Abstract
Previous studies have reached differing conclusions about the importance of general versus central markers of adiposity to blood pressure, leading to suggestions that population-specific adiposity thresholds may be needed. We examined the relevance of adiposity to blood pressure among 111,911 men and women who, when recruited into the Mexico City Prospective Study, were aged 35-89, had no chronic disease, and were not taking antihypertensives. Linear regression was used to estimate the effects on systolic (SBP) and diastolic (DBP) blood pressure of two markers of general adiposity (body-mass index [BMI, height-adjusted-weight [HtaW]) and four markers of central adiposity (waist-circumference [WC], hip-circumferences [HC], their ratio [WHR] and waist-height ratio [WHtR]), adjusted for relevant confounders. Mean (SD) adiposity levels were: BMI (28.7±4.5 kg/m2); HtaW (70.2±11.2 kgs); WC (93.3±10.6 cms); HC (104.0±9.0 cms); WHR (0.90±0.06); and WHtR (0.60±0.07). Associations with blood pressure were linear with no threshold levels below which lower general or central adiposity was not associated with lower blood pressure. On average, each 1 standard deviation (SD) higher measured adiposity marker was associated with a 3 mmHg higher SBP and 2 mmHg higher DBP (SEs <0.1 mmHg), but for the WHR, associations were only half as strong. General adiposity associations were independent of central adiposity, but central adiposity associations were substantially reduced by adjustment for general adiposity. Findings were similar for men and women. In Mexican adults, often overweight or obese, markers of general adiposity were stronger predictors of blood pressure than measured markers of central adiposity, with no threshold effects.
Keywords: cross-sectional study, blood pressure, adiposity, obesity, Hispanic population
Introduction
Adiposity and blood pressure are major modifiable risk factors for cardiovascular and other chronic diseases.1–4 Levels of adiposity5 and blood pressure6 are increasing in many populations and are estimated to be responsible for a substantial proportion of morbidity and mortality globally.7 Body mass index (BMI), the most commonly used marker of adiposity, is strongly related to blood pressure,1 and Mendelian randomisation studies8–10 and randomised intervention trials of weight-loss11,12 suggest this relationship to be causal. A recent study of 0.5 million mostly lean Chinese adults found that systolic blood pressure increased by about 8 mmHg for each 5 kg/m2 higher BMI,13 somewhat greater than has been documented in Western populations.1 In addition to varying between populations, the relevance of adiposity to blood pressure may vary within a population over time, perhaps because of changing levels of other characteristics. Different markers of adiposity also differ in their relevance to blood pressure. For example, while some studies have found BMI to be more strongly related to blood pressure than waist circumference or the waist-to-hip ratio,13,14 others have found the opposite,15–17 whereas BMI and the waist-height ratio have been found to exhibit similar associations with blood pressure in some studies.14,18
In 2008, a World Health Organisation (WHO) Expert Consultation on waist circumference and waist-hip ratio,19 recommended that further studies are needed to determine whether existing recommended adiposity “cut-off” points should be population-specific, and noted that there was little existing evidence among Hispanic populations. We report the relevance of several common markers of adiposity to blood pressure among 150,000 men and women from Mexico City who were recruited into a prospective study at the start of the 21st century.20,21
Methods
The rationale and design of the Mexico City Prospective Study has been described in detail previously; 20,21 a summary is given below.
Recruitment and baseline assessment
Between 1998 and 2004, 159,755 participants aged 35 years and over from the Coyoacán and Iztapalapa districts of Mexico City were visited in their homes and agreed to take part in a prospective cohort study. Trained nurses recorded data directly into a handheld electronic device, with subsequent automated checks for unusual values or data entry errors. Age, sex, socioeconomic status, lifestyle (tobacco use, alcohol consumption, physical activity and diet), disease history and medication were recorded.20 Weight (wearing light clothes), standing height, waist and hip circumferences` were measured to the nearest 0.1 kg or 0.1 cms respectively. Regularly-calibrated electronic scales, fixed stadiometers and non-stretchable tapes were employed according to a standard protocol. Waist circumference was measured at the mid-point between the iliac crest and the lower rib and hip circumference was measured at the widest circumference over the gluteal muscles. Seated blood pressure was measured after 5 minutes of rest, using a manual sphygmomanometer and suitably sized cuff. Three blood pressure measurements were taken over about a 6 minute period, with the average of the three measures used in analyses.
