Abstract
Pulmonary infections in critically ill patients are common and associated with high morbidity and mortality. Piperacillin-tazobactam is a frequently used therapy in critically ill patients with pulmonary infection. Antibiotic concentrations in the lung reflect target site antibiotic concentrations in patients with pneumonia. The aim of this study was to assess the plasma and intra-pulmonary pharmacokinetics (PK) of piperacillin-tazobactam in critically ill patients administered standard piperacillin-tazobactam regimens. A population PK model was developed to describe plasma and intra-pulmonary piperacillin and tazobactam concentrations. The probability of piperacillin exposures reaching pharmacodynamic endpoints and the impact of pulmonary permeability on piperacillin and tazobactam pulmonary penetration was explored. The median piperacillin and tazobactam pulmonary penetration ratio was 49.3% and 121.2%, respectively. Pulmonary piperacillin and tazobactam concentration were unpredictable and negatively correlated to pulmonary permeability. Current piperacillin-tazobactam regimens may be insufficient to treat pneumonia caused by piperacillin-tazobactam susceptible organisms in some critically ill patients.
Keywords: Piperacillin, tazobactam, population pharmacokinetics, critical care, pneumonia
Introduction
Pulmonary infection in critically ill patients results in an unacceptably high mortality and morbidity, which increases the length of hospital stay and associated healthcare costs1,2. Approximately 16% of patients admitted to intensive care units (ICU) present with a pulmonary infection3. Additionally, the lung is the primary site of infection in over 60% of nosocomial infections occurring within the ICU3. Attributable mortality from ventilator-associated pneumonia is estimated to be 13%, but may be as high as 69% in certain subgroups4. Pulmonary infections in critically ill patients are caused by a wide range of organisms, including difficult-to-treat organisms such as Pseudomonas aeruginosa5. Use of appropriately targeted antimicrobial chemotherapy is associated with improved clinical outcomes6. However, clinical outcomes in patients that are infected with a susceptible organism receiving an appropriate antimicrobial agent remain sub-optimal. This is partly due to marked pharmacokinetic (PK) variability occurring in critically ill patients7. The PK of critically ill patients may be affected by physiological changes associated with illness, which typically results in a higher proportion of patients receiving sub-optimal drug exposure when a fixed regimen is used7–9. Additionally, many currently licensed drug regimens are informed by studies performed in non-critically ill patients, and may not necessarily be appropriate outside that context.
Piperacillin-tazobactam is a combination of an extended-spectrum β-lactam antibiotic (piperacillin) with a β-lactamase inhibitor (tazobactam). Piperacillin-tazobactam has a broad-spectrum of action that includes Gram-positive, Gram-negative and anaerobic bacteria10. Consequently, piperacillin-tazobactam is a common choice for both directed and empirical treatment of critically ill patients11. The pharmacodynamic index that best links piperacillin concentrations with its antimicrobial effect is the fraction of the dosing interval that unbound piperacillin concentrations are above the minimum inhibitory concentration (MIC)12. Near-maximal antimicrobial effect is generally observed when free piperacillin concentrations exceed the MIC for at least 50% of the dosing interval (50% fT>MIC)13. However, 100% fT>MIC may be more appropriate for critically ill patients14. The global increase in the incidence of antimicrobial resistance has focused attention on antimicrobial drug regimens that are safe, effective and also minimise the probability of the emergence of antimicrobial resistance15. We recently used a hollow fibre infection model of piperacillin-tazobactam versus Pseudomonas aeruginosa to demonstrate a trough (Cmin) total piperacillin concentration-to-MIC ratio of between 3 and 10 prevents the emergence of antimicrobial resistance16. Identification of piperacillin-tazobactam regimens that enable the attainment of pharmacodynamic targets for both efficacy and suppression of emergence of antimicrobial resistance may led to improved clinical outcomes and increase the clinical longevity of this commonly used agent.
Adequate antibiotic concentrations at the site of infection are required for effective antimicrobial activity17. For pulmonary infection, the epithelial lining fluid (ELF) represents a compartment that is both clinically relevant and accessible for measurement of drug concentrations18,19. In general, clinical β-lactam exposure–response relationships within ELF are poorly defined18. An understanding of drug penetration into ELF and drug exposure-response relationships within that compartment are an important consideration when bridging from pre-clinical to clinical studies20. The pulmonary penetration ratio, or partition coefficient, relates drug exposure in ELF to drug exposure in plasma. Healthy volunteer data suggests the area under the concentration (AUC) time curve in ELF is ≈25% and ≈50% of the plasma piperacillin and tazobactam AUCs, respectively21. While there is a general paucity of information regarding ELF penetration of antimicrobial agents in critically ill patients, two studies suggest that piperacillin and tazobactam ELF concentrations are ≈50% and 65-90% of their respective paired plasma concentrations22,23.
The primary aim of this clinical study was to quantify the pulmonary penetration of piperacillin and tazobactam in critically ill patients. We also investigated factors that may influence the penetration of drug into the lung. A population pharmacokinetic model was used to describe the observed plasma and ELF concentrations of piperacillin and tazobactam in critically ill patients. Monte Carlo simulation was used to explore the impact of pharmacokinetic variability on plasma and ELF piperacillin exposures to achieve the desired pharmacodynamic target. Additionally, the influence of pulmonary permeability on pulmonary piperacillin and tazobactam concentrations was investigated.
Results
Pharmacokinetic study
Between June 2012 and July 2013 eighteen critically ill patients were enrolled with a mean age of 56 years and mean APACHE II score of 15 (Table 1). One patient who was infected with a novel coronavirus was excluded from all analyses because of issues related to biosafety. First-dose pharmacokinetics were assessed in four patients. Steady state pharmacokinetics were assessed in seventeen patients who had received a mean of 8.8 doses (range 2-16). Four patients were on renal replacement therapy and received piperacillin-tazobactam every 12 hours. The remaining 13 patients received piperacillin-tazobactam every 8 hours. Five patients received piperacillin-tazobactam over 5 minutes while the remaining 12 patients received piperacillin-tazobactam over 30 minutes. In total, 128 plasma and 31 ELF samples were obtained for pharmacokinetic analyses. Three piperacillin plasma samples, 3 piperacillin ELF samples and 14 tazobactam plasma samples were below the limit of assay quantification.
Table 1. Table showing the patients underlying demographics, severity of disease and outcome.
Creatinine clearance: calculated by Cockgroft-Gault; patients on renal replacement therapy exclude.
| Characteristics | ||
|---|---|---|
| Age (years) (mean (median) [range]) | 56.0 (53.5) [31.4-80.8] | |
| Height (metres) (mean (median) [range]) | 1.70 (1.74) [1.40-1.83] | |
| Weight (kg) (mean (median) [range]) | 80.0 (75.0) [47.0-140.0] | |
| BMI (kg/m2) (mean (median) [range]) | 27.7 (25.4) [20.9-44.2] | |
|
| ||
| Sex (n(%)) | Male | 9 (52.9%) |
| Female | 8 (47.1%) | |
|
| ||
| Race (n(%)) | White | 16 (94.1%) |
| Bangladeshi | 1 (5.9%) | |
|
| ||
| Clinical pulmonary infection score (mean (median) [range]) | 5.6 (5.3) [3.0-9.0] | |
| APACHE II score (mean (median) [range]) | 14.9 (15.0) [8.0-24.0] | |
| SOFA score (first dose) (mean (median) [range]) | 6.1 (6.0) [2.0-14.0] | |
| SOFA score (steady state) (mean (median) [range]) | 5.8 (6.0) [1.0-10.0] | |
| Creatinine clearance (ml/min) (mean (median) [range]) | 106.9 (106.9) [18.3-230.2] | |
|
| ||
| Renal replacement therapy (n(%)) | None | 13 (76.5%) |
| Yes | 4 (23.5%) | |
|
| ||
| Outcome (n(%)) | Alive | 14 (82.4%) |
| Dead | 3 (17.6%) | |
Three non-directed bronchial lavage (NBL) specimens (two from a single patient) were not collected because of a clinical requirement for a high fraction of inspired oxygen (FiO2) that precluded sampling. A single patient had a drop in oxygen saturation from 95% to 88% that required a temporary increase in FiO2. A change in oxygen saturation was not observed in any other patients. No other changes in respiratory or cardiovascular parameters were observed in the four hours following collections of the other NBL samples.
