Abstract
Expression of the CTLA-4 gene is absolutely required for immune homeostasis but aspects of its molecular nature remain undefined. In particular, the characterization of the soluble CTLA-4 (sCTLA-4) protein isoform generated by an alternatively spliced mRNA of CTLA4 lacking transmembrane-encoding exon 3 has been hindered by the difficulty in distinguishing it from the transmembrane isoform of CTLA-4, Tm-CTLA-4. In the present study, sCTLA-4 has been analyzed using novel monoclonal and polyclonal antibodies specific for its unique C-terminal amino acid sequence. We demonstrate that the sCTLA-4 protein is secreted at low levels following the activation of primary human CD4+ T cells and is increased only rarely in the serum of autoimmune patients. Unexpectedly, during our studies aimed to define the kinetics of sCTLA-4 produced by activated human CD4+ T cells, we discovered that Tm-CTLA-4 is associated with microvesicles (mvCTLA-4) produced by the activated cells. The functional roles of sCTLA-4 and microvesicle-associated Tm-CTLA-4 warrant further investigation, especially as they relate to the multiple mechanisms of action described for the more commonly studied cell-associated Tm-CTLA-4.
Introduction
The Tm-CTLA-4 receptor plays a crucial role in the downregulation of the immune response and the maintenance of immune homeostasis as shown by the lymphoproliferative syndrome and early lethality of CTLA-4-deficient mice (1-3). Tm-CTLA-4 is expressed by activated T cells whereas it is constitutively expressed and required for Treg suppression (4-6). At the molecular level, previous studies have provided evidence that an alternatively spliced mRNA of the CTLA-4 gene that lacks exon 3 is expressed in human, mouse and rat immune cells (7, 8). As a result of splicing between exons 2 and 4, the predicted soluble CTLA-4 (sCTLA-4) isoform does not have a transmembrane domain or the membrane-proximal cysteine residue required for covalent homodimerization of the conventional transmembrane isoform of CTLA-4 (Tm-CTLA-4) (9), thereby predicting a secreted, or soluble, isoform of monomeric CTLA-4 (sCTLA-4). The skipping of exon 3 predicts a shift in the reading frame generating a C-terminal amino acid sequence that distinguishes sCTLA-4 from Tm-CTLA-4 (7). In both human and mouse sCTLA-4 mRNA expression is mainly detected in resting T cells and its level is similar to that of Tm-CTLA-4 mRNA, whereas, following T cell activation, Tm-CTLA-4 is rapidly upregulated and becomes the predominant transcript (7, 8, 10-12). In humans, SNP CT60 (rs3087243) in the 3′ untranslated region of human CTLA4 is associated with multiple autoimmune diseases including type 1 diabetes (T1D), Graves’ disease (GD), rheumatoid arthritis and coeliac disease (10, 13-16). At the cellular level SNP CT60 is correlated with changes in mRNA levels of sCTLA-4; lower levels of sCTLA-4 mRNA were detected in resting CD4+ T cells and CD4+ CD25+ FOXP3+ regulatory T cells (Tregs) of healthy donors carrying a T1D susceptible genotype at SNP CT60 as compared with donors having the protective genotype (10, 17).
The extracellular domain of sCTLA-4, similar to that of the integral membrane isoform, contains the MYPPY motif involved in binding to the CD28–shared CD80/CD86 ligands on antigen presenting cells (APC). In a mixed lymphocyte response, recombinant sCTLA-4 showed immunomodulatory properties capable of suppressing cell proliferation in a dose-dependent manner (7). Levels ranging from 2 to 96 ng/ml of a material reported to be sCTLA-4 have been detected in the serum of patients with autoimmune thyroid diseases (18), systemic lupus erythematosus (SLE) (19, 20), spondylarthropathies (20), coeliac disease (21), Crohn’s disease (22), cutaneous systemic sclerosis (23), type 1 diabetes (24, 25) and were correlated with disease activity and clinical features (20-23). All of the studies on patients’ sera used immunoglobulin-based binding assays recognizing the extracellular domain of CTLA-4, not antibodies specific for the soluble isoform of CTLA-4. The true molecular nature of the material in these sera recognized by anti-CTLA-4 antibodies has been questioned (26) by the same laboratory that originally reported the increase of sCTLA-4 in autoimmune disease (18). Analysis of proteins immunoprecipitated from plasma donated by patients with autoimmune disease with a pool of anti-CTLA-4 antibodies specific for the N-terminal CD80/CD86 binding domain of CTLA-4 has shown that the isolated molecules exhibited characteristics common to immunoglobulins and were able to interact with CD80 and CD86 ligands, but did not have the sequence of an isoform of CTLA-4 (26).
The accurate detection of human sCTLA-4 protein has been hampered by the lack of validated antibodies that specifically target this isoform with high affinity. In this study antibodies that specifically recognize the recombinant soluble isoform of CTLA-4 have been generated and characterized to determine if primary human T cells produce the sCTLA-4 protein in addition to expressing the alternatively spliced message and to evaluate sCTLA-4 levels in patients with autoimmune disease. We report that sCTLA-4 is secreted by in vitro activated human CD4+ T cells. However, sCTLA-4 is only rarely detected in serum samples from patients with autoimmune diseases or from healthy volunteers consistent with the findings of Oaks and colleagues (26). In addition to characterizing sCTLA-4 protein secreted from in vitro activated T cells, we observed that these cells also released Tm-CTLA-4 associated with nano-sized microvesicles (mvCTLA-4).
Materials and Methods
Subjects
Blood samples for CD4+ T cell purification were obtained from Cambridge BioResource donors not having any known autoimmune disease with the prior approval of the National Health Service Cambridgeshire Research Ethics Committee. Serum/plasma collections were obtained from patients with T1D and GD. The 15 female and 3 male GD patients whose sera were tested ranged in age from 20 to 54 years; sera were collected prior to treatment. Sera from GD patients and from healthy donors (n=15) matched in age and sex to the GD patients were kindly provided by Professor Krishna Chatterjee (University of Cambridge). T1D patients were 7 females and 7 males and ranged in age from 23 to 53 years. Ten T1D patients had comorbid medical conditions: 8 patients had GD, one had multiple sclerosis and GD and one was affected with rheumatoid arthritis. Sera from healthy volunteers (n=14) that were matched in age and sex with the T1D patients were analyzed as controls.
RNA extraction and cDNA synthesis
Total RNA from purified human CD4+ T cells and splenic CD4+ T cells from C57BL/10 mice was extracted using Trizol reagent (Invitrogen) according to the manufacturer’s instructions. First strand complementary DNA from total RNA was synthesized using Superscript II reverse transcriptase (Invitrogen) according to the manufacturer’s instructions.
Construction of recombinant expression vectors
The entire open reading frame encoding human CTLA-4 was obtained by PCR amplification of cDNA from human CD4+ T cells using the following primers: forward GAACACCGCTCCCATAAAG, reverse GGTTTCTCAATTGATGGGAATAA. The entire mouse Ctla4 open reading frame was amplified by PCR of cDNA derived from CD4+ T cells isolated from C57BL/10 mice using the following primers: forward GCCATGGCTTGTCTTGGACT, reverse AACGGCCTTTCAGTTGATG. Human and mouse Tm-CTLA-4 and sCTLA-4 PCR products were gel purified with QIAquick Gel Extraction kit (QIAGEN) and cloned into the pcDNA™3.1/V5-HIS-TOPO expression vector (Invitrogen) according to the manufacturer’s instructions. The CTLA4 stop codon was included in the vector thereby preventing the inclusion of the polyhistidine tag in the recombinant protein. Clones were verified by sequencing on an ABI PRISM 3700 DNA sequencer (Applied Biosystems). Endofree plasmid maxi kit (Qiagen) was used to generate endotoxin free DNA for transfection.
Generation of sCTLA-4-specific polyclonal and monoclonal antibodies
Antibodies reactive with sCTLA-4 but not Tm-CTLA-4 were generated in collaboration with Cambridge Research Biochemical, Cambridge, UK. Polyclonal antibody 4017 was generated by immunisation of rabbits with a modified human sCTLA-4 synthetic peptide, C-Ahx-ENAPNRARM-acid, conjugated to keyhole limpet hemocyanin (KLH) through the N-terminal cysteine using m-maleimidobenzoyI-N-hydroxysuccinimide ester. Aminohexanoic acid (Ahx) was added to the sequence as a spacer to increase the distance of the peptide from the KLH protein carrier. Antibodies with reactivity against the sCTLA-4 peptide were affinity-purified on a peptide-conjugated column followed by depletion of any remaining anti-KLH antibodies using a KLH-coupled affinity matrix. The 4B8 and 10D1 mAbs were developed following immunisation of BALB/c mice with the modified sCTLA-4 synthetic peptide [C]-IAKEKKPSYNRGLSENAPNRARM-acid conjugated to KLH through the N-terminal cysteine. Spleen cells of mice with serum reactivity against both the synthetic peptide and recombinant sCTLA-4 were used for the production of hybridomas. sCTLA-4-specific antibody-producing clones 4B8 and 10D1 were identified by binding to the peptide used for immunization and verified by binding to recombinant human sCTLA-4 but not Tm-CTLA-4. Following repeated cloning to obtain stable production, bulk quantities of 4B8 and 10D1 (fermentation/purification) were obtained from Bio X Cell, West Lebanon, NH.
HeLa transient cell transfection, total protein extracts and cell supernatant collection
HeLa cells were grown in DMEM supplemented with 10% heat inactivated FBS, 100 units penicillin and 100 μg streptomycin (Invitrogen) and 2mM L-Glutamine (Sigma-Aldrich) at 37 °C in a humidified 5% CO2 incubator. For transient plasmid transfection of HeLa cells, PolyJet™ transfection reagent (SignaGen Laboratories) was used according to the manufacturer’s protocol. HeLa cells were seeded at 7 × 105 cells per well in a 6 well plate in complete DMEM medium and allowed to attach for 24 hours before transfection. Transfected cells were harvested after 72 hours with 0.25% trypsin-EDTA solution (Sigma-Aldrich). For tunicamycin treatment, transfected cells were cultured for 48 hours and then incubated with 5 μg/ml of tunicamycin for an additional 5 hours. Washed cell pellets were resuspended in lysis buffer (50 mM Tris pH8.0, 150 mM NaCl, 2 mM EDTA, 1% IGEPAL CA-630 (Sigma-Aldrich) containing protease and phosphatase inhibitors (1 mM NaF, 1 mM Na3VO4, 1% protease inhibitor cocktail (Sigma-Aldrich)) for 30 minutes on ice followed by centrifugation at 13,000 × g to remove cell debris. Culture supernatants from transfected HeLa cells were centrifuged at 500 × g, followed by filtration through a 0.22 μM filter. Cell lysates and culture supernatants were stored at −80°C.
CD4+ T cell isolation and stimulation
CD4+ T cells were enriched by negative selection from whole blood freshly collected in heparinized tubes using an immunorosetting method according to the manufacturer’s protocol (RosetteSep™ Human CD4+ T Cell Enrichment Cocktail, STEMCELL Technologies). CD4+ T cells were resuspended at 1-3 × 106 cells/ml in exosome-depleted 10% FBS X-VIVO medium and stimulated either with plate-coated anti-CD3 (OKT3, 0.5 μg/ml, Bio X Cell, West Lebanon, NH) and anti-CD2 mAbs (T1.11, T1.12 1 μg/ml each, antibodies-online.com) or with anti-CD3/CD28 Dynabeads (Invitrogen, Life Technologies) at a cell to bead ratio 1:0.5. Exosome-depleted medium was generated by overnight centrifugation at 100000 × g at 4°C of X-VIVO medium plus 20% FBS. Medium was filtered through a 0.22 μm filter and diluted at a final concentration of 10% FBS with X-VIVO medium plus penicillin/streptomycin. Total cell lysates were made as described for HeLa cell transfectants and stored at −80°C.
