Abstract
Individual participant data meta-analysis (IPDMA) projects obtain, check, harmonise and synthesise raw data from multiple studies. When undertaking the meta-analysis, researchers must decide between a two-stage or a one-stage approach. In a two-stage approach, the IPD are first analysed separately within each study to obtain aggregate data (e.g., treatment effect estimates and standard errors); then, in the second stage, these aggregate data are combined in a standard meta-analysis model (e.g., common-effect or random-effects). In a one-stage approach, the IPD from all studies are analysed in a single step using an appropriate model that accounts for clustering of participants within studies and, potentially, between-study heterogeneity (e.g., a general or generalised linear mixed model). The best approach to take is debated in the literature, and so here we provide clearer guidance for a broad audience. Both approaches are important tools for IPDMA researchers and neither are a panacea. If most studies in the IPDMA are small (few participants or events), a one-stage approach is recommended due to using a more exact likelihood. However, in other situations, researchers can choose either approach, carefully following best practice. Some previous claims recommending to always use a one-stage approach are misleading, and the two-stage approach will often suffice for most researchers. When differences do arise between the two approaches, often it is caused by researchers using different modelling assumptions or estimation methods, rather than using one or two stages per se.
Keywords: individual participant data (IPD), meta-analysis, one-stage approach, two-stage approach
1. Introduction
Individual participant data meta-analysis (IPDMA) projects obtain, check, harmonise and synthesise raw data from multiple studies.1 When undertaking an IPDMA, researchers must decide between a two-stage or a one-stage approach to data synthesis.2,3 For example, in a meta-analysis of randomised trials comparing a treatment to a control, the two-stage approach first analyses the IPD separately within each trial to obtain aggregate data, such as the treatment effect estimate and its standard error. The second stage then combines these aggregate data using a standard meta-analysis model (e.g., inverse-variance weighting) to produce summary results. In contrast, the one-stage approach analyses all trials in a single step using an appropriate regression model.4 Some methodology articles strongly advocate a one-stage approach,5,6 whilst others defend the two-stage.7–9 This article aims to provide clearer guidance on when each approach can be used and emphasises that both are valuable tools in the IPDMA field. Our examples primarily focus on IPDMA of randomised trials to examine intervention effects, but the key messages also apply to most other situations where an effect estimate is of interest (e.g., prognostic factor studies).
2. One-Stage Approach Is Preferred When Most Studies Have Sparse Numbers Of Participants Or Events
In a two-stage IPDMA approach, the effect estimates derived for each study in the first stage are assumed to follow a normal sampling distribution with a known variance in the second stage.5,10–13 These assumptions are sensible if most studies have moderate to large sample sizes, as effect estimates derived using maximum likelihood estimation are asymptotically normally distributed, and variances can be estimated with reasonable accuracy.13 However, these assumptions are unreliable when most of the included studies are small (e.g., <20–30 participants in each group) or, specifically for binary, count and time-to-event outcomes, when most studies have few (e.g., <10) or no outcome events in one or more groups.5 Furthermore, effect estimates (e.g., odds ratios) in generalised linear models, such as logistic regression, are upwardly biased when outcome events are sparse,14,15 unless a debiasing approach such as Firth's correction is used.14
In contrast, by analysing all the IPD together in a single model (e.g., a general or generalised linear mixed model accounting for clustering of participants within studies5,16) the one-stage IPDMA approach avoids making assumptions of normality and known variances of effect estimates in each study. In other words, the one-stage approach allows a more exact likelihood specification in the statistical modelling. This also helps avoid the need for continuity corrections, often employed in the first stage of the two-stage approach when studies have zero outcome events in one of the (treatment) groups. Therefore, a one-stage approach is recommended in situations where most of the included studies are small in terms of the number of participants or outcome events.
