden instruments8.
In this study, we aimed to quantify perceived treatment burden in CF adults. Moreover, we hypothesized that high treatment burden is associated with more treatments, longer treatment time, and more complex treatment; therefore, we assessed the performance of the two available treatment burden subscales in CF-specific quality of life measures (CFQ-R and CFQoL) and the generic treatment burden measure (MTBQ) in capturing perceived treatment burden and their correlation with each other. A secondary aim was to explore the relationship between perceived treatment burden and disease severity.
Methods
Study population
This cross-sectional, observational survey study recruited CF adults aged 18 years or older between July and October 2020 from an adult CF center in London, UK. The study was undertaken as part of a larger study investigating Evidence-based VALUation of patient outcomes in Cystic Fibrosis (the VALU-CF study). The participants completed an online survey that contained treatment burden subscales from the CFQ-R, CFQoL and the MTBQ14. Also, the VALU-CF study collected discrete choice experiment (DCE) in the survey and time trade-off through interviews, which will be undertaken by a different study. The VALU-CF sample was determined using a rule of thumb calculation to estimate the sample needed for the DCE element of the survey15. Based on the calculation, and allowing for a 15% drop out rate, the sample size was set at 108 patients.
The sample were recruited through telephone and email to complete an online or PDF survey. A £10 financial incentive was offered to the participants for completing the survey. Ethical approval was received for the VALU-CF study (REC:19/YH/0423). An online written informed consent was obtained from the participants prior to completing the survey for participation and Registry data linkage.
Measures
Demographic and clinical variables
Demographic (age, gender, ethnicity, education level, marital status, employment status) and clinical (height, weight, body mass index “BMI”, percent predicted forced expiratory volume in 1 second “ppFEV1”, number of IV antibiotic courses received in the year prior to enrollment) variables for the participants were collected from the survey, the closest encounter data within the UK CF Registry and their CF center’s medical record.
Treatment descriptors
The participants were asked to provide information related to their CF treatment including how much time they spent on inhaled therapies, chest physiotherapy, and other treatments. Based on these questions, total treatment time was calculated. Furthermore, the number of treatments, their types, (inhalers, nebulizers, and chest physiotherapy) and frequencies were collected from the Registry.
To assess the difficulty of doing these treatments, a treatment complexity score (TCS) was estimated for each participant. This measure was developed by Sawicki et al.7 to give each CF treatment a score, ranging between 1 and 3, based on its frequency, administration time, and method. The scores for all treatments a participant was taking were added together to give a single TCS score (range 0 – 73)7. A high TCS score suggests high treatment complexity. The TCS scoring in this study was based on the Sawicki et al.7 study with some additions/modification, generated by an expert group including pwCF (Table 1).
Table 1. The modified version of Sawicki et al.7’s treatment complexity score table.
| TCS Score = 1 point | TCS Score = 2 points | TCS Score = 3 points |
|---|---|---|
| Acid blockers | Antibiotics (nebulized OD) | Antifungals (inhaled) * |
| Analgesics | DNase (OD / OR) | Antibiotics (nebulized (BD/TDS) |
| Angiotensin receptor agonists * | Hypertonic saline (OD) | DNase (BD) * |
| Antibiotics (inhaled DPI) * | Pancreatic enzymes | Hypertonic saline (BD) * |
| Anticoagulants * | CFTR modulator * | Mannitol (DPI) |
| Antidepressants | Insulin | |
| Antiemetics * | Colistin (nebulized) * | |
| Antiepileptic * | Oxygen | |
| Antifungals (oral) * | Airway clearance | |
| Antihistamines * | Noninvasive ventilation * | |
| Anti-inflammatories * | ||
| Antiviral * | ||
| Beta blocker * | ||
| Bisphosphonates * | ||
| Bronchodilators (inhaled) | ||
| Bronchodilators (oral) | ||
| Chronic oral antibiotics | ||
| Corticosteroids (inhaled) | ||
| Corticosteroids (inhaled) + LABA | ||
| Corticosteroids (oral) | ||
| Diuretics | ||
| Immunosuppressants (oral) * | ||
| Tranexamic acid 1 gm (TDS, PRN) * | ||
| Metformin * | ||
| Migraine prophylaxis * | ||
| Minerals (oral) | ||
| Nasal rinse/ spray * | ||
| Prophylactic antibiotics (oral) | ||
| Ropinirole * | ||
| Statin * | ||
| Tamoxifen * | ||
| Vitamins (oral) | ||
| Gastrointestinal medicines * |
The newly added treatments to Sawicki et al.7’s original version – none of the assigned treatments from the original version were moved to different categories or removed from the scale.
Abbreviations: TCS = treatment complexity score, DPI = dry powder inhaler, LABA = long-acting beta agonist, TDS = three times a day, PRN = as required, OD = once a day, OR = other regimen, BD = twice a day.
Treatment burden
Treatment burden was assessed using the CF-specific quality of life subscales from the CFQ-R (adult version), and the CFQoL, in addition to the generic treatment burden measure the MTBQ. Table 2 describes the treatment burden instruments used in this study, their development, validation and their items. Each of the treatment burden subscales in the CFQ-R and the CFQoL has three items that are scored on a 0 to 100-point scale; high scores indicate low perceived treatment burden10,11. The MTBQ is a generic treatment burden instrument that was developed in older adults with chronic conditions and consists of 13 items that capture treatment burden in people with multimorbidity12. The MTBQ items generate a global score that ranges from 0 to 100, high scores indicate high perceived treatment burden12.
Table 2. Description of the treatment burden measures used in this study.
| Questionnaire | Development and validation | Type of instrument | Items related to treatment burden |
|---|---|---|---|
| CFQ-R “Treatment burden” domain | Developed by Henry et al.17 and revised and validated by Quittner et al.11 for CF. | A treatment burden subscale from a CF-specific quality of life measure. | Over the last two weeks, to what extent do your treatments make your daily life more difficult? |
| Over the last two weeks, how much time do you currently spend each day on your treatments? | |||
| Over the last two weeks, how difficult is it for you to do your treatments (including medications) each day? | |||
| CFQoL “Treatment issues” domain | Developed and validated by Gee et al.10 for CF. | A treatment burden subscale from a CF-specific quality of life measure. | Over the last two weeks, I have found my treatments (physio, enzymes etc.) very time consuming. |
| During the last two weeks, my treatments have interfered with other things that I have wanted to do. | |||
| Over the last two weeks, I have found that my treatments have interfered with my enjoyment of life. | |||
| MTBQ | Developed and validated by Duncan et al. 12 for patients with multimorbidity. | A generic treatment burden measure. | Taking lots of medications |
| Remembering how and when to take medication | |||
| Paying for prescriptions, over the counter medication or equipment | |||
| Collecting prescription medication | |||
| Monitoring your medical conditions (e.g. checking your blood sugar, monitoring your symptoms etc.) | |||
| Arranging appointments with health professionals | |||
| Seeing lots of different health professionals | |||
| Attending appointments with health professionals (e.g. getting time off work, arranging transport etc.) | |||
| Getting health care in the evenings and at weekends | |||
| Getting help from community services (e.g. physiotherapy, district nurses etc.) | |||
| Obtaining clear and up-to-date information about your condition | |||
| Making recommended lifestyle changes (e.g. diet and exercise etc.) | |||
| Having to rely on help from family and friends |
Statistical analysis
SPSS version 25 (IBM SPSS Statistics, RRID:SCR_016479) was used for data analysis. Descriptive statistics were derived for demographic and clinical variables, treatment descriptors (number of treatments, total treatment time, and TCS), and the treatment burden instruments. The MTBQ global score was reversed to ease the comparison with the CFQ-R and CFQoL (so that in all instruments; a high score represented low treatment burden). Shapiro-Wilk tests were carried out to determine normality of the data distribution for all variables. To explore how treatment burden differed according to disease severity, participants were divided into two disease severity groups based on their ppFEV1; mild: ≥70%, and moderate to severe: ≤69%.
Descriptive and inferential statistical analysis were employed to assess the three treatment burden instruments. First, a descriptive analysis was conducted on the three treatment burden instruments based on the disease severity groups. Then, to determine the nature of relationship between disease severity and treatment burden, we assessed the difference of the treatment burden reported by each of the three instruments between the disease severity groups. Due to skewedness of the treatment burden data, a Mann-Whitney test was used to determine the significance of the difference.
The associations between the three treatment burden instruments were investigated using Spearman’s Rank correlation test due to the lack of normality in the data. This helped in assessing the relationship between the treatment burden captured by the three instruments. A correlation was considered significant if the p-value was less than 0.05. A correlation coefficient was considered strong if it was higher than 0.7, moderate strength if it was between 0.7 and 0.3, and weak correlation if it was less than 0.316. Furthermore, Spearman’s Rank test was conducted for each of the treatment burden instruments and demographic, clinical, and treatment descriptors (number of treatments, TCS, and total time of treatments) variables to assess the nature of their relationship.
Results
Descriptive statistics
The sample included 103 participants out of 276 invitations sent (response rate 37%), and two were excluded due to unavailability of their clinical and demographic data; therefore, 101 participants were included in the final analysis. Table 3 illustrates the demographic and clinical data. Table 4 shows detailed descriptive statistics of the treatments the participants were receiving at the time the study was conducted.
Table 3. Demographic and clinical variables for the sample.
| Age in years (n=101) | Height in cm (n=101) | ||
|---|---|---|---|
| Mean (SD) | 35.7 (11.4) | Mean (SD) | 168 (9.6) |
| Median (IQR) | 34 (27 – 44) | Median (IQR) | 168 (160.5 – 176.5) |
| Range | 18 – 75 | Range | 143 – 187 |
| Gender, n (%), (n=101) | Weight in kg (n=101) | ||
| Female | 52 (51.5%) | Mean (SD) | 64.7 (13) |
| Male | 49 (48.5%) | Median (IQR) | 63 (54.6 – 73.5) |
| Range | 40.3 – 108 | ||
| Ethnicity, n (%), (n=101) | BMI (n=101) | ||
| White | 98 (97%) | Mean (SD) | 22.7 (3.1) |
| Other | 3 (3%) | Median (IQR) | 22.3 (20.8 – 24.4) |
| Range | 15.7 – 39.7 | ||
| Education level, n (%), (n=101) | ppFEV1 (n=99)* | ||
| University | 50 (49.5%) | Mean (SD) | 69.4 (22.2) |
| College | 27 (26.7%) | Median (IQR) | 69.1 (52.8 – 83) |
| High school | 9 (8.9%) | Range | 25.1 – 123.6 |
| Less than high school | 2 (2%) | ||
| Not known | 13 (12.9%) | ||
| Marital status, n (%), (n=101) | FEV1 in liter (n=98)** | ||
| Single | 40 (39.6%) | Mean (SD) | 2.47 (1.04) |
| Married | 39 (38.6%) | Median (IQR) | 2.31 (1.65 – 3) |
| Long-term partner | 18 (17.8%) | Range | 0.91 – 7 |
| Divorced | 2 (2%) | ||
| Separated | 1 (1%) | ||
| Not known | 1 (1%) | ||
| Employment status, n (%), (n=101) | Number of IV antibiotic courses last year (n=101) | ||
| Full-time | 52 (51%) | Mean (SD) | 0.62 (1.20) |
| Part-time | 21 (20.6%) | Median (IQR) | 0 (0 – 1) |
| Student | 12 (11.8%) | Range | 0 – 5 |
| Unemployed | 8 (7.88%) | Number of IV antibiotic days last year (n=101) | |
| Homemaker | 3 (2.9%) | Mean (SD) | 10.2 (22.1) |
| Retired | 1 (1%) | Median (IQR) | 0 (0 – 14) |
| Disabled | 1 (1%) | Range | 0 – 124 |
| Not known | 4 (3.9%) | CFRD, n (%), (n=101) | |
| CFRD | 29 (28.7%) | ||
Two participants did not have a reported ppFEV1.
Three participants did not have a reported FEV1 in liters.
Abbreviations: BMI = body mass index, ppFEV1 = percent predicted of forced expired volume in one second, CFRD = cystic fibrosis related diabetes.
Table 4. Descriptive statistics for the received treatments at the time of the study.
| Total(n=101) | |
|---|---|
| Number of treatments | |
| Mean (SD) | 13.2 (4.8) |
| Median (IQR) | 13 (11 –16) |
| Range | 0 – 31 |
| Number of inhalers | |
| Mean (SD) | 2 (1.2) |
| Median (IQR) | 2 (1 – 3) |
| Range | 0 – 5 |
| Number of nebulizers | |
| Mean (SD) | 2.3 (1.1) |
| Median (IQR) | 2 (2 – 3) |
| Range | 0 – 5 |
| Number of chest physiotherapies | |
| Mean (SD) | 1.5 (0.6) |
| Median (IQR) | 1 (1 – 2) |
| Range | 0 – 3 |
| Type of primary chest physiotherapy, n (%) | |
| Autogenic drainage | 36 (35.6%) |
| Active cycle breathing techniques | 21 (20.8%) |
| Oscillating PEP | 21 (20.8%) |
| Other | 13 (12.9%) |
| None | 10 (9.9%) |
| Inhaled medication time in minutes (min/day) | |
| Mean (SD) | 42.6 (38.2) |
| Median (IQR) | 30 (20 – 60) |
| Range | 0 – 180 |
| Chest physiotherapy time in minutes (min/day) | |
| Mean (SD) | 36.3 (31.8) |
| Median (IQR) | 30 (17.5 – 50) |
| Range | 0 – 180 |
| Other treatments time in minutes (min/day) | |
| Mean (SD) | 12 (20) |
| Median (IQR) | 5 (0 – 15) |
| Range | 0 – 120 |
| Total treatment time in minutes (min/day) | |
| Mean (SD) | 91 (70.7) |
| Median (IQR) | 80 (45 – 108.5) |
| Range | 0 – 420 |
| TCS (treatment complexity score) | |
| Mean (SD) | 22 (7.4) |
| Median (IQR) | 23 (18 – 27) |
| Range | 0 – 40 |
| CFTR Modulators, n (%), | |
| On CFTR modulator | 66 (65.3%) |
| On
Elexacaftor/tezacaftor/ivacaftor (Trikafta/Kaftrio©) |
33 (32.7%) |
Treatment burden and disease severity
Table 5 shows the treatment descriptors, and the treatment burden instruments descriptive statistics across the whole sample and the ppFEV1 disease severity groups. All disease severity groups had more than half of their participants receiving CFTR modulators (mild group; 61% and moderate to severe group; 70%). Half of those on CFTR modulators were taking elexacaftor/tezacaftor/ivacaftor (Trikafta/Kaftrio©) in both disease severity groups. There were no statistically significant differences between disease severity groups for the CFQ-R subscale (U = 980.00, z = -1.73, p = 0.08), the CFQoL subscale (U = 1170.50, z= -0.38, p = 0.70), or the MTBQ reversed global score (U = 1028.00, z = -1.38, p = 0.16).
