Abstract
Rationale
Subcellular Ca2+ indicators have yet to be developed for the myofilament where disease mutation, or small molecules may alter contractility through myofilament Ca2+ sensitivity. Here we develop and characterise genetically encoded Ca2+ indicators restricted to the myofilament to directly visualise Ca2 changes in the sarcomere.
Objective
To produce and validate myofilament restricted Ca2+ imaging probes in an adenoviral transduction adult cardiomyocyte model using drugs that alter myofilament function (MYK-461, omecamtiv mecarbil and levosimendan) or following co-transduction of two established hypertrophic cardiomyopathy (HCM) disease causing mutants (cTnT R92Q and cTnI R145G) that alter myofilament Ca2+ handling.
Methods and Results
When expressed in adult ventricular cardiomyocytes RGECO-TnT/TnI sensors localise correctly to the sarcomere without contractile impairment. Both sensors report cyclical changes in fluorescence in paced cardiomyocytes with reduced Ca2+ on and increased Ca2+ off rates compared with unconjugated RGECO. RGECO-TnT/TnI revealed changes to localised Ca2+ handling conferred by MYK-461 and levosimendan, including an increase in Ca2+ binding rates with both levosimendan and MYK-461 not detected by an unrestricted protein sensor. Co-adenoviral transduction of RGECO-TnT/TnI with HCM causing thin filament mutants showed that the mutations increase myofilament [Ca2+] in systole, lengthen time to peak systolic [Ca2+], and delay [Ca2+] release. This contrasts with the effect of the same mutations on cytoplasmic Ca2+, when measured using unrestricted RGECO where changes to peak systolic Ca2+ are inconsistent between the two mutations. These data contrast with previous findings using chemical dyes that show no alteration of [Ca2+] transient amplitude or time to peak Ca2+.
Conclusions
RGECO-TnT/TnI are functionally equivalent. They visualise Ca2+ within the myofilament and reveal unrecognised aspects of small molecule and disease associated mutations in living cells.
Keywords: Hypertrophic cardiomyopathy, calcium, contractility, genetically encoded Ca2+ indicators, excitation-contraction coupling, fluorescent imaging, mechanisms
Subject Terms: Basic Science Research, Calcium Cycling/Excitation-Contraction Coupling, Cardiomyopathy, Hypertrophy, Myocardial Biology
Introduction
The myofilament converts the chemical energy of ATP into mechanical energy, a process regulated by Ca2+. Mutations in myofilament components cause common (1:500) inherited conditions like hypertrophic cardiomyopathy (HCM)1,2, 3. HCM causing mutations produce hypercontractility, energetic compromise4–6 and change Ca2+ utilization within the cardiomyocyte. Altered intracellular Ca2+ may be directly proarrhythmic, causing sudden death, and activate hypertrophic signalling pathways that produce the cardiac hypertrophy, and premature heart failure, observed in HCM patients. Interestingly, increased myofilament Ca2+ affinity arises from different mutations7, 8. Prevalent thick filament mutations increase the Ca2+ sensitivity of contractility by altering acto-myosin affinity and modifying conformational changes in the myosin motor domain9. Conversely, thin filament mutations in the regulatory components troponin T (TnT) and I (TnI) increase the affinity of troponin C (TnC) for Ca2+. Some consequences of trapping Ca2+ in the sarcomere by the introduction of Ca2+ sensitizing HCM mutations are known10–12. Briefly, raised myofilament Ca2+ binding produces secondary alterations in cytoplasmic and SR [Ca2+] in addition to altered activation/regulation of key Ca2+ handling proteins (e.g. Ryanodine Receptor, SERCA2a and phospholamban). Hypertrophic signalling via calcineurin/NFAT and ERK promotes cellular hypertrophy13. These factors, combined with altered mechanosensing14 and energetics2, 15, drive the stereotyped end-organ changes seen in patients.
Ca2+ cycling changes in HCM are typically assessed using chemical Ca2+ dyes10, 11, 13. However, dyes are not spatially restricted 16–19 and thus report whole cell phenomena. The patch clamp technique20 can resolve subcellular Ca2+ events10, 11 but is technically challenging and low throughput. Genetically encoded calcium indicators (GECIs) offer an alternative strategy for Ca2+ assessment17, 19, and may be restricted to subcellular compartments by a defined sequence tag or protein fusion. Myofilament specific calcium probes remain elusive, in part due to the concern that the bulky 30x40x70Å adducts of the smallest GECIs21 are unlikely to be tolerated by the paracrystalline sarcomeric environment22, 23 leading to perturbed function of the indicator, the fusion partner, or the cell. However, fluorescence resonance energy transfer-based cAMP indicators conjugated to myofilament proteins that do not affect cardiomyocyte contractility have been reported24.
GECIs are available with different calcium sensor domains, tuned to different affinities, in a range of spectral hues. The CaM/M13 calcium sensor domain appears in most of the indicators successfully reported in cardiomyocytes, but not all GECIs work in all cardiac models17. For example, tools improved for neuronal applications may lose functionality in cardiac cells17 eg TN-XL25 and TN-XXL26. Subcellular targeting of GECIs within cardiomyocytes to probe Ca2+ in the SR27 and, by conjugation of GCaMP2.2 to FKBP12.6, Ca2+ efflux from the SR28 has been demonstrated. These probes visualise the Ca2+ store, but currently no equivalent tool to study Ca2+ at the myofilament, where Ca2+ regulates contraction exists.
Since contractility underpins cardiac function there is interest in development of small molecule modulators of myofilament contractility22, 29–31. Importantly these agents should not affect Ca2+ handling, which may be pro-arrhythmic. Application of unrestricted, or myofilament localised, indicators may give greater mechanistic insight into this subclass of drugs, which include the myosin ATPase inhibitor MYK-46130, a novel therapy for hypertrophic cardiomyopathy, and levosimendan31 a myofilament activator developed for heart failure.
Here we produce, and characterize myofilament localized Ca2+ sensors to directly visualize changes in Ca2+ flux at the myofilament occurring in response to small molecules or disease causing mutations. We reveal how two well characterised thin filament HCM causing mutations in cTnT (R92Q)4, 10, 32, 33 and cTnI (R145G)10, 34–36 are from a Ca2+ handling perspective mechanistically similar at the myofilament, but distinct in the cytoplasm. The combination of probes reveals biology previously inferred. The method increase scale, reduces animal use, and is compatible with existing imaging infrastructure and single cell protocols.
Methods
The software, the plasmids or the data that support the findings of this study are available from the corresponding author upon reasonable request.
Isolation of guinea pig left ventricular cardiomyocytes
This investigation was approved by the Animal Welfare and Ethical Review Board at the University of Oxford and conforms to the UK Animals (Scientific Procedures) Act, 1986, incorporating Directive 2010/63/EU of the European Parliament. As described10, left ventricular cardiomyocytes were isolated from male (to prevent confounding effects of hormonal cycle) adolescent (400 g) guinea pig hearts by collagenase perfusion for 5 minutes then placed on a shaker for a further 10 minutes. Left ventricular cardiomyocytes (1.5x105 cells per ml) were incubated in ACCITT3 culture medium37 at 37°C and 5%CO2.
Adenoviral transduction
RGECO-TnT (plus BamHI linker) and RGECO-TnI (plus XhoI linker) were cloned into a shuttle vector. RGECO and RGECO-TnI adenoviruses were generated, purified and titred by Welgen, Inc. (Worcester, MA, USA). RGECO-TnT, WT cTnT, cTnT R92Q, WT cTnI, and cTnI R145G adenoviruses were generated as described10. Immediately after isolation GPCMs were adenovirally co-transduced for 48 hours with RGECO (MOI=444) and either WT cTnT (795), cTnT R92Q (933), WT cTnI (795), or cTnI R145G (795). Co-transductions of RGECO-TnT (MOI=795) were with either WT cTnI (795), or cTnI R145G (1590). Co-transductions of RGECO-TnI (MOI=444) were with either WT cTnT (795) or cTnT R92Q (1493).
Protein purification
N- and C-terminal eGFP conjugates of human recombinant TnT, TnI and TnC were cloned into pMW172 vector using 3’ NdeI and 5’ EcoRI restriction sites and an internal HindIII restriction site linker. RGECO and RGECO-TnT were similarly sub-cloned into pMW172. Proteins were expressed in BL21-DE3(pLysS) E.coli induced using 0.4mmol/L Isopropyl β-D-1-thiogalactopyranoside for 4 hours. Bacterial pellets recovered by centrifugation (10,000xg for 10mins) were lysed in buffer containing 25mmol/L Tris-HCl, pH 7.5, 20% sucrose, 1mmol/L EDTA, 200mmol/L NaCl,5 mol/L urea, 0.1% Triton X-100. All proteins were purified using an AKTA-UPC900 FPLC using HiTrap FF chromatography columns (GE Healthcare, Amersham). GFP-TnT and TnT-GFP were purified using sequential cation (in buffer containing 6mol/L urea, 1mmol/L EDTA, 1mmol/L 2-mercaptoethanol, 20mmol/L MOPS, pH 6.0) followed by anion (in buffer containing 6mol/L urea, 1mmol/L EDTA, 1mmol/L 2-mercaptoethanol 50mmol/L Tris-HCl pH 8.0) exchange chromatography. GFP-TnC and TnC-GFP were purified by anion (pH 8.5) exchange chromatography. GFP-TnI and TnI-GFP were purified by sequential cation and anion exchange chromatography. RGECO and RGECO-TnT were purified using sequential anion (pH 8.0) exchange chromatography, ammonium sulphate fractionation (to 50% for RGECO and 35% for RGECO-TnT) and finally Hydrophobic Interaction Chromatography (HIC) (in buffer containing 30% ammonium sulphate, 200mmol/L NaCl2 1mmol/L ditiothretol and 30mmol/L 4-(2-hydroxyethyl)-1-piperazineethanesulphonic acid (HEPES)). Ion exchange columns were eluted using a 0-2mol/L NaCl gradient, the HIC column was eluted with a 30–0% ammonium sulphate gradient. 6-Histidine-tagged RGECO-TnI was cloned into a PET23a vector and expressed as above, and purified using a HisTrap HP column (GE Healthcare) in a buffer containing 15.48mmol/L Na2HPO4, 4.52mmol/L NaH2PO4, 500mmol/L NaCl, and 6mol/L Urea (Histag buffer), followed by washing in Histag buffer with 20mmol/L Imidazole (pH 7.0), then eluted in an increasing Histag buffer gradient containing 500mmol/L Imidazole (pH 7.0). Eluted fractions were assessed for purity using 12% SDS-PAGE gels, stained with Coomassie brilliant blue. Histag was cleaved using a thrombin kit (Merck) following the manufactures instructions. Wild type human recombinant TnT, TnI, TnC and Ala-Ser-α-TM39 were purified as previously described38. Troponin complex containing either WT, GFP-TnT, TnT-GFP, GFP-TnC, TnC-GFP, GFP-TnI, or TnI-GFP were reconstituted by dialysis into buffer containing 10mmol/L imidazole pH 7.0, 1mmol/L DTT, 0.01% azide, 0.1mol/L CaCl2, 6mol/L urea and 1mol/L KCl. Urea was reduced stepwise from to 2 then 0mol/L, then KCl was reduced stepwise from 1mol/L to 800 – 600 – 400 – 200mmol/L KCl in a series of 3 hour dialyses. Tn Complex was purified using size exclusion chromatography in 200mmol/L KCl dialysis buffer. Purity was analysed by SDS-PAGE. Purified troponin complexes were dialysed into buffer containing 5mmol/L 1,4-Piperazinediethanesulphate pH 7.0, 3.87mmol/L MgCl2, 1mmol/L DTT for ATPase assay experiments. Actin and myosin-S1 was extracted from rabbit skeletal muscle as described39, 40.
In vitro acto-myosin ATPase assays
ATPase assays were carried out as described8, 38. Briefly, a master stock of 3.5μmol/L actin, 0.5μmol/L myosin S1, 0.5μmol/L Ala-Ser-α-TM and 0.5μmol/L Tn complex were mixed in buffer containing 5mmol/L 1,4-Piperazinediethanesulphate pH 7.0, 3.87mmol/L MgCl2, and 1mmol/L DTT. To ensure precise thin filament protein stoichiometry, each stock was centrifuged at 384000xg for 15 minutes. Recovered pellets were aliquoted and set to a range of [Ca2+]free from pCa 4.5-8.5 using Maxchelatior (http://maxchelator.stanford.edu/CaEGTA-TS.htm). ATPase reactions were initiated by addition of 3mmol/L ATP and incubated at 37°C for 15 minutes. Each reaction was quenched in 5% TCA, finally 1% ammonium molybdate in 0.5mol/L H2SO4, followed by 40% iron(II)sulphate in 0.5mol/L H2SO4 was used to measure inorganic phosphate. Absorbance (A700) measurements were converted to absolute activity (sec-1). Calcium-sensitivity data was fitted to the Hill equation using KaleidaGraph (Synergy Software).
Hill equation:
Where: A=ATPase rate; Amin=Minimum ATPase rate; Amax=Maximum ATPase rate; pCa=-log [Ca2+]; pCa50=- log [Ca2+] required for half maximum ATPase activity; nH=Hill coefficient.
Calcium binding Kd calculations
For steady state Ca2+ binding affinity (Kd) for RGECO, RGECO-TnI and RGECO-TnT, 3μmol/L of protein was dialysed into buffer containing 130mmol/L NaCl, 10mmol/L 4-(2-hydroxyethyl)-1- piperazineethanesulphonic acid (HEPES), 1mmol/L dithiothretol, 1.3mmol/L MgCl2, pH 7.3. A range of free[Ca2+] conditions were set between 3.16nmol/L (pCa 8.5) and 31.6μmol/L (pCa 4.5) using 1mmol/L EGTA and the corresponding concentration of CaCl2. Steady state fluorescence readings were made in an Ultraclear bottom 96-well microplate using a FLUOstar Omega plate reader (BMG LABTEC, Germany), using 544nm excitation and 590/10nm emission filters at both 25 and 37°C. Fluorescence emission intensities were plotted vs free[Ca2+] and fitted to the Hill equation to calculate Kd values for each protein and condition. For Ca2+ displacement (koff), 125nmol/L RGECO-TnT plus 5µmol/L CaCl2 was mixed with 5mmol/L EGTA in a buffer containing 130mmol/L NaCl, 10mmol/L 4-(2- hydroxyethyl)-1-piperazineethanesulphonic acid (HEPES) 1.3mmol/L MgCl2, 1mmol/L dithiothretol, pH 7.3 with NaOH. RGECO or RGECO-TnT was loaded into a Stopped-flow system (HiTech Scientific, Bradford-on-Avon, UK), concentrations after mixing 1:1 in the stopped-flow. Fluorescence was excited at 546nm (100W Xe/Hg lamp and monochromator) and emission monitored through an OG-590 glass filter. Data was fitted to a single exponential decrease in fluorescence of 50-100%, depending upon temperature. For calcium binding (kon), 125nmol/L RGECO-TnT was measured at 10µmol/L free calcium by mixing with a buffer containing 2.125mmol/L Ca. EGTA and 0.2mmol/L EGTA with the same filter set as before. Fluorescence increase upon Ca2+ addition was fitted to a single exponential. The observed single exponential rate constant, kobs, was extracted for kon and koff for both sensors, at a range of temperatures between 25 and 37°C. To estimate the dissociation constant, we using the equations Kd = kobs-off [Ca]/ kobs on; these were comparable to steady state Kd values.
Determination of Quantum Yield and Molar Extinction Co-efficient
Quantum yield and molar extinction co-efficient was determined for each Ca2+ sensor following41. Quantum yield standards were mCherry (for RGECO) and RGECO for RGECO-TnT. The concentration of protein in buffer containing 10 mM HEPES, 1.3mmol/L MgCl2 and 1mmol/L dithiothreitol was determined using BCA assay (Pierce) and set to either pCa 4.5 of 8.5.The protein concentration was reduced to an absorbance at the excitation wavelength between 0.2 and 0.6. Dilutions to absorbance’s of 0.01, 0.02, 0.03 and 0.04 were made for each protein solution and standard. The fluorescence emission spectra at Ex F568 were recorded using an RF-1501 spectrofluorimeter (Shimadzu, Japan). Total fluorescence intensities were obtained by integration. Integrated fluorescence intensity vs. absorbance was plotted for each protein and each standard. Quantum yields were determined from the slopes (S) of each line using the equation: Φprotein = Φstandard × (Sprotein/Sstandard). Extinction coefficients were determined from the absorption spectrum of both RGECO and RGECO-TnT at pCa 8.5 and 4.5 in the buffer above using a plate reader (BMG LABTECH, Germany). Peak Absorbance wavelengths were determined to be A465 in low Ca2+ and A581 in high Ca2+. Absorbance measurements were converted to 1 cm path length using BMG Omega software. Extinction coefficients were calculated by dividing the peak absorbance maximum by protein concentration.
Immunofluorescence
GPCMs were fixed in 4% paraformaldehyde, washed in PBS, permeabilized and blocked in 0.1% Triton X-100, 3% BSA in PBS. Primary antibodies (1:500 anti-alpha actinin (Sigma, clone EA-53, A7811), 1:200 anti-DsRed (Clontech, 632496), 1:8 anti-Flagtag (Sigma, F1804)) were added overnight at 4°C, washed in PBS, and secondary antibodies added (goat anti-rabbit IgG Alexa 568 (1:200) (Invitrogen, A21069) and goat anti-mouse IgG Alexa 633 (1:200) (Invitrogen, A21053)) for 1 hour at room temperature, washed in PBS and mounted on slides in ProLong Diamond antifade with DAPI (ThermoFisher). Slides were imaged on a Leica TCS SP5 confocal microscope with a 63x oil immersion lens, images data was extracted with Leica LAS and ImageJ (NIH, USA). Control slides were prepared excluding the primary antibody for all IF experiments, negligible background fluorescence was detected in all cases.
Subcellular fractionation and western blotting
GPCMs were fractionated to recover cytoplasmic and sarcomeric/cytoskeletal samples following42. 300,000 cardiomyocytes were centrifuged, re-suspended in buffer containing, 20mmol/L Tris-HCl pH 7.4, 2mmol/L EDTA, 0.5mmol/L EGTA, 0.3mmol/L sucrose and homogenised for 1 minute. Cells were pelleted at 1000xg for 5mins, the supernatant/cytoplasmic fraction was retained for SDS-PAGE analysis and western blotting. The cell pellet was washed 3 times in fractionation buffer + 1% Triton X-100 each time pelleting the sarcomeric fraction by centrifugation at 1000xg for 5mins. Finally, the sarcomeric fraction was re-suspended in fractionation buffer (without Triton X-100) and prepared for western blotting. Subcellular fractions and GPCM lysates were run on a 12% polyacrylamide gel, transferred onto PVDF membrane, and blocked with 5% bovine milk in Tris buffered saline, 0.1% Tween-20 (TBS-T) for 1hour. Primary antibodies were incubated overnight at 4°C in 5% bovine milk in TBS-T (1:2000 anti-cTnT (Sigma, SAB2108239), 1:4000 anti-ERK (Cell Signaling Technologies, 4695s), 1:5000 anti-FLAG-tag (Sigma, F3165), 1:10000 anti-GAPDH (Millipore, ABS16), 1:2000 anti-TnI (TNNI3, Aviva Systems Biology, ARP41391_P050). Membranes washed in TBS-T were incubated in secondary antibodies (1:10000 anti-rabbit HRP (GE Healthcare, NA934), 1:10000 anti-mouse HRP (GE Healthcare, NA931)) for 1 hour at room temperature, washed in TBS-T then developed with ECL select (GE Healthcare) and imaged on a ChemiDoc MP (BioRad). Densitometric measurements to compare single verses double infected levels of FLAG-tag protein were carried out using Image Lab software (BioRad), and normalised to GAPDH loading controls for each comparison.
Sarcomere length measurements
Sarcomere length measurements were performed using IonOptix µstep apparatus and the manufacturers’ standard operating instructions. Cells, electrically paced at 40 volts, 0.5 Hz, 37°C were perfused with buffer containing 150mmol/L NaCl, 10mmol/L HEPES, 7mmol/L glucose, 1mmol/L MgCl2, 1mmol/L KCl, 0.3mmol/L NaH2PO3, 1.8mmol/L CaCl2, at pH 7.4. Cells displaying asynchronous contractility, excessive blebbing/dysmorphology were ignored for acquisition. Similarly cells with contractile magnitudes or velocities exceeding 2 standard deviations from the mean upon analysis were also excluded due to phenotypic heterogeneity arising in cultured primary cells.
Imaging and analysis
GPCMs imaged on an Olympus IX81 inverted microscope (Olympus, Japan) with a C-1900 EMCCD camera (Hamamatsu, Japan) were electrically paced at 0.5Hz in a humidified chamber at 37°C. Videos (28seconds, 25fps) were acquired through an Olympus UPlanFLN 10x lens (NA 0.3) with the RFP filter set of 560/25 nm (excitation), 620/60 nm (emission) with a 565 nm dichroic mirror using CellR software (Olympus) as previously described43. RGECO, RGECO-TnI and RGECO-TnT adenovirally transduced GPCMs were incubated with 250nmol/L MYK-461, 200µmol/L omecamtiv mecarbil or 10µmol/L levosimendan 20mins before imaging. For Fluo-4 comparison, RGECO-TnT transduced cardiomyocytes were loaded with 1μmol/L Fluo-4 as per the manufacturer’s instructions for 5minutes and imaged using RFP and GFP (485/20-25 nm (excitation), 525/50 nm (emission) with a 495 nm dichroic mirror) filter sets.
Raw image data was extracted using CellR (Olympus), and analysed in Excel (Microsoft). From a single cell, 10 transients were extracted and averaged to give a single transient in a 2 second interval per cell. Time to 50% contraction, time to 50% baseline (from peak), time of peak, or time above 50% was determined. Peak intensity analysis was performed as previously described for intensiometric sensors44, 45
Where F(t) is the fluorescence intensity at time (t), and F(min) the minimum fluorescence intensity during the averaged transient.
Statistics
For all single cells experiments, comparisons were from at least three separate cell isolations, where approximately equal numbers of cells (±5) were taken from each preparation on an experiment-to-experiment basis. Data was firstly tested for normality (D’Agostino-Pearson). Sarcomere length measurements were made using unpaired Students t-test. Wilcoxon T-test was used for the comparison of Fluo-4 to RGECO-TnT. RGECO to RGECO-TnT/TnI and pacing frequencies were compared using non-parametric Kruskal-Wallis one-way ANOVA. Drugs and WT to mutant troponin were compared using non-parametric Mann-Whitney test (Graphpad Prism). Once acquired, all data was blinded prior to extraction and analysis.
Results
Development and In vitro characterisation of myofilament RGECO Ca2+ sensors
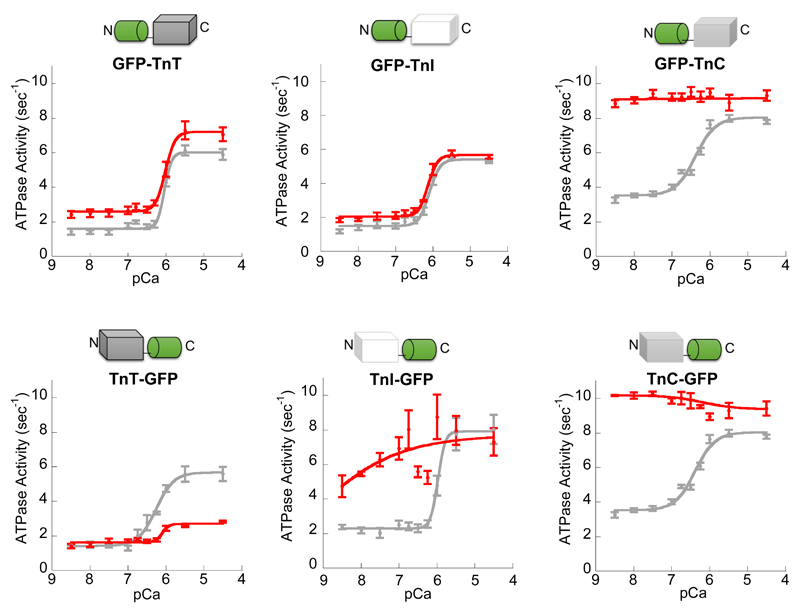
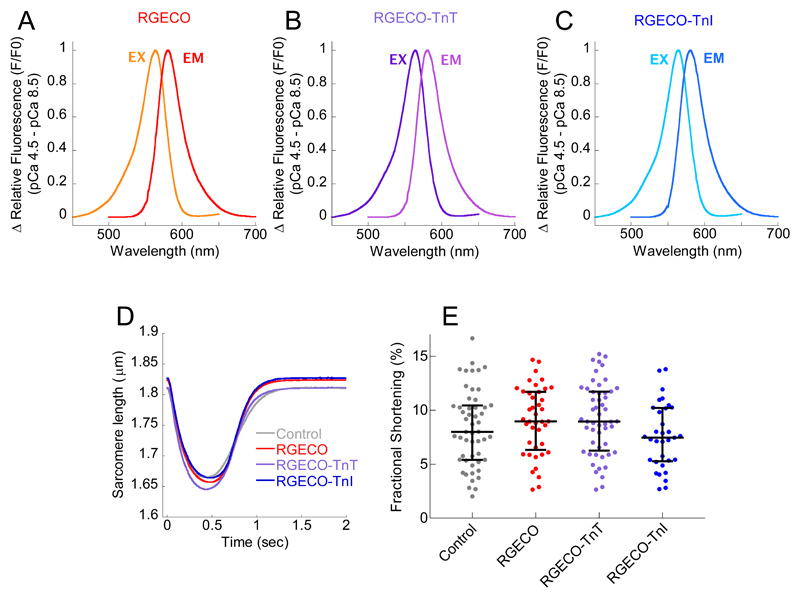
To develop a myofilament-restricted GECI, fusion proteins of green fluorescent protein (GFP) at the N- and C-terminus of each troponin subunit were screened to identify sites preserving in vitro acto-myosin ATPase Ca2+ dependent regulation. GFP conjugation to the N-terminus of either TnT or TnI maintained Ca2+ regulation (Figure 1, Online Table I). Subsequently, the red GECI RGECO41 was conjugated to the N-terminus of troponin-T and troponin-I (Online Figure X, XI). In vitro characterisation of the calcium indicator properties of RGECO-TnT and RGECO-TnI showed Kd of 764.5±17.6nmol/L, and 657.3±27.3nmol/L respectively under physiological pH46, temperature and magnesium concentration47 (Online Figure I), with preservation of dynamic range and excitation/emission spectra (Figure 2A-C, Online Table II). This is compatible with previous reports41 (RGECO Kd = 484nmol/L at 25°C and 3mmol/L MgCl2). At physiological temperature, Ca2+ on (kobs 16.7μmol/L-1s-1 at 10μmol/L free Ca2+) and off (koff = 16.9s-1) rates for myofilament RGECO were approximately twice those observed at 25ºC (Online Figure II). Importantly in intact, but unloaded, GPCMs the presence of RGECO-TnT/TnI did not affect sarcomere shortening compared to uninfected controls (Figure 2D and E, Online Figure III).
Figure 1. The effect of GFP conjugation to the N and C terminus of troponin subunits on myofilament function.
Myofilament function was assessed using in vitro actin activated acto-myosin S1 ATPase assays. Control (unconjugated) troponin complexes (grey lines) were compared pairwise to troponin complex reconstituted with subunits conjugated to the N or the C terminus of GFP as illustrated (red lines). n=3-5 error bars are ± SEM.
Figure 2. Fluorescent and contractile properties of RGECO, RGECO-TnT and RGECO-TnI.
Steady state fluorescence excitation, emission spectra (peak excitation (Ex) = 564nm) / peak emission (Em) = 581nm) were obtained at pCa4.5 and subtracted from paired spectra at pCa8.5 for purified recombinant RGECO (A), RGECO-TnT (B) and RGECO-TnI (C). Sarcomere shortening during electrical pacing (0.5Hz) of isolated adult cardiomyocytes was used to test cardiac contractile function in non-transduced and either RGECO, RGECO-TnT or RGECO-TnI transduced GPCMs by measurement of the sarcomeric length during contraction (n=33-52) (D) or by fractional shortening (E).
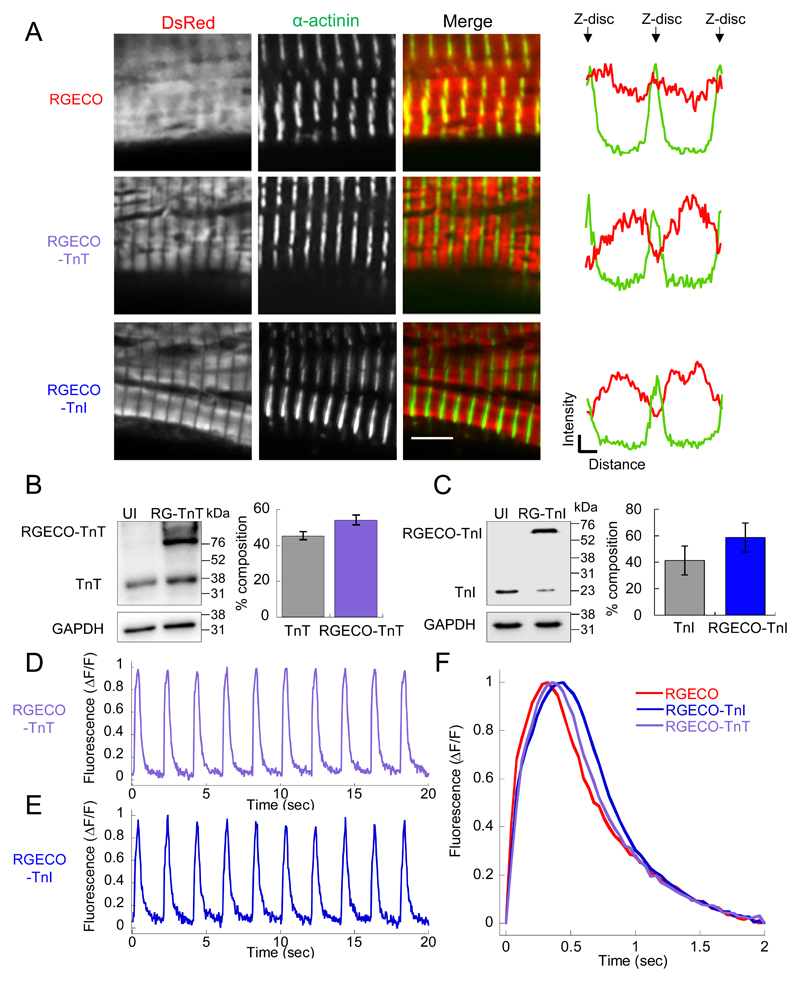
Characterisation of RGECO-TnT and RGECO-TnI Ca2+ sensors in cardiomyocytes
RGECO-TnT or RGECO-TnI localize to the sarcomere, without Z-disk accumulation, following adenoviral transduction of GPCMs. Conversely, unconjugated RGECO is broadly distributed with weak Z-disk accumulation (Figure 3A, Online Figure IV). 48 hours following viral infection, total TnI contained 58.7±11.0% (n=5) RGECO-TnI and similarly TnT contained 54.3±5.5% (n=4) RGECO-TnT (Figure 3B and C). RGECO-TnI and RGECO-TnT both show cyclical fluorescence in paced cardiomyocytes (Figure 3D and E), with equivalent kinetics in untreated GPCMs stimulated at 0.5Hz (Figure 3F, Online table III). The on and off rates of fluorescence differ in both myofilament localised indicators compared to the unrestricted RGECO. On rates were significantly slower (ΔT50 on = 47±5 and 39±4msec for RGECO-TnT and RGECO-TnI respectively), whilst off rates were significantly faster (ΔT50 off = -26±8 and -41±11msec for RGECO-TnT and RGECO-TnI respectively) than unrestricted RGECO (Online Table III). Interestingly, these rate differences are qualitatively preserved when RGECO-TnT emissions are compared to the chemical dye Fluo-4 (Online Figure V).
Figure 3. Characterisation of RGECO, RGECO-TnT and RGECO-TnI in GPCMs.
Adenovirally expressed RGECO-TnT and RGECO-TnI (red in the merged images) localises to the I band in confocal microscopy of GPCMs, whilst RGECO shows diffuse staining (n=4) (A); Z-disks are revealed by α-actinin staining (green in the merged images). Scale bar = 5μm. Intensity profile plots spanning two sarcomeres, α-actinin (green line) labels the z-disc, DsRed (red) labels the Ca2+ sensors. Western blot analysis of GPCMs transduced with RGECO-TnT (B) or RGECO-TnI (C) indicates that 54.3±5.5% (n=5)/58.7±11.0% (n=4), respectively, of Troponin is composed of RGECO conjugated Troponin. Raw Ca2+ transients of paced GPCMs transduced with RGECO-TnT (D) or RGECO-TnI (E). Averaged Ca2+ transients of 0.5Hz paced GPCMs transduced with RGECO, RGECO-TnT or RGECO-TnI (F) was used to compare Ca2+ transients between cytoplasmic RGECO and myofilament specific RGECO-TnT and RGECO-TnI.
To explore the sensitivity of RGECO-TnI/RGECO-TnT to detect changes in Ca2+ transient duration or magnitude that might be provoked by small molecules or disease causing mutations we performed a series of experiments with well annotated modifiers of cardiac physiology. To ensure changes in Ca2+ kinetics can be observed we used the reverse-rate dependence phenomenon that accompanies increasing frequency of electrical stimulation. All genetically encoded probes respond to increased pacing frequencies (0.5, 1 and 2 Hz) with increased speed of binding and release as the Ca2+ transient duration shortens (Online Figure VI). Since the lowest pacing frequency produces the longest Ca2+ transient, and maximizes experimental duration, we performed subsequent experiments at 0.5 Hz.
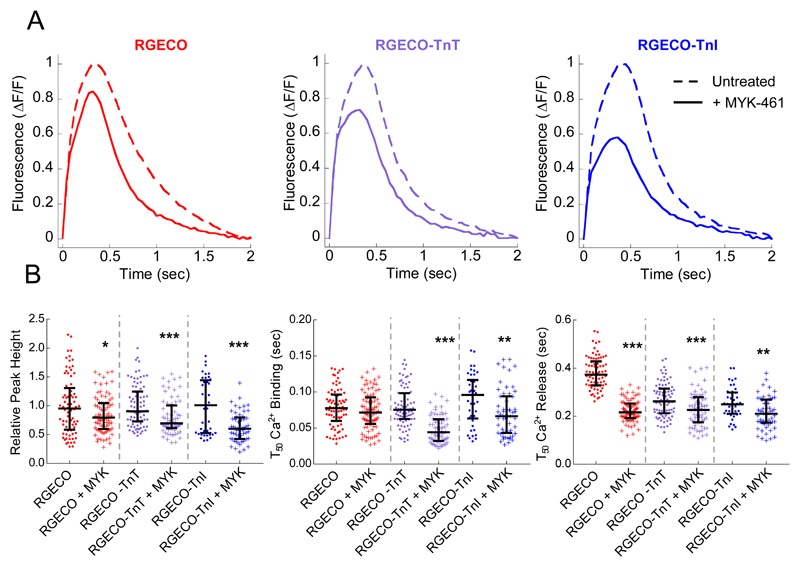
Small molecule effects on cytoplasmic and myofilament Ca2+ dynamics
To investigate the ability of RGECO-TnI/RGECO-TnT to detect localized changes in Ca2+ compared to an unrestricted sensor we used three small molecule modulators of myofilament contractility. MYK-461 was selected as a myosin ATPase inhibitor (Figure 4). Omecamtiv mecarbil, which increases the interaction between actin and myosin independently of Ca2+ was selected as a myosin activator (Figure 5), and finally, the inodilator levosimendan which stabilizes the Ca2+ bound form of TnC activating the myofilament (Figure 6). In agreement with previous observations48 omecamtiv mecarbil did not change any aspect of the Ca2+ transient with any probe (Figure 5). By contrast, peak amplitudes increase in the presence of levosimendan, and reduce in the presence of MYK-461. The myofilament restricted indicators report greater changes in peak amplitude ratio compared to the unrestricted control. The relative reductions in fluorescence conferred by MYK-461 were -9.5±3.8 %, -21.4±4.3% and -42.7±4.1% for RGECO, RGECO-TnT and RGECO-TnI respectively. Analogous increases in fluorescent amplitude following levosimendan treatment were +47.5±6.6%, +198.8±23.8% and +170.8±16.5% for RGECO, RGECO-TnT and RGECO-TnI respectively. Additionally, the myofilament localised RGECO reveals changes to the rate of Ca2+ binding and release in the presence of both MYK-461 and levosimendan contrasting with the results obtained with the cytoplasmic probe (Figure 4 and 6). Both myofilament restricted indicators in response to 250 nM MYK-461 and 10 μM levosimendan reduce the T50On times (RGECO-TnT -0.031±0.002 sec, -0.008±0.002 sec; RGECO-TnI -0.019±0.004 sec to -0.018±0.002 sec for MYK-461 and levosimendan respectively) whilst RGECO detects no change. Interestingly the unrestricted RGECO reports greater changes to T50Off compared to the restricted sensors (Figure 4, and 6), which might reflect hierarchical Ca2+ reuptake. Importantly, neither compound affects the intrinsic Ca2+ sensor function of RGECO-TnT (Online Figure VII).
Figure 4. The effects of MYK-461 on Ca2+ transient measurements in GPCMs with RGECO, RGECO-TnT or RGECO-TnI.
Averaged Ca2+ transients of 0.5 Hz paced GPCMs transduced with RGECO, RGECO-TnT or RGECO-TnI was used to compare the effects of 250nmol/L MYK-461 (A). Each comparison is made in paired experiments between drug treated (solid lines) and DMSO control treated (dashed lines) for RGECO infected (red), RGECO-TnT infected (purple) and RGECO-TnI infected (blue) cells. Dot plots for all extracted parameters are plotted in (B) (n=43-82 cells from n=3 isolations). Lines are median average and error bars are interquartile range, **= p<0.01 and ***= p<0.001 using an unpaired Mann-Whitney test comparing untreated to treated cells.
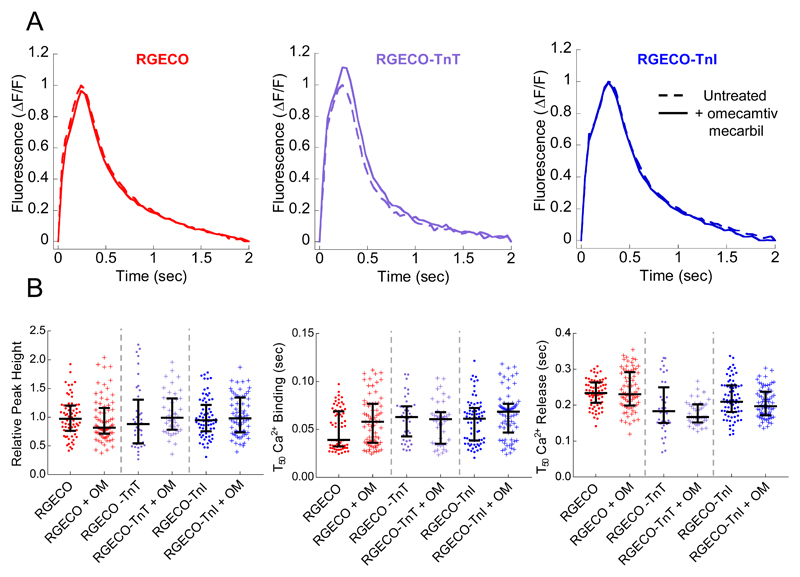
Figure 5. The effects of omecamtiv mecarbil on Ca2+ transient measurements in GPCMs with RGECO, RGECO-TnT or RGECO-TnI.
Averaged Ca2+ transients of 0.5Hz paced GPCMs transduced with RGECO, RGECO-TnT or RGECO-TnI was used to compare the effects 200nmol/L omecamtiv mecarbil (A). Each comparison is made in paired experiments between drug treated (solid lines) and DMSO control treated (dashed lines) for RGECO infected (red), RGECO-TnT infected (purple) and RGECO-TnI infected (blue) cells Dot plots for all extracted parameters are plotted in (B) (n=42-75 cells from n=3 isolations). Lines are median average and error bars are interquartile range, all groups were not significant using an unpaired Mann-Whitney test comparing untreated to treated cells.
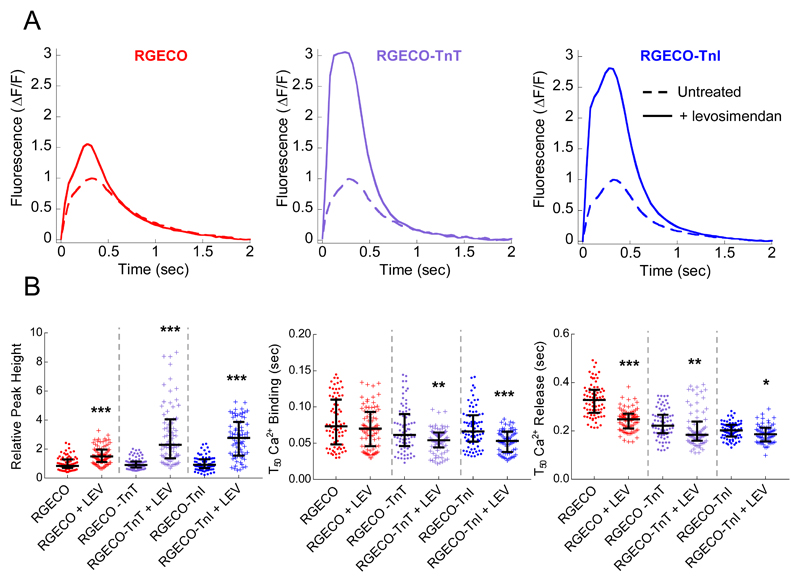
Figure 6. The effects of levosimendan on Ca2+ transient measurements in GPCMs with RGECO, RGECO-TnT or RGECO-TnI.
Averaged Ca2+ transients of 0.5Hz paced GPCMs transduced with RGECO, RGECO-TnT or RGECO-TnI was used to compare the effects 10μmol/L levosimendan (A). Each comparison is made in paired experiments between drug treated (solid lines) and DMSO control treated (dashed lines) for RGECO infected (red), RGECO-TnT infected (purple) and RGECO-TnI infected (blue) cells. Dot plots for all extracted parameters are plotted in (B) (n=71-83 cells from n=3 isolations). Lines are median average and error bars are interquartile range, *=p<0.05 **= p<0.01 and ***= p<0.001 using an unpaired Mann-Whitney test comparing untreated to treated cells.
Cytoplasmic and myofilament localised Ca2+ dynamics in HCM
Small molecule action in intact cells may include both on- and off-target components. Therefore, we explored whether the targeted RGECO strategy identified alterations in the calcium transient driven by HCM causing mutations, which should principally work through the myofilament. Specifically, previous contractility data suggests that peak amplitude should increase, and also phase shift by ~100 msec, however these have been undetectable with fura-28. Recombinant adenovirus expressing RGECO-TnT was used to study the effects of wild type (WT) cTnI or cTnI R145G expression; conversely, adenovirus expressing RGECO-TnI was used to observe the effects of WT cTnT or cTnT R92Q in GPCMs. The mutually exclusive expression of HCM mutant protein and sensor conjugate allows changes in Ca2+ flux to be attributed to the mutation independently of the consequence of the mutation itself.
Previously we showed a mutant transgene expression approach models autosomal dominant human HCM (~54% for cTnT R92Q and ~49% for cTnI R14510) and produces hypercontractility as a cellular manifestation of disease phenotype. Here, as we co-transduced separate adenoviruses containing the disease gene and the complementary Ca2+ indicator, adjustments to expression levels of singly verses doubly transduced cells required optimization of the multiplicities of infection (MOI), with subsequent western blot analysis to ensure doubly transduced cells had equivalent FLAG-tagged protein expression to singly transduced cells10 (Online Figure VIII). Immunolocalization experiments using DsRed and FLAG-tag antibodies to detect RGECO and HCM mutant troponin show no alterations to protein localization or sarcomeric structure as previously described10 (Online Figure IX).
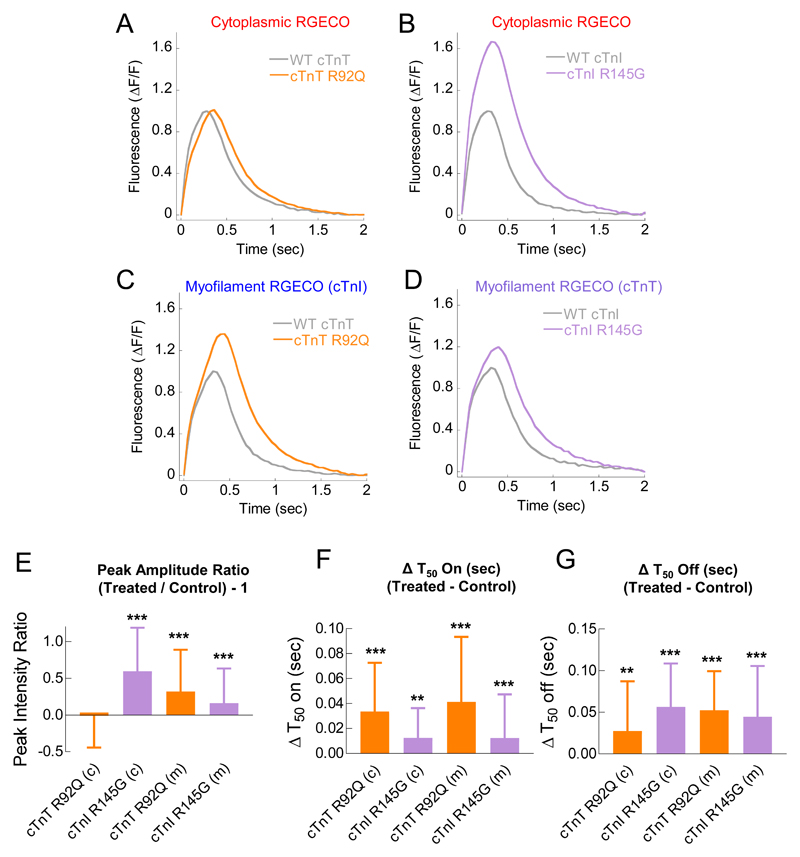
At the myofilament, compared to the WT control, both cTnT R92Q and cTnI R145G exert similar effects. The peak amplitude is delayed and elevated combined with slower T50 release times indicative of HCM causing thin filament mutations promoting more Ca2+ at the myofilament for longer intervals. Conversely, the whole cell indicator reports differential changes in peak systolic Ca2+ only for cTnI R145G, and no change in systolic Ca2+ for cTnT R92Q (Figure 7A-E, Online Table IV). The delay in time of peak Ca2+ correlates with previously published sarcomere length traces showing a delayed peak contraction time, which are overlooked by chemical dyes10. All indicator combinations detected increased time to 50% binding in both cTnT R92Q and cTnI R145G (Figure 7F, Online Table IV) and T50 release predicted (Online Table IV) from previous work measuring whole cell Ca2+ dynamics10.
Figure 7. Cytoplasmic and myofilament localised Ca2+ transients with adenovirally transduced cTnT R92Q and cTnI R145G.
Averaged Ca2+ transients of 0.5Hz paced GPCMs transduced with RGECO (A and B) or RGECO-TnI/RGECO-TnT (C and D) was used to compare Ca2+ transient effects between GPCMs transduced with either WT cTnT/cTnT R92Q (A and C), or WT cTnI/cTnI R145G (B and D). Peak amplitude ratio (E) and Δvalues for time to 50% binding (On) (F) and 50% release (Off) (G) are plotted including significance and labelled cytoplasmic (c) and myofilament (m) (n=94-124 cells from n=3 isolations). Error bars are SD, **= p<0.01 and ***= p<0.001 using a Mann-Whitney test comparing WT troponin to mutant troponin transduced cells.
Discussion
Here we show that a genetically encoded Ca2+ sensor, RGECO, can be targeted to the myofilament without perturbing contractility, or indicator function. This allows direct Ca2+ measurement in a key compartment of the cardiomyocyte historically studied indirectly. The availability of two targeted sensors, which are almost functionally equivalent, should facilitate studies of calcium handling at the myofilament in response to drugs or disease causing mutation.
GECIs applied to GPCMs reveal findings that contrast with calcium dyes. For example GECIs show the myosin ATPase inhibitor MYK-461 alters Ca2+ binding, release and signal amplitude, none of which were previously described in chemical dye studies30. Furthermore, myofilament targeting enhances the observed effect size when cardiomyocytes are treated with levosimendan. The mechanism of levosimendan action is debated, with a direct Ca2+ sensitizing effect meditated through TnC, a cAMP mediated effect through phosphodiesterase III inhibition49, and mitochondrial potassium channel activation50 all reported. While our data do not define the relative contributions, or the intermediates in the mode of action, they do show potent elevation of myofilament Ca2+ is combined with an increase in total cell Ca2+. The whole cell consequences are undesirable, and possibly attributable to off-target effects, as the R92Q-TnT mutant demonstrates that increased myofilament Ca2+ need not translate into increased whole cell Ca2+. Similarly, omecamtiv mecarbil48 alters contraction but does not change Ca2+ at the whole cell, or myofilament level in this model.
The myofilament restricted Ca2+ indicators reveal both cTnT R92Q and cTnI R145G HCM causing variants increase myofilament peak Ca2+ and delay release. Therefore the increased myofilament Ca2+ affinity common to both mutations8 directly correlates with increased microdomain [Ca2+]. This is compatible with previous work showing the same mutations increased myofilament Ca2+ buffering and altered [Ca2+] inferred by a rise in diastolic fura2 fluorescence10. The RGECO-TnI/TnT data contrast with results from the unrestricted RGECO indicator; where systolic peak intensity differences are observed only for cTnI R145G (a large increase) but not cTnT R92Q suggesting distinct consequences of these mutations. Since prior work excluded other factors such as fractional Ca2+ release from the SR10, the differences appear determined by what happens at the myofilament. This is mechanistically plausible as the cTnI R145G mutation directly increases Ca2+ binding to the regulatory site (I) of cTnC, whereas cTnT R92Q is structurally distant from the Ca2+ binding sites in the troponin complex and sensitizes myofilament Ca2+ binding via alterations to co-operative communication8. Furthermore previous studies show the cTnI R145G mutation has a greater effect on Ca2+ buffering than TnT R92Q (TnT R92Q ΔKd=582nmol/L, TnI R145G ΔKd=1082nmol/L compared to WT)10. We believe greater severity of the R145G mutation, which has a more pronounced contractility effect8, underpins the differential observations of changes to bulk Ca2+ with RGECO between the two mutants although exactly what makes the R145G cTnI mutation more severe is unknown. Interestingly a CRISPR engineered thick filament HCM iPS-CM model (MYH7 R453C) has raised peak systolic Ca2+ visualized by unrestricted RGECO51. From this we postulate that cytoplasmic Ca2+ increases could be a hallmark of some HCM causing mutations. This raises an important, potentially clinically significant, concept. HCM represents a common clinical end-point of many different mutations. There is an unmet need to understand the shared and distinct consequences of individual mutations. Common mechanisms central to disease pathogenesis may be preferable as therapeutic targets, but they may leave residual aspects of individual mutations untreated. The impact of this is currently uncertain, but we may gain insight in to this through trials such as EXPLORER investigating MYK-461 in HCM cohorts.
Ca2+ overload specifically at the myofilament is thought to activate hypertrophic signalling pathways as a component of the HCM disease mechanism13, 52, 53, however measuring this directly in living cells has remained elusive. This is the first study to not only show this occurs, but also that the phase shift in contractility is paralleled by a shift in the Ca2+ transient using any of the three protein indicators tested. These indicators simplify, and accelerate the process of studying Ca2+ dynamics at the myofilament without the need for multiple inferred observations of total and free Ca2+ using simultaneous patch clamping and chemical Ca2+ dyes10, 11, 20. Although the proteins used to detect Ca2+ are physically bulky and may have unmeasured effects on the intricate structure of the myofilament, or myofilament Ca2+ buffering capacity, contractile impairment is not seen in the GPCM transient expression model; this contrasts with the chemical dyes typically used to study Ca2+10, 54. A limitation of the RGECO indicators is their intensiometric nature, which precludes robust calibration allowing an observed signal to be converted to [Ca2+]. However, GECIs reveal changes in Ca2+ amplitude and kinetics that are overlooked with dye based probes. This opens a new investigative pathway in understanding this important microdomain within contractile cells which should be generally applicable to conditions affecting cardiac contractility and Ca2+ handling. They improve the fidelity of screening tools for small molecule evaluation in the heart.
Supplementary Material
Novelty and Significance.
What Is Known?
Hypertrophic cardiomyopathy (HCM) mutations and small molecule modulators of contractility alter how the cardiomyocyte handles calcium.
Historical methods to measure calcium at the myofilament are indirect because the chemical calcium dyes commonly used to visualise calcium are not possible to confine to subcellular regions.
An additional limitation of using chemical calcium dyes in this context is their reported attenuation of contractility.
What New Information Does This Article Contribute?
Calcium sensitive proteins, here we use RGECO, can be fused to two components of the thin filament (troponin I and troponin T) without adversely affecting the indicator, or native protein function, allowing calcium measurement from the sarcomere directly.
We find that in spite of their size and calcium binding, amino terminal fusions are well tolerated and do not alter contractility biochemically or in intact cells.
GECIs localised to the sarcomere detect changes to calcium amplitude or kinetics conferred by small molecules and HCM mutations that were not seen by traditional chemical calcium dyes or unrestricted GECIs that distribute throughout the cell.
We apply the virally delivered genetically encoded calcium indicators RGECO to measure beat-to-beat calcium transients in cardiomyocytes. By direct fusion to troponin I or troponin T, we have localised RGECO to measure calcium cycling within the contractile apparatus, where calcium is the master regulator of force production. Small molecule regulators of contractility (MYK-461, omecamtiv mecarbil and levosimendan) exert subtle changes to calcium at the myofilament which are more easily detected by these indicators working without the background noise coming from the whole cell. We find these tools increase our understanding of the mechanism by which HCM causing mutations alter microdomain calcium handling to drive disease state remodelling. Importantly the kinetic changes in contractility that arise in response to disease causing mutation are now mirrored by protein-based calcium indicators. Overall, our work has developed novel tools to study myofilament domain calcium directly without several of the limitations encountered in previous strategies. We hope this study will inform deeper mechanistic understanding of contractile aspects of cardiovascular disease and lead to broader uptake of genetically encoded indicators to study cardiovascular physiology.
Sources of Funding
This work was supported by the British Heart Foundation (Programme grant RG/12/16/29939 to HW and CR) and the British Heart Foundation Centre of Research Excellence (Oxford, RE/13/1/30181). Y-FC was supported by a pump priming grant from the British Heart Foundation Centre of Excellence award to Oxford University (RE/08/004/23915 and RE/13/1/30181). MJD is funded by the Wellcome Trust (WT098519MA) and the Japan Society for the Promotion of Science (JSPS) international joint research promotion program at Osaka University.
Nonstandard Abbreviations and Acronyms
- CaM
Calmodulin
- CaMKII
Ca2+/calmodulin dependant kinase II
- cAMP
Cyclic AMP
- GECI
Genetically encoded calcium indicator
- GFP
Green fluorescent protein
- GPCM
Guinea pig cardiomyocyte
- HCM
Hypertrophic cardiomyopathy
- MOI
Multiplicity of infection
- NCX
Sodium calcium exchanger
- PLN
Phospholamban
- TnC
Troponin C
- TnI
Troponin I
- TnT
Troponin T
- RyR
Ryanodine Receptor
- SERCA
Sarco-endoplasmic reticulum ATPase
- SR
Sarcoplasmic reticulum
- T50
Time to 50%
- WT
Wild Type
Footnotes
Disclosures
None.
References
- 1.Maron BJ, Gardin JM, Flack JM, Gidding SS, Kurosaki TT, Bild DE. Prevalence of hypertrophic cardiomyopathy in a general population of young adults. Echocardiographic analysis of 4111 subjects in the CARDIA Study. Coronary Artery Risk Development in (Young) Adults. Circulation. 1995;92:785–9. doi: 10.1161/01.cir.92.4.785. [DOI] [PubMed] [Google Scholar]
- 2.Watkins H, Ashrafian H, Redwood C. Inherited cardiomyopathies. N Engl J Med. 2011;364:1643–56. doi: 10.1056/NEJMra0902923. [DOI] [PubMed] [Google Scholar]
- 3.Walsh R, Buchan R, Wilk A, John S, Felkin LE, Thomson KL, Chiaw TH, Loong CCW, Pua CJ, Raphael C, Prasad S, et al. Defining the genetic architecture of hypertrophic cardiomyopathy: re-evaluating the role of non-sarcomeric genes. Eur Heart J. 2017;38:3461–3468. doi: 10.1093/eurheartj/ehw603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Redwood CS, Moolman-Smook JC, Watkins H. Properties of mutant contractile proteins that cause hypertrophic cardiomyopathy. Cardiovasc Res. 1999;44:20–36. doi: 10.1016/s0008-6363(99)00213-8. [DOI] [PubMed] [Google Scholar]
- 5.Knollmann BC, Kirchhof P, Sirenko SG, Degen H, Greene AE, Schober T, Mackow JC, Fabritz L, Potter JD, Morad M. Familial hypertrophic cardiomyopathy-linked mutant troponin T causes stress-induced ventricular tachycardia and Ca2+-dependent action potential remodeling. Circ Res. 2003;92:428–36. doi: 10.1161/01.RES.0000059562.91384.1A. [DOI] [PubMed] [Google Scholar]
- 6.Spindler M, Saupe KW, Christe ME, Sweeney HL, Seidman CE, Seidman JG, Ingwall JS. Diastolic dysfunction and altered energetics in the alphaMHC403/+ mouse model of familial hypertrophic cardiomyopathy. J Clin Invest. 1998;101:1775–83. doi: 10.1172/JCI1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kobayashi T, Solaro RJ. Increased Ca2+-affinity of cardiac thin filaments reconstituted with cardiomyopathy-related mutant cardiac troponin I. J Biol Chem. 2006;12:13471–7. doi: 10.1074/jbc.M509561200. [DOI] [PubMed] [Google Scholar]
- 8.Robinson P, Griffiths PJ, Watkins H, Redwood CS. Dilated and hypertrophic cardiomyopathy mutations in troponin and alpha-tropomyosin have opposing effects on the calcium affinity of cardiac thin filaments. Circ Res. 2007;101:1266–73. doi: 10.1161/CIRCRESAHA.107.156380. [DOI] [PubMed] [Google Scholar]
- 9.Adhikari AS, Kooiker KB, Sarkar SS, Liu C, Bernstein D, Spudich JA, Ruppel KM. Early-Onset Hypertrophic Cardiomyopathy Mutations Significantly Increase the Velocity, Force, and Actin-Activated ATPase Activity of Human beta-Cardiac Myosin. Cell Rep. 2016;17:2857–2864. doi: 10.1016/j.celrep.2016.11.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robinson P, Liu X, Sparrow A, Patel S, Zhang YH, Casadei B, Watkins H, Redwood C. Hypertrophic cardiomyopathