Abstract
Hydrogen peroxide (H2O2) is an early danger cue required for innate immune cell recruitment to wounds. To date, little is known about whether H2O2 is required for the migration of human adaptive immune cells to sites of inflammation. However, oxidative stress is known to impair T cell activity, induce actin stiffness and inhibit cell polarisation. Here, we show that low oxidative concentrations of H2O2 also impede chemokinesis and chemotaxis of previously activated human T cells to CXCL11, but not CXCL10 or CXCL12. We show this deficiency in migration is due to a reduction in inflammatory chemokine receptor CXCR3 surface expression and cellular activation of lipid phosphatase SHIP-1. We demonstrate that H2O2 acts through a Src kinase to activate a negative regulator of PI3K signalling, SHIP-1 via phosphorylation providing a molecular mechanism for H2O2 induced chemotaxis deficiency. We hypothesise that although H2O2 serves as an early recruitment trigger for innate immune cells, it appears to operate as an inhibitor of T lymphocyte immune adaptive responses that are not required until later in the repair process.
Introduction
Reactive oxygen species (ROS) are known to influence the outcome of T-cell responses. Depending on concentration, exposure time and microenvironment, the effects of ROS on T cells can be very distinct and affect a variety of physiological events including cell proliferation, host defence, differentiation, apoptosis, senescence and activation of growth-related signaling pathways. T cells can physiologically produce low levels of hydrogen peroxide (H2O2) upon TCR and chemokine stimulation, which have been shown to facilitate T cell activation (1, 2). In addition, T lymphocytes are known to express NADPH oxidase enzymes NOX2 (2) and DUOX 1 that catalyze the reduction of molecular oxygen to generate superoxide O2-, which can dismute to generate ROS species. These ROS participate in host defence by killing or damaging invading microbes.(3). However, in several human pathologies including cancer and a variety of autoimmune disorders high levels of pro-oxidants are known to induce T lymphocyte hypo-responsiveness (4). In cancer, this can be harmful due to suppression of potentially tumour reactive T cells (5) whereas in autoimmune disease high levels of ROS are thought to help control self-reactive T cells. As such, the level of ROS within the microenvironment appears to be an important control mechanism influencing T cell fate.
H2O2 has been demonstrated to act as an important early damage cue triggering innate immune cell migration in Drosophila and zebrafish models of in vivo inflammation (6–8). In addition H2O2 has been shown to act as a chemoattractant for mouse peritoneal neutrophils at low concentrations (9) and human neutrophil chemotaxis in response to gradients of H2O2 has been observed in vitro (8). Thus H2O2 appears to be required for innate immune cell migration, however little is known about whether H2O2 is required for the migration of human adaptive immune cells. Recently, H2O2 uptake, through aquaporin-3, was shown to be required for efficient mouse T lymphocyte migration towards CXCL12 (1) suggesting a role in regulating the migration of adaptive immune cells.
Unravelling the mechanism through which H2O2 modulates signalling pathways is vital for understanding its role in T lymphocyte biology. It is widely accepted that H2O2 and ROS can act as second messengers through their ability to reversibly oxidize specific cysteine residues in proteins (10). Indeed, ROS can oxidise phosphatases (11), kinases (8) transcription factors (12) and ion channels (13) to alter intracellular signalling. Cellular signalling cascades commonly activated by several types of reactive oxygen species include the PI3K pathway and Src family kinases, which regulate cellular survival activation and migration, thus establishing a link between oxidative conditions and cellular signalling (14, 15). H2O2 has been shown to enhance PI3K signalling by inactivating the lipid phosphatase PTEN (14). PI3K can also be negatively regulated by the SH2-containing inositol 5'-phosphatase 1 (SHIP-1) that is primarily expressed in hematopoietic cells. SHIP-1 dephosphorylates PtdIns(3,4,5)P3, generating PtdIns(3,4)P2, which leads to inhibition of PH-domain-containing enzymes, that are dependent on PtdIns (3,4,5) P3 for their activation. Whether or not H2O2 has an effect upon SHIP-1 has yet to be determined.
In this study, we show that oxidative signalling inhibits T lymphocyte chemotaxis to the inflammatory chemokine CXCL11, without affecting migration to CXCL12 or CXCL10. We go on to show that this H2O2 induced chemotactic deficiency is due to both reduced surface expression of CXCR3 as well as SHIP-1 activation through activation of a redox sensitive Src family kinase. Similarly, pharmacological activation of SHIP-1 with the allosteric activator AQX1 impaired CXCL11-induced chemotaxis by manipulating PI3K signalling and ERM phosphorylation, providing an exciting new mechanism for the targeted inhibition of PI3K mediated signaling in leukocytes with potential therapeutic opportunities in T lymphocyte driven pathologies.
Materials and Methods
Chemicals
PP2 is an ATP competitive inhibitor of Src-family kinases purchased from Calbiochem. An allosteric SHIP-1 activator referred to as AQX1 was supplied to SGW by Aquinox for research purposes only, the structure of which is shown in Supplementary Figure 1A.
PBMC and naïve CD4+ T lymphocyte isolation from whole blood
Blood (50-100ml) was collected aseptically from healthy volunteers of both sexes within an age range of 21-65 years into sterile disposable 50 ml syringe prepared with 2 U/ml heparin (Sigma-Aldrich). The blood was subsequently diluted with warm sterile RPMI-1640 media without supplements in a ratio of 1:1. 25-35ml of the diluted blood was carefully layered onto 15 ml of Lymphoprep (Axis Shield) in 50ml plastic tubes. Preparations were spun at 250 x g for 30 min; following centrifugation, the mononuclear cell rich interface containing the PBMCs was diluted 1:1 with RPMI-1640 media. PBMCs were washed by centrifugation and re-suspended in un-supplemented RPMI-1640. Naïve CD4+ T lymphocytes were isolated from the freshly isolated PBMC using the naïve CD4+ T cell isolation kit II (Miltenyi Biotec) and the LS column following manufacturers’ instructions.
To clonally expand CD4+ lymphocytes, the washed PBMCs were re-suspended in fully supplemented RPMI-1640 media (10% FCS, 10 μg/ml penicillin, 10μg/ml streptomycin) at an equal volume to that of the original volume of whole blood collected from the donor. Staphylococcal enterotoxin B (SEB) (Sigma-Aldrich) was added at a final concentration of 1 µg/ml for 72 h. The suspension cells were then washed in un-supplemented RPMI-1640 media and re-suspended in the same volume of complete media supplemented with IL-2 (Chemicon) at a final concentration 36 U/ml. The cells were washed, re-suspended and supplemented with fresh IL-2 every two days for 10-14 days maintain cell confluency between 0.1-1x 106 cells/ml. Cells were used 8-14 days post isolation and rested in complete media without IL-2 for 16 h before use. All procedures using human blood were carried out under The University of Bath safety and ethical guidelines for the use of human tissue.
Flow cytometry
Freshly isolated naïve CD4+ and SEB-activated T lymphocytes were washed three times by centrifugation at 250 x g and re-suspended in non-supplemented RPMI-1640 media. After treatment with vehicle or activator as described in the figure legends, cells were fixed using BD Fixation and Permeabilization solution (containing formaldehyde; BD Biosciences) for 30 min at 4°C to allow intracellular staining of proteins. Cells were washed twice in BD PERM/Wash solution (containing sodium azide and saponin; BD Biosciences) solution and incubated with 0.02% (v:v) anti-phospho ERM (Cell Signalling Technology), anti-phospho-SHIP-1 (Cell signalling) diluted in BD PERM/Wash for 30 min at 4°C. Cells were washed twice by centrifugation at 250g and re-suspension BD PERM/Wash solution and then incubated with 0.01% (v:v) anti-rabbit IgG FITC conjugated secondary antibody (Sigma) for 30 min at 4°C. Alternatively, cells were stained with TRITC conjugated phallodin for 30 min. Cells were washed twice in BD PERM/Wash solution, re-suspended in 400 μl ice cold PBS + 1% (v:v) FBS in 5ml rounded-bottom FACs tubes for analysis by BD FACS Canto II flow cytometer and BD FACS DIVA software (BD Biosciences). TRITC stained cells were excited at 547 nm and emission recorded at 573 nm whereas FITC stained cells were excited at 495 nm and emission recorded at 519 nm. Mean fluorescence index (MFI) was used to describe the level of phosphorylated ERM, SHIP-1 protein or actin polymerisation.
Surface receptor expression by flow cytometry
SEB activated T lymphocytes were re-suspended in fully supplemented RMPI-1640 at a concentration of 1*106 cells/ml. Cells were treated with either vehicle or stated concentrations of drugs for 30 min. Cells were washed twice with ice cold FACs buffer (PBS + 2% FCS) then re-suspended in diluted 1/50 (v:v) phycoerythrin (PE) conjugated anti-CXCR3 antibody (R&D biosciences) or PE conjugated IgG isotype control (1/50 v:v dilution; R&D biosciences). Alternatively cells were labelled with either Anti-human CD11a PE-conjugated monoclonal antibody (1/50 v:v dilution; ImmunoTools), anti-human CD49d PE-conjugated monoclonal antibody (ImmunoTools) or PE conjugated IgG antibody. Cell were labelled on ice for 1 h then washed twice more in FACs buffer. Alternatively, cells were incubated with primary antibody 10 μg/ml KIM127 mAb (Gift from Nancy Hogg) for 30 min then washed and incubated to secondary anti-mouse FITC conjugated antibody (dilution 1/50 v:v). Alternatively, cells were incubated with live/dead stain Zombie yellow, CD3 PerCP- , CD4 AF700-, CD8 PECy7-, CD127 PECy5- and CD25 BV421-conjugated monoclonal antibodies (Biolegend) for 30 min on ice. Finally, cells were re-suspended in PBS and placed in 5 ml round-bottomed tubes for analysis by flow cytometry. PE-fluorescence was detected by exciting cells at 496 nm and emission recorded at 576 nm recorded by BD FACSAria flow cytometer and analysed by BD FACs Diva Software. Mean fluorescence index (MFI) was used to describe the level of CXCR3, CD11a and CD49d expression and percentage positive used to describe the subsets of T lymphocytes.
Chemotaxis assay
Cell migration assays were performed using a 96-well plate-based chemotaxis system (NeuroProbe, Inc). Cells were suspended in phenol red free RPMI 1640 with 0.1% BSA at 3.2×106 and treated as described in each figure legend. Lower chambers of the 96-well plate were loaded with 29 μl RPMI (basal conditions) or CXCL11 (10 nM, Peprotech). This was overlaid with a 5-μm pore-size filter and 25 μl of the cell suspension placed above each required well. The plate was incubated at 37°C, 5% CO2 for 3 h after which viable cells in the bottom chamber were counted by flow cytometric analysis. Cell viability was routinely determined with annexin V and propidum iodide staining followed by flow cytometry.
SHIP-1 immunoprecipitation and malachite green phosphate assay
The malachite green phosphate assay was carried out using full-length recombinant SHIP-1 (provided by GlaxoSmithKline) and immunoprecipitated SHIP-1. SEB-activated T lymphocytes were collected by centrifugation at 250 x g and re-suspended in serum free RMPI-1640 media. 1 x 106 cells were lysed for each reaction of the malachite green assay. Samples were rotated for 30 min at 4°C to assist cell lysis after which cells were centrifuged 153 x g, 4°C for 10 min. The supernatant containing SHIP-1 was incubated overnight in 0.01% (v:v) SHIP-1 monoclonal antibody (Cell Signaling Technology). A/G Agarose beads (Peprotech) (5 μl per point of malachite green) were washed twice in lysis buffer without inhibitors, re-suspended in 100 μl and added to the cell lysis of the SEB activated T cells for at least 2 h. Samples were then washed 3 x in 1 ml lysis buffer and 3 x in malachite green reaction buffer (5% (v:v) glycerol, 20mM Tris HCl, 10mM MgCl2; pH 7.4) to remove all proteins not attached to the A/G agarose beads and re-suspended in 20 μl of reaction buffer/point. The immunoprecipitated SHIP-1 was then used in the malachite green phosphate assay. Full length recombinant SHIP-1 was diluted to 1μM in reaction buffer and assessed in the malachite green reaction. SHIP-1 can dephosphorylate the in vitro substrate D-Ins(1,3,4,5) tetrakisphosphate to produce Ins(1,3,4)P3 and free phosphate. A malachite green solution can react with the free phosphate to give a rapid colour change from yellow to green. 20 μl of immunoprecipitated SHIP-1 solution, or 1 μM recombinant SHIP-1 was added to each of the required wells of a 96 well plate and incubated with SHIP-1 activators, inhibitors or H2O2 at given concentrations for 5 min at room temperature. 100µM substrate D-Ins (1,3,4,5)P4 (Echelon Biosciences) was added for 30 min at 37°C. 100 µl malachite green solution (Echelon) was added to each well and incubated for 15 min at room temperature in the dark. The plate was then read at 650 nm using a FluoStar Optima plate reader.
Immunoblotting
To analyse the effect of exogenous H2O2 on SHIP-1 activity, cells were treated as described in RPMI 1640 medium, centrifuged and lysed in 50 μl lysis buffer (50 mM Tris-HCl [pH 7.5], 150 mM NaCl, 1% Nonidet P-40, 5 mM EDTA, 1 mM sodium vanadate, 1 mM sodium molybdate, 10 mM sodium fluoride, 40 μg/ml PMSF, 0.7 μg/ml pepstatin A, 10 μg/ml aprotinin, 10 μg/ml leupeptin and 10 μg/ml soybean trypsin inhibitor). Samples were rotated at 4°C for 20 min and centrifuged at 600 x g for 10 min. Supernatant was transferred to fresh tubes and diluted 1:5 with 10% SDS containing sample buffer and samples were subjected to SDS-PAGE electrophoresis and immunoblotting following standard procedures.
Adhesion assay
A flat-bottomed 96-well plate was coated with either 10 µg/ml recombinant human fibronectin (R & D systems) or 10 µg/ml recombinant human ICAM-1 (R & D systems) overnight. Plate was washed twice with pre-warmed PBS, then un-supplemented RPMI media (without phenol red). SEB activated cells were washed twice into un-supplemented media and treated with the stated concentrations of compounds for 30 min. Cells were then added to the 96-well plate and stimulated with the TCR antagonist UCHT-1 at a concentration of 10μg/ml. The plate was sealed and incubated for 30 min at 37°C to allow cells to adhere. The plate was then inverted for 15 min after which seal was removed whilst the plate was still inverted, all media and non-adherent cells removed from plate and wells washed gently with PBS. The adherent cells were quantified using the MTT assay as per manufacturers’ instructions and absorbance was recorded using a FluoStar Optima plate reader at 540 nm.
Immunostaining and confocal microscopy
1x 106 cells were stimulated as required and fixed in BD Fixation and Permeabilization (PERM) solution (BD Biosciences) for 30 min at 4°C. Cells were washed twice via centrifugation at 250 x g and re-suspension in BD PERM/Wash solution (containing sodium azide and saponin; BD Biosciences) and then incubated with 0.02% (v:v) anti-phospho ERM antibody (Cell Signalling Technology) in BD PERM/Wash solution overnight at 4°C. Cells were washed twice in BD PERM/Wash solution, re-suspended in 0.01% (v:v) goat anti-rabbit Fluorescein isothiocyanate (FITC) conjugated secondary antibody diluted in PERM/Wash solution overnight at 4°C. Cells were then washed and re-suspended in 20μl PERM solution, and cells pipetted into Mowiol to adhere coverslips to slides. Cells were visualized using a Zeiss LSM 510 Meta confocal microscope using Plan-Apochromat 63x/1.4 Oil DIC objectives. Cells were excited by 488nm light and fluorescence emission was collected at 520nm with a band pass filter of 530 ± 15nm. Images were collected at 2 x zoom.
Data analysis
Data was normalised as described in the figure legends. Values are presented as mean ± standard error of the mean (SEM) and n represents the total number of donors or individual repeats of each study. Statistical analysis was undertaken using GraphPad Prism software. Data was analysed using a One Way ANOVA followed by a Dunnett’s post-test to determine significant difference as compared to control or when there were two independent variables a two-way ANOVA with Bonferrori post-test was used Differences were considered significant when * P<0.05, **P<0.01 ***P<0.001.
Results
H2O2 potently impairs T lymphocyte migration to CXCL11 but not to CXCL12 or CXCL10
To investigate the affect of H2O2 on migration of human T lymphocytes we used a neuroprobe migration assay to firstly test whether H2O2 can act as chemo-attractant for SEB-activated human T cells. Surprisingly, H2O2 added to the bottom well of the neuroprobe plate caused a concentration dependent decrease in SEB-activated T lymphocyte migration when compared to media alone. Migration was significantly impaired at 10 μM H2O2 and by 1 mM almost completely inhibited with an IC50 of 2.5 μM (Figure 1A).
Figure 1. Hydrogen peroxide potently inhibits T lymphocyte migration to CXCL11.
(A) SEB activated T cell migration towards either basal or increasing concentrations of H2O2 (**p<0.01). (B) Basal or CXCL11 (10nM) induced migration of SEB activated T cells pre-treated with increasing concentrations of H2O2 (*p<0.05, **p<0.01 or ***p<0.001). (C) Basal or chemokine induced migration of SEB activated T cells pre-treated with indicated concentrations of catalase (*p<0.05, ##p<0.01, ###p<0.001). (D) Basal or CXCL11 (10nM) induced migration of SEB activated T cells pre-treated with increasing concentrations of H2O2 (*p<0.05, **p<0.01 or ***p<0.001). (E) Basal or CXCL11 (10nM) induced migration of SEB activated T cells pre-treated with increasing concentrations of SOD dismutase mimetic, MnTBAP chloride (*p<0.05, **p<0.01 or ***p<0.001). (F) Basal or CXCL10 (10nM) induced migration of SEB activated T cells pre-treated with increasing concentrations of H2O2 (*p<0.05 or **p<0.01). (G) Basal or CXCL12 (10nM) induced migration of SEB activated T cells pre-treated with increasing concentrations of H2O2 (*p<0.05 or **p<0.01). For all graphs, migrated cells were counted using flow cytometry, data are the mean values ± SEM of three or four independent experiments.
Since H2O2 appears to operate as a negative regulator of T cell migration, we investigated the effect of pre-treating T lymphocytes directly with H2O2 to further examine its impact on both basal and CXCL11-induced migration. Basal migration was not significantly inhibited except at a concentration of 100 μM H2O2 (Figure 1B). However, CXCL11-induced SEB-activated T lymphocyte migration was significantly reduced by H2O2 in a concentration-dependent manner (Figure 1B). Consistent with this negative role of H2O2, scavenging of extracellular H2O2 via the addition of catalase, resulted in an increase of both basal and CXCL11-stimulated T cell migration (Figure 1C), whilst heat-inactivated catalase had no effect (data not shown).
We next investigated the chemotactic responses of SEB-activated T lymphocytes towards increasing concentrations of CXCL11 following pre-treatment with 100 μM H2O2. Maximal migration occurred at 10 nM for both vehicle control and H2O2 pre-treated cells, demonstrating that H2O2 does not alter T lymphocyte sensitivity to CXCL11 (Figure 1D). Maximal migration could not be reached by increasing the concentration of CXCL11, suggesting that H2O2 is not acting as a competitive inhibitor of CXCL11. Consistent with H2O2 pre-treatment, SOD dismutase mimetic, MnTBAP chloride, which increases intracellular H2O2 (increased intracellular ROS levels were observed using DCF shown in Supplementary Figure 2B), inhibited SEB-activated T lymphocyte basal and CXCL11-induced migration (Figure 1E).
As H2O2 significantly impaired migration towards CXCL11, we next investigated its effect upon chemotactic migration to another CXCR3 ligand, the inflammatory chemokine CXCL10, as well as the homeostatic chemokine CXCL12 that binds to CXCR4 (Figure 1F-G). Although CXCL11 and CXCL10 are both induced by IFNγ and thought to promote Th1 immune responses (16–18), they have previously been shown to have distinct expression patterns, potencies and efficacies in a number of assays, including internalisation and migration (19–21). In the neuroprobe assay, CXCL11 significantly increased SEB T lymphocyte migration 6.9 ± 0.9 fold over basal migration, whereas CXCL10 was less potent and migration was increased 3.1 ± 0.9 fold over basal migration (data not shown). The fact that CXCL10 and CXCL11 exhibit distinct efficacies to CXCR3 suggest that they interact with CXCR3 in different ways and are likely to stabilize different conformations of the receptor (22). Strikingly, H2O2 exposure had no affect on CXCL10-induced migration with migration only becoming inhibited upon exposure to extremely high concentrations (1 mM) (Figure 1F). This shows that H2O2 specifically affects CXCL11-induced migration and not migration to CXCL10 despite the two engaging the same receptor (CXCR3).
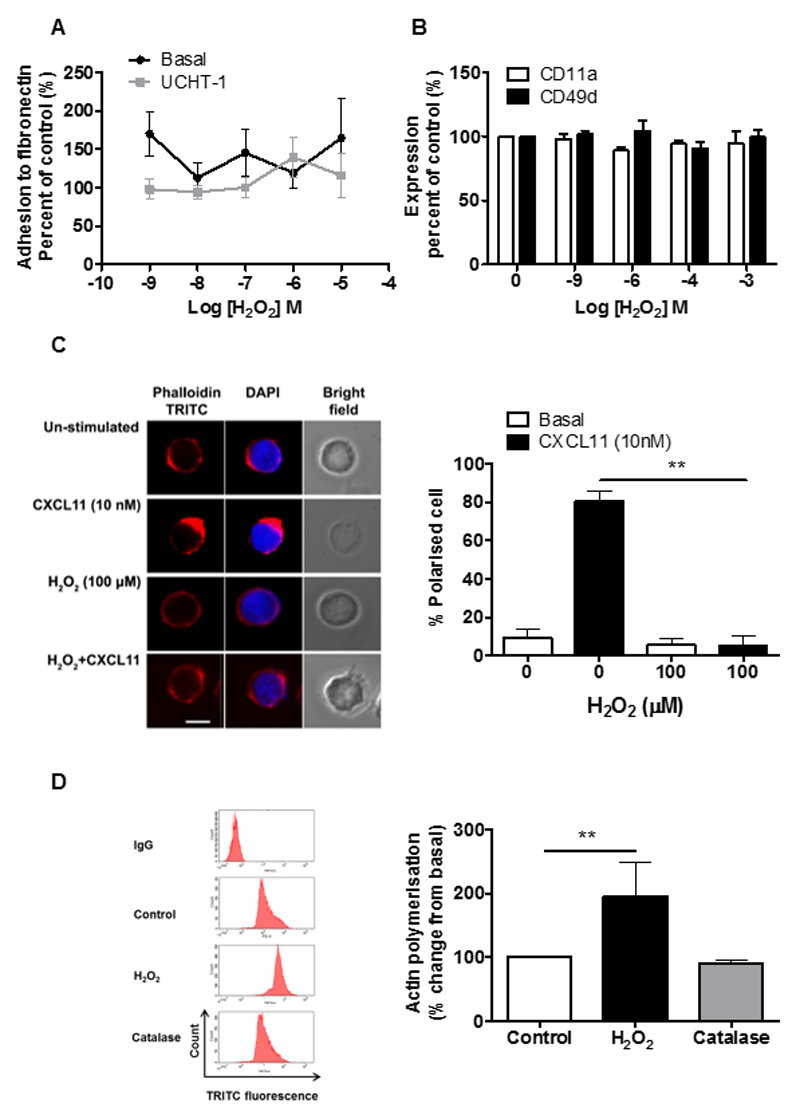
H2O2 causes a defect in actin polarisation in T cells but has no effect upon adhesion
Ligation of the TCR is known to increase adhesion of T lymphocytes to both the extracellular matrix and other cells, which is critical for their migration, extravasation, and formation of immunological synapses (23). The adhesion of SEB-activated T lymphocytes was examined following H2O2 treatment to determine whether altered adhesion could be the underlying reason for their reduced ability to migrate. Interestingly, H2O2 had no effect upon basal or UCHT-1-induced adhesion to fibronectin (Figure 2A) and had no effect upon the expression of the α-subunit of integrin receptors LFA-1 (CD11a subunit) or α4β1 (CD49 subunit) (Figure 2B). H2O2-induced inhibition of T cell chemotaxis is therefore not due to disrupted adhesion.
Figure 2. Effect of H2O2 and CXCL11 upon polarisation of SEB-activated T lymphocytes.
(A) 1 x106 SEB-activated T lymphocytes (8-12 days post isolation) were pre-treated with 100 μM H2O2 for 30 min then stimulated with 10 nM CXCL11 for 5 min. Then cells were fixed in BD fixation reagent, permeabilised with BD permeabilisation reagent and stained with TRITC tagged phallodin and DAPI. (Left panel) Immunofluorescence microscopy representative images showing actin and DAPI staining. The scale bar represents 10 μm. (Right panel) Represents the mean ± SEM percentage of polarised cells observed from three independent donors, with 20 cells counted for each condition. Statistical significance was determined by two-way ANOVA with a Bonferroni post-test where **p<0.01 compared to control. (B) H2O2, but not catalase, increases actin polymerisation of SEB-activated T lymphocytes. 1 million SEB-activated T lymphocytes (8-12 days post isolation) were washed three times in serum free media and treated with H2O2 (100 μM) or catalase (1 mg/ml) for 30 min. Cells were fixed using BD fixation reagent for 20 min, permeabilized and incubated with TRITC tagged phallodin for 30 min. Mean fluorescence intensity per 10,000 cell was measured using flow cytometry. Data are (left panel) representative FAC plots from one donor and (right panel) mean ± SEM minus IgG control, normalised to the untreated control from three independent donors. Statistical significance was determined by one way-ANOVA with Dunnett’s post-test where **p<0.01 compared to control. (C) 1 x 106 SEB-activated T lymphocytes were pre-treated with increasing concentrations of H2O2 for 30 min. Cells were stimulated with UCHT-1 (10µg/ml) for 5 min, before being allowed to adhere to fibronectin (10µg/ml) coated 96 well plates for 30 min. The plate was sealed and turned upside down for 15 min. Wells were washed gently with PBS to remove any un-adhered cells. Cells were then scrapped and counted using flow cytometry. Graph to show percent change from basal. (D) Cells were treated with increasing concentrations of H2O2 for 30 min and then expression of CD11a and CD49d were assessed using PE-conjugated antibodies and analysed by flow cytometry. Data are represented as percentage change from basal and mean ± SEM of three independent experiments.
In response to chemotactic signals, T cells reorganize their actin cytoskeleton and become polarized towards the chemoattractant gradient, which leads to chemotaxis and T cell trafficking (24, 25). CXCL11-stimulated T cells develop a polarized morphology at the leading edge known as the uropod (26), which was visualized with phalloidin staining (Figure 2C). In contrast, H2O2 treated T cells failed to develop uropods; instead they exhibited irregular patch-like F-actin staining (Figure 2D). CXCL11-induced polarization was significantly impaired in H2O2 treated T cells (Figure 2C). Interestingly, H2O2 significantly increased the level of polymerised F-actin detected to 195 ± 30% of control levels with catalase pre-treatment being able to rescue the effect upon the level of polymerised F-actin (Figure 2D). Our data suggest that high concentrations of H2O2 could impair T lymphocyte migration by mis-regulation of the actin cytoskeleton inhibiting the ability of the cell to polarise towards CXCL11.
