Abstract
Centrally administered glucagon-like peptide-1 (GLP-1) supresses food intake. Here we demonstrate that GLP-1-producing (PPG) neurons in the nucleus tractus solitarii (NTS) are the predominant source of endogenous GLP-1 within the brain. Selective ablation of NTS PPG neurons by viral expression of diphtheria toxin subunit A (DTA) substantially reduced active GLP-1 concentrations in brain and spinal cord. Contrary to expectations, this loss of central GLP-1 had no significant effect on ad libitum feeding of mice, affecting neither daily chow intake nor body weight or glucose tolerance. Only after bigger challenges to homeostasis were PPG neurons necessary for food intake control. PPG-ablated mice increased food intake following a prolonged fast and after a liquid diet preload. Consistent with our ablation data, acute inhibition of hM4Di-expressing PPG neurons did not affect ad libitum feeding, however, it increased post-fast refeeding intake and blocked stress-induced hypophagia. Additionally, chemogenetic PPG neuron activation through hM3Dq caused a strong acute anorectic effect. We conclude that PPG neurons are not involved in primary intake regulation, but form part of a secondary satiation/satiety circuit, activated by both psychogenic stress and large meals. Given their hypophagic capacity, PPG neurons might be an attractive drug target in obesity treatment.
Keywords: GLP-1, Preproglucagon, Food intake, DREADD, hM4Di, DTA, restraint stress, satiation, satiety, GCG neurons
Introduction
Glucagon-like peptide-1 (GLP-1) is found in the CNS, with the highest levels reported in the hypothalamus, a major projection target of preproglucagon (PPG) neurons. PPG neurons are the presumptive main source of endogenous central GLP-1 and are expected to exert effects similar to those of exogenously delivered GLP-1. The most notable of these are reduced food intake and bodyweight loss. PPG neurons are in a prime position to fulfil this role since they innervate all areas identified as mediating GLP-1 effects in the CNS (1–4) and are sensitive to peripheral satiety signals, including gastric distension, leptin, and CCK (5–8). However, doubts have been raised whether PPG neurons are involved in the homeostatic regulation of food intake or whether they signal interoceptive stress and only regulate food intake under pathophysiological conditions (9–13). Three recent studies demonstrated that activation of PPG neurons in vivo using Gq-coupled DREADD or optogenetic stimulation reduces food intake and maintains glucose homeostasis (14–16). Whilst these studies confirmed that PPG neurons have the capacity to modulate food intake and glucose tolerance, they did not address the question of whether PPG neurons play a role in the regulation of appetite or blood glucose under physiological conditions.
Here we use a mouse line expressing Cre-recombinase (Cre) under the control of the glucagon promoter (17) to selectively target NTS PPG neurons. Pharmacogenetic activation, confirmed using in vitro Ca2+ imaging, acutely reduced food intake, replicating previous studies, but failed to have a lasting impact on body weight. Selective ablation of these neurons significantly reduced active GLP-1 concentrations in hypothalamus, brainstem, and spinal cord but did not affect bodyweight or daily food intake. However, PPG-ablated mice ate more chow post-fast than control littermates and were less sensitive to the satiating effects of a liquid diet preload. Similarly, pharmacogenetic inhibition of NTS PPG neurons, confirmed in vitro using patch-clamp electrophysiology, had no effect in ad libitum fed mice, but significantly increased food intake after a long fast and prevented the hypophagic effect of acute restraint stress.
Research Design and Methods
Animal models
Adult male and female Glu-Cre/tdRFP (17), Glu-Cre/GCaMP3 (18; 19), and Glu-YFP (20) mice were group-housed whenever possible on a 12h light/dark cycle with chow and water available ad libitum unless otherwise stated. All experiments were performed in accordance with the U.K. Animals (Scientific Procedures) Act, 1986, with appropriate ethical approval.
Mice were anaesthetised with intramuscular ketamine (50mg/kg) and medetomidine (1mg/kg) or 1.5-2.5% isoflurane and injected with virus (200-250nl, bilaterally; Table 1) using a pressurized glass needle at the following coordinates from the calamus scriptorius: 500μm lateral, 100μm rostral, and 350μm ventral to transduce PPG neurons and were left for at least two weeks before experiments started.
Table 1. Sources of virus and antibody preparations used.
| Virus/Antibody Titer/dilution | Application | Source | References |
|---|---|---|---|
| AAV2-FLEX-hM3Dq:mCherry 6.1x1012 | Activation of Cre-expressing PPG neurons | UNC Vectorcore | pAAV-hSyn-DIO-hM3D(Gq)-mCherry was a gift from Bryan Roth (49) |
| AAV8-FLEX-hM3Dq:mCherry 4x1012 | Activation of Cre-expressing PPG neurons | VVF, ZNZ, Zurich | pAAV-hSyn-DIO-hM3D(Gq)-mCherry was a gift from Bryan Roth (49) |
| AAV8-mCherry-FLEX-DTA 3.3x1012 | Ablation of Cre-expressing PPG neurons | UNC Vectorcore | pAAV-mCherry-flex-dtA was a gift from Naoshige Uchida. |
| AAV2-FLEX-hM4Di:mCherry 6.4x1012 | Inhibition of Cre-expressing PPG neurons | VVF, ZNZ, Zurich | pAAV-hSyn-DIO-hM4D(Gi)-mCherry was a gift from Bryan Roth (49) |
| AAV1/2-FLEX-Perceval Titer not determined | Control for viral transduction | Made in house. | pAAV-FLEX-empty was a gift from Bill Wisden (50) pShuttleCMV-Perceval was a gift from Guy Rutter |
| AAV8-FLEX-EGFP; 8x1012 | Control for viral transduction | VVF, ZNZ, Zurich | pAAV-hSyn-DIO-EGFP was a gift from Bryan Roth |
| PRSx8-AlstR-EGFP-LV 1x1010 | Identification of Phox2b neurons | Sergei Kasparov | (26) |
| Chicken anti-GFP; Alexa488 goat anti- chicken; 1:1000 | GCaMP3, EGFP, YFP | Abcam AB13970; Invitrogen #A-11039 | (18) |
| Rabbit anti-dsRed; Cy3 sheep anti-rabbit; 1:1000 | mCherry, tdRFP | Takara Bio #632496; Sigma #C2306 | |
| Rabbit anti-cFOS 1:500; Alexa488-goat anti-rabbit 1:1000 | cFOS | Merck #ABE457; Invitrogen #A-11008 |
Ca2+ imaging and electrophysiology
Coronal brainstem sections (200μm) were prepared as previously described (18).
Ca2+ imaging was performed in widefield configuration using a 40x water immersion lens (18). Excitation and emission light were filtered at 470±20nm and 515±17nm, respectively (Chroma 59004) and images captured on a CCD camera (Q-click; QImaging). Camera and LED light source were controlled using Micro-Manager (21). Electrical activity of PPG neurons was recorded in cell-attached configuration as described previously (22). Currents were filtered at 1.0kHz and digitised at 3kHz. Recordings were analyzed with WinEDR Software (University of Strathclyde, Glasgow, United Kingdom).
Active GLP-1 assay
Brains were rapidly extracted from the skull and lower brainstem, hypothalamus, cerebellum, olfactory bulbs and spinal cord were isolated, snap frozen and homogenised by pestle and mortar then trituration in 500μl ACSF supplemented with DPP-4 inhibitor (Millipore) through a 29G insulin syringe, before storage for 24hs at -80°C. To generate a crude protein lysate samples were thawed on ice and clarified twice by centrifugation at 500g for 10min and the supernatant collected. The active GLP-1 concentration was determined using a MSD kit (K150JWC-1; Meso Scale Diagnostics, Rockville, Maryland, USA). A Bradford protein assay was performed (Bio-Rad). Absorbance was determined using a Lab Systems Multiscan MS.
Immunohistochemistry
Mice were transcardially perfuse-fixed with 4% PFA, brains sectioned at 30μm and immunostained for GCaMP3, EGFP, YFP, tdRFP, mCherry or cFOS (for details see Table 1) as previously described (18). Sections were incubated overnight at 4°C with primary antibodies in blocking solution followed by fluorophore-conjugated secondary antibody in blocking solution for 2h. Immunofluorescence was visualised on an upright microscope (Leica). Images were captured using a Retiga3000 camera (QImaging). Brightness and contrast were adjusted using Fiji software (23).
cFOS expression in PPG neurons
Mice expressing hM3Dq in NTS PPG neurons were food-restricted for 3h prior to injection of vehicle or clozapine-N-oxide (CNO), which was administered 2mg/kg i.p. in 5ml/kg saline, 30mins before dark onset for all in vivo chemogenetic experiments. Mice were transcardially perfused 90mins after injection, tissue processed and immunostained for cFOS as described above.
Glu-YFP mice were trained to consume Vanilla Ensure. Following three days of stable Ensure intake, mice were randomly allocated into control (n=5) and Ensure-fed groups (n=5) and fasted for 3h. Control mice had no access to chow or Ensure, whereas Ensure-fed mice had access to Vanilla Ensure for 120 mins. At that point mice were transcardially perfused and tissues immunostained for cFOS and YFP.
