Abstract
Background
Lumiracoxib is a selective cyclooxygenase-2 (COX-2) inhibitor. COX-2 inhibitors were developed to avoid COX-1-related gastrointestinal (GI) problems while maintaining the analgesic and anti-inflammatory activity of traditional non-steriodal anti-inflammatory drugs (NSAIDs).
Objectives
To review the analgesic efficacy, duration of analgesia, and adverse effects of a single oral dose of lumiracoxib for moderate to severe postoperative pain in adults.
Search methods
We searched Cochrane CENTRAL, MEDLINE, and EMBASE to February 2010.
Selection criteria
Single oral dose, randomised, double-blind, placebo-controlled trials of lumiracoxib for relief of established moderate to severe postoperative pain in adults.
Data collection and analysis
Studies were assessed for methodological quality and the data extracted by two review authors independently. Summed total pain relief over six hours (TOTPAR 6) was used to calculate the number of participants achieving at least 50% pain relief. These derived results were used to calculate, with 95% confidence intervals, the relative benefit compared to placebo, and the number needed to treat (NNT) for one participant to experience at least 50% pain relief over six hours. Numbers of participants using rescue medication, and time to use of rescue medication, were sought as additional measures of efficacy. Information on adverse events and withdrawals was collected.
Main results
In this updated review four studies met the inclusion criteria. In total 366 participants were treated with lumiracoxib 400 mg, 51 with lumiracoxib 100 mg, and 212 with placebo. Active comparators were naproxen 500 mg, rofecoxib 50 mg, celecoxib 200 mg, celecoxib 400 mg, and ibuprofen 400 mg. With lumiracoxib 400 mg 50% of participants had at least 50% pain relief over six hours, compared with 8% given placebo; RB 6.9 (95% CI 4.1 to 12), NNT 2.4 (2.1 to 2.8).
Median time to onset of analgesia was shorter for lumiracoxib 400 mg (0.6 to 1.5 hours) than placebo (>12 hours). Fewer participants needed rescue medication with lumiracoxib (64%) than with placebo (91%) over 12 to 24 hours; NNT to prevent remedication 3.7 (2.9 to 5.0). The weighted median time to use of rescue medication was 9.4 hours for lumiracoxib 400 mg and 1.7 hours for placebo.
Adverse events were generally mild to moderate in severity, with one serious event reported in a placebo patient.
Authors’ conclusions
Lumiracoxib 400 mg given as a single oral dose is an effective analgesic for acute postoperative pain, and has a relatively long duration of action. Adverse events with lumiracoxib did not differ from placebo.
Medical Subject Headings (MeSH): Acute Disease; Administration, Oral; Cyclooxygenase 2 Inhibitors [*administration & dosage]; Diclofenac [administration & dosage; *analogs & derivatives]; Pain, Postoperative [*drug therapy]; Randomized Controlled Trials as Topic; Time Factors
MeSH check words: Adult, Humans
BACKGROUND
This is an update of Single dose lumiracoxib for acute postoperative pain, published in The Cochrane Library in Issue 4, 2007 (Roy 2007). The title has been changed to reflect that the review considered only studies in adults.
Acute pain occurs as a result of tissue damage either accidentally due to an injury or as a result of surgery. Acute postoperative pain is a manifestation of inflammation due to tissue injury. The management of postoperative pain and inflammation is a critical component of patient care.
This is one of a series of reviews whose aim is to increase awareness of the range of analgesics that are potentially available, and present evidence for relative analgesic efficacy through indirect comparisons with placebo, in very similar trials performed in a standard manner, with very similar outcomes, and over the same duration. Such relative analgesic efficacy does not in itself determine choice of drug for any situation or patient, but guides policy-making at the local level. The series includes well established analgesics such as paracetamol (Toms 2008), naproxen (Derry C 2009a), diclofenac (Derry P 2009), and ibuprofen (Derry C 2009b), newer cyclooxygenase-2 selective analgesics, such as celecoxib (Derry 2008), etoricoxib (Clarke 2009), and parecoxib (Lloyd 2009), and opioid/paracetamol combinations, such as paracetamol and codeine (Toms 2009).
Acute pain trials
Single dose trials in acute pain are commonly short in duration, rarely lasting longer than 12 hours. The numbers of participants are small, allowing no reliable conclusions to be drawn about safety. To show that the analgesic is working, it is necessary to use placebo (McQuay 2005). There are clear ethical considerations in doing this. These ethical considerations are answered by using acute pain situations where the pain is expected to go away, and by providing additional analgesia, commonly called rescue analgesia, if the pain has not diminished after about an hour. This is reasonable, because not all participants given an analgesic will have significant pain relief. Approximately 18% of participants given placebo will have significant pain relief (Moore 2006), and up to 50% may have inadequate analgesia with active medicines. The use of additional or rescue analgesia is hence important for all participants in the trials.
Clinical trials measuring the efficacy of analgesics in acute pain have been standardised over many years. Trials have to be randomised and double blind. Typically, in the first few hours or days after an operation, patients develop pain that is moderate to severe in intensity, and will then be given the test analgesic or placebo. Pain is measured using standard pain intensity scales immediately before the intervention, and then using pain intensity and pain relief scales over the following 4 to 6 hours for shorter acting drugs, and up to 12 or 24 hours for longer acting drugs. Pain relief of half the maximum possible pain relief or better (at least 50% pain relief) is typically regarded as a clinically useful outcome. For patients given rescue medication it is usual for no additional pain measurements to be made, and for all subsequent measures to be recorded as initial pain intensity or baseline (zero) pain relief (baseline observation carried forward). This process ensures that analgesia from the rescue medication is not wrongly ascribed to the test intervention. In some trials the last observation is carried forward, which gives an inflated response for the test intervention compared to placebo, but the effect has been shown to be negligible over 4 to 6 hours (Moore 2005a). Patients usually remain in the hospital or clinic for at least the first 6 hours following the intervention, with measurements supervised, although they may then be allowed home to make their own measurements in trials of longer duration.
NSAIDs have pain-relieving, antipyretic and anti-inflammatory properties, and have proven efficacy following day surgery and minor surgery. They reversibly inhibit cyclooxygenase (prostaglandin endoperoxide synthase), the enzyme mediating production of prostaglandins (PGs) and thromboxane A2 (Fitzgerald 2001; Hawkey 1999). A major concern regarding the use of traditional NSAIDs, such as ibuprofen, naproxen and diclofenac, postoperatively is the possibility of bleeding from both the operative site (because of the inhibition of platelet aggregation) (Forrest 2002) and from the upper gastrointestinal tract, (especially in patients stressed by surgery, the elderly, frail, or dehydrated). Drug treatments that combine the pain-relieving properties of NSAIDs without these adverse effects are likely to have a place in clinical practice.
Selective cyclo-oxygenase-2 (COX-2) inhibitors were developed to address the problem of upper gastrointestinal bleeding (Hawkey 2001). NSAIDs are thought to relieve pain by inhibiting cyclo-oxygenases and thus the production of prostaglandins. Prostaglandins occur throughout body tissues and fluids and act to stimulate pain nerve endings and promote/inhibit the aggregation of blood platelets. Cyclo-oxygenase has at least two isoforms: COX-1 and COX-2. COX-1 is constitutive while COX-2 is induced at sites of inflammation and produces the prostaglandins involved in inflammatory responses and pain mediation (Grahame-Smith 2002). Unlike traditional NSAIDs, COX-2 inhibitors block primarily the action of COX-2 and cause fewer gastrointestinal effects (Moore 2005b). In common with other NSAIDs, COX-2 inhibitors can give rise to fluid retention and renal damage (Garner 2002), so particular caution is needed in the elderly (Hawkey 2001). They have also been associated with increased cardiovascular problems, mainly in trials in patients with pre-cancerous colorectal polyps. (Kearney 2006; Patrono 2009). Use of coxibs and non-selective NSAIDs in patients with bowel problems such as ulcerative colitis and Crohn’s Disease is complicated (Hawkey 2006).
