Abstract
Purpose
To systematically study somatic variants arising during development in the human brain across a spectrum of neurodegenerative disorders.
Methods
In this study we developed a pipeline to identify somatic variants from exome sequencing data in 1461 diseased and control human brains. 88% of the DNA samples were extracted from the cerebellum. Identified somatic variants were validated by targeted amplicon sequencing and/or PyroMark® Q24.
Results
We observed somatic coding variants present in >10% of sampled cells in at least 1% of brains. The mutational signature of the detected variants showed a predominance of C>T variants most consistent with arising from DNA mis-match repair, occurred frequently in genes that are highly expressed within the central nervous system, and with a minimum somatic mutation rate of 4.25x10-10 per base pair per individual.
Conclusion
These findings provide proof-of-principle that deleterious somatic variants can affect sizeable brain regions in at least 1% of the population, and thus have the potential to contribute to the pathogenesis of common neurodegenerative diseases.
Keywords: somatic variant, brain, neurodegenerative disorders, exome sequencing, embryogenesis
Introduction
Pathogenic genetic variants affecting over 50 nuclear genes contribute to the pathogenesis of late onset neurological disorders 1. Present in every cell in the body, these genetic variants are either inherited or arise through a de novo variant in the gamete. In contrast, some age-related disorders such as cancer arise through the accumulation of somatic variants within a cell lineage during life, creating genetic heterogeneity within a tissue or organ (somatic mosaicism). Almost half of these variants arise decades before tumour initiation 2–4, raising the possibility that somatic variants acquired by a similar process during development are also present within non-malignant human tissues. Within the nervous system, somatic variants have been identified in rare, early onset, focal neurological disorders such hemimegalencephaly and lissencephaly 5–8, demonstrating that protein-coding variants with mosaic allelic fractions as low as 8% in the brain can cause macroscopically overt structural neurological diseases 6, though even lower allelic fractions of around 1% may cause milder phenotypes such as focal cortical dysplasia 9. To date however, the frequency of somatic variants in the human brain, and particularly in those late-onset neurological disorders has not been studied systematically.
Material and Methods
Brain samples
DNA was extracted from 1461 human brains (cerebellum: n=1281 (87.7%), cerebral cortex: n=94 (6.5%), basal ganglia: n=8 (0.5%), not classified: n=78 (5.3%)) from 1099 patients with neurodegenerative diseases including Alzheimer’s disease, Frontotemporal dementia or Amyotrophic lateral sclerosis (FTD-ALS), Creutzfeldt Jackob disease (CJD), Parkinson’s disease and Dementia with Lewy bodies (PD-DLB) and 362 age-matched controls within the Medical Research Council (MRC) UK Brain Bank Network. Controls were defined as having no ante mortem history of neurological disease, no neuropathological features of any neurodegenerative disease and a Braak neurofibrillary tangle stage of ≤ 2 (Figure 1a, b, Supplementary Material Table 1 for demographics & clinical data). The characteristics of the study group have been described previously 10. Brain regions were sampled from available brain regions with the maximum DNA extraction yield per milligram of tissue.
Figure 1. Detection of somatic variants in 1461 post mortem human brains.
(a) Brain regions sampled within the study. (b) The proportion and number of individuals in each cohort. (c) Unfiltered VAF with between 10% and 35% against relative exome sequencing depth. Those that were present before and after filtering are shown (red and blue respectively). (d) Variant detection pipeline. Section I - Exons are shown in red, with intergeneic and intronic regions as a black line. II - Regions of high genomic complexity and common structural variants (determined from population databases and previous studies) were removed (yellow line / grey box). III- relative sequencing depth of each exon is shown in blue above the relevant exon. Bases in which the sequencing depth was below 30 (as depicted by the red dashed line) in an individual were removed. These regions are then shown by grey boxes on the schematic exome and were also removed. IV – Finally, regions in which copy number variants (gains or losses) were called from array genotyping10 were also removed from the overall panel. An example plot of the array genotyping in which a copy number gain has been detected is shown. Again the corresponding region was removed from the exome depicted by a grey box on the exome panel. After these steps, remaining regions were subsequently subjected to analysis by deepSNV and a binomial test against the mean VAF for heterozygous variants (47%). (e) Schematic representation of the putative somatic alleles in the dataset. A distribution of VAF in the whole dataset is show (pink histogram). Putative somatic alleles were those in which the VAF was greater than base error rate (as determined from DeepSNV (green box and linked inset)), and those that also differed from the binomial threshold (<1x10-5) compared to an assumed VAF of 47% for heterozygosity.