Statistical analyses
Six adiposity variables, either directly measured or derived, were assessed, including two anthropometric markers of “general adiposity” (height-adjusted weight [HtaW] and BMI) and four anthropometric markers of “central adiposity” (waist circumference [WC], hip circumference [HC], the waist-hip ratio [WHR] and the waist-height ratio [WHtR]). BMI was calculated as weight in kgs divided by the square of height in metres. HtaW was calculated in men through the equation HtaW=weight in kgs + 0.852 x (164.8 – height in cms), and in women through the equation HtaW=weight in kgs + 0.682 x (151.8 – height in cms), based on the coefficients of the sex-specific linear regression models of weight on height. To limit the effects of measurement errors, very extreme or implausible values of adiposity or blood pressure were excluded (see footnote to Table 1 for exact exclusion criteria). In addition, to limit reverse causation, those taking blood pressure lowering medication (regularly in the last year) and those previously diagnosed with diabetes, cancer, liver cirrhosis, vascular, respiratory, or chronic kidney diseases, were also excluded, as were those aged ≥90 years, or with missing data on any confounder (see below).
Table 1. Age- and sex-specific measures of adiposity and blood pressure among 111,911 participants who were aged 35-89 at recruitment, were not taking blood pressure lowering drugs and had no known chronic diseases.
Mean (SD) shown; BMI=Body mass index; DBP=Diastolic blood pressure; HC=Hip circumference; SBP=Systolic blood pressure; WC=Waist circumference; WHR=Waist:hip ratio; WHtR=Waist:height ratio. Analyses are limited to those aged 35-89 at recruitment, and exclude anyone with chronic disease (diabetes, vascular disease, chronic kidney disease, cirrhosis, cancer, emphysema), those taking blood pressure lowering drugs at recruitment, and those with extreme or implausible measures of adiposity or blood pressure (SBP <80 or >250 mmHg, DBP <40 or >150 mmHg, SBP minus DBP ≤15 mmHg, weight <40 or >250 kg in men, or <35 or >250 kg in women, height <140 or >200 cms in men, or <120 or >180 cms in women, BMI <15 or >50 kg/m2, WC <60 or >150cms, HC <70 or >150cms in men, or <70 or >160 cms in women, or WHR <0.7 or >1.2).
| Age, years | n | Height, cm | Weight, kg | BMI, kg/m² | WC, cm | HC, cm | WHR | WHtR | SBP, mmHg | DBP, mmHg |
|---|---|---|---|---|---|---|---|---|---|---|
| Men | ||||||||||
| 35-39 | 8249 | 167 (7) | 77 (13) | 27.7 (4.2) | 94 (10) | 101 (8) | 0.93 (0.05) | 0.56 (0.06) | 123 (12) | 82 (9) |
| 40-49 | 12 591 | 166 (7) | 77 (13) | 28.1 (4.1) | 95 (10) | 101 (7) | 0.94 (0.05) | 0.58 (0.06) | 124 (13) | 83 (9) |
| 50-59 | 8704 | 164 (7) | 76 (12) | 28.1 (4.0) | 97 (10) | 101 (7) | 0.96 (0.05) | 0.59 (0.06) | 128 (14) | 85 (10) |
| 60-69 | 4942 | 163 (7) | 74 (12) | 27.7 (4.1) | 97 (10) | 101 (8) | 0.97 (0.06) | 0.60 (0.06) | 132 (16) | 85 (10) |
| 70-79 | 2914 | 161 (7) | 70 (11) | 26.9 (3.9) | 97 (10) | 100 (8) | 0.97 (0.06) | 0.60 (0.06) | 134 (17) | 84 (10) |
| 80-89 | 938 | 159 (7) | 65 (11) | 25.7 (3.7) | 95 (10) | 99 (8) | 0.96 (0.06) | 0.60 (0.06) | 134 (18) | 83 (10) |
| Total | 38 338 | 165 (7) | 76 (13) | 27.8 (4.1) | 96 (10) | 101 (7) | 0.95 (0.06) | 0.58 (0.06) | 127 (14) | 84 (9) |
| Women | ||||||||||
| 35-39 | 18 290 | 154 (6) | 67 (12) | 28.6 (4.9) | 89 (11) | 104 (10) | 0.86 (0.06) | 0.58 (0.07) | 117 (12) | 78 (9) |
| 40-49 | 27 058 | 153 (6) | 68 (12) | 29.4 (4.9) | 91 (11) | 106 (10) | 0.86 (0.06) | 0.60 (0.07) | 121 (13) | 80 (9) |
| 50-59 | 15 284 | 151 (6) | 68 (12) | 29.9 (5.0) | 94 (11) | 107 (11) | 0.88 (0.06) | 0.62 (0.08) | 126 (15) | 83 (10) |
| 60-69 | 7476 | 149 (6) | 66 (12) | 29.6 (4.9) | 96 (11) | 107 (11) | 0.89 (0.06) | 0.64 (0.08) | 131 (16) | 84 (10) |
| 70-79 | 4088 | 147 (6) | 62 (12) | 28.4 (4.9) | 95 (11) | 105 (11) | 0.91 (0.07) | 0.65 (0.08) | 134 (17) | 84 (10) |
| 80-89 | 1377 | 145 (6) | 56 (11) | 26.8 (4.7) | 95 (11) | 102 (11) | 0.93 (0.07) | 0.66 (0.08) | 136 (18) | 83 (11) |
| Total | 73 573 | 152 (6) | 67 (12) | 29.2 (4.9) | 92 (11) | 106 (10) | 0.87 (0.06) | 0.61 (0.08) | 123 (15) | 81 (10) |
For “categorical” analyses of each anthropometric adiposity marker, individuals were split into ten equally-sized groups (ie, by the deciles of the sex-specific distributions). For each group, adjusted means of baseline SBP and DBP were calculated using standard regression techniques, with adjustment for baseline age, residential district, education, smoking status, level of physical activity and alcohol consumption (see Table 1 and Supplementary Table S1 for groupings used for covariates). Analyses were also either adjusted for sex, or done separately in men and women. Mean adjusted blood pressure estimates together with their 95% confidence intervals (CIs) were plotted against the mean adiposity levels for each group. For visual comparability of the plots between the different markers of adiposity, each horizontal axis extends across 4SDs, from -2SD below, to +2SD above the mean level observed in all participants. To separate the effects of general adiposity from any independent effects of central markers of adiposity (and vice versa), analyses of each marker were done before and after further adjustment for other markers. For example, HtaW and BMI associations were estimated before and after adjustment for WHR (or waist and hip considered separately), and WC and HC associations were estimated before and after adjustment for BMI (waist and hip associations were also estimated before and after adjustment for each other). WHtR associations were adjusted for weight only (as height is already included in the derivation of WHtR). Subsequently, “continuous” analyses were done to estimate the mean difference in SBP and DBP, associated with a 1SD higher level of adiposity (with the same covariate adjustments as for the categorical analyses). Analyses were done using SAS version 9.3 and R version 2.11.1.
Ethics approval and funding
Ethics approval was granted by the Mexican National Council of Science and Technology, the Mexican Ministry of Health and the University of Oxford. All study participants gave informed consent. Funding was received from the British Heart Foundation, the UK Medical Research Council, The Wellcome Trust (grant 058299/Z/99), and the Mexican Ministry of Health (Secretaria de Salud, Mexico). The funders had no input on the collection, analysis, or reporting of the data.
Results
Study participants
Of the 159,755 recruited participants, 4892 were excluded because they were aged 90+ at recruitment, had extreme measured values for blood pressure or the adiposity markers, or missing covariate data, and a further 42,952 were excluded because they had a prior diagnosis of chronic disease or were taking blood pressure lowering medication. The remaining 111,911 participants included 38,338 men (mean age 51 years) and 73,573 women (mean age 49 years).
Baseline markers of adiposity, blood pressure, and covariates
The age and sex-specific mean (±SD) levels of each of the anthropometric measures, derived markers of adiposity, and blood pressure, are shown in Table 1. On average, across all ages, mean height was 165±7 cm in men and 152±6 cm in women, mean weight was 76±13 kgs in men and 67±12 kgs in women, and mean BMI was 27.8±4.1 kg/m2 in men and 29.2±4.9 kg/m2 in women. At every age, mean BMI and HC were lower, and mean WC higher, among men, and consequently mean WHR was higher in men than women at every age (mean across all ages 0.95±0.06 versus 0.87±0.06, respectively). The WHtR increased with age in both sexes and was, on average, slightly lower among men (0.58±0.06 versus 0.61±0.08). Mean SBP increased with age, from 123±12 mmHg at ages 35-39 years to 134±18 mmHg at ages 80-89 years in men and, even more steeply, from 117±12 mmHg to 136±18 mmHg in women. DBP was less strongly, and somewhat less monotonically, related to age.
The correlations between the different adiposity markers are shown in Supplemental Figures S1 and S2. In both men and women, weight, waist-circumference and hip-circumference were all highly correlated (each pairwise age-adjusted correlation coefficient >0.80). By contrast, height was only weakly positively correlated with waist and hip circumference in men, and nearly uncorrelated in women. BMI and WHR were weakly correlated with each other in women (adjusted r=0.25), but somewhat more strongly correlated in men (adjusted r=0.48).