Lumiracoxib (Prexige®) is a novel selective COX-2 inhibitor with claimed improved biochemical selectivity over that of currently available coxibs (Mysler 2004). It is structurally distinct from other COX-2 selective inhibitors in that it has mildly acidic properties (pKa 4.7). This acidity may be the reason for its distinct pharmacokinetic and pharmacodynamic profile, as weak acids have been shown to be readily sequestered into acidic environments such as inflamed joints (Day 1988). It is used for the symptomatic relief of osteoarthritis at 100 to 200 mg/day with clinical efficacy similar to that of diclofenac 150 mg/day and celecoxib 200 mg/day. Patients with rheumatoid arthritis benefit from a daily dose of 200 to 400 mg daily. Furthermore, it has been found to be effective for acute pain associated with primary dysmenorrhoea, dental surgery and orthopaedic surgery, at a dose of 400 mg daily (Bannwarth 2005). Lumiracoxib is believed to be as effective as traditional NSAIDs but is thought to have superior gastrointestinal safety, especially in the reduction of ulcer complications (Schnitzer 2004a). In 2007 lumiracoxib was withdrawn from the Australian market because of concerns about liver damage, and a number of other countries have since withdrawn it. Lumiracoxib has never been licensed in the USA, but is available in some countries in south and central America.
Since the original review was published in 2007, another relevant study has been published (previously in “ongoing studies”). Inclusion of this study in the review substantially increases the number of participants treated with lumiracoxib, providing more confidence in the results.
OBJECTIVES
To evaluate the analgesic efficacy and safety of lumiracoxib in the treatment of acute postoperative pain, using methods that permit comparison with other analgesics evaluated in the same way, and criteria of efficacy recommended by an in-depth study at the individual patient level (Moore 2005a).
METHODS
Criteria for considering studies for this review
Types of studies
Reports were included if they were published randomised placebo controlled, double blind trials of a single oral dose of lumiracoxib, with a minimum of 10 participants per treatment arm. Multiple dose studies were included if appropriate data from the first dose were available, and cross-over studies were included provided that data from the first arm were presented separately.
Abstracts, review articles, case reports, and clinical observations were excluded, as were reports that did not clearly state that the interventions had been randomly allocated, were concerned with other pain conditions, or used experimental pain or volunteer participants, or both.
Types of participants
Male or female patients (aged 15 years and above) experiencing postoperative pain of moderate to severe intensity, which is defined as ≥3 on a 4 point categorical scale or ≥30 mm on a 100 mm Visual Analogue Scale (VAS).
Types of interventions
Single dose oral lumiracoxib or placebo administered postoperatively when pain intensity was moderate or severe.
Types of outcome measures
Data were collected on the following outcomes:
patient characteristics;
pain model (dental or other type of surgery);
patient reported pain at baseline (physician, nurse, or carer reported pain will not be included in the analysis);
Patient-reported pain relief and/or pain intensity expressed hourly over four to six hours using validated pain scales (pain intensity and pain relief in the form of visual analogue scales (VAS) or categorical scales, or both), or reported total pain relief (TOTPAR) or summed pain intensity difference (SPID) at four to six hours;
number of participants using rescue medication;
time to use of rescue medication, and the time of assessment;
withdrawals - all cause, adverse event;
adverse events - participants experiencing one or more, and any serious adverse event, and the time of assessment.
Search methods for identification of studies
We searched the following databases:
Cochrane CENTRAL, Issue 1 2006 for the original review and March 2010 for the update;
MEDLINE (via OVID), 1966 to February 2007 for the original review and March 2010 for the update;
EMBASE (via OVID), 1974 to February 2007 for the original review and March 2010 for the update;
PaPaS Trials Register, February 2007 for the original review and March 2010 for the update
Reference lists of retrieved studies were also manually searched. Search strategies for MEDLINE, EMBASE and CENTRAL can be found in Appendix 1, Appendix 2 and Appendix 3 respectively.
Language
No language restriction was applied.
Additional sources
For the original review, authors of the included studies were contacted for additional numerical data, but none was supplied. The manufacturer of lumiracoxib (Norvatis Pharmaceuticals Corporation) was also contacted for further published or unpublished trials and abstracts. They provided information on two new ongoing trials, and also supplied additional data for the included studies. One of the ongoing trials has been published and is now included in this update. We are unable to find the other trial, but it may be a study comparing pre- and postoperative administration of lumiracoxib in knee arthroscopy, which would not qualify for inclusion in this review.
No further unpublished studies were identified in www.clinicaltrials.gov for the update.
Data collection and analysis
Two review authors independently carried out searches, reviewed the titles and abstracts retrieved, and agreed upon the reports that would be retrieved in full for assessment for inclusion in the review. Disagreements were resolved by discussion with the third author.
Quality Assessment
Two review authors independently assessed the included studies for quality using a five-point scale (Jadad 1996).
The scale used is as follows:
Is the study randomised? If yes - one point;
Is the randomisation procedure reported and is it appropriate? If yes add one point, if no deduct one point;
Is the study double blind? If yes then add one point;
Is the double blind method reported and is it appropriate? If yes add 1 point, if no deduct one point;
Are the reasons for patient withdrawals and dropouts described? If yes add one point.
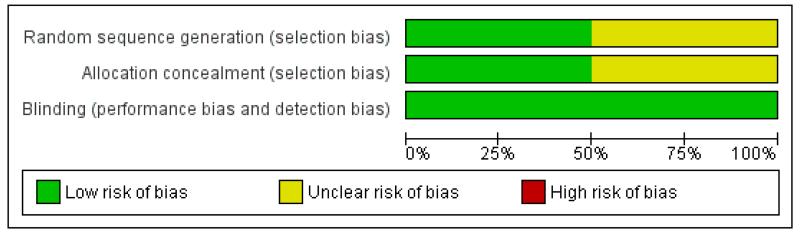
A Risk of bias table was completed for the categories of randomisation, allocation concealment and blinding.
Data management
Data were extracted by two of the review authors and recorded on a standard data extraction form. Data suitable for pooling were entered into RevMan 5.0.
Data analysis
QUOROM guidelines were followed where appropriate (Moher 1999). For efficacy analyses we used the number of participants in each treatment group who were randomised, received medication, and provided at least one post-baseline assessment. For safety analyses we used number of participants randomised to each treatment group. Analyses were planned for different doses (where there were at least 200 participants). Sensitivity analyses were planned for pain model (dental versus other postoperative pain), trial size (39 or fewer versus 40 or more per treatment arm), and quality score (2 versus 3 or more).
Primary outcome: Number of participants achieving at least 50% pain relief
For each study, mean TOTPAR (total pain relief) or SPID (summed pain intensity difference) for active and placebo groups were converted to %maxTOTPAR or %maxSPID by division into the calculated maximum value (Cooper 1991). The proportion of participants in each treatment group who achieved at least 50%maxTOTPAR was calculated using verified equations (Moore 1996; Moore 1997a; Moore 1997b). These proportions were then converted into the number of participants achieving at least 50%maxTOTPAR by multiplying by the total number of participants in the treatment group. Information on the number of participants with at least 50%maxTOTPAR for active treatment and placebo was then used to calculate relative benefit (RR) and number needed to treat to benefit (NNT).
Pain measures accepted for the calculation of TOTPAR or SPID were:
five-point categorical pain relief (PR) scales with comparable wording to “none, slight, moderate, good or complete”;
four-point categorical pain intensity (PI) scales with comparable wording to “none, mild, moderate, severe”;
Visual analogue scales (VAS) for pain relief;
VAS for pain intensity;
five-point categorical global scale with the wording “poor, fair, good, very good, excellent” (Collins 2001).
Secondary outcomes
1. Use of rescue medication
Numbers of participants requiring rescue medication were used to calculate NNTs to prevent use of rescue medication for treatment and placebo groups. Median (or mean) time to use of rescue medication was used to calculate the weighted mean of the median (or mean) for the outcome. Weighting was by number of participants.
2. Adverse events
Numbers of participants reporting adverse events for each treatment group were used to calculate relative risk (RR) and numbers needed to treat to harm (NNH) estimates for:
any adverse event
any serious adverse event (as reported in the study)
withdrawal due to an adverse event
3. Other withdrawals
Withdrawals for reasons other than lack of efficacy (participants using rescue medication - see above) and adverse events were noted.
Relative benefit or risk estimates were calculated with 95% confidence intervals (CI) using a fixed-effect model (Morris 1995). NNT or NNH with 95% CI were calculated using the pooled number of events by the method of Cook and Sackett (Cook 1995). A statistically significant difference from control was assumed when the 95% CI of the relative benefit did not include one.
Homogeneity of studies was assessed visually (L’Abbe 1987). The z test (Tramer 1997) would be used to determine if there was a significant difference between NNTs for different doses of active treatment, or between groups in the sensitivity analyses.
RESULTS
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies.
Searches for the original review identified five studies, and updated searches identified one more. Of these, four studies met the inclusion criteria and were included in the review (Chan 2005; Fricke 2008; Kellstein 2004; Zelenakas 2004). All studies were funded by Novartis Pharmaceuticals, the manufacturer of lumiracoxib, and were identified as potential randomised controlled trials (RCTs) that assessed the effectiveness of lumiracoxib 400 mg in acute postoperative pain compared to placebo. The other two studies were not in postoperative pain and were excluded. The study by Bitner 2004 was a study on the treatment of primary dysmenorrhoea and the study by Schnitzer 2004 was in patients with knee or hip primary osteoarthritis.
Chan 2005 studied postoperative total knee or hip arthroplasty patients with moderate to severe pain. One hundred and eighty patients were recruited, 60 patients received 400 mg single dose lumiracoxib, 60 received 500 mg naproxen, and 60 received placebo. Fricke 2008 studied postoperative dental patients, with third molar extractions who had moderate to severe pain. Three hundred and sixty-four participants were recruited: 156 received lumiracoxib 400 mg, 156 received celecoxib 400 mg, and 52 received placebo.
Kellstein 2004 was also a postoperative dental surgery study, of third molar extraction for patients with moderate to severe pain. Three hundred and fifty five patients were recruited, 101 received lumiracoxib 400 mg, 102 received rofecoxib 50 mg, 101 received celecoxib 200 mg and 51 received placebo.
Zelenakas 2004 was another postoperative dental surgery study, of third molar extraction for patients with moderate to severe pain. Two hundred and two patients were recruited. Fifty received lumiracoxib 400 mg, and 51 received lumiracoxib 100 mg, 51 received ibuprofen 400 mg and 50 received placebo.
All studies used a single dose of study medication, or single dose phase, and all used a parallel group design. One study lasted for 12 hours (Zelenakas 2004), and two (Fricke 2008, Kellstein 2004) for 24 hours, and one had a 12 hour single dose phase followed by a multiple dose phase lasting up to 96 hours (Chan 2005).
Risk of bias in included studies
Two studies (Chan 2005; Fricke 2008) scored 5/5, one (Zelenakas 2004) scored 4/5 and one (Kellstein 2004) scored 3/5 on the Oxford Quality Score. Points were lost due to failure to adequately describe the methods of randomisation, and Kellstein 2004 did not report on withdrawals. Details are in the “Characetistics of included studies” table.
The Risk of bias table did not indicate significant risk of bias in any study (Figure 1).
Figure 1 . Methodological quality graph: review authors’ judgements about each methodological quality item presented as percentages across all included studies.
Effects of interventions
Four studies provided data for analysis. Three studies (Chan 2005; Fricke 2008; Kellstein 2004) assessed one 400 mg single dose of lumiracoxib. The other (Zelenakas 2004) assessed 400 and 100 mg doses. Data analysis was carried out on 366 patients who received lumiracoxib 400 mg, and the 212 patients who received placebo. No analysis was carried out for the 51 participants receiving lumiracoxib 100 mg in Zelenakas 2004, as patient numbers were too small (Moore 1998).
Novartis Pharmaceuticals kindly supplied tables of pain relief over time for three trials (Chan 2005; Kellstein 2004; Zelenakas 2004). Patient data was not available for one patient in each of the lumiracoxib 400 mg and placebo arms of the Chan 2005 study, although these patients completed the study. For efficacy outcomes, these patients were assumed to have not had an event, and the study did not contribute data for adverse event analysis. No study authors supplied any additional information.
Details of efficacy outcomes, and adverse events and withdrawals in individual studies are available in Appendix 5 and Appendix 6 respectively.
Efficacy
Details of efficacy outcomes in individual studies are in Appendix 5, and of adverse events and withdrawals in Appendix 6.
Participants achieving at least 50% pain relief over 6 hours
Lumiracoxib 400 mg versus placebo
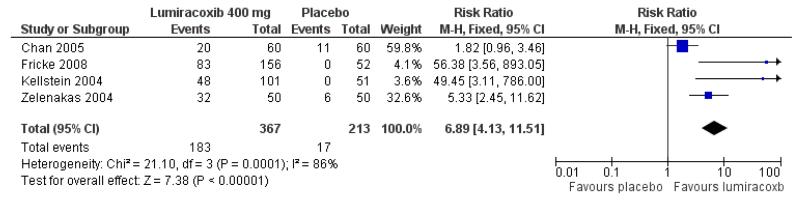
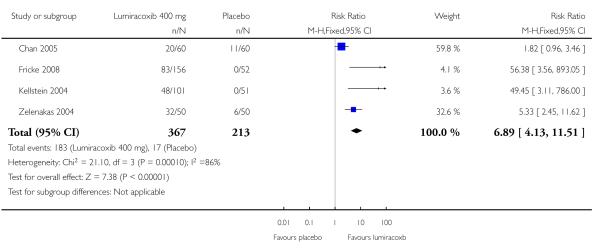
Four studies provided data (Chan 2005; Fricke 2008; Kellstein 2004; Zelenakas 2004); 336 participants were treated with lumiracoxib 400 mg and 212 with placebo (Figure 2).
Figure 2 . Forest plot of comparison: 1 Lumiracoxib versus placebo, outcome: 1.1 Participants with at least 50% pain relief at 6 hours.
The proportion of participants experiencing at least 50% pain relief over six hours with lumiracoxib 400 mg was 50% (183/366).
The proportion of participants experiencing at least 50% pain relief over six hours with placebo was 8% (17/212).
The relative benefit of treatment compared with placebo was 6.9 (4.1 to 11).
The NNT for at least 50% pain relief over six hours for lumiracoxib 400 mg compared with placebo was 2.4 (2.1 to 2.8).
For every five participants treated with lumiracoxib 400 mg, two would experience at least 50% pain relief who would not have done so with placebo.
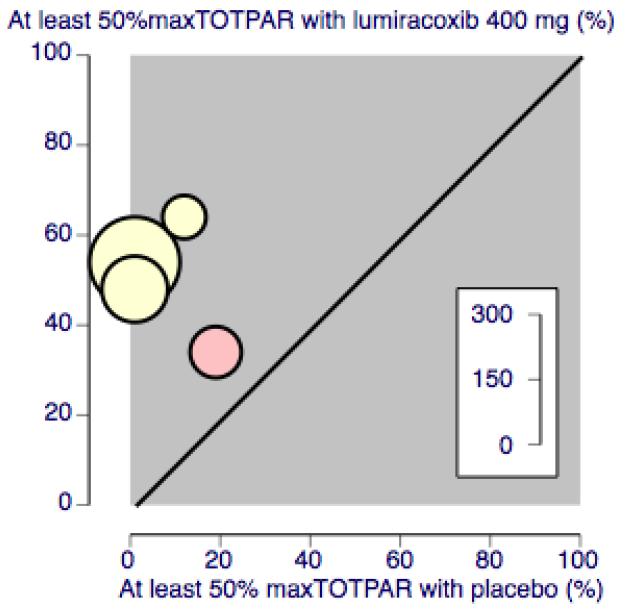
(Figure 3)
Figure 3 . L’Abbé plot of the four trials, with proportion achieving at least 50% pain relief over six hours with lumiracoxib 400 mg and placebo. The size of the symbol is proportional to the size of the study. Yellow = dental studies, pink = orthopaedic study.
Subgroup analysis for pain model
There were insufficient data from non-dental studies to compare the two groups, but removing the study in orthopaedic surgery from the analysis gave a relative benefit of 9.7 (4.3 to 22), and an NNT of 2.1 (1.8 to 2.7).
Sensitivity analyses
All included studies had more than 40 participants in each treatment group, and all scored 3/5 or more on the Oxford Quality Score, so no sensitivity analyses could be carried out for these criteria.
Lumiracoxib versus active comparators
There were insufficient data to allow direct comparison between lumiracoxib 400 mg and any individual active comparator.
Time to onset of analgesia
The median time to onset of analgesia for lumiracoxib 400 mg was 1.5 hours in Chan 2005, 0.6 hours in Fricke 2008, 0.7 hours in Kellstein 2004, and 0.6 hours in Zelenakas 2004. In all studies the median time to onset for placebo was not estimable (>12 hours), because the number of participants achieving onset was too low.
Use of rescue medication
Two studies reported numbers of patients requiring rescue medication within 12 hours (Chan 2005; Zelenakas 2004), and one within 24 hours (Fricke 2008). These were combined for analysis as it was likely that most participants requiring rescue medication following dental surgery would have done so by 12 hours, and the data for Fricke were very similar to the others (Analysis 1.2).
The proportion of participants requiring rescue medication within 12 to 24 hours with lumiracoxib 400 mg was 64% (169/ 266).
The proportion of participants requiring rescue medication within 12 to 24 hours with placebo was 91% (147/162).
The relative risk of treatment compared with placebo was 0.68 (0.61 to 0.76).
The NNT to prevent use of rescue medication within 12 to 24 hours for lumiracoxib 400 mg compared with placebo was 3.7 (2.9 to 5.0). For every four participants treated with lumiracoxib 400 mg, one would not require rescue medication within 12 to 24 hours who would have done with placebo.
Median time to use of rescue medication was reported for all trials, ranging from 3.8 hours to >12 hours for lumiracoxib 400 mg, and 1.3 to 2 hours for placebo. The weighted mean of the median time to use of rescue medication was 9.4 hours for lumiracoxib 400 mg and 1.7 for placebo. The short time of 3.8 hours reported in Chan 2005 may reflect that this study was carried out in orthopaedic patients, while the others were in dental patients. For dental studies only the median time to use of rescue medication was 10.5 hours with lumiracoxib 400 mg.
Patient global assessment
All studies used a four point scale (poor, fair, good and excellent). The numbers of patients reporting ’excellent’ at 12 hours were 116/366 (32%) for lumiracoxib and 6/213 (3%) for placebo.
Adverse events and withdrawals
One study (Chan 2005) appeared to report adverse events only at 96 hours, after a multiple dose phase, so provided no data for this analysis. Details of methods used to collect adverse events (spontaneous report, open question list) were not consistently reported. Three studies (Fricke 2008; Kellstein 2004; Zelenakas 2004, 252 participants) provided information on numbers of patients with one or more adverse events (Analysis 1.3).
The proportion of participants experiencing at least one adverse event with lumiracoxib 400 mg was 15% (22/151);
The proportion of participants experiencing at least one adverse event with placebo was 19% (19/101);
The relative benefit of treatment compared with placebo was 0.69 (0.37 to 1.27);
The NNT was not calculated.
There was only one withdrawal due to an adverse event, in a patient given ibuprofen, who had postoperative bleeding at the suture site (Zelenakas 2004). There was no reported adjudication of relationship to the test drug. There was also only one serious adverse event, in a patient given placebo, who had a deep vein thrombosis (DVT) (Zelenakas 2004).
Adverse events were generally described as mild to moderate in severity, and were probably mostly related to the postoperative status of the patients.
DISCUSSION
Summary of main results
This review is an update of an earlier Cochrane review published in 2007, and examines the efficacy of lumiracoxib, a COX-2 inhibitor, in providing postoperative pain relief. Four studies fulfilled inclusion criteria, three following dental surgery (Fricke 2008; Kellstein 2004; Zelenakas 2004), and one (Chan 2005) following orthopaedic surgery. The addition of Fricke 2008 in this update increases the number of participants treated with lumiracoxib 400 mg by 73%, giving greater confidence in results, although the overall findings are not changed. There remain no, or insufficient, data for analysis of doses other than 400 mg.
With lumiracoxib 400 mg, half of participants experienced at least 50% pain relief over 6 hours, compared to less than 10% with placebo; the NNT was 2.4 (2.1 to 2.8). Fewer participants needed rescue medication at any point during the study (12 or 24 hours) with lumiracoxib (64%) than with placebo (91%), and the median time to use of rescue medication was 9.4 hours for lumiracoxib and 1.7 hours for placebo. Results of the four studies were in good agreement (Figure 3), and while results from the study in orthopaedic surgery (Chan 2005) might be taken to suggest that lumiracoxib is less effective in this situation, such a conclusion cannot be drawn with only 118 participants.
Adverse events did not occur more often with lumiracoxib than placebo, and there were no serious adverse events or withdrawals due to adverse events in participants treated with lumiracoxib in these studies.
Indirect comparisons of NNTs for at least 50% pain relief over 4 to 6 hours in reviews of other analgesics using identical methods indicate that lumiracoxib has equivalent efficacy to ibuprofen 400 mg (Derry C 2009b; NNT 2.5 (2.4 to 2.6)), is more effective than paracetamol 1000 mg (Toms 2008; NNT 3.6 (3.4 to 4.0)) and less effective than etoricoxib 120 mg (Clarke 2009; 1.9 (1.7 to 2.1)).
Overall completeness and applicability of evidence
Most of the data came from participants who had third molar dental extractions, who are generally in their early twenties, and otherwise fit and healthy; other patient groups may not give an identical response. There were insufficient data to determine whether type of surgery influenced outcome. A review in 2004 found no systematic difference in analgesic response between dental and other types of surgery (Barden 2004), but this will be addressed in a planned Cochrane overview of analgesics in acute postoperative pain.
Information on adverse events was not reported by all studies, and single dose studies are not designed to investigate drug safety, so the results presented in this review should be interpreted within the context of these studies.
Quality of the evidence
The methodological quality of the included studies was good, with all scoring adequately on the Oxford Quality Score and Cochrane Risk of Bias assessment to avoid risk of bias from randomisation, blinding and withdrawals. All the studies in the review used “last observation carried forward” (LOCF) for missing data, for example when a patient uses rescue medication and provides no further efficacy measurements. This tends to overestimate efficacy compared with placebo, and the degree of overestimation increases with time as more patients use rescue medication, so that analyses over periods greater than six hours become unreliable (Moore 2005a). We chose to analyse pain relief at 6 hours to avoid problems with LOCF, and for comparability with many other reviews. All studies enrolled participants with established pain following surgery, with pain levels sufficient to demonstrate reduction, or otherwise, due to treatment.
All studies were funded by the manufacturer of lumiracoxib. Such involvement does not necessarily imply bias, as long as original data rather than authors’ conclusions are utilised, and study validity is not compromised (Barden 2006); these criteria have been satisfied here.
Potential biases in the review process
The included studies were identified from a comprehensive search of published papers, and standard methods have been used for analysis. We cannot exclude the possibility that undiscovered studies exist that show no benefit, but we can calculate the number of participants in trials of zero benefit (relative risk of 1) that would be required for the absolute benefit to reduce beneficial effects to a negligible amount (Moore 2008). If an NNT of 8 for at least 50% pain relief were considered clinically irrelevant, then there would have to be 1349 participants in zero effect studies. This would require at least 13 studies with 100 participants, and that number of unavailable studies seems unlikely.
Agreements and disagreements with other studies or reviews
We know of no other reviews of lumiracoxib in acute postoperative pain.
AUTHORS’ CONCLUSIONS
Implications for practice
This review has found that lumiracoxib is effective at providing postoperative pain relief in approximately half of adult patients, and is comparable to ibuprofen 400 mg, but with a median time to use of rescue medication it has a longer duration of analgesia. It was not associated with any serious adverse events in this limited data set.
Implications for research
We see no implications for research in the field of single dose acute pain studies. What is lacking are pragmatic studies determining how to ensure that patients achieve clinically relevant, say 50% pain relief, rather than exploratory studies which show that a drug is an analgesic.
In terms of adverse event profiles, this is difficult in a drug like lumiracoxib when it is used for short term studies only. A possible approach might be to study time to event data in large trials of chronic use, although the study population is likely to differ.
PLAIN LANGUAGE SUMMARY.