Glucose Tolerance Test
Mice were placed into new cages, given ad libitum access to water and fasted for 18h. Animals were injected with glucose (1g/kg i.p,, 5ml/kg, Sigma). Blood glucose measurements were repeatedly taken from the tail over two hours and analyzed using a Roche Accu-Chek Glucose Meter.
Feeding paradigms
Intake was measured using standard chow or Vanilla Ensure liquid diet. Mice were weighed daily and habituated to 5ml/kg i.p. saline injection and food intake measurements. On experimental days, food was removed 3h prior to dark onset (except for overnight fast/refeed paradigm) thus standardising the time all mice had their first meal.
Repeated injections of CNO
Using a between-subjects, repeated-measures design, body weight and food intake of control and hM3Dq-expressing mice were measured daily for five days. On the sixth day, twice daily injections of CNO were started.
Normal chow intake
The PPG-ablation study was a between-subjects design, while the activation study (hM3Dq) was a counterbalanced, within-subject design and the acute inhibition study (hM4Di) was a mixed-model design. Mice were transferred to individual cages and food removed 3h or 18h prior to dark onset. Chow was returned at dark onset and intake was measured manually in the following hours.
Ensure preload
This experiment was a between-subjects design. PPG-ablated and control mice were transferred to individual cages and food removed 3h prior to dark onset. Vanilla Ensure was provided for 15 mins at dark onset and intake measured manually, with this protocol repeated for several days until intake was stable (Fig 6C). On test day, chow intake was measured for 1h immediately after Ensure access.
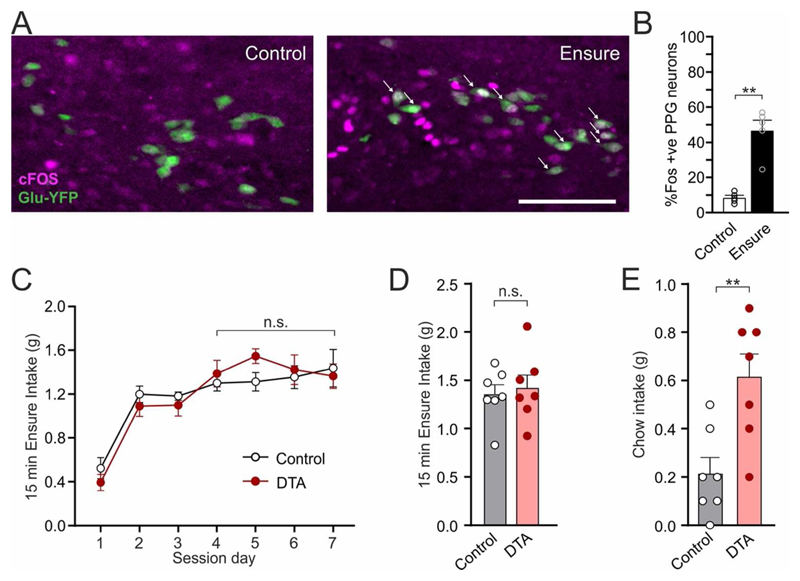
Figure 6. Intake of large volumes of highly palatable diet activates PPG neurons.
(A) Expression of the immediate early gene cFOS (green) in PPG neurons following 30 mins access to Vanilla Ensure or no access to food (Control). White arrows: Representative cFOS-positive PPG neurons. Scale bar: 100 μm. (B) Percentage of PPG neurons expressing cFOS 90 mins after 30 mins access to Vanilla Ensure or no access to food. Data given as mean±SEM, n=3 (Control), n=3 (Ensure). p=0.0079 (Mann-Whitney UTest). (C) Ensure intake during 15-min access at dark onset over several days of habituation in control and PPG-ablated (DTA) mice. Data given as mean±SEM, n=7 (Control), n=7 (DTA). No interaction virus × time (F(3, 36)=0.592, p=0.62) and no significant main effect of virus (F(1, 12)=1.135, p=0.31) or time (F(3, 36)=0.19, p=0.90).). (D) Ensure intake during 15-min access period on the test day in control and PPG-ablated (DTA) mice. Data given as mean±SEM, n=7 (Control), n=7 (DTA). p=0.70 (unpaired t-test). (E) Chow intake of control and PPG-ablated (DTA) mice for one hour following 15-min access to Vanilla Ensure. Data given as mean±SEM, n=7 (Control), n=7 (DTA). p=0.0052 (unpaired t-test). **: p<0.01; n.s.: not significant.
Stress-induced hypophagia
Stress-induced hypophagia was assessed using a mixed-model design. Control (EGFP-expressing) and hM4Di-expressing mice were transferred to individual cages without food 3h prior to dark onset. All mice received CNO 1h before dark onset. Thirty minutes before dark onset, mice were restrained in plastic bags with a breathing hole for 30 mins. At dark onset, they were returned to their cages and chow intake was measured in the following hours.
Statistical analysis
Statistical analysis was performed in GraphPad Prism7.0. Summary data are presented as mean±SEM. Statistical significance was tested using nonparametric tests, t-tests, three-way mixed-model ANOVA, two-way mixed-model or repeated measures ANOVA, and simple main effects as appropriate and as indicated in figure legends.
Results
Pharmacogenetic activation of PPG neurons robustly reduces food intake
To assess the role of PPG neurons in feeding, we first confirmed and extended previous findings that PPG neurons have the capacity to reduce food intake (14; 15). We used transgenic mice expressing Cre under glucagon promotor control (Glu-Cre) and a Cre-dependent reporter (red fluorescent protein (RFP) or the Ca2+ indicator GCaMP3 (18; 19)). GCaMP3-positive cells in this mouse are GLP-1-immunoreactive (19), and as an additional control we crossed this mouse with the Glu-YFP mouse that expresses YFP under glucagon promoter control. YFP-expressing neurons in the NTS of Glu-YFP mice have been shown to express preproglucagon mRNA by single-cell RT-PCR (6). The Glu-YFP/Glu-Cre cross revealed an almost complete overlap of these cell populations; more than 85% of YFP-expressing cells expressed RFP and less than 5% of RFP cells did not express YFP (Fig S1A). Previous reports used a Phox2b transgenic mouse to target PPG neurons, assuming Phox2b is expressed and active in PPG neurons (24; 25). However, targeting the lower brainstem with a lentivirus expressing GFP under the promoter responsive to Phox2b (PRSx8-AlstR-IRES-EGFP-LV; (26)) yielded no co-localisation between GFP and RFP (Fig S1B).
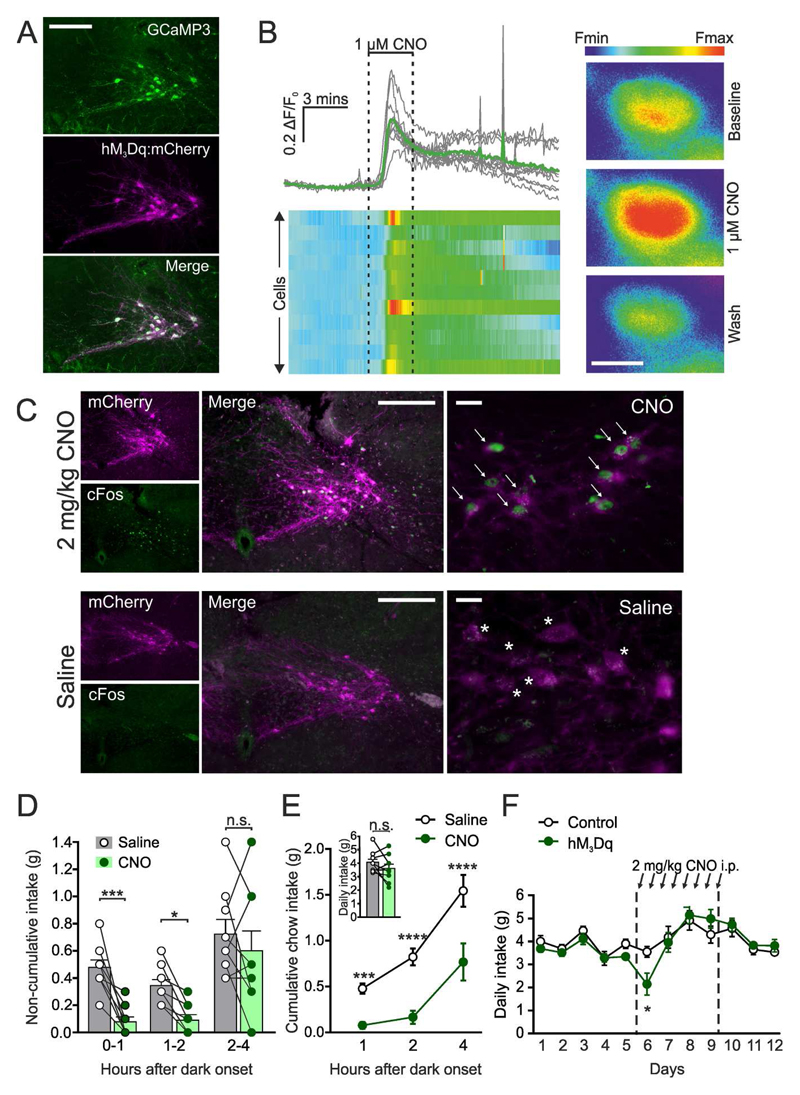
To selectively activate NTS PPG neurons in vivo, the excitatory DREADD hM3Dq was expressed by stereotaxic injection of AAV2-FLEX-hM3Dq:mcherry into Glu-Cre mice (Fig 1A). Activation of hM3Dq with CNO substantially increased [Ca2+]i in brainstem slices (Fig 1B). Similarly, in awake mice, CNO injection elicited cFOS immunoreactivity in PPG neurons (Fig 1C).