The extent to which average levels of each of the adiposity markers varied depending on residential area, attained educational level, smoking status, frequency of physical activity and alcohol consumption are shown in Supplemental Tables S1 and S2. Average adiposity profiles tended to be less favourable (eg, higher general and central adiposity) among those from the poorer of the two studied districts (Iztapalapa), among the physically inactive, and, particularly for women, among the less well educated. Anthropometric markers of adiposity were, however, largely unrelated to smoking status or alcohol consumption.
Relevance of adiposity to SBP
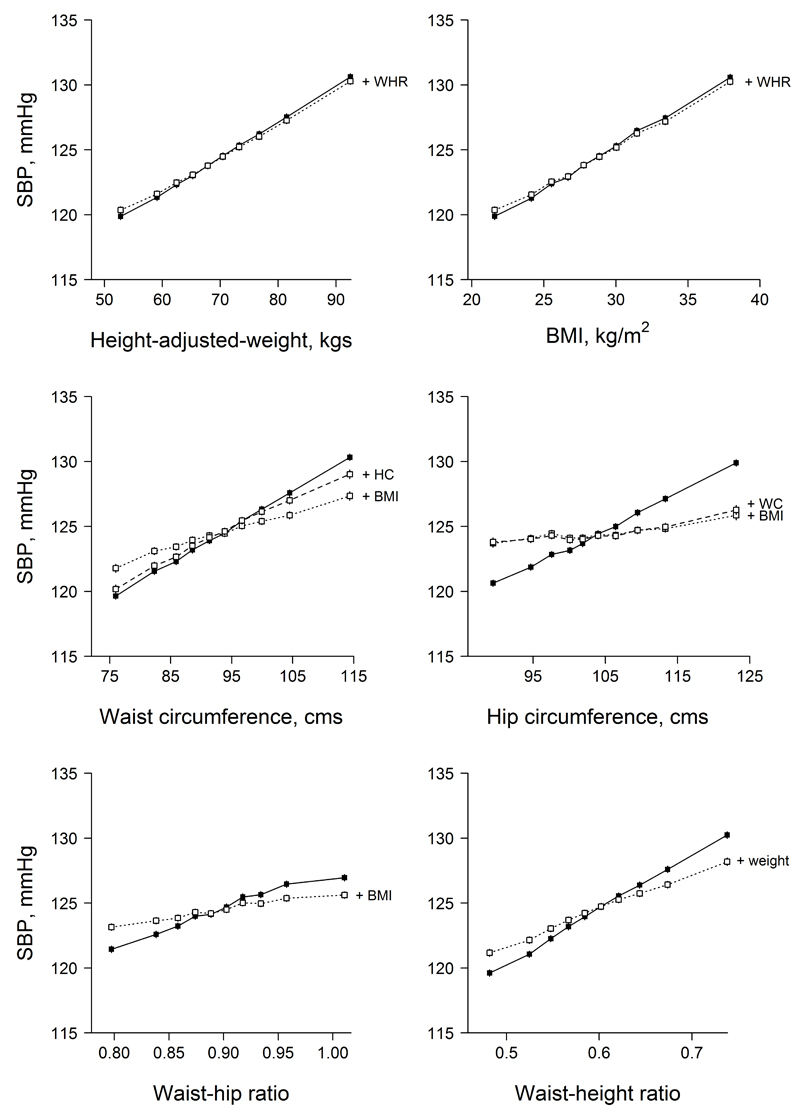
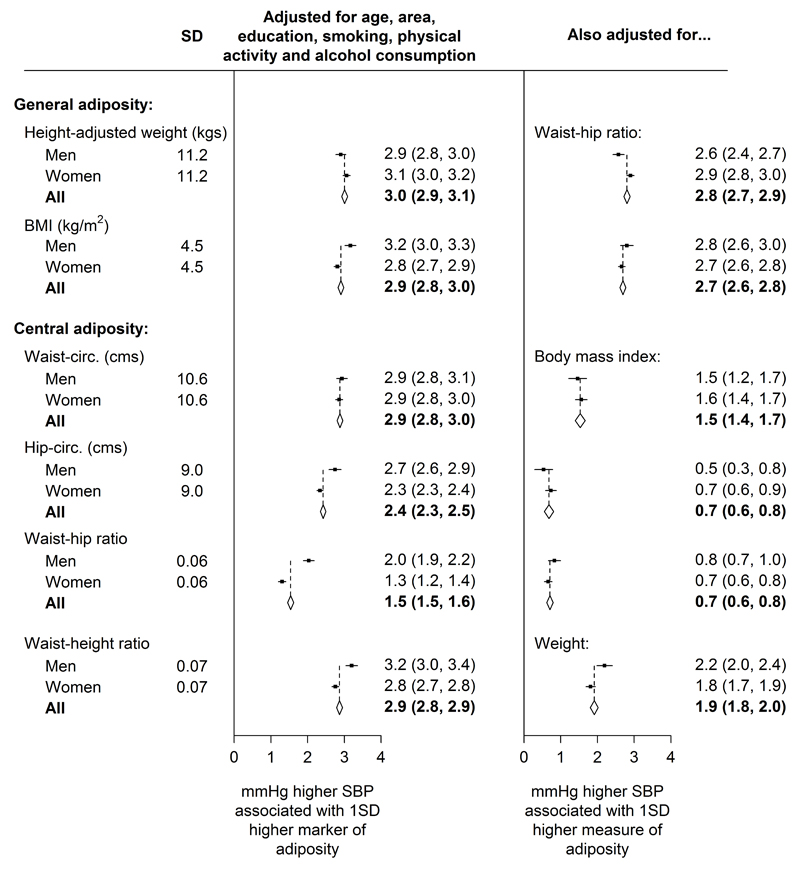
The two markers of general adiposity, HtaW and BMI, were both positively, and linearly, associated with SBP, with each 1SD higher level associated with about a 3 mmHg higher SBP (Figures 1 and 2). Adjustment for the WHR had virtually no effect on the shape or strength of these associations (reducing the strength of the association only marginally) (Figures 1 and 2).