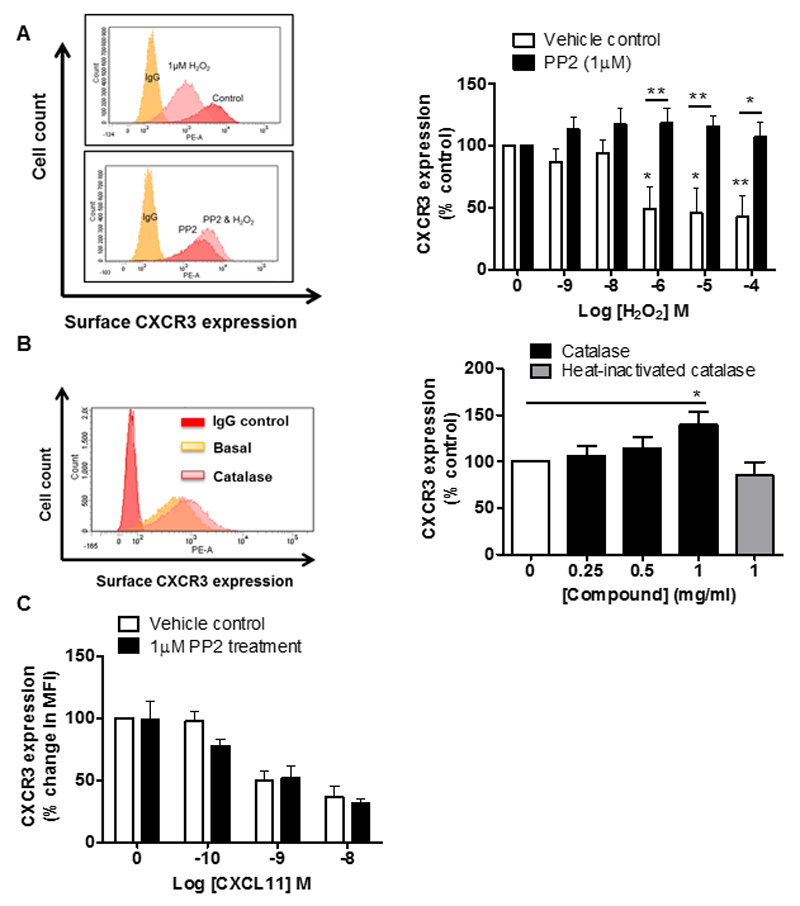
Src Family Kinases are required for the H2O2-induced decrease in CXCR3 surface expression
One potential mechanism by which H2O2 may act as an inhibitor of CXCL11-induced migration and actin polarisation is by affecting the trafficking of the CXCL11 receptor. Following antigen encounter, the chemokine receptor CXCR3 is up-regulated on T lymphocytes and is crucial for their CXCL11-guided recruitment into inflamed tissues (17). To determine the effect of H2O2 on CXCR3 surface expression, SEB-activated T lymphocytes were treated with increasing concentrations of H2O2 for 30 min and CXCR3 surface expression was determined by flow cytometry. H2O2 treatment caused a reduction in CXCR3 expression with an IC50 2 μM (Figure 3A). Thus, H2O2 significantly decreased the expression of CXCR3 at concentrations that affect migration but are not cytotoxic (Supplementary Figure 3) and have no effect on polarisation to different T cell subsets (Supplementary Figure 4 A-C). Since cells were exposed to H2O2 for only 30 min prior to analysis, this change in surface expression is unlikely to be due to transcriptional changes, but is more likely due to an effect upon CXCR3 trafficking. Consistent with this, we found that addition of catalase led to an increase in surface expression levels of CXCR3, which was not observed when using heat-inactivated catalase (Figure 3B).
Figure 3. Exogenous H2O2 requires Src kinase to reduce surface expression of CXCR3.
(A) Left panel shows representative FACS plots from a single donor showing affect of H2O2 on CXCR3 expression in SEB-activated T lymphocyte with or without PP2 (1μM) treatment. Right panel shows the mean ± SEM of three independent donors, normalised to the un-treated control. Statistical significance was determined by two-way ANOVA with Bonferroni’s post-test where *p<0.05 or **p<0.01 as compared to control and #p<0.05, #p<0.01 comparison with H2O2. (B) Left panel shows a representative FACS plot for a single donor showing effect of catalase on CXCR3 expression. Right panel shows the mean ± SEM of three independent donors, normalised to the un-treated control. Statistical significance was determined by one way-ANOVA with Dunnett’s post-test where *p<0.05 as compared to control. (C) Graph showing effect of increasing concentrations of CXCL11 on CXCR3 expression in SEB activated T lymphocytes pre-treated with Src kinase inhibitor PP2 (1 μM). Level of surface CXCR3 expression was determined using PE conjugated CXCR3 antibody. Data are mean values ± SEM of three independent experiments.
Studies in zebrafish and Drosophila have identified the Src family kinase Lyn (Src42A in Drosophila) as being a target of H2O2 in blood cells (8, 27) with this kinase containing a critical redox sensitive cysteine residue. In order to test whether Src family kinases are playing a role in H2O2 induced inhibition of T cell migration, cells were pre-treated with the Src-Family Kinase inhibitor PP2 which abrogated down-regulation of CXCR3 surface expression triggered by H2O2 (Figure 3A). This suggests therefore, that H2O2-induced CXCR3 down-regulation in activated T lymphocytes requires Src family kinase (SFK) signalling.
CXCR3 internalisation occurs rapidly upon agonist activation of the receptor and is a critical mechanism by which GPCR signalling is regulated. As H2O2 also appears able to regulate the expression of CXCR3 through SFK signalling, we were interested if CXCL11 also internalises the receptor through SFK signalling. CXCL11 evoked a concentration dependent reduction in the expression of CXCR3, however SFK inhibition had no effect upon CXCL11-induced down-regulation of CXCR3 (Figure 3C). This demonstrates that H2O2 and CXCL11 induce distinct intracellular signalling mechanisms to internalise the CXCR3 receptor.
Our results show that H2O2 specifically affects CXCL11 induced migration but not migration to CXCL10, despite them engaging the same receptor. We therefore wanted to determine whether they have differential effects upon CXCR3 internalisation, which could provide a potential explanation for the distinct migratory effects. We and others have previously shown that CXCL11 was more potent than CXCL10 at reducing the expression of CXCR3 (28, 29). Thus, decreased CXCR3 surface expression following H2O2 exposure could lead to desensitisation of the T cell to CXCL11, whilst leaving sufficient CXCR3 expression for sensitivity towards CXCL10. As expected, CXCL12 triggered internalisation of its receptor CXCR4 but not CXCR3 (Data not shown). Consistent with its lack of effect upon CXCL12 induced migration, H2O2 had no effect upon the surface expression of CXCR4 (Data not shown).
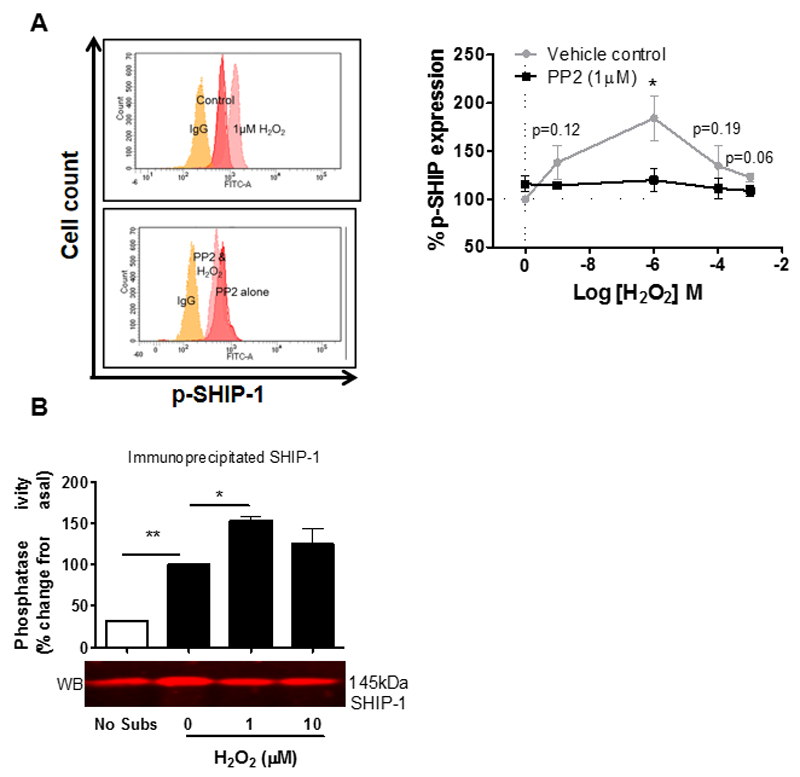
Src kinases are required for H2O2-induced SHIP-1 phosphorylation and activation of its catalytic activity
The effect of H2O2 upon SHIP-1 has not been established, although SHIP-1 expression has been shown to enhance cell survival in response to oxidative stress (30) and SHIP-1 has been shown to have vital roles in the regulation of human SEB-activated T lymphocytes ( 31). Upon cell stimulation, SHIP-1 is recruited to the membrane where it is tyrosine phosphorylated upon Y1020, which lies in the second NPXY motif towards its C-terminal. Phosphorylation is used as a marker of activated SHIP-1, when SHIP-1 is located at the cell membrane (32) and is able to bind the phosphotyrosine binding (PTB) domains of Shc (33), Dok1 and Dok2 (34). We found that H2O2 increased SHIP-1 phosphorylation in a dose dependent manner; with maximal phosphorylation at 1 μM (Figure 4A) SHIP-1 phosphorylation occurs at concentrations of H2O2 that do not affect cellular viability, but do significantly alter the migration of T lymphocytes to CXCL11. In addition, we examined the effect of high concentrations H2O2 upon total SHIP-1 protein by Western Blot and determined that H2O2 has no effect upon degradation of SHIP-1 (Supplementary Figure 4D).
Figure 4. H2O2 requires a Src-family kinase to phosphorylate and enhance the catalytic activity of SHIP-1.
(A) Left panel shows a representative FACS overlay from one donor showing effect of H2O2 on anti-phospho SHIP-1 levels in T cells with or without PP2 treatment (1 μM). Right panel shows the mean values ± SEM from 4 independent donors. (B) effect of H2O2 (1 μM) on the catalytic activity of SHIP-1 protein immunoprecipitated from 1 x 106 SEB activated T lymphocytes. Catalytic activity was quantified using a malachite green phosphatase assay and protein concentration determined by western blot. Data are mean values ± SEM of three independent experiments.
Since SHIP-1 phosphorylation has previously been described to be dependent on SFKs in B lymphocytes (35), we wondered whether this H2O2-mediated effect might also be operating via Src family kinases. We found that PP2 significantly impaired H2O2-induced SHIP-1 phosphorylation (Figure 4A), indicating that H2O2-induced SHIP-1 phosphorylation does indeed require SFK activity. As SHIP-1 phosphorylation is used as a marker of activated SHIP-1, we wanted to determine whether H2O2 has an effect upon the catalytic ability of SHIP-1. Subsequent analysis showed that H2O2 had no effect upon the catalytic ability of recombinant SHIP-1 on a malachite green phosphatase assay (data not shown). Therefore unlike PTEN, the catalytic activity of SHIP-1 does not appear to be decreased by oxidation.
Since SHIP-1 phosphorylation required SFK activity, we wanted to understand how H2O2-induced cellular signalling could alter the catalytic activity of native SHIP-1. Directly treating immunoprecipitated SHIP-1 with H2O2 does not allow for any H2O2-induced signalling that could alter the catalytic activity of SHIP-1 within the cell. Therefore, SHIP-1 was immunoprecipitated from either untreated or H2O2-treated T cells and the catalytic activity determined by malachite green assay. The amount of immunoprecipitated SHIP-1 in each sample was determined by western blot. SHIP-1 immunoprecipitated from the cells treated with H2O2 had significantly increased catalytic activity as compared to the untreated controls (Figure 4B). These results show that oxidative signalling plays a key role in activating the lipid phosphatase SHIP-1 via a Src family kinase and that this SHIP activation then negatively regulates CXCL11 induced migration.
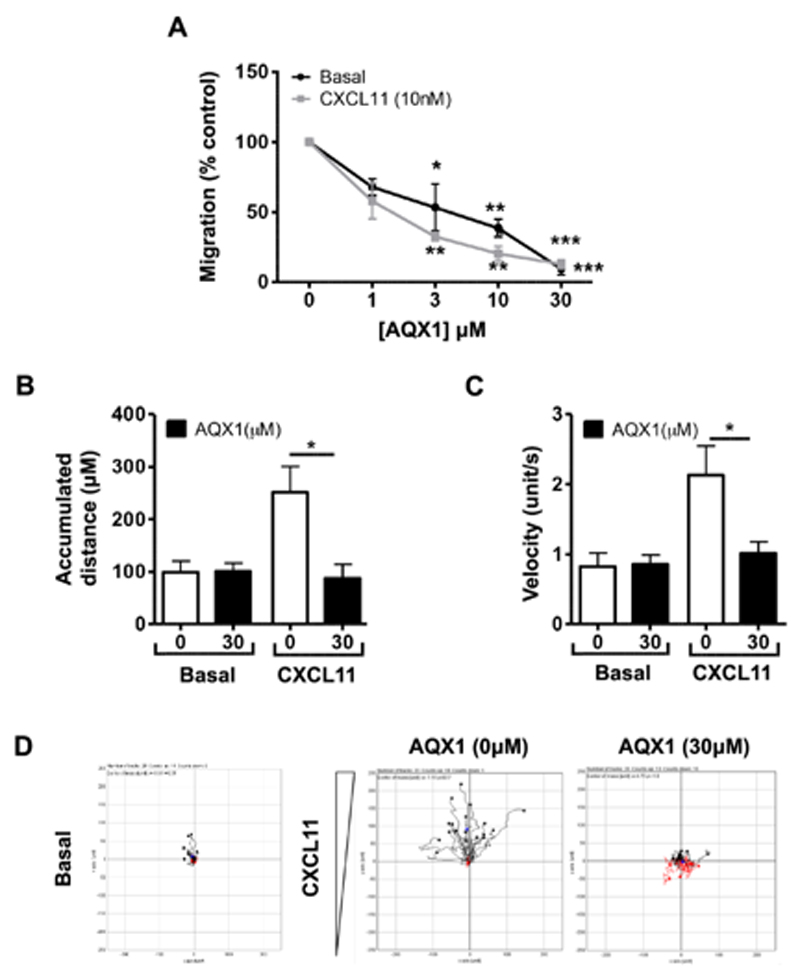
Pharmacological activation of SHIP-1 inhibits the migration of lymphocytes by reducing PI3K signalling and modulating ERM proteins phosphorylation
Similar to the activation of SHIP-1 by H2O2 and the chemotactic inhibition of T cells towards CXCL11 post treatment with H2O2, the allosteric SHIP-1 activator, AQX1 also significantly impeded previously activated T lymphocyte migration to the same chemokine on a Neuroprobe assay (Figure 5A). The ability of AQX1 to activate SHIP-1 was verified by direct application of AQX1 on recombinant SHIP-1 (Supplementary Figure 1B). Migration of T cells in presence of AQX1 was also assessed using the IBIDI μ-slide chemotaxis assay that allows tracking of individual cells across a fibronectin-coated surface (Figure 5B, C and D). Pharmacological activation of SHIP-1 was found to abrogate CXCL11 mediated migration as measured by accumulated distance and velocity. Using the IBIDI assay, we did not observe a reduction in basal migration in the presence of AQX1. However, this assay has negligible basal migration compared to the NeuroProbe assay. Although pharmacological activation of SHIP-1 had no effect upon CXCR3 expression (data not shown), consistent with the impaired migration ability AQX1-mediated SHIP-1 activation was found to reduce CXCR3/CXCL11 induced phosphorylation of Akt (Figure 6B).
Figure 5. SHIP-1 modulation reduces CXCL11 mediated migratory responses in activated T lymphocytes.
(A) Previously SEB-activated T cells were treated with AQX1 (1-30 µM) for 30 min. Basal and chemotactic migration to CXCL11 (10 nM) was assessed using the Neuroprobe chemotaxis assay as described in the Materials and Methods. Data is expressed as % inhibition of migration and is mean ± SEM of three independent experiments. (B-D) In addition, the migration of previously activated T cells treated with AQX1 (30 µM) with or without CXCL11 (100 nM) gradient was also assessed using IBIDI 2D Chemotaxis μ-slides and video microscopy as described in the Materials and Methods. Data represents three separate experiments with twenty cells recorded under each condition in each experiment, where (B) accumulated distance (µm) and (C) velocity (unit/second) are the mean ± SEM from three independent experiments. Panel (D) represents individual tracks of cell tracks from a single representative experiment. Significance is represented * p<0.05, **p<0.01 and ***p<0.001 (one way ANOVA with Dunnett’s post-test).
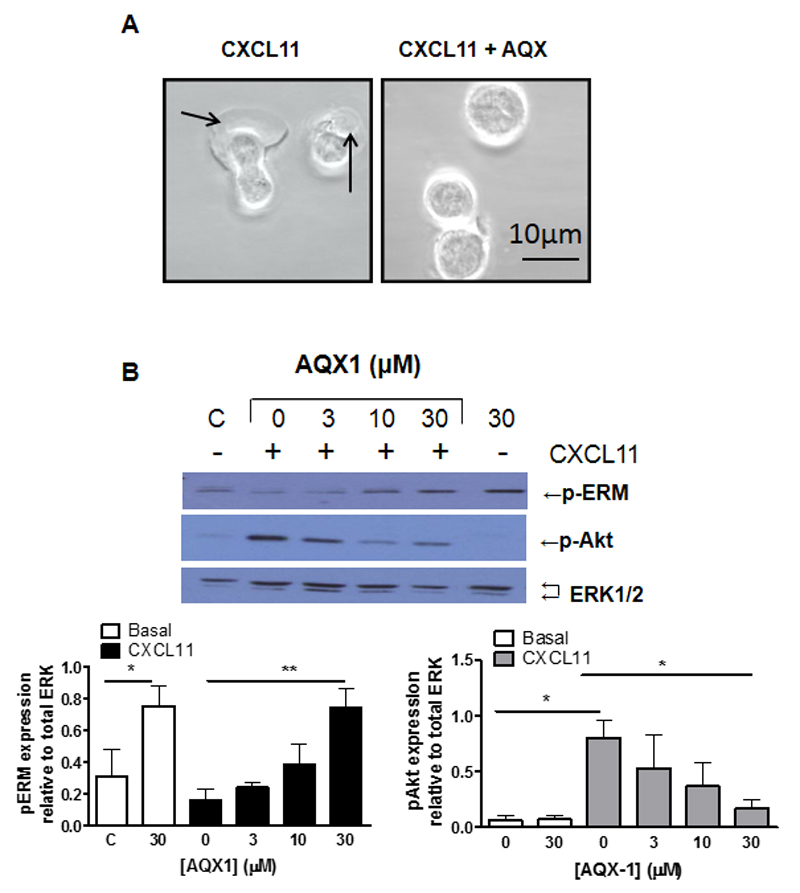
Figure 6. SHIP-1 modulation inhibits polarisation and alters the phosphorylation state of ERM proteins in T lymphocytes.
(A) Previously activated T cells were treated with AQX1 (30 µM) and allowed to equilibrate upon a poly-L-lysine (0.1 mg/ml) coated IBIDI µ-slides. Cells were stimulated with CXCL11 (100 nM) and lamellipodia extension observed using the Zeiss LSM 510 META microscope. (B) Previously-activated T lymphocytes were incubated either with vehicle control (labelled C) or AQX1 (3-30 µM) for 30 min then stimulated with CXCL11 (10 nM) as indicated for 5 min. Levels of phosphorylated ERM, phosphorylated Akt and total ERK were assessed using immunoblotting. Upper panel is a representative Westerns blot from a single experiment. The right panel are mean ± SEM of phosphorylated ERM relative to total ERK and left panel mean ± SEM of phosphorylated Akt relative to total ERK, from three independent experiments. Significance is represented *p<0.05 & **p<0.01 (one way ANOVA with Dunnett’s post-test).
In addition, SHIP-1 activation and inhibition prevented lamellipodia extension (Figure 6A). Phosphorylation of ezrin, radixin and moesin (ERM) proteins, which link the actin cytoskeleton to the cell surface membrane, have previously been implicated in cell migration and adhesion (36). In T lymphocytes, the phosphorylation of ERM proteins is rapidly reduced by chemokine stimulation (37). In addition, silencing of SHIP-1 expression in T lymphocytes was found to cause the de-phosphorylation of ERM proteins (31). Pharmacological SHIP-1 activation by AQX1 treatment enhanced the phosphorylation of ERM proteins in previously activated T lymphocytes under unstimulated conditions, whilst exposure to chemokine CXCL11 (Figure 6B) caused a de-phosphorylation of ERM proteins. However, activation of SHIP-1 with AQX1, prevented CXCL11 mediated ERM de-phosphorylation (Figure 6B).
Discussion
In this study we have shown that H2O2 pre-treatment induced a selective and robust inhibition of T cell chemotactic migration towards CXCL11 but not towards CXCL12 or CXCL10. This implies that H2O2 has a precise signalling effect upon the CXCR3 receptor. We addressed whether H2O2 treatment could alter the ability of T lymphocytes to adhere, as the adhesion of lymphocytes to components of the extracellular matrix and other cells is critical for successful cell migration, extravasation and the formation of immunological synapses (38). It has also been previously reported that H2O2 can alter β2- integrin CD11b/CD18-activation and enhance neutrophil adhesion (39). Furthermore, H2O2 has been described to induce VCAM-1 expression in B cells through extracellular Ca2+ influx (40) and enhance leukocyte adhesion to endothelial cells via NFκβ dependent gene regulation of VCAM-1 (41). Our experiments (data not shown) revealed that H2O2 had no effect upon either basal or TCR-stimulated adhesion to fibronectin nor on expression of the integrin receptors, LFA-1 (CD11a expression) and α4β1 (CD49d expression) in SEB-activated T lymphocytes. Defective adhesion cannot therefore explain the inhibitory effect of H2O2 on CXCL11 induced migration.
Instead, our results show that H2O2 has an important role in actin regulation within activated T lymphocytes. H2O2 significantly increased the level of F-actin and inhibited actin polarisation to CXCL11 in SEB-activated T lymphocytes. This effect on the actin cytoskeleton is likely to be one mechanism underlying the ability of high concentrations of H2O2 to inhibit migration and is consistent with previous studies showing that preventing H2O2 uptake impairs actin polymerisation in murine T lymphocytes (1), whilst oxidative stress enhances actin polymerisation and impairs actin polarisation to chemokine stimulation in human naïve T lymphocytes (42).
To further dissect the mechanism underlying the H2O2 induced migratory defect, we evaluated the effect of H2O2 upon the surface expression of CXCR3, the cognate receptor of CXCL11. Chemokine receptors, such as CXCR3 undergo internalisation and recycling to regulate their signalling. Receptor internalisation decreases the amount of available receptor on the cell surface, attenuating receptor mediated signalling and migration (43, 44). The H2O2 treatment we performed was limited to 30 min so that changes in surface expression were likely to affect the internalisation of the receptor and not the overall expression of the receptor through gene transcription. Consistently with the migratory defect, non-toxic concentrations of H2O2 significantly decreased the cell surface expression of CXCR3 in our model. Moreover, SFK inhibition completely attenuated this effect. H2O2 inactivates the phosphatase PTEN (14, 15) and therefore has been presumed to also inactivate the lipid phosphatase SHIP-1, which acts by dephosphorylating the membrane-bound PtdIns(3,4,5)P3, generated by PI3Kinase, and has thus been described as a negative regulator of immune receptor, cytokine and growth factor receptor signalling. Furthermore, SHIP-1 can interact with a large number of proteins via its SH2 and NPXY containing domains influencing numerous signalling pathways. We found that low concentrations of H2O2 induced the phosphorylation and enhanced the catalytic activity of cellular SHIP-1 through SFK-dependent signalling. We have shown that SHIP-1 activation severely impedes the migration of activated T lymphocytes and that SHIP-1 activation enhances the phosphorylation of ERM proteins. Although we have not definitively shown that H2O2 can induce the phosphorylation of ERM in T lymphocytes, it has previously been shown in other cells to be induced by H2O2 (45) and we therefore suggest that SHIP-1 activation offers one potential mechanism by which H2O2 impairs T cell migration..
The down-regulation of CXCR3 and the enhanced activity of SHIP-1 triggered by H2O2 could operate in concert to inhibit CXCL11 dependent T cell migration. Since we have shown that both these effects are dependent on SFK activity it now becomes important to identify which kinase mediates these responses. The SFK member Lyn has been indicated as a redox sensor involved in early neutrophil recruitment to H2O2 at wounds. Mutation of a single conserved cysteine residue to alanine at position Cys466 abolished the ability of Lyn to be oxidised by H2O2. This mutation resulted in an inability of the cell to detect and migrate towards a H2O2 gradient (8). Lck and Fyn are expressed in T lymphocytes and contain the critical cysteine 466 residue and Lck has been reported to have redox sensitivity (46). Further work is needed to address the precise role of Lck and Fyn in regulating T cell migration downstream of ROS.
There is growing evidence that ROS are not merely an unwanted by-product of aerobic respiration that cause unwanted damage. Instead they are critical signalling molecules that are required for co-ordinating crucial physiological processes. The unconventional concentration dependent effect with increasing concentrations of H2O2, likely reflects that H2O2 is known to have many diverse effects upon signalling proteins and hence, oxidation of different additional proteins could occur at distinct concentrations. We have shown that H2O2 has significant functional and signalling responses at low physiological concentrations, which have no effect on cell viability.
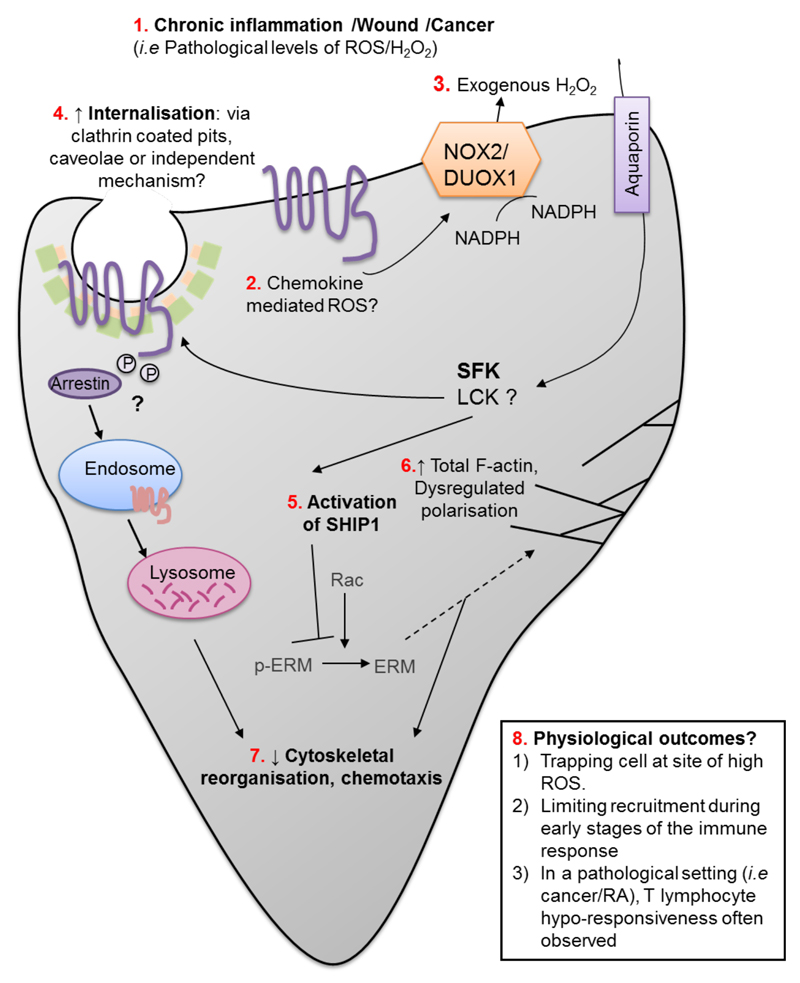
Previous studies have shown that ROS can influence the migration of innate immune cells in many systems and in this study we identify a novel effect of ROS on human T cell migration. We propose that such inhibition could dampen the recruitment of adaptive immune cells that are required later in the wound repair process. In contrast, exposure of T cells to low levels of ROS could restrict them to inflamed sites facilitating the resolution of inflammation whereas in a pathological setting, high ROS levels could cause wide-spread suppression of T lymphocyte migration and aid cancer cell survival or prolong chronic infection (Figure 7).
Figure 7. Model of ROS-induced suppression of T lymphocyte migration.
1) Several pathologies result in accumulation of high levels of ROS including wounds, chronic infection and cancer. 2) Chemokine stimulation also produces exogenous H2O2 through NOX2/DUOX enzymes, which are known to be expressed on T lymphocytes. 3) Signalling concentrations of exogenous H2O2 enters the cell through aquaporin channels and can manipulate proteins in the cytosol. 4) H2O2 signals through SFKs to internalise chemokine receptor CXCR3, internalisation could occur through arrestin recruitment/ clathrin coated pits, caveolae or an independent mechanism. Once internalised, CXCR3 is degraded in the endosome. 5) H2O2 also signals through SFKs to phosphorylate and activate SHIP-1. SHIP-1 activation inhibits the ability of CXCL11 to de-phosphorylate cytoskeletal proteins ezrin, radixin and ERM and 6) inhibits actin polarisation. H2O2 also increases total F-actin. 7) Collectively, chemokine internalisation, SHIP-1 activation and actin regulation reduces cytoskeletal re-organisation and cell chemotaxis. 8) Proposed outcomes of migration deficiency in T lymphocytes.
Importantly, the timing and subcellular localization of ROS generation are likely of greater influence in T cell responses than overall redox balance. Interestingly, controlled clinical trials have failed to show a consistent benefit of antioxidants in disease settings (47–49)). This supports our observation that oxidants are not solely toxic to the human body and that ROS can be both protective and deleterious depending on concentration and physiological setting.
Supplementary Material
Acknowledgements
We would like to thank the University of Bath Bioimaging Facility.
This work was supported by Wellcome Trust Grant 099154/Z/12/Z (to WW and SGW) and 107940/Z/15/Z (to WW).
References
- 1.Hara-Chikuma M, Chikuma S, Sugiyama Y, Kabashima K, Verkman AS, Inoue S, Miyachi Y. Chemokine-dependent T cell migration requires aquaporin-3-mediated hydrogen peroxide uptake. J Exp Med. 2012;209:1743–1752. doi: 10.1084/jem.20112398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jackson SH, Devadas S, Kwon J, Pinto LA, Williams MS. T cells express a phagocyte-type NADPH oxidase that is activated after T cell receptor stimulation. Nat Immunol. 2004;5:818–827. doi: 10.1038/ni1096. [DOI] [PubMed] [Google Scholar]
- 3.Kwon J, Shatynski KE, Chen H, Morand S, de Deken X, Miot F, Leto TL, Williams MS. The nonphagocytic NADPH oxidase Duox1 mediates a positive feedback loop during T cell receptor signaling. Sci Signal. 2010;3:ra59. doi: 10.1126/scisignal.2000976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schmielau J, Finn OJ. Activated granulocytes and granulocyte-derived hydrogen peroxide are the underlying mechanism of suppression of t-cell function in advanced cancer patients. Cancer Res. 2001;61:4756–4760. [PubMed] [Google Scholar]
- 5.Otsuji M, Kimura Y, Aoe T, Okamoto Y, Saito T. Oxidative stress by tumor-derived macrophages suppresses the expression of CD3 zeta chain of T-cell receptor complex and antigen-specific T-cell responses. Proc Natl Acad Sci U S A. 1996;93:13119–13124. doi: 10.1073/pnas.93.23.13119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moreira S, Stramer B, Evans I, Wood W, Martin P. Prioritization of competing damage and developmental signals by migrating macrophages in the Drosophila embryo. Curr Biol. 2010;20:464–470. doi: 10.1016/j.cub.2010.01.047. [DOI] [PubMed] [Google Scholar]
- 7.Niethammer P, Grabher C, Look AT, Mitchison TJ. A tissue-scale gradient of hydrogen peroxide mediates rapid wound detection in zebrafish. Nature. 2009;459:996–999. doi: 10.1038/nature08119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoo SK, Starnes TW, Deng Q, Huttenlocher A. Lyn is a redox sensor that mediates leukocyte wound attraction in vivo. Nature. 2011;480:109–112. doi: 10.1038/nature10632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klyubin IV, Kirpichnikova KM, Gamaley IA. Hydrogen peroxide-induced chemotaxis of mouse peritoneal neutrophils. Eur J Cell Biol. 1996;70:347–351. [PubMed] [Google Scholar]
- 10.D'Autreaux B, Toledano MB. Nat Rev Mol Cell Biol. England: 2007. ROS as signalling molecules: mechanisms that generate specificity in ROS homeostasis; pp. 813–824. [DOI] [PubMed] [Google Scholar]
- 11.Denu JM, Tanner KG. Biochemistry. United States: 1998. Specific and reversible inactivation of protein tyrosine phosphatases by hydrogen peroxide: evidence for a sulfenic acid intermediate and implications for redox regulation; pp. 5633–5642. [DOI] [PubMed] [Google Scholar]
- 12.Haddad JJ. Science review: Redox and oxygen-sensitive transcription factors in the regulation of oxidant-mediated lung injury: role for nuclear factor-kappaB. Crit Care. 2002;6:481–490. doi: 10.1186/cc1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bogeski I, Kummerow C, Al-Ansary D, Schwarz EC, Koehler R, Kozai D, Takahashi N, Peinelt C, Griesemer D, Bozem M, Mori Y, et al. Sci Signal. United States: 2010. Differential redox regulation of ORAI ion channels: a mechanism to tune cellular calcium signaling; p. ra24. [DOI] [PubMed] [Google Scholar]
- 14.Lee SR, Yang KS, Kwon J, Lee C, Jeong W, Rhee SG. The Journal of biological chemistry. United States: 2002. Reversible inactivation of the tumor suppressor PTEN by H2O2; pp. 20336–20342. [DOI] [PubMed] [Google Scholar]
- 15.Kwon J, Lee SR, Yang KS, Ahn Y, Kim YJ, Stadtman ER, Rhee SG. Proc Natl Acad Sci U S A. United States: 2004. Reversible oxidation and inactivation of the tumor suppressor PTEN in cells stimulated with peptide growth factors; pp. 16419–16424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Farber JM. A macrophage mRNA selectively induced by gamma-interferon encodes a member of the platelet factor 4 family of cytokines. Proc Natl Acad Sci U S A. 1990;87:5238–5242. doi: 10.1073/pnas.87.14.5238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cole KE, Strick CA, Paradis TJ, Ogborne KT, Loetscher M, Gladue RP, Lin W, Boyd JG, Moser B, Wood DE, Sahagan BG, et al. Interferon-inducible T cell alpha chemoattractant (I-TAC): a novel non-ELR CXC chemokine with potent activity on activated T cells through selective high affinity binding to CXCR3. J Exp Med. 1998;187:2009–2021. doi: 10.1084/jem.187.12.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luster AD, Unkeless JC, Ravetch JV. Gamma-interferon transcriptionally regulates an early-response gene containing homology to platelet proteins. Nature. 1985;315:672–676. doi: 10.1038/315672a0. [DOI] [PubMed] [Google Scholar]
- 19.Xanthou G, Williams TJ, Pease JE. Molecular characterization of the chemokine receptor CXCR3: evidence for the involvement of distinct extracellular domains in a multi-step model of ligand binding and receptor activation. Eur J Immunol. 2003;33:2927–2936. doi: 10.1002/eji.200324235. [DOI] [PubMed] [Google Scholar]
- 20.Colvin RA, Campanella GS, Manice LA, Luster AD. Mol Cell Biol. United States: 2006. CXCR3 requires tyrosine sulfation for ligand binding and a second extracellular loop arginine residue for ligand-induced chemotaxis; pp. 5838–5849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dagan-Berger M, Feniger-Barish R, Avniel S, Wald H, Galun E, Grabovsky V, Alon R, Nagler A, Ben-Baruch A, Peled A. Blood. United States: 2006. Role of CXCR3 carboxyl terminus and third intracellular loop in receptor-mediated migration, adhesion and internalization in response to CXCL11; pp. 3821–3831. [DOI] [PubMed] [Google Scholar]
- 22.Nedjai B, Li H, Stroke IL, Wise EL, Webb ML, Merritt JR, Henderson I, Klon AE, Cole AG, Horuk R, Vaidehi N, et al. Small molecule chemokine mimetics suggest a molecular basis for the observation that CXCL10 and CXCL11 are allosteric ligands of CXCR3. Br J Pharmacol. 2012;166:912–923. doi: 10.1111/j.1476-5381.2011.01660.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simonson WT, Franco SJ, Huttenlocher A. Talin1 regulates TCR-mediated LFA-1 function. Journal of immunology (Baltimore, Md. : 1950) 2006;177:7707–7714. doi: 10.4049/jimmunol.177.11.7707. [DOI] [PubMed] [Google Scholar]
- 24.Burkhardt JK, Carrizosa E, Shaffer MH. The actin cytoskeleton in T cell activation. Annu Rev Immunol. 2008;26:233–259. doi: 10.1146/annurev.immunol.26.021607.090347. [DOI] [PubMed] [Google Scholar]
- 25.Tybulewicz VL, Henderson RB. Rho family GTPases and their regulators in lymphocytes. Nat Rev Immunol. 2009;9:630–644. doi: 10.1038/nri2606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fais S, Malorni W. Leukocyte uropod formation and membrane/cytoskeleton linkage in immune interactions. J Leukoc Biol. 2003;73:556–563. doi: 10.1189/jlb.1102568. [DOI] [PubMed] [Google Scholar]
- 27.Evans IR, Rodrigues FS, Armitage EL, Wood W. Draper/CED-1 mediates an ancient damage response to control inflammatory blood cell migration in vivo. Curr Biol. 2015;25:1606–1612. doi: 10.1016/j.cub.2015.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Korniejewska A, McKnight A, Johnson Z, Watson ML, Ward SG. Expression and agonist responsiveness of CXCR3 variants in human T lymphocytes. Immunology. 2011;132(4):503–515. doi: 10.1111/j.1365-2567.2010.03384.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sauty A, Colvin RA, Wagner L, Rochat S, Spertini F, Luster AD. CXCR3 Internalization Following T Cell-Endothelial Cell Contact: Preferential Role of IFN-Inducible T Cell α Chemoattractant (CXCL11) J Immunol. 2001;167:7084–7093. doi: 10.4049/jimmunol.167.12.7084. [DOI] [PubMed] [Google Scholar]
- 30.Gloire G, Charlier E, Rahmouni S, Volanti C, Chariot A, Erneux C, Piette J. Oncogene. England: 2006. Restoration of SHIP-1 activity in human leukemic cells modifies NF-kappaB activation pathway and cellular survival upon oxidative stress; pp. 5485–5494. [DOI] [PubMed] [Google Scholar]
- 31.Harris SJ, P RV, Foster JG, Blunt MD, Wang A, Marelli-Berg F, Westwick J, Ward SG. Evidence that the lipid phosphatase SHIP-1 regulates T lymphocyte morphology and motility. Journal of immunology. 2011;186:4936–4945. doi: 10.4049/jimmunol.1002350. [DOI] [PubMed] [Google Scholar]
- 32.Phee H, Jacob A, Coggeshall KM. Enzymatic activity of the Src homology 2 domain-containing inositol phosphatase is regulated by a plasma membrane location. The Journal of biological chemistry. 2000;275:19090–19097. doi: 10.1074/jbc.M001093200. [DOI] [PubMed] [Google Scholar]
- 33.Lioubin MN, Algate PA, Tsai S, Carlberg K, Aebersold A, Rohrschneider LR. p150Ship, a signal transduction molecule with inositol polyphosphate-5-phosphatase activity. Genes & development. 1996;10:1084–1095. doi: 10.1101/gad.10.9.1084. [DOI] [PubMed] [Google Scholar]
- 34.Dong S, Corre B, Foulon E, Dufour E, Veillette A, Acuto O, Michel F. J Exp Med. United States: 2006. T cell receptor for antigen induces linker for activation of T cell-dependent activation of a negative signaling complex involving Dok-2, SHIP-1, and Grb-2; pp. 2509–2518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O'Neill SK, Getahun A, Gauld SB, Merrell KT, Tamir I, Smith MJ, Dal Porto JM, Li QZ, Cambier JC. Monophosphorylation of CD79a and CD79b ITAM motifs initiates a SHIP-1 phosphatase-mediated inhibitory signaling cascade required for B cell anergy. Immunity. 2011;35:746–756. doi: 10.1016/j.immuni.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arpin M, Chirivino D, Naba A, Zwaenepoel I. Emerging role for ERM proteins in cell adhesion and migration. Cell Adh Migr. 2011;5:199–206. doi: 10.4161/cam.5.2.15081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brown MJ, Nijhara R, Hallam JA, Gignac M, Yamada KM, Erlandsen SL, Delon J, Kruhlak M, Shaw S. Chemokine stimulation of human peripheral blood T lymphocytes induces rapid dephosphorylation of ERM proteins, which facilitates loss of microvilli and polarization. Blood. 2003;102:3890–3899. doi: 10.1182/blood-2002-12-3807. [DOI] [PubMed] [Google Scholar]
- 38.Hogg N, Patzak I, Willenbrock F. The insider's guide to leukocyte integrin signalling and function. Nat Rev Immunol. 2011;11:416–426. doi: 10.1038/nri2986. [DOI] [PubMed] [Google Scholar]
- 39.Blouin E, Halbwachs-Mecarelli L, Rieu P. Redox regulation of β2-integrin CD11b/CD18 activation. European Journal of Immunology. 1999;29:3419–3431. doi: 10.1002/(SICI)1521-4141(199911)29:11<3419::AID-IMMU3419>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 40.Lee S, Ha IS, Kim JH, Park KS, Han KH, Kim SH, Chae YC, Kim YH, Suh PG, Ryu SH, Kim JE, et al. Hydrogen peroxide-induced VCAM-1 expression in pancreatic islets and β-Cells through extracellular Ca2+ influx. Transplantation. 2008;86:1257–1266. doi: 10.1097/TP.0b013e318188ab04. [DOI] [PubMed] [Google Scholar]
- 41.Lee S, Chung J, Ha IS, Yi K, Lee JE, Kang HG, Choi I, Oh KH, Kim JY, Surh CD, Ahn C. Hydrogen peroxide increases human leukocyte adhesion to porcine aortic endothelial cells via NFκB-dependent up-regulation of VCAM-1. International Immunology. 2007;19:1349–1359. doi: 10.1093/intimm/dxm104. [DOI] [PubMed] [Google Scholar]
- 42.Klemke M, Wabnitz GH, Funke F, Funk B, Kirchgessner H, Samstag Y. Oxidation of cofilin mediates T cell hyporesponsiveness under oxidative stress conditions. Immunity. 2008;29:404–413. doi: 10.1016/j.immuni.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 43.Morris AJ, Malbon CC. Physiological regulation of G protein-linked signaling. Physiol Rev. 1999;79:1373–1430. doi: 10.1152/physrev.1999.79.4.1373. [DOI] [PubMed] [Google Scholar]
- 44.Lefkowitz RJ. G protein-coupled receptors. III. New roles for receptor kinases and beta-arrestins in receptor signaling and desensitization. The Journal of biological chemistry. 1998;273:18677–18680. doi: 10.1074/jbc.273.30.18677. [DOI] [PubMed] [Google Scholar]
- 45.Fidalgo M1, Guerrero A, Fraile M, Iglesias C, Pombo CM, Zalvide J. Adaptor protein cerebral cavernous malformation 3 (CCM3) mediates phosphorylation of the cytoskeletal proteins ezrin/radixin/moesin by mammalian Ste20-4 to protect cells from oxidative stress. J Biol Chem. 2012;287(14):11556–65. doi: 10.1074/jbc.M111.320259. 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nakamura K, Hori T, Sato N, Sugie K, Kawakami T, Yodoi J. Redox regulation of a src family protein tyrosine kinase p56lck in T cells. Oncogene. 1993;8:3133–3139. [PubMed] [Google Scholar]
- 47.Rapola JM, Virtamo J, Ripatti S, Huttunen JK, Albanes D, Taylor PR, Heinonen OP. Randomised trial of alpha-tocopherol and beta-carotene supplements on incidence of major coronary events in men with previous myocardial infarction. Lancet. 1997;349:1715–1720. doi: 10.1016/S0140-6736(97)01234-8. [DOI] [PubMed] [Google Scholar]
- 48.Yusuf S, Dagenais G, Pogue J, Bosch J, Sleight P. Vitamin E supplementation and cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. The New England journal of medicine. 2000;342:154–160. doi: 10.1056/NEJM200001203420302. [DOI] [PubMed] [Google Scholar]
- 49.Tang H, Hao Q, Rutherford SA, Low B, Zhao ZJ. Inactivation of SRC family tyrosine kinases by reactive oxygen species in vivo. The Journal of biological chemistry. 2005;280:23918–23925. doi: 10.1074/jbc.M503498200. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.