Western Blot analysis
Samples were denatured at 70°C in NuPAGE LDS sample buffer (Invitrogen) for 10 minutes and separated on NuPAGE Novex 10% Bis-Tris or 3-8% Tris Acetate gels (Invitrogen) under reducing and non-reducing conditons. Lysates from 2 × 104 and 5-10 × 103 cells of sCTLA-4 and Tm-CTLA-4 HeLa transfectants or from 5-10 × 104 anti-CD3/CD2 stimulated CD4+ T cells were loaded per well. Proteins were electrophoretically transferred to Invitrolon PVDF (Invitrogen) membranes in transfer buffer (2.5 mM TRIS, 19.2 mM glycine, 0.1% SDS) with 20% methanol. Membranes were blocked with 2% ECL Advance Blocking Agent (GE Healthcare) in PBS with 0.05% (w/v) Tween 20 (PBS-T). Primary antibodies against specific proteins were incubated in 1% ECL Advance Blocking Agent PBS-T overnight at 4°C. Antibody reactivity was detected following 1 hour incubation at room temperature with peroxidase-conjugated secondary antibodies using a chemiluminescent detection system (Pierce® ECL 2 Western Blotting substrate, Thermo Scientific) and visualised by exposure to Amersham Hyperfilm™ ECL (GE Healthcare). Primary and secondary antibodies used were: anti-CTLA-4 (C19), a polyclonal Ab generated in goat using the C-terminal sequence from Tm-CTLA-4, (Santa Cruz Biotechnology) followed by Pierce peroxidase-conjugated recombinant protein G (Thermo Scientific), anti-CD3ζ (D-4), anti-HLA class I (HP1F7) (Santa Cruz Biotechnology), anti-CD63 (H5C6), anti-CD107b (LAMP2, H4B4) (BD Pharmingen), anti-sCTLA-4 4B8 and anti-sCTLA-4 10D1 followed by peroxidaseconjugated anti-mouse IgG (Santa Cruz Biotechnology) and anti-sCTLA-4 4017 followed by peroxidase-conjugated anti-rabbit IgG (Vector Laboratories).
Immunoprecipitation
Immunoprecipitation was performed using Dynabeads Co-Immunoprecipitation Kit (Invitrogen) according to manufacturer’s instructions. Briefly, 6 μg of 4B8 or isotype control mouse IgG2b mAb (BioLegend) were coupled to 5 mg of Dynabeads M-270 Epoxy (Life Technologies). Between 1.5-2 mg coupled Dynabeads were used to immunoprecipitate sCTLA-4. Immunoprecipitation was carried out overnight at 4oC under rotation followed by elution of precipitated protein in the provided extraction buffer (pH 2.8).
Isolation of microvesicles
Microvesicle isolation was performed on supernatant harvested from CD4+ T cells cultured in X-VIVO/10% FBS exosome-depleted medium after 72 hour stimulation with plate-coated anti-CD3 and anti-CD2. Microvesicle isolation was based on the protocol previously published (27). CD4+ T cell culture supernatants were sequentially centrifuged to eliminate cell debris, apoptotic bodies and microvesicles >100 nm (all carried out at 4oC): 300 × g for 5 minutes, 1200 × g for 20 minutes and 10000 × g for 30 minutes (28, 29). Final supernatants were filtered through a 0.22 μM filter and ultracentrifuged at 100,000 × g for 1 hour at 4oC, pellets were resuspended in 10 ml ice-cold PBS and ultracentrifuged at 100,000 × g for 1 hour. Microvesicle isolation from plasma and serum samples was performed as previously published (29). In brief, 5 to 7 ml plasma or serum samples diluted 1:1 in DPBS (PAA, GE Healthcare) were centrifuged at 2000 × g for 30 minutes and 12000 × g for 45 minutes followed by 2 hours at 110,000 × g. Pellets were resuspended in 10 ml ice-cold PBS, filtered through a 0.22 μM filter and ultracentrifuged at 110,000 × g for 70 minutes; wash and ultracentrifugation steps were repeated.Microvesicle-containing pellets were resuspended in 100μl PBS for electron microscopy and Western blot analyses or in 100 μl of the 1% IGEPAL lysis buffer described above for CTLA-4 immunoassays.
Immunoelectron Microscopy
Microvesicle fractions resuspended in PBS obtained from ultracentrifugation of culture supernatants of CD4+ T cells after 72 hours of stimulation were bound to glow-discharged formvar-coated grids contrasted with 1% uranyl acetate. Immunogold labelling of vesicles for CD63 was performed by staining with mouse anti-human CD63 mAb MEM-259 (Abcam) followed by goat anti-mouse IgG coupled to 10 nm gold (BBInternational). Samples were viewed with a FEI™ Tecnai G20 transmission electron microscope operated at 120kV. Images were captured using an AMT XR60B (Deben) digital camera running Deben software.
Flow cytometric analysis
HeLa cells were dissociated with trypsin, washed twice in PBS, fixed with Cytofix/Cytoperm (BD Bioscience) for 20 minutes at 4°C, washed twice with 1X Perm/Wash (BD Bioscience) and resuspended in 1X Perm/Wash. sCTLA-4-specific rabbit anti-human 4017 polyclonal Ab, mouse IgG1 anti-human 10D1 mAb and mouse IgG2b anti-human 4B8 mAb were labelled with Zenon Alexafluor 647 rabbit IgG Labelling Kit, Zenon Alexafluor 647 mouse IgG1 Labelling Kit or Zenon AlexaFluor 647 mouse IgG2b Labelling Kit, (Molecular Probes, Life technologies). Matched isotype controls, rabbit IgG (Southern Biotech) and mouse IgG1 and IgG2b (Biolegend), were similarly labelled and used as negative controls. Cells were stained with each of the above antibodies together with anti-CD152/CTLA-4-PE BN13 or a mouse IgG2a-PE (BD Bioscience) isotype control for 30 minutes at 4°C, washed twice and resuspended in Cell Wash (BD Bioscience). For microvesicle staining, 50-100 μl of microvesicles purified from CD4+ T cell culture supernatant or plasma/serum were incubated with 10 μl of 4 μM aldehyde/sulphate polystyrene latex beads (Molecular Probes, Invitrogen) for 15 min at room temperature. The volume was brought to 1 ml with PBS followed by gentle rotation for 2 h. Any remaining binding sites on the beads were then saturated by incubation with glycine (100 mM final in PBS) for 30 min, washed three times with PBS/0.5% BSA and resupended in 500 μl of PBS/BSA. 10 μl coated beads were incubated for 30 min at 4°C with anti-CD63-PE (H5C6) or anti-CD152-PE (BN13) or their respective isotype controls, mouse IgG1-PE or mouse IgG2a-PE and washed twice with PBS/BSA.
Samples were processed on a BD LSRFortessa cell analyzer (BD Bioscience). Data were analyzed with FlowJo software (Tree Star).
Immunoassays for human CTLA-4 and sCTLA-4
Human pan-CTLA-4 immunoassay: 96 well EIA/RIA flat bottom plates (Corning Costar) were coated with 100 μl of either anti-CD152 BN13 mAb or mouse IgG2aκ (clone G155-178, BD Pharmingen) isotype control diluted at 2 μg/ml in coating buffer (0.1 M sodium phosphate, pH 9). After overnight incubation at 4°C, plates were washed with PBS-T (0.05% Tween-20 in PBS) and 100 μl of sample diluted in DMEM/10% FBS/0.05% Tween-20 were added to each well (Tween-20 is added to prevent non-specific binding throughout the assay following the coating step). Following overnight incubation at 4°C and plate washing with PBS-T, detection was performed by addition of 100 μl/well of anti-CTLA-4 biotinylated mAb clone 14D3 (eBioscience) at 2 μg/ml in PBS-T for 1 hour at 4°C. Wells were washed with PBS-T and the bound biotinylated protein was detected by incubation with 100 μl/well of 0.1 μl/ml europium-labelled streptavidin (PerkinElmer) for 1 h at 4°C followed by washes in PBS-T and addition of 100 μl/well of DELFIA Enhancement Solution (PerkinElmer). Measurements were performed with a time-resolved Victor × reader (PerkinElmer). Each assay point was performed in duplicate. A standard curve was generated with the use of serial dilutions of a commercially available human CTLA-4/Fc fusion protein (Chimerigen Laboratories). sCTLA-4 concentrations in HeLa supernatants were estimated in this assay format considering a molar equivalent of one 90 kDa dimeric CTLA-4/Fc with two sCTLA-4 monomers each with a predicted molecular mass of 15.4 kDa.
Human sCTLA-4 immunoassay: 96 well plates were coated with BN13 or isotype control as described above for the human CTLA-4 assay and 180 μl of sample diluted in DMEM/10% FBS/0.05% Tween-20 was added to each well. After overnight incubation at 4°C and without washing, 20 μl/well of 0.1 μg/ml 4B8 diluted in DMEM/10% FBS/0.05% Tween-20 was added to each sample. Omitting the wash step that would normally be performed in most binding protocols increased the sensitivity of the assay approximately 2-fold. Following overnight incubation at 4°C, wells were washed with PBS-T and 100 μl/well of rat anti-mouse IgG2b biotin mAb (clone RMG2b-1, BioLegend) at 200 ng/ml in PBS-T was added. The plate was incubated 1 h on ice. Detection of biotinylated protein was carried out as described for the human CTLA-4 assay.
Statistical test
Comparisons of means between two groups were performed using the Mann-Whitney U-test.
Results
Characterization of anti-human sCTLA-4 antibodies
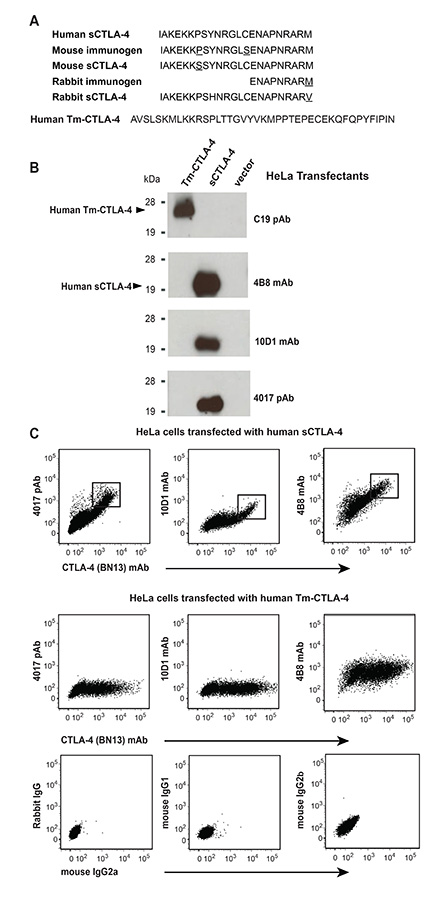
A polyclonal antibody, termed 4017, was raised in rabbit against a synthetic peptide corresponding to the final 9 C-terminal amino acid residues (ENAPNRARM) at position 166-174 of human sCTLA-4 and two monoclonal antibodies, 10D1 and 4B8, were raised in mouse against the 23 amino acids unique to sCTLA-4 (Fig. 1A). Their specific binding to sCTLA-4 was validated by Western blot (Fig. 1B) and flow cytometric (Fig. 1C) analyses using HeLa cells expressing recombinant sCTLA-4 and Tm-CTLA-4 proteins. In both assays, all three antibodies 4017, 4B8 and 10D1 bound to human sCTLA-4 but not to human Tm-CTLA-4 which has a different amino acid sequence at the C terminal region of the protein (Fig. 1A). Production of Tm-CTLA-4 by the transfected HeLa cells was confirmed using a commercially available polyclonal antibody (C19) generated by immunizing goats with the C-terminal amino acid sequence unique to the transmembrane isoform (Fig. 1B). As expected, C19 did not bind to recombinant human sCTLA-4. One clone, BN13, that recognizes an epitope in the CD80/CD86-binding domain common to sCTLA-4 and Tm-CTLA-4 can be used to detect -the intracellular expression levels of both recombinant sCTLA-4 and Tm-CTLA-4 in transfected HeLa cells by flow cytometry (Fig. 1C). All three sCTLA-4 specific antibodies co-stained along with BN13 the transfected HeLa cells expressing sCTLA-4 but not the Tm-CTLA-4 transfectants.
Figure 1.
Development of antibodies specific for the soluble CTLA-4 isoform. (A) Human (NP_001032720.1), rabbit and mouse (ENSMUSP00000095327) amino acid sequences at the C terminal region of sCTLA-4 are aligned with the synthetic peptides used for immunization of rabbits (P1_rabbit) and mice (P2_mouse). The cytoplasmic tail of TM-CTLA-4 is shown for comparison at the bottom of the panel (P16410, UniProt). Mouse and human nucleotide sequences encoding sCTLA-4 have been confirmed in our laboratory by sequencing. Rabbit amino acid sequence was determined from the deposited Tm-CTLA-4 nucleotide sequence (CTLA4_rabbit ENSOCUG00000017274) after alignment with human sCTLA-4 nucleotide sequence (NM_001037631.2). The 9 amino acid peptide used to immunize rabbits differs at a single residue from the rabbit sequence, a methionine for valine substitution at position 174 of rabbit sCTLA-4. The 23 amino acid synthetic peptide having the human sequence used to immunize mice differs at position 158 from the endogenous mouse sequence, a proline replaces serine. A serine for cysteine substitution in the 23 amino acid peptide was made at the residue corresponding to position 165 of the mature sCTLA-4 protein to prevent the formation of disulphide bonds in the peptide preparation and the peptide-KLH conjugate used for immunization. (B) 4B8 mAb, 10D1 mAb and 4017 polyclonal Ab validation by Western blot under reducing conditions on detergent lysates of HeLa cells expressing human recombinant Tm-CTLA-4, sCTLA-4 and vector only. Specific detection of Tm-CTLA-4 is performed with CTLA-4 (C19) polyclonal Ab. (C) sCTLA-4 antibody specificity was confirmed by flow cytometry using HeLa cells transfected with sCTLA-4 (top row) or Tm-CTLA-4 (middle row). As a control, HeLa cells transfected with Tm-CTLA-4 were stained with isotype-matched control antibodies (bottom row); similar results were obtained using HeLa cells transfected with sCTLA-4 (not shown). All experiments are representative of at least three independent observations.
10D1 mAb and 4017 polyclonal Ab specific for human sCTLA-4 bind mouse sCTLA-4
Human, rabbit and mouse sCTLA-4 C-terminal regions share 95% amino acid sequence identity. However, rabbit and mouse sCTLA-4 molecules differ from the human sequence at distinct residues (Fig. 1A) raising the possibility that the anti-human sCTLA-4 antibodies we have generated may in these two species recognize distinct epitopes on sCTLA-4. Data consistent with this hypothesis were obtained when we tested the two mAbs 4B8 and 10D1 and the polyclonal Ab 4017 on mouse sCTLA-4 recombinant protein by Western blot (Supplemental Fig. 1). Since human and mouse sCTLA-4 molecules share a methionine at the final residue of sCTLA-4 but differ from the rabbit sequence at the final residue of sCTLA-4, it was not surprising that we observed binding to mouse sCTLA-4 recombinant protein by the rabbit polyclonal anti-human sCTLA-4 antibodies (Supplemental Fig. 1A, top panel). The immunizing peptide for the rabbits contained only the final 9 amino acids of the sCTLA-4 protein; therefore, it is highly likely that the binding of the rabbit polyclonal Ab is focused on the terminal methionine residue. The expected lack of cross-reactivity to mouse sCTLA-4 of a mouse mAb generated by immunization with a peptide of human sCTLA-4 was observed with the 4B8 mAb (Supplemental Fig. 1A, lower panel) indicating that 4B8 binding most likely requires the human sequence-specific proline residue at position 158 instead of the mouse serine residue (Fig. 1A). Unexpectedly, the 10D1 anti-human sCTLA-4 mAb did bind to mouse sCTLA-4 (Supplemental Fig. 1A, middle panel) indicating that the human-specific proline residue is not required for binding by the 10D1 mAb and that the epitopes in the C terminal region recognized by the two anti-human sCTLA-4 mAb are not identical. As predicted, no binding of anti-human sCTLA-4 Ab to recombinant mouse Tm-CTLA-4 was observed (Supplemental Fig. 1A, right lanes).
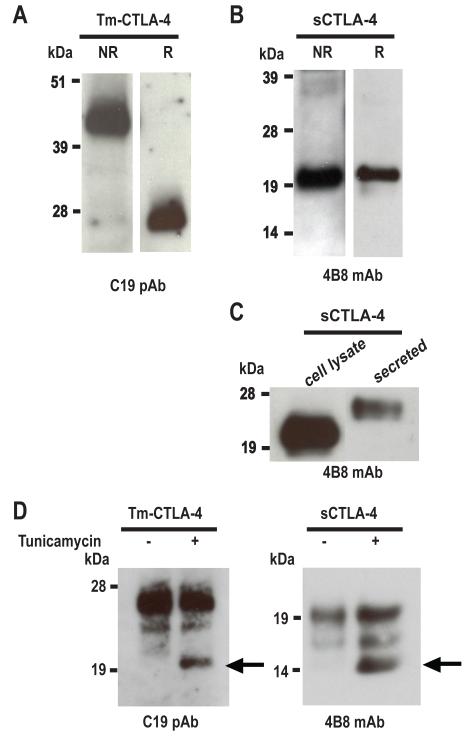
Human and mouse sCTLA-4 isoforms are expressed as glycosylated monomers
Tm-CTLA-4 covalent homodimerisation, required for its high avidity binding to CD80/CD86 ligands, is mediated by a cysteine at position 122 (9). As expected, under non-reducing conditions, recombinant Tm-CTLA-4 present in detergent lysates of transfected HeLa cells migrated as a dimer of ~42-45 kDa and under reducing conditions as a monomer of ~26-28 kDa (Fig. 2A). The soluble isoform, as a consequence of exon 3 skipping, lacks this cysteine residue predicting that the protein is expressed as a monomer. Indeed, Western blot analysis under both non-reducing and reducing conditions of detergent lysates from HeLa cells transfected with human sCTLA-4 showed a single immunoreactive species corresponding to the monomeric protein with an apparent molecular mass of ~20-22 kDa (Fig. 2B). Furthermore, sCTLA-4 was present in HeLa cell culture medium though with a higher molecular mass (~24-26 kDa) than that observed for the cell-associated protein suggesting that once the sCTLA-4 is fully glycosylated it is secreted by the transfected cells (Fig. 2C). Human Tm-CTLA-4 and sCTLA-4 monomers have predicted molecular masses based on their unmodified full-length amino acid sequences of 20.6 kDa and 15.4 kDa, respectively, which are lower than the apparent molecular mass observed by Western blot analysis. The extracellular regions of both Tm-CTLA-4 and sCTLA-4 contain, at positions 113 and 145, two potential sites for N-linked glycosylation. To investigate whether the observed shift in molecular mass is the consequence of post-translational modification, HeLa transfectants expressing sCTLA-4 and Tm-CTLA-4 recombinant proteins were incubated with tunicamycin, an inhibitor of N-glycosylation, followed by Western blot analysis of cell lysates. Consistent with the presence of N-linked glycosylation sites on both CTLA-4 isoforms, the addition of tunicamycin revealed novel immunoreactive species in the lysates from HeLa cells expressing either isoform (Fig. 2D). The migration positions of the tunicamycin-dependent protein bands for both isoforms that presumably lack the addition of any carbohydrate moieties were in agreement with their predicted apparent molecular masses (Fig. 2D).
Figure 2.
sCTLA-4 is secreted and expressed as a glycosylated monomer. (A) Human Tm-CTLA-4 protein is detected as a dimer under non-reducing conditions (NR) and as a monomer under reducing conditions (R) in lysates from HeLa cells transfected with human Tm-CTLA-4 cDNA. (B) Lysates from HeLa cells transfected with human sCTLA-4 cDNA contain sCTLA-4 protein that migrates as a monomer in both non-reducing and reducing conditions. (C) Under reducing conditions, sCTLA-4 protein secreted into the culture medium of HeLa cells transfected with sCTLA-4 cDNA migrates more slowly than sCTLA-4 present in cell lysates. (D) N-glycan addition contributes to the molecular masses of Tm-CTLA-4 and sCTLA-4. Following culture with or without tunicamycin, detergent lysates from HeLa cells transfected with Tm-CTLA-4 or sCTLA were analyzed by Western blot under reducing conditions using C19 polyclonal Ab or 4B8 mAb, respectively. Arrows indicate the protein species lacking N-linked glycans. All experiments are representative of at least three independent observations.
As demonstrated by Western blot analysis and similar to its human counterparts, mouse sCTLA-4 migrates as a monomer and mouse Tm-CTLA-4 migrates as a dimer (Supplemental Fig. 1B). Detergent lysates from HeLa cells transfected with mouse sCTLA-4 contained immunoreactive species with an apparent molecular mass of ~24-26 kDa (Supplemental Fig. 1B, 1C) and similar to the observations made with cells expressing human sCTLA-4, mouse sCTLA-4 secreted from transfected HeLa cells migrated as a larger protein species of ~28 kDa (Supplemental Fig. 1C). Mouse Tm-CTLA-4 is expressed as a dimer of ~48-50 kDa consisting of two monomeric subunits of ~28-30 kDa (Supplemental Fig. 1B). Mouse Tm-CTLA-4 and sCTLA-4 monomers have predicted molecular masses of 20.9 kDa and 15.4 kDa, respectively. However, by Western blot analysis we found that both mouse recombinant proteins migrated not only at a higher molecular mass than predicted from their amino acid sequence but also higher than that of the corresponding human isoforms (Supplemental Fig. 1C and compare Supplemental Figs. 1B and 1D with Fig. 2A, 2B and 2D). These apparent mass differences were postulated to be the consequence of increased post-translational N-glycosylation for the mouse proteins as compared to the human isoforms. Indeed, tunicamycin treatment of HeLa cells transfected with mouse Tm-CTLA-4 and sCTLA-4 yielded products that migrated at the expected molecular masses (Supplemental Fig. 1D).
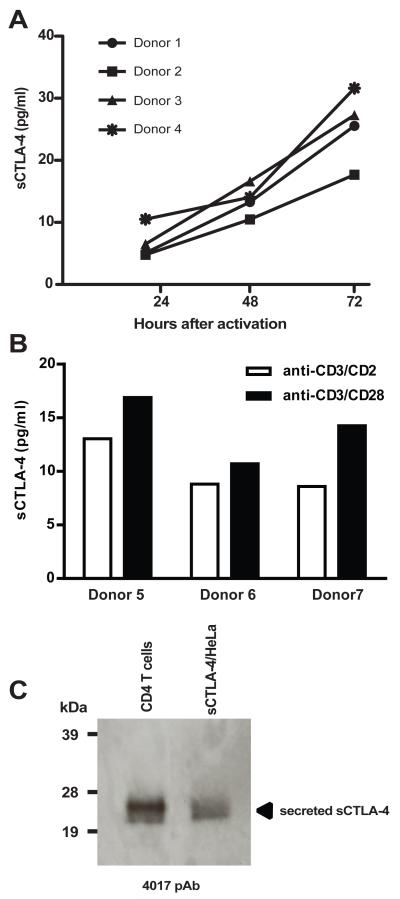
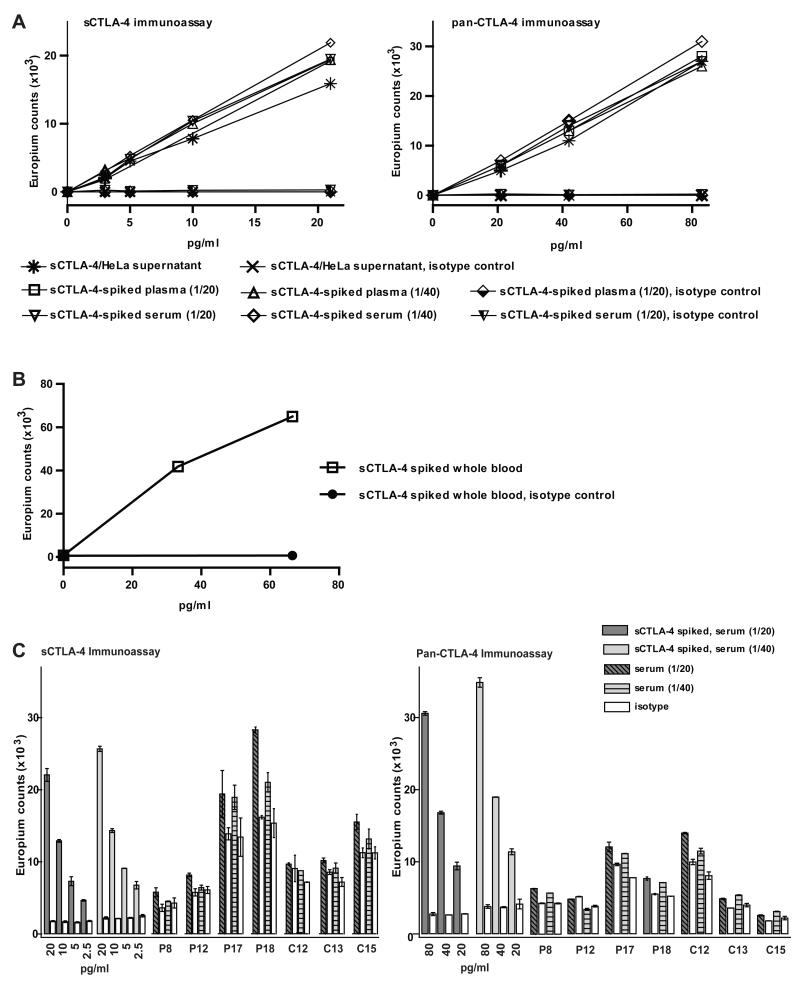
In vitro activated human CD4+ T cells secrete sCTLA-4
To optimize our ability to quantify the production of sCTLA-4 from human cells, we tested a number of potential binding assay formats utilizing the mAbs specific for sCTLA-4 as capture and detection reagents together with various mAbs binding the sCTLA-4 isoform via its N-terminal CD80/CD86-binding domain. The most sensitive format of the assay identified uses N-terminal-specific anti-CTLA-4 mAb BN13 as the capture antibody and sCTLA-4-specific 4B8 mAb as the detection antibody; the lower limit of detection of recombinant sCTLA-4 with this assay is approximately 2 pg/ml (Supplemental Fig. 2A, right panel). Recombinant sCTLA-4 secreted from transfected HeLa cells is used to generate the standard curve for quantifying the levels of sCTLA-4 in serum, cell culture supernatants and cell lysates. The quantification of recombinant sCTLA-4 was derived from its activity in a pan-CTLA-4 assay based on two mAbs both recognising the N-terminal region of CTLA-4, which is present in both sCTLA-4 and Tm-CTLA-4, using a commercially available fusion protein between CTLA-4 and the Fc portion of human IgG1 (CTLA-4/Fc) as a standard (Supplemental Fig. 2B). The pan-CTLA-4 assay, with a lower limit of sensitivity of approximately 20 pg/ml, is 10-fold less sensitive than the sCTLA-4-specific assay in detecting sCTLA-4 (Supplemental Fig. 2C, right panel). Having validated the specificity of the sCTLA-4 antibodies and developed a sensitive binding assay we then investigated if sCTLA-4 protein is produced by human CD4+ T cells.
CD4+ T cells isolated from whole blood of four healthy donors were analyzed for sCTLA-4 and Tm-CTLA-4 proteins ex vivo and after 24, 48 and 72 hours of activation with anti-CD3/CD2 antibodies. Cell lysates and culture supernatants were assessed using the specific and highly sensitive sCTLA-4 mAb-based assay described above. sCTLA-4 was detected in CD4+ T cell supernatants after activation in a time-dependent manner ranging between 17-32 pg/ml after 72 hours in culture (Fig. 3A). Similar levels of sCTLA-4 were detected in the supernatants of CD4+ T cells purified from three healthy donors comparing two activation protocols: anti-CD3/CD28 microbeads and anti-CD3/CD2 mAbs (Fig. 3B). Likely as a consequence of the low expression levels and rapid secretion of the mature protein we did not detect sCTLA-4 in detergent lysates from CD4+ T cells before or after activation by immunoassay or Western blot analysis. Similarly sCTLA-4 was not detected in activated CD4+ T cells by flow cytometry using any of the three sCTLA-4-specific antibodies (not shown).
Figure 3.
(A) In vitro activation of CD4+ T cells induces secretion of sCTLA-4. CD4+ T cells of four healthy donors were stimulated in vitro with anti-CD3/CD2 mAb and culture supernatants harvested at the indicated time points. CD4+ T cells (3 × 106 cells/ml) from the four donors were cultured on separate days. Isotype controls were negative for all samples (not shown). (B) Secretion of sCTLA-4 by CD4+ T cells (1 × 106 cells/ml) of three independent donors stimulated for 72 hours in vitro with either anti-CD3/CD2 mAb or anti-CD3/CD28 microbeads. (C) Detection of sCTLA-4 following immunoprecipitation and Western blot analysis. sCTLA-4 protein in culture supernatants from activated CD4+ T cells and from HeLa cells transfected with sCTLA-4 were immunoprecipitated using 4B8 mAb followed by 4017 polyclonal Ab immunoblotting. No sCTLA-4 was immunoprecipitated with the corresponding IgG2b isotype control (not shown). Western blot gel is representative of more than three independent experiments.
sCTLA-4 protein in culture supernatants from activated CD4+ T cells detected by immunoassay could not be directly detected by Western blot analysis as a result of the detection limit of approximately 240 pg/ml, compared to the 2 pg/ml detection limit of the sCTLA-4 immunoassay (Supplemental Fig. 2D, 2A). Therefore, to provide further evidence that sCTLA-4 is secreted by CD4+ T cells, immunoprecipitation with anti-sCTLA-4 mAb followed by Western blot analysis was performed using culture supernatants from T cells activated for 72 hours (Fig. 3C). Importantly, T cell derived sCTLA-4 migrated equivalently to recombinant sCTLA-4 secreted from transfected HeLa cells indicating that sCTLA-4 secreted by primary T cells is glycosylated.
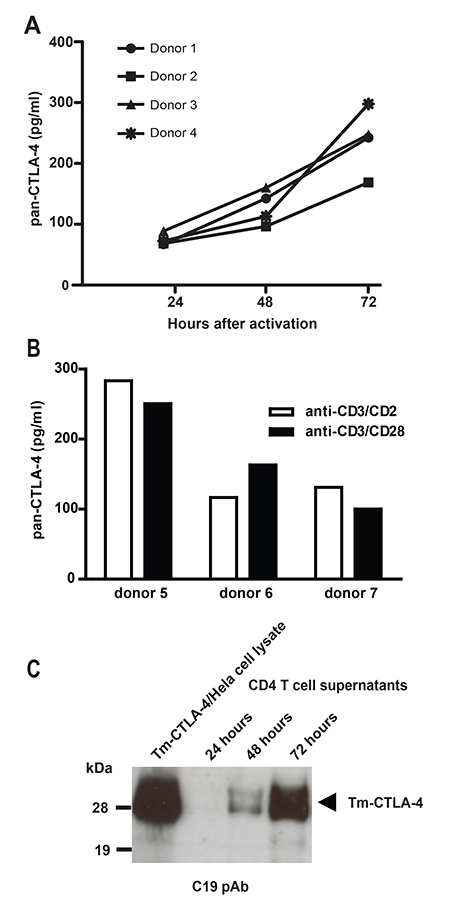
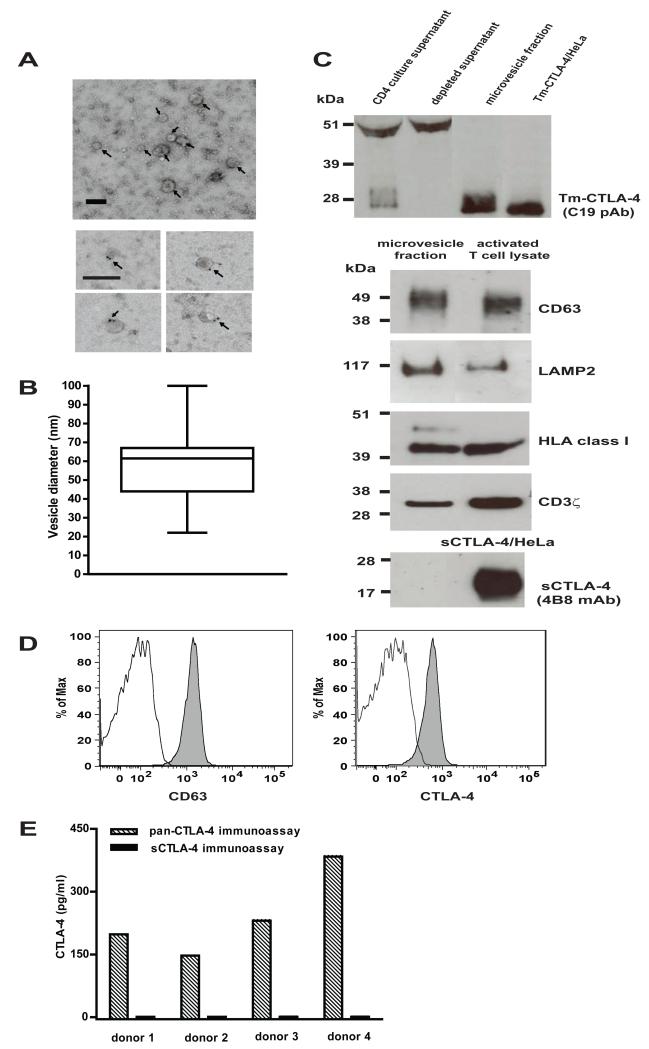
Release of Tm-CTLA-4 following CD4+ T cell activation is associated with microvesicles
Remarkably, we observed that in the pan-CTLA-4 immunoassay (Fig. 4A, 4B), where both CTLA-4 isoforms can be detected, the CTLA-4 concentration in CD4+ T cell supernatant samples was ~10-fold higher than that observed using the sCTLA-4 immunoassay with either anti-CD3/CD2 mAb or anti-CD3/CD28 microbeads (compare Fig. 4A, 4B and Fig. 3A, 3B). CD4+ T cell supernatants were therefore analyzed by Western blot for the presence of Tm-CTLA-4. A band corresponding to Tm-CTLA-4 was detected in 48 and 72 hours activated T cell supernatants (Fig. 4C). Since the immunoblot was probed with an antibody against the intracellular domain of Tm-CTLA-4 and the apparent molecular mass of the band corresponded to the entire Tm-CTLA-4 protein, proteolytic cleavage of the transmembrane receptor from the T cell surface does not account for the release of Tm-CTLA-4. We therefore tested the hypothesis that Tm-CTLA-4 is expressed in the microvesicles previously described to be secreted from activated T cells (30). T cell supernatants were sequentially ultracentrifuged to isolate the microvesicle-containing fraction. Electron microscopic analysis of the pellet showed membrane encapsulated vesicles with a size ranging between 20 and 100 nm with cup–shaped morphology similar to that reported for cell-derived vesicles of endocytic origin termed exosomes (Fig. 5A, 5B). Moreover, these microvesicles express CD63, a tetraspanin shown to be enriched in exosomes (Fig. 5A, bottom panel) (31). Western blot analysis further showed that Tm-CTLA-4, CD63, lysosomal-associated membrane protein 2 (LAMP2; another established constituent of exosomes), HLA class I and T cell-type specific protein CD3ζ were detected in the vesicle-containing fraction purified from supernatants of activated CD4+ T cells (Fig. 5C) (27, 31). No sCTLA-4 was observed in the ultracentrifuged pellet (Fig. 5C, lowest panel). We confirmed expression of surface CD63 and CTLA-4 on CD4+ T cell-derived exosomal-like vesicles by flow cytometry (Fig. 5D). Furthermore, exosome enriched fractions isolated from culture supernatants of 72 hour in vitro activated CD4+ T cells from four healthy donors were analyzed using the two CTLA-4-based assays confirming the presence of mvCTLA-4 but not sCTLA-4 (Fig. 5E).
