Abstract
The Internet is now all-pervasive across much of the globe. While it has positive uses (e.g. prompt access to information, rapid news dissemination), many individuals develop Problematic Use of the Internet (PUI), an umbrella term incorporating a range of repetitive impairing behaviours. The Internet can act as a conduit for, and may contribute to, functionally impairing behaviours including excessive and compulsive video gaming, compulsive sexual behaviour, buying, gambling, streaming or social networks use. There is growing public and National health authority concern about the health and societal costs of PUI across the lifespan. Gaming Disorder is being considered for inclusion as a mental disorder in diagnostic classification systems, and was listed in the ICD-11 version released for consideration by Member States (http://www.who.int/classifications/icd/revision/timeline/en/). More research is needed into disorder definitions, validation of clinical tools, prevalence, clinical parameters, brain-based biology, socio-health-economic impact, and empirically validated intervention and policy approaches. Potential cultural differences in the magnitudes and natures of types and patterns of PUI need to be better understood, to inform optimal health policy and service development. To this end, the EU under Horizon 2020 has launched a new four-year European Cooperation in Science and Technology (COST) Action Programme (CA 16207), bringing together scientists and clinicians from across the fields of impulsive, compulsive, and addictive disorders, to advance networked interdisciplinary research into PUI across Europe and beyond, ultimately seeking to inform regulatory policies and clinical practice. This paper describes nine critical and achievable research priorities identified by the Network, needed in order to advance understanding of PUI, with a view towards identifying vulnerable individuals for early intervention. The network shall enable collaborative research networks, shared multinational databases, multicentre studies and joint publications.
Keywords: problematic Internet use, compulsive, behavioural addiction, video gaming, pornography
Introduction
The public health and societal costs of Problematic use of the Internet (PUI) (World Health Organization, 2014) are increasingly recognised, constituting a growing concern across all age groups, and an emerging challenge for mental health research (Ioannidis et al., 2018). We use the umbrella term PUI to encompass all potentially problematic Internet related behaviours, including those relating to gaming, gambling, buying, pornography viewing, social networking, ‘cyber-bullying,’ ‘cyberchondria’, among others. PUI may have mental and physical health consequences. The Internet is now an integral part of modern life (Anderson et al., 2017), but as its use has grown, it has provided a new environment in which a wide range of problematic behaviours may emerge.
A spectrum of Internet usage, from controlled and “adaptive” to uncontrolled and “maladaptive”, is recognised (Billieux et al., 2017). Disordered online behaviours, such as excessive video gaming, pornography viewing, buying, gambling, or streaming and social networks use (Ioannidis et al., 2018) have been associated with marked functional impairment including loss of productivity (or reduced scholastic achievement), and mental health sequelae including mood and anxiety disorders (Derbyshire et al., 2013; Ho et al., 2014). Clinical services for PUI are available only in some geographical jurisdictions, and therefore many affected individuals do not have access to support and treatment (Lam and Lam, 2016; Winkler et al., 2013). National health authorities are expressing concern (Byrne et al., 2016; Parliament (UK), 2017) and there is a growing interest by some governments in implementing policies aimed at curbing PUI (Kiraly et al., 2017a). Psychiatry is beginning to acknowledge PUI and Internet Gaming Disorder is listed as a candidate mental disorder in need of further study in the Diagnostic and Statistical Manual (DSM-5) (2012), and Gaming Disorder is being actively considered (King et al., 2018) by the International Classification of Diseases (ICD) for inclusion in the section of disorders due to addictive behaviours in the upcoming 11th Edition. Indeed Gaming Disorder has recently been included in the ICD-11 version released to Member States (https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/1448597234).
As noted, PUI envelops a wide range of activities including video gaming, pornography viewing (and other compulsive sexual behaviours), buying, gambling, web-streaming, social media use and other behaviours. Some of these behaviours may fall into an existing mental disorder in psychiatric nomenclature (e.g. gambling disorder), whereas others are likely to be formally recognized in future DSM/ICD revisions, notably Internet Gaming Disorder (Kim et al., 2016b). Different types of PUI often start in childhood or adolescence (Volpe et al., 2015), but broad age ranges can be affected (Ioannidis et al., 2018). Age and gender relate importantly to PUI behaviours, with younger people typically having problems with gaming and media streaming, males with gaming, gambling and pornography viewing and females with social media and buying (Andreassen et al., 2016). The Internet provides ready, immediate, and seemingly limitless pseudo-anonymous (meaning perceived as anonymous, but in reality not necessarily) access to these activities. Furthermore, Internet sites, by collecting user data (‘big data’), are potentially capable of building artificial intelligence (machine learning) models with the aim of reinforcing behaviour, by generating algorithm-based personalized content and site architecture. Whereas these interactive qualities are viewed on the one hand as having value for the user, they suggest that the Internet may not simply act as a passive conduit, but its composite behaviours may amplify a sense or reward and relief of tension, thereby providing increased reinforcement (Grant and Chamberlain, 2014). Being ‘cut off’ from the Internet in some individuals may generate a sense of dysphoria akin to withdrawal.
Important inroads have been made into defining diagnostic criteria and developing rating scales for some forms of PUI (i.e. Internet Gaming Disorder) (Kiraly et al., 2015), but networked research is needed to understand better the nature and extent of the broader range of PUI phenomena across jurisdictions and cultures. The behavioural phenotypes of different types of PUI need to be translated into valid and reliable diagnostic criteria and assessment tools devised and developed to sensitively and specifically quantify the magnitude of the problem. In turn, this would permit the systematic investigation of aetiological factors (genetic, developmental, psychosocial, cultural) and brain-based (biological and neuropsychological) mechanisms, as a platform for the development of preventative and therapeutic interventions. A coordinated multi-national research approach would thus be invaluable to allow the results to be tested across countries and cultures, to produce richer datasets with a view to ensuring findings can be generalized; and also in order to study local culture-specific issues of relevance to understanding PUI.
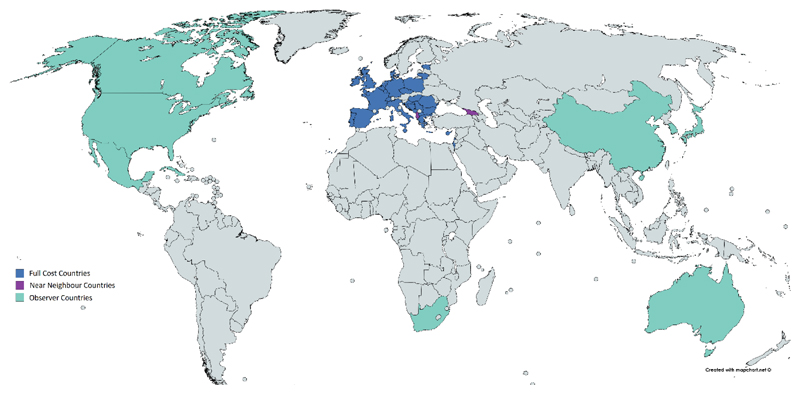
In response to the emerging public health importance of PUI, the newly created European Problematic Use of the Internet (EU-PUI) Research Network was formed, to bring together expert researchers and national and international scientific initiatives under one Europeanled Network (Cost Action; www.cost.eu/COST_Actions/ca/CA16207) to leverage existing funded research into a more coherent programme (Figure 1). The Network (currently 109 participants from 37 countries) connects a multidisciplinary group of geographically diverse expert researchers in neurosciences, genetics, and epidemiology, clinicians including child psychiatrists and psychologists, experts in bio-technology and information-technology industry, health economists, policy makers, and service planners, to develop fruitful collaborations to advance the understanding and treatment of PUI. Additionally, through an interactive Dissemination Plan (including website, social media, blogs) we are reaching out to relevant stakeholders at international and national levels with an emphasis on encouraging people with the lived experience of PUI to become involved in the Action. To this end, our first International Congress (Barcelona, October 10th 2018) includes a large public-facing meeting devoted to the lived experience of PUI, with people with the disorders and their families speaking about their experience of PUI as an integral part of the symposium. . Raising awareness of the lived experience of people with PUI and harnessing their energy via the network is likely to be of particular value for directing science and health policy and practice. A better understanding of the nature of different forms of PUI and their societal cost and burden would be expected to spearhead the development of systematic and adaptive treatment and prevention programmes. Table 1 summarises the eight nine achievable research priorities that we believe will drive the field forward over the next ten years.
Figure 1. Map of the 27 COST Member countries and 10 International Observer countries, with 1 or more members participating in the COST Action EU-PUI Network.
Table 1. Summary of key research priorities to advance the understanding of PUI.
|
1.1. Reliable consensus-driven conceptualisations of different forms of PUI (phenomenologies, comorbidities, and brain-based mechanisms)
The term ‘addiction’ is derived from the antiquated legal Latin term addicere which roughly means “enslaved by”, indicating a person who, having difficulties in paying debts, was assigned to a creditor. Over the past 100 years or so, this term has been mainly used in relation to the poorly controlled use of psychoactive substances, although recently behavioural addictions have been receiving more attention. Addiction is not a unitary construct. Core aspects of addiction, according to the DSM-5, include impaired control (e.g. unsuccessful attempts to reduce intake), craving (e.g., strong preoccupations or motivational drives that lead to behavioural engagement), impairment (e.g. neglect of other areas of life that may lead to occupational, relational and other problems), risky/harmful use (persisting intake despite awareness of damaging psychological or physiological effects or other negative consequences), and physiological features (e.g., tolerance, withdrawal). Certain psychiatric syndromes characterised by harmful repetitive behaviours share significant phenomenological, biological, clinical, comorbidity, genetic, prevention, treatment and other parallels with substance addictions (Petry, 2006; Potenza, 2006), and have thus been argued to represent candidate ‘behavioural addictions’. Accordingly, the DSM-5 introduced the category ‘Substance Related and Addictive Disorders’, and included gambling disorder as a behavioural addiction (Chamberlain et al., 2016; Potenza et al., 2009; Wareham and Potenza, 2010). Additionally, gambling disorder shows differences from obsessive compulsive disorder (OCD) in some of these multiple domains, informing the nosologic decision to classify it as a Substance Related and Addictive Disorder rather than an Obsessive Compulsive Related Disorder (Potenza et al., 2009).