Figure 1. Association between each adiposity measure and SBP.
BMI=Body mass index; HC=Hip circumference; SBP=Systolic blood pressure; WC=Waist circumference; WHR=Waist–hip ratio. All estimates are adjusted for age, sex, residential area, education, smoking, physical activity and alcohol consumption. Additional further adjustments for the dotted and dashed lines are stated on the plot. Analyses exclude those taking antihypertensive treatment at recruitment, those with prior chronic disease, and those with extreme or implausible values of adiposity or blood pressure (see footnote to Table 1).
Figure 2. Overall and sex–specific relevance of each adiposity measure to SBP, before and after additional adjustment for other adiposity measures.
Each diamond represents the inverse–variance–weighted average of the two estimates above it. For each marker of adiposity, the SD shown is the average of the SD in men and the SD in women (see Table 1 for the age– and sex–specific values). Values in parentheses are 95% confidence intervals.
Similarly, all four markers of central adiposity (WC, HC, WHR and WHtR) were also positively, and linearly, related to SBP. However, while the strength of association for WC, HC and WHtR was comparable with that seen for HtaW and BMI, the strength of association for the measured WHR was only about half as big (1.5 mmHg higher SBP for each 1SD higher WHR, with a bigger effect seen in men [2.0 mmHg] than in women [1.3 mmHg]; Figures 1 and 2). Moreover, adjustment for BMI (or, in the case of WHtR, for weight) reduced the magnitude of these associations considerably (Figure 2), as well as the difference between men and women in the relevance of the WHR to SBP. Among the markers of central adiposity, the association between WC and SBP was little affected by adjustment for HC, whereas the association between HC and SBP was substantially attenuated by adjustment for WC (with little further effect of adjustment for BMI; Figure 1 and Supplemental Figures S3 and S4). With the exception of the relevance of WHR to SBP, findings were broadly similar for men and women (Figure 2 and Supplemental Figures S3 and S4).
Relevance of adiposity to DBP
The relevance of the different anthropometric markers of adiposity to DBP is provided in Supplemental Figures S5-S8. With the exception of the WHR, each 1SD higher adiposity level was associated with about a 2 mmHg higher DBP (for the WHR the association was only half as strong). Again, the positive, linear associations between each marker of general adiposity and DBP were largely unaffected by adjustment for central adiposity, whereas the associations between the markers of central adiposity and DBP were greatly attenuated after adjustment for general adiposity.
Relevance of BMI to blood pressure at different ages
The relevance of BMI to both SBP and DBP was somewhat weaker at older ages (especially among those aged ≥70 years) than at younger ages (Supplemental Figure S9). Among the large numbers of participants who were aged <60 at recruitment, however, the strength of association between BMI and blood pressure was virtually the same within each age range.
Discussion
In this study of 110,000 Mexican adults free from known chronic diseases and not taking antihypertensive medication at the time of assessment, the anthropometric markers of adiposity that were most predictive of blood pressure were the measures of general adiposity. Within the ranges studied, there was no evidence of any threshold level below which less adiposity was not associated with lower blood pressure. On average, each 4.5 kg/m2 higher BMI (or each 11 kilograms of weight-for-height), was associated with a 3 mmHg higher SBP and a 2 mmHg higher DBP. For a given amount of general adiposity, any marker of central adiposity, including the ratio of waist-to-hip circumference or of waist-to-height, was much less strongly related.