Figure 1. Pharmacogenetic activation of PPG neurons robustly reduces food intake.
(A) Expression of hM3Dq:mCherry (magenta) in PPG neurons (detected with an anti-GFP antibody, green) three weeks after stereotaxic injection of AAV2-hM3Dq:mCherry into the NTS of Glu-Cre/GCaMP3 mice. Scale bar: 100 μm. (B) Increase in [Ca2+]i in GCaMP3-expressing PPG neurons in response to superfusion of ex vivo brainstem slices with 1 μM CNO. Data are displayed as traces (top panel) and a heat map (bottom panel) representing the fractional change in fluorescence from baseline. Right panel: Representative pseudocoloured cell responding to 1 μM CNO with an increase in [Ca2+]i. Scale: 10 μm, n=11 cells. (C) Expression of the immediate early gene cFOS (green) in PPG neurons expressing hM3Dq:mCherry (magenta) following i.p. injection of 2 mg/kg CNO (top panels) or saline (bottom panels). White arrows: Representative cFOS-positive hM3Dq-expressing cells. White stars: Representative cFOS-negative hM3Dq-positive cells. Scale bars: 100 μm (middle panel) and 20 μm (right panel). (D-E) Non-cumulative (D) and cumulative (E) food intake in the first four hours of dark phase following injection of CNO (2 mg/kg i.p.) or saline. CNO was delivered 30 mins prior to dark onset. Data given as mean±SEM, n=9 mice. D: No significant time × drug interaction (F(2, 16) = 2.897, p=0.0844), but a significant main effect of drug treatment (F(1,8)=17.31, p=0.0032); E: Significant time × drug interaction (F(2,16)=5.626, p=0.0141). 1h p=0.0005, 2h p<0.0001, 4h p<0.0001 (Sidak’s multiple comparisons test). Inset: p=0.20 (paired t-test). (F) Daily chow intake in hM3Dq-expressing (n=7) and control (n=6) Glu-Cre mice in response to twice daily i.p. injection of 2 mg/kg CNO (indicated with black arrows). Significant time × virus interaction (F(11, 121) = 2.06, p=0.0283); day 6 p=0.0119 (Sidak’s multiple comparisons test). Data given as mean±SEM. *p<0.05, ***p<0.001, ****p<0.0001.
Having confirmed that CNO activates PPG neurons both in vitro and in vivo, we explored whether in vivo activation suppresses feeding. First, we confirmed that viral over-expression of hM3Dq in PPG neurons had no intrinsic effect on food intake, nor did administration of CNO in mice transduced with a control virus (Fig S2). Subsequently, ad libitum dark onset food intake was measured in mice expressing hM3Dq in NTS PPG neurons in a counterbalanced cross-over design. CNO-injected mice consumed substantially less chow than when injected with saline in both the first and second hour (Fig 1D) and cumulative intake was suppressed over the first four hours after dark onset (Fig 1E). The effect of CNO disappeared over 21h with cumulative daily intake unaffected by PPG activation (Fig 1E).
To determine whether this was simply due to washout of CNO, we injected another cohort of hM3Dq-expressing and control mice with CNO every 12 hours (at dark and light onset) for four days. Twice-daily PPG activation initially suppressed feeding, with significantly lower 24h intake following the first injections, however intake suppression was not sustained (Fig 1F).
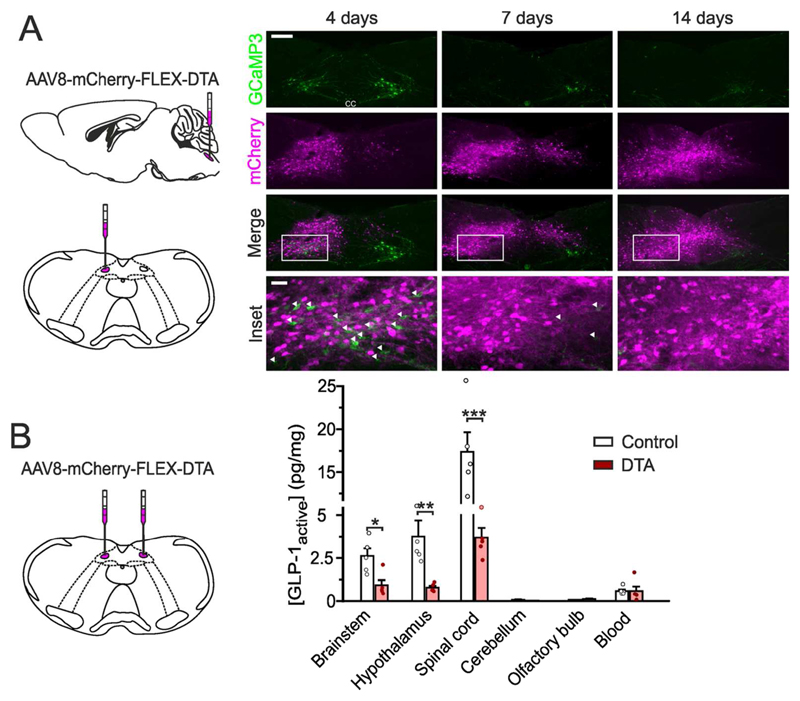
NTS PPG neurons are the main source of GLP-1 in brain
Whilst the above results demonstrate the capacity of PPG neurons to reduce feeding, they do not prove that brain GLP-1 is derived from these neurons. To address this, we used an AAV Cre-dependently encoding diphtheria toxin subunit A (DTA). Unilateral targeting of the NTS in Glu-Cre mice with AAV8-mCherry-FLEX-DTA selectively ablated PPG neurons, with complete disappearance of cell bodies within 14 days, whilst contralateral PPG neurons remained intact (Fig 2A). Bilateral ablation of NTS PPG neurons dramatically reduced active GLP-1 levels in brainstem, hypothalamus, and spinal cord (Fig. 2B), demonstrating that NTS PPG neurons are the main source of GLP-1 in these areas.
Figure 2. NTS PPG neurons are the main source of brain GLP-1.
(A) Expression of mCherry and GCaMP3 (as a marker for PPG neurons) four, seven, and 14 days after unilateral stereotaxic injection of AAV8-mCherry-FLEX-DTA into the NTS of a Glu-Cre/GCaMP3 mouse (schematic on left). White arrows indicate GCaMP3-positive PPG neurons remaining. Scale bars: 100 μm (top panels) and 20 μm (inset).
(B) Protein levels of active GLP-1 (normalised to total protein) detected in several brain regions after bilateral stereotaxic injection of AAV8-mCherry-FLEX-DTA or a control virus (AAV1/2-FLEX-Perceval). Brainstem: p=0.0317, Hypothalamus: p=0.0079, (Mann-Whitney U Test); Spinal cord: p=0.0004 (unpaired t-test). Data given as mean±SEM, n=5 in each group. *p<0.05, **p<0.01, ***p<0.001.
Active GLP-1 concentrations in brainstem, hypothalamus, and spinal cord were 4-fold, 6-fold, and 29-fold larger, respectively, than those from concurrent systemic blood samples, indicating that blood contained within the brain samples was not the source of the GLP-1. Consistent with this, amounts of active GLP-1 in cerebellum, which does not receive projections from PPG neurons (3), were negligible, and neither blood nor cerebellar concentrations were affected by PPG neuron ablation. Similarly, the GLP-1 concentration in the olfactory bulb, a confirmed location of additional PPG neurons (27; 28), was very low and not affected by DTA ablation in the brainstem.
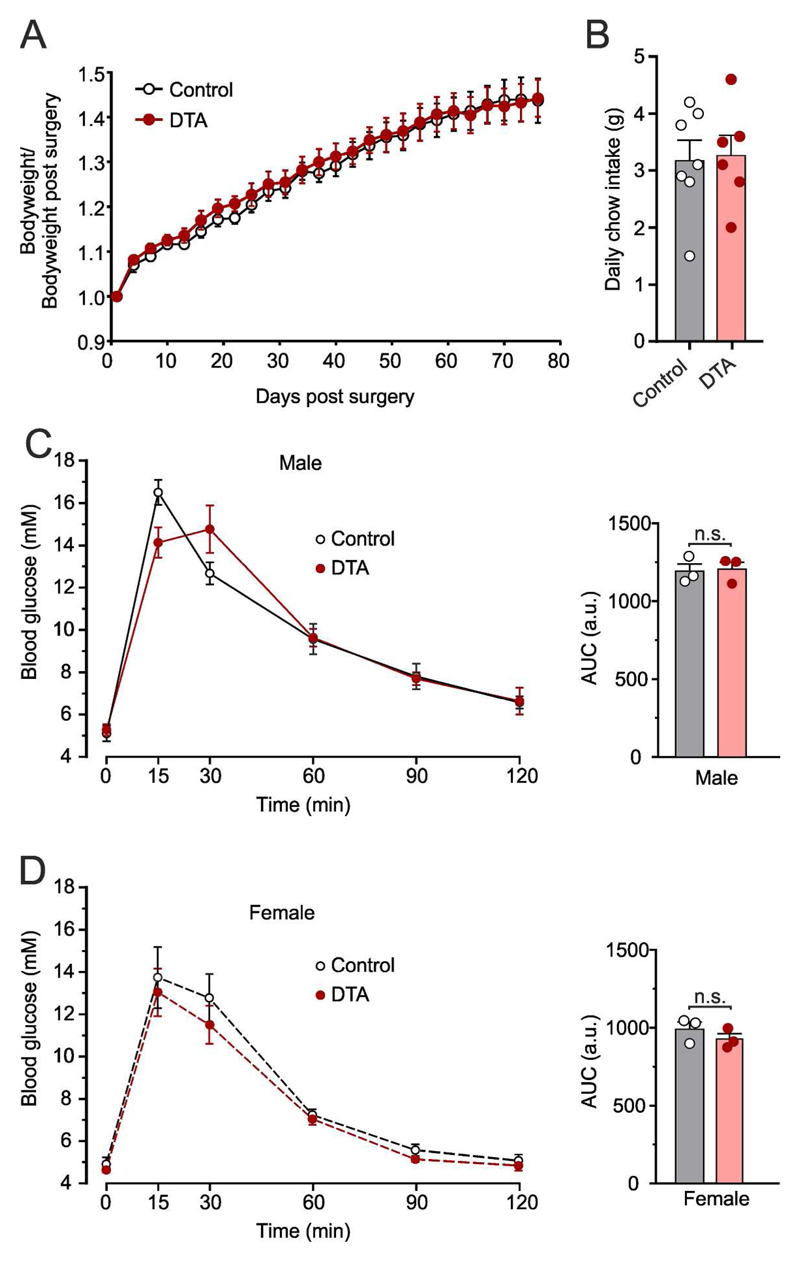
Ablation of NTS PPG neurons does not impact bodyweight, daily food intake, or glucose tolerance
Although activation of PPG neurons robustly suppressed short-term feeding, sufficiency does not prove necessity. We therefore explored physiological conditions under which PPG neurons might regulate food intake. Bodyweight and daily food intake were recorded over two months in Glu-Cre mice injected bilaterally with AAV8-mCherry-FLEX-DTA or AAV1/2-FLEX-Perceval as control. Ablation of NTS PPG neurons did not affect bodyweight (Fig 3A) or daily food intake when fed ad libitum (Fig. 3B), suggesting no significant impact on long-term energy balance under these conditions.
Figure 3. Ablation of NTS PPG neurons has no impact on body weight, food intake, or glucose tolerance.
(A-B) Bodyweight change (A) and daily chow intake (B) following stereotaxic injection of AAV8-mCherry-FLEX-DTA or control virus. Bodyweight was measured every 2-3 days over two months. Mean±SEM, n=7 (control), n=6 (DTA). A: No significant time × virus interaction (F(1, 12)=0.08578, p=0.7746) and no significant main effect of virus (F(1, 12)=0.08578, p=0.7746); B: p=0.45 (unpaired t-test). (C-D) Blood glucose in response to an i.p. injection of glucose (1 g/kg) at t=0 seven weeks after stereotaxic injection of DTA or control virus in six male (C) and six female (D) Glu-Cre mice. Area under the curve (AUC) of the i.p. glucose tolerance test for each group is given on the right of each graph. Data given as mean±SEM. Glucose concentrations: There was a significant time × virus interaction for males (F(5, 20)=3.83, p=0.014), but no significant difference between DTA and control mice at any timepoint. There was no significant time × virus interaction for females (F(5, 20)=0.19, p=0.96) and no significant main effect of virus (F(1, 4)=1.08, p=0.36). AUC: No effect of virus for males (p>0.99, Mann-Whitney U test) or females (p=0.34, unpaired t-test).
PPG neurons were recently shown to be sufficient to improve glucose tolerance (16). We therefore investigated whether NTS PPG ablation affects the response to an intraperitoneal glucose load (Fig 3C,D). Before ablation, there was no difference in glucose tolerance, with males having poorer glucose tolerance than females (Fig S3). Seven weeks after PPG ablation, sex differences were still evident, but loss of NTS PPG neurons did not affect glucose tolerance (Fig 3C,D).
Ad libitum food intake is unaffected by ablation or acute inhibition of NTS PPG neurons
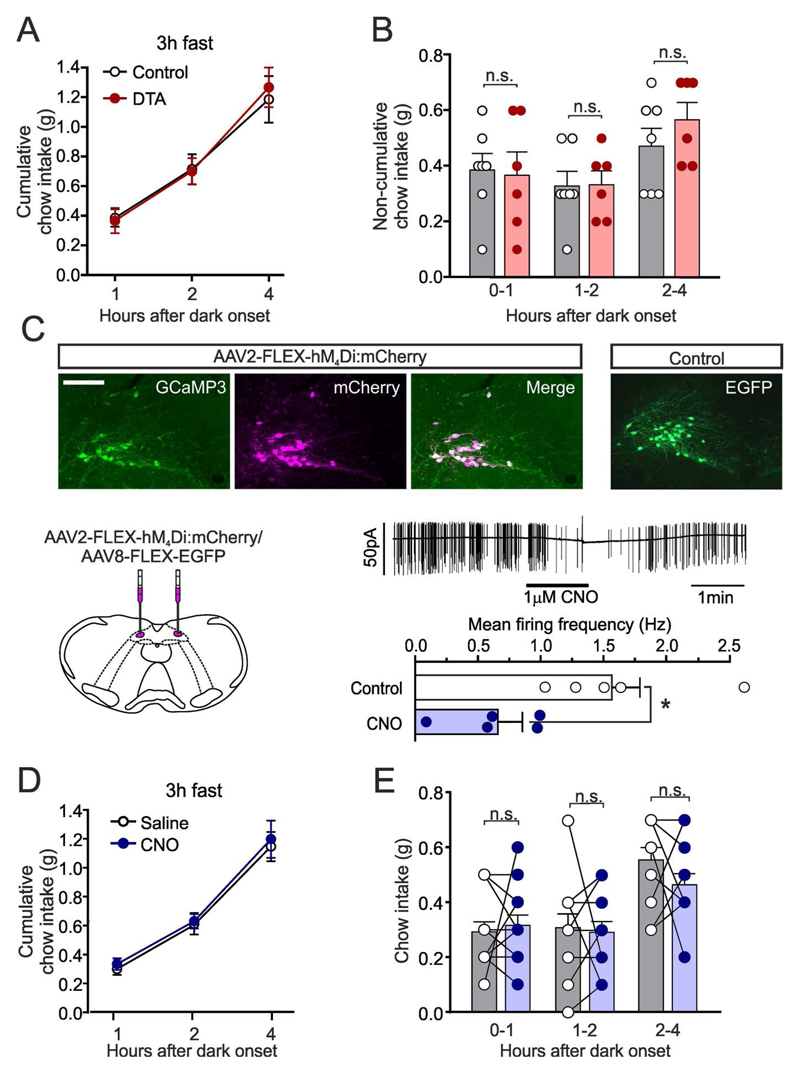
Having found no evidence that NTS PPG neurons regulate long-term energy balance, we next asked whether PPG neurons are necessary for short-term regulation of feeding. PPG ablation had no effect on cumulative (Fig 4A) or non-cumulative chow intake (Fig 4B) over 4h after dark onset, suggesting that although activation of PPG neurons is sufficient to reduce food intake, they are not necessary to regulate ad libitum feeding.
Figure 4. Ad libitum food intake is unaffected by ablation or acute inhibition of NTS PPG neurons.
(A-B) Cumulative (A) and non-cumulative (B) food intake of control and PPG-ablated (DTA) mice in the first four hours of the dark phase. Data given as mean±SEM, n=7 (control), n=6 (DTA). n.s.: not significant. A: No significant time × virus interaction (F(2, 22)=0.5406, p=0.5900) and no significant main effect of virus (F(1, 11)=0.012, p=0.91); B: No significant time × virus interaction (F(2, 22)=0.834, p=0.4476) and no significant main effect of virus (F(1, 11)=0.1472, p=0.7085). (C) Cre-dependent expression of hM4Di and EGFP as control in the NTS of Glu-Cre/GCaMP3 mice. Bottom left: Schematic of bilateral injections. Bottom right: Representative voltage-clamp recording (top) and summary data (bottom) of hM4Di-expressing PPG neurons in ex vivo slice preparation superfused with CNO (1 μM). Data given as mean±SEM, n=5. *p<0.05 (paired t-test).