Population pharmacokinetic analysis
The fit of the mathematical model to the observed data was acceptable. A linear regression of the predicted-versus-observed plasma piperacillin and tazobactam concentrations revealed the following relationship: Observed Piperacillin Concentration = 0.884 × Predicted Piperacillin Concentration + 2.01; r2 = 0.901. Similarly, the Observed Tazobactam Concentration = 0.880 × Predicted Tazobactam Concentration + 0.165; r2 = 0.839. A linear regression of the predicted and observed piperacillin and tazobactam concentrations in the ELF was given by: Observed Piperacillin Concentration = 0.790 × Predicted Piperacillin Concentration – 1.65; r2 = 0.812; and Observed Tazobactam Concentration = 0.827 × Predicted Tazobactam Concentration + 1.21; r2 = 0.878. For plasma piperacillin and tazobactam concentrations, the mean weighted bias was −0.00999 and 0.0214, respectively; and the bias-adjusted mean weighted precision was 25.5 and 1.22, respectively. For piperacillin and tazobactam concentrations in ELF, the mean weighted bias was −0.057 and 0.169, and of bias-adjusted mean weighted precision was 0.124 and 7.23, respectively. The parameter estimates from the population analysis are summarized in Table 2. The inter-compartmental piperacillin clearance between the central and peripheral and central and ELF compartments were 153.87 L/hour and 2.64L/hour, respectively. The inter-compartmental tazobactam clearance between the central and peripheral and central and ELF compartments were 144.15 L/hour and 6.45 L/hour, respectively. The volume of the peripheral compartment was 7.65 L and 6.78 L for piperacillin and tazobactam, respectively.
Table 2. Piperacillin and tazobactam population pharmacokinetic parameter estimates obtained by Pmetrics.
Cl (L/hr) is the clearance, and Vc is the volume of the central compartment (L). Kcp, Kpc, KcELF and KELFc are the first-order inter-compartmental rate constants (hr−1) between the central and peripheral and central and ELF compartments.
|
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Parameters | Cl (liters/hr) | Vc (liters) | kcp (hr−1) | kpc (hr−1) | kcELF (hr−1) | kELFc (hr−1) | VELF (liters) | |
| Piperacillin | Mean | 12.122 | 11.717 | 13.132 | 20.107 | 0.225 | 0.559 | 16.847 |
| Median | 9.337 | 10.556 | 10.503 | 25.135 | 0.158 | 0.343 | 18.884 | |
| SD | 6.833 | 4.921 | 8.672 | 10.15 | 0.212 | 0.693 | 7.834 | |
|
| ||||||||
| Tazobactam | Mean | 9.675 | 14.795 | 9.743 | 21.317 | 0.436 | 1.074 | 15.84 |
| Median | 7.177 | 15.661 | 5.277 | 28.681 | 0.219 | 0.235 | 21.282 | |
| SD | 5.645 | 8.762 | 8.905 | 10.847 | 0.465 | 1.847 | 9.326 | |
External validation of the population pharmacokinetic analysis
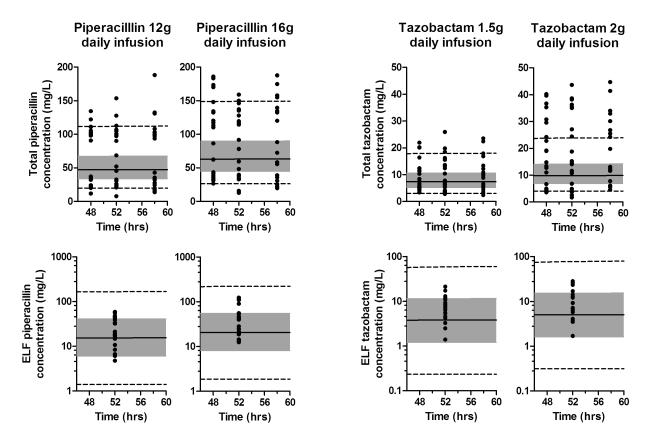
A plot of observed piperacillin and tazobactam concentrations from a previously published study overlaid by the predicted 5th, 25th, 50th,75th and 95th centile drug concentrations from this study (simulated using the population pharmacokinetic model) revealed a high degree of concordance (Figure 1)22.
Figure 1. External validation of piperacillin and tazobactam population model.
The top row of panels show total plasma drug concentration and the lower panels show ELF drug concentrations. Each panel shows the median drug concentration (solid black line), the inter-quartile range (shaded grey area) and the 5th and 95th centiles (dotted black lines). Overlying data points represent observed data from Boselli et al22.
Plasma piperacillin/tazobactam concentration and pulmonary penetration
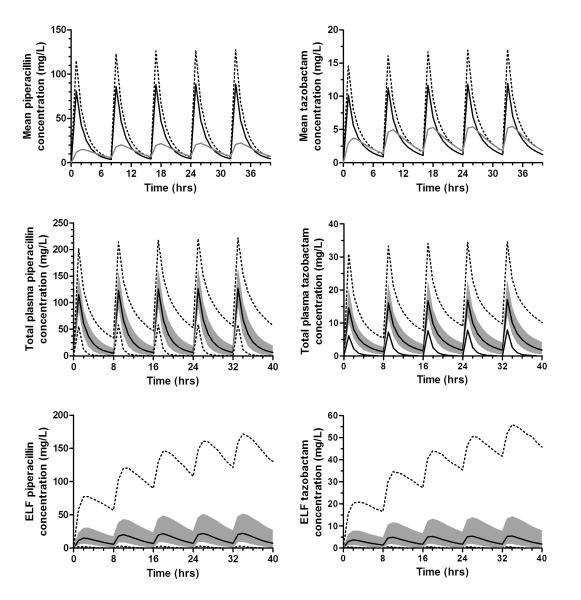
Simulated concentration-time profiles, showing the median, 5th, 25th, 75th and 95th centile drug concentrations in both plasma and ELF, following administration of five simulated doses of piperacillin 4 grams and tazobactam 0.5 grams, each as a 30 minute infusion every eight hours, are shown in Figure 2. The median AUCELF/AUCunbound plasma penetration ratio was 49.3% (range: 2.0% -515.9%) for piperacillin and 121.2% (range: 11.0% - 391.3%) for tazobactam.
Figure 2. Concentration-time profiles for piperacillin (left) and tazobactam (right).
The top panel compares total drug concentration (dotted line), unbound drug concentration (solid, black line) and ELF drug concentration (solid grey line). The middle panels show unbound plasma concentration while the lower two panels show ELF concentrations with median drug concentration (solid black line), the inter-quartile range (shaded grey area) and the 5th and 95th centiles (dotted black lines).
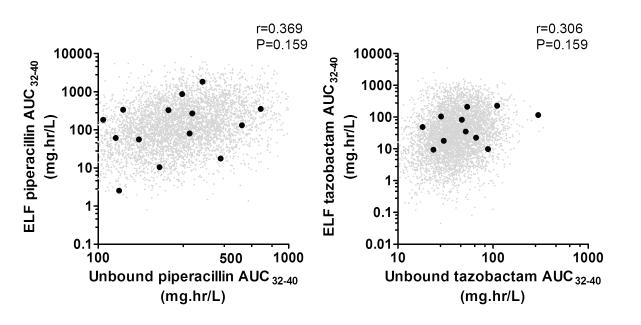
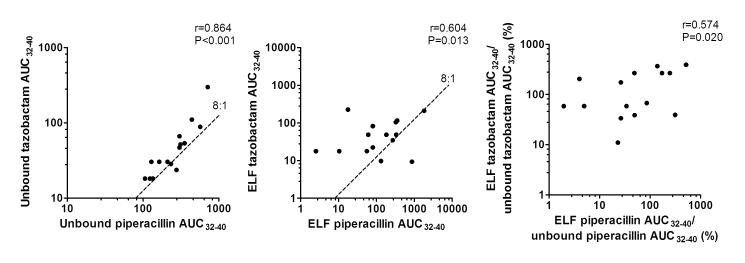
Simulated plasma and ELF exposures for each individual patient (using the Bayesian posterior parameter estimates) allowed an assessment of the drug penetration from plasma to ELF and the inter-relationship between the two co-administered drugs. There was no statistically significant correlation between ELF piperacillin exposure (AUCELF) and unbound plasma piperacillin exposure (AUCunbound plasma) (r=0.369, P=0.159; Figure 3). Similarly, there was no statistically significant correlation between ELF tazobactam exposure (AUCELF) and unbound plasma tazobactam exposure (AUCunbound plasma) (r=0.306, P=0.248; Figure 3). Unbound tazobactam exposure in the plasma of critically ill patients was statistically significantly positively correlated with unbound piperacillin plasma exposures (AUCunbound plasma) (r=0.864; P<0.0001; Figure 4). There was also a statistically significant positive correlation between tazobactam and piperacillin ELF exposures (AUCELF) (r=0.604; P=0.013; Figure 4).
Figure 3. Relationship between unbound plasma and ELF drug concentrations for piperacillin (left) and tazobactam (right) for each of the observed trial patients (black dots) and for 5,000 simulated patients (small grey dots).
Figure 4. Comparison of the piperacillin and tazobactam exposures in the plasma (left), ELF (centre) and the plasma:ELF ratio (right).
The dotted lines illustrate the 8:1 ratio of piperacillin to tazobactam in the administered piperacillin 4.0 gram/tazobactam 0.5 gram preparation.
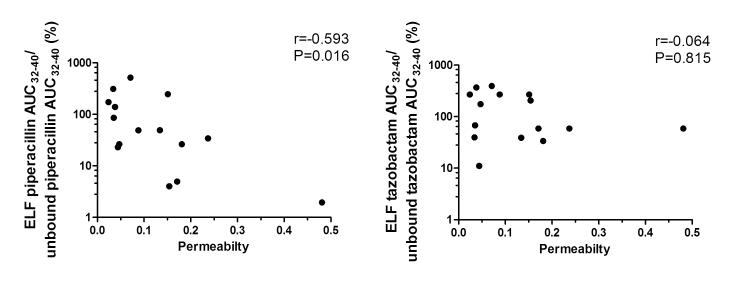
Mean pulmonary permeability, as estimated by the ratio of urea-corrected total protein in ELF to plasma total protein concentration, was 0.1226 (median = 0.0795; S.D. = 0.1155). A statistically significant negative correlation was observed between the piperacillin penetration ratio (AUCELF/AUCunbound plasma) and pulmonary permeability (r=-0.593; P=0.016, Figure 5). In contrast, no statistically significant correlation was seen between the tazobactam penetration ratio (AUCELF/AUCunbound plasma) and pulmonary permeability (r=−0.064; P=0.815, Figure 5).
Figure 5. Comparison of the plasma:ELF ratio for piperacillin (left) and tazobactam (right) exposure with pulmonary permeability.
Probability of target attainment analysis
Monte Carlo simulation was used to estimate the probability of achieving predefined pharmacodynamic targets. The results of the probability of target attainment analysis for piperacillin are shown in Figure 6. The administration of piperacillin 4g three times daily, as a 30 minute infusion to treat an organism with an MIC of 1 mg/L resulted in 96%, 77% and 64% of patients achieving a pharmacodynamic target of 50% fT>MIC, 100% fT>MIC and Cmin/MIC>3.4, respectively. The treatment of an organism with an MIC of 16 mg/L (i.e. the current CLSI and EUCAST breakpoint for Pseudomonas auriginosa24,25) resulted in 54%, 20% and 6% patients achieving a pharmacodynamic target of 50% fT>MIC, 100% fT>MIC and Cmin/MIC>3.4, respectively.
Figure 6. Results of the Monte Carlo simulation with the probability of target attainments, for unbound (solid line) and ELF (dashed line) piperacillin, against a range of MICs.
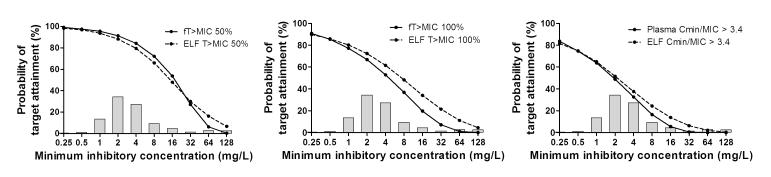
The pharmacodynamic targets are the fraction of patients whose drug concentration was about the MIC for 50% (left panel) or 100% (middle panel) of the dosing interval and the fraction of patients whose trough piperacillin concentration to MIC ratio was ≥ 3.4. Histogram shows MIC distribution for organisms causing hospital-acquired and ventilator-associated pneumonia26.
The predicted target attainments in plasma and ELF, for each MIC, were similar. For example, the target attainment rate using an endpoint of unbound piperacillin concentrations that were 50% fT>MIC was 96% and 54% for MICs of 1 and 16 mg/L, respectively. In comparison, the use of the same pharmacodynamic target in ELF (i.e. 50% T>MIC) resulted in target attainment rates of 94% and 48% for MICs if 1 and 16 mg/L, respectively. For the most susceptible organisms (i.e. MICs in the range 0.25-1 mg/L) both the unbound plasma and ELF concentrations were above the MIC for 50% of the dosing interval in over >90% of simulated patients.
From the frequency distribution of piperacillin-tazobactam susceptibilities of isolates causing hospital-acquired and ventilator-associated pneumonia the overall response rate of critically ill patients with VAP can be estimated (Figure 6)26. If piperacillin was administered empirically (i.e. the MIC is not known) 80% of critically ill patients with VAP would achieve plasma 50% fT>MIC and 77% of patients would achieve ELF 50% T>MIC. In contrast, if piperacillin was administered in critically ill patients with VAP caused by a susceptible organism (i.e. MIC ≤ 16 mg/L) 86% of patients would achieve plasma 50% fT>MIC and 82% of patients would achieve ELF 50% T>MIC. For suppression of emergence of antimicrobial resistance following empirical administration of piperacillin, 38% of critically ill patients with VAP would achieve plasma Cmin/MIC>3.4 and 41% of patients would achieve ELF Cmin/MIC>3.4. If piperacillin was administered critically ill patients with VAP caused by a susceptible organism 42% of patients would achieve plasma Cmin/MIC>3.4 and 45% of patients would achieve ELF Cmin/MIC>3.4.