Figure 4.
Immunoassay and Western blot analysis of Tm-CTLA-4 present in culture supernatants from activated CD4+ T cells. (A) Culture supernatants from 3 × 106 cells/ml CD4+ T cells activated with anti-CD3/CD2 mAbs in vitro from four donors cultured on different days were harvested at the indicated time points and analyzed using the pan-CTLA-4 immunoassay. (B) Analyses of supernatants of CD4+ T cells (1 × 106 cells/ml) of three donors cultured on different days stimulated in vitro for 72 hours with either anti-CD3/CD2 mAbs or anti-CD3/CD28 microbeads. (C) Release of Tm-CTLA-4 in a time-dependent manner in culture supernatants of activated CD4+ T cells was confirmed by Western blot analysis using Tm-CTLA-4 C-terminus C19 polyclonal Ab. Western blot gel is representative of at least four independent experiments.
Figure 5.
Characterization of exosome-like vesicles secreted by activated CD4+ T cells. (A) Top panel: representative electron micrographs of microvesicles, as indicated by arrows, showing vesicles with low electron density as well as characteristic shape and size of exosomes (scale bar; 100 nm). Bottom panel: anti-CD63 immunogold labelling of CD4+ T cells-derived microvesicles. Arrows indicate immunogold-positive labelling (scale bar; 100 nm). (B) The size distribution of microvesicles is plotted as a box plot; the box span the 25thand 75th percentile, the horizontal line represents the median diameter and the whiskers mark the extremes of the distribution ( n = 24 microvesicles). (C) Top panel: Western blot analysis of activated CD4+ T cell supernatant before and after ultracentrifugation, microvesicle fraction isolated from the T cell supernatant and detergent lysates from Tm-CTLA-4/HeLa cells with anti-Tm-CTLA-4 C19 polyclonal Ab; bottom panels: Western blot analysis of microvesicle fraction isolated from the T cell supernatant with anti-CD63, anti-LAMP2, anti-HLA class I, anti-CD3ξ and anti-sCTLA-4 antibodies. CD4+ T cell or sCTLA-4/HeLa detergent lysates were used as positive controls. (D) Microvesicle fraction derived from activated CD4+ T cells were coated onto latex beads, surface stained with anti-CD63 and anti-CTLA-4 (BN13) (filled grey histogram) antibodies or the corresponding isotype controls (open histogram) and analyzed by flow cytometry. E) sCTLA-4 is not expressed in exosomal-like vesicles. The microvesicle fractions were isolated from supernatants of activated CD4+ T cells of 4 donors after 3 days of stimulation with anti-CD3/CD2 mAb and then tested in the pan-CTLA-4 and s-CTLA-4 immunoassays. All experiments are representative of at least three independent observations.
Analysis of circulating sCTLA-4 in human serum
Previous studies, using antibody-based assays in which both capture and detection antibodies were specific for the N-terminal region of CTLA-4, reported circulating levels of sCTLA-4 in serum from patients with autoimmune diseases in the 2-97 ng/ml range (18-25). In order to investigate whether sCTLA-4 could be detected in serum or plasma samples using a sCTLA-4-specific immunoassay, we first determined plasma and serum tolerability in both assay formats (sCTLA-4 specific and pan-CTLA-4) and found that a 1/20 dilution was the highest concentration of both biological fluids that could be tested without observing greater than 20% inhibition of samples spikes with sCTLA-4 protein (data not shown). Thus, based on the spike and recovery analysis in 1/20 dilutions of serum and plasma the lower limit of detection of recombinant sCTLA-4 in neat serum and plasma is 40 pg/ml in the sCTLA-4 specific assay and 400 pg/ml in the pan-CTLA-4 assay. Spike and recovery experiments were also performed as represented in Fig. 6A using 1/20 and 1/40 sera and plasma dilutions spiked with 2-fold serial dilutions of recombinant sCTLA-4. In both assays we obtained good recovery and dilutional linearity (all r2 > 0.98) of spiked sCTLA-4 with sensitivity and detection limits similar to those measured in the culture medium of sCTLA-4/HeLa transfectants (Fig 6A and Supplemental Fig. 2A, 2C, right panels). Good spike recovery was also observed in plasma samples derived from heparinized whole human blood that had been incubated with recombinant sCTLA-4 at 37°C for 2 hours thus providing evidence that sCTLA-4 is likely to be stable in the circulation in vivo (Fig. 6B).
Figure 6.
Detection of sCTLA-4 protein in plasma and serum samples. A) Analysis by sCTLA-4 (left panel) and pan-CTLA-4 (right panel) immunoassays of 2-fold serial dilutions of recombinant sCTLA-4 spiked into 1/20 and 1/40 dilutions of plasma and serum samples. An isotype-matched mouse IgG2a aκ capture antibody is used as a negative control. Serial dilutions of culture supernatant of sCTLA-4 HeLa cell transfectants in standard assay buffer were included in each assay. B) Detection of recombinant sCTLA-4 spiked into human whole blood. Mouse IgG2a aκ isotype-matched antibody used as capturing reagent served as a negative control. C) Analysis of sCTLA-4 in serum samples from autoimmune patients and controls using the sCTLA-4 immunoassay (left panel) and the pan-CTLA-4 immunoassay (right panel). Serial dilutions of recombinant sCTLA-4 were spiked into serum diluted 1:20 (dark grey columns) and 1:40 (light grey columns) and representative examples from a total of 61 donors are shown (see Supplemental Fig. 3 for results from all donors): 4 GD patients and 3 age- and sex-matched, healthy volunteers, sera diluted 1/20 (dark shaded columns) and 1/40 (light shaded columns). For all samples, including the spiked serum samples, the mouse IgG2a κ isotype control is shown (open columns). Columns, mean of duplicate measurements; bars, ± SD.
We then examined serum at 1/20 and 1/40 dilutions from individuals affected with T1D and GD compared to age- and sex-matched healthy controls using the sCTLA-4 as well as the pan-CTLA-4 assay (Fig. 6C for representative data, Supplemental Fig. 3A-D shows raw data for all samples). In both assay formats the binding determined with the anti-CTLA-4 capture antibody was compared with an isotype-matched control to detect the presence of heterophilic antibodies or other serum components that bind mouse immunoglobulin molecules; such molecules interfere with the interpretation of immunoassays (32, 33) and are present in varying levels in human plasma and serum. The definition for positive samples was a signal above the isotype control background that proportionally decreased as a consequence of serum dilution as exemplified by the spiked serum samples (1/20 and 1/40 dilutions) on the left hand portion of each panel of Fig. 6C where the specific signal decreased with dilution whereas the signal observed from the isotype control remained the same. In Fig. 6C seven representative samples from the GD patients and matched healthy control cohorts (Supplemental Fig. 3A, 3B) are shown for both assays at 1/20 and 1/40 dilutions. In all the patient and control serum samples, except for GD P18, similar signal intensities were obtained using 20-fold and 40-fold serum dilutions in both the specific and isotype control assay in both formats (Fig. 6C and Supplemental Fig. 3). Interestingly, in the sCTLA-4 immunoassay, GD P18, was the only sample for which we observed approximately 2-fold signal reduction at the 1/40 serum dilution compared with the 1/20 serum dilution whereas the read-out from the isotype control remained similar for both dilutions (Fig 6C, left panel). The concentration of sCTLA-4 in GD P18 serum, determined using the sCTLA-4 immunoassay, is 260 pg/ml and is below the limit of detection of the N-terminus pan-CTLA-4 immunoassay (Fig 6C, right panel). Thus, the concentration of circulating sCTLA-4 we have detected in this single patient is at least 10-fold lower than the 2000-97000 pg/ml sCTLA-4 that has been reported for autoimmune patients in previous studies (18-25). Overall, our results indicate that sCTLA-4 does not represent a significant serum protein component in autoimmune diseases.
On a technical note, the result of all sera tested in both assay formats (Supplemental Fig. 3) reinforces previous observations that heterophilic antibodies (32-34) are present in variable levels in human serum and can be a confounder of antibody-based immunoassays. In Supplemental Fig. 3 we have organised the results in the CTLA-4 portion of the assay from lowest to highest in each cohort to demonstrate that the variation of binding by the samples in the specific assay is generally mimicked by the isotype binding thus suggesting that a “background” anti-mouse IgG reactivity is being observed and that this varies between people. It is notable that the pan-CTLA-4 immunoassay has in general less background than the sCTLA-4 immunoassay. Possibly this is the consequence of the different anti-CTLA-4 detection reagents; the pan-CTLA-4 detection reagent is directly biotinylated whereas the anti-sCTLA-4 reagent is detected by a secondary biotinylated anti-mouse IgG2b mAb.
Tm-CTLA-4 associated with microvesicles is not detected in human serum
mvCTLA-4 was not detected at levels above 400 pg/ml in serum of T1D and GD patients or matched healthy volunteers using the pan-CTLA-4 assay (Fig. 6C, right panel and Supplemental Fig. 3B, 3C). We further investigated if isolation of microvesicles from serum could increase the sensitivity of Tm-CTLA-4 detection. Microvesicles prepared from serial ultracentrifugation of sera from T1D and healthy volunteers were analyzed by Western blot and found to express CD63 and CD3ζ (Supplemental Fig. 4). As expected due to the diverse tissue sources of microvesicles in the blood (27), CD63, a constitutive marker of all exosomes (31), was significantly more abundant than the T cell-specific CD3ζ molecule as compared with the microvesicle-like exosomes that were isolated from activated CD4+ T cells (Supplemental Fig. 4, Fig. 5C). mvCTLA-4 was not found in the serum-derived microvesicles by Western blot analysis (not shown), confirming the results of the pan-CTLA-4 immunoassay.
Discussion
Biochemical and immunological characterization of the soluble isoform of CTLA-4 has been hindered by the lack of specific high affinity reagents that binds to this isoform. In this study we have developed and characterized several sCTLA-4-specific reagents, including two monoclonal antibodies, and use them to measure sCTLA-4 levels present in vivo and from cultured primary, activated T cells. We have shown that using a sCTLA-4 assay with a 2 pg/ml sensitivity in tissue culture supernatant samples, CD4+ T cells upon stimulation secrete 17-32 pg/ml sCTLA-4. Nonetheless, with a detection limit of 40 pg/ml in serum and plasma samples, sCTLA-4 was detected in only one out of 32 serum samples from autoimmune disease patients and none of the samples from 29 healthy controls.
Our results are in contrast with previous studies reporting levels of circulating sCTLA-4 in the 2-97 ng/ml range in a large proportion of patients with various autoimmune diseases (18-25). The immunoassays used in these previous studies relied on antibodies that recognize the IgV-like extracellular region of CTLA-4 (35), similar to the pan-CTLA-4 immunoassay employed in the current study, in only two is an isotype control used to adjust for individual variation in nonspecific binding and none of the studies reported linearity of the binding assay utilized at the concentrations of serum tested by spiking with known concentrations of sCTLA-4 (18, 25). Recently, Tector and Oaks et al. (26) showed that CTLA-4 positive plasma of patients with myasthenia gravis after purification and enrichment by an N-terminus CTLA-4 mAb column specifically bound anti-CTLA-4 antibodies and the CTLA-4 ligands CD80/CD86 fusion proteins. However, the eluted plasma material was also shown to be captured by a protein A column unlike recombinant sCTLA-4 which was detected in the flow-through. This result indicates that the immunoreactive material isolated from the plasma, which had been captured by anti-CTLA-4 Abs and the CD80/CD86 molecules, both consisting of two extracellular Ig-like domains (36, 37) and fused to the Fc region of the mouse Ig, was not sCTLA-4 but a material that possessed immunoglobulin-like properties. Together with these recent findings from Tector and Oaks et al. (26), our current results suggest that a reassessment of what are termed circulating levels of the sCTLA-4 isoform should be made and that the molecular basis of the CTLA-4-like immunoreactive material present in the circulation of some autoimmune patients and healthy controls warrants further study. However, even though circulating levels of the sCTLA-4 isoform are generally below the limit of sensitivity of our sCTLA-4-specific assay (40 pg/ml), this does not rule out the possibility that secreted sCTLA-4 plays a functional role locally in tissues where activated T cells and APCs are interacting.
As predicted by its lack of the cysteine residue at position 122 (C122), which mediates the covalent homodimerization of CTLA-4 (38), our data indicate that recombinant sCTLA-4 from HeLa transfected cells migrates as a monomer under non-reducing conditions. However, it has been reported that a mutation, which abrogates intermolecular disulfide bonding at C122, reduces but does not inhibit dimerization of CTLA-4. N-glycosylation at the Asn113 and Asn145 residues of the extracellular domain appear to promote the cys-independent dimerization of CTLA-4 (9). By treating sCTLA-4/HeLa transfectants with tunicamycin, an inhibitor of N-glycan processing, we have demonstrated that sCTLA-4 is N-glycosylated and therefore the potential for cys-independent homodimer formation exists for secreted sCTLA-4. It is also possible that functional dimerization occurs after binding to CD80/CD86 ligands at the T cell-APC interface (9). Notably, we have also shown that sCTLA-4 secreted by primary human T cells has the same apparent molecular mass as fully N-glycosylated recombinant sCTLA-4. Furthermore, our data show a positive correlation between the low expression levels of sCTLA-4 protein detected in human T cells and the reported moderate increase of sCTLA-4 mRNA following in vitro activation (7, 11).
It is noteworthy that two of the anti-human sCTLA-4-specific antibodies, 10D1 mAb and 4017 pAb, recognize mouse recombinant sCTLA-4. We have shown in transfected HeLa cells that like human sCTLA-4, mouse sCTLA-4 is secreted as an N-glycosylated monomer. Of interest, given their higher molecular masses, both human and mouse sCTLA-4 secreted into the culture media might represent the fully glycosylated form compared to the protein detected in the cell lysates. Furthermore, variation in N-glycosylation based on protein structure probably accounts for the molecular mass differences of the mouse Tm-CTLA-4 and sCTLA-4 proteins relative to their human counterparts.
The biological relevance of our observations requires further investigation. Despite being expressed as a monomer, recombinant sCTLA-4 was reported to block T cell proliferation, an effect that could be dampened by the addition of anti-CTLA-4 antibodies (7). Recombinant sCTLA-4 was also able to inhibit the co-stimulatory signal of CHO cells expressing CD80 similarly to what was observed after addition of CTLA-4Ig (7). Soluble CTLA-4Ig has been shown to modulate the CD28/CD80-CD86 pathway and inhibit T cell activation (39-44); in clinical trials, formulations of CTLA-4Ig have proved to be effective in the treatment of autoimmune diseases and allograft rejection (45-51). Thus, sCTLA-4, in vivo, might modulate local T cell-APC interaction with a mode-of-action similar to the one observed for the CTLA-4Ig. Although, in vivo, the secretion of sCTLA-4 might represent a further mechanism to dampen an ongoing immune response, the release of this molecule might also be a distinctive feature of a specialised subset of T cells such as Tregs that constitutively express and require CTLA-4 for their suppressive activity (5, 6, 52).
Another major finding of our study is that microvesicles that express covalent homodimers of Tm-CTLA-4, that we have termed mvCTLA-4, are secreted in the culture supernatant of activated CD4+ T cells. The low electron density regular cup-shaped microvesicles isolated from the culture supernatants with a diameter between 20-100 nm and expressing CD63 and LAMP2 (28, 53) presented characteristics typical of exosomes, small membrane vesicles of endocytic origin which have been shown to carry a specific array of proteins, mRNA and miRNA (31, 54). Exosomes have been shown to be secreted by both innate and adaptive cells (30, 53, 55, 56) in various biological fluids such as blood, saliva, urine and breast milk (27, 57-59) where they appear to play an important role in intercellular communication and immunoregulation (30, 53, 55, 60). It has been reported that CD4+ T cells activated via the TCR secrete vesicles that exhibit characteristics and markers of exosomes and express T cell adhesion molecules, such as CD2 and CXCR4, and the TCR/CD3/ζ complex (30, 61). Others have shown that activated T cells release exosomes expressing apoptosis-inducing molecules such as FAS ligand and APO2 ligand (62). Exosomes from activated T cells have been shown to endow APCs with the capacity to stimulate or inhibit T cell responses (63, 64) or directly induce proliferation in autologous resting T cells accompanied by a change in the cytokine/chemokine profile (65). We speculate that the presence of Tm-CTLA-4 on microvesicles/exosomes might be responsible for a portion of the biologic functions ascribed in these published studies and we are currently investigating the ability of mvCTLA-4 to inhibit CD80/CD86-mediated costimulation.
Of note, mvCTLA-4 was not detected, using the pan CTLA-4 immunoassay, in human sera of GD and T1D patients or healthy controls, even after isolation of microvesicles. Nevertheless, we cannot exclude that the lack of detection of microvesicles carrying Tm-CTLA-4 was due to the large proportion of non-T cell-derived microvesicles in the serum samples and mv-CTLA-4 might be detectable in serum from humans having a high degree of cell activation such as in acute graft-versus-host disease.
We suggest that these two forms of CTLA-4, sCTLA-4 and mvCTLA-4, constitute novel mechanisms by which T cells can alter in the local milieu APC function via binding to CD80/CD86 ligands. Release of CTLA-4 soluble forms possibly by directional secretion as shown for IL-2 and IFNγ (66) from a T cell subset such as activated Tregs might modify expression of CD80 and CD86 on nearby APCs thereby influencing CD28 engagement (6, 67, 68), as well as inducing immunosuppression via, for example, an IDO-dependent pathway (69). In conclusion, our study provides novel evidence documenting the secretion of both sCTLA-4 and mv-CTLA-4 from human primary, activated T cells and prompts further investigation to gain insight into their functions.
Supplementary Material
Acknowledgements
We thank all donors from the National Institute for Health Research Cambridge BioResource for taking part in this study. We gratefully acknowledge the National Institute for Health Research Cambridge BioResource Scientific Advisory Board and Management Committee. We thank Kelly Beer, Tracy Cook, Susan Hall and Jamie Rice for sample collection and processing and Matthew Woodburn and Tony Attwood for contributing to sample management. We thank Dr Jeremy N. Skepper (Department of Physiology, Development and Neuroscience, University of Cambridge) for his expert help in electron microscopy. We thank Dr Jonathan S. Dodd, Dr Antony J. Cutler and Dr Yang D. Dai (Torrey Pines Institute for Molecular Studies) for their critical reading of the manuscript.
This work was supported by Wellcome Trust Grant 091157, JDRF International Grant 9-2011-253, the National Institute for Health Research Cambridge Biomedical Research Centre, the Juvenile Diabetes Research Foundation International, Centre for Diabetes—Genes, Autoimmunity, and Prevention Grant 4-2007-1003, and Award P01AI039671 (to L.S.W. and J.A.T.) from the National Institute of Allergy and Infectious Diseases (NIAID). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Allergy and Infectious Diseases or the National Institutes of Health. The Cambridge Institute for Medical Research is in receipt of Wellcome Trust Strategic Award 100140.
Abbreviations
- CTLA-4
cytotoxic T lymphocyte antigen 4
- GD
Graves’ disease
- KLH
keyhole limpet hemocyanin
- SNP
single nucleotide polymorphism
- T1D
type 1 diabetes
- Treg
regulatory T cell
Footnotes
Disclosures: The authors have no financial conflicts of interest.