Our findings in this adipose Mexican metropolitan population differ to some extent from those previously seen in other populations. For example, in a previous meta-analysis of 900,000 individuals from mostly Western populations recruited during the second half of the 20th century (and with, on average, only moderate levels of adiposity), a 5 kg/m2 higher BMI was associated with about a 5 mmHg higher SBP,1 while a more contemporary study of 500,000 mostly lean Chinese adults found that 5 kg/m2 higher BMI was associated with an 8 mmHg higher SBP.13 Our findings from this study of Mexican adults (with very high levels of adiposity) give more modest estimates. Chinese dietary intake of sodium (estimated by 24 hours urinary excretion) is higher than in Mexico,22 as well as in many Western populations,23,24 and since dietary sodium predicts SBP independently of BMI,25,26 variation in sodium intake may partly account for these between-population differences.
Alternatively, differences may reflect the way in which blood pressure or central anthropometry was measured. By contrast with the use of automated blood pressure machines in the China Kadoorie study,13 blood pressure at entry into our study (as for most other cohort studies) relied on use of manual sphygmomanometers, which is subject to observer-dependent random error, as well as digit preference.26 In addition, while we excluded from our analyses very extreme values, more modest measurement errors in our anthropometric measurements would tend to lead to some underestimation of the associations seen with blood pressure, with the magnitude of bias higher for those markers that are more difficult to measure precisely (eg, the WHR). Our estimates from this Hispanic population are, however, broadly comparable with estimates obtained by Mendelian-randomisation studies of the relevance of adiposity to blood pressure that have been conducted in other populations. For example, a Mendelian randomisation study of 14 BMI-associated single-nucleotide polymorphisms (SNPs) measured in 34,500 adults from 8 European population-based cohorts found that a 1 kg/m2 ‘genetically-elevated’ BMI increased SBP by 0.7 (95% CI 0.2-1.2) mmHg.9 Similarly, an FTO polymorphism study in over 145,000 participants from 30 mostly Caucasian cohorts found 1 kg/m2 genetically-elevated BMI to be associated with a 0.9 (95% 0.5–1.3) mmHg increase in SBP and 0.6 (95% 0.6–0.7) mmHg increase in DBP.10
Our results are consistent with the hypothesis generated by other studies that, in Mexican adults, adipose tissue in general may be more relevant to blood pressure than the site of the adipose tissue per se.27,28 This is again consistent with analyses of 500,000 Chinese adults, in which there was little association between central markers of adiposity and blood pressure after adjustment for BMI, and no suggestion of any threshold levels.13 However, some studies in other populations have indicated that while general and central anthropometrically defined adiposity both predict the development of hypertension,16 markers of central adiposity may be more discriminatory for predicting cardiovascular risk factors than markers of general adiposity.15
Proposed mechanisms behind the association of adiposity with blood pressure are complex, and include dysfunctional adipose tissue promoting activation of the sympathetic nervous system and the renin-angiotensin-aldosterone pathway, and adiponectin deficiency reducing nitric oxide production and increasing systemic inflammation and oxidative stress.27,28 We studied six commonly used anthropometric markers of adiposity, but others (directly measured and calculated), together with body imaging (through Dual-Energy X-ray Absorptiometry or Magnetic Resonance Imaging) could further disentangle the relevance to blood pressure of visceral versus other fat depots, as well as of muscle or lean mass. Such measures are however difficult to collect in large prospective studies in low- or middle-income countries where resources for research may be more limited. In the current study, a resurvey of 10,000 surviving participants involving additional bio-impedance measures is currently underway. Future work will therefore allow some exploration of how blood pressure in Hispanics varies with, for instance, measures of total fat mass. Elsewhere, the more advanced imaging methods of phenotyping adiposity are being used in populations with moderate levels of adiposity (such as abdominal magnetic resonance imaging currently being employed in a 100,000 subset of UK Biobank participants), allowing for an even more detailed investigation of the role of adiposity on blood pressure in that mostly Caucasian population.
In our study, just 7671/111,911 participants (7%) had a BMI <22.5 kg/m2, but in other populations the relationship between BMI and blood pressure has been shown to continue down to at least 18 kg/m2.1 Despite this, however, those same studies have shown that the risk of death from cardiovascular disease is, if anything, higher at BMI <22.5 kg/m2 than at 22.5 kg/m2,1 , 29 suggesting that low BMI may be correlated with other factors that have strong adverse effects on health. Adiposity influences blood lipids and glucose as well as blood pressure, and together these three risk factors have been estimated to explain 46% of the excess ischaemic heart disease risk and 76% of the excess stroke risk associated with higher BMI (though the true percentages may be higher as these estimates do not take account of measurement errors).30 Cardiovascular risk reduction through weight reduction is likely to act largely through these causal pathways. Indeed, risk scores for the prediction of cardiovascular events have only tended to include markers of adiposity when information on these other risk factors is not available. 31
Perspectives
In Mexico, adiposity is extremely common, and its consequences through blood pressure and diabetes are a major public health concern.3,4,17,32 In 2013, Mexico’s National Strategy for Prevention and Control of Overweight, Obesity and Diabetes, included a range of programs related to health education, improved exercise opportunities, and taxation (eg, of sugary drinks). 33 Our results indicate that, should this strategy be successful, it may lead to considerable population-wide benefits through blood pressure reduction as well as the benefits to be gained by reducing the incidence of diabetes.