For example, Box 1 presents an IPDMA of seven randomised trials with sparse outcome events in most trials. Performing a two-stage approach (with continuity corrections of +0.5 where necessary in the first stage) gives a summary odds ratio of 1.31 (95% CI: 0.33–5.16) and a between-trial variance estimate of zero, whilst a one-stage approach gives a larger summary odds ratio of 1.91 (95% CI: 0.36-10.15) and a larger between-trial variance estimate of 0.57.17,18
Box 1. Example of a situation where a one-stage IPDMA is preferred to a two-stage approach. Case study uses data from Simmonds and Higgins,17 as adapted by Riley and Debray,18 who combine IPD from seven randomised trials examining the effect of hormone replacement therapy (HRT) on the incidence of heart disease.
Data: Aggregate data derived from the IPD are shown for each trial below.
| No. women | No. cardiovascular events | |||
|---|---|---|---|---|
| Trial | Control | Treatment | Control | Treatment |
| 1 | 174 | 701 | 0 | 5 |
| 2 | 14 | 15 | 1 | 0 |
| 3 | 16 | 15 | 0 | 1 |
| 4 | 20 | 20 | 1 | 1 |
| 5 | 26 | 29 | 0 | 1 |
| 6 | 84 | 84 | 3 | 1 |
| 7 | 66 | 68 | 0 | 3 |
Methods: We used these aggregate data to reconstruct the IPD, with a row for each participant in the dataset denoting their trial, treatment group, and outcome event. We then used maximum likelihood (ML) estimation to fit a one-stage logistic regression model to this IPD, with the intercept stratified by trial and assuming random treatment effects. This one-stage approach directly models the binomial likelihood, and so handles trials with zero events in one group.
To improve ML estimation of the between-trial variance we used trial-specific centering of the treatment group variable (i.e., 1/0 for treatment/control minus the proportion of participants in the treatment group for that trial). Confidence intervals were derived using the t-distribution with six degrees of freedom.
A two-stage approach was also applied. In the first stage, a logistic regression model was fitted using ML estimation to each trial separately, with continuity corrections of +0.5 added in trials with zero events, to obtain a treatment effect estimate (log odds ratio, ) and its variance (var) for each trial. Using these aggregate data, the second stage then fitted a standard random-effects meta-analysis model using REML estimation with confidence interval derived by the Hartung-Knapp Sidik-Jonkman approach.
Results: The one-stage approach gives a summary odds ratio (exp) of 1.91 (95% CI: 0.36 to 10.15), and between-trial variance of 0.57. The wide confidence interval and large heterogeneity suggest the findings are inconclusive and additional trials are required to investigate the association between HRT and cardiovascular disease risk. Results are very different when applying a two-stage approach with continuity corrections, as the summary odds ratio is 1.31 (95% CI: 0.33 to 5.16) and is 0.
3. Unless Data Are Sparse, Evidence Shows Two-Stage And One-Stage IPDMA Results Closely Agree, Provided They Use The Same Modelling Assumptions And Estimation Method
Several articles have investigated the difference between one-stage and two-stage IPDMA results,6–10,19–28 either empirically, via simulation, or theoretically. Where the esti-mand is a summary effect of a particular variable (e.g., a treatment effect in terms of a mean difference, odds ratio or hazard ratio), most studies conclude that one-stage and two-stage approaches give very similar results, except when most studies have sparse numbers of participants or events. For example, for binary outcomes, Stewart et al.8 conclude that ‘one-stage statistical analyses may not add much value to simpler two-stage approaches’. For time-to-event outcomes, Bowden et al.9 conclude: ‘there appears to be only a very small gain in fitting more complex and computationally intensive one-stage models’. For continuous outcomes, Morris et al.7 concluded that ‘the number of stages used to fit this model is irrelevant’ as ‘provided the same underlying model is used, inference from one- and two-stage procedures is practically equivalent’.