(D-E) Cumulative (D) and non-cumulative (E) food intake of hM4Di-expressing mice injected with saline or CNO (2 mg/kg, i.p., 30 mins prior to dark onset) in the first four hours of the dark phase. Data given as mean±SEM, n=12. D: No significant main effect of virus (F(1,21)=1.19, p=0.29) or drug (F(1,21)=0.002, p=0.96); E: No significant main effect of virus (F(1,20)=0.11, p=0.75) or drug (F(1,20)=0.045, p=0.83). Data from mice expressing control virus (Fig S4) included in analysis. n.s.: not significant.
Although ablations were inflicted in adult mice, compensatory responses could account for the lack of effect on long-term energy balance. We therefore assessed the effect of acute inhibition of PPG neurons using the inhibitory DREADD hM4Di.
To assess whether hM4Di stimulation inhibits PPG neurons in vitro, virally transduced PPG neurons were identified by mCherry fluorescence in brainstem slices and electrical activity recorded in the cell-attached configuration. PPG neurons were spontaneously firing at 1.57±0.22 Hz, consistent with previous observations (6; 18). CNO superfusion reduced firing frequency to 0.66±0.20Hz (Fig 4C).
hM4Di expression did not affect bodyweight or food intake in the absence of CNO (Fig S4) and daily food intake was unaffected after a single dose of CNO at dark onset (Fig S4C). As with ablation, acute inhibition of PPG neurons did not affect dark onset feeding (Fig 4D,E). The data from both ablation and acute inhibition therefore suggest PPG neurons are not necessary for the regulation of long-term or short-term food intake in ad libitum fed mice.
PPG neurons limit fasting-induced refeeding
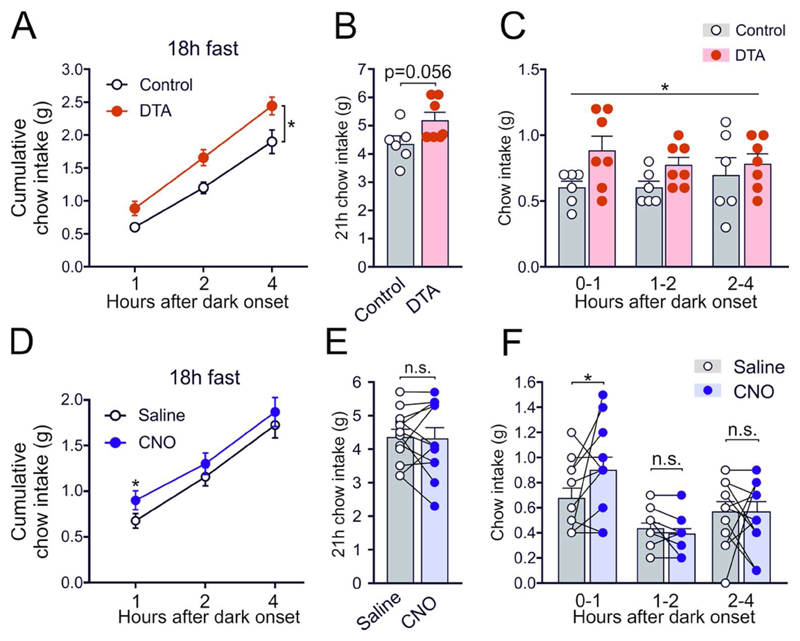
Having found no major role of NTS PPG neurons in ad libitum feeding, we next investigated whether PPG neurons need abnormally large meals to become engaged as suggested for rats (9; 10). To encourage significant refeeding, we fasted mice for 18h prior to intake measurements from dark onset. Control animals ate 0.6±0.05g chow in the first hour compared to 0.4±0.06g when food-restricted only briefly (Fig 5C and Fig 4A, respectively), whilst PPG-ablated animals ate 0.9±0.11g (Fig 5C). This elevated post-fast chow intake was evident over 4h (Fig 5A), but did not last overnight, although there was a trend towards increased intake (Fig 5B).
Figure 5. Ablation or acute inhibition of PPG neurons increases food intake only after a large meal.
(A-C) Cumulative (A-B) and non-cumulative (C) food intake of control and PPG-ablated mice in the first four hours (A,C) and 21 hours (B) after onset of the dark phase following 18 hours of food-deprivation prior to the onset of dark. Data given as mean±SEM, n=7 (control), n=6 (DTA). A: No significant virus × time interaction (F(2, 22) = 1.81, p=0.19), but a significant main effect of virus (F(1,11)=8.0, p=0.016); B: p=0.056 (unpaired t-test); C: No significant virus × time interaction (F(2, 22)=0.75, p=0.49), but a significant main effect of virus (F(1,11)=6.1, p=0.031).
(D-F) Cumulative (D-E) and non-cumulative (F) food intake of hM4Di-expressing mice injected with saline or CNO (2 mg/kg, i.p., 30 mins prior to dark onset) in the first four hours of the dark phase following 18 hours of food-deprivation prior to the onset of dark. Data given as mean±SEM, n=12. D: There was a significant virus × drug interaction at hour 1 (F(1, 21)=4.733, p=0.0411), p=0.038 (CNO vs Saline, Sidak’s multiple comparisons test); E: No significant virus × drug interaction (F(1, 21)=1.245, p=0.28) and no significant main effect of drug (F(1, 21)=1.67, p=0.21) or virus (F(1, 21)=0.084, p=0.77); F: There was a significant virus × drug interaction at hour 1 (F(1, 21)=4.733, p=0.0411), p=0.038 (CNO vs Saline, Sidak’s multiple comparisons test). Data from mice expressing control virus included in analysis. *: p<0.05, n.s.: not significant.
Similarly, CNO-injected hM4Di-expressing mice ate 0.23±0.1g more chow in the first hour of refeeding compared to when injected with saline (Fig 5F). This hypophagic effect was not sustained beyond 1h (Fig 5D) and there was no impact on 21h chow intake (Fig 5E).
PPG neurons limit chow intake following a liquid diet preload
Results from these two independent, complementary experiments suggest that PPG neurons may be recruited following unusually large intakes to limit subsequent feeding. To further investigate this hypothesis, we encouraged high intakes by provision of a highly-palatable liquid diet (Vanilla Ensure). Mice were habituated to dark onset Ensure access for eight days, during which 30min intake stabilised at 1.7±0.1g from day four. On day nine mice were randomly allocated to Ensure or fasted groups and subsequent analysis of cFOS immunoreactivity revealed that 45% of PPG neurons were activated following Ensure intake, compared to 10% activation in fasted controls (Fig 6A,B).
To determine whether ablation of PPG neurons affects feeding under these conditions, mice were habituated to consume a 15min Ensure preload at dark onset which stabilised at 1.4±0.04g after four sessions (Fig 6C). Ensure intake between PPG-ablated and control mice did not differ at the beginning (Fig 6C) or end (Fig 6D) of the habituation. Following the final Ensure session, chow intake was lower in the control group than usually seen 1h into dark phase, with control mice eating roughly half their normal intake (Fig 6E, 0.21±0.06g vs 0.4±0.06g in Fig 4B). In contrast, PPG-ablated mice ate significantly more than control mice, with 0.61±0.1g of chow eaten 1h after Ensure preload (Fig 6E). These data support the hypothesis that unusually large intakes recruit NTS PPG neurons to limit subsequent feeding.
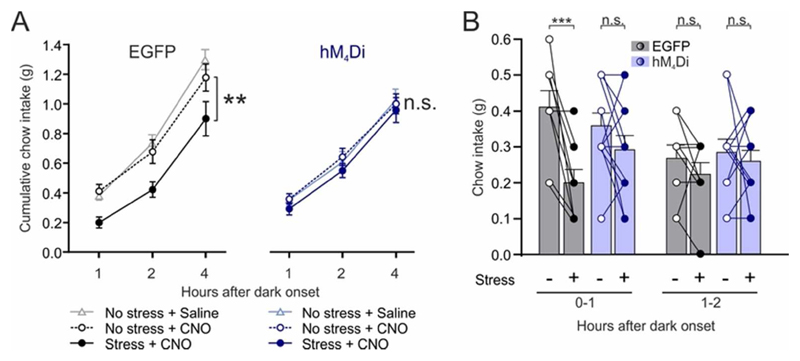
Stress-induced hypophagia requires PPG neurons
We next explored whether there are other conditions under which PPG neurons are necessary for anorectic effects. Previous work suggests that central GLP-1 contributes to the intake suppression following acute stress in rats (29). To investigate whether PPG neurons contribute to the hypophagic response to restraint stress, we acutely inhibited PPG neurons in vivo by activating the hM4Di receptor. Control and PPG-inhibited mice were exposed to 30mins restraint stress and subsequent food intake was measured. Restraint stress significantly suppressed cumulative feeding over 4h in control mice, whereas PPG-inhibited mice displayed no stress-induced hypophagia (Fig 7A). In the absence of stress, CNO had no effect on food intake in both control and PPG-inhibited mice as compared to vehicle (Fig 7A). Stress-induced hypophagia was seen in the first hour (Fig 7B), during which intake in control mice was reduced by 50±8%, whereas intake was unaffected by stress in the PPG-inhibited group. There was no clear suppression of chow intake in hour 2. These data demonstrate that PPG neurons are required for the hypophagic response to acute restraint stress.
Figure 7. Stress-induced hypophagia requires PPG neurons.
(A-B) Cumulative (A) and non-cumulative (B) chow intake of mice expressing EGFP or hM4Di injected with 2 mg/kg CNO i.p. 60 mins prior to dark onset and left undisturbed or exposed to 30 mins restraint stress 30 mins prior to dark onset. Also included in (A) is data from the same EGFP- and hM4Di-expressing mice injected with saline and left undisturbed. Data given as mean±SEM, n=9 (Control), n=12 (hM4Di). A: Significant main effect of stress for control (F(1, 8)=14.14, p=0.0055), but not hM4Di: (F(1, 11)=0.8684, p=0.37). No effect of CNO on food intake in both control (p=0.5) and PPG-inhibited mice (p=0.98) as compared to saline vehicle in the absence of stress. B: Hour 0-1: Significant effect of stress in the EGFP group (p=0.0008), but not in the hM4Di group (p=0.25) (Sidak’s multiple comparisons test). Hour 1-2: No significant virus × stress interaction (F(1, 19)=0.091, p=0.77) and no main effect of virus (F(1, 19)=0.49, p=0.49) or stress (F(1, 19)=1.16, p=0.29). **: p<0.01; ***: p<0.001; n.s.: not significant.
Discussion
We demonstrate here that NTS PPG neurons are the main source of brain GLP-1. Active GLP-1 was reduced by >60% in brainstem, and almost 80% in hypothalamus and spinal cord following ablation of NTS PPG neurons. In contrast, circulating GLP-1 levels, which were substantially lower than in brain, were unaffected by ablation and levels in cerebellum, which receives no projections from PPG neurons (3), were negligible, and likely reflect only the vascular supply throughout the brain. Remaining GLP-1 levels in the sampled CNS regions after ablation likely reflect the IRT and ventral midline PPG cells, which were left intact in our study. These neurons make up 44% (29) and 32% (1) of all PPG neurons in the brainstem in rat and mouse, respectively. Outside the brainstem, small populations of PPG neurons have been described in olfactory bulb (27; 28), piriform cortex (3), and lumbar-sacral spinal cord (1). Of these, the olfactory bulb neurons project only locally (28), and the spinal neurons do not project to the brain (1), excluding these populations as the source of remaining GLP-1 after ablation of NTS PPG neurons. Approximately 50% of PPG neurons have axons projecting to the autonomic control areas of the spinal cord (1). The current study adds to the significance of these projections by demonstrating a high GLP-1 content in spinal cord, the majority of which is supplied by NTS PPG neurons. This suggests a significant physiological role for spinal GLP-1 release, an intriguing path for future research considering the role of GLP-1 in sympathetic outflow (30–33).
In addition to providing unequivocal evidence that PPG neurons are the main source of brain GLP-1, these results validate that our genetic approach targets the cells that provide GLP-1 in the CNS. In contrast, injection of a lentivirus that expresses GFP in Phox2b-expressing cells (PRSx8-AlstR-EGFP-LV; (26)), failed to show any co-localisation with Cre-expressing PPG neurons, indicating that the transcription factor Phox2b is not expressed in adult PPG neurons. Transgenic mice expressing Cre under the control of Phox2b have been used previously to target PPG neurons (24; 25). Whilst our results do not exclude the possibility that PPG neurons express Phox2b during development, they clearly show that using adult Phox2b-Cre mice combined with Cre-dependent viruses is not a valid approach to target PPG neurons. This substantiates previous concerns about that approach (34; 35).
Recent studies have pharmacogenetically and optogenetically activated PPG neurons, using a mouse model produced independently from ours but using an equivalent strategy (14–16). Based on those results and our observations, NTS PPG neurons are sufficient to suppress feeding in mice. Here we also demonstrate that repeated, twice daily chemogenetic activation of NTS PPG neurons leads to a transient decrease in food intake reminiscent of results reported for both CCK- and DBH-expressing NTS neurons (36). In both cases there was a strong short-term reduction in intake, but either no effect (CCK cells) or only a small effect (DBH cells) on 24h food intake. A similar lack of long-term effects has been observed with ICV GLP-1 infusions in rat (37) and it seems likely that compensatory mechanisms are activated to maintain energy balance and avoid excessive weight loss, although we cannot exclude that continued activation downregulates DREADD receptors.
Gaykema et al. (14) argued that chemogenetic activation using hM3Dq is comparable to activation by physiological stimuli, such as leptin and CCK. However, with <50% of PPG neurons activated, our cFOS-expression study demonstrated that even a large volume of Ensure did not activate PPG neurons to the same degree as hM3Dq-activation (98%; (14)). Similarly, acute stress in rats activated ~74% of GLP-1-producing neurons (29), suggesting that chemogenetic activation of PPG neurons is a supraphysiological stimulus.
Prompted by these limitations we attempted to determine the physiological role of PPG neurons in food intake. Although Liu et al. (15) did address the role of endogenous GLP-1 in food intake by optogenetically inhibiting NTSPPG→PVN projections, the specific physiological conditions under which PPG neurons influence food intake were not investigated. Whilst chemogenetic activation strongly suppressed feeding, ablation of NTS PPG neurons had no effect on 24h intake or bodyweight in mice with ad libitum access to food. Not only was long-term energy balance unaltered by loss of NTS PPG neurons, neither ablation nor acute inhibition affected dark onset food intake when mice were fed ad libitum. Similarly, Liu et al. failed to observe persistent increases in food intake over 7 daily injections of 0.3mg/kg CNO (15), although this dose schedule may not provide lasting inhibition of the PPG neurons (38). This suggests that PPG neurons do not produce an obligatory meal termination signal required for normal satiation, a conclusion supported by both experimental approaches used here. Loss of NTS PPG neurons also failed to affect glucose tolerance, consistent with previous reports that central GLP-1R are not necessary for glucose control in mouse (39). However, both ablation and acute inactivation left a proportion of PPG neurons, in the IRT, intact. It is conceivable that only a small fraction of PPG neurons is needed to maintain satiation and that complete loss of PPG neurons could reveal a role in ad libitum feeding. This reliance on a few neurons only was demonstrated for orexin neurons, where >90% loss was necessary to reveal the cataplexy phenotype (40). Whilst this is difficult to categorically exclude, our results suggest that PPG neurons are not normally recruited in response to ad libitum feeding, but point to a role for PPG neurons in suppressing food intake in response to stronger physiological stimuli, such as a large meal or acute stress. In support, global and central knockdown of GLP-1R has little impact on food intake and body weight in mice (39; 41).
In contrast, studies in rat have provided some evidence for a role of endogenous GLP-1 in the control of normal feeding and glucose control (35; 42; 43). Infusion of exendin-9 into the ventricular system or knockdown of GLP-1 receptors in discrete nuclei increase food intake and shRNA-mediated knockdown of PPG in the brainstem led to increased bodyweight gain and hyperphagia (35; 44). It is unclear if these different observations reflect species differences and, in that case, which rodent species is the best model of human physiology (35; 45).
Several studies in rat support the idea that GLP-1-producing neurons are mainly recruited following intake of a large meal. An unusually large meal is required to activate GLP-1-producing neurons in the NTS (10), gastric distension activates GLP-1 neurons (7), and the ensuing decrease in food intake is mediated by central GLP-1 signalling (46). In support of these findings, we demonstrate here that NTS PPG neurons are necessary for satiation/satiety following intake of a large meal, either encouraged by food-depriving mice for 18 hours or by providing them with access to a highly palatable diet. Seemingly contradictory findings by previous studies in rat suggest that GLP-1 neurons are inhibited by negative energy balance following an overnight fast, rendering them less sensitive to stimulation with CCK or acute stress (29; 47). However, we demonstrate here that a large meal following food deprivation is sufficient to recruit NTS PPG neurons to limit overeating as was previously suggested in rat (10).
In addition to playing a role in satiation/satiety following a large meal, we found that hypophagia induced by acute restraint stress was dependent on PPG neuron activity. In support of a role for central GLP-1 in stress regulation, central infusion of GLP-1 increases plasma ACTH and corticosterone levels and elicits anxiety-like behaviour in rats (48). Conversely, 3rd ventricular exendin-9 attenuated the rise in corticosterone after psychogenic stress, demonstrating HPA axis activation by exogenous as well as endogenous GLP-1. However, chemogenetic activation of PPG neurons in mouse did not affect stress hormone levels or anxiety-related behaviour (14), suggesting the restraint stress-induced hypophagia investigated in our study may not involve activation of the HPA axis, but employs different pathways. In ad libitum fed rats, restraint stress induces cFOS-expression in GLP-1-immunoreactive neurons and restraint stress-induced hypophagia can be reversed by lateral ventricular exendin-9 (29). Those findings are in line with the effects of direct inhibition of PPG neurons that we report here and suggest that these neurons play a central role in restraint stress-induced hypophagia in both mouse and rat. This places PPG neurons at the centre of behavioural decisions to maintain energy intake vs avoiding danger and stress.
Conclusions
We report that NTS PPG neurons of the lower brainstem are the main source of the GLP-1 found in the CNS, that these neurons have the capacity to significantly suppress food intake, and describe conditions under which they are necessary for the control of feeding. Our results suggest that PPG neurons may not control ad libitum food intake but are essential for short term limitation of feeding following unusually large intakes, and in mediating stress-induced hypophagia. We thus conclude that PPG neurons likely form part of a secondary satiation/satiety circuit, activated by both psychogenic stress and presumptive gastric distension from unusually large intake. PPG neurons thus constitute a regulator with scope for substantial hypophagia, without being involved in day-to-day energy balance, and as such they may be an attractive target for pharmaceutical intervention to reduce body weight.
Supplementary Material
Acknowledgments
This study was supported by grants MR/J013293/2 and MR/N02589X/1 from the MRC and BHF grant FS/14/43/30960 (PhD studentship DRC) to S.T., and a UCL Graduate Research Studentship and a Bogue Fellowship to M.K.H.
We thank Bill Wisden, Guy Rutter, Sergey Kasparov, Naoshige Uchida and Bryan Roth for plasmids and viruses as listed in Table 1. We thank Alexander Gourine, UCL, for advice regarding the stereotaxic brainstem injections, Ian Edwards, UCL, for assistance with the extraction of spinal cords, and we thank Linda Rinaman, Florida State University, for critical comments on the manuscript.
S.T. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Author Contributions
Conceptualization, S.T., J.E.R and M.K.H.; Methodology, S.T., J.E.R., M.K.H., D.I.B. and D.L.W., Investigation, M.K.H., J.E.R. D.R.C., S.T. and D.I.B.; Resources, F.R. and F.M.G.; Writing-Original Draft, M.K.H. J.E.R. and S.T.; Writing – Review & Editing, S.T., J.E.R., M.K.H., D.I.B., F.R., F.M.G., D.L.W. and D.R.C.; Supervision, S.T., J.E.R. and D.L.W. Funding Acquisition, S.T., M.K.H.
Duality of Interest
The authors declare no competing interests.
References
- 1.Llewellyn-Smith IJ, Marina N, Manton RN, Reimann F, Gribble FM, Trapp S. Spinally projecting preproglucagon axons preferentially innervate sympathetic preganglionic neurons. Neuroscience. 2015;284:872–887. doi: 10.1016/j.neuroscience.2014.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Llewellyn-Smith IJ, Gnanamanickam GJ, Reimann F, Gribble FM, Trapp S. Preproglucagon (PPG) neurons innervate neurochemically identified autonomic neurons in the mouse brainstem. Neuroscience. 2013;229:130–143. doi: 10.1016/j.neuroscience.2012.09.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Llewellyn-Smith IJ, Reimann F, Gribble FM, Trapp S. Preproglucagon neurons project widely to autonomic control areas in the mouse brain. Neuroscience. 2011;180:111–121. doi: 10.1016/j.neuroscience.2011.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Larsen PJ, Tang-Christensen M, Holst JJ, Orskov C. Distribution of glucagon-like peptide-1 and other preproglucagon-derived peptides in the rat hypothalamus and brainstem. Neuroscience. 1997;77:257–270. doi: 10.1016/s0306-4522(96)00434-4. [DOI] [PubMed] [Google Scholar]
- 5.Hisadome K, Reimann F, Gribble FM, Trapp S. CCK Stimulation of GLP-1 Neurons Involves {alpha}1-Adrenoceptor-Mediated Increase in Glutamatergic Synaptic Inputs. Diabetes. 2011;60:2701–2709. doi: 10.2337/db11-0489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hisadome K, Reimann F, Gribble FM, Trapp S. Leptin directly depolarizes preproglucagon neurons in the nucleus tractus solitarius: electrical properties of glucagon-like Peptide 1 neurons. Diabetes. 2010;59:1890–1898. doi: 10.2337/db10-0128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vrang N, Phifer CB, Corkern MM, Berthoud HR. Gastric distension induces c-Fos in medullary GLP-1/2-containing neurons. Am J Physiol Regul Integr Comp Physiol. 2003;285:R470–478. doi: 10.1152/ajpregu.00732.2002. [DOI] [PubMed] [Google Scholar]
- 8.Rinaman L. Interoceptive stress activates glucagon-like peptide-1 neurons that project to the hypothalamus. Am J Physiol. 1999;277:R582–590. doi: 10.1152/ajpregu.1999.277.2.R582. [DOI] [PubMed] [Google Scholar]
- 9.Kreisler AD, Rinaman L. Hindbrain glucagon-like peptide-1 neurons track intake volume and contribute to injection stress-induced hypophagia in meal-entrained rats. Am J Physiol Regul Integr Comp Physiol. 2016;310:R906–916. doi: 10.1152/ajpregu.00243.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kreisler AD, Davis EA, Rinaman L. Differential activation of chemically identified neurons in the caudal nucleus of the solitary tract in non-entrained rats after intake of satiating vs. non-satiating meals. Physiol Behav. 2014;136:47–54. doi: 10.1016/j.physbeh.2014.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maniscalco JW, Kreisler AD, Rinaman L. Satiation and stress-induced hypophagia: examining the role of hindbrain neurons expressing prolactin-releasing Peptide or glucagon-like Peptide 1. Frontiers in neuroscience. 2012;6:199. doi: 10.3389/fnins.2012.00199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holt MK, Trapp S. The physiological role of the brain GLP-1 system in stress. Cogent Biol. 2016;2 doi: 10.1080/23312025.2016.1229086. 1229086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maniscalco JW, Rinaman L. Interoceptive modulation of neuroendocrine, emotional, and hypophagic responses to stress. Physiol Behav. 2017;176:195–206. doi: 10.1016/j.physbeh.2017.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gaykema RP, Newmyer BA, Ottolini M, Raje V, Warthen DM, Lambeth PS, Niccum M, Yao T, Huang Y, Schulman IG, Harris TE, et al. Activation of murine pre-proglucagon-producing neurons reduces food intake and body weight. J Clin Invest. 2017;127:1031–1045. doi: 10.1172/JCI81335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu J, Conde K, Zhang P, Lilascharoen V, Xu Z, Lim BK, Seeley RJ, Zhu JJ, Scott MM, Pang ZP. Enhanced AMPA Receptor Trafficking Mediates the Anorexigenic Effect of Endogenous Glucagon-like Peptide-1 in the Paraventricular Hypothalamus. Neuron. 2017 doi: 10.1016/j.neuron.2017.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shi X, Chacko S, Li F, Li D, Burrin D, Chan L, Guan X. Acute activation of GLP-1-expressing neurons promotes glucose homeostasis and insulin sensitivity. Molecular metabolism. 2017;6:1350–1359. doi: 10.1016/j.molmet.2017.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parker HE, Adriaenssens A, Rogers G, Richards P, Koepsell H, Reimann F, Gribble FM. Predominant role of active versus facilitative glucose transport for glucagon-like peptide-1 secretion. Diabetologia. 2012;55:2445–2455. doi: 10.1007/s00125-012-2585-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holt MK, Llewellyn-Smith IJ, Reimann F, Gribble FM, Trapp S. Serotonergic modulation of the activity of GLP-1 producing neurons in the nucleus of the solitary tract in mouse. Molecular metabolism. 2017;6:909–921. doi: 10.1016/j.molmet.2017.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anesten F, Holt MK, Schele E, Palsdottir V, Reimann F, Gribble FM, Safari C, Skibicka KP, Trapp S, Jansson JO. Preproglucagon neurons in the hindbrain have IL-6 receptor-alpha and show Ca2+ influx in response to IL-6. Am J Physiol Regul Integr Comp Physiol. 2016;311:R115–123. doi: 10.1152/ajpregu.00383.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reimann F, Habib AM, Tolhurst G, Parker HE, Rogers GJ, Gribble FM. Glucose sensing in L cells: a primary cell study. Cell Metab. 2008;8:532–539. doi: 10.1016/j.cmet.2008.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Edelstein AD, Tsuchida MA, Amodaj N, Pinkard H, Vale RD, Stuurman N. Advanced methods of microscope control using muManager software. J Biol Methods. 2014;1 doi: 10.14440/jbm.2014.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Machhada A, Trapp S, Marina N, Stephens RCM, Whittle J, Lythgoe MF, Kasparov S, Ackland GL, Gourine AV. Vagal determinants of exercise capacity. Nature communications. 2017;8 doi: 10.1038/ncomms15097. 15097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schindelin J, Arganda-Carreras I, Frise E, Kaynig V, Longair M, Pietzsch T, Preibisch S, Rueden C, Saalfeld S, Schmid B, Tinevez JY, et al. Fiji: an open-source platform for biological-image analysis. Nat Methods. 2012;9:676–682. doi: 10.1038/nmeth.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scott MM, Williams KW, Rossi J, Lee CE, Elmquist JK. Leptin receptor expression in hindbrain Glp-1 neurons regulates food intake and energy balance in mice. J Clin Invest. 2011;121:2413–2421. doi: 10.1172/JCI43703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang XF, Liu JJ, Xia J, Liu J, Mirabella V, Pang ZP. Endogenous Glucagon-like Peptide-1 Suppresses High-Fat Food Intake by Reducing Synaptic Drive onto Mesolimbic Dopamine Neurons. Cell Rep. 2015;12:726–733. doi: 10.1016/j.celrep.2015.06.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marina N, Abdala AP, Trapp S, Li A, Nattie EE, Hewinson J, Smith JC, Paton JF, Gourine AV. Essential role of Phox2b-expressing ventrolateral brainstem neurons in the chemosensory control of inspiration and expiration. J Neurosci. 2010;30:12466–12473. doi: 10.1523/JNEUROSCI.3141-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Merchenthaler I, Lane M, Shughrue P. Distribution of pre-pro-glucagon and glucagon-like peptide-1 receptor messenger RNAs in the rat central nervous system. J Comp Neurol. 1999;403:261–280. doi: 10.1002/(sici)1096-9861(19990111)403:2<261::aid-cne8>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 28.Thiebaud N, Llewellyn-Smith IJ, Gribble F, Reimann F, Trapp S, Fadool DA. The incretin hormone glucagon-like peptide 1 increases mitral cell excitability by decreasing conductance of a voltage-dependent potassium channel. J Physiol. 2016;594:2607–2628. doi: 10.1113/JP272322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maniscalco JW, Zheng H, Gordon PJ, Rinaman L. Negative Energy Balance Blocks Neural and Behavioral Responses to Acute Stress by "Silencing" Central Glucagon-Like Peptide 1 Signaling in Rats. J Neurosci. 2015;35:10701–10714. doi: 10.1523/JNEUROSCI.3464-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yamamoto H, Kishi T, Lee CE, Choi BJ, Fang H, Hollenberg AN, Drucker DJ, Elmquist JK. Glucagon-like peptide-1-responsive catecholamine neurons in the area postrema link peripheral glucagon-like peptide-1 with central autonomic control sites. J Neurosci. 2003;23:2939–2946. doi: 10.1523/JNEUROSCI.23-07-02939.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yamamoto H, Lee CE, Marcus JN, Williams TD, Overton JM, Lopez ME, Hollenberg AN, Baggio L, Saper CB, Drucker DJ, Elmquist JK. Glucagon-like peptide-1 receptor stimulation increases blood pressure and heart rate and activates autonomic regulatory neurons. J Clin Invest. 2002;110:43–52. doi: 10.1172/JCI15595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ghosal S, Packard AEB, Mahbod P, McKlveen JM, Seeley RJ, Myers B, Ulrich-Lai Y, Smith EP, D'Alessio DA, Herman JP. Disruption of Glucagon-Like Peptide 1 Signaling in Sim1 Neurons Reduces Physiological and Behavioral Reactivity to Acute and Chronic Stress. Journal of Neuroscience. 2017;37:184–193. doi: 10.1523/JNEUROSCI.1104-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee SJ, Sanchez-Watts G, Krieger JP, Pignalosa A, Norell PN, Cortella A, Pettersen KG, Vrdoljak D, Hayes MR, Kanoski S, Langhans W, et al. Loss of dorsomedial hypothalamic GLP-1 signaling reduces BAT thermogenesis and increases adiposity. Molecular metabolism. 2018;11:33–46. doi: 10.1016/j.molmet.2018.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tuesta LM, Chen Z, Duncan A, Fowler CD, Ishikawa M, Lee BR, Liu XA, Lu Q, Cameron M, Hayes MR, Kamenecka TM, et al. GLP-1 acts on habenular avoidance circuits to control nicotine intake. Nat Neurosci. 2017;20:708–716. doi: 10.1038/nn.4540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kanoski SE, Hayes MR, Skibicka KP. GLP-1 and weight loss: unraveling the diverse neural circuitry. Am J Physiol Regul Integr Comp Physiol. 2016;310:R885–895. doi: 10.1152/ajpregu.00520.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roman CW, Derkach VA, Palmiter RD. Genetically and functionally defined NTS to PBN brain circuits mediating anorexia. Nature communications. 2016;7 doi: 10.1038/ncomms11905. 11905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Donahey JC, van Dijk G, Woods SC, Seeley RJ. Intraventricular GLP-1 reduces short- but not long-term food intake or body weight in lean and obese rats. Brain Res. 1998;779:75–83. doi: 10.1016/s0006-8993(97)01057-3. [DOI] [PubMed] [Google Scholar]
- 38.Roth BL. DREADDs for Neuroscientists. Neuron. 2016;89:683–694. doi: 10.1016/j.neuron.2016.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sisley S, Gutierrez-Aguilar R, Scott M, D'Alessio DA, Sandoval DA, Seeley RJ. Neuronal GLP1R mediates liraglutide's anorectic but not glucose-lowering effect. J Clin Invest. 2014;124:2456–2463. doi: 10.1172/JCI72434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tabuchi S, Tsunematsu T, Black SW, Tominaga M, Maruyama M, Takagi K, Minokoshi Y, Sakurai T, Kilduff TS, Yamanaka A. Conditional ablation of orexin/hypocretin neurons: a new mouse model for the study of narcolepsy and orexin system function. J Neurosci. 2014;34:6495–6509. doi: 10.1523/JNEUROSCI.0073-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scrocchi LA, Hill ME, Saleh J, Perkins B, Drucker DJ. Elimination of glucagon-like peptide 1R signaling does not modify weight gain and islet adaptation in mice with combined disruption of leptin and GLP-1 action. Diabetes. 2000;49:1552–1560. doi: 10.2337/diabetes.49.9.1552. [DOI] [PubMed] [Google Scholar]
- 42.Sandoval DA, D'Alessio DA. Physiology of proglucagon peptides: role of glucagon and GLP-1 in health and disease. Physiol Rev. 2015;95:513–548. doi: 10.1152/physrev.00013.2014. [DOI] [PubMed] [Google Scholar]
- 43.Jessen L, Smith EP, Ulrich-Lai Y, Herman JP, Seeley RJ, Sandoval D, D'Alessio D. Central Nervous System GLP-1 Receptors Regulate Islet Hormone Secretion and Glucose Homeostasis in Male Rats. Endocrinology. 2017;158:2124–2133. doi: 10.1210/en.2016-1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barrera JG, Jones KR, Herman JP, D'Alessio DA, Woods SC, Seeley RJ. Hyperphagia and increased fat accumulation in two models of chronic CNS glucagon-like peptide-1 loss of function. J Neurosci. 2011;31:3904–3913. doi: 10.1523/JNEUROSCI.2212-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mietlicki-Baase EG, Liberini CG, Workinger JL, Bonaccorso RL, Borner T, Reiner DJ, Koch-Laskowski K, McGrath LE, Lhamo R, Stein LM, De Jonghe BC, et al. A vitamin B12 conjugate of exendin-4 improves glucose tolerance without associated nausea or hypophagia in rodents. Diabetes, obesity & metabolism. 2018;20(5):1223–1234. doi: 10.1111/dom.13222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hayes MR, Bradley L, Grill HJ. Endogenous hindbrain glucagon-like peptide-1 receptor activation contributes to the control of food intake by mediating gastric satiation signaling. Endocrinology. 2009;150:2654–2659. doi: 10.1210/en.2008-1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Maniscalco JW, Rinaman L. Overnight food deprivation markedly attenuates hindbrain noradrenergic, glucagon-like peptide-1, and hypothalamic neural responses to exogenous cholecystokinin in male rats. Physiol Behav. 2013 doi: 10.1016/j.physbeh.2013.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kinzig KP, D'Alessio DA, Herman JP, Sakai RR, Vahl TP, Figueiredo HF, Murphy EK, Seeley RJ. CNS glucagon-like peptide-1 receptors mediate endocrine and anxiety responses to interoceptive and psychogenic stressors. J Neurosci. 2003;23:6163–6170. doi: 10.1523/JNEUROSCI.23-15-06163.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Krashes MJ, Koda S, Ye C, Rogan SC, Adams AC, Cusher DS, Maratos-Flier E, Roth BL, Lowell BB. Rapid, reversible activation of AgRP neurons drives feeding behavior in mice. J Clin Invest. 2011;121:1424–1428. doi: 10.1172/JCI46229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Murray AJ, Sauer JF, Riedel G, McClure C, Ansel L, Cheyne L, Bartos M, Wisden W, Wulff P. Parvalbumin-positive CA1 interneurons are required for spatial working but not for reference memory. Nat Neurosci. 2011;14:297–299. doi: 10.1038/nn.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.