Discussion
Inspection of the concentration-time profiles for both piperacillin and tazobactam illustrates marked pharmacokinetic variability in critically ill patients (Figure 2). The pharmacokinetic variability is notably more evident in the lung compared with plasma for both compounds. The estimates of clearance and volume of the central compartment from the population PK model are consistent with previously published values9,27,28. The validity and generalizability of our results are further suggested by the concordance of simulated concentrations from the population PK model with data from a previously published group of critically ill patients (see Figure 1)22.
Beta-lactam antibiotics penetrate the lung by passive diffusion18,29. Diffusion into tissues is dependent on the concentration gradient across biological membranes, the surface area of the membrane and a diffusion coefficent30. The diffusion coefficient is principally influenced by physicochemical characteristics of the drug (e.g. the degree of lipophilicity) and the extent of protein binding31,32. There was a positive correlation between plasma and ELF exposures for both piperacillin and tazobactam. However, these relationships did not reach statistical significance which is unexpected and perhaps due to the modest number of patients in the study. In this study we used the ratio of total protein in ELF to plasma as a surrogate measure of lung permeability33. We expected to see an increase in diffusion of drug with increasing pulmonary protein penetration. However, we observed a statistically significant negative correlation between the piperacillin pulmonary penetration ratio (AUCELF/AUCunbound plasma) and pulmonary permeability (Figure 5). As pulmonary permeability increased, there was a reduction in the relative proportion of piperacillin penetrating the lung. For tazobactam there was no statistically significant correlation between the pulmonary penetration ratio (AUCELF/AUCunbound plasma) and pulmonary permeability. The relationship between pulmonary permeability and pulmonary drug concentration has not previously been investigated for β-lactam antibiotics. Pulmonary vancomycin penetration has been shown to be higher in patients with increased pulmonary permeability as measured by ELF albumin concentration34. Lung penetration of β-lactam antibiotics has been shown to be dependent on plasma albumin concentration31,35,36. Increased tissue penetration occurs when higher unbound plasma β-lactam antibiotic concentrations are observed in patients with hypoalbuminaemia. This phenomenon primarily affects highly protein bound agents such as ertapenem and flucloxacillin31,35,36. There are a number of potential explanations for the relationship between piperacillin lung penetration and permeability. Methodologically, this is a small study with extreme PK variability in both the observed plasma and ELF drug concentration. Multiplication of the measured pulmonary sample concentration by a dilution factor, derived from comparison of urea concentrations in plasma and pulmonary samples37,38, may contribute to the greater variability observed in the pulmonary drug concentrations when compared with plasma concentrations. A possible biological explanation includes dilution of intra-pulmonary piperacillin due to larger ELF volumes that are associated with increasing pulmonary permeability. Alternatively, β-lactam antibiotics are substrates for organic anion transporters in other organs such as the kidney39. Disruption of an active transport system may occur in the injured lungs of critically ill patients, which exhibit increased permeability to protein. Another explanation may be that an increase in pulmonary protein permeability preferentially affects diffusion of piperacillin and tazobactam in and out of the lung. Therefore in lungs with low protein permeability, piperacillin diffuses into the lung faster than it diffuses out. The reverse occurs in lungs with higher protein permeability. Validation of negative correlation of pulmonary piperacillin penetration and pulmonary permeability is required in a similar clinical cohort.
Measurement of antimicrobial agents in ELF may not truly reflect drug concentration within other pulmonary sub-compartments. Micro-dialysis techniques may provide a better estimate of pulmonary drug concentrations than bronchoalveolar lavage for quantifying drug concentrations in ELF40. However, due to practical difficulties with pulmonary micro-dialysis, ELF sampling remains the most commonly utilised technique in both pre-clinical and clinical studies17,41. In this study we used NBL. NBL is a safe and effective way of sampling the lung and quantifying antimicrobial drug concentrations in the ELF of critically ill patients42. NBL is less invasive than bronchoscopy and bronchoalveolar lavage (BAL), allowing multiple NBL samples to be collected throughout the dosing interval. The collection of two NBL samples from each patient, rather than one BAL provides a more robust estimate of the concentration-time profile in the ELF of individual patients. Only one minor adverse event was reported following NBL.
For β-lactam antibiotics, the pharmacodynamic index that best links drug exposure with the antibacterial effect is the fraction of the dosing interval that the free drug concentrations are above the MIC12. For piperacillin the unbound piperacillin concentration must be above the MIC for at least 50% of the dosing interval is generally associated with near maximal efficacy (50% fT>MIC)13. We recently demonstrated a trough unbound piperacillin concentration to MIC ratio of >3.4 is required to suppress the emergence of antimicrobial resistance (Cmin/MIC>3.4)16. From the target attainment analysis (Figure 6) the empirical administration of piperacillin 4g three times daily, as a 30 minute infusion (i.e. the MIC is not known) results in an 80% probability of attainment of a pharmacodynamic target of plasma 50% fT>MIC or a 77% probability of attainment of a pharmacodynamic target of 50% ELF T>MIC. The probability of achieving the same pharmacodynamic targets increases to 86% and 82%, for plasma and ELF respectively, when the MIC is known and organisms with MICs beyond the breakpoint (i.e.>16 mg/L) are excluded. Therefore, 14-18% of patients with a “susceptible” organism will have sub-optimal drug exposure. Furthermore, approximately 60% of patients will not achieve the plasma or ELF pharmacodynamic targets associated with suppression of antimicrobial resistance (Cmin/MIC>3.4). This analysis identifies two important issues. Firstly, piperacillin 4g three times daily, as a 30 minute infusion, is inadequate for effective treatment and suppression of emergence of antimicrobial resistance in an unacceptably high proportion of critically ill patients, and especially those with pneumonia resulting from infection with a less susceptible organism. Secondly, the probability of achieving each of the pharmacodynamic targets (i.e. fT>MIC, Cmin/MIC etc) in plasma and ELF are similar. Plasma piperacillin concentrations do not precisely predict ELF piperacillin concentrations. Consequently, some individuals with “sufficient” plasma piperacillin exposure will have inadequate ELF piperacillin exposures and vice-versa. ELF rather than plasma exposure has been shown to predict outcome for other antimicrobial agents17. The causative organisms were not isolated in our 17 patients which makes exploration of the relationship between piperacillin plasma and ELF pharmacokinetics, pharmacodynamic (fT>MIC, Cmin/MIC) and clinical outcome impossible. Further appropriately powered clinical studies are required to examine whether piperacillin exposure in plasma or ELF better predicts clinical outcomes.
The addition of tazobactam to piperacillin extends the activity of the β-lactam to β-lactamase producing strains of organisms such as Enterobacteriaceae, Staphylococcus aureus., H. influenzae and M. catarrhalis43. The current regimen of piperacillin-tazobactam, at a fixed 8:1 ratio, is supported by in-vitro studies44–46. However, the pharmacodynamic index that best links β-lactamase inhibitor exposure with effect is poorly defined. Both: (i) the fraction of the dosing interval the β-lactamase inhibitor concentration is above a threshold (T>threshold) and (ii) the area under the β-lactamase inhibitor concentration time curve have been suggested as the relevant pharmacodynamic indeces47–49. The required concentration of β-lactamase inhibitor is dependent on the amount and type of β-lactamase50. Tazobactam penetrates the lung of most critically ill patients, but there is marked variability. Therefore, a subset of patients may have insufficient pulmonary tazobactam concentrations to adequately inhibit some β-lactamases that cause hydrolysis of piperacillin and clinical failure despite adequate piperacillin exposure. Increasing the tazobactam dosage (while maintaining the piperacillin dosage) may overcome β-lactamase production as has been demonstrated in an in-vivo meningitis model51. As plasma tazobactam exposure does not reflect tazobactam exposure in ELF, the identification of patients with poor pulmonary tazobactam penetration is difficult and appears to require direct sampling from the lung.
In conclusion, the primary aim of this study was to develop and validate a mathematical model to describe piperacillin and tazobactam concentration in plasma and the lung of critically ill patients. Additionally we show an unexpected relationship of increased pulmonary permeability being associated with a reduction in pulmonary piperacillin penetration. We also demonstrated that predicting pulmonary piperacillin and tazobactam exposures on the basis of plasma drug exposures may be unreliable. Approprialty powered clinical trials are required to further defined the relationship between plasma and pulmonary drug exposures and establish the impact of pulmonary, rather than plasma, drug exposure on clinical outcome. Additionally pre-clinical and clinical studies are required to investigate mechanisms lung penetration in patients with pneumonia. Biomarkers related to pulmonary permeability or drug penetration could be incorportated as covariates into mathematical models to improve predictions of pulmonary drug exposures. New regimens of piperacillin-tazobactam may be required which optimise drug concentrations in the lung, at the site of infection. It is likely that a single regimen is not suitable for all individuals. If ELF exposure is shown to predict clinical outcome, with great accuracy than plasma exposure, and covariates for pulmonary drug penetration cannot be identified then direct measurement of drug concentrations in the pulmonary compartment, and adjustment of individual regimens may be required.
Methods
Pharmacokinetic study
This was a prospective open-label single arm pharmacokinetic study. The study was conducted in accordance with the Declaration of Helsinki and approved in the UK by both the local Research Ethics Committee and the Medicine and Healthcare Products Regulatory Agency (EudraCT number: 2011-004470-28). Intubated patients who received piperacillin-tazobactam for suspected or documented pulmonary infection at the University Hospital of South Manchester NHS Trust, Manchester, UK were eligible for inclusion. Piperacillin-Tazobactam 4g/0.5g (Stragen, UK) was administered over less than 30 minutes every eight hours except in patients with a creatinine clearance of <20ml/min or those on renal replacement therapy who were administered the drug every 12 hours. Written informed consent was obtained from the next of kin of all patients participating in the study. Additionally retrospective informed consent was obtained from all patients that survived and regained capacity to give consent. Demographic data (including age, sex, race, height, weight), disease severity (by APACHE II and SOFA score), underlying renal function, presence of renal replacement therapy and clinical outcome were recorded.
Sampling was performed following administration of the first dose of piperacillin-tazobactam if possible. All patients underwent sampling at steady-state. The mean half-life of piperacillin is ≈0.75 hr so patients were assumed to be at steady-state by the second dose9. A previously published, optimally designed sampling schedule was used to inform the timings for collection of the plasma samples9. Plasma samples were collected at ½, 1½, 2½, 3¾, 5, 6 hours after initiation of the infusion for the first dose and immediately prior to the dose and ¼, ¾, 2, 3½ and 4½ hours following initiation of the infusion at steady state. All plasma samples were collected in lithium heparin containing tubes. As soon as collected all plasma samples were centrifuged at 1,400 x g for 12 minutes. Samples were stored at −80 °C in 0.4 mL aliquots prior to analysis.
Non-directed bronchial lavage (NBL) were assumed to be equivalent to bronchoalveolar lavage and were used for recovery of intra-pulmonary samples42. Two intra-pulmonary samples were collected on each patient during the steady-state dosing interval. Samples were collected at ¾ and 2 or ¾ and 3½ hours following initiation of the infusion. Patients (a) requiring > 80% inspired oxygen; (b) requiring > 12 cmH20 positive end expiratory pressure; (c) in whom endotracheal suction leads to a severe and prolonged desaturation; (d) with severe bronchospasm; (e) with uncontrolled or persistently raised intracranial pressure or (f) with severe disseminated intravascular coagulation did not have NBL samples collected. Briefly, suitable patients were pre-oxygenated with 100% oxygen for 2 minutes prior to sampling. A suction catheter was introduced into the bronchia tree until wedged and 20 mL of sterile normal (0.9%) saline was instilled over 5-10 seconds and then immediately aspirated. Typically 10 mLs of normal saline was recovered. Patients were monitored for four hours after the NBL for signs of cardio-respiratory compromise. As soon as collected all NBL samples were filtered through a 48 μm filter and centrifuged at 2,000 x g for 10 minutes. Samples were stored at −80 °C in 0.5 mL aliquots prior to analysis.
Piperacillin, tazobactam, urea and protein assays
Piperacillin and tazobactam concentrations in plasma and lavage fluid were measured using a validated liquid chromatography–tandem mass spectrometry (LC/MS/MS) method with an Agilent 6420 Triple Quad Mass spectrometer (Agilent Technologies UK Ltd, Cheshire, UK). Twenty μL of extracted sample was injected onto a Synergi 4u Hydro RP 80A 100×2.0mm column (Phenomenex, Cheshire, UK). The standard curves for piperacillin and tazobactam encompassing the concentration ranges of 0.02-10.0 mg/L and 0.02-5.0 mg/L respectively for plasma and 0.02-10.0 mg/L for lavage fluid were constructed in plasma and blank lavage fluid, respectively. The standard curves were made from a stock solution of 1 mg/L of piperacillin and tazobactam, respectively. The internal standard was caffeine in water at 0.1 mg/L (Sigma Aldrich, Dorset, UK). The between-day coefficients of variation were <17.4% for piperacillin and <15.5% for tazobactam. The lower limit of detection for piperacillin and tazobactam in plasma and lavage fluid was 0.02 mg/L.
Urea concentrations in plasma and lavage fluid were performed using a colorimetric technique (QuantiChromTM Urea Assay Kit DIUR-500, Gentaur BVBA – Bioxys, Belgium). The standard curve for the urea assay is linear over a concentration range of 0-100 mg/dL. Plasma samples were diluted 1:5 prior to measure of urea. Drug concentrations in NBL samples were assumed to reflect ELF drug concentrations once corrected for the dilution, introduced by lavage sampling, using the urea dilution method37,38. Urea concentration was assumed to be the same in plasma and ELF. Therefore comparison of urea concentration in the plasma and lavage fluid allows estimation of the dilution caused by instillation of lavage fluid to the lung. The concentration of piperacillin and tazobactam in ELF was estimated using the following formula:
Where [Drug]ELF and [Drug]lavage are the concentration of either piperacillin or tazobactam in ELF and lavage fluid, respectively. [Urea]plasma and [Urea]lavage are the concentrations of urea in the plasma and lavage, respectively.
Pulmonary permeability was assumed to be proportional to the ratio of the mean total protein concentrations in plasma and ELF33. Total protein was quantified in plasma using the Total Protein assay on an Abbott Architect C16000 (Abbott Laboratories, IL, USA). This colorimetric assay uses with biuret reagent to detect the presence of peptide bonds. The limit of detection for total protein was 0.5 g/dL. The limit of quantification was 0.76 g/dL. The imprecision of the Total Protein assay is ≤ 3% total coefficient of variation. Protein in ELF was quantified using UPro assay on an Abbott Architect c8000 (Abbott Laboratories, IL, USA). This assay uses a turbidimetric procedure in which benzethonium chloride is used as the protein denaturing agent. The limit of quantification and detection for the UPro assay is 6.75 mg/dL. The imprecision of the assay is ≤ 7.8% total coefficient of variation. ELF protein concentration was corrected for dilution using the urea dilution method described above.