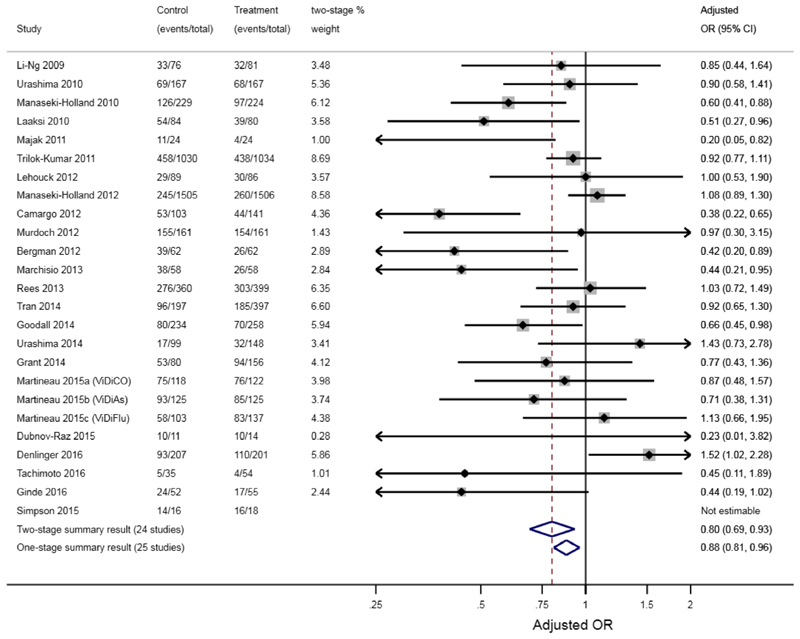
In practice, researchers may observe non-negligible differences between one-stage and two-stage IPDMA results. Box 2 catalogues the reasons why this can happen.29,30 Observed differences are usually due to researchers using different models, assumptions or estimation methods, rather than using one or two stages per se. For example, Figure 1 shows results from an IPDMA,31 with quite a large difference in the summary treatment effect from a one-stage approach (odds ratio = 0.88, 95% CI: 0.81–0.96) and a two-stage approach (odds ratio = 0.80, 95% CI: 0.69–0.93). Our instinct may be to conclude that this difference is due to the one-stage approach using a model with a more exact likelihood; however, most trials are large, and events are not sparse, therefore the two-stage approach should be a good approximation here. Instinct might also blame the exclusion of the Simpson trial from the two-stage approach, due to an adjusted odds ratio estimate being inestimable in that trial (the authors say31: ‘an estimate for the effect of the intervention in the study could not be obtained in the regression model owing to small sample size’). However, the Simpson trial is very small and so should have very little contribution to the one-stage meta-analysis anyway.
Box 2. Key reasons why researchers may observe non-negligible differences between one-stage and two-stage IPDMA results; adapted from Riley et al.29 and Burke et al.30.
More exact one-stage likelihood versus approximate two-stage likelihood—when most studies are small (few participants or events), the assumed normal likelihood for the model in the second stage of the two-stage approach can be a poor approximation.5
How clustering of participants within studies is modelled—for example, a two-stage approach estimates the intercept separately by study—but a one-stage model ignores clustering entirely or assumes a random intercept.4
Specification of nuisance parameters, such as prognostic factor and adjustment terms, and residual variances— for example, stratified by study in the two-stage approach, but assumed common or random in a one-stage model.29
Different estimation methods for τ2—for example, DerSimonian and Laird to fit the second stage of a two-stage model and maximum likelihood estimation to fit the one-stage model.
Choice of common effect or random effects for the parameter of interest (e.g., treatment effect).
Derivation of confidence intervals—for example, the one-stage approach may derive intervals using Wald-based confidence intervals, but the two-stage approach may use a t-distribution.32
Accounting for correlation amongst multiple outcomes or time-points—for example, the one-stage approach may synthesise all time-points together accounting for their correlation, whilst the two-stage approach may synthesise results for each time-point separately in the second stage.34
Handling of within-study and across-study relationships—for example, a two-stage approach may summarise treatment-covariate interactions based on only within-trial information but a one-stage model may amalgamate within-trial and across-trial information.35
Different studies or participants included in the one-stage and two-stage approaches.
Differences in other modelling choices—for example, how non-linear trends are modelled, the set of adjustment factors included, the use of automated selection procedures, and so forth.
Unintentional errors—for example, pooling odds ratios (rather than log odds ratios) in the second stage of the two-stage approach.
Figure 1. Example of a notable difference between one-stage and two-stage IPDMA results, as reported by Martineau et al.31 who synthesise IPD from 25 randomised controlled trials (10,933 participants) to examine whether Vitamin D supplementation prevented acute respiratory tract infections. Case study and figure originally shown by Riley et al.29 [Colour figure can be viewed at wileyonlinelibrary.com].
Rather, the difference is due to the use of different estimation methods to fit the random-effects models: maximum likelihood estimation for the one-stage model and DerSimonian and Laird for the second stage model of the two-stage approach. These lead to different estimates of between-study variance different trial weights in the meta-analyses, and subsequently different summary treatment effect estimates and confidence intervals. If we rather constrain to be the same in one-stage and two-stage analyses, the results are practically identical. For example, a two-stage IPDMA constraining to be zero gives a summary OR of 0.88 (95% CI: 0.81–0.96), identical to results from the one-stage model (Figure 1). Hence, the decision here is more about choosing the best estimation method, rather than deciding between a one-stage or two-stage approach—indeed, simulation studies suggest REML estimation is preferred for either the one-stage or two-stage approaches assuming random treatment effects, unless outcome events are sparse in most studies.32,33
4. One-Stage To Rule Them All? Claims To Always Use The One-Stage Approach Are Misleading
Some previous claims of superiority for the one-stage approach are unfair. For example, Mathew and Nördstrom suggest that ‘significant loss of precision may result from using the two-step IPD meta-analysis estimator’.26 However, their main example of an inequality was when the intercept term was assumed common to all trials, which is of no practical interest as it breaks randomisation in each trial.4
Similarly, Kontopantelis conclude that ‘a fully specified one-stage model should be preferred, especially when investigating interactions’ because it leads to more precise interaction estimates.6 However, on inspection of their simulation results, there is nothing to separate the two procedures when focusing on the overall treatment effect in the absence of an interaction. When examining treatment-covariate interactions, the one-stage model performs better but only because it allowed both within-trial and across-trial information to contribute (whereas the two-stage approach only used within-trial information). Incorporation of across-trial information introduces aggregation bias due to trial-level confounding and breaks the within-trial exchangeability afforded by randomisation.36,37 The setting investigated by Kontopantelis was the very narrow situation of no trial-level confounding, but trial-level confounding often occurs in practice. Further, if desired, the two-stage approach can also be extended to combine both within-trial and across-trial information, by pooling the summary estimate from a meta-analysis of within-trial interaction estimates with the across-trial association estimate from a meta-regression.35 Thus, their general recommendation to prefer one-stage models is not justified or fair.
Statisticians might envisage that a one-stage model is more powerful as it estimates all parameters simultaneously. However, in situations where all parameters are estimated in every study, and nuisance parameters are stratified by study, accounting for their correlation has surprisingly little impact on the summary effect of inter-est.23 Gains only arise if stronger assumptions are made that are hard to justify, such as placing between-study distributional assumptions on nuisance parameters.
5. One-Stage-Fits-All? Perceived Flexibility Of One-Stage Models Is Deceiving
Some researchers advocate the one-stage approach due to its ‘increasing flexibility’ in the modelling, in terms of the assumptions or model specification. For example, one-stage models can easily specify residual variances to be the same in every study38; study intercepts to be drawn from some distribution, or study baseline hazard functions to be proportional. However, the flipside to this ‘flexibility’ is that it can lead to modelling mistakes (e.g., ignoring clustering) and unjustified strong assumptions, which may produce biased or overly precise con-clusions.4,30,39 Further, many bespoke one-stage models can be replicated in a two-stage approach anyway,40 for example by extending to a multivariate framework in the second stage to place distributional assumptions on nuisance parameters, such as residual variances.41,42
Therefore, the promise of one-stage ‘flexibility’ is often more about convenience than a scientific advantage. It is even deceiving, as the two-stage approach could also be portrayed as more flexible than the one-stage approach. For example, when synthesising studies with different and complex designs (e.g., cluster trials, parallel-group trials), the first stage of the two-stage approach can easily tailor models to address the design of study,43 whereas this is more challenging in a one-stage approach (though possi- ble34,44,45). A two-stage approach is also more practical when the IPD from all studies cannot be harmonised altogether (e.g., if data sharing agreements for some studies only allow IPD to be accessed remotely at the host institution), or when needing to include aggregate data from studies not providing IPD.1 Visualisation of a two-stage meta-analysis is also easier, for example via a forest plot containing study-specific estimates, percentage study weights and summary results.
Finally, the two approaches do not make any different default assumptions about missing data: complete case analysis is valid when missing outcomes and missing covariates are missing depending only on the values of (other) covariates included in the model. If the approach to handling missing data needs to differ in each study, this may be more convenient to handle in the first stage of the two-stage approach via study-specific (imputation) models. However, if there are systematically missing covariates, a one-stage model for imputation may be preferable to allow borrowing of information across studies.46 Regardless of how missing data are handled (e.g., whether missing values are multiply imputed based on a one-stage model or study-specific models), in principle either two-stage or one-stage IPD meta-analysis models could still be used for the main analysis if they are congenial with the imputation model.
6. Discussion And Recommendations
So, two-stage or not two-stage? If most studies in the IPDMA are small (few participants or events), a one-stage approach is recommended. In other situations, researchers can choose either approach, carefully following best practice.1 Although one-stage models are a suitable choice, they require much care to specify correctly (see example code at https://www.ipdma.co.uk/one-stage-ipd-ma) and deal with complexities, such as centering covariates,32 and separating within-study and across-study relationships.35 For this reason, unless data are sparse, the two-stage approach will often suffice, with dedicated software options either for both stages (ipdmetan47) or just the second stage (e.g., metan,48 and metafor49). Where feasible, it can be helpful and transparent to do both one-stage and two-stage analyses, and report both. If their results are appreciably different, it is important to identify and understand why, guided by the reasons listed in Box 2 and related guidance.29
Highlights.
What is already known
An individual participant data meta-analysis (IPDMA) can be undertaken using either a two-stage or a one-stage approach.
In a two-stage approach, the IPD are first analysed separately within each study to obtain aggregate data; then, in the second stage, these aggregate data are combined in a standard meta-analysis model.
In a one-stage approach, the IPD from all studies are analysed in a single step using an appropriate model that accounts for clustering of participants within studies.
The best approach to take is debated in the literature.
What is new
If most studies in the IPDMA are small (few participants or events), a one-stage approach is recommended due to using a more exact likelihood.
In other situations, researchers can choose either approach, carefully following best practice.
Previous claims in favour of always using a one-stage approach are often misleading.
Neither approach is a panacea, but both are important tools for IPDMA projects.
Potential impact for Research Synthesis Methods readers
Unless most studies are small (few participants or events), any observed differences between one-stage and two-stage approaches are likely due to researchers using different models, assumptions or estimation methods, rather than using one or two stages per se.
One-stage models require great care to specify correctly and so, unless data are sparse, the two-stage approach will often suffice for most researchers.
Funding Information
Richard D. Riley and Joie Ensor were supported by an MRC-NIHR Better Methods Better Research grant (reference: MR/V038168/1), and the NIHR Birmingham Biomedical Research Centre at the University Hospitals Birmingham NHS Foundation Trust and the University of Birmingham. Tim P. Morris is funded by the UKRI Medical Research Council (grants MC_UU_00004/06 and MC_UU_00004/07). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Funding information
Medical Research Council & National Institute for Health and Care Research, Grant/Award Number: MR/V038168/1; National Institute for Health and Care Research Birmingham Biomedical Research Centre; UKRI Medical Research Council, Grant/Award Numbers: MC_UU_00004/07, MC_UU_00004/06
Footnotes
Author Contributions
Richard D. Riley: Conceptualization; investigation; methodology; writing – original draft; writing – review and editing; software; formal analysis; data curation; supervision; project administration. Joie Ensor: Writing – review and editing; methodology; investigation; project administration. Miriam Hattle: Writing – review and editing; methodology. Katerina Papadimitropou- lou: Writing – review and editing; methodology. Tim P. Morris: Methodology; writing – review and editing.
Conflict Of Interest Statement
Richard Riley is the lead Editor on the book ‘Individual Participant Data Meta-Analysis: A Handbook for Healthcare Research’ for which he receives royalties.
Richard D. Riley @Richard_D_Riley
Data Availability Statement
Data sharing not applicable to this article as no datasets with individual participant data were generated or analysed during the current study. The aggregate data for the trials of the two main examples is already provided in Figure 1 and Box 1.
References
- 1.Riley RD, Tierney JF, Stewart LA, editors. Individual Participant Data Meta-Analysis: A Handbook for Healthcare Research. Wiley; 2021. [Google Scholar]
- 2.Simmonds MC, Higgins JPT, Stewart LA, Tierney JF, Clarke MJ, Thompson SG. Meta-analysis of individual patient data from randomized trials: a review of methods used in practice. Clin Trials. 2005;2:209–217. doi: 10.1191/1740774505cn087oa. [DOI] [PubMed] [Google Scholar]
- 3.Riley RD, Lambert PC, Abo-Zaid G. Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ. 2010;340:c221. doi: 10.1136/bmj.c221. [DOI] [PubMed] [Google Scholar]
- 4.Abo-Zaid G, Guo B, Deeks JJ, et al. Individual participant data meta-analyses should not ignore clustering. J Clin Epidemiol. 2013;66(8):865–873.:e4. doi: 10.1016/j.jclinepi.2012.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stijnen T, Hamza TH, Özdemir P. Random effects meta-analysis of event outcome in the framework of the generalized linear mixed model with applications in sparse data. Stat Med. 2010;29:3046–3067. doi: 10.1002/sim.4040. [DOI] [PubMed] [Google Scholar]
- 6.Kontopantelis E. A comparison of one-stage vs two-stage individual patient data meta-analysis methods: a simulation study. Res Synth Methods. 2018;9(3):417–430. doi: 10.1002/jrsm.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morris TP, Fisher DJ, Kenward MG, Carpenter JR. meta-analysis of gaussian individual patient data: two-stage or not two-stage? Stat Med. 2018;37(9):1419–1438. doi: 10.1002/sim.7589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stewart GB, Altman DG, Askie LM, Duley L, Simmonds MC, Stewart LA. Statistical analysis of individual participant data meta-analyses: a comparison of methods and recommendations for practice. PloS One. 2012;7(10):e46042. doi: 10.1371/journal.pone.0046042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bowden J, Tierney JF, Simmonds M, Copas AJ, Higgins JP. Individual patient data meta-analysis of time-to-event outcomes: one-stage versus two-stage approaches for estimating the hazard ratio under a random effects model. Res Synth Methods. 2011;2(3):150–162. doi: 10.1002/jrsm.45. [DOI] [PubMed] [Google Scholar]
- 10.Debray TP, Moons KG, Abo-Zaid GM, Koffijberg H, Riley RD. Individual participant data meta-analysis for a binary outcome: one-stage or two-stage? PloS One. 2013;8(4):e60650. doi: 10.1371/journal.pone.0060650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hamza TH, van Houwelingen HC, Stijnen T. The binomial distribution of meta-analysis was preferred to model within-study variability. J Clin Epidemiol. 2008;61(1):41–51. doi: 10.1016/j.jclinepi.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 12.Turner RM, Omar RZ, Yang M, Goldstein H, Thompson SG. A multilevel model framework for meta-analysis of clinical trials with binary outcomes. Stat Med. 2000;19(24):3417–3432. doi: 10.1002/1097-0258(20001230)19:24<3417::aid-sim614>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 13.Jackson D, White IR. When should meta-analysis avoid making hidden normality assumptions? Biom J. 2018;60(6):1040–1058. doi: 10.1002/bimj.201800071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Firth D. Bias reduction of maximum likelihood estimates. Bio-metrika. 1993;80(1):27–38. [Google Scholar]
- 15.Greenland S, Mansournia MA, Altman DG. Sparse data bias: a problem hiding in plain sight. BMJ. 2016;352:i1981. doi: 10.1136/bmj.i1981. [DOI] [PubMed] [Google Scholar]
- 16.Crowther MJ, Riley RD, Staessen JA, Wang J, Gueyffier F, Lambert PC. Individual patient data meta-analysis of survival data using Poisson regression models. BMC Med Res Methodol. 2012;12:34. doi: 10.1186/1471-2288-12-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Simmonds MC, Higgins JP. A general framework for the use of logistic regression models in meta-analysis. Stat Methods Med Res. 2016;25(6):2858–2877. doi: 10.1177/0962280214534409. [DOI] [PubMed] [Google Scholar]
- 18.Riley RD, Debray TP. In: Individual Participant Data Meta-Analysis: A Handbook for Healthcare Research. Riley RD, Tierney JF, Stewart LA, editors. Wiley; 2021. Chapter 6: The one-stage approach to IPD meta-analysis. [Google Scholar]
- 19.Koopman L, van der Heijden GJ, Hoes AW, Grobbee DE, Rovers MM. Empirical comparison of subgroup effects in conventional and individual patient data meta-analyses. Int J Tech-nol Assess Health Care. 2008;24(3):358–361. doi: 10.1017/S0266462308080471. [DOI] [PubMed] [Google Scholar]
- 20.Tudur Smith C, Williamson PR. A comparison of methods for fixed effects meta-analysis of individual patient data with time to event outcomes. Clin Trials. 2007;4(6):621–630. doi: 10.1177/1740774507085276. [DOI] [PubMed] [Google Scholar]
- 21.Steinberg KK, Smith SJ, Stroup DF, et al. Comparison of effect estimates from a meta-analysis of summary data from published studies and from a meta-analysis using individual patient data for ovarian cancer studies. Am J Epidemiol. 1997;145(10):917–925. doi: 10.1093/oxfordjournals.aje.a009051. [DOI] [PubMed] [Google Scholar]
- 22.Debray TP, Moons KG, van Valkenhoef G, et al. Get real in individual participant data (IPD) meta-analysis: a review of the methodology. Res Synth Methods. 2015;6(4):293–309. doi: 10.1002/jrsm.1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lin DY, Zeng D. On the relative efficiency of using summary statistics versus individual-level data in meta-analysis. Biometrika. 2010;97(2):321–332. doi: 10.1093/biomet/asq006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tierney JF, Vale C, Riley R, et al. Individual participant data (IPD) meta-analyses of randomised controlled trials: guidance on their use. PLoS Med. 2015;12(7):e1001855. doi: 10.1371/journal.pmed.1001855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mathew T, Nordstrom K. On the equivalence of meta-analysis using literature and using individual patient data. Biometrics. 1999;55(4):1221–1223. doi: 10.1111/j.0006-341x.1999.01221.x. [DOI] [PubMed] [Google Scholar]
- 26.Mathew T, Nordström K. Comparison of one-step and two-step meta-analysis models using individual patient data. Biom J. 2010;52:271–287. doi: 10.1002/bimj.200900143. [DOI] [PubMed] [Google Scholar]
- 27.Olkin I, Sampson A. Comparison of meta-analysis versus analysis of variance of individual patient data. Biometrics. 1998;54(1):317–322. [PubMed] [Google Scholar]
- 28.Senn S. Hans van Houwelingen and the art of summing up. Biom J. 2010;52(1):85–94. doi: 10.1002/bimj.200900074. [DOI] [PubMed] [Google Scholar]
- 29.Riley RD, Burke DL, Morris TP. In: Individual Participant Data Meta-Analysis: A Handbook for Healthcare Research. Riley RD, Tierney JF, Stewart LA, editors. Wiley; 2021. Chapter 8: One-stage versus two-stage approach to IPD meta-analysis: differences and recommendations. [Google Scholar]
- 30.Burke DL, Ensor J, Riley RD. Meta-analysis using individual participant data: one-stage and two-stage approaches, and why they may differ. Stat Med. 2017;36(5):855–875. doi: 10.1002/sim.7141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Martineau AR, Jolliffe DA, Hooper RL, et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583. doi: 10.1136/bmj.i6583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Riley RD, Legha A, Jackson D, et al. One-stage individual participant data meta-analysis models for continuous and binary outcomes: comparison of treatment coding options and estimation methods. Stat Med. 2020;39(19):2536–2555. doi: 10.1002/sim.8555. [DOI] [PubMed] [Google Scholar]
- 33.Langan D, Higgins JPT, Jackson D, et al. A comparison of heterogeneity variance estimators in simulated random-effects meta-analyses. Res Synth Methods. 2019;10(1):83–98. doi: 10.1002/jrsm.1316. [DOI] [PubMed] [Google Scholar]
- 34.Jones AP, Riley RD, Williamson PR, Whitehead A. meta-analysis of individual patient data versus aggregate data from longitudinal clinical trials. Clin Trials. 2009;6(1):16–27. doi: 10.1177/1740774508100984. [DOI] [PubMed] [Google Scholar]
- 35.Riley RD, Debray TPA, Fisher D, et al. Individual participant data meta-analysis to examine interactions between treatment effect and participant-level covariates: statistical recommendations for conduct and planning. Stat Med. 2020;39(15):2115–2137. doi: 10.1002/sim.8516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hua H, Burke DL, Crowther MJ, Ensor J, Tudur Smith C, Riley RD. One-stage individual participant data meta-analysis models: estimation of treatment-covariate interactions must avoid ecological bias by separating out within-trial and across-trial information. Stat Med. 2017;36(5):772–789. doi: 10.1002/sim.7171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fisher DJ, Carpenter JR, Morris TP, Freeman SC, Tierney JF. Meta-analytical methods to identify who benefits most from treatments: daft, deluded, or deft approach? BMJ. 2017;356:j573. doi: 10.1136/bmj.j573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Papadimitropoulou K, Stijnen T, Dekkers OM, le Cessie S. One-stage random effects meta-analysis using linear mixed models for aggregate continuous outcome data. Res Synth Methods. 2019;10(3):360–375. doi: 10.1002/jrsm.1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Abo-Zaid G, Sauerbrei W, Riley RD. Individual participant data meta-analysis of prognostic factor studies: state of the art? BMC Med Res Methodol. 2012;12:56. doi: 10.1186/1471-2288-12-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Senn S. The many modes of meta. Drug Inf J. 2000;34(2):535–549. [Google Scholar]
- 41.Senn S, Schmitz S, Schritz A, Salah S. Random main effects of treatment: a case study with a network meta-analysis. Biom J. 2019;61(2):379–390. doi: 10.1002/bimj.201700265. [DOI] [PubMed] [Google Scholar]
- 42.Senn S. Various varying variances: the challenge of nuisance parameters to the practising biostatistician. Stat Methods Med Res. 2015;24(4):403–419. doi: 10.1177/0962280214520728. [DOI] [PubMed] [Google Scholar]
- 43.Brunner M, Keller L, Stallasch SE, et al. Meta-analyzing individual participant data from studies with complex survey designs: a tutorial on using the two-stage approach for data from educational large-scale assessments. Res Synth Methods. 2023;14(1):5–35. doi: 10.1002/jrsm.1584. [DOI] [PubMed] [Google Scholar]
- 44.Sutton AJ, Kendrick D, Coupland CA. Meta-analysis of individual-and aggregate-level data. Stat Med. 2008;27:651–669. doi: 10.1002/sim.2916. [DOI] [PubMed] [Google Scholar]
- 45.Riley RD, Lambert PC, Staessen JA, et al. Meta-analysis of continuous outcomes combining individual patient data and aggregate data. Stat Med. 2008;27(11):1870–1893. doi: 10.1002/sim.3165. [DOI] [PubMed] [Google Scholar]
- 46.Quartagno M, Carpenter JR. Multiple imputation for discrete data: evaluation of the joint latent normal model. Biom J. 2019;61(4):1003–1019. doi: 10.1002/bimj.201800222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fisher DJ. Two-stage individual participant data meta-analysis and generalized forest plots. Stata J. 2015;15(2):369–396. [Google Scholar]
- 48.Fisher D, Harris R, Bradburn M, et al. METAN: Stata Module for Fixed and Random Effects Meta-Analysis. 2022 [Google Scholar]
- 49.Viechtbauer W. Conducting meta-analyses in R with the Meta-for Package 2010. J Stat Softw. 2010;36(3):48. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets with individual participant data were generated or analysed during the current study. The aggregate data for the trials of the two main examples is already provided in Figure 1 and Box 1.