‘Internet addiction’ was considered by the DSM-5 Substance Use Disorder workgroup and Internet Gaming Disorder was included in Section III of DSM-5 as a potential disorder worthy of further study (2012). More recently, the preliminary beta-draft of the 11th revision of the International Classification of Diseases (ICD-11) included ‘Gaming Disorder’ in its section on “Disorders Due to Substance Use or Addictive Behaviours” and characterised it by 1) impaired control, 2) increasing priority given to gaming resulting in precedence over other life interests and daily activities, and 3) continued use despite the occurrence of negative consequences. The evidence for this decision of the expert group of the WHO can be found in Saunders et al., 2017. Not all forms of PUI may meet the threshold for a diagnosable condition; for example, if there were no obvious functional impairment attributable to the Internet usage, the diagnostic threshold for a disorder would not be met, though such behaviours may presage the development of subsequent pathology (Billieux et al., 2017). Therefore, alternatives to diagnostic entities also warrant consideration so that public health may be promoted. Consistent with this notion, definitions for ‘hazardous gaming’ and ‘hazardous gambling’ are currently proposed for ICD-11, similar to what currently exists for some addictive behaviours in ICD-10 (e.g., hazardous drinking of alcohol) (Reid et al., 1999). Although – on the basis of the current evidence – DSM-5 and ICD-11 come to the conclusion that PUI (in the guise of Gaming Disorder) should be considered as an addictive behaviour, alternative frameworks merit scrutiny in future studies.
The clinical aspects of some Internet-related behaviours appear phenomenologically much like addiction (e.g. gambling or viewing pornography), and demonstrate impaired control (unsuccessful attempts to reduce or cease the behaviour), preoccupation (craving) associated functional impairment (neglect of other areas of life) and persistence despite damaging effects (Billieux et al., 2015; Ioannidis et al., 2016; Kardefelt-Winther, 2017). However, it remains less clear whether, apart from gambling disorder, these other forms of PUI meet the physiological criteria relating to addiction (tolerance, withdrawal). Other PUI behaviours may share more similarities with OCD and other obsessive-compulsive related disorders (e.g., repeatedly checking e-mails or social media, digital hoarding) or social anxiety disorder (e.g., excessive use of social media as an avoidance of face-to-face social contact) (Ioannidis et al., 2016). Interestingly, obsessive-compulsive personality traits are common in excessive Internet users and are associated with problematic Internet use (Chamberlain et al., 2017b), hinting that compulsive behaviours contribute to some forms of PUI. Some forms of online shopping or cybersex, on the other hand, may closely resemble ICD-10 or DSM-IV impulse control or sexual disorders (Volpe et al., 2015). ‘Cyberchondria’ is defined as excessive or repeated online searching for health-related information and, viewed through the prism of hypochondriasis, may represent a multidimensional Internet-related psychopathology associated with intolerance of uncertainty driving compulsive reassurance seeking (Volpe et al., 2015). Paradoxically, cyberchondria may increase rather than resolve anxiety, perhaps due to the discovery of new triggers for health-related worries, and may reinforce further compulsive checking. Such an “amplification mechanism” may relate to the characteristic of the Internet of not having been designed to provide unambiguous reliable health information, thereby increasing uncertainty and worrying (Fergus, 2013; Fergus and Spada, 2017). Thus, while phenotypic similarities to behavioural addictions may pertain to some forms of PUI, for others, similarities with social anxiety, impulse-control disorders and OCD may be more prominent. To address this issue further, it may be helpful to study intermediate phenotypes, as discussed later.
Data suggest that different forms of PUI are associated with psychiatric comorbidities including affective disorders (including bipolar), anxiety disorders, substance-use disorders (SUDs), sleep disorders, attention-deficit/hyperactivity disorder (ADHD) and impulse-control disorders (Carter et al., 2016; Chamberlain et al., 2017a; Ho et al., 2014; Liu et al., 2011). However, comorbidities are also seen with OCD, obsessive-compulsive personality traits (e.g. rigidity, perfectionism, reluctance to delegate), and autism-spectrum disorder (ASD), implying the existence of relationships between PUI and disorders of compulsivity (Chamberlain et al., 2017a; Finkenauer et al., 2012; Ioannidis et al., 2016). Initial data also suggest that PUI may be associated with increased rates of suicidality and/or self-harm (Cheng et al., 2018; Durkee et al., 2016; Fischer et al., 2012; Liu et al., 2017; Marchant et al., 2017).
Neuroscience research of other disorders of repetitive urge-driven behaviours, such as obsessive-compulsive and related disorders and SUDs, supports a complex neuro-psychological model indicating impaired ‘top-down’ cortical behavioural control underpinned by abnormal activation in specific components of brain circuitry encoding affective, cognitive and motor control of instrumental behaviour (Fineberg et al., 2018). Implicated neural regions include cortical regions (such as orbitofrontal, inferior-frontal and anterior cingulate regions), and the striatal ventral regions (involved in reward-driven behaviours) and dorsal regions (proposed to be more involved in ingrained habits but also relevant to craving in addictions) (Chamberlain and Menzies, 2009; Clark and Limbrick-Oldfield, 2013). Recent models explaining the development and maintenance of diverse types of PUI reflect the aforementioned main mechanisms (e.g. impaired cortical top-down control and increased affective reactions linked to ventral striatum activity) (Brand et al., 2016b; Dong and Potenza, 2014). Although few neuroimaging investigations have been conducted to examine different types of PUI, the proposed diagnostic criteria for Internet Gaming Disorder have facilitated research into this population. In a systematic review of the neuroimaging literature, at least two studies found reduced grey matter in the anterior cingulate, insula, supplementary motor area, and inferior temporal gyrus, in individuals with Internet Gaming Disorder compared to non-affected control individuals (Weinstein et al., 2017). These structural findings were confirmed in a subsequent meta-analysis, which also identified abnormal activation patterns (fMRI) in these and other regions (including in the caudate) (Yao et al., 2017). In a recent meta-analysis of cognitive findings in PUI, significant deficits were identified in case versus control participants in inhibitory control, decision-making, and working memory (preprint: https://osf.io/5kb7h), thereby suggesting the likely involvement of neural regions involved in top-down control. An initial case-control study reported that PUI without comorbidities was associated with impaired quality of life, but that significant cognitive deficits were not apparent on the domains examined; whereas impaired cognition was found in comorbid cases for inhibitory control and decision-making (Chamberlain et al., 2018). Thus, the cognitive profile of PUI is influenced by comorbidities.
Better understanding the similarities and differences among the genetic, neurobiological and socio-demographic determinants of the different forms of PUI and the characteristics of their treatment-responses would help clarify the nosological relationships between a range of mental disorders characterised primarily by impulsive, compulsive, habitual and addictive behaviours. As a vital first step, studies are needed to fully describe the range of behaviours and disorders that comprise PUI, across genders, age groups and cultures, from the perspective of the content of the repetitive behaviours, maladaptive consequences and other features, so as to reach consensus on the diagnostic thresholds and criteria that may be used to define the disorders and other levels of behaviours warranting consideration from personal and public health perspectives. Once operational diagnostic criteria are established, standardised databases could be built to facilitate reliable research. However, understanding the determinants of disease and basing a new classification on these disorders may not necessarily improve clinical outcomes for affected individuals; field-testing of the proposed diagnostic criteria across an integrated network of research centres is also required, as is currently being conducted for Gaming Disorder in some jurisdictions, to facilitate subsequent rigorous intervention trials, including early intervention in vulnerable individuals who have yet to develop full pathology. Taken together, such improvements would be expected to have a positive impact upon the accuracy of prognostication and lead to better health services informatics, planning and delivery.
2.2. Age- and culture-appropriate assessment instruments to screen, diagnose and measure the severity of the different forms of PUI
Validated instruments are needed in order to identify mental disorders germane to PUI (screening and diagnosis), and to quantify their severity. Several such instruments have been developed in this field, as reviewed in detail elsewhere (Kiraly et al., 2015). Some have argued that a single instrument capturing all the current forms of PUI would be too bulky and impracticable be used clinically. However, the converse may also be true, i.e. a series of separate instruments for each form of PUI may not gain traction outside the research setting, except for conditions that soon may be included in nosologic systems (e.g. Gaming Disorder). Several scales have been developed to measure broad types of PUI (Kiraly et al., 2015). For example, Young’s Internet Addiction Diagnostic Questionnaire (IADQ) and Internet Addiction Test (IAT) were derived in part from original diagnostic criteria for gambling disorder (Young, 2009; Young, 1998). More recent developments, examining a broader range of features (not focusing only on ‘addiction’) include the Problematic Internet Use Questionnaire (PIUQ) (Demetrovics et al., 2016; Kiraly et al., 2015) which has a replicable factor structure and good test-retest properties, also being available in short form. The PIUQ has a factor structure relating to obsession, neglect, and loss of control. Instruments have also been developed to assess specific types of problem behaviour (Kiraly et al., 2015), such as the Problematic Online Gaming Questionnaire (POGQ), including a short form, which again has a replicable factor structure and sound psychometric properties (Demetrovics et al., 2012). There is also the Internet Gaming Disorder 20 (IGD-20), which has good psychometric properties and a six-factor structure (Pontes et al., 2014). Another short instrument, the Ten-Item Internet Gaming Disorder Test (IGDT-10), assessing IGD as proposed in the DSM-5 showed good psychometric properties and measurement invariance across seven languages (Kiraly et al., 2017b).