Exome sequencing (WES) and somatic variant calling
Exome sequencing was performed on all samples as previously described 10. Sequencing data was aligned against the UCSC hg19 human reference genome using Burrows-Wheeler Aligner (BWA) 11. GATK’s Haplotype Caller from Genome Analysis Toolkit (GATK version 3.4) was used to determine allelic counts and genotypes across the genome 12. We excluded the following regions within quality control: (1) regions with the higher likelihood of misalignment and PCR artefacts in the genome 2; (2) specific small CNVs in 1321 individuals called by array genotyping 10; and (3) sites with read depth < 30x in any sample (Figure 1c, d, Supplementary Material Figure 1 and 2). This resulted in a total of 5,906,849 base pairs (bp) per individual available for subsequent analysis.
To detect putative somatic variants, we used a modified work-flow that was initially described by Genovese et al 2, but this time using a pan-exome approach. Firstly, we restricted variants to single nucleotide variants and excluded all variants with the relatively high variant allele fraction (VAF, the ratio of variant allele : total allele) >50% or <10% (Figure 1c). VAF were subsequently identified which significantly differed from the mean VAF for heterozygous variants (47% in our dataset, Binomial test P < 1 x 10-5) (Figure 1e). We also excluded those variants present more than once in the cohort, and those with a minor allelic frequency (MAF) >0.5% within the ExAC database of Human Exome Variation 13 (Supplementary Material Figure 3).
In order to confirm that detected putative somatic alleles also significantly differed from the base error rate in addition to the mean allelic frequency for a heterozygous variant, we utilized deepSNV 14,15 to compare the nucleotide counts for each putative somatic variant against 328 random samples within the same dataset. Relative read counts were retrieved from the BAM file of each case, and the individual of interest was compared against the variant allele counts for the other 328 individuals using a betabinomial distribution. Variants with a p-value < 0.001 were included as putative somatic variants. This ensured putative somatic alleles passing both thresholds differed from both the observed VAF of heterozygous variants, and from the local base error rate (Figure 1e). All putative somatic variants were confirmed by inspection in Integrative Genomic Viewer 16,17 and were annotated using ANNOVAR 18 (Supplementary Material Figure 2).
Variant validation
Variants remaining after the above filtering strategy were then validated by targeted amplicon sequencing to confirm a somatic variant in cases, together with their absence from controls (VAF <1%). Specific primers spanning putative somatic alleles were designed using NCBIPrimerBLAST (https://www.ncbi.nlm.nih.gov/tools/primer-blast/). Amplicons were generated that spanned the putative somatic variant, and were sequenced in the sample containing the putative somatic allele and in a control case with DNA extracted from the same brain region. PCRs were performed using MyTaq HS polymerase (Bioline, USA), and pooled amplicons were sequenced using MiSeq Reagent Kit v3.0 (Illumina, CA, USA) with paired-end, 150 bp reads. FASTQ files were analysed using in-house bioinformatic pipelines. Reads were aligned to the UCSC hg19 human genome reference using BWA11. Variant calling was performed using GATK’s Haplotype Caller 12 (minimum depth = 500x, minimum supporting reads = 40, base quality ≥ 30 and mapping quality ≥ 20), and variant to reference allelic frequencies manually extracted from BAM files. Subsequently, all validated variants were manually inspected and confirmed in Integrative Genomic Viewer (IGV) 16,17 (Supplementary Material Figure 2).
Five variants from five cases fulfilling the above criteria were also randomly selected for validation by PyroMark® Q24 using standard protocols (Qiagen Inc). Data was analysed using the PyroMark Q24 software for AQ quantitation, with relevant allelic frequencies determined from the sequencing pyrogram. Each sample and control was run in duplicate and the mean of the VAF determined for each allele in each sample and control.
Occurrence of somatic variants at methylated bases
We downloaded genome bisulphite sequencing (WGBS) data from the Inner Cell Mass (ICM) of an early developmental human embryo 19. In total, 476,286,624 of 3,095,693,981 total bases were methylated (15.4%). We subsequently sought to determine whether there was enrichment of somatic mutagenesis at methylated sites by performing a binomial test using 15.4% as the background probability against the proportion of validated variants that occurred at methylated bases.
Mutational spectra and signatures
Mutational spectra were derived directly from the reference and alternative allele at each somatic variant allele. To understand the potential mechanisms of somatic mutagenesis we compared the somatic mutation spectrum and triplet allele (reference allele either side of the somatic allele) against 30 previously defined mutational signatures in cancer 20 and against the mutational signatures to de novo genetic variants derived from trio studies in the population 21.
Variants in the brain proteome
All gene expression data was downloaded from the Human Protein Atlas 22, and each gene containing a somatic variant was annotated according to the expression classification within the brain. Genes were classed as either; (1) Elevated in brain, (2) Expressed in all, (3) Mixed expression pattern, (4) Not detected in brain, (5) Not detected in any tissue as determined by the Human Protein Atlas. Binomial testing was performed in R (v3.3) (http://CRAN.R-project.org/) to determine whether genes containing somatic variants were significantly different from the expression profile of all genes across the human genome within these 5 categories.
Conserved genes
To determine the relative constraint for mis-sense variation within the germline for each gene containing a somatic variant, we annotated each gene with the mis-sense Z score as determined by The Exome Aggregation Consortium (ExAC) 13. Binomial testing was performed to compare the proportion of genes within each quartile of the spectrum of mis-sense constraint as determined by ExAC in R.
Data availability
Clinical, pathological, and genetic data from this study have been submitted to the European Genome-phenome Archive (EGA, https://www.ebi.ac.uk/ega/home) under accession number EGAS00001001599 (password available on request). VCF files and associated and annotated metadata (clinical and neuropathological diagnosis, age of disease onset, and age of death) are available for download through this archive. All requests for data should be made to the Data Access Committee as identified through http://www.mrc.ac.uk/research/facilities/brain-banks/.
Results
Characteristics of variants
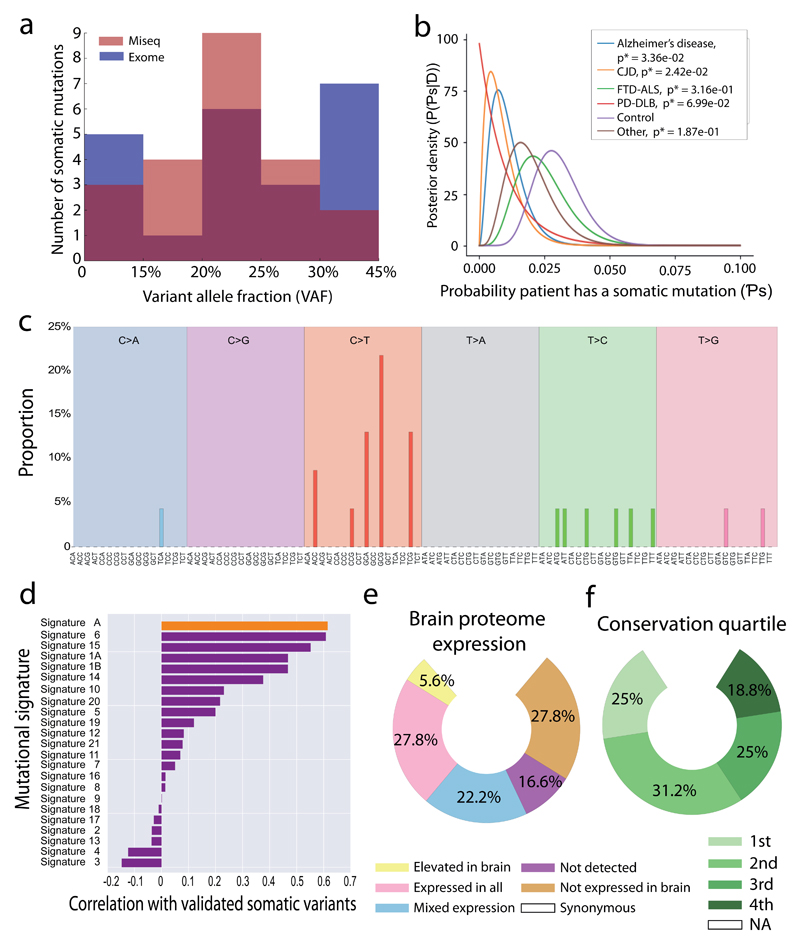
Exome sequencing was performed on 1461 human brain samples from 1099 patients with neurodegenerative diseases and 362 age-matched controls (Figure 1a, b, Supplementary Material Table 1). Mean sequencing depth of WES from 1461 samples was 51.9-fold (SD=12.9), with no significant difference between any disease or controls (one-way ANOVA test P > 0.05) (Supplementary Material Figure 1). Using the described filtration steps we detected 56 somatic variants in 46 brains (3.2% of 1461) (Supplementary Material Table 2). Specific short primer sequences were able to be designed for 40 of the 56 variants using two orthogonal methods (Supplementary Material Figure 2), and confirmed the presence of a somatic variant in 22 (55.0%) of tested alleles; a confirmation rate in keeping with other studies of somatic variation 23 (Figure 2a, Table 1, Supplementary Material Figure 4). The majority of validated variants were transitions (86.4%, n=19) with 23.4% (n=3) transversions. C>T variants were by far the most common (59.1%) 24, and 27.2% (n=6/22) of the validated variants occurred at bases methylated in the inner cell mass 19. In addition, 11 of the 13 C>T mutations (84.6%) were present at CpG sites within the genome. None of the identified somatic variants were seen in the heterozygote state in the 1461 brains, and all were extremely rare in the background population 13. There was also no difference in the frequency of somatic variants between the different disease and control groups (Fisher exact test P > 0.05) (Figure 2b) indicating that, whilst mutational rates may not be increased in patients with neurodegenerative diseases compared to healthy aged individuals, somatic variants at high variant allele frequencies are relatively common in the human brain.
Figure 2. Distribution and mutational profile of the validated somatic variants.
(a) Distribution of allele frequencies for the validated variants in the study are shown, with the relative VAF for each allele as detected on both the MiSeq (pink), Exome sequencing (blue), and overlapping between two platforms (purple) shown. (b) Probability of a variant occurring in each cohort assuming a uniform prior probability and that each person is a Bernoulli trial with probability Ps of developing a mutation. (c) Mutational signature of all validated somatic variants. The mutated allele plus the flanking 3’ and 5’ base are shown. (d) Correlation between the mutational signature of validated somatic variants and the mutational profiles observed in de novo germline variants detected in the population21 (top orange bar – Signature A) and 21 forms of cancer 20 (purple bars). The probable disease associations, or type of cancer in which the signature was detected by Alexandrov (2013) are shown next to the signature number. The Pearson’s correlation coefficient is shown for each signature. (e) Proportion of validated variants within genes grouped by brain proteome expression 22. (f) Proportion of validated variants based on each quartile of the gene conservation scores within the germline (4th quartile being the most conserved in the germ line).
Table 1. Validated somatic variants in 1461 human brains.
| Variant data | Clinical data | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chromosome | Base position | Ref allele | Alt allele | Mutation | Gene | AA change | ExAC | SIFT score | SIFT | Human Proteome Expression | Conservation quartile | Methylated in ICM | Exome VAF | Sample ID | Gender | Brain region | Disease group |
| chr1 | 248224344 | C | T | Non-syn | OR2L3 | p.R121C | 4.94E-05 | 0.02 | D | Not detected | 2 | N | 15.2% | 1 | M | Cerebellum | Control |
| chr7 | 150815676 | C | T | Non-syn | AGAP3 | p.S81L | N/A | 0.02 | D | Expressed in all | 4 | N | 22.3% | 2 | M | Temporal cortex | Control |
| chr11 | 104905100 | T | G | Non-syn | CASP1 | p.K37Q | 4.10E-03 | 0.59 | T | Expressed in all | 2 | N | 16.9% | 3 | M | Cerebellum | Control |
| chr17 | 39502849 | T | G | Non-syn | KRT33A | p.R316S | 1.10E-03 | 0.67 | T | Not expressed brain | 2 | N | 22.1% | 4 | M | Cerebellum | CJD |
| chr3 | 45837911 | T | C | Start lost | SLC6A20 | p.M1V | 8.77E-05 | 0.43 | T | Not expressed brain | 3 | N | 20.3% | 5 | M | Cerebellum | Alzheimer’s disease |
| chr3 | 122629742 | T | C | Non-syn | SEMA5B | p.H59R | N/A | 0.02 | D | Elevated brain | 4 | N | 19.3% | 5 | M | Cerebellum | Alzheimer’s disease |
| chr19 | 36275201 | G | A | Non-syn | ARHGAP3 3 |
p.A517T | N/A | 0.13 | T | Mixed expression | 3 | N | 26.0% | 6 | M | Cerebellum | Other (PSP) |
| chr12 | 6138596 | C | T | Non-syn | VWF | p.R960P | 8.24E-06 | 0.26 | T | Mixed expression | 3 | N | 19.5% | 7 | F | Cerebellum | Control |
| chr11 | 56344581 | G | T | Non-syn | OR5M10 | p.T206N | 1.20E-03 | 1 | T | Not detected | 2 | N | 13.0% | 8 | F | Cerebellum | Other (Epilepsy) |
| chr16 | 4833750 | A | G | Non-syn | SETP12 | p.I131T | 1.68E-05 | 0.01 | D | Not expressed brain | 1 | N | 22.8% | 9 | M | Frontal cortex | Control |
| chr7 | 1535876 | C | T | Non-syn | INTS1 | p.D671N | 8.26E-06 | 0 | D | Expressed in all | 3 | N | 14.7% | 9 | M | Frontal cortex | Control |
| chr8 | 144921555 | T | C | Non-syn | NRBP2 | p.I171V | 3.32E-04 | 0.15 | T | Expressed in all | 2 | N | 30.4% | 9 | M | Frontal cortex | Control |
| chr2 | 85991195 | C | T | Non-syn | ATOH8 | p.R284W | 8.30E-06 | 0 | D | Mixed expression | 4 | Y | 28.3% | 10 | F | Temporal cortex | Control |
| chr1 | 24125194 | G | A | Non-syn | GALE | p.R50W | 1.66E-05 | 0.02 | D | Expressed in all | 2 | Y | 21.7% | 11 | F | Cerebellum | Control |
| chr1 | 17570577 | T | C | Non-syn | PADI1 | p.C126R | N/A | 0.01 | D | Not expressed brain | 1 | N | 25.3% | 12 | M | Cerebellum | Other (Dementia) |
| chr17 | 76499013 | G | A | Syn | DNAH17 | N/A | 4.05E-03 | N/A | N/A | Not expressed brain | N/A | Y | 28.2% | 12 | M | Cerebellum | Other (Dementia) |