References
- 1.Tivol EA, Borriello F, Schweitzer AN, Lynch WP, Bluestone JA, Sharpe AH. Loss of CTLA-4 leads to massive lymphoproliferation and fatal multiorgan tissue destruction, revealing a critical negative regulatory role of CTLA-4. Immunity. 1995;3:541–547. doi: 10.1016/1074-7613(95)90125-6. [DOI] [PubMed] [Google Scholar]
- 2.Walunas TL, Lenschow DJ, Bakker CY, Linsley PS, Freeman GJ, Green JM, Thompson CB, Bluestone JA. CTLA-4 can function as a negative regulator of T cell activation. Immunity. 1994;1:405–413. doi: 10.1016/1074-7613(94)90071-x. [DOI] [PubMed] [Google Scholar]
- 3.Waterhouse P, Penninger JM, Timms E, Wakeham A, Shahinian A, Lee KP, Thompson CB, Griesser H, Mak TW. Lymphoproliferative disorders with early lethality in mice deficient in Ctla-4. Science. 1995;270:985–988. doi: 10.1126/science.270.5238.985. [DOI] [PubMed] [Google Scholar]
- 4.Read S, Greenwald R, Izcue A, Robinson N, Mandelbrot D, Francisco L, Sharpe AH, Powrie F. Blockade of CTLA-4 on CD4+CD25+ regulatory T cells abrogates their function in vivo. J. Immunol. 2006;177:4376–4383. doi: 10.4049/jimmunol.177.7.4376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Read S, Malmstrom V, Powrie F. Cytotoxic T lymphocyte-associated antigen 4 plays an essential role in the function of CD25+CD4+ regulatory cells that control intestinal inflammation. J. Exp. Med. 2000;192:295–302. doi: 10.1084/jem.192.2.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wing K, Onishi Y, Prieto-Martin P, Yamaguchi T, Miyara M, Fehervari Z, Nomura T, Sakaguchi S. CTLA-4 control over Foxp3+ regulatory T cell function. Science. 2008;322:271–275. doi: 10.1126/science.1160062. [DOI] [PubMed] [Google Scholar]
- 7.Oaks MK, Hallett KM, Penwell RT, Stauber EC, Warren SJ, Tector AJ. A native soluble form of CTLA-4. Cell. Immunol. 2000;201:144–153. doi: 10.1006/cimm.2000.1649. [DOI] [PubMed] [Google Scholar]
- 8.Magistrelli G, Jeannin P, Herbault N, Benoit De Coignac A, Gauchat JF, Bonnefoy JY, Delneste Y. A soluble form of CTLA-4 generated by alternative splicing is expressed by nonstimulated human T cells. Eur. J. Immunol. 1999;29:3596–3602. doi: 10.1002/(SICI)1521-4141(199911)29:11<3596::AID-IMMU3596>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 9.Darlington PJ, Kirchhof MG, Criado G, Sondhi J, Madrenas J. Hierarchical regulation of CTLA-4 dimer-based lattice formation and its biological relevance for T cell inactivation. J. Immunol. 2005;175:996–1004. doi: 10.4049/jimmunol.175.2.996. [DOI] [PubMed] [Google Scholar]
- 10.Ueda H, Howson JM, Esposito L, Heward J, Snook H, Chamberlain G, Rainbow DB, Hunter KM, Smith AN, Di Genova G, Herr MH, Dahlman I, Payne F, Smyth D, Lowe C, Twells RC, Howlett S, Healy B, Nutland S, Rance HE, Everett V, Smink LJ, Lam AC, Cordell HJ, Walker NM, Bordin C, Hulme J, Motzo C, Cucca F, Hess JF, Metzker ML, Rogers J, Gregory S, Allahabadia A, Nithiyananthan R, Tuomilehto-Wolf E, Tuomilehto J, Bingley P, Gillespie KM, Undlien DE, Ronningen KS, Guja C, Ionescu-Tirgoviste C, Savage DA, Maxwell AP, Carson DJ, Patterson CC, Franklyn JA, Clayton DG, Peterson LB, Wicker LS, Todd JA, Gough SC. Association of the T-cell regulatory gene CTLA4 with susceptibility to autoimmune disease. Nature. 2003;423:506–511. doi: 10.1038/nature01621. [DOI] [PubMed] [Google Scholar]
- 11.Perez-Garcia A, Osca G, Bosch-Vizcaya A, Kelleher N, Santos NY, Rodriguez R, Gonzalez Y, Roncero JM, Coll R, Serrando M, Lloveras N, Tuset E, Gallardo D. Kinetics of the CTLA-4 isoforms expression after T-lymphocyte activation and role of the promoter polymorphisms on CTLA-4 gene transcription. Hum. Immunol. 2013;74:1219–1224. doi: 10.1016/j.humimm.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 12.Wicker LS, Chamberlain G, Hunter K, Rainbow D, Howlett S, Tiffen P, Clark J, Gonzalez-Munoz A, Cumiskey AM, Rosa RL, Howson JM, Smink LJ, Kingsnorth A, Lyons PA, Gregory S, Rogers J, Todd JA, Peterson LB. Fine mapping, gene content, comparative sequencing, and expression analyses support Ctla4 and Nramp1 as candidates for Idd5.1 and Idd5.2 in the nonobese diabetic mouse. J. Immunol. 2004;173:164–173. doi: 10.4049/jimmunol.173.1.164. [DOI] [PubMed] [Google Scholar]
- 13.Barrett JC, Clayton DG, Concannon P, Akolkar B, Cooper JD, Erlich HA, Julier C, Morahan G, Nerup J, Nierras C, Plagnol V, Pociot F, Schuilenburg H, Smyth DJ, Stevens H, Todd JA, Walker NM, Rich SS, C. Type 1 Diabetes Genetics Genome-wide association study and meta-analysis find that over 40 loci affect risk of type 1 diabetes. Nat. Genet. 2009;41:703–707. doi: 10.1038/ng.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Plant D, Flynn E, Mbarek H, Dieude P, Cornelis F, Arlestig L, Dahlqvist SR, Goulielmos G, Boumpas DT, Sidiropoulos P, Johansen JS, Ornbjerg LM, Hetland ML, Klareskog L, Filer A, Buckley CD, Raza K, Witte T, Schmidt RE, Worthington J. Investigation of potential non-HLA rheumatoid arthritis susceptibility loci in a European cohort increases the evidence for nine markers. Ann. Rheum. Dis. 2010;69:1548–1553. doi: 10.1136/ard.2009.121020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smyth DJ, Plagnol V, Walker NM, Cooper JD, Downes K, Yang JH, Howson JM, Stevens H, McManus R, Wijmenga C, Heap GA, Dubois PC, Clayton DG, Hunt KA, van Heel DA, Todd JA. Shared and distinct genetic variants in type 1 diabetes and celiac disease. N. Engl. J. Med. 2008;359:2767–2777. doi: 10.1056/NEJMoa0807917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stahl EA, Raychaudhuri S, Remmers EF, Xie G, Eyre S, Thomson BP, Li Y, Kurreeman FA, Zhernakova A, Hinks A, Guiducci C, Chen R, Alfredsson L, Amos CI, Ardlie KG, BIRAC Consortium. Barton A, Bowes J, Brouwer E, Burtt NP, Catanese JJ, Coblyn J, Coenen MJ, Costenbader KH, Criswell LA, Crusius JB, Cui J, de Bakker PI, De Jager PL, Ding B, Emery P, Flynn E, Harrison P, Hocking LJ, Huizinga TW, Kastner DL, Ke X, Lee AT, Liu X, Martin P, Morgan AW, Padyukov L, Posthumus MD, Radstake TR, Reid DM, Seielstad M, Seldin MF, Shadick NA, Steer S, Tak PP, Thomson W, van der Helm-van Mil AH, van der Horst-Bruinsma IE, van der Schoot CE, van Riel PL, Weinblatt ME, Wilson AG, Wolbink GJ, Wordsworth BP, Consortium Y, Wijmenga C, Karlson EW, Toes RE, de Vries N, Begovich AB, Worthington J, Siminovitch KA, Gregersen PK, Klareskog L, Plenge RM. Genome-wide association study meta-analysis identifies seven new rheumatoid arthritis risk loci. Nat. Genet. 2010;42:508–514. doi: 10.1038/ng.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Atabani SF, Thio CL, Divanovic S, Trompette A, Belkaid Y, Thomas DL, Karp CL. Association of CTLA4 polymorphism with regulatory T cell frequency. Eur. J. Immunol. 2005;35:2157–2162. doi: 10.1002/eji.200526168. [DOI] [PubMed] [Google Scholar]
- 18.Oaks MK, Hallett KM. Cutting edge: a soluble form of CTLA-4 in patients with autoimmune thyroid disease. J. Immunol. 2000;164:5015–5018. doi: 10.4049/jimmunol.164.10.5015. [DOI] [PubMed] [Google Scholar]
- 19.Liu MF, Wang CR, Chen PC, Fung LL. Increased expression of soluble cytotoxic T-lymphocyte-associated antigen-4 molecule in patients with systemic lupus erythematosus. Scand. J. Immunol. 2003;57:568–572. doi: 10.1046/j.1365-3083.2003.01232.x. [DOI] [PubMed] [Google Scholar]
- 20.Toussirot E, Saas P, Deschamps M, Pouthier F, Perrot L, Perruche S, Chabod J, Tiberghien P, Wendling D. Increased production of soluble CTLA-4 in patients with spondylarthropathies correlates with disease activity. Arthritis Res. Ther. 2009;11:R101. doi: 10.1186/ar2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Simone R, Brizzolara R, Chiappori A, Milintenda-Floriani F, Natale C, Greco L, Schiavo M, Bagnasco M, Pesce G, Saverino D. A functional soluble form of CTLA-4 is present in the serum of celiac patients and correlates with mucosal injury. Int. Immunol. 2009;21:1037–1045. doi: 10.1093/intimm/dxp069. [DOI] [PubMed] [Google Scholar]
- 22.Chen Z, Zhou F, Huang S, Jiang T, Chen L, Ge L, Xia B. Association of cytotoxic T lymphocyte associated antigen-4 gene (rs60872763) polymorphism with Crohn’s disease and high levels of serum sCTLA-4 in Crohn’s disease. J. Gastroenterol. Hepatol. 2011;26:924–930. doi: 10.1111/j.1440-1746.2011.06662.x. [DOI] [PubMed] [Google Scholar]
- 23.Sato S, Fujimoto M, Hasegawa M, Komura K, Yanaba K, Hayakawa I, Matsushita T, Takehara K. Serum soluble CTLA-4 levels are increased in diffuse cutaneous systemic sclerosis. Rheumatology. 2004;43:1261–1266. doi: 10.1093/rheumatology/keh303. [DOI] [PubMed] [Google Scholar]
- 24.Purohit S, Podolsky R, Collins C, Zheng W, Schatz D, Muir A, Hopkins D, Huang YH, She JX. Lack of correlation between the levels of soluble cytotoxic T-lymphocyte associated antigen-4 (CTLA-4) and the CT-60 genotypes. J. Autoimmune Dis. 2005;2:8. doi: 10.1186/1740-2557-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berry A, Tector M, Oaks MK. Lack of association between sCTLA-4 levels in human plasma and common CTLA-4 polymorphisms. J. Negat. Results Biomed. 2008;7:8. doi: 10.1186/1477-5751-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tector M, Khatri BO, Kozinski K, Dennert K, Oaks MK. Biochemical analysis of CTLA-4 immunoreactive material from human blood. BMC Immunol. 2009;10:51. doi: 10.1186/1471-2172-10-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Caby MP, Lankar D, Vincendeau-Scherrer C, Raposo G, Bonnerot C. Exosomal-like vesicles are present in human blood plasma. Int. Immunol. 2005;17:879–887. doi: 10.1093/intimm/dxh267. [DOI] [PubMed] [Google Scholar]
- 28.Crescitelli R, Lasser C, Szabo TG, Kittel A, Eldh M, Dianzani I, Buzas EI, Lotvall J. Distinct RNA profiles in subpopulations of extracellular vesicles: apoptotic bodies, microvesicles and exosomes. J. Extracell. Vesicles. 2013;2:20677. doi: 10.3402/jev.v2i0.20677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thery C, Amigorena S, Raposo G, Clayton A. Isolation and characterization of exosomes from cell culture supernatants and biological fluids. Curr. Protoc. Cell Biol. 2006 doi: 10.1002/0471143030.cb0322s30. Chapter 3: Unit 3.22. [DOI] [PubMed] [Google Scholar]
- 30.Blanchard N, Lankar D, Faure F, Regnault A, Dumont C, Raposo G, Hivroz C. TCR activation of human T cells induces the production of exosomes bearing the TCR/CD3/zeta complex. J. Immunol. 2002;168:3235–3241. doi: 10.4049/jimmunol.168.7.3235. [DOI] [PubMed] [Google Scholar]
- 31.Thery C, Zitvogel L, Amigorena S. Exosomes: composition, biogenesis and function. Nat. Rev. Immunol. 2002;2:569–579. doi: 10.1038/nri855. [DOI] [PubMed] [Google Scholar]
- 32.Boscato LM, Stuart MC. Heterophilic antibodies: a problem for all immunoassays. Clin. Chem. 1988;34:27–33. [PubMed] [Google Scholar]
- 33.Kaplan IV, Levinson SS. When is a heterophile antibody not a heterophile antibody? When it is an antibody against a specific immunogen. Clin. Chem. 1999;45:616–618. [PubMed] [Google Scholar]
- 34.Aly T, Devendra D, Barker J, Liu E, Yu L, Eisenbarth GS. Heterophile antibodies masquerade as interferon-alpha in subjects with new-onset type 1 diabetes. Diabetes Care. 2004;27:1205–1206. doi: 10.2337/diacare.27.5.1205. [DOI] [PubMed] [Google Scholar]