Table 5. Treatment descriptors and treatment burden instruments descriptive statistics based on disease severity groups.
| Mild severity (n=49) |
Moderate to severe severity (n=50) |
Total (n=99)* | |
|---|---|---|---|
| Number of treatments | |||
| Mean (SD) | 11.3(4.1) | 15 (4.9) | 13.2 (4.8) |
| Median (IQR) | 12 (9 – 13.5) | 15 (13 – 17) | 13 (11 – 16) |
| Range | 2 – 20 | 0 – 31 | 0 – 31 |
| TCS | |||
| Mean (SD) | 19 (6.4) | 24.8 (7.3) | 22 (7.5) |
| Median (IQR) | 19 (14.5 – 24) | 24 (21 – 29.5) | 23 (18 – 27) |
| Range | 5 – 32 | 0 – 40 | 0 – 40 |
| Total treatment time (min/day) | |||
| Mean (SD) | 78.3 (45.1) | 106 (87.5) | 92.2 (70.8) |
| Median (IQR) | 80 (45 – 100) | 90 (50 – 125) | 85 (50 – 110) |
| Range | 0 – 190 | 0 – 420 | 0 – 420 |
| CFQ-R ‘treatment burden” domain | |||
| Mean (SD) | 57.3 (22.1) | 49.7 (23) | 53.5 (22.7) |
| Median (IQR) | 55.5 (44.4 – 72.2) | 50 (33.3 – 66.6) | 55.5 (33.3 – 66.6) |
| Range | 11.1 – 100 | 11.1 – 100 | 11.1 – 100 |
| CFQoL ‘treatment issues” domain | |||
| Mean (SD) | 64.7 (26.2) | 63.3 (25.4) | 64 (25.7) |
| Median (IQR) | 73.3 (53.3 – 86.6) | 66.6 (46.6 – 86.6) | 66.6 (46.6 – 86.6) |
| Range | 0 – 100 | 0 – 100 | 0 – 100 |
| MTBQ reversed global score | |||
| Mean (SD) | 83.1 (13.6) | 79.5 (14.1) | 81.3 (14) |
| Median (IQR) | 84.6 (74 – 94.2) | 83.6 (69.2 – 90.3) | 84.6 (73.1 – 92.3) |
| Range | 46.1 – 100 | 42.3 – 100 | 42.3 – 100 |
Two participants were not included due to the unavailability of their ppFEV1 data.
Abbreviations: TCS = treatment complexity score.
Correlation between the treatment burden instruments
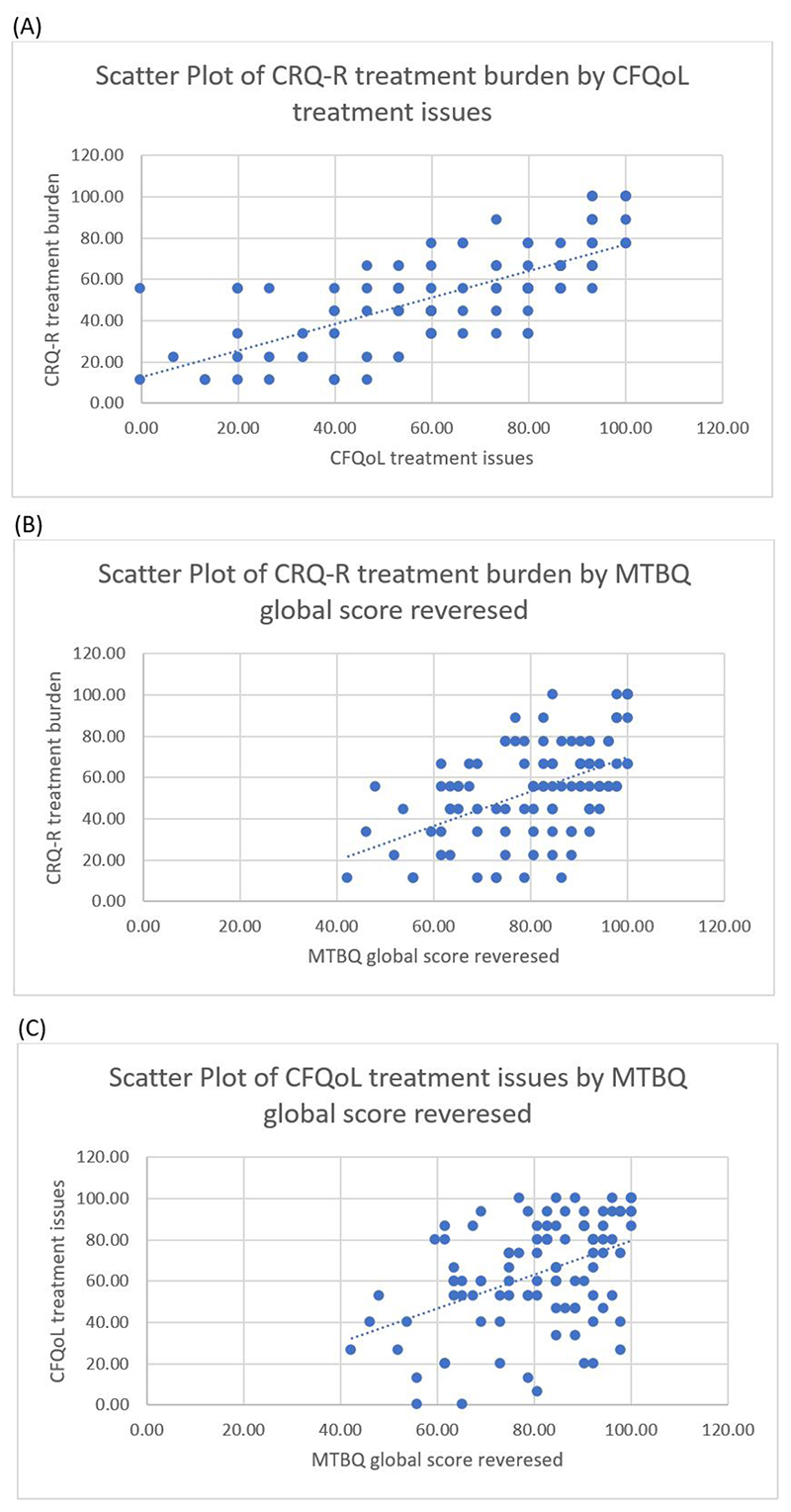
Across the whole sample, statistically significant strong to moderate positive correlations were observed between treatment burden measured by the CFQ-R and CFQoL subscales (rs = 0.727, p <0.001), between the CFQ-R subscale and the MTBQ reversed score (rs = 0.511, p <0.001), and between the CFQoL subscale and the MTBQ (rs = 0.433, p <0.001). These correlations indicate that low observed treatment burden in any of the three instruments is associated with low treatment burden reported by the other instruments. Figure 1 shows the scatter plots of the correlation between the three treatment burden instruments.
Figure 1. Scatter plots for the correlations between the three treatment burden instruments.
(A) the correlation between the CFQoL and the CFQ-R treatment burden subscales. (B) the correlation between the CFQ-R treatment burden subscale and the MTBQ. (C) the correlation between the CFQoL treatment burden subscale and the MTBQ.
Correlation between the treatment burden instruments and demographic, clinical, and treatment descriptors variables
Age, gender, BMI, and the number of IV antibiotic courses received last year demonstrated no association with perceived treatment burden measured by any of the three instruments. Treatment burden measured by CFQ-R (rs = -0.424, p <0.01), CFQoL (rs = -0.305, p <0.01), and the MTBQ reversed score (rs = -0.220, p = 0.02) revealed significant moderate to weak negative correlations with the number of treatments, indicating that treatment burden may increase with more daily treatments. Among the treatment types, treatment burden measured by the CFQ-R demonstrated significant moderate associations with the number of inhaled therapies (rs= -0.324, p <0.01) and the number of nebulized therapies (rs = -0.363, p <0.01). Treatment burden measured by the CFQoL illustrated a significant weak correlation with the number of chest physiotherapy treatments (rs = -0.250, p = 0.01). The MTBQ reversed score showed a significant weak correlation with the number of inhaled therapies (rs = -0.261, p <0.01).
Treatment burden measured by the CFQ-R and CFQoL subscales showed significant negative moderate associations with TCS (rs = -0.428, p <0.01 and rs = -0.309, p <0.01, respectively). This indicates that high treatment complexity may associate with high perceived treatment burden. The MTBQ reversed score did not demonstrate any association with TCS (rs = -0.126, p = 0.12).
Total treatment time demonstrated significantly moderate to weak negative correlations with both CFQ-R and CFQoL treatment burden subscales with rs = -0.352, p <0.01 and rs = -0.246, p = 0.01, respectively. These results suggest that long treatment time could be associated with high perceived treatment burden. The MTBQ reversed score did not show any association with total treatment time (rs = -0.076, p = 0.45). Both CFQ-R and CFQoL demonstrated significantly moderate to weak negative correlations with inhaled medication time, (rs = -0.386, p <0.01 and rs = -0.243, p = 0.01, respectively). Only treatment burden measured by CFQ-R showed a significant weak negative correlation with chest physiotherapy time (rs = -0.210, p = 0.03). These findings indicate that long inhaled therapies and/or chest physiotherapy time might be associated with high perceived treatment burden.
Discussion
A high degree of treatment burden was reported by pwCF, as measured by the CFQ-R and CFQoL. The MTBQ showed a slightly lower level of treatment burden compared to the other two subscales. There was no association observed between perceived treatment burden and the demographic and clinical variables; in addition to no significant difference in treatment burden between the disease severity groups categorized by lung function.
This study also aimed to assess the performance of the three treatment burden instruments (CFQ-R, CFQoL, MTBQ) and their correlation with each other. The CFQ-R and CFQoL subscales illustrated significant associations with treatment descriptors and had strong correlation between each other. However, when the distribution of the three treatment burden instruments was assessed, the CFQoL illustrated a wider distribution across the sample compared to the other two instruments (ranging between 0 to 100). Despite the variation between the MTBQ and the two CF-specific subscales, all three instruments were associated with each other. The generic MTBQ illustrated moderate strength correlation with both subscales. This indicates that the MTBQ could be capturing some similar aspects of treatment burden to that measured by the two subscales.
The MTBQ is a generic measure of treatment burden that was developed for patients with multimorbidity. Despite CF being a multimorbidity condition, pwCF may not commonly relate to some of its items. For example, some items ask about the financial impact caused by treatment expenses12; however, the majority of the sample did not have to pay for treatments. Some MTBQ items focus on the administrative aspect of treatment burden (monitoring health, arranging appointments, and collecting prescribed medications) and others on lifestyle changes caused by the disease (dieting and exercising)18. These items could have captured perceived treatment burden based on the mentioned aspects; however, this cannot be confirmed since none of these aspects were used to assess the performance of the treatment burden instruments in this study. The other CF-specific subscales focus on treatment time and difficulty, in addition, to the psychological impact of the treatment i.e. life happiness. The variables used to describe treatments in this study (the number of treatments, treatment time, and complexity) capture some of the concepts in the CF-specific subscales, but not the generic MTBQ. Therefore, it is not surprising to find an association between the two CF-specific subscales and those variables. Moreover, the MTBQ was originally developed on a population older than the average age range of a person with CF (and the average age of this sample); hence, the generic MTBQ may lack face validity when it is used in pwCF.
The lack of correlation between perceived treatment burden and, age, gender and disease severity correspond with Sawicki et al.3 findings. In their study, they only used the CFQ-R subscale to capture treatment burden, while this study used the CFQ-R in addition to the CFQoL subscale and the generic MTBQ. Moreover, we observed no difference in treatment burden between disease severity groups based on lung function, which agrees with Sawicki et al.3 observation. These findings indicate that in CF, perceived treatment burden might be independent of age, gender, or the level of disease severity and cannot be predicted by them. This is perhaps not surprising as CF standards of care include a relatively strict regimen of therapies across the disease spectrum.
We found moderate to weak correlations between treatment burden, measured by CFQ-R, CFQoL subscales, and MTBQ and the number of daily treatments (the number of inhaled therapies, nebulized therapies, and chest physiotherapies). These findings correspond with Sawicki et al.3 as they also found an association between treatment burden measured via CFQ-R and the number of nebulized therapies and chest physiotherapies. Based on these moderate to weak correlations, we assumed that the number of daily treatments might not have heavily impacted perceived treatment burden for pwCF as we expected. A person with multiple treatments may have less treatment burden if the treatments are easy to administer and fast to take than a person with fewer treatments but harder to administer and require longer time to take. Therefore, we assessed treatment complexity and treatment time.
The inverse correlations between perceived treatment burden measured by the CFQ-R and CFQoL subscales and the TCS were moderate in strength. The Sawicki et al.7 study also showed negative correlation between treatment burden measured by CFQ-R and the TCS, however, the correlation was weak. Nonetheless, our findings do not imply that TCS fully capture the concepts covered by both treatment burden subscales. It is important to remember that TCS is an objective measure of complexity; while perceived treatment burden is based on how pwCF view their treatment and this may vary between different individuals.
Compared to the Sawicki et al.3 study, our sample reported lower total treatment time in minutes per day (80 vs. 108 min). Also, we found moderate to weak associations between treatment burden measured by CFQ-R and CFQoL subscales and total treatment time which resembles Sawicki et al.’s3 observations. These associations were anticipated since both CFQ-R and CFQoL subscales have items that ask about time spent in completing treatments.
Our study is the first to apply a generic measure of perceived treatment burden in a CF population and to compare the performance of different treatment burden instruments in CF. Nonetheless, this study had several limitations. First, the study included CF adults from one CF center which limits the generalizability of its results. Moreover, the cross-sectional nature of the study makes it hard to distinguish the confounding variables which makes it difficult to clearly interpret the results of the study. Further longitudinal studies are needed to confirm these outcomes and the ability of these instruments to capture changes of treatment burden over time. Some variables like treatment time were collected from the survey which is based on the participants memory and that can potentially introduce recollection bias. Also, the sample size in the overall study and across the disease severity groups were small due to the low survey response rate. This might have contributed in the lack of statistical significance of some of the observations, in particular the lack of variation between all the treatment burden instruments when compared across the disease severity groups.
Conclusions
Treatment burden is considered a substantial problem for the CF population. Until now, the CFQ-R and CFQoL subscales are the only available measures to capture their perceived treatment burden. They both illustrated that treatment burden increases with more treatments, longer treatment time and more complex treatments. The generic MTBQ measure was not developed on a CF population and had almost no association with the treatment descriptors but showed correlations with the CFQ-R and CFQoL subscales. This is the first study to compare the performance of different treatment burden measures in CF adults, adding important insights into this high priority field. Further studies on this topic are needed, particularly if treatment recommendations change in the era of CFTR modulators. Qualitative studies that clearly describe the perceived treatment burden will be vital to capture these important issues as the health status and treatment options in CF continue to evolve.
Plain English summary.
People with cystic fibrosis (CF) are required to adhere to a very complicated and exhausting treatment plan daily. This can result in the patients experiencing excessive burden from the high healthcare workload needed to maintain their health. Therefore, it is important to look for ways to reduce their treatment burden. Treatment burden is not yet a fully understood concept in CF and different people could perceive treatment burden differently. This study aims to measure the treatment burden perceived by adults with CF and investigate the performance of three different treatment burden questionnaires.
This single survey study targeted 101 adults with CF in a large UK adult center. Participants completed an online survey that contained three different treatment burden measures; two short (three questions each) CF-specific questionnaires, and one generic (13 questions) questionnaire that captures treatment burden in people with long-term conditions.
The participants’ responses suggested that people with CF have a high level of treatment burden according to the two CF-specific questionnaires, but not with the generic one. An important finding was that the severity of the participants’ disease (based on their lung function) did not appear to affect the reported treatment burden. We found that age, gender, body mass index, and the number of intravenous antibiotic courses received in the previous year did not affect the reported treatment burden. Treatment burden was higher in people who had more treatment, spent more time doing their daily treatments, and received more complex treatment plans.
Currently, the CF-specific treatment burden questionnaires appear to be the most appropriate way to capture treatment burden in adults with CF. We believe that including treatment burden evaluation in the process of treatment decision-making is important as it takes into perspective the CF patient’s point of view about their treatment plan.
Open Peer Review.
Current Peer Review Status: ✔ ✔
Version 1
Reviewer Report 10 November 2022
https://doi.org/10.3310/nihropenres.14376.r28841
© 2022 Kashirskaya N. This is an open access peer review report distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
✔ Nataliya Kashirskaya iD
Research Centre for Medical Genetics, Moscow, Russian Federation
Treatment burden in CF is substantial and multifactorial and its complexity increases dramatically with age. High treatment complexity tends to undermine quality of life and adherence to these treatments. In light of the recent progress toward normalizing the health of PwCF by restoring CFTR activity with a use of CFTR modulators, the need for symptomatic treatments that have been recommended for decades is being questioned in the last few years (chest physiotherapy, mucolytics, bronchodilators, nebulized antibiotics and macrolides, etc.). As it is mentioned by Altabee R. et al the only currently available instruments to capture perceived treatment burden for pwCF are the treatment burden subscales of the CF-specific quality of life measures; the CF questionnaire revised (CFQ-R) and the CF quality of life (CFQoL) instruments. Both subscales cover some concepts of treatment burden such as time spent on treatment, difficulties caused by the treatments, and interference with life and happiness, but don't cover, for example, the burden of financial and managerial requirements associated with treatment. That's why the authors decided to use an extra measurement - a generic treatment burden instrument - the Multimorbidity Treatment Burden Questionnaire (MTBQ) developed for a UK population. This generic instrument has not been evaluated in PwCF.
This single survey study targeted 101 adults with CF in a large UK adult center. Participants completed an online survey that contained three different treatment burden measures; two short (three questions each) CF-specific questionnaires, and one generic (13 questions) questionnaire that captures treatment burden in people with long-term conditions. The study aimed to quantify perceived treatment burden in CF adults and to explore the relationship between perceived treatment burden and disease severity. This study also aimed to assess the performance of the three treatment burden instruments (CFQ-R, CFQoL, MTBQ) and their correlation with each other. The study was well designed and the data was statistically correctly processed. I have no major suggestions for revision or improvement of the study. The manuscript is very well illustrated.
A high degree of treatment burden was reported by pwCF, as measured by the CFQ-R and CFQoL. The MTBQ showed slightly lower level of treatment burden compared to the other two subscales. There was no association observed between perceived treatment burden and the demographic and clinical variables; in addition to no significant difference in treatment burden between the disease severity groups categorized by lung function.
The CFQoL illustrated a wider distribution across the sample compared to the other two instruments. Despite the variation between the MTBQ and the two CF-specific subscales, all three instruments were associated with each other. The generic MTBQ illustrated moderate strength correlation with both subscales. This indicates that the MTBQ could be capturing some similar aspects of treatment burden to that measured by the two subscales and can be used in future research in pwCF. This is the first study to compare the performance of different treatment burden measures in CF adults, adding important insights into this high priority field. By including treatment burden evaluation in the process of treatment decision-making is important as it takes into perspective the CF patient's point of view about their treatment plan.