| chr11 | 1718844 | T | C | Syn | KRTAP5-6 | N/A | 1.65E-05 | N/A | N/A | Not detected | N/A | N | 14.9% | 13 | F | Cerebellum | FTD-ALS |
| chr19 | 9361855 | G | A | Non-syn | OR7E24 | p.A46T | 2.50E-05 | 0 | D | Not expressed brain | 1 | Y | 30.2% | 13 | F | Cerebellum | FTD-ALS |
| chr20 | 60888258 | G | A | Syn | LAMA5 | N/A | N/A | N/A | N/A | Expressed in all | N/A | N | 23.0% | 13 | F | Cerebellum | FTD-ALS |
| chr16 | 88712548 | G | A | Syn | CYBA | N/A | N/A | N/A | N/A | Expressed in all | 2 | Y | 23.5% | 14 | F | Cerebellum | Control |
| chr22 | 50752254 | G | A | Non-syn | DENND6B | p.R398W | 1.66E-05 | 0 | D | Mixed expression | 1 | Y | 20.2% | 15 | M | Cerebellum | FTD-ALS |
| chr6 | 5004177 | G | A | Syn | RPP40 | N/A | 4.12E-05 | N/A | N/A | Expressed in all | N/A | N | 22.9% | 15 | M | Cerebellum | FTD-ALS |
Variant data shows the chromosome, base position and reference and alternate allele (hg19 build), together with the amino-acid change, frequency in the ExAC population dataset 13, SIFT annotation score and classification 24, expression cohort in the Human Proteome Atlas 21, the quartile of genetic conservation within the human genome 13, presence of methylation at that base in the ICM of an early developmental human embryo18, and the VAF in the WES data. Clinical data for each individual comprising sample ID, gender, brain region and disease group are shown. Abbreviations: CJD, Creutzfeldt Jakob Disease; FTD-ALS, Frontotemporal dementia – Amyotrophic lateral sclerosis; PD-DLB, Parkinson’s disease – Dementia with Lewy Bodies; PSP, Progressive Supranuclear Palsy; Syn, Synonymous; Non-syn, Non-synonymous; D, Deleterious; T, Tolerated; N/A, Not-applicable.
Mutational spectrum and signatures
We further examined the correlation between the observed signature of base mutagenesis with the signature observed in cancer 20, observing the strongest correlation with variants thought to be due to mis-match repair errors occurring during DNA replication and recombination (Pearson’s product moment test r2=0.61, P = 5.02x10-11) (Figure 2c, d). The data were also compared to the mutational profile of de novo germline variants in the population derived from the de-novo db mutation database 21, also revealing a strong association with the mutational profile of de novo variation (Pearson’s product moment test r2=0.62, P = 2.74x10-11) (Figure 2c, d).
Pattern of gene expression and selection pressure
We subsequently determined the tissue expression pattern of each gene in which a somatic variant was observed, and saw that ten (58.8%) of the non-synonymous or start-loss variants were present in genes expressed within the brain. These data are consistent with the notion that the somatic variants were not selected against based on tissue expression, and were equally distributed across the expression profile of the human genome. This raises the possibility that somatic variants contribute to disease pathogenesis in several human tissues, including the brain (Figure 2e, Supplementary Material Table 3). Although speculative, VAF of the observed somatic variants could actually reflect positive selection of some variants, particularly if they arose in later stages of development.
We also found no evidence that the selection pressures seen within the germline also act on the somatic variants we observed in the brain, with non-synonymous somatic variants evenly distributed across conserved and non-conserved regions of the human genome (Binomial test P = NS) (Figure 2f).
Finally, we determined that 58.8% of the non-synonymous or start lost variants (10/17) were predicted to be deleterious by SIFT 25 suggesting that they are highly likely to have detrimental effects on gene expression (Table 1). When taken together, these findings suggest that somatic variants in the brain may not been subject to the same constraints as genetic variation in the germ-line 26, rendering all regions of the brain exome vulnerable to somatic mutagenesis, and therefore potentially conferring the possibility of causing a wide range of neurodegenerative diseases.
Estimates of the mutation rate in human brains
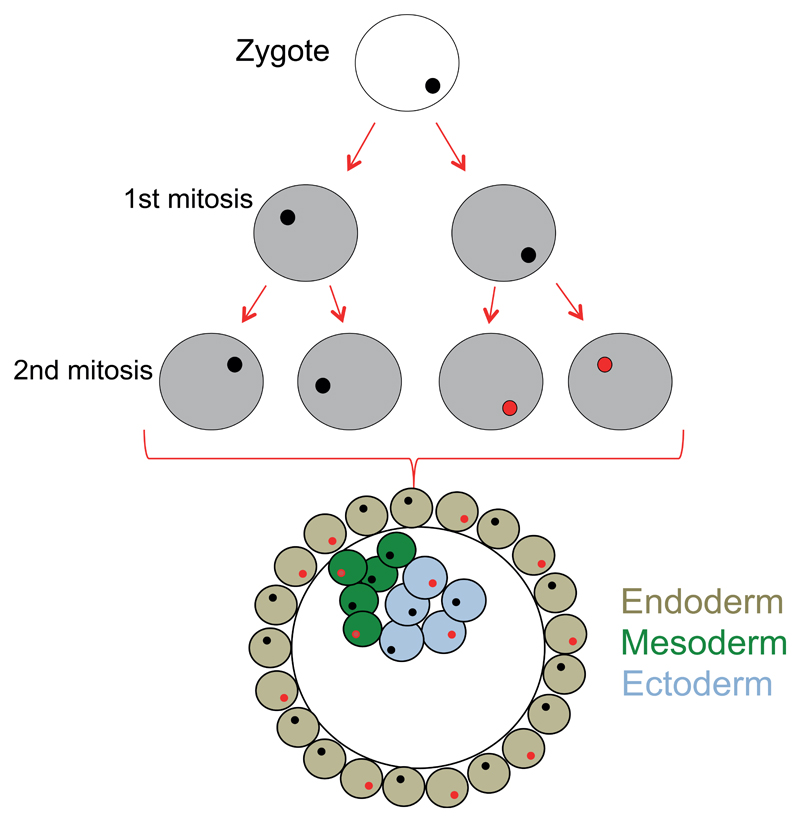
To determine the somatic mutation rate observed within the human brain we first assumed that the variants occurring within the first 2 cell divisions of the human zygote would give rise to VAF of 10-30%, and would likely be present in all human tissues, having arisen before tissue differentiation 27 (Figure 3). In this study, after QC and the removal of structural variation, we analysed 5,906,849 nucleotide bases in each individual brain (see Methods). Across the whole cohort (n=1461 cases), this resulted in the analysis of 8,629,906,389 nucleotide bases which contained 22 validated somatic variants. This equates to a mutation rate of 2.55x10-9. Assuming that the detectable variants occur at either the first or second cell divisions (corresponding in an allelic fraction of 0.25 and 0.125 respectively, and arising from a total of 6 cells; Figure 2a, Figure 3), this results in a minimum somatic mutational rate across the human exome of 4.25x10-10 per base pair per individual in the first two cell divisions of the human zygote. This is slightly lower than previously calculated human somatic mutation rates of 2.67x10-9 26, endorsing the sensitivity of our approach. Finally, assuming 3 billion bases in the full human genome, our data suggest that ~ 1.3 somatic variants across the whole genome will occur during the first 2 cell divisions (3x109 multiplied by 4.25 x 10-10). This is slightly lower than recent estimates using genome sequencing where ~3 variants were estimated to occur per cell per division in very early development 23. This difference could reflect methodological differences such as the particularly conservative nature of our validation algorithm, or be due to a lower mutation rate across the human exome when compared to non-coding regions.
Figure 3. Early cell division after fertilization.
Schematic diagram showing early embryonic development. An example of somatic variant (red) is shown, with the subsequent distribution of this variant within the embryo.
Discussion
These data are the first to quantify the degree of high level (VAF > 10%) somatic mosaicism within the human brain, and show that at least 1% of people possess a somatic protein coding variant within the central nervous system. Given the close correlation between our observed somatic mutation rate and previous estimates, when extrapolated across the whole genome (of 3 billion bases), our data suggests that each human brain may possess at lease ~1.3 high frequency (>10% VAF) somatic variants which have arisen during the first two embryonic cell divisions. When considered alongside the slightly higher mutation rates within the male germline of 1.28x10-8, which confers an average of 76.9 de novo germline variants in each individual 28, then the degree of non-anticipated inherited or acquired genetic variation within an individual can be extensive (~80 alleles). This has important implications in considering the potential genetic aetiology of human neurological diseases.
Whilst the number of validated somatic protein coding variants in our study was small at 22, we saw no evidence of the same selective constraints seen within the germline, which would otherwise limit the number of potentially detrimental germline alleles acquired during development 13. Given the predominance of C>T somatic variants, the observation that 27.2% (n=6/22) of the validated variants occurred at bases methylated in the inner cell mass (Table 1)19 implicates the deamination of methylated cytosines as one potential mechanism, particularly given the enrichment for C>T variants at CpG sites. It was also surprising that there was a relatively strong association with the mutational signatures seen with de novo mutagenesis within the germline 21, suggesting that similar mechanisms of mutagenesis may be involved in the formation of these variants 23, albeit that they do not appear to be selected against in the brain.