Population pharmacokinetic analysis
All data were analyzed using a population pharmacokinetic methodology with the non-parametric adaptive grid (NPAG) program Pmetrics 1.1.352. For both piperacillin and tazobactam a three-compartment structural mathematical models was assumed to be most appropriate for population analysis.
| Equation 1: |
| Equation 2: |
| Equation 3: |
The differential equations for the three-compartment structural mathematical model used are shown above. X1, X2 and X3 are the amounts of piperacillin (in mg) in the central, peripheral and ELF compartments, respectively. R(1) represents the infusion of piperacillin. Cl (L/hr) is the clearance, and Vc is the volume of the central compartment (L). Kcp, Kpc, KcELF and KELFc are the first-order inter-compartmental rate constants between the central and peripheral and central and ELF compartments. Covariates were not included in the structural model.
Elimination and movement of drug to and from the central compartment to the peripheral or ELF compartments was a first-order process. The pharmacokinetic data were weighted by the inverse of the measured assay variance for both piperacillin and tazobactam. Samples with drug concentration below the limit of assay quantification were excluded from analysis. A polynomial describing the assay variance was derived from regression of the measured mean drug concentrations and the standard deviation for samples with known high and low piperacillin and tazobactam concentrations. The means, medians, and standard deviations of the population parameters were estimated. Bayesian posterior estimates for each parameter were also obtained for each patient (using the “population of one” utility in NPAG). Scatter plots of observed versus predicted piperacillin concentrations were examined for the population as a whole and for individual patients. The fit of the structural model to the data were assessed in the following way: (a) the log-likelihood value; (b) the coefficients of determination (r2), slope and y-intercept from regression of the observed- predicted plots before and after the Bayesian step; and (c) the Akaike information criterion (AIC).
Inter-compartmental clearance and the volume of the peripheral compartment was estimated algebraically using the equation below.
Where Q is the inter-compartmental clearance (in L/hour); Vc and Vp are the volumes of the central and periperpheral compartments, respectively and k12 and k21 are the inter-compartmental rate constants (hr−1).
External validation of the population pharmacokinetic analysis
All simulations were performed in ADPAT 553. Observed data from a previous pharmacokinetic study was used as a validation dataset22. In this study, by Boselli et al22, 40 patients were administered a 30 minute intravenous loading dose of piperacillin-tazobactam 4/0.5 g followed by a daily continuous infusion of either 12/1.5 g or 16/2 g. Three plasma samples (at least 4 hours apart) and one NBL sample were collected after at least 48 hours of piperacillin-tazobactam. Five thousand subjects Monte Carlo simulations were performed of the regimens utilised by Boselli et al22. The parameter estimates (i.e. estimates of clearance, volume etc) from the population pharmacokinetic analysis outlined in this study (rather than the Boselli study) were utilised. The median, 5th, 25th, 75th and 95th centile piperacillin and tazobactam concentration in plasma and ELF from the simulation were plotted. The observed piperacillin and tazobactam concentration in plasma and ELF, from Boselli et al, was overlaid on the simulated data. Visual inspection was made of the ability of the population pharmacokinetic model to predict the validation data.
Simulations to estimate piperacillin-tazobactam exposure in plasma and ELF
Monte Carlo simulation was performed using a 5,000-subject simulation. The mean parameter vector and the full covariance matrix from the population PK analysis was embedded in subroutine PRIOR of the ADAPT5 program53,54. Normal and log-normal parameter distributions were explored in the simulations. The ability to recapitulate the original parameter values and their dispersions was used to select which parameter distribution was selected. For piperacillin and tazobactam the median, 5th-percentile 25th-percentile, 75th-percentile and 95th-percentile total, unbound and ELF concentrations for the population were identified every hour. Again a regimen of piperacillin-tazobactam 4/0.5 grams, administered over 30 minutes, every 8 hours was used for the simulations. The unbound plasma and ELF AUCs, for both drugs, were calculated for the fifth dose (32 to 40 hours after initiation of therapy).
Simulation, for each of the 17 patients, was performed using the Bayesian posterior (individual) parameter estimates (i.e. clearance, volume of the central compartment and inter-compartmental rate constants). A regimen of piperacillin-tazobactam 4/0.5 grams, administered over 30 minutes, every 8 hours was used for the simulations except for the 3 patients administered piperacillin-tazobactam 4/0.5 grams, administered over 30 minutes, every 12 hours due to renal impairment. For both piperacillin and tazobactam the area under the concentration time curve (AUC) was estimated in plasma, for the unbound plasma fraction, and in the total ELF. Protein binding for both piperacillin and tazobactam was assumed to be 30%55. The AUCs were calculated at steady-state (5 doses/32 hours after initiation of therapy for patients with an eGFR≥20ml/min or 4 doses/36 hours after initiation of therapy for patients with an eGFR<20ml/min) . The correlation of total ELF to unbound plasma exposure for both piperacillin and tazobactam were assessed. Similarly the correlation of pulmonary permeability to pulmonary piperacillin and tazobactam penetration ratios was assessed. All correlations were analysed using Spearman rank tes (GraphPad Prism version 5 for Windows, GraphPad Software, San Diego California USA, www.graphpad.com).
Finally a 5,000-subject simulation was performed using piperacillin 4 grams, administered over 30 minutes, every 8 hours. The fraction of simulated subjects who achieved six pre-defined pharmacodynamic targets for a range of MICs from 0.5 to 128 mg/L was determined. The pharmacodynamic targets, assumed to be relevant in critically ill patients, were an unbound plasma or ELF piperacillin concentration above the MIC for 50% of the dosing interval (50% fT>MIC), 100% of the dosing interval (100% fT>MIC) or a trough piperacillin concentration to MIC ratio of ≥ 3.4. The cumulative response of patients, with a range of MICs defined as susceptible to piperacillin and achieving each of the pharmacodynamic targets was estimated using a published MIC distribution for organisms causing hospital-acquired and ventilator-associated pneumonia26.
Supplementary Material
Study highlights.
• What is the current knowledge on the topic?
Studies of healthy volunteers show that piperacillin and tazobactam exposure in the lung is approximately 50% of the piperacillin and tazobactam exposure in plasma. There is a paucity of data describing piperacillin and tazobactam penetration in lung of critically ill patients administered standard bolus regimens of piperacillin and tazobactam.
• What question this study addressed?
This study assessed piperacillin and tazobactam plasma and intra-pulmonary pharmacokinetics. Factors influencing pulmonary penetration of piperacillin and tazobactam were investigated.
• What this study adds to our knowledge?
Intra-pulmonary piperacillin and tazobactam exposure is highly variable and unrelated to plasma piperacillin and tazobactam exposure or pulmonary permeability.
• How this might change clinical pharmacology and therapeutics?
Dose optimisation following therapeutic drug monitoring of pulmonary piperacillin and tazobactam concentrations may improve outcomes in patients with pneumonia.
Acknowledgments
Conflict of interest/Disclosure: Dr Felton is a MRC Clinical Training Fellow supported by the North West England Medical Research Council Fellowship Scheme in Clinical Pharmacology and Therapeutics, which is funded by the Medical Research Council (grant number G1000417/94909), ICON, GlaxoSmithKline, AstraZeneca and the Medical Evaluation Unit. Professor Hope is supported by a Clinician Scientist Fellowship from the National Institute of Health Research (NIHR).
The authors would like to acknowledge the support of the National Institute for Health Research Greater Manchester Comprehensive Local Research Network and the University Hospital of South Manchester NHS Foundation Trust.