I read with interest the comments by Reviewer #1 (Latchford G), Hoo ZH and Wildman M, and the response to them by Rana Altabee on behalf of the authors of the manuscript. Further studies on this topic are needed taking in mind that treatment recommendations will be definitely changing in the era of CFTR modulators.
Is the work clearly and accurately presented and does it cite the current literature?
Yes
Is the study design appropriate and is the work technically sound?
Yes
Are sufficient details of methods and analysis provided to allow replication by others?
Yes
If applicable, is the statistical analysis and its interpretation appropriate?
Yes
Are all the source data underlying the results available to ensure full reproducibility?
Yes
Are the conclusions drawn adequately supported by the results?
Yes
Competing Interests: No competing interests were disclosed.
Reviewer Expertise: Cystic fibrosis
I confirm that I have read this submission and believe that I have an appropriate level of expertise to confirm that it is of an acceptable scientific standard.
Author Response 14 Nov 2022
Rana Altabee, University of East Anglia, Norwich, UK
We thank the reviewer for her helpful and valuable feedback.
Currently, the CF-specific quality of life measures (CFQ-R and CFQoL) treatment burden subscales are the only available methods used to capture treatment burden from the pwCF perspective. However, treatment burden is much bigger in concept than what's covered by the 3-itemed subscales. Therefore, we hope with this study to highlight the importance of treatment burden for the CF population, especially with the availability of the CFTR modulators.
Competing Interests: No competing interests were disclosed.
Reviewer Report 01 June 2022
https://doi.org/10.3310/nihropenres.14376.r28651
© 2022 Latchford G. This is an open access peer review report distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
✔ Gary Latchford
Leeds Institute of Health Sciences, University of Leeds, Leeds, UK
This study focusses on a very important area within CF - treatment burden. As they say, it was ranked the top research question by the James Lind Alliance.
It's an important but quite tricky concept - as they note, it means different things to different people. This paper focused on measurement, and was a well conducted, very sensible piece of research. I have no major suggestions for revision or improvement.
Using a cross sectional sample of 101 participants from one large UK CF centre in London, they compared the performance of the very short treatment burden subscales from two QoL measures (CFQ-R and CFQoL), and a generic treatment burden measure (MTBQ). They also very wisely used Sawicki's treatment complexity score to allow for some interesting analysis.
The findings are pretty intuitive, but very useful to see properly explored. All the measures correlate with each other and all showed a higher treatment burden to be associated with more treatments. The CFQ-R and CFQol both performed better with CF patients however, demonstrating an association between longer treatment times and more complex treatments with a higher treatment burden that was not present in the MTBQ data. This makes sense. Many of the items on the MTBQ do not translate well onto the treatment context associated with CF. They note this and I'd go further - one of the key features of CF treatment is that it is delivered via a dedicated, accessible team in a specialist centre normally very well known to the person with CF. I expect this minimises a lot of the practical challenges other patients may face.
It's interesting that severity is not associated with treatment burden. They note that this most likely reflects the considerable treatment regimen all are asked to follow. I wonder too whether it reflects the ongoing, day to day routine of this burden - I expect when asked about treatment burden people will tend to recall a generic rather than specific memory.
Finally, I agree that this is a particularly important area just now, with the potential in the future for modulator therapies to mean other treatments may no longer be needed. It's important to track this change. The two CF QoL measures seem adequate, but that might change as the nature of the treatment in CF changes. I wondered if there were any thoughts about developing a new measure?
Data availability - consent was only for the current study but the data may be available with permission from the hospital.
Is the work clearly and accurately presented and does it cite the current literature?
Yes
Is the study design appropriate and is the work technically sound?
Yes
Are sufficient details of methods and analysis provided to allow replication by others?
Yes
If applicable, is the statistical analysis and its interpretation appropriate?
Yes
Are all the source data underlying the results available to ensure full reproducibility?
Partly
Are the conclusions drawn adequately supported by the results?
Yes
Competing Interests: No competing interests were disclosed.
Reviewer Expertise: Clinical Health Psychology; Motivational interviewing; cystic fibrosis
I confirm that I have read this submission and believe that I have an appropriate level of expertise to confirm that it is of an acceptable scientific standard.
Author Response 08 Jun 2022
Rana Altabee, University of East Anglia, Norwich, UK
We thank the reviewer for his kind and helpful comments.
We hope that this study would highlight the importance of capturing treatment burden in people with CF, especially with the new era of modulators. Since the CF-specific treatment burden subscales were the most adequate in capturing treatment burden in CF, it would be great to see future studies developing a new treatment burden instrument for CF.
Competing Interests: No competing interests were disclosed.
Comments on this article
Version 1
Author Response 01Jul 2022
Rana Altabee, University of East Anglia, Norwich, UK
We thank Hoo and Wildman for their interesting thoughts about our study. Nobody has yet defined what treatment burden is for people with CF. In order to do that, a comprehensive qualitative study needs to explain what treatment burden means for people with CF. Treatment time, complexity, and the number of treatments are all different aspects of the overall treatment burden. The CFQ-R and CFQoL subscales are the only available instruments that claim to subjectively capture treatment burden for people with CF.
We looked at the internal consistency of the CFQ-R and the CFQoL treatment burden domains in our study and found them both acceptable (CFQ-R Cronbach's alpha= 0.73 and CFQoL Cronbach's alpha= 0.88). However, treatment burden is bigger than to be captured in a three items subscale. Thus, we assessed the performance of the 13-item generic MTBQ compared to the condition-specific subscale, but unfortunately, it underperformed the other two subscales in people with CF. Therefore, we believe that it is greatly important to develop a treatment burden measure that looks into all the aspects that affect treatment burden from the CF population's perspective.
Competing Interests: No competing interests were disclosed.
Reader Comment 15 Jun 2022
Zhe Hui Hoo, University of Sheffield, UK
We read with interest the paper by Altabee T et al and the comment by Reviewer #1 (Latchford G). One of the conclusions was that a CF-specific tool, such as CFQ-R, is a suitable method to evaluate perceived treatment burden among people with CF. Perceived treatment burden is intriguing. In the multi-centre ACtiF trial with 607 participants which achieved a sustained increase in objectively-measured adherence versus usual care, the increase in treatment taking was accompanied by clinically important reduction in perceived treatment burden (mean 3.9 points in the CFQ-R treatment burden subscale)1. This finding highlights that perceived burden can fall whilst the amount of treatment increases.
The CFQ-R items used to measure perceived burden have interesting differences in their emphasis, hence the perceived treatment burden subscale of CFQ-R may lack internal consistency. In the ACtiF pilot dataset2, the Cronbach's alpha for the perceived treatment burden subscale of CFQ-R was only 0.453 when a value of 0.70 or above are required for a scale to be considered as having satisfactory internal consistency4. Table 2 of the paper by Altabee T et al displays the three items within the treatment burden subscale of CFQ-R: "to what extent do your treatments make your daily life more difficult?" (which we denote as "I1"), "how much time do you currently spend each day on your treatments?" ("I2") and "how difficult is it for you to do your treatments (including medications) each day?" ("I3"). In ACtiF pilot dataset2, Cronbach's alpha for I1-I2, I2-I3 and I1-I3 pairs were 0.35, -0.12 and 0.64 respectively3. This finding suggests that I2 (time spent on treatments) is measuring a different construct compared to I1 (the extent that treatments made daily life more difficult) and I3 (the difficulty of performing treatments). In the original 2005 validation study for CFQ-R, the I1-I2 pair had Cronbach's alpha of only 0.18; hence the third item (I3) was added5. The psychometric properties of CFQ-R was re-evaluated among 4,679 teenagers and adults as part of the Epidemiologic Study of Cystic Fibrosis (ESCF) in 2012, yet the Cronbach's alpha for the 3-item burden subscale was only 0.51, which was the lowest Cronbach's alpha among all 13 subscales of the CFQ-R6.
If the findings from the ACtiF pilot is replicable in other datasets, it would hint that people with CF may not necessarily equate greater length of time spent time on treatment as a major contributor to treatment burden. Altabee T et al could investigate this by calculating the Cronbach's alpha for the treatment burden subscale of CFQ-R in their study. If the Altabee T dataset also demonstrates the lack of internal consistency for the time spent on treatments item (I2), this might challenge Altabee T et al's conclusion that "perceived treatment burden increases with more treatments, longer treatment time, and more complex treatments".
In the 607-participant ACtiF trial1, perceived burden actually fell with more treatment, longer treatment time and greater complexity since the intervention arm took significantly more treatment whilst significantly dropping burden and effort. A potential explanation is that the psychological burden associated with treatment taking may predominantly lie in the instigation phase of the behaviour rather than execution7–10. An analogy is that getting the bicycle out of the garage requires distinct effort whereas riding the same bicycle for ten minutes rather than five minutes is part of a continuous sequence of behaviour that may add only trivial additional burden. People with CF adding dornase alfa to tobramycin in their treatment regimen may only add a little extra burden once the nebuliser is set up. In other words, the deliberative processes required to decide to instigate a behaviour may be more psychologically burdensome compared to the execution of the behaviour to completion. If that is the case, the actual time spent on completing a treatment regimen may not be the most important determinant of perceived burden. In the ACtiF pilot dataset2, there was a lack of relationship between treatment complexity measured with TCS and perceived burden among the participants3. Another study among adults with CF in Sheffield showed the potential attenuation of perceived treatment burden by habit strength where the habit strength is linked to behavioural instigation10.
Since the Altabee T et al study has not measured psychological factors that can influence treatment taking and perceived treatment burden, such as habit strength11, the dataset cannot fully explore these issues. Exploration of the determinants for perceived treatment burden in the Altabee T et al study may also miss critical unmeasured confounding factors.
The determinants of perceived treatment burden remain intriguing and it would be informative if Altabee T et al were to present the Cronbach's alpha for perceived treatment burden subscale of CFQ-R, to explore whether they also identify that time spent on treatments (I2) is inconsistent with treatments making daily life more difficult (I1) and the difficulty of performing treatments (I3). These results could help with the interpretation of their findings and improve our understanding of treatment burden in CF. We whole-heartedly agree with both Altabee T et al and Reviewer #1 that it is important to study perceived treatment burden among people with CF. Studying perceived treatment burden within the framework of a comprehensive behaviour change theory such as The Capability, Opportunity and Motivation (COM-B) model13 will allow a mechanistic understanding of CF treatment burden in the context of routinisation and automaticity, which in turn may enable the development of effective behavioural interventions to reduce perceived treatment burden such as those employed in CFHealthHub1.
Hoo ZH & Wildman MJ, on behalf of the CFHealthHub Learning Health System
Competing Interests: We have completed a £2m NIHR programme grant (supported by £4m of CQUIN funding by NHS England) to develop and evaluate a complex self-management intervention to increase and sustain adherence to inhaled therapies among adults with cystic fibrosis.
- 1.Wildman MJ, O'Cathain A, Maguire C, et al. Self-management intervention to reduce pulmonary exacerbations by supporting treatment adherence in adults with cystic fibrosis: a randomised controlled trial. Thorax. 2022;77(5):461–9. doi: 10.1136/thoraxjnl-2021-217594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hind D, Drabble SJ, Arden MA, et al. Supporting medication adherence for adults with cystic fibrosis: a randomised feasibility study. BMC Pulm Med. 2019;19(1):77. doi: 10.1186/s12890-019-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoo ZH. Clinical and psychological factors associated with nebuliser adherence among adults with cystic fibrosis. PhD thesis, University of Sheffield; 2018. [Google Scholar]
- 4.Bland JM, Altman DG. Cronbach's alpha. BMJ. 1997;314(7080):572. doi: 10.1136/bmj.314.7080.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Quittner AL, Buu A, Messer MA, Modi AC, Watrous M. Development and validation of The Cystic Fibrosis Questionnaire in the United States: a health-related quality-of-life measure for cystic fibrosis. Chest. 2005;128(4):2347–54. doi: 10.1378/chest.128.4.2347. [DOI] [PubMed] [Google Scholar]
- 6.Quittner AL, Sawicki GS, McMullen A, et al. Psychometric evaluation of the Cystic Fibrosis Questionnaire-Revised in a national sample. Qual Life Res. 2012;21(7):1267–78. doi: 10.1007/s11136-011-0036-z. [DOI] [PubMed] [Google Scholar]
- 7.Phillips LA, Gardner B. Habitual exercise instigation (vs. execution) predicts healthy adults' exercise frequency. Health Psychol. 2016;35(1): 69–77. doi: 10.1037/hea0000249. [DOI] [PubMed] [Google Scholar]
- 8.Gardner B, Phillips LA, Judah G. Habitual instigation and habitual execution: Definition, measurement, and effects on behaviour frequency. Br J Health Psychol. 2016;21(3):613–30. doi: 10.1111/bjhp.12189. [DOI] [PubMed] [Google Scholar]
- 9.Gardner B, Rebar AL, Lally P. 'Habitually deciding' or 'habitually doing'? A response to Hagger (2019) Psychol Sport Exerc. 2020;47:101539. [Google Scholar]
- 10.Hoo ZH, Boote J, Wildman MJ, et al. Determinants of objective adherence to nebulised medications among adults with cystic fibrosis: an exploratory mixed methods study comparing low and high adherers. Health Psychol Behav Med. 2017;5(1):299–316. [Google Scholar]
- 11.Hoo ZH, Gardner B, Arden MA, et al. Role of habit in treatment adherence among adults with cystic fibrosis. Thorax. 2019;74(2):197–9. doi: 10.1136/thoraxjnl-2017-211453. [DOI] [PubMed] [Google Scholar]
- 12.Sawicki GS, Ren CL, Konstan MW, Millar SJ, Pasta DJ, Quittner AL, Investigators and Coordinators of the Epidemiologic Study of Cystic Fibrosis Treatment complexity in cystic fibrosis: trends over time and associations with site-specific outcomes. J Cyst Fibros. 2013;12(5):461–7. doi: 10.1016/j.jcf.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Acknowledgements
We would like to thank Dr. Garry Barton for his valuable contribution in the final draft for this manuscript.
Grant information: This project is funded by the National Institute for Health Research (NIHR) under its Research for Patient Benefit (RfPB) Programme (Grant Reference Number PB-PG-1217-20018). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. RA is funded by a PhD studentship from King Saud bin Abdulaziz University for Health Sciences (KSAU-HS). JW and RC involvement were also supported by the National Institute of Health Research (NIHR) Applied Research Collaboration East of England (ARC EoE) program.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Competing interests: RA, JA, RCo, DO, JM, RCa, DT, SC, NS and JW have no direct conflicts of interest to declare in relation to this study. Outside of the submitted work, SC has served on advisory boards and/or given educational lectures for which she or her institution have received fees for (Vertex, Chiesi, and Profile Pharma). NS has served on advisory boards and/or given educational lectures for which he has received consultancy fees (Vertex, Gilead, Chiesi, Zambon, Roche, and Menarini).
Data availability
Underlying data
The study sample was recruited from people attending the Adult Cystic Fibrosis Center at the Royal Brompton Hospital, linked demographic and clinical data were obtained from the UK CF Registry. Participants’ consent was associated only with the VALU-CF study, and not future studies. Additional permission must be sought from the hospital to use this data in further research. To request access to the full raw data, please contact Dr. Siobhan B. Carr, S.Carr@rbht.nhs.uk. Extensive summary data can be found in the article.
Extended data
Figshare: Extended data for ‘Exploring the nature of perceived treatment burden: a study to compare treatment burden measures in adults with cystic fibrosis’. https://doi.org/10.6084/m9.figshare.1953856014.
Data are available under the terms of the Creative Commons Zero “No rights reserved” data waiver (CC0 Public domain dedication).
References
- 1.UK CF Registry annual report 2020. Vol. 1. Cystic Fibrosis Trust; 2021. [Google Scholar]
- 2.Keogh RH, Szczesniak R, Taylor-Robinson D, et al. Up-to-date and projected estimates of survival for people with cystic fibrosis using baseline characteristics: A longitudinal study using UK patient registry data. J Cyst Fibros. 2018;17(2):218–227. doi: 10.1016/j.jcf.2017.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sawicki GS, Sellers DE, Robinson WM. High treatment burden in adults with cystic fibrosis: challenges to disease self-management. J Cyst Fibros. 2009;8(2):91–6. doi: 10.1016/j.jcf.2008.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eton DT, Ramalho de Oliveira D, Egginton JS, et al. Building a measurement framework of burden of treatment in complex patients with chronic conditions: a qualitative study. Patient Relat Outcome Meas. 2012;3:39–49. doi: 10.2147/PROM.S34681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.May C, Montori VM, Mair FS. We need minimally disruptive medicine. BMJ. 2009;339:b2803. doi: 10.1136/bmj.b2803. [DOI] [PubMed] [Google Scholar]
- 6.Rowbotham NJ, Smith SJ, Elliott ZC, et al. Adapting the James Lind Alliance priority setting process to better support patient participation: an example from cystic fibrosis. Res Involv Engagem. 2019;5(1):24. doi: 10.1186/s40900-019-0159-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sawicki GS, Ren CL, Konstan MW, et al. Treatment complexity in cystic fibrosis: trends over time and associations with site-specific outcomes. J Cyst Fibros. 2013;12(5):461–7. doi: 10.1016/j.jcf.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sheehan OC, Leff B, Ritchie CS, et al. A systematic literature review of the assessment of treatment burden experienced by patients and their caregivers. BMC Geriatr. 2019;19(1):262. doi: 10.1186/s12877-019-1222-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sav A, King MA, Whitty JA, et al. Burden of treatment for chronic illness: a concept analysis and review of the literature. Health Expect. 2015;18(3):312–24. doi: 10.1111/hex.12046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gee L, Abbott J, Conway SP, et al. Development of a disease specific health related quality of life measure for adults and adolescents with cystic fibrosis. Thorax. 2000;55(11):946–54. doi: 10.1136/thorax.55.11.946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Quittner AL, Buu A, Messer MA, et al. Development and validation of The Cystic Fibrosis Questionnaire in the United States: a health-related quality-of-life measure for cystic fibrosis. Chest. 2005;128(4):2347–54. doi: 10.1378/chest.128.4.2347. [DOI] [PubMed] [Google Scholar]
- 12.Duncan P, Murphy M, Man MS, et al. Development and validation of the Multimorbidity Treatment Burden Questionnaire (MTBQ) BMJ Open. 2018;8(4):e019413. doi: 10.1136/bmjopen-2017-019413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tran VT, Harrington M, Montori VM, et al. Adaptation and validation of the Treatment Burden Questionnaire (TBQ) in English using an internet platform. BMC Med. 2014;12:109. doi: 10.1186/1741-7015-12-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Altabee R. VALU-CF study questionnaire. figshare. 2022 doi: 10.6084/m9.figshare.19538560.v1. Data. [DOI] [Google Scholar]
- 15.de Bekker-Grob EW, Donkers B, Jonker MF, et al. Sample Size Requirements for Discrete-Choice Experiments in Healthcare: a Practical Guide. Patient. 2015;8(5):373–384. doi: 10.1007/s40271-015-0118-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ratner B. The correlation coefficient: Its values range between +1/−1, or do they? J Target Meas Anal Mark. 2009;17(2):139–142. doi: 10.1057/jt.2009.5. [DOI] [Google Scholar]
- 17.Bernadette H, Aussage P, Grosskopf C, et al. Development of the Cystic Fibrosis Questionnaire (CFQ) for Assessing Quality of Life in Pediatric and Adult Patients. Qual Life Res. 2003;12(1):63–76. doi: 10.1023/a:1022037320039. [DOI] [PubMed] [Google Scholar]
- 18.Sav A, Salehi A, Mair FS, et al. Measuring the burden of treatment for chronic disease: implications of a scoping review of the literature. BMC Med Res Methodol. 2017;17(1):140. doi: 10.1186/s12874-017-0411-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Underlying data
The study sample was recruited from people attending the Adult Cystic Fibrosis Center at the Royal Brompton Hospital, linked demographic and clinical data were obtained from the UK CF Registry. Participants’ consent was associated only with the VALU-CF study, and not future studies. Additional permission must be sought from the hospital to use this data in further research. To request access to the full raw data, please contact Dr. Siobhan B. Carr, S.Carr@rbht.nhs.uk. Extensive summary data can be found in the article.
Extended data
Figshare: Extended data for ‘Exploring the nature of perceived treatment burden: a study to compare treatment burden measures in adults with cystic fibrosis’. https://doi.org/10.6084/m9.figshare.1953856014.
Data are available under the terms of the Creative Commons Zero “No rights reserved” data waiver (CC0 Public domain dedication).