A second possibility is that the detected variants were truly focal within the human brain, having arisen during corticogenesis, and subsequent to tissue differentiation during embryogenesis. For example, Poduri et al.,7 detected a focal somatic variant with a VAF of 17% within the brain causing hemimegancephaly which was not present in the patient’s blood. Without additional tissue samples from other organs we cannot exclude this possibility in the cases we studied here. However, the lack of bias for detectable mosiacism in any of the brain regions samples (Cerebellum; 17/22 (Fisher exact test vs other brain regions P = 0.18) (Figure 1a, Table 1), together with the lack of focal morphological abnormalities such as those observed by Poduri et al., point towards an early developmental origin rather than a late focal origin for the variants we report here. However, we do appreciate that we cannot confirm this directly. These problems are likely to be overcome by large scale, higher depth sequencing which will detect lower levels of mosaicism. This will refine the mutation rates and clarify the origin of variants within individuals with neurodegenerative disorders. However, based on the data we report here, mosaicism should also be considered as a potential source of unexpected genetic findings following diagnostic exome and genome sequencing in neurological disorders.
It should be noted that 88% of the DNA samples studied were extracted from the cerebellum, with no enrichment for cerebellar or non-cerebellar extraction sites within any disease group or controls. It will be important to validate these findings in other brain regions. This is particularly relevant for the investigation of neurodegenerative diseases where there is little in the way of cerebellar pathology. Nonetheless, we have demonstrated that at least 1% of human brain samples contain high level somatic variants present in at least 10% cells. Many of these variants were extremely rare in the germline of the population, were highly expressed within the brain, and conferred the ability to markedly alter protein function. Based on the observed mutational signatures, we determine that they are likely to be driven by DNA mis-match repair, and assuming an early developmental origin, are consistent with a somatic mutation rate in the human exome of at least 4.25x10-10 per base pair per individual. Taken together these data determine the frequency, nature and likely origin of high frequency somatic variants in the human brain and show how they have the potential to contribute to a range of neurological disorders.
Supplementary Material
Acknowledgements
This work was funded by the UK Medical Research Council (13044). PFC is a Wellcome Trust Senior Fellow in Clinical Science (101876/Z/13/Z), and a UK NIHR Senior Investigator, who receives support from the Medical Research Council Mitochondrial Biology Unit (MC_UP_1501/2), the Medical Research Council (UK) Centre for Translational Muscle Disease (G0601943), EU FP7 TIRCON, and the National Institute for Health Research (NIHR) Biomedical Research Centre based at Cambridge University Hospitals NHS Foundation Trust and the University of Cambridge. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Footnotes
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- 1.Tsuji S. Genetics of neurodegenerative diseases: insights from high-throughput resequencing. Human molecular genetics. 2010;19(R1):R65–70. doi: 10.1093/hmg/ddq162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Genovese G, Kahler AK, Handsaker RE, et al. Clonal hematopoiesis and blood-cancer risk inferred from blood DNA sequence. N Engl J Med. 2014;371(26):2477–2487. doi: 10.1056/NEJMoa1409405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reya T, Morrison SJ, Clarke MF, Weissman IL. Stem cells, cancer, and cancer stem cells. Nature. 2001;414(6859):105–111. doi: 10.1038/35102167. [DOI] [PubMed] [Google Scholar]
- 4.Tomasetti C, Vogelstein B, Parmigiani G. Half or more of the somatic mutations in cancers of self-renewing tissues originate prior to tumor initiation. Proceedings of the National Academy of Sciences of the United States of America. 2013;110(6):1999–2004. doi: 10.1073/pnas.1221068110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gleeson JG, Minnerath S, Kuzniecky RI, et al. Somatic and germline mosaic mutations in the doublecortin gene are associated with variable phenotypes. American journal of human genetics. 2000;67(3):574–581. doi: 10.1086/303043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee JH, Huynh M, Silhavy JL, et al. De novo somatic mutations in components of the PI3K-AKT3-mTOR pathway cause hemimegalencephaly. Nature genetics. 2012;44(8):941–945. doi: 10.1038/ng.2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poduri A, Evrony GD, Cai X, et al. Somatic activation of AKT3 causes hemispheric developmental brain malformations. Neuron. 2012;74(1):41–48. doi: 10.1016/j.neuron.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sicca F, Kelemen A, Genton P, et al. Mosaic mutations of the LIS1 gene cause subcortical band heterotopia. Neurology. 2003;61(8):1042–1046. doi: 10.1212/wnl.61.8.1042. [DOI] [PubMed] [Google Scholar]
- 9.Lim JS, Kim WI, Kang HC, et al. Brain somatic mutations in MTOR cause focal cortical dysplasia type II leading to intractable epilepsy. Nat Med. 2015;21(4):395–400. doi: 10.1038/nm.3824. [DOI] [PubMed] [Google Scholar]
- 10.Keogh MJ, Wei W, Wilson I, et al. Genetic compendium of 1511 human brains available through the UK Medical Research Council Brain Banks Network Resource. Genome Research. 2017;27(1):165–173. doi: 10.1101/gr.210609.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li H, Durbin R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics. 2009;25(14):1754–1760. doi: 10.1093/bioinformatics/btp324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McKenna A, Hanna M, Banks E, et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 2010;20(9):1297–1303. doi: 10.1101/gr.107524.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lek M, Karczewski KJ, Minikel EV, et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature. 2016;536(7616):285–291. doi: 10.1038/nature19057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gerstung M, Beisel C, Rechsteiner M, et al. Reliable detection of subclonal single-nucleotide variants in tumour cell populations. Nat Commun. 2012;3:811. doi: 10.1038/ncomms1814. [DOI] [PubMed] [Google Scholar]
- 15.Gerstung M, Papaemmanuil E, Campbell PJ. Subclonal variant calling with multiple samples and prior knowledge. Bioinformatics. 2014;30(9):1198–1204. doi: 10.1093/bioinformatics/btt750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Robinson JT, Thorvaldsdottir H, Winckler W, et al. Integrative genomics viewer. Nat Biotechnol. 2011;29(1):24–26. doi: 10.1038/nbt.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thorvaldsdottir H, Robinson JT, Mesirov JP. Integrative Genomics Viewer (IGV): high-performance genomics data visualization and exploration. Brief Bioinform. 2013;14(2):178–192. doi: 10.1093/bib/bbs017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang K, Li M, Hakonarson H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 2010;38(16):e164. doi: 10.1093/nar/gkq603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guo HS, Zhu P, Yan LY, et al. The DNA methylation landscape of human early embryos. Nature. 2014;511(7511):606. doi: 10.1038/nature13544. [DOI] [PubMed] [Google Scholar]
- 20.Alexandrov LB, Nik-Zainal S, Wedge DC, et al. Signatures of mutational processes in human cancer. Nature. 2013;500(7463):415–421. doi: 10.1038/nature12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turner TN, Yi Q, Krumm N, et al. denovo-db: a compendium of human de novo variants. Nucleic Acids Res. 2017;45(D1):D804–D811. doi: 10.1093/nar/gkw865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Uhlen M, Fagerberg L, Hallstrom BM, et al. Proteomics. Tissue-based map of the human proteome. Science. 2015;347(6220) doi: 10.1126/science.1260419. 1260419. [DOI] [PubMed] [Google Scholar]
- 23.Ju YS, Martincorena I, Gerstung M, et al. Somatic mutations reveal asymmetric cellular dynamics in the early human embryo. Nature. 2017;543(7647):714–718. doi: 10.1038/nature21703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ostrow SL, Barshir R, DeGregori J, Yeger-Lotem E, Hershberg R. Cancer evolution is associated with pervasive positive selection on globally expressed genes. PLoS genetics. 2014;10(3):e1004239. doi: 10.1371/journal.pgen.1004239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sim NL, Kumar P, Hu J, Henikoff S, Schneider G, Ng PC. SIFT web server: predicting effects of amino acid substitutions on proteins. Nucleic acids research. 2012;40(Web Server issue):W452–457. doi: 10.1093/nar/gks539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Milholland B, Dong X, Zhang L, Hao XX, Suh Y, Vijg J. Differences between germline and somatic mutation rates in humans and mice. Nat Commun. 2017;8 doi: 10.1038/ncomms15183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yadav VK, DeGregori J, De S. The landscape of somatic mutations in protein coding genes in apparently benign human tissues carries signatures of relaxed purifying selection. Nucleic acids research. 2016;44(5):2075–2084. doi: 10.1093/nar/gkw086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rahbari R, Wuster A, Lindsay SJ, et al. Timing, rates and spectra of human germline mutation. Nature genetics. 2016;48(2):126–133. doi: 10.1038/ng.3469. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Clinical, pathological, and genetic data from this study have been submitted to the European Genome-phenome Archive (EGA, https://www.ebi.ac.uk/ega/home) under accession number EGAS00001001599 (password available on request). VCF files and associated and annotated metadata (clinical and neuropathological diagnosis, age of disease onset, and age of death) are available for download through this archive. All requests for data should be made to the Data Access Committee as identified through http://www.mrc.ac.uk/research/facilities/brain-banks/.