Single dose oral lumiracoxib (Prexige®) for acute postoperative pain relief in adults
Postoperative pain is often poorly managed. Cyclooxygenase inhibitors (COX-2) pain relieving drugs were developed with the aim of reducing the gastrointestinal side effects of non-steroidal anti-inflammatory drugs (NSAIDs). Lumiracoxib 400 mg provided rapid, effective, and sustained relief of postoperative pain in four studies in dental and orthopaedic surgery. Of 366 participants treated with lumiracoxib 400 mg half experienced a high level of pain relief (at least 50% pain relief over a six hour period), compared with 8% given placebo. The duration of analgesia was relatively long at 9 hours, and fewer participants needed to use rescue medication with lumiracoxib than with placebo. Adverse event data was inconsistently reported, but no serious adverse events occurred in any patient taking lumiracoxib in these studies.
ACKNOWLEDGEMENTS
Novartis Pharmaceuticals were contacted for the initial review and kindly supplied information on two new ongoing trials. They also supplied additional data for the included studies.
SOURCES OF SUPPORT
Internal sources
Oxford Pain Relief Trust, UK.
External sources
NHS Cochrane Collaboration Grant, UK.
NIHR Biomedical Research Centre Programme, UK.
CHARACTERISTICS OF STUDIES
Characteristics of included studies [ordered by study ID]
| Methods | RCT, DB, DD, placebo and active controlled parallel-group study, 12 hour single dose phase, followed by multi-dose phase up to 96 hours. Medication administered when pain intensity was moderate to severe | |
| Participants | Post operative total knee or hip arthroplasty surgery Male and females Mean age 64 years (SD 11.0, range 18 to 80 years) N=180 |
|
| Interventions | Lumiracoxib 400 mg, n = 60 Naproxen 500 mg, n = 60 Placebo, n = 60 |
|
| Outcomes | ≥50% PR over six hours Time to onset of analgesia Use of rescue medication Adverse events Withdrawals |
|
| Notes | Oxford Quality Score: R2, DB2, W1. Total = 5 | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “validated automated system” |
| Allocation concealment (selection bias) | Low risk | Remote allocation |
| Blinding (performance bias and detection bias) All outcomes |
Low risk | “double dummy” |
| Methods | RCT, DB, DD, placebo and active controlled parallel group study, single oral dose. Medication administered when pain intensity was moderate to severe. Study duration 24 hours |
|
| Participants | Post-operative dental surgery, third molar extraction Male and females Mean age 23 years (range 18 to 52 years) N = 364 |
|
| Interventions | Lumiracoxib 400 mg, n = 156 Celecoxib 400 mg, n = 156 Placebo, n = 52 |
|
| Outcomes | ≥50% PR over six hours Time to onset of analgesia Use of rescue medication Adverse events Withdrawals |
|
| Notes | Oxford Quality Score: R2, DB2, W1. Total = 5 | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “validated automated system” |
| Allocation concealment (selection bias) | Low risk | Remote allocation |
| Blinding (performance bias and detection bias) All outcomes |
Low risk | “double dummy” |
| Methods | RCT, DB, DD, placebo and active controlled parallel group study, single oral dose. Medication administered when pain intensity was moderate to severe. Study duration 24 hours |
|
| Participants | Post-operative dental surgery, third molar extraction Male and females Mean age 22 years (range 17 to 41 years) N = 355 |
|
| Interventions | Lumiracoxib 400 mg, n = 101 Rofecoxib 50 mg, n = 102 Celecoxib 200 mg, n = 101 Placebo, n = 51 |
|
| Outcomes | ≥50% PR over six hours Time to onset of analgesia Use of rescue medication Adverse events |
|
| Notes | Oxford Quality Score: R1, DB2, W0. Total = 3 | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes |
Low risk | “double dummy” |
| Methods | RCT, DB, DD, placebo and active controlled, parallel-group, single oral dose. Medication administered when pain intensity was moderate to severe. Study duration 12 hours | |
| Participants | Post-operative dental surgery, third molar extraction Male and females Mean age 22 years (SD 5.0, all >17 years) N = 202 |
|
| Interventions | Lumiracoxib 400 mg, n = 50 Lumiracoxib 100 mg, n = 51 Ibuprofen 400 mg, n = 51 Placebo, n = 50 |
|
| Outcomes | ≥50% PR over six hours Time to onset of analgesia Use of rescue medication Adverse events Withdrawals |
|
| Notes | Oxford Quality Score: R1, DB2, W1. Total = 4 | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes |
Low risk | “double dummy” |
DB - double blind, DD - Double Dummy, N - number of participants in study, n - number of participants in treatment arm, PR -pain relief, R - randomised, RCT - Randomised Controlled Trial, W - withdrawals
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bitner 2004 | Not post operative pain |
| Schnitzer 2004 | Not post operative pain |
DATA AND ANALYSES
Comparison 1. Lumiracoxib versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Participants with at least 50% pain relief at 6 hours | 4 | 580 | Risk Ratio (M-H, Fixed, 95% CI) | 6.89 [4.13, 11.51] |
| 2 Participants using rescue medication | 3 | 428 | Risk Ratio (M-H, Fixed, 95% CI) | 0.68 [0.61, 0.77] |
| 3 Participants with at least one adverse event | 3 | 460 | Risk Ratio (M-H, Fixed, 95% CI) | 0.68 [0.42, 1.09] |
Analysis 1.1. Comparison 1 Lumiracoxib versus placebo, Outcome 1 Participants with at least 50% pain relief at 6 hours.
Review: Single dose oral lumiracoxib for postoperative pain in adults
Comparison: 1 Lumiracoxib versus placebo
Outcome: 1 Participants with at least 50% pain relief at 6 hours
 |
Analysis 1.2. Comparison 1 Lumiracoxib versus placebo, Outcome 2 Participants using rescue medication.
Review: Single dose oral lumiracoxib for postoperative pain in adults
Comparison: 1 Lumiracoxib versus placebo
Outcome: 2 Participants using rescue medication
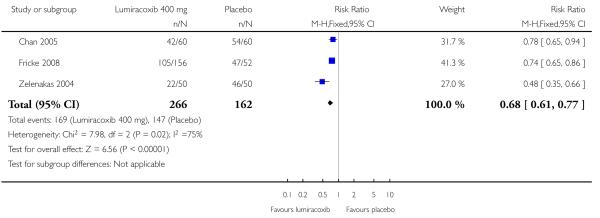 |
Analysis 1.3. Comparison 1 Lumiracoxib versus placebo, Outcome 3 Participants with at least one adverse event.
Review: Single dose oral lumiracoxib for postoperative pain in adults
Comparison: 1 Lumiracoxib versus placebo
Outcome: 3 Participants with at least one adverse event
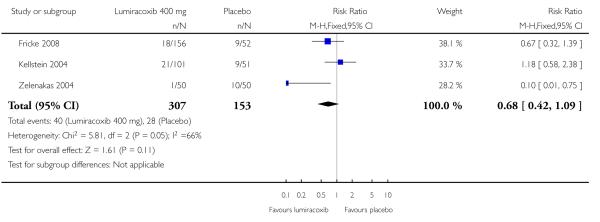 |
Appendix 1. MEDLINE via OVID search strategy
lumiracoxib or Prexige.mp.
Pain, Postoperative/
((postoperative adj4 pain*) or (post-operative adj4 pain*) or post-operative-pain* or (post* adj4 pain*) or (postoperative adj4 analgesi*) or (post-operative adj4 analgesi*) or “post-operative analgesi*”).mp.
((post-surgical adj4 pain*) or (“post surgical” adj4 pain*) or (post-surgery adj4 pain*)).mp.
(“pain-relief after surg*” or “pain following surg*” or “pain control after”).mp.
((“post surg*” or post-surg*) and (pain* or discomfort)).mp.
((pain* adj4 “after surg*”) or (pain* adj4 “after operat*”) or (pain* adj4 “follow* operat*”) or (pain* adj4 “follow* surg*”)).mp.
((analgesi* adj4 “after surg*”) or (analgesi* adj4 “after operat*”) or (analgesi* adj4 “follow* operat*”) or (analgesi* adj4 “follow* surg*”)).mp.
exp Surgical Procedures, Operative/
or/2-9
randomized controlled trial.pt.
controlled clinical trial.pt.
randomized.ab.
placebo.ab.
drug therapy.fs.
randomly.ab.
trial.ab.
groups.ab.
or/11-18
1 and 10 and 19
Appendix 2. EMBASE (via OVID) search strategy
Lumiracoxib/
(Lumiracoxib or Prexige).mp.
OR/1-2
Pain, postoperative/
((postoperative adj4 pain*) or (post-operative adj4 pain*) or post-operative-pain* or (post* adj4 pain*) or (postoperative adj4 analgesi*) or (post-operative adj4 analgesi*) or (“post-operative analgesi*”)).mp.
((post-surgical adj4 pain*) or (“post surgical” adj4 pain*) or (post-surgery adj4 pain*)).mp.
((“pain-relief after surg*”) or (“pain following surg*”) or (“pain control after”)).mp.
((“post surg*” or post-surg*) AND (pain* or discomfort)).mp.
((pain* adj4 “after surg*”) or (pain* adj4 “after operat*”) or (pain* adj4 “follow* operat*”) or (pain* adj4 “follow* surg*”)).mp.
((analgesi* adj4 “after surg*”) or (analgesi* adj4 “after operat*”) or (analgesi* adj4 “follow* operat*”) or (analgesi* adj4 “follow* surg*”)).mp.
OR/4-10
clinical trials.sh.
controlled clinical trials.sh.
randomized controlled trial.sh.
double-blind procedure.sh.
(clin* adj25 trial*)
((doubl* or trebl* or tripl*) adj25 (blind* or mask*))
placebo*
random*
OR/12-19
3 AND 11 AND 20
Appendix 3. CENTRAL search strategy
(lumiracoxib or Prexige):ti,ab,kw.
MESH descriptor Pain, postoperative
((postoperative near/4 pain*) or (post-operative near/4 pain*) or post-operative-pain* or (post* near/4 pain*) or (postoperative near/4 analgesi*) or (post-operative near/4 analgesi*) or (“post-operative analgesi*”)):ti,ab,kw.
((post-surgical near/4 pain*) or (“post surgical” near/4 pain*) or (post-surgery near/4 pain*)):ti,ab,kw.
((“pain-relief after surg*”) or (“pain following surg*”) or (“pain control after”)):ti,ab,kw.
((“post surg*” or post-surg*) AND (pain* or discomfort)):ti,ab,kw.
((pain* near/4 “after surg*”) or (pain* near/4 “after operat*”) or (pain* near/4 “follow* operat*”) or (pain* near/4 “follow* surg*”)):ti,ab,kw.
((analgesi* near/4 “after surg*”) or (analgesi* near/4 “after operat*”) or (analgesi* near/4 “follow$ operat*”) or (analgesi* near/4 “follow* surg*”)):ti,ab,kw.
or/2-8
1 AND 9
Limit 10 to Clinical Trials (CENTRAL)
Appendix 4. Glossary
Categorical rating scale
The commonest is the five category scale (none, slight, moderate, good or lots, and complete). For analysis numbers are given to the verbal categories (for pain intensity, none=0, mild=1, moderate=2 and severe=3, and for relief none=0, slight= 1, moderate=2, good or lots=3 and complete=4). Data from different subjects is then combined to produce means (rarely medians) and measures of dispersion (usually standard errors of means). The validity of converting categories into numerical scores was checked by comparison with concurrent visual analogue scale measurements. Good correlation was found, especially between pain relief scales using cross-modality matching techniques. Results are usually reported as continuous data, mean or median pain relief or intensity. Few studies present results as discrete data, giving the number of participants who report a certain level of pain intensity or relief at any given assessment point. The main advantages of the categorical scales are that they are quick and simple. The small number of descriptors may force the scorer to choose a particular category when none describes the pain satisfactorily.
VAS
Visual analogue scale: lines with left end labelled “no relief of pain” and right end labelled “complete relief of pain”, seem to overcome this limitation. Patients mark the line at the point which corresponds to their pain. The scores are obtained by measuring the distance between the no relief end and the patient’s mark, usually in millimetres. The main advantages of VAS are that they are simple and quick to score, avoid imprecise descriptive terms and provide many points from which to choose. More concentration and coordination are needed, which can be difficult post-operatively or with neurological disorders.
TOTPAR
Total pain relief (TOTPAR) is calculated as the sum of pain relief scores over a period of time. If a patient had complete pain relief immediately after taking an analgesic, and maintained that level of pain relief for six hours, they would have a six-hour TOTPAR of the maximum of 24. Differences between pain relief values at the start and end of a measurement period are dealt with by the composite trapezoidal rule. This is a simple method that approximately calculates the definite integral of the area under the pain relief curve by calculating the sum of the areas of several trapezoids that together closely approximate to the area under the curve.
SPID
Summed pain intensity difference (SPID) is calculated as the sum of the differences between the pain scores over a period of time. Differences between pain intensity values at the start and end of a measurement period are dealt with by the trapezoidal rule.
VAS TOTPAR and VAS SPID are visual analogue versions of TOTPAR and SPID.
See “Measuring pain” in Bandolier’s Little Book of Pain, Oxford University Press, Oxford. 2003; pp 7-13 (Moore 2003).
Appendix 5. Summary of efficacy outcomes in individual studies
| Analgesia | Rescue medication | ||||||
|---|---|---|---|---|---|---|---|
| Study ID | Treatment | PI or PR | Number with 50% PR | PGE: excellent | Median time to onset | Median time to use (h) | % using |
| Chan 2005 | (1) lumira-coxib 400 mg, n=60 (2) naproxen 500 mg, n=60 (3) placebo, n=60 |
TOTPAR 6: (1) 8.19 (3) 5.58 |
(1) 20/59 (3) 11/59 |
(1) 16/60 (3) 1/60 |
(1) 0.62 (3) >12 |
(1) 3.8 (3) 2.0 |
at 12 h: (1) 42/60 (3) 54/60 |
| Fricke 2008 | (1) lumiracoxib 400 mg, n = 156 (2) celecoxib 400 mg, n = 156 (3) placebo, n = 52 |
TOTPAR 6: (1) 11.71 (3) 1.79 |
(1) 83/156 (3) 0/52 |
(1) 45/156 (3) 1/52 |
(1) 0.63 (3) not estimable |
(1) 12.1 (3) 1.3 |
at 24 h: (1) 105/156 (3) 47/52 |
| Kellstein 2004 | (1) lumiracoxib 400 mg, n=101 (2) rofe-coxib50mg, n=102 (3) cele-coxib 200mg, n=101 (4) placebo, n=51 |
TOTPAR 6: (1) 10.68 (4) 1.40 |
(1) 48/101 (4) 0/51 |
(1) 32/101 (4) 1/51 |
(1) 0.66 (4) >12 |
(1) 7.2 (4) 1.3 |
14.9% of whole group |
| Zelenekas 2004 | (1) lumiracoxib 400 mg, n=50 (2) Ibuprofen 400 mg, n=51 (3) placebo, n=50 |
TOTPAR 6: (1) 13.63 (3) 4.16 |
(1) 32/50 (3) 6/50 |
(1) 23/50 (3) 3/50 |
(1) 0.62 (3) >12 |
(1) >12 (3) 2 |
at 12 h: (1) 22/50 (3) 46/50 |
Appendix 6. Summary of adverse events and withdrawals
| Adverse events | Withdrawals | ||||
|---|---|---|---|---|---|
| Study ID | Treatment | Any | Serious | Adverse event | Other |
| Chan 2005 | (1) lumiracoxib 400 mg, n=60 (2) naproxen 500 mg, n=60 (3) placebo, n=60 |
no single dose data | None | None | None |
| Fricke 2008 | (1) lumiracoxib 400 mg, n = 156 (2) celecoxib 400 mg, n = 156 (3) placebo, n = 52 |
(1) 18/156 (3) 9/52 |
None | None | None |
| Kellstein 2004 | (1) lumiracoxib 400 mg, n=101 (2) rofecoxib50mg, n=102 (3) celecoxib 200mg, n=101 (4) placebo, n=51 |
(1) 21/101 (4) 9/51 |
None | None | None |
| Zelenekas 2004 | (1) lumiracoxib 400 mg, n=50 (2) Ibuprofen 400 mg, n=51 (3) placebo, n=50 |
(1) 1/50 (3) 10/50 |
(1) 0/50 (3) 1/50 (DVT) |
(1) 0/50 (2) 1/51 (3) 0/50 |
None |
WHAT’S NEW
Last assessed as up-to-date: 5 March 2010.
| Date | Event | Description |
|---|---|---|
| 25 April 2012 | Review declared as stable | The authors have checked the literature in 2012 and believe it unlikely there will be any new additional studies to include in this review for at least five years |
HISTORY
Review first published: Issue 4, 2007
| Date | Event | Description |
|---|---|---|
| 17 June 2010 | New search has been performed | New search February 2010 |
| 5 March 2010 | New citation required but conclusions have not changed | One new study identified and included in analyses, increasing number of participants treated with lumira-coxib 400 mg by 73%. Conclusions are unchanged, but confidence in results is increased |
| 7 November 2008 | Amended | Minor change to in-house referencing code |
| 6 May 2008 | Amended | Converted to new review format. |
| 24 January 2008 | Amended | On November 2007 the UK Medicines and Healthcare Regulatory Authority suspended the marketing authorisation for Lumiracoxib following safety concerns relating to liver damage in patients prescribed the drug for chronic/long term condiions such as osteoarthritis |
Footnotes
DECLARATIONS OF INTEREST
SD and RAM have received research support from charities, government and industry sources at various times, but no such support was received for this work. RAM and HJM have consulted for various pharmaceutical companies. RAM has received lecture fees from pharmaceutical companies related to analgesics and other healthcare interventions. YMR is employed by the PaPaS Review Group.
References to studies included in this review
- Chan 2005 {published data only} .Chan VWS, Clark AJ, Davis JC, Wolf RS, Kellstein D, Jayawardene S. The post-operative analgesic efficacy and tolerability of lumiracoxib compared with placebo and naproxen after total knee or hip arthroplasty. Acta Anaesthesiologica Scandinavica. 2005 Nov 49;(10):1491–500. doi: 10.1111/j.1399-6576.2005.00782.x. [DOI] [PubMed] [Google Scholar]
- Fricke 2008 {published data only} .Fricke J, Davis N, Yu V, Krammer G. Lumiracoxib 400 mg compared with celecoxib 400 mg and placebo for treating pain following dental surgery: a randomized, controlled trial. Journal of Pain. 2008;9(1):20–7. doi: 10.1016/j.jpain.2007.08.004. DOI: 10.1016/j.jpain.2007.08.004. [DOI] [PubMed] [Google Scholar]
- Kellstein 2004 {published data only} .Kellstein D, Ott D, Jayawardene S, Fricke J. Analgesic efficacy of a single dose of lumiracoxib compared with rofecoxib, celecoxib and placebo in the treatment of post-operative dental pain. International Journal of Clinical Practice. 2004;58(3):244–50. doi: 10.1111/j.1368-5031.2004.00155.x. [DOI] [PubMed] [Google Scholar]
- Zelenakas 2004 {published data only} .Zelenakas K, Fricke JR, Jr, Jayawardene S, Kellstein D. Analgesic efficacy of single oral doses of lumiracoxib andibuprofen in patients with postoperative dental pain. International Journal of Clinical Practice. 2004;58(3):251–6. doi: 10.1111/j.1368-5031.2004.00156.x. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Bitner 2004 {published data only} .Bitner M, Katterhorn J, Hatfield C, Gao J, Kellstein D. Efficacy and tolerability of lumiracoxib in the treatment of primary dysmenorrhoea. International Journal Clinical Practice. 2004;58(4):340–5. doi: 10.1111/j.1368-5031.2004.00179.x. [DOI] [PubMed] [Google Scholar]
- Schnitzer 2004 {published data only} .Schnitzer TJ, Beier J, Geusens P, Hasler P, Patel SK, Senftleber I, et al. Efficacy and safety of four doses of lumiracoxib versus diclofenac in patients with knee or hip primary osteoarthritis: A phase II, four week, multicenter randomised, double blind, placebo-controlled trial. Arthritis and Rheumatism. 2004;51(4):549–57. doi: 10.1002/art.20525. [DOI] [PubMed] [Google Scholar]
Additional references
- Bannwarth 2005 .Bannworth B, Berenbaum F. Clinical pharmacology of lumiracoxib, a second generation cyclooxygenase 2 selective inhibitor. Expert Opinion on Investigational Drugs. 2005;14(4):521–33. doi: 10.1517/13543784.14.4.521. [DOI] [PubMed] [Google Scholar]
- Barden 2004 .Barden J, Edwards JE, McQuay HJ, Moore RA. Pain and analgesic response after third molar extraction and other postsurgical pain. Pain. 2004;107:86–90. doi: 10.1016/j.pain.2003.09.021. [DOI] [PubMed] [Google Scholar]
- Barden 2006 .Barden J, Derry S, McQuay HJ, Moore RA. Bias from industry trial funding? A framework, a suggested approach, and a negative result. Pain. 2006;121(3):207–18. doi: 10.1016/j.pain.2005.12.011. DOI: 10.1016/j.pain.2005.12.011. [DOI] [PubMed] [Google Scholar]
- Clarke 2009 .Clarke R, Derry S, Moore RA, McQuay HJ. Single dose oral etoricoxib for postoperative pain. Cochrane Database of Systematic Reviews. 2009;(2) doi: 10.1002/14651858.CD004309.pub2. DOI: 10.1002/14651858.CD004309.pub2. [DOI] [PubMed] [Google Scholar]
- Collins 2001 .Collins SL, Edwards J, Moore RA, Smith LA, McQuay HJ. Seeking a simple measure of analgesia for mega-trials: is a single global assessment good enough? Pain. 2001;91((1-2):189–94. doi: 10.1016/s0304-3959(00)00435-8. [DOI] [PubMed] [Google Scholar]
- Cook 1995 .Cook RJ, Sackett DL. The number needed to treat: a clinically useful measure of treatment effect. BMJ. 1995;310:452–4. doi: 10.1136/bmj.310.6977.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper 1991 .Cooper SA. Single-dose analgesic studies: the upside and downside of assay sensitivity. In: Max MB, Portenoy RK, Laska EM, editors. The design of analgesic clinical trials. Advances in Pain Research and Therapy. Vol. 18. Raven Press; New York: 1991. pp. 117–24. [Google Scholar]
- Day 1988 .Day RO, McLachlan AJ, Graham GG, Williams KM. Pharmokinetics of non-steroidal anti-inflammatory drugs in synovial fluid. Baillieres Clinical Rheumatology. 1988;2:363–93. doi: 10.1016/s0950-3579(88)80019-0. [DOI] [PubMed] [Google Scholar]
- Derry 2008 .Derry S, Barden J, McQuay HJ, Moore RA. Single dose oral celecoxib for acute postoperative pain in adults. Cochrane Database of Systematic Reviews. 2008;(4) doi: 10.1002/14651858.CD004233.pub2. DOI: 10.1002/14651858.CD004233.pub2. [DOI] [PubMed] [Google Scholar]
- Derry C 2009a .Derry C, Derry S, Moore RA, McQuay HJ. Single dose oral naproxen and naproxen sodium for acute postoperative pain in adults. Cochrane Database of Systematic Reviews. 2009;(1) doi: 10.1002/14651858.CD004234.pub3. DOI: 10.1002/14651858.CD004234.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derry C 2009b .Derry C, Derry S, Moore RA, McQuay HJ. Single dose oral ibuprofen for acute postoperative pain in adults. Cochrane Database of Systematic Reviews. 2009;(3) doi: 10.1002/14651858.CD001548.pub2. DOI: 10.1002/14651858.CD001548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derry P 2009 .Derry P, Derry S, Moore RA, McQuay HJ. Single dose oral diclofenac for acute postoperative pain in adults. Cochrane Database of Systematic Reviews. 2009;(2) doi: 10.1002/14651858.CD004768.pub2. DOI: 10.1002/14651858.CD004768.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FitzGerald GA, Patrono C. The coxibs, selective inhibitors of cyclooxygenase-2. New England Journal of Medicine. 2001;345(6):433–42. doi: 10.1056/NEJM200108093450607. [DOI] [PubMed] [Google Scholar]
- Forrest 2002 .Forrest JB, Camu F, Greer IA, Kehlet H, Abdalla M, Bonnet F. Ketorolac, diclofenac, and ketoprofen are equally safe for pain relief after major surgery. British Journal of Anaesthesia. 2002;88(2):227–33. doi: 10.1093/bja/88.2.227. [DOI] [PubMed] [Google Scholar]
- Garner 2002 .Garner S, Fidan D, Frankish R, Judd M, Towheed T, Wells G, Tugwell P. Rofecoxib for the treatment of rheumatoid arthritis. Cochrane Database of Systematic Reviews. 2002;(2) DOI: 10.1002/14651858.CD003685.pub2. [Google Scholar]
- Grahame-Smith 2002 .Grahame-Smith DG, Aronson JK. Oxford textbook of clinical pharmacology and drug therapy. 3rd Edition. Oxford University Press; Oxford: 2002. [Google Scholar]
- Hawkey 1999 .Hawkey CJ. Cox-2 inhibitors. Lancet. 1999;353(9149):307–14. doi: 10.1016/s0140-6736(98)12154-2. [DOI] [PubMed] [Google Scholar]
- Hawkey 2001 .Hawkey CJ. Gastrointestinal safety of COX-2 specific inhibitors. Gastroenterology Clinics of North America. 2001;30(4):921–36. doi: 10.1016/s0889-8553(05)70220-x. [DOI] [PubMed] [Google Scholar]
- Hawkey 2006 .Hawkey CJ. NSAIDs, coxibs, and the intestine. Journal of Cardiovascular Pharmacology. 2006;47(Suppl 1):S72–5. doi: 10.1097/00005344-200605001-00013. [DOI] [PubMed] [Google Scholar]
- Jadad 1996 .Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Controlled Clinical Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- Kearney 2006 .Kearney PM, Baigent C, Godwin J, Halls H, Emberson JR, Patrono Do selective cyclo-oxygenase-2 inhibitors and traditional non-steroidal anti-inflammatory drugs increase the risk of atherothrombosis? Meta-analysis of randomised trials. BMJ. 2006;332:1302–08. doi: 10.1136/bmj.332.7553.1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- L’Abbe 1987 .L’Abbe KA, Detsky AS, O’Rourke K. Meta-analysis in clinical research. Annals of Internal Medicine. 1987;107:224–33. doi: 10.7326/0003-4819-107-2-224. [DOI] [PubMed] [Google Scholar]
- Lloyd 2009 .Lloyd R, Derry S, Moore RA, McQuay HJ. Intravenous parecoxib for acute postoperative pain in adults. Cochrane Database of Systematic Reviews. 2009;(2) doi: 10.1002/14651858.CD004771.pub4. DOI: 10.1002/14651858.CD004771.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuay 2005 .McQuay HJ, Moore RA. Placebo. Postgraduate Medical Journal. 2005;81:155–60. doi: 10.1136/pgmj.2004.024737. DOI: 10.1136/ pgmj.2004.024737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher 1999 .Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of meta-analyses of randomised controlled trials: the QUOROM statement. Lancet. 1999;354:1896–900. doi: 10.1016/s0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- Moore 1996 .Moore A, McQuay H, Gavaghan D. Deriving dichotomous outcome measures from continuous data in randomised controlled trials of analgesics. Pain. 1996;66(2-3):229–37. doi: 10.1016/0304-3959(96)03032-1. [DOI] [PubMed] [Google Scholar]
- Moore 1997a .Moore A, McQuay H, Gavaghan D. Deriving dichotomous outcome measures from continuous data in randomised controlled trials of analgesics: Verification from independent data. Pain. 1997;69(1-2):127–30. doi: 10.1016/s0304-3959(96)03251-4. [DOI] [PubMed] [Google Scholar]
- Moore 1997b .Moore A, Moore O, McQuay H, Gavaghan D. Deriving dichotomous outcome measures from continuous data in randomised controlled trials of analgesics: Use of pain intensity and visual analogue scales. Pain. 1997;69(3):311–5. doi: 10.1016/S0304-3959(96)03306-4. [DOI] [PubMed] [Google Scholar]
- Moore 1998 .Moore RA, Gavaghan D, Tramer MR, Collins SL, McQuay HJ. Size is everything - large amounts of information are needed to overcome random effects in estimating direction and magnitude of treatment effects. Pain. 1998;78(3):209–16. doi: 10.1016/S0304-3959(98)00140-7. [DOI] [PubMed] [Google Scholar]
- Moore 2003 .Moore RA, Edwards J, Barden J, McQuay HJ. Bandolier’s Little Book of Pain. Oxford University Press; Oxford: 2003. ISBN: 0-19-263247-7. [Google Scholar]
- Moore 2005a .Moore RA, Edwards JE, McQuay HJM. Acute pain: individual patient meta-analysis shows the impact of different ways of analysing and presenting results. Pain. 2005;116:322–31. doi: 10.1016/j.pain.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Moore 2005b .Moore RA, Derry S, Makinson GT, McQuay HJ. Tolerability and adverse events in clinical trials of celecoxib in osteoarthritis and rheumatoid arthritis: systematic review and meta-analysis of information from company clinical trial reports. Arthritis Research and Therapeutics. 2005;7(3):R644–65. doi: 10.1186/ar1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore 2006 .Moore A, McQuay H. Bandolier’s Little Book of Making Sense of the Medical Evidence. Oxford University Press; Oxford: 2006. ISBN: 0-19-856604-2. [Google Scholar]
- Moore 2008 .Moore RA, Barden J, Derry S, McQuay HJ. Managing potential publication bias. In: McQuay HJ, Kalso E, Moore RA, editors. Systematic Reviews in Pain Research: Methodology Refined. IASP Press; Seattle: 2008. pp. 15–24. ISBN: 978-0-931092-69-5. [Google Scholar]
- Morris 1995 .Morris JA, Gardner MJ. Calculating confidence intervals for relative risk, odds ratio and standardised ratios and rates. In: Gardner MJ, Altman DG, editors. Statistics with confidence - confidence intervals and statistical guidelines. BMJ; London: 1995. pp. 50–63. [Google Scholar]
- Mysler 2004 .Mysler E. Lumiracoxib (Prexige): a new selective COX-2 inhibitor. International Journal of Clinical Practice. 2004;58(6):606–11. doi: 10.1111/j.1368-5031.2004.00199.x. [DOI] [PubMed] [Google Scholar]
- Patrono 2009 .Patrono C, Baigent C. Low-dose aspirin, coxibs, and other NSAIDS: a clinical mosaic emerges. Molecular Interventions. 2009;9(1):31–9. doi: 10.1124/mi.9.1.8. DOI: 10.1124/mi.9.1.8. [DOI] [PubMed] [Google Scholar]
- Schnitzer 2004a .Schnitzer TJ, Burmester GR, Mysler E, Hochberg MC, Doherty M, Ehrsam E, et al. Comparison of lumiracoxib with naproxen and ibuprofen in the Therapeutic Arthritis Research and Gastrointestinal Event Trial (TARGET), reduction in ulcer complications: randomised controlled trial. Lancet. 2004;364(9435):665–74. doi: 10.1016/S0140-6736(04)16893-1. [DOI] [PubMed] [Google Scholar]
- Toms 2008 .Toms L, McQuay HJ, Derry S, Moore RA. Single dose oral paracetamol (acetaminophen) for postoperative pain in adults. Cochrane Database of Systematic Reviews. 2008;(4) doi: 10.1002/14651858.CD004602.pub2. DOI: 10.1002/14651858.CD004602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toms 2009 .Toms L, Derry S, Moore RA, McQuay HJ. Single dose oral paracetamol (acetaminophen) with codeine for postoperative pain in adults. Cochrane Database of Systematic Reviews. 2009;(1) doi: 10.1002/14651858.CD001547.pub2. DOI: 10.1002/14651858.CD001547.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tramer 1997 .Tramèr MR, Reynolds DJM, Moore RA, McQuay HJ. Impact of covert duplicate results on meta-analysis: a case study. BMJ. 1997;315:635–9. doi: 10.1136/bmj.315.7109.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
- Roy 2007 .Roy YM, Derry S, Moore RA. Single dose oral lumiracoxib for postoperative pain. Cochrane Database of Systematic Reviews. 2007;(4) doi: 10.1002/14651858.CD006865. DOI: 10.1002/14651858.CD006865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Indicates the major publication for the study