- 35.Brunet JF, Denizot F, Luciani MF, Roux-Dosseto M, Suzan M, Mattei MG, Golstein P. A new member of the immunoglobulin superfamily--CTLA-4. Nature. 1987;328:267–270. doi: 10.1038/328267a0. [DOI] [PubMed] [Google Scholar]
- 36.Freeman GJ, Freedman AS, Segil JM, Lee G, Whitman JF, Nadler LM. B7, a new member of the Ig superfamily with unique expression on activated and neoplastic B cells. J. Immunol. 1989;143:2714–2722. [PubMed] [Google Scholar]
- 37.Freeman GJ, Gribben JG, Boussiotis VA, Ng JW, Restivo VA, Jr., Lombard LA, Gray GS, Nadler LM. Cloning of B7-2: a CTLA-4 counter-receptor that costimulates human T cell proliferation. Science. 1993;262:909–911. doi: 10.1126/science.7694363. [DOI] [PubMed] [Google Scholar]
- 38.Linsley PS, Nadler SG, Bajorath J, Peach R, Leung HT, Rogers J, Bradshaw J, Stebbins M, Leytze G, Brady W, et al. Binding stoichiometry of the cytotoxic T lymphocyte-associated molecule-4 (CTLA-4). A disulfide-linked homodimer binds two CD86 molecules. J. Biol. Chem. 1995;270:15417–15424. doi: 10.1074/jbc.270.25.15417. [DOI] [PubMed] [Google Scholar]
- 39.Linsley PS, Wallace PM, Johnson J, Gibson MG, Greene JL, Ledbetter JA, Singh C, Tepper MA. Immunosuppression in vivo by a soluble form of the CTLA-4 T cell activation molecule. Science. 1992;257:792–795. doi: 10.1126/science.1496399. [DOI] [PubMed] [Google Scholar]
- 40.Lenschow DJ, Zeng Y, Thistlethwaite JR, Montag A, Brady W, Gibson MG, Linsley PS, Bluestone JA. Long-term survival of xenogeneic pancreatic islet grafts induced by CTLA4lg. Science. 1992;257:789–792. doi: 10.1126/science.1323143. [DOI] [PubMed] [Google Scholar]
- 41.Lin H, Bolling SF, Linsley PS, Wei RQ, Gordon D, Thompson CB, Turka LA. Long-term acceptance of major histocompatibility complex mismatched cardiac allografts induced by CTLA4Ig plus donor-specific transfusion. J. Exp. Med. 1993;178:1801–1806. doi: 10.1084/jem.178.5.1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Finck BK, Linsley PS, Wofsy D. Treatment of murine lupus with CTLA4Ig. Science. 1994;265:1225–1227. doi: 10.1126/science.7520604. [DOI] [PubMed] [Google Scholar]
- 43.Cross AH, Girard TJ, Giacoletto KS, Evans RJ, Keeling RM, Lin RF, Trotter JL, Karr RW. Long-term inhibition of murine experimental autoimmune encephalomyelitis using CTLA-4-Fc supports a key role for CD28 costimulation. J. Clin. Invest. 1995;95:2783–2789. doi: 10.1172/JCI117982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tivol EA, Boyd SD, McKeon S, Borriello F, Nickerson P, Strom TB, Sharpe AH. CTLA4Ig prevents lymphoproliferation and fatal multiorgan tissue destruction in CTLA-4-deficient mice. J. Immunol. 1997;158:5091–5094. [PubMed] [Google Scholar]
- 45.Genant HK, Peterfy CG, Westhovens R, Becker JC, Aranda R, Vratsanos G, Teng J, Kremer JM. Abatacept inhibits progression of structural damage in rheumatoid arthritis: results from the long-term extension of the AIM trial. Ann. Rheum. Dis. 2008;67:1084–1089. doi: 10.1136/ard.2007.085084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ruperto N, Lovell DJ, Quartier P, Paz E, Rubio-Perez N, Silva CA, Abud-Mendoza C, Burgos-Vargas R, Gerloni V, Melo-Gomes JA, Saad-Magalhaes C, Sztajnbok F, Goldenstein-Schainberg C, Scheinberg M, Penades IC, Fischbach M, Orozco J, Hashkes PJ, Hom C, Jung L, Lepore L, Oliveira S, Wallace CA, Sigal LH, Block AJ, Covucci A, Martini A, Giannini EH. Abatacept in children with juvenile idiopathic arthritis: a randomised, double-blind, placebo-controlled withdrawal trial. Lancet. 2008;372:383–391. doi: 10.1016/S0140-6736(08)60998-8. [DOI] [PubMed] [Google Scholar]
- 47.Kremer JM, Russell AS, Emery P, Abud-Mendoza C, Szechinski J, Westhovens R, Li T, Zhou X, Becker JC, Aranda R, Peterfy C, Genant HK. Long-term safety, efficacy and inhibition of radiographic progression with abatacept treatment in patients with rheumatoid arthritis and an inadequate response to methotrexate: 3-year results from the AIM trial. Ann. Rheum. Dis. 2011;70:1826–1830. doi: 10.1136/ard.2010.139345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Leffers HC, Ostergaard M, Glintborg B, Krogh NS, Foged H, Tarp U, Lorenzen T, Hansen A, Hansen MS, Jacobsen MS, Dreyer L, Hetland ML, all departments of rheumatology in Denmark Efficacy of abatacept and tocilizumab in patients with rheumatoid arthritis treated in clinical practice: results from the nationwide Danish DANBIO registry. Ann. Rheum. Dis. 2011;70:1216–1222. doi: 10.1136/ard.2010.140129. [DOI] [PubMed] [Google Scholar]
- 49.Takahashi N, Kojima T, Terabe K, Kaneko A, Kida D, Hirano Y, Fujibayashi T, Yabe Y, Takagi H, Oguchi T, Miyake H, Kato T, Fukaya N, Ishikawa H, Hayashi M, Tsuboi S, Kato D, Funahashi K, Matsubara H, Hattori Y, Hanabayashi M, Hirabara S, Yoshioka Y, Ishiguro N. Clinical efficacy of abatacept in Japanese rheumatoid arthritis patients. Mod. Rheumatol. 2013;23:904–912. doi: 10.1007/s10165-012-0760-4. [DOI] [PubMed] [Google Scholar]
- 50.Orban T, Bundy B, Becker DJ, DiMeglio LA, Gitelman SE, Goland R, Gottlieb PA, Greenbaum CJ, Marks JB, Monzavi R, Moran A, Raskin P, Rodriguez H, Russell WE, Schatz D, Wherrett D, Wilson DM, Krischer JP, Skyler JS. Co-stimulation modulation with abatacept in patients with recent-onset type 1 diabetes: a randomised, double-blind, placebo-controlled trial. Lancet. 2011;378:412–419. doi: 10.1016/S0140-6736(11)60886-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vincenti F, Larsen C, Durrbach A, Wekerle T, Nashan B, Blancho G, Lang P, Grinyo J, Halloran PF, Solez K, Hagerty D, Levy E, Zhou W, Natarajan K, Charpentier B, Belatacept Study Group Costimulation blockade with belatacept in renal transplantation. N. Engl. J. Med. 2005;353:770–781. doi: 10.1056/NEJMoa050085. [DOI] [PubMed] [Google Scholar]
- 52.Takahashi T, Tagami T, Yamazaki S, Uede T, Shimizu J, Sakaguchi N, Mak TW, Sakaguchi S. Immunologic self-tolerance maintained by CD25(+)CD4(+) regulatory T cells constitutively expressing cytotoxic T lymphocyte-associated antigen 4. J. Exp. Med. 2000;192:303–310. doi: 10.1084/jem.192.2.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thery C, Boussac M, Veron P, Ricciardi-Castagnoli P, Raposo G, Garin J, Amigorena S. Proteomic analysis of dendritic cell-derived exosomes: a secreted subcellular compartment distinct from apoptotic vesicles. J. Immunol. 2001;166:7309–7318. doi: 10.4049/jimmunol.166.12.7309. [DOI] [PubMed] [Google Scholar]
- 54.Valadi H, Ekstrom K, Bossios A, Sjostrand M, Lee JJ, Lotvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat. Cell. Biol. 2007;9:654–659. doi: 10.1038/ncb1596. [DOI] [PubMed] [Google Scholar]
- 55.Raposo G, Nijman HW, Stoorvogel W, Liejendekker R, Harding CV, Melief CJ, Geuze HJ. B lymphocytes secrete antigen-presenting vesicles. J. Exp. Med. 1996;183:1161–1172. doi: 10.1084/jem.183.3.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Raposo G, Tenza D, Mecheri S, Peronet R, Bonnerot C, Desaymard C. Accumulation of major histocompatibility complex class II molecules in mast cell secretory granules and their release upon degranulation. Mol. Biol. Cell. 1997;8:2631–2645. doi: 10.1091/mbc.8.12.2631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Admyre C, Johansson SM, Qazi KR, Filen JJ, Lahesmaa R, Norman M, Neve EP, Scheynius A, Gabrielsson S. Exosomes with immune modulatory features are present in human breast milk. J. Immunol. 2007;179:1969–1978. doi: 10.4049/jimmunol.179.3.1969. [DOI] [PubMed] [Google Scholar]
- 58.Pisitkun T, Shen RF, Knepper MA. Identification and proteomic profiling of exosomes in human urine. Proc. Natl. Acad. Sci. USA. 2004;101:13368–13373. doi: 10.1073/pnas.0403453101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gonzalez-Begne M, Lu B, Han X, Hagen FK, Hand AR, Melvin JE, Yates JR. Proteomic analysis of human parotid gland exosomes by multidimensional protein identification technology (MudPIT) J. Proteome. Res. 2009;8:1304–1314. doi: 10.1021/pr800658c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mittelbrunn M, Gutierrez-Vazquez C, Villarroya-Beltri C, Gonzalez S, Sanchez-Cabo F, Gonzalez MA, Bernad A, Sanchez-Madrid F. Unidirectional transfer of microRNA-loaded exosomes from T cells to antigen-presenting cells. Nat. Commun. 2011;2:282. doi: 10.1038/ncomms1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Choudhuri K, Llodra J, Roth EW, Tsai J, Gordo S, Wucherpfennig KW, Kam LC, Stokes DL, Dustin ML. Polarized release of T-cell-receptor-enriched microvesicles at the immunological synapse. Nature. 2014;507:118–123. doi: 10.1038/nature12951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Martinez-Lorenzo MJ, Anel A, Gamen S, Monle n I, Lasierra P, Larrad L, Pineiro A, Alava MA, Naval J. Activated human T cells release bioactive Fas ligand and APO2 ligand in microvesicles. J. Immunol. 1999;163:1274–1281. [PubMed] [Google Scholar]
- 63.Nolte-’t Hoen EN, Wagenaar-Hilbers JP, Peters PJ, Gadella BM, van Eden W, Wauben MH. Uptake of membrane molecules from T cells endows antigen-presenting cells with novel functional properties. Eur. J. Immunol. 2004;34:3115–3125. doi: 10.1002/eji.200324711. [DOI] [PubMed] [Google Scholar]
- 64.Xie Y, Zhang H, Li W, Deng Y, Munegowda MA, Chibbar R, Qureshi M, Xiang J. Dendritic cells recruit T cell exosomes via exosomal LFA-1 leading to inhibition of CD8+ CTL responses through downregulation of peptide/MHC class I and Fas ligand-mediated cytotoxicity. J. Immunol. 2010;185:5268–5278. doi: 10.4049/jimmunol.1000386. [DOI] [PubMed] [Google Scholar]
- 65.Wahlgren J, Karlson Tde L, Glader P, Telemo E, Valadi H. Activated human T cells secrete exosomes that participate in IL-2 mediated immune response signaling. PLoS One. 2012;7:e49723. doi: 10.1371/journal.pone.0049723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Huse M, Lillemeier BF, Kuhns MS, Chen DS, Davis MM. T cells use two directionally distinct pathways for cytokine secretion. Nat. Immunol. 2006;7:247–255. doi: 10.1038/ni1304. [DOI] [PubMed] [Google Scholar]
- 67.Oderup C, Cederbom L, Makowska A, Cilio CM, Ivars F. Cytotoxic T lymphocyte antigen-4-dependent down-modulation of costimulatory molecules on dendritic cells in CD4+ CD25+ regulatory T-cell-mediated suppression. Immunology. 2006;118:240–249. doi: 10.1111/j.1365-2567.2006.02362.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Onishi Y, Fehervari Z, Yamaguchi T, Sakaguchi S. Foxp3+ natural regulatory T cells preferentially form aggregates on dendritic cells in vitro and actively inhibit their maturation. Proc. Natl. Acad. Sci. USA. 2008;105:10113–10118. doi: 10.1073/pnas.0711106105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Grohmann U, Orabona C, Fallarino F, Vacca C, Calcinaro F, Falorni A, Candeloro P, Belladonna ML, Bianchi R, Fioretti MC, Puccetti P. CTLA-4-Ig regulates tryptophan catabolism in vivo. Nat. Immunol. 2002;3:1097–1101. doi: 10.1038/ni846. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.