There nevertheless remains room for the development of a standardised contemporary measure focussing on PUI severity that is sensitive to change (e.g. treatment effects) and that could be broadly applied across all – or almost all clinically relevant forms of PUI. Examples from different fields include the different versions of the Yale Brown Obsessive Compulsive Scale that was successfully adapted for a broad range of disorders (Pallanti et al., 2005). Consideration of PUI from different but non-mutually exclusive and complementary perspectives including those related to addiction, impulsivity, and compulsivity, may in the future mean that more of its features can be captured, understood and addressed. Other key objectives for research in this area include the need to more rigorously assess the impact of comorbidities (e.g. OCD, ADHD, impulse-control disorders) on functional impairment and treatment outcomes, further work on the longitudinal profiles of different types of PUI, and the extent to which instruments can be shown to be sensitive to the effects of treatment. In particular, there is a need for the validation of instruments besides factorial validity using external measures confirming concurrent and predictive validity. Such external measures need to be based on gold standard assessments such as standardized clinical interviews and measures of functional impairment. To date, only few clinical instruments exist and validation needs to be confirmed. In general, there is an urgent need to harmonize assessment tools in order to assure comparability of findings. Considering the digital form of the disorder, digital tools may be used as objective and continuous monitor of the pathological behaviour. Once developed and validated in clinical trials, these Internet-based tools may serve both as monitoring and as interventional utensils.
3. Characterise the impacts of different forms of PUI on health and quality of life
Increasing exposure to the Internet, coupled with poor personal control over its use, suggests that the societal risk of PUI may be growing. PUI is presently attracting considerable media attention. Parental concern is understandable, since PUI may start in childhood or adolescence and potentially alter developmental trajectories or increase in severity over time. For example, in a nationally representative sample of students, adolescents who spent more time on screen and engaged in electronic communication (including Internet use) had lower psychological well-being and the converse also appeared to be the case (greater happiness with lower use) (Twenge et al., 2018). Thus, the economic burden of PUI may grow as direct health costs accumulate.
Several existing epidemiological studies of PUI have provided useful data on the prevalence and functional impact of PUI (Dell'Osso et al., 2006; Kuss et al., 2014). Differences in methodologies complicate comparisons across different studies, and have contributed to wide variation in estimates. For example, for Internet Addiction, prevalence rates of 0.8-26.7% were reported (Kuss et al., 2014). Similarly, for Internet gaming disorder, a systematic review reported prevalence estimates of 0.7-27.5% (Mihara and Higuchi, 2017). Such variability across studies may reflect differences in assessment instruments and thresholds applied across studies; discrepancies in Internet availability; social, cultural and demographic differences in Internet use behaviours and attitudes; as well as other factors. On the other hand, the public health burden of PUI may be greater than its prevalence may suggest if one also considers comorbidities.
At the individual level, PUI has been associated with relationship difficulties, academic and employment underperformance, financial problems and other concerns (Billieux et al., 2017). Among college students, PUI was associated with a poorer ‘grade point’ average, less frequent exercise, and higher distress (stress scores and low mood) (Derbyshire et al., 2013). Among high-school students, PUI occurred in ~4% of the sample and was significantly associated with substance-use disorders, depression, aggression and other concerns (Liu et al., 2011). There is thus a clear need for further large-scale community-based studies to robustly explore the direct and indirect costs of PUI across the lifespan. Specifically, we need to obtain reliable estimates of incidence, cumulative prevalence across the age-range and remission rates along with associated clinical and demographic determinants that may alter the trajectories of specific forms of PUI. Such primary data would also be required to calculate the relative cost and outcome of ‘evidence-based’ interventions, as they develop, for individuals with various levels of severity and comorbidities. With these data we could refine socio-health-economic models, develop meaningful public health policies, and direct resources towards the greatest need also taking into consideration the degree of suffering and life impairment associated with the different forms of PUI.
4. Defining the clinical courses of different forms of PUI using longitudinal studies
Remarkably little prospective research has been conducted on the courses of different forms of PUI and we remain relatively ignorant of key factors affecting long-term outcomes. Such data are of crucial importance in understanding aetiology, planning treatment and improving prognostication. For example, for some individuals PUI may represent a temporary phenomenon and spontaneously resolve (e.g., in some young people as brain systems mature), whereas for others PUI may become chronic. Consequently, there is a pressing need for prospective longitudinal community-based analysis of incidence, comorbidity and remission, using age-defined cohorts including young children, adolescents and the elderly. Studies such as these would provide fresh data on the critical trajectories that occur over the lifespan and may inform new aetiological theories linking these behaviours and disorders. In a two-year longitudinal study in school students, depression, anxiety, social phobia, and lower school performance, appeared to arise as a consequence of pathological gaming (Gentile et al., 2011). In a large cross-sectional two-site questionnaire study, PUI in older age was particularly strongly associated with OCD and generalized anxiety disorder; whereas in young individuals, the associations were strongest for ADHD and social anxiety disorder (Ioannidis et al., 2018). Thus, further longitudinal evaluation of different forms of PUI and their clinical associations would be valuable as such information may inform the need for different interventions and preventative measures. Furthermore, longitudinal studies are needed to examine protective factors and with a view to facilitating resilience.
5. Reduce obstacles to timely recognition and intervention
Lack of awareness, and the shame and secrecy that may surround different forms of PUI may constitute important obstacles to recognition, diagnosis and ultimately intervention. Consequently, although the increasing number of published reports of treatment seeking cases in 2016-2017 suggests the numbers are rising (Billieux et al., 2017), it is likely that only a minority of cases are detected and offered treatment. Comorbidity (e.g. depression) may increase the likelihood that the individual will present to a clinician, but may often fail to improve detection of PUI as PUI may commonly be overlooked by healthcare providers, due to a lack of established diagnostic criteria, training regarding recognition and treatment, awareness (education), reimbursement, or other factors.
The likely long-term, societal costs of early-onset PUI highlight the importance of delivering interventions at the earliest signs of illness and at the greatest level of efficacy and tolerability. Early intervention may be particularly relevant for disorders associated with considerable psychiatric comorbidity, since the early detection and treatment of the primary disorder could also prevent the onset of the secondary comorbidity. At the same time early intervention in PUI might prevent the development of secondary comorbid disorders. Data from compulsive disorders such as OCD indicate that longer duration of illness is associated with a poorer clinical outcome (Dell'Osso et al., 2013; Jakubovski et al., 2013). A potential for early detection lies in identifying early signs of PUI. Maladaptive use of the Internet in adolescence may predict the development of PUI and have severe consequences for the longer term. Educating parents around appropriate use of the Internet, through developing public education programs, to enable them to identify young people at increased risk of PUI is an approach that could be adopted without delay. Digital monitoring with appropriate consent could be another promising tool as it is inexpensive and could be used for screening and monitoring of PUI. Developing and validating an application (‘app’), which remotely, objectively monitors Internet use and sends an alert to the patient and ‘trust-buddy’ (i.e., family member or friend) might be an innovative approach to be included in future studies and surveys.
6. Clarify the possible role of genetics and personality features in different forms of PUI
PUI includes a complex spectrum of behaviours, and genetic and environmental factors are therefore likely to indicate multifactorial aetiologies, as with substance addictions (Kreek et al., 2005) or gambling (Gyollai et al., 2014). Indeed, there has been some initial research into the heritability of PUI, in which behavioural traits were also considered.
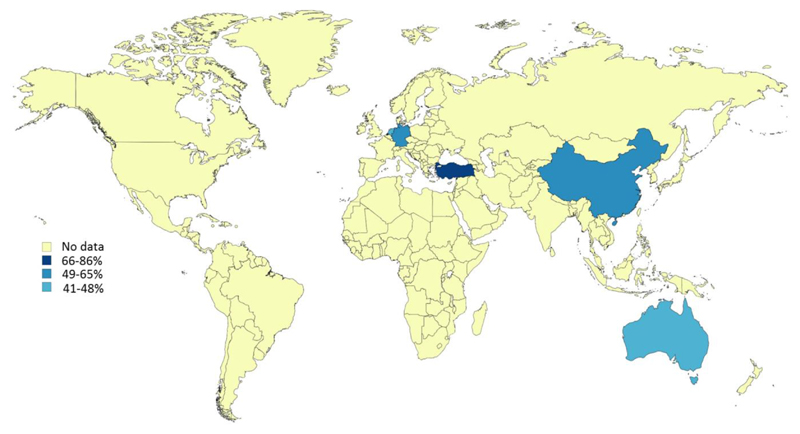
Heritability estimates of generalized Internet addiction in one study were 58% for females and 66% for males, while the remaining variance was explained by unique environmental influences (Li et al., 2014). In a Turkish study of young twin-pairs, genetic influences upon PUI were estimated at 19%-86% (Deryakulu and Ursavas, 2014). Elsewhere, in a study in the Netherlands, the heritability of PUI was estimated at 48% (Vink et al., 2016). Similarly, a study investigating the frequency of Internet use in young adult twins from Brisbane found that 41% of variance in the frequency of Internet use was attributable to genetic factors (Long et al., 2016). On the other hand, in 784 adult German twins, generalized PUI could be explained by shared and non-shared environmental factors while genetic influence did not play a significant role (Hahn et al., 2017). However, in one personality trait (‘self-directedness’), a high estimated heritability was found amounting to 59%, while the remaining 41% was accounted to non-shared environmental factors (Hahn et al., 2017). A summary of all current heritability studies is represented in Figure 2. Despite limited research, maladaptive Internet use has been shown to be moderately heritable in some studies, perhaps more strongly so in males. However, due to varied definitions, age at time of study and cultural differences, this issue needs to be further investigated in a more systematic manner.
Figure 2. PUI heritability estimates linked to populations studied.
Preliminary data exist from molecular genetic studies showing possible specific genetic associations with PUI. These studies have suggested that variants in the dopamine receptor gene (DRD2) (Han et al., 2007), catecholamine-O-methyltransferase gene (COMT) (Han et al., 2007), serotonin transporter gene (5HTTLPR/ SLC6A4) (Lee et al., 2008), nicotine acetylcholine receptor gene (CHRNA4) (Jeong et al., 2017; Montag et al., 2012) and neurotrophic tyrosine kinase type 3 receptor gene (NTRK3) (Ki et al., 2016a) are associated with PUI. Variants in these genes (DRD2, COMT, 5HTTLPR, CHRNA4) have also been associated with substance use and substance addiction (Breitling et al., 2009; Feng et al., 2004; Han et al., 2011; Le Foll et al., 2009; Su et al., 2015; Tammimaki and Mannisto, 2010; Yang et al., 2013b), possibly suggesting that PUI might be influenced by similar genes as in addiction. Similarly, several communalities exist between these candidate genes and OCD as well as ADHD (Brem et al., 2014; Grunblatt et al., 2018), perhaps pointing to some overlapping risk genes and traits for these disorders. However, in order to have reliable results, replications and well powered phenotyping study populations are required. Moreover, future studies should focus on finding relevant genes by conducting genome-wide association studies (GWAS) that enable hypothesis-free (data-driven) search of risk genes. Similarly, to more fully consider environmental influences on gene expression, epigenetic measurements would be necessary.