This report is independent research supported by the National Institute for Health Research Clinical Research Facility at University Hospital of South Manchester NHS Foundation Trust. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
References
- 1.Vincent J-L, et al. Sepsis in European intensive care units: results of the SOAP study. Crit. Care Med. 2006;34:344–53. doi: 10.1097/01.ccm.0000194725.48928.3a. [DOI] [PubMed] [Google Scholar]
- 2.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N. Engl. J. Med. 2003;348:1546–54. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 3.Vincent JL, et al. International Study of the Prevalence and Outcomes of Infection in Intensive Care Units. JAMA. 2009;302:2323–2329. doi: 10.1001/jama.2009.1754. [DOI] [PubMed] [Google Scholar]
- 4.Melsen WG, et al. Attributable mortality of ventilator-associated pneumonia: a meta-analysis of individual patient data from randomised prevention studies. Lancet Infect. Dis. 2013;13:665–71. doi: 10.1016/S1473-3099(13)70081-1. [DOI] [PubMed] [Google Scholar]
- 5.Kollef MH, et al. Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest. 2005;128:3854–62. doi: 10.1378/chest.128.6.3854. [DOI] [PubMed] [Google Scholar]
- 6.Kollef MH. Inadequate Antimicrobial Treatment of Infections: A Risk Factor for Hospital Mortality Among Critically Ill Patients. Chest. 1999;115:462–474. doi: 10.1378/chest.115.2.462. [DOI] [PubMed] [Google Scholar]
- 7.Patel N, Scheetz MH, Drusano GL, Lodise TP. Identification of optimal renal dosage adjustments for traditional and extended-infusion piperacillin-tazobactam dosing regimens in hospitalized patients. Antimicrob. Agents Chemother. 2010;54:460–5. doi: 10.1128/AAC.00296-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Udy A. a, Roberts J. a, Lipman J. Clinical implications of antibiotic pharmacokinetic principles in the critically ill. Intensive Care Med. 2013;39:2070–82. doi: 10.1007/s00134-013-3088-4. [DOI] [PubMed] [Google Scholar]
- 9.Felton TW, et al. Population pharmacokinetics of extended-infusion piperacillin tazobactam in hospitalized patients with nosocomial infections. Antimicrob. Agents Chemother. 2012;56:4087–94. doi: 10.1128/AAC.00521-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hayashi Y, Roberts JA, Paterson DL, Lipman J. Pharmacokinetic evaluation of piperacillin-tazobactam. Expert Opin. Drug Metab. Toxicol. 2010;6:1017–31. doi: 10.1517/17425255.2010.506187. [DOI] [PubMed] [Google Scholar]
- 11.Malacarne P, Rossi C, Bertolini G. Antibiotic usage in intensive care units: a pharmaco-epidemiological multicentre study. J. Antimicrob. Chemother. 2004;54:221–4. doi: 10.1093/jac/dkh299. [DOI] [PubMed] [Google Scholar]
- 12.Craig WA. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin. Infect. Dis. 1998;26:1–10. doi: 10.1086/516284. [DOI] [PubMed] [Google Scholar]
- 13.Drusano GL. Antimicrobial pharmacodynamics: critical interactions of “bug and drug”. Nat. Rev. Microbiol. 2004;2:289–300. doi: 10.1038/nrmicro862. [DOI] [PubMed] [Google Scholar]
- 14.McKinnon PS, Paladino JA, Schentag JJ. Evaluation of area under the inhibitory curve (AUIC) and time above the minimum inhibitory concentration (T>MIC) as predictors of outcome for cefepime and ceftazidime in serious bacterial infections. Int. J. Antimicrob. Agents. 2008;31:345–51. doi: 10.1016/j.ijantimicag.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 15.Boucher HW, et al. Bad bugs, no drugs: no ESKAPE An update from the Infectious Diseases Society of America. Clin. Infect. Dis. 2009;48:1–12. doi: 10.1086/595011. [DOI] [PubMed] [Google Scholar]
- 16.Felton TW, et al. Impact of Bolus Dosing versus Continuous Infusion of Piperacillin and Tazobactam on the Development of Antimicrobial Resistance in Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 2013;57:5811–5819. doi: 10.1128/AAC.00867-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ambrose PG, Bhavnani SM, Ellis-Grosse EJ, Drusano GL. Pharmacokinetic-pharmacodynamic considerations in the design of hospital-acquired or ventilator-associated bacterial pneumonia studies: look before you leap. Clin. Infect. Dis. 2010;51(Suppl 1):S103–10. doi: 10.1086/653057. [DOI] [PubMed] [Google Scholar]
- 18.Rodvold K. a, George JM, Yoo L. Penetration of anti-infective agents into pulmonary epithelial lining fluid: focus on antibacterial agents. Clin. Pharmacokinet. 2011;50:637–64. doi: 10.2165/11594090-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 19.Drusano GL. Infection site concentrations: their therapeutic importance and the macrolide and macrolide-like class of antibiotics. Pharmacotherapy. 2005;25:150S–158S. doi: 10.1592/phco.2005.25.12part2.150S. [DOI] [PubMed] [Google Scholar]
- 20.Rodvold K. a, et al. Identifying exposure targets for treatment of staphylococcal pneumonia with ceftobiprole. Antimicrob. Agents Chemother. 2009;53:3294–301. doi: 10.1128/AAC.00144-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chandorkar G, Huntington J. a, Gotfried MH, Rodvold K. a, Umeh O. Intrapulmonary penetration of ceftolozane/tazobactam and piperacillin/tazobactam in healthy adult subjects. J. Antimicrob. Chemother. 2012;67:2463–9. doi: 10.1093/jac/dks246. [DOI] [PubMed] [Google Scholar]
- 22.Boselli E, et al. Alveolar concentrations of piperacillin/tazobactam administered in continuous infusion to patients with ventilator-associated pneumonia. Crit. Care Med. 2008;36:1500–6. doi: 10.1097/CCM.0b013e318170ba21. [DOI] [PubMed] [Google Scholar]
- 23.Boselli E, et al. Steady-state plasma and intrapulmonary concentrations of piperacillin/tazobactam 4 g/0.5 g administered to critically ill patients with severe nosocomial pneumonia. Intensive Care Med. 2004;30:976–9. doi: 10.1007/s00134-004-2222-8. [DOI] [PubMed] [Google Scholar]
- 24.European Committee on Antimicrobial Susceptibility Testing EUCAST MIC Distribution Piperacillin-tazobactam / Pseudomonas aeruginosa. 2013 http://mic.eucast.org/Eucast2/regShow.jsp?Id=6919#histogram_data.
- 25.Clinical and Laboratory Standards Institute Performance Standards for Antimicrobial Susceptibility Testing; Twenty-First Informational Supplement. 2013. (CLSI document M100-S23).
- 26.Masterton RG, et al. Guidelines for the management of hospital-acquired pneumonia in the UK: report of the working party on hospital-acquired pneumonia of the British Society for Antimicrobial Chemotherapy. J. Antimicrob. Chemother. 2008;62:5–34. doi: 10.1093/jac/dkn162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lodise TP, Lomaestro BM, Rodvold KA, Danziger LH, Drusano GL. Pharmacodynamic profiling of piperacillin in the presence of tazobactam in patients through the use of population pharmacokinetic models and Monte Carlo simulation. Antimicrob. Agents Chemother. 2004;48:4718–4724. doi: 10.1128/AAC.48.12.4718-4724.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roberts J. a, Kirkpatrick CMJ, Roberts MS, Dalley AJ, Lipman J. First-dose and steady-state population pharmacokinetics and pharmacodynamics of piperacillin by continuous or intermittent dosing in critically ill patients with sepsis. Int. J. Antimicrob. Agents. 2010;35:156–63. doi: 10.1016/j.ijantimicag.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 29.Honeybourne D. Antibiotic penetration into lung tissues. Thorax. 1994;49:104–6. doi: 10.1136/thx.49.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barza M, Cuchural G. General principles of antibiotic tissue penetration. J. Antimicrob. Chemother. 1985;15(Suppl A):59–75. doi: 10.1093/jac/15.suppl_a.59. [DOI] [PubMed] [Google Scholar]
- 31.Ulldemolins M, Roberts JA, Wallis SC, Rello J, Lipman J. Flucloxacillin dosing in critically ill patients with hypoalbuminaemia: special emphasis on unbound pharmacokinetics. J. Antimicrob. Chemother. 2010;65:1771–8. doi: 10.1093/jac/dkq184. [DOI] [PubMed] [Google Scholar]
- 32.Pennington JE. Penetration of antibiotics into respiratory secretions. Rev. Infect. Dis. 1981;3:67–73. doi: 10.1093/clinids/3.1.67. [DOI] [PubMed] [Google Scholar]
- 33.Holter JF, Weiland JE, Pacht ER, Gadek JE, Davis WB. Protein permeability in the adult respiratory distress syndrome. Loss of size selectivity of the alveolar epithelium. J. Clin. Invest. 1986;78:1513–22. doi: 10.1172/JCI112743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lamer C, et al. Analysis of vancomycin entry into pulmonary lining fluid by bronchoalveolar lavage in critically ill patients. Antimicrob. Agents Chemother. 1993;37:281–6. doi: 10.1128/aac.37.2.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brink AJ, Richards GA, Schillack V, Kiem S, Schentag J. Pharmacokinetics of once-daily dosing of ertapenem in critically ill patients with severe sepsis. Int. J. Antimicrob. Agents. 2009;33:432–6. doi: 10.1016/j.ijantimicag.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 36.Burkhardt O, et al. Ertapenem in critically ill patients with early-onset ventilator-associated pneumonia: pharmacokinetics with special consideration of free-drug concentration. J. Antimicrob. Chemother. 2007;59:277–84. doi: 10.1093/jac/dkl485. [DOI] [PubMed] [Google Scholar]
- 37.Yamazaki K, Ogura S, Ishizaka A, Oh-hara T, Nishimura M. Bronchoscopic microsampling method for measuring drug concentration in epithelial lining fluid. Am. J. Respir. Crit. Care Med. 2003;168:1304–7. doi: 10.1164/rccm.200301-111OC. [DOI] [PubMed] [Google Scholar]
- 38.Dargaville PA, South M, Vervaart P, Dougall PN. Validity of markers of dilution in small volume lung lavage. Am J Respir Crit Care Med. 1999;160:778–784. doi: 10.1164/ajrccm.160.3.9811049. [DOI] [PubMed] [Google Scholar]
- 39.Burckhardt G, Burckhardt BC. In vitro and in vivo evidence of the importance of organic anion transporters (OATs) in drug therapy. Handb. Exp. Pharmacol. 2011;201:29–104. doi: 10.1007/978-3-642-14541-4_2. [DOI] [PubMed] [Google Scholar]
- 40.Kiem S, Schentag JJ. Interpretation of antibiotic concentration ratios measured in epithelial lining fluid. Antimicrob. Agents Chemother. 2008;52:24–36. doi: 10.1128/AAC.00133-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dhanani J, et al. Antimicrobial chemotherapy and lung microdialysis: a review. Int. J. Antimicrob. Agents. 2010;36:491–500. doi: 10.1016/j.ijantimicag.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 42.Boselli E, et al. Reliability of mini-bronchoalveolar lavage for the measurement of epithelial lining fluid concentrations of tobramycin in critically ill patients. Intensive Care Med. 2007;33:1519–23. doi: 10.1007/s00134-007-0688-x. [DOI] [PubMed] [Google Scholar]
- 43.Drawz SM, Bonomo R. a. Three decades of beta-lactamase inhibitors. Clin. Microbiol. Rev. 2010;23:160–201. doi: 10.1128/CMR.00037-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jones RN, Barry AL. Studies to optimize the in vitro testing of piperacillin combined with tazobactam (YTR 830) Diagn. Microbiol. Infect. Dis. 12:495–510. doi: 10.1016/0732-8893(89)90084-9. [DOI] [PubMed] [Google Scholar]
- 45.Aronoff SC, Jacobs MR, Johenning S, Yamabe S. Comparative activities of the beta-lactamase inhibitors YTR 830, sodium clavulanate, and sulbactam combined with amoxicillin or ampicillin. Antimicrob. Agents Chemother. 1984;26:580–2. doi: 10.1128/aac.26.4.580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jacobs MR, Aronoff SC, Johenning S, Shlaes DM, Yamabe S. Comparative activities of the beta-lactamase inhibitors YTR 830, clavulanate, and sulbactam combined with ampicillin and broad-spectrum penicillins against defined beta-lactamase-producing aerobic gram-negative bacilli. Antimicrob. Agents Chemother. 1986;29:980–5. doi: 10.1128/aac.29.6.980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vanscoy B, et al. Pharmacological basis of β-lactamase inhibitor therapeutics: tazobactam in combination with Ceftolozane. Antimicrob. Agents Chemother. 2013;57:5924–30. doi: 10.1128/AAC.00656-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Craig WA, Andes DR. In vivo activities of ceftolozane, a new cephalosporin, with and without tazobactam against Pseudomonas aeruginosa and Enterobacteriaceae, including strains with extended-spectrum β-lactamases, in the thighs of neutropenic mice. Antimicrob. Agents Chemother. 2013;57:1577–82. doi: 10.1128/AAC.01590-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Strayer AH, et al. Pharmacodynamics of piperacillin alone and in combination with tazobactam against piperacillin-resistant and -susceptible organisms in an in vitro model of infection. Antimicrob. Agents Chemother. 1994;38:2351–6. doi: 10.1128/aac.38.10.2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lister PD, Prevan a M., Sanders CC. Importance of beta-lactamase inhibitor pharmacokinetics in the pharmacodynamics of inhibitor-drug combinations: studies with piperacillin-tazobactam and piperacillin-sulbactam. Antimicrob. Agents Chemother. 1997;41:721–7. doi: 10.1128/aac.41.4.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Leleu G, Kitzis MD, Vallois JM, Gutmann L, Decazes JM. Different ratios of the piperacillin-tazobactam combination for treatment of experimental meningitis due to Klebsiella pneumoniae producing the TEM-3 extended-spectrum beta-lactamase. Antimicrob. Agents Chemother. 1994;38:195–9. doi: 10.1128/aac.38.2.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Neely MN, Guilder M. G. van, Yamada WM, Schumitzky A, Jelliffe RW. Accurate detection of outliers and subpopulations with Pmetrics, a nonparametric and parametric pharmacometric modeling and simulation package for R. Ther. Drug Monit. 2012;34:467–76. doi: 10.1097/FTD.0b013e31825c4ba6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.D’Argenio DZ, Schumitzky A, Xiaoning W. ADAPT 5 User’s Guide: Pharmacokinetic/Pharmacodynamic Systems Analysis Software. 2009.
- 54.D’Argenio DZ, Schumitzky A. A program package for simulation and parameter estimation in pharmacokinetic systems. Comput. Programs Biomed. 1979;9:115–34. doi: 10.1016/0010-468x(79)90025-4. [DOI] [PubMed] [Google Scholar]
- 55.Sörgel F, Kinzig M. The chemistry, pharmacokinetics and tissue distribution of piperacillin/tazobactam. J. Antimicrob. Chemother. 1993;31(Suppl A):39–60. doi: 10.1093/jac/31.suppl_a.39. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.