Supplementary Material
Novelty and Significance.
What is New?
A need for population-specific thresholds for central adiposity in relation to vascular risk has been proposed, but evidence from Hispanic populations is scarce.
We examined the association of six markers of adiposity to blood pressure among 110,000 Mexican adults.
What is relevant?
All markers of general and central adiposity were continuously and linearly related to blood pressure, with no threshold levels below which less adiposity was not associated with lower blood pressure.
Whereas the relevance of general adiposity to blood pressure was independent of central adiposity, much of the apparent relevance of central adiposity to blood pressure was explained by general adiposity.
Summary.
In this Mexican population, general adiposity was a stronger independent predictor of blood pressure than central adiposity in both men and women, with no evidence of any ‘threshold’ effects.
Acknowledgements
The chief acknowledgement is to the study participants.
Sources of Funding
This work was supported by the Wellcome Trust (grant numbers 058299/Z/99, 090532, 098381), the Mexican Health Ministry (SSA), the National Council of Science and Technology (CONACYT), Cancer Research UK, British Heart Foundation, and the UK Medical Research Council.
Footnotes
Conflicts of interest: None
References
- 1.Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, Qizilbash N, Collins R, Peto R. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. The Lancet. 2009;373:1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. The Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 3.Forouzanfar MH, Alexander L, Anderson HR, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet. 2015;386:2287–2323. doi: 10.1016/S0140-6736(15)00128-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2012;380:2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The NCD Risk Factor Collaboration. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. The Lancet. 2016;387:1377–1396. doi: 10.1016/S0140-6736(16)30054-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The NCD Risk Factors Collaboration. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. The Lancet. 2016;16:31919–31915. doi: 10.1016/S0140-6736(16)31919-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lim SS, Vos T, Flaxman AD, Danaei G, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Timpson NJ, Harbord R, Davey Smith G, Zacho J, Tybjærg-Hansen A, Nordestgaard BG. Does Greater Adiposity Increase Blood Pressure and Hypertension Risk?: Mendelian Randomization Using the FTO/MC4R Genotype. Hypertension. 2009;54:84–90. doi: 10.1161/HYPERTENSIONAHA.109.130005. [DOI] [PubMed] [Google Scholar]
- 9.Holmes Michael V, Lange Leslie A, Palmer T, et al. Causal Effects of Body Mass Index on Cardiometabolic Traits and Events: A Mendelian Randomization Analysis. American Journal of Human Genetics. 2014;94:198–208. doi: 10.1016/j.ajhg.2013.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fall T, Hägg S, Mägi R, et al. The Role of Adiposity in Cardiometabolic Traits: A Mendelian Randomization Analysis. PLoS Med. 2013;10:e1001474. doi: 10.1371/journal.pmed.1001474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42:878–884. doi: 10.1161/01.HYP.0000094221.86888.AE. [DOI] [PubMed] [Google Scholar]
- 12.Wing RR, Bolin P, Brancati FL, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med. 2013;369:145–154. doi: 10.1056/NEJMoa1212914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen Z, Smith M, Du H, Guo Y, Clarke R, Bian Z, Collins R, Chen J, Qian Y, Wang X, Chen X, et al. Blood pressure in relation to general and central adiposity among 500 000 adult Chinese men and women. Int J of Epidemiol. 2015;44:1305–1319. doi: 10.1093/ije/dyv012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The Decoda Study Group. BMI Compared With Central Obesity Indicators in Relation to Diabetes and Hypertension in Asians. Obesity. 2008;16:1622–1635. doi: 10.1038/oby.2008.73. [DOI] [PubMed] [Google Scholar]
- 15.Lee CMY, Huxley RR, Wildman RP, Woodward M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J of Clinical Epidemiology. 2008;61:646–653. doi: 10.1016/j.jclinepi.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 16.Huxley R, James WPT, Barzi F, Patel JV, Lear SA, Suriyawongpaisal P, Janus E, Caterson I, Zimmet P, Prabhakaran D, Reddy S, et al. Ethnic comparisons of the cross-sectional relationships between measures of body size with diabetes and hypertension. Obesity Reviews. 2008;9:53–61. doi: 10.1111/j.1467-789X.2007.00439.x. [DOI] [PubMed] [Google Scholar]
- 17.Sánchez-Castillo CP, Velásquez-Monroy O, Lara-Esqueda A, Berber A, Sepulveda J, Tapia-Conyer R, James T, Philip W. Diabetes and hypertension increases in a society with abdominal obesity: results of the Mexican National Health Survey 2000. Public Health Nutrition. 2005;8:53–60. doi: 10.1079/phn2005659. [DOI] [PubMed] [Google Scholar]
- 18.Berber A, G-S R, Fanghänel G, Sánchez-Reyes L. Anthropometric indexes in the prediction of type 2 diabetes mellitus, hypertension and dyslipidaemia in a Mexican population. Int J of Obesity. 2001;25:1794–1799. doi: 10.1038/sj.ijo.0801827. [DOI] [PubMed] [Google Scholar]
- 19.The World Health Organisation. Waist Circumference and Waist-Hip Ratio. Report of a WHO Expert Consultation. Geneva: WHO Institutional Repository for Information Sharing; 2008. [Accessed September 20, 2016]. http://apps.who.int/iris/handle/10665/44583. [Google Scholar]
- 20.Tapia-Conyer R, Kuri-Morales P, Alegre-Diaz J, Whitlock G, Emberson J, Clark S, Peto R, Collins R. Cohort profile: the Mexico City Prospective Study. Int J Epidemiol. 2006;35:243–249. doi: 10.1093/ije/dyl042. [DOI] [PubMed] [Google Scholar]
- 21.Kuri-Morales P, Emberson J, Alegre-Diaz J, Tapia-Conyer R, Collins R, Peto R, Whitlock G. The prevalence of chronic diseases and major disease risk factors at different ages among 150,000 men and women living in Mexico City: cross-sectional analyses of a prospective study. BMC Public Health. 2009;9:9. doi: 10.1186/1471-2458-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dyer AR, Elliott P, Shipley M, Stamler R, Stamler J. Body mass index and associations of sodium and potassium with blood pressure in INTERSALT. Hypertension. 1994;23:729–736. doi: 10.1161/01.hyp.23.6.729. [DOI] [PubMed] [Google Scholar]
- 23.Owen CG, Whincup PH, Cook DG. Are early life factors responsible for international differences in adult blood pressure? An ecological study. Int J of Epidemiol. 2005;34:649–654. doi: 10.1093/ije/dyi046. [DOI] [PubMed] [Google Scholar]
- 24.O'Donnell M, Mente A, Rangarajan S, et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014;371:612–623. doi: 10.1056/NEJMoa1311889. [DOI] [PubMed] [Google Scholar]
- 25.He FJ, Li J, Macgregor GA. Effect of longer-term modest salt reduction on blood pressure. The Cochrane Database of Systematic Reviews. 2013:CD004937. doi: 10.1002/14651858.CD004937.pub2. [DOI] [PubMed] [Google Scholar]
- 26.O'Brien E, Asmar R, Beilin L, et al. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821–848. doi: 10.1097/00004872-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Kotsis V, Stabouli S, Papakatsika S, Rizos Z, Parati G. Mechanisms of obesity-induced hypertension. Hypertens Res. 2010;33:386–393. doi: 10.1038/hr.2010.9. [DOI] [PubMed] [Google Scholar]
- 28.Dorresteijn JAN, Visseren FLJ, Spiering W. Mechanisms linking obesity to hypertension. Obesity Reviews. 2012;13:17–26. doi: 10.1111/j.1467-789X.2011.00914.x. [DOI] [PubMed] [Google Scholar]
- 29.The Global BMI Mortality Collaboration. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. The Lancet. 2016;388:776–786. doi: 10.1016/S0140-6736(16)30175-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, Danaei G, for The Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects) Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants. The Lancet. 2014;383:970–983. doi: 10.1016/S0140-6736(13)61836-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.D'Agostino RB, Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 32.Alegre-Díaz J, Herrington W, López-Cervantes M, Gnatiuc L, Ramirez R, Hill M, Baigent C, McCarthy MI, Lewington S, Collins R, Whitlock G, et al. Diabetes and Cause-Specific Mortality in Mexico City. N Engl J Med. 2016;375:1961–1971. doi: 10.1056/NEJMoa1605368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Astudillo O. Country in focus: Mexico's growing obesity problem. Lancet Diabetes and Endocrino. 2014;2:15–16. doi: 10.1016/S2213-8587(13)70160-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.