Personality traits (e.g., relating to impulsivity and rigidity) have been associated with PUI (Chamberlain et al., 2017b; Ioannidis et al., 2016). For example, low self-directedness exceeded high neuroticism in predicting high Internet addiction test scores (Montag et al., 2010). This trait was highly heritable in an adolescent twin study, though PUI was not (Hahn et al., 2017). Indeed, such personality factors (e.g. neuroticism, extraversion, conscientiousness, openness and impulsivity) were already suggested in GWAS studies to be highly heritable with overlapping genetic components influencing various brain disorders (Anttila et al., 2016; Gray et al., 2018; Lo et al., 2017). Moreover, personality features seem to influence diverse substance use disorders (Feng et al., 2004; Few et al., 2014; Kreek et al., 2005; Munafo et al., 2007; Pinto et al., 2008; Su et al., 2015). Therefore, it would be important to undertake GWAS analysis of PUI, including personality features as an additional facet. In this regard it would be important to include not only measures of impulsivity but also recently developed trans-diagnostic measures of compulsivity (Chamberlain and Grant, 2018), as well as other intermediate phenotypes.
7. Consider the impact of social factors in the development of PUI
While genetics and personality factors may play a role in PUI, social factors associated with PUI such as family and cultural factors and website architecture may be more amenable to modification and public health policy intervention.
Specific familial influences may contribute to the increased or decreased likelihood of an adolescent developing problem gaming. In a review of 14 recent studies, relevant family-related variables included: (a) parent status (e.g., socioeconomic status and mental health), (b) parent-child relationship (e.g., warmth, conflict, and abuse), (c) parental influence on gaming (e.g., supervision of gaming, modeling, and attitudes toward gaming), and (d) family environment (e.g., household composition) (Schneider et al., 2017). Most of the studies have focused on parent-child relationships, reporting that poorer quality relationships may be associated with increased severity of problem gaming, with some gender-specific influences. However, the review authors found that much of this research was limited by reliance on adolescent self-reports, without corroboration from parents and other family members, and so the intergenerational effects of problem gaming require further research. Notwithstanding, there is evidence to suggest that prevention programs and interventions for adolescents may be more effective in some cases if they can address familial influences on problem gaming, with the active co-participation of parents, rather than focussing on individual-based methods to the exclusion of the family (Schneider et al., 2017).
The role of cultural factors is of particular interest, given the higher estimated prevalence of PUI in some geographical locations than others, yet most studies have not specifically explored transcultural issues. In a recent online survey of 2,775 young adults (aged 18-29 years) recruited across different European Universities covering a wide geographical range, Northern and Southern regions reported the heaviest use of mobile phones, whereas perceived dependence was less prevalent in the Eastern region (Lopez-Fernandez et al., 2017). The proportion of highly dependent mobile phone users was highest in Belgium, UK, and France. Regression analysis identified several risk factors for increased self-reported mobile-phone dependence, including higher frequency of usage, specific Internet application usage (social networking, playing video games, shopping and viewing TV shows through the Internet, chatting and messaging), and being female. In a smaller questionnaire study (Yang et al., 2013a), in which Japanese students were more likely to demonstrate PUI than their Chinese counterparts, depression and perceived maternal care were identified as moderating factors associated with this cross-national difference.
Engagement in addictive behaviours on the Internet may be strongly linked to exposure to reward-dependent cues. For this reason, specific aspects of website architecture (form, content, reinforcing schedules) are likely to have an important effect on rates of Internet usage. Research in this area however is difficult to assess, as much is undertaken in commercial settings and is not available to the scientific community. Specific psychoactive substances and forms of gambling differ in their propensities for repetition, due to variable effects on the brain’s reward circuitry. For gambling, maximal engagement in gambling activities may be facilitated by incorporating psychologically relevant features such as variable ratio of reinforcement, losses-disguised-as-wins, and sense of control; and by encouraging perception of ‘near misses’ (Murch and Clark, 2016). Therefore, gambling researchers have highlighted the importance of focusing on the interaction between the ‘player’ and the ‘product’ from a public health perspective (Korn and Shaffer, 1999; Murch and Clark, 2016). We suggest that a similar strategy is needed for understanding PUI.
It is likely that structural elements of websites and applications serve to favour excessive use in vulnerable individuals, but that these elements may differ depending on the precise type of online activity considered. For video gaming, it appears that specific structural characteristics of the games (e.g., in-game reward system capitalizing on intermittent reinforcement, daily updated international rankings) may potentiate addictive/excessive usage (Griffiths and Nuyens, 2017). For problematic online sexual behaviour (e.g. cybersex), three structural elements have been highlighted as being important contributors per the so-termed Triple A Model involving: accessibility, affordability, and anonymity (Cooper, 1998; Cooper et al., 1999), though more research is needed on this topic (Brand et al., 2016a; Wery and Billieux, 2017). Another similar proposed framework is the ACE Model (anonymity, convenience, and escape) (Young, 2008). For excessive streaming (watching videos excessively), important structural features may include the ability of given programmes to grab attention by activating a biological ‘orientating response’, mediated through techniques including the use of attention-grabbing noises, zooming/panning, and presentation of rewarding stimuli (e.g., of a sexual or thrilling nature) (Flayelle et al., 2017; Flayelle et al., 2018). Collectively, public research into the structural elements that may promote PUI in different contexts is lacking.
8. Generate and validate effective interventions, both to prevent PUI, and to treat its various forms once established
Early identification of individuals at risk of developing different types of PUI, with a view to early intervention strategies, could in the future reduce the burden of disease and help to prevent untoward functional consequences. This suggestion draws parallels from positive findings in other related areas of mental health, such as early intervention for substance addictions, to mitigate suffering and public health burden (Tanner-Smith and Risser, 2016). In a systematic review of the available literature, only five data papers were identified that described and assessed preventative interventions for PUI (Vondrackova and Gabrhelik, 2016). The review authors found that there was high risk of bias in the core empirical papers examined, and reported that the main target groups for intervention were young people, parents of young people, and employees. In view of the heterogenous nature of the interventions used, inconsistent methodologies, and above-noted high risk of bias, rigorous early intervention studies are urgently needed before any definitive conclusions may be drawn as to whether particular early interventions are clinically effective and cost effective.
For most forms of PUI, no ‘evidence based’ treatments exist and clinical research remains at early stages. Several meta-analyses of available treatments have been conducted, which have highlighted methodological flaws in the extant literature, such as (but not limited to) small samples, lack of appropriate control conditions (e.g., lack of active control conditions as opposed to a waiting list control), limited information on adherence to treatment, and inconsistent diagnostic definitions and measurements of symptom severity (King et al., 2017; Zajac et al., 2017). To date, the strongest evidence appears to be for cognitive behaviour therapy (CBT) but due to study limitations definitive statements as to its benefits await further testing (King et al., 2017). A CBT model specifically designed for PUI has been piloted (Young, 2013). Appropriate controlled pharmacological treatment trials for PUI are absent. Future pharmacological treatment trials for PUI could be informed by findings from existing addictions and impulsive-compulsive disorders. For example, glutamate modulators and opioid antagonists show promise in certain behavioural addictions (Grant et al., 2016; Grant et al., 2008; Grant et al., 2014) and serotonin reuptake inhibitors are first-line treatment for OCD (Bandelow et al., 2008; Fineberg et al., 2015; Koran and Blair Simpson, 2013). Future work could also consider evaluating neuromodulatory treatments that are promising in other contexts, such as transcranial magnetic stimulation (Carmi et al., 2018). In addition, there is a need for developing early interventions and preventive measures which should include behavioural interventions as well as structural prevention related to game design, protection of youth and other measures that counteract excessive or addictive use.
9. Identify biomarkers, to improve early detection and intervention
Treating various forms of PUI from the outset using the most appropriate strategies (balancing patient risks and benefits, along with resource costs) is likely to produce better outcomes and represent better value than treating more severe presentations later in their courses. Translational studies targeting pathogenic mechanisms at genetic and intermediate phenotype levels (i.e., early stage vulnerability factors), may clarify crucial neurobiological mechanisms and form the basis for early illness-detection. Specifically, the discovery of a reliable set of markers of psychopathology, neuropsychology and neuroimaging may provide an innovative platform of screening tools with a sufficiently high level of specificity and sensitivity to detect PUI early in its onset. The Internet also opens new avenues for different types of biomarkers for PUI, e.g., digital fingerprinting / phenotyping. With the aid of appropriate algorithms, careful continuous monitoring of behaviours of individuals via digital tools with informed consent may help identify accurate biomarkers of PUI.
Extending ‘biomarkers’ research to young individuals at theoretical risk of developing PUI (such as the unaffected relatives of people with PUI) or prodromal phases of PUI, may permit early interventions that might alter the trajectory of the disorder toward a better long-term outcome. For example, if various forms of PUI could be reliably predicted from recognized traits and symptomatologies, such as tendencies toward disordered compulsive (urge-driven) behaviours, this could potentially have important implications for early identification of “at risk” individuals and timely intervention before problems take hold. However, the promise of identifying “at-risk” individuals and effectively preventing the development of such disorders has remained challenging, as continued youth engagement in addictive behaviours and disorders over time suggest (Potenza, 2013). Nonetheless, the Internet offers perhaps some unique opportunities for public policy interventions found useful for other risk behaviors (e.g., taxation to reduce tobacco use) (Gearhardt et al., 2011). Given differences across jurisdictions in Internet regulation, having a research network focused on PUI will be valuable in promoting health worldwide.
Conclusions
PUI represents an umbrella term for an emerging range of costly and burdensome behaviours that can occur across a large age range. Despite dedicated research and some breakthroughs in the scientific understanding of relevant neurobiological and psychosocial factors, the risk factors for PUI need future research. The current level of evidence has to be increased to promote the accurate diagnosis, prediction of prognosis, and development of effective interventional approaches. Action is needed to develop strategies to identify those who might be at increased risk of PUI at the earliest stages, in order to facilitate prompt and reliable diagnosis and devise preventative or therapeutic interventions at local and societal levels. In line with EU health priorities (Europe 2020, European Pact for Mental Health, EPMH), these actions would be expected to optimize health outcomes, improve quality of life and productivity and reduce overall disease burden. The EU-PUI Network brings together individuals with the knowledge and skills to set in motion a programme of research aimed at addressing these needs through networked research. Priorities include the following areas for different forms of PUI: reaching a consensus on conceptualisation, describing and defining the diagnostic criteria, developing and validating reliable tools, and quantifying the clinical and health economic impact. It will also be important, for different forms of PUI, to identify the underpinning brain-based mechanisms including the contribution of compulsive, impulsive and habit mechanisms as potential targets for intervention and biomarkers (including digital biomarkers) to advance early diagnosis, monitoring, management and public health policy. Through establishing shared multinational databases and collaborative research networks, it is anticipated that progress will be made. A multinational trans-cultural approach would ensure the generalizability of the results across Europe and beyond.
Funding
This publication is based upon work from COST Action CA16207 “European Network for Problematic Usage of the Internet”, supported by COST (European Cooperation in Science and Technology: www.cost.eu). The publication is also based on work supported by the European College of Neuropsychopharmacology Networks and the International College of Obsessive Compulsive Spectrum Disorders. Dr Chamberlain’s involvement in this project was supported by a Clinical Fellowship from the Wellcome Trust (UK; 110049/Z/15/Z). Zsolt Demetrovics acknowledges the support of the Hungarian National Research, Development and Innovation Office (Grant numbers: K111938, KKP126835). Dr Ioannidis involvement was supported by Health Education East of England Higher Training Special Interest sessions. Dr. Potenza’s involvement was supported by the National Center for Responsible Gaming through a Center of Excellence grant, the Connecticut Council on Problem Gambling and the Connecticut Department of Mental Health and Addiction Services. Dr King’s involvement was supported by a Discovery Early Career Researcher Award (DECRA) DE170101198 funded by the Australian Research Council (ARC). The funding agencies did not have input into the content of the manuscript and the views described in the manuscript reflect those of the authors and not necessarily those of the funding agencies. Dr Yucel was supported by a National Health and Medical Research Council of Australia Fellowship (#APP1117188) and the David Winston Turner Endowment Fund.
Footnotes
Disclosures: The authors report no conflict of interest with respect to the content of this manuscript. In the past year, NF has received research support from European College of Neuropsychopharmacology (ECNP), National Institute for Health Research, Wellcome Foundation. Dr Fineberg has received honoraria for lectures at scientific meetings from Abbott, Wiley, and British Association for Psychopharmacology (BAP). Dr Fineberg has received financial support to attend scientific meetings from the International Society for Affective Disorders, International Forum of Mood and Anxiety Disorders, ECNP, BAP and Royal College of Psychiatrists. Dr Fineberg has received financial royalties for publications from Oxford University Press and payment for editorial duties from Taylor and Francis. Dr Chamberlain receives an editorial fee from Elsevier in his capacity as associate editor at Neuroscience and Biobehavioral Reviews (NBBR). Dr Chamberlain consults for Cambridge Cognition and Shire. Dr. Hollander has received research grants in the past year from Department of Defense (DOD), Orphan Products Division of Food and Drug Administration (FDA), Roche, Curemark, Takeda, Avanir, and Neurocrine, Dr. Pallanti has received research grant in the past and current year from National Institute of Mental Health (NIMH) for a R21 on Theta Burst Stimulation in Gambling Disorder. Dr. Dell’Osso has received research grants in the past year from Angelini, Lundbeck and FB Health. Dr. Potenza has consulted for and advised Rivermend Health, Opiant/Lakelight Therapeutics and Jazz Pharmaceuticals; received research support (to Yale) from the Mohegan Sun Casino and the National Center for Responsible Gaming; consulted for or advised legal and gambling entities on issues related to impulse control and addictive behaviours; provided clinical care related to impulse control and addictive behaviours; performed grant reviews; edited journals/journal sections; given academic lectures in grand rounds, CME events and other clinical/scientific venues; and generated books or chapters for publishers of mental health texts. In the past 3 years, Dr. Stein has received research grants and/or consultancy honoraria from Biocodex, Lundbeck, Servier, and Sun. Joseph Zohar has received grant/research support from Lundbeck, Servier, Brainsway and Pfizer, has served as a consultant or on advisory boards for Servier, Pfizer, Abbott, Lilly, Actelion, AstraZeneca and Roche, and has served on speakers’ bureaus for Lundbeck, Roch, Lilly, Servier, Pfizer and Abbott. Dr. Grant has received research grants from TLC Foundation for Body Focused Repetitive Behaviors, NIAAA, and Takeda Pharmaceuticals. Dr. Burkauskas has served as a scientific consultant to CogState, Ltd. In the past 24 months, Dr. Van Ameringen has been on the Advisory Boards of Purdue, Allergan and Lundbeck, and Speaker’s Bureau for Purdue, Allergan, Lundbeck and Pfizer and has received research support from Janssen-Ortho Inc, Pfizer and the Hamilton Academic Health Sciences Organization (HAHSO) Innovation Grant (AFP Innovation Grant). Dr Yucel has received funding from law firms in relation to expert witness reports/statements; no funding was received in relation to the present article. The other authors report no disclosures.
References
- 2012. www.dsm5.org. American Psychiatric Association (APA)
- Anderson EL, Steen E, Stavropoulos V. Internet use and Problematic Internet Use: a systematic review of longitudinal research trends in adolescence and emergent adulthood. International Journal of Adolescence and Youth. 2017;22:430–454. [Google Scholar]
- Andreassen CS, Billieux J, Griffiths MD, Kuss DJ, Demetrovics Z, Mazzoni E, Pallesen S. The relationship between addictive use of social media and video games and symptoms of psychiatric disorders: A large-scale cross-sectional study. Psychol Addict Behav. 2016;30:252–262. doi: 10.1037/adb0000160. [DOI] [PubMed] [Google Scholar]
- Anttila V, Bulik-Sullivan B, Finucane H, Walters R, Bras J, Duncan L, Escott-Price V, Falcone G, PGormley P, RMalik R, Patsopoulos N, et al. Analysis of shared heritability in common disorders of the brain. bioRxiv. 2016 doi: 10.1126/science.aap8757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandelow B, Zohar J, Hollander E, Kasper S, Moller HJ, Zohar J, Hollander E, Kasper S, Moller HJ, Bandelow B, Allgulander C, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive-compulsive and post-traumatic stress disorders - first revision. World J Biol Psychiatry. 2008;9:248–312. doi: 10.1080/15622970802465807. [DOI] [PubMed] [Google Scholar]
- Billieux J, King DL, Higuchi S, Achab S, Bowden-Jones H, Hao W, Long J, Lee HK, Potenza MN, Saunders JB, Poznyak V. Functional impairment matters in the screening and diagnosis of gaming disorder. J Behav Addict. 2017;6:285–289. doi: 10.1556/2006.6.2017.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billieux J, Thorens G, Khazaal Y, Zullino D, Achab S, Van der Linden M. Problematic involvement in online games: A cluster analytic approach. Computers in Human Behavior. 2015;43:242–250. [Google Scholar]
- Brand M, Snagowski J, Laier C, Maderwald S. Ventral striatum activity when watching preferred pornographic pictures is correlated with symptoms of Internet pornography addiction. Neuroimage. 2016a;129:224–232. doi: 10.1016/j.neuroimage.2016.01.033. [DOI] [PubMed] [Google Scholar]
- Brand M, Young KS, Laier C, Wolfling K, Potenza MN. Integrating psychological and neurobiological considerations regarding the development and maintenance of specific Internet-use disorders: An Interaction of Person-Affect-Cognition-Execution (I-PACE) model. Neurosci Biobehav Rev. 2016b;71:252–266. doi: 10.1016/j.neubiorev.2016.08.033. [DOI] [PubMed] [Google Scholar]
- Breitling LP, Dahmen N, Mittelstrass K, Rujescu D, Gallinat J, Fehr C, Giegling I, Lamina C, Illig T, Muller H, Raum E, et al. Association of nicotinic acetylcholine receptor subunit alpha 4 polymorphisms with nicotine dependence in 5500 Germans. Pharmacogenomics J. 2009;9:219–224. doi: 10.1038/tpj.2009.6. [DOI] [PubMed] [Google Scholar]
- Brem S, Grunblatt E, Drechsler R, Riederer P, Walitza S. The neurobiological link between OCD and ADHD. Atten Defic Hyperact Disord. 2014;6:175–202. doi: 10.1007/s12402-014-0146-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne J, Albright K, Kardefelt-Winther D. Using research findings for policy-making. Global Kids Online; London: 2016. [Google Scholar]
- Carmi L, Alyagon U, Barnea-Ygael N, Zohar J, Dar R, Zangen A. Clinical and electrophysiological outcomes of deep TMS over the medial prefrontal and anterior cingulate cortices in OCD patients. Brain Stimul. 2018;11:158–165. doi: 10.1016/j.brs.2017.09.004. [DOI] [PubMed] [Google Scholar]
- Carter B, Rees P, Hale L, Bhattacharjee D, Paradkar MS. Association Between Portable Screen-Based Media Device Access or Use and Sleep Outcomes: A Systematic Review and Meta-analysis. JAMA Pediatr. 2016;170:1202–1208. doi: 10.1001/jamapediatrics.2016.2341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain SR, Grant JE. Initial Validation of a Trans-diagnostic Compulsivity Questionnaire: The Cambridge-Chicago Compulsivity Trait Scale. CNS Spectrums. 2018 doi: 10.1017/S1092852918000810. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain SR, Ioannidis K, Grant JE. The impact of comorbid impulsive/compulsive disorders in problematic Internet use. J Behav Addict. 2018:1–7. doi: 10.1556/2006.7.2018.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain SR, Ioannidis K, Leppink EW, Niaz F, Redden SA, Grant JE. ADHD symptoms in non-treatment seeking young adults: relationship with other forms of impulsivity. CNS Spectr. 2017a;22:22–30. doi: 10.1017/S1092852915000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain SR, Lochner C, Stein DJ, Goudriaan AE, van Holst RJ, Zohar J, Grant JE. Behavioural addiction-A rising tide? Eur Neuropsychopharmacol. 2016;26:841–855. doi: 10.1016/j.euroneuro.2015.08.013. [DOI] [PubMed] [Google Scholar]
- Chamberlain SR, Menzies L. Endophenotypes of obsessive-compulsive disorder: rationale, evidence and future potential. Expert Rev Neurother. 2009;9:1133–1146. doi: 10.1586/ern.09.36. [DOI] [PubMed] [Google Scholar]
- Chamberlain SR, Redden SA, Stein DJ, Lochner C, Grant JE. Impact of obsessive-compulsive personality disorder symptoms in Internet users. Ann Clin Psychiatry. 2017b;29:173–181. [PMC free article] [PubMed] [Google Scholar]
- Cheng YS, Tseng PT, Lin PY, Chen TY, Stubbs B, Carvalho AF, Wu CK, Chen YW, Wu MK. Internet Addiction and Its Relationship With Suicidal Behaviors: A Meta-Analysis of Multinational Observational Studies. J Clin Psychiatry. 2018;79 doi: 10.4088/JCP.17r11761. [DOI] [PubMed] [Google Scholar]
- Clark L, Limbrick-Oldfield EH. Disordered gambling: a behavioral addiction. Curr Opin Neurobiol. 2013;23:655–659. doi: 10.1016/j.conb.2013.01.004. [DOI] [PubMed] [Google Scholar]
- Cooper A. Sexuality and the Internet: Surfing into the new millennium. Cyberpsychology & Behavior. 1998;1:181–187. [Google Scholar]
- Cooper A, Scherer CR, Boies SC, Gordon BL. Sexuality on the Internet: From sexual exploration to pathological expression. Professional Psychology: Research and Practice. 1999;30:154–164. [Google Scholar]
- Dell'Osso B, Altamura AC, Allen A, Marazziti D, Hollander E. Epidemiologic and clinical updates on impulse control disorders: a critical review. Eur Arch Psychiatry Clin Neurosci. 2006;256:464–475. doi: 10.1007/s00406-006-0668-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dell'Osso B, Benatti B, Buoli M, Altamura AC, Marazziti D, Hollander E, Fineberg N, Stein DJ, Pallanti S, Nicolini H, Van Ameringen M, et al. The influence of age at onset and duration of illness on long-term outcome in patients with obsessive-compulsive disorder: a report from the International College of Obsessive Compulsive Spectrum Disorders (ICOCS) Eur Neuropsychopharmacol. 2013;23:865–871. doi: 10.1016/j.euroneuro.2013.05.004. [DOI] [PubMed] [Google Scholar]
- Demetrovics Z, Kiraly O, Koronczai B, Griffiths MD, Nagygyorgy K, Elekes Z, Tamas D, Kun B, Kokonyei G, Urban R. Psychometric Properties of the Problematic Internet Use Questionnaire Short-Form (PIUQ-SF-6) in a Nationally Representative Sample of Adolescents. PLoS One. 2016;11:e0159409. doi: 10.1371/journal.pone.0159409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demetrovics Z, Urban R, Nagygyorgy K, Farkas J, Griffiths MD, Papay O, Kokonyei G, Felvinczi K, Olah A. The development of the Problematic Online Gaming Questionnaire (POGQ) PLoS One. 2012;7:e36417. doi: 10.1371/journal.pone.0036417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derbyshire KL, Lust KA, Schreiber LR, Odlaug BL, Christenson GA, Golden DJ, Grant JE. Problematic Internet use and associated risks in a college sample. Compr Psychiatry. 2013;54:415–422. doi: 10.1016/j.comppsych.2012.11.003. [DOI] [PubMed] [Google Scholar]
- Deryakulu D, Ursavas OF. Genetic and environmental influences on problematic Internet use: A twin study. Comput Hum Behav. 2014;39:331–338. [Google Scholar]
- Dong G, Potenza MN. A cognitive-behavioral model of Internet gaming disorder: theoretical underpinnings and clinical implications. J Psychiatr Res. 2014;58:7–11. doi: 10.1016/j.jpsychires.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkee T, Carli V, Floderus B, Wasserman C, Sarchiapone M, Apter A, Balazs JA, Bobes J, Brunner R, Corcoran P, Cosman D, et al. Pathological Internet Use and Risk-Behaviors among European Adolescents. Int J Environ Res Public Health. 2016;13 doi: 10.3390/ijerph13030294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Y, Niu T, Xing H, Xu X, Chen C, Peng S, Wang L, Laird N, Xu X. A common haplotype of the nicotine acetylcholine receptor alpha 4 subunit gene is associated with vulnerability to nicotine addiction in men. Am J Hum Genet. 2004;75:112–121. doi: 10.1086/422194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergus TA. Cyberchondria and intolerance of uncertainty: examining when individuals experience health anxiety in response to Internet searches for medical information. Cyberpsychol Behav Soc Netw. 2013;16:735–739. doi: 10.1089/cyber.2012.0671. [DOI] [PubMed] [Google Scholar]
- Fergus TA, Spada MM. Cyberchondria: Examining relations with problematic Internet use and metacognitive beliefs. Clin Psychol Psychother. 2017;24:1322–1330. doi: 10.1002/cpp.2102. [DOI] [PubMed] [Google Scholar]
- Few LR, Grant JD, Trull TJ, Statham DJ, Martin NG, Lynskey MT, Agrawal A. Genetic variation in personality traits explains genetic overlap between borderline personality features and substance use disorders. Addiction. 2014;109:2118–2127. doi: 10.1111/add.12690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fineberg NA, Apergis-Schoute AM, Vaghi MM, Banca P, Gillan CM, Voon V, Chamberlain SR, Cinosi E, Reid J, Shahper S, Bullmore ET, et al. Mapping Compulsivity in the DSM-5 Obsessive Compulsive and Related Disorders: Cognitive Domains, Neural Circuitry, and Treatment. Int J Neuropsychopharmacol. 2018;21:42–58. doi: 10.1093/ijnp/pyx088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fineberg NA, Reghunandanan S, Simpson HB, Phillips KA, Richter MA, Matthews K, Stein DJ, Sareen J, Brown A, Sookman D, Accreditation Task Force of The Canadian Institute for Obsessive Compulsive, D. Obsessive-compulsive disorder (OCD): Practical strategies for pharmacological and somatic treatment in adults. Psychiatry Res. 2015;227:114–125. doi: 10.1016/j.psychres.2014.12.003. [DOI] [PubMed] [Google Scholar]
- Finkenauer C, Pollmann MM, Begeer S, Kerkhof P. Brief report: examining the link between autistic traits and compulsive Internet use in a non-clinical sample. J Autism Dev Disord. 2012;42:2252–2256. doi: 10.1007/s10803-012-1465-4. [DOI] [PubMed] [Google Scholar]
- Fischer G, Brunner R, Parzer P, Klug K, Durkee T, Carli V, Wasserman D, Vonderlin E, Resch F, Kaess M. [Depression, deliberate self-harm and suicidal behaviour in adolescents engaging in risky and pathological internet use] Prax Kinderpsychol Kinderpsychiatr. 2012;61:16–31. doi: 10.13109/prkk.2012.61.1.16. [DOI] [PubMed] [Google Scholar]
- Flayelle M, Maurage P, Billieux J. Toward a qualitative understanding of binge-watching behaviors: A focus group approach. J Behav Addict. 2017;6:457–471. doi: 10.1556/2006.6.2017.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flayelle M, Maurage P, Vogele C, Karila L, Billieux J. Time for a Plot Twist: Beyond Confirmatory Approaches to Binge-Watching Research. Psychology of Popular Media Culture. 2018 In press. Available via pre-print respository: http://orbilu.uni.lu/handle/10993/35101. [Google Scholar]
- Gearhardt AN, Grilo CM, DiLeone RJ, Brownell KD, Potenza MN. Can food be addictive? Public health and policy implications. Addiction. 2011;106:1208–1212. doi: 10.1111/j.1360-0443.2010.03301.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentile DA, Choo H, Liau A, Sim T, Li D, Fung D, Khoo A. Pathological video game use among youths: a two-year longitudinal study. Pediatrics. 2011;127:e319–329. doi: 10.1542/peds.2010-1353. [DOI] [PubMed] [Google Scholar]
- Grant JE, Chamberlain SR. Impulsive action and impulsive choice across substance and behavioral addictions: cause or consequence? Addict Behav. 2014;39:1632–1639. doi: 10.1016/j.addbeh.2014.04.022. [DOI] [PubMed] [Google Scholar]
- Grant JE, Chamberlain SR, Redden SA, Leppink EW, Odlaug BL, Kim SW. N-Acetylcysteine in the Treatment of Excoriation Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2016;73:490–496. doi: 10.1001/jamapsychiatry.2016.0060. [DOI] [PubMed] [Google Scholar]
- Grant JE, Kim SW, Hartman BK. A double-blind, placebo-controlled study of the opiate antagonist naltrexone in the treatment of pathological gambling urges. J Clin Psychiatry. 2008;69:783–789. doi: 10.4088/jcp.v69n0511. [DOI] [PubMed] [Google Scholar]
- Grant JE, Odlaug BL, Chamberlain SR, Potenza MN, Schreiber LR, Donahue CB, Kim SW. A randomized, placebo-controlled trial of N-acetylcysteine plus imaginal desensitization for nicotine-dependent pathological gamblers. J Clin Psychiatry. 2014;75:39–45. doi: 10.4088/JCP.13m08411. [DOI] [PubMed] [Google Scholar]
- Gray JC, MacKillop J, Weafer J, Hernandez KM, Gao J, Palmer AA, de Wit H. Genetic analysis of impulsive personality traits: Examination of a priori candidates and genome-wide variation. Psychiatry Res. 2018;259:398–404. doi: 10.1016/j.psychres.2017.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths MD, Nuyens F. An Overview of Structural Characteristics in Problematic Video Game Playing. Curr Addict Rep. 2017;4:272–283. doi: 10.1007/s40429-017-0162-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grunblatt E, Marinova Z, Roth A, Gardini E, Ball J, Geissler J, Wojdacz TK, Romanos M, Walitza S. Combining genetic and epigenetic parameters of the serotonin transporter gene in obsessive-compulsive disorder. J Psychiatr Res. 2018;96:209–217. doi: 10.1016/j.jpsychires.2017.10.010. [DOI] [PubMed] [Google Scholar]
- Gyollai A, Griffiths MD, Barta C, Vereczkei A, Urban R, Kun B, Kokonyei G, Szekely A, Sasvari-Szekely M, Blum K, Demetrovics Z. The genetics of problem and pathological gambling: a systematic review. Curr Pharm Des. 2014;20:3993–3999. doi: 10.2174/13816128113199990626. [DOI] [PubMed] [Google Scholar]
- Hahn E, Reuter M, Spinath FM, Montag C. Internet addiction and its facets: The role of genetics and the relation to self-directedness. Addict Behav. 2017;65:137–146. doi: 10.1016/j.addbeh.2016.10.018. [DOI] [PubMed] [Google Scholar]
- Han DH, Lee YS, Yang KC, Kim EY, Lyoo IK, Renshaw PF. Dopamine genes and reward dependence in adolescents with excessive internet video game play. J Addict Med. 2007;1:133–138. doi: 10.1097/ADM.0b013e31811f465f. [DOI] [PubMed] [Google Scholar]
- Han S, Yang BZ, Kranzler HR, Oslin D, Anton R, Gelernter J. Association of CHRNA4 polymorphisms with smoking behavior in two populations. Am J Med Genet B Neuropsychiatr Genet. 2011;156B:421–429. doi: 10.1002/ajmg.b.31177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho RC, Zhang MW, Tsang TY, Toh AH, Pan F, Lu Y, Cheng C, Yip PS, Lam LT, Lai CM, Watanabe H, et al. The association between internet addiction and psychiatric co-morbidity: a meta-analysis. BMC Psychiatry. 2014;14:183. doi: 10.1186/1471-244X-14-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ioannidis K, Chamberlain SR, Treder MS, Kiraly F, Leppink EW, Redden SA, Stein DJ, Lochner C, Grant JE. Problematic internet use (PIU): Associations with the impulsive-compulsive spectrum. An application of machine learning in psychiatry. J Psychiatr Res. 2016;83:94–102. doi: 10.1016/j.jpsychires.2016.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ioannidis K, Treder MS, Chamberlain SR, Kiraly F, Redden SA, Stein DJ, Lochner C, Grant JE. Problematic internet use as an age-related multifaceted problem: Evidence from a two-site survey. Addict Behav. 2018;81:157–166. doi: 10.1016/j.addbeh.2018.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakubovski E, Diniz JB, Valerio C, Fossaluza V, Belotto-Silva C, Gorenstein C, Miguel E, Shavitt RG. Clinical predictors of long-term outcome in obsessive-compulsive disorder. Depress Anxiety. 2013;30:763–772. doi: 10.1002/da.22013. [DOI] [PubMed] [Google Scholar]
- Jeong JE, Rhee JK, Kim TM, Kwak SM, Bang SH, Cho H, Cheon YH, Min JA, Yoo GS, Kim K, Choi JS, et al. The association between the nicotinic acetylcholine receptor alpha4 subunit gene (CHRNA4) rs1044396 and Internet gaming disorder in Korean male adults. PLoS One. 2017;12:e0188358. doi: 10.1371/journal.pone.0188358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kardefelt-Winther D. Conceptualizing Internet use disorders: Addiction or coping process? Psychiatry Clin Neurosci. 2017;71:459–466. doi: 10.1111/pcn.12413. [DOI] [PubMed] [Google Scholar]
- Kim JY, Jeong JE, Rhee JK, Cho H, Chun JW, Kim TM, Choi SW, Choi JS, Kim DJ. Targeted exome sequencing for the identification of a protective variant against Internet gaming disorder at rs2229910 of neurotrophic tyrosine kinase receptor, type 3 (NTRK3): A pilot study. J Behav Addict. 2016a;5:631–638. doi: 10.1556/2006.5.2016.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim NR, Hwang SS, Choi JS, Kim DJ, Demetrovics Z, Kiraly O, Nagygyorgy K, Griffiths MD, Hyun SY, Youn HC, Choi SW. Characteristics and Psychiatric Symptoms of Internet Gaming Disorder among Adults Using Self-Reported DSM-5 Criteria. Psychiatry Investig. 2016b;13:58–66. doi: 10.4306/pi.2016.13.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King DL, Delfabbro PH, Potenza MN, Demetrovics Z, Billieux J, Brand M. Internet gaming disorder should qualify as a mental disorder. Aust N Z J Psychiatry. 2018 doi: 10.1177/0004867418771189. 4867418771189. [DOI] [PubMed] [Google Scholar]
- King DL, Delfabbro PH, Wu AMS, Doh YY, Kuss DJ, Pallesen S, Mentzoni R, Carragher N, Sakuma H. Treatment of Internet gaming disorder: An international systematic review and CONSORT evaluation. Clin Psychol Rev. 2017;54:123–133. doi: 10.1016/j.cpr.2017.04.002. [DOI] [PubMed] [Google Scholar]
- Kiraly O, Griffiths MD, King DL, Lee HK, Lee SY, Banyai F, Zsila A, Takacs ZK, Demetrovics Z. Policy responses to problematic video game use: A systematic review of current measures and future possibilities. J Behav Addict. 2017a:1–15. doi: 10.1556/2006.6.2017.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiraly O, Nagygyorgy BK, Koronczai B, Griffiths MD, Demetrovics Z. Assessment of Problematic Internet Use and Online Video Gaming. In: Aboujaoude E, Starcevic V, editors. Mental Health in the Digital Age. Oxford University Press; 2015. [Google Scholar]
- Kiraly O, Sleczka P, Pontes HM, Urban R, Griffiths MD, Demetrovics Z. Validation of the Ten-Item Internet Gaming Disorder Test (IGDT-10) and evaluation of the nine DSM-5 Internet Gaming Disorder criteria. Addict Behav. 2017b;64:253–260. doi: 10.1016/j.addbeh.2015.11.005. [DOI] [PubMed] [Google Scholar]
- Koran LM, Blair Simpson H. Guideline Watch (March 2013): Practice Guideline for the Treatment of Patients with Obsessive-Compulsive Disorder. APA Practice Guidelines. 2013:1–22. [Google Scholar]
- Korn DA, Shaffer HJ. Gambling and the Health of the Public: Adopting a Public Health Perspective. J Gambl Stud. 1999;15:289–365. doi: 10.1023/a:1023005115932. [DOI] [PubMed] [Google Scholar]
- Kreek MJ, Nielsen DA, Butelman ER, LaForge KS. Genetic influences on impulsivity, risk taking, stress responsivity and vulnerability to drug abuse and addiction. Nat Neurosci. 2005;8:1450–1457. doi: 10.1038/nn1583. [DOI] [PubMed] [Google Scholar]
- Kuss DJ, Griffiths MD, Karila L, Billieux J. Internet addiction: a systematic review of epidemiological research for the last decade. Curr Pharm Des. 2014;20:4026–4052. doi: 10.2174/13816128113199990617. [DOI] [PubMed] [Google Scholar]
- Lam LT, Lam MK. eHealth Intervention for Problematic Internet Use (PIU) Curr Psychiatry Rep. 2016;18:107. doi: 10.1007/s11920-016-0747-5. [DOI] [PubMed] [Google Scholar]
- Le Foll B, Gallo A, Le Strat Y, Lu L, Gorwood P. Genetics of dopamine receptors and drug addiction: a comprehensive review. Behav Pharmacol. 2009;20:1–17. doi: 10.1097/FBP.0b013e3283242f05. [DOI] [PubMed] [Google Scholar]
- Lee YS, Han DH, Yang KC, Daniels MA, Na C, Kee BS, Renshaw PF. Depression like characteristics of 5HTTLPR polymorphism and temperament in excessive internet users. J Affect Disord. 2008;109:165–169. doi: 10.1016/j.jad.2007.10.020. [DOI] [PubMed] [Google Scholar]
- Li M, Chen J, Li N, Li X. A twin study of problematic internet use: its heritability and genetic association with effortful control. Twin Res Hum Genet. 2014;17:279–287. doi: 10.1017/thg.2014.32. [DOI] [PubMed] [Google Scholar]
- Liu HC, Liu SI, Tjung JJ, Sun FJ, Huang HC, Fang CK. Self-harm and its association with internet addiction and internet exposure to suicidal thought in adolescents. J Formos Med Assoc. 2017;116:153–160. doi: 10.1016/j.jfma.2016.03.010. [DOI] [PubMed] [Google Scholar]
- Liu TC, Desai RA, Krishnan-Sarin S, Cavallo DA, Potenza MN. Problematic Internet use and health in adolescents: data from a high school survey in Connecticut. J Clin Psychiatry. 2011;72:836–845. doi: 10.4088/JCP.10m06057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo MT, Hinds DA, Tung JY, Franz C, Fan CC, Wang Y, Smeland OB, Schork A, Holland D, Kauppi K, Sanyal N, et al. Genome-wide analyses for personality traits identify six genomic loci and show correlations with psychiatric disorders. Nat Genet. 2017;49:152–156. doi: 10.1038/ng.3736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long EC, Verhulst B, Neale MC, Lind PA, Hickie IB, Martin NG, Gillespie NA. The Genetic and Environmental Contributions to Internet Use and Associations With Psychopathology: A Twin Study. Twin Res Hum Genet. 2016;19:1–9. doi: 10.1017/thg.2015.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Fernandez O, Kuss DJ, Romo L, Morvan Y, Kern L, Graziani P, Rousseau A, Rumpf HJ, Bischof A, Gassler AK, Schimmenti A, et al. Self-reported dependence on mobile phones in young adults: A European cross-cultural empirical survey. J Behav Addict. 2017;6:168–177. doi: 10.1556/2006.6.2017.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchant A, Hawton K, Stewart A, Montgomery P, Singaravelu V, Lloyd K, Purdy N, Daine K, John A. A systematic review of the relationship between internet use, self-harm and suicidal behaviour in young people: The good, the bad and the unknown. PLoS One. 2017;12:e0181722. doi: 10.1371/journal.pone.0181722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihara S, Higuchi S. Cross-sectional and longitudinal epidemiological studies of Internet gaming disorder: A systematic review of the literature. Psychiatry Clin Neurosci. 2017;71:425–444. doi: 10.1111/pcn.12532. [DOI] [PubMed] [Google Scholar]
- Montag C, Jurkiewicz M, Reuter M. Low self-directedness is a better predictor for problematic internet use than high neuroticism. Comput Hum Behav. 2010;26:1531–1535. [Google Scholar]
- Montag C, Kirsch P, Sauer C, Markett S, Reuter M. The role of the CHRNA4 gene in Internet addiction: a case-control study. J Addict Med. 2012;6:191–195. doi: 10.1097/ADM.0b013e31825ba7e7. [DOI] [PubMed] [Google Scholar]
- Munafo MR, Matheson IJ, Flint J. Association of the DRD2 gene Taq1A polymorphism and alcoholism: a meta-analysis of case-control studies and evidence of publication bias. Mol Psychiatry. 2007;12:454–461. doi: 10.1038/sj.mp.4001938. [DOI] [PubMed] [Google Scholar]
- Murch WS, Clark L. Games in the Brain: Neural Substrates of Gambling Addiction. Neuroscientist. 2016;22:534–545. doi: 10.1177/1073858415591474. [DOI] [PubMed] [Google Scholar]
- Pallanti S, DeCaria CM, Grant JE, Urpe M, Hollander E. Reliability and validity of the pathological gambling adaptation of the Yale-Brown Obsessive-Compulsive Scale (PG-YBOCS) J Gambl Stud. 2005;21:431–443. doi: 10.1007/s10899-005-5557-3. [DOI] [PubMed] [Google Scholar]
- Parliament (UK) Parliamentary Archives. 2017. Select Committee on Communications: Growing up with the Internet: HL Paper 130. (020 7129 3074) [Google Scholar]
- Petry NM. Should the scope of addictive behaviors be broadened to include pathological gambling? Addiction. 2006;101(Suppl 1):152–160. doi: 10.1111/j.1360-0443.2006.01593.x. [DOI] [PubMed] [Google Scholar]
- Pinto E, Reggers J, Gorwood P, Boni C, Scantamburlo G, Pitchot W, Ansseau M. The short allele of the serotonin transporter promoter polymorphism influences relapse in alcohol dependence. Alcohol Alcohol. 2008;43:398–400. doi: 10.1093/alcalc/agn015. [DOI] [PubMed] [Google Scholar]
- Pontes HM, Kiraly O, Demetrovics Z, Griffiths MD. The conceptualisation and measurement of DSM-5 Internet Gaming Disorder: the development of the IGD-20 Test. PloS one. 2014;9:e110137. doi: 10.1371/journal.pone.0110137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potenza MN. Should addictive disorders include non-substance-related conditions? Addiction. 2006;101(Suppl 1):142–151. doi: 10.1111/j.1360-0443.2006.01591.x. [DOI] [PubMed] [Google Scholar]
- Potenza MN. Biological contributions to addictions in adolescents and adults: prevention, treatment, and policy implications. J Adolesc Health. 2013;52:S22–32. doi: 10.1016/j.jadohealth.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potenza MN, Higuchi S, Brand M. Call for research into a wider range of behavioural addictions. Nature. 2018;555:30. doi: 10.1038/d41586-018-02568-z. [DOI] [PubMed] [Google Scholar]
- Potenza MN, Koran LM, Pallanti S. The relationship between impulse-control disorders and obsessive-compulsive disorder: a current understanding and future research directions. Psychiatry Res. 2009;170:22–31. doi: 10.1016/j.psychres.2008.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid MC, Fiellin DA, O'Connor PG. Hazardous and harmful alcohol consumption in primary care. Arch Intern Med. 1999;159:1681–1689. doi: 10.1001/archinte.159.15.1681. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Hao W, Long J, King DL, Mann K, Fauth-Buhler M, Rumpf HJ, Bowden-Jones H, Rahimi-Movaghar A, Chung T, Chan E, et al. Gaming disorder: Its delineation as an important condition for diagnosis, management, and prevention. J Behav Addict. 2017;6:271–279. doi: 10.1556/2006.6.2017.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider LA, King DL, Delfabbro PH. Family factors in adolescent problematic Internet gaming: A systematic review. J Behav Addict. 2017;6:321–333. doi: 10.1556/2006.6.2017.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su H, Li Z, Du J, Jiang H, Chen Z, Sun H, Zhao M. Predictors of heroin relapse: Personality traits, impulsivity, COMT gene Val158met polymorphism in a 5-year prospective study in Shanghai, China. Am J Med Genet B Neuropsychiatr Genet. 2015;168:712–719. doi: 10.1002/ajmg.b.32376. [DOI] [PubMed] [Google Scholar]
- Tammimaki AE, Mannisto PT. Are genetic variants of COMT associated with addiction? Pharmacogenet Genomics. 2010;20:717–741. doi: 10.1097/FPC.0b013e328340bdf2. [DOI] [PubMed] [Google Scholar]
- Tanner-Smith EE, Risser MD. A meta-analysis of brief alcohol interventions for adolescents and young adults: variability in effects across alcohol measures. Am J Drug Alcohol Abuse. 2016;42:140–151. doi: 10.3109/00952990.2015.1136638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge JM, Martin GN, Campbell WK. Decreases in Psychological Well-Being Among American Adolescents After 2012 and Links to Screen Time During the Rise of Smartphone Technology. Emotion. 2018 doi: 10.1037/emo0000403. [DOI] [PubMed] [Google Scholar]
- Vink JM, van Beijsterveldt TC, Huppertz C, Bartels M, Boomsma DI. Heritability of compulsive Internet use in adolescents. Addict Biol. 2016;21:460–468. doi: 10.1111/adb.12218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volpe U, Del'Osso B, Fiorillo A, Mucic D, Aboujaoude E. Internet-related psychopathology: clinical phenotypes and perspectives in an evolving field. Journal of Psychopathology. 2015:406–414. [Google Scholar]
- Vondrackova P, Gabrhelik R. Prevention of Internet addiction: A systematic review. J Behav Addict. 2016;5:568–579. doi: 10.1556/2006.5.2016.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wareham JD, Potenza MN. Pathological gambling and substance use disorders. Am J Drug Alcohol Abuse. 2010;36:242–247. doi: 10.3109/00952991003721118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein A, Livny A, Weizman A. New developments in brain research of internet and gaming disorder. Neurosci Biobehav Rev. 2017;75:314–330. doi: 10.1016/j.neubiorev.2017.01.040. [DOI] [PubMed] [Google Scholar]
- Wery A, Billieux J. Problematic cybersex: Conceptualization, assessment, and treatment. Addict Behav. 2017;64:238–246. doi: 10.1016/j.addbeh.2015.11.007. [DOI] [PubMed] [Google Scholar]
- Winkler A, Dorsing B, Rief W, Shen Y, Glombiewski JA. Treatment of internet addiction: a meta-analysis. Clin Psychol Rev. 2013;33:317–329. doi: 10.1016/j.cpr.2012.12.005. [DOI] [PubMed] [Google Scholar]
- World Health Organization. 2014. Public Health Implications of Excessive Use of the Internet, Computers, Smartphones, and Similar Electronic Devices. [Google Scholar]
- Yang CY, Sato T, Yamawaki N, Miyata M. Prevalence and risk factors of problematic Internet use: a cross-national comparison of Japanese and Chinese university students. Transcult Psychiatry. 2013a;50:263–279. doi: 10.1177/1363461513488876. [DOI] [PubMed] [Google Scholar]
- Yang Z, Seneviratne C, Wang S, Ma JZ, Payne TJ, Wang J, Li MD. Serotonin transporter and receptor genes significantly impact nicotine dependence through genetic interactions in both European American and African American smokers. Drug Alcohol Depend. 2013b;129:217–225. doi: 10.1016/j.drugalcdep.2012.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao YW, Liu L, Ma SS, Shi XH, Zhou N, Zhang JT, Potenza MN. Functional and structural neural alterations in Internet gaming disorder: A systematic review and meta-analysis. Neurosci Biobehav Rev. 2017;83:313–324. doi: 10.1016/j.neubiorev.2017.10.029. [DOI] [PubMed] [Google Scholar]
- Young K. Internet Addiction: The Emergence of a New Clinical Disorder. Cyberpsychol & Behav. 2009:237–244. [Google Scholar]
- Young KS. Caught in the net: how to recognize the signs of internet addiction – and a winning strategy for recovery. Wiley; New York: 1998. [Google Scholar]
- Young KS. Internet sex addiction: Risk factors, stages of development, and treatment. American Behavioral Scientist. 2008;52:21–37. [Google Scholar]
- Young KS. Treatment outcomes using CBT-IA with Internet-addicted patients. J Behav Addict. 2013;2:209–215. doi: 10.1556/JBA.2.2013.4.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zajac K, Ginley MK, Chang R, Petry NM. Treatments for Internet gaming disorder and Internet addiction: A systematic review. Psychol Addict Behav. 2017;31:979–994. doi: 10.1037/adb0000315. [DOI] [PMC free article] [PubMed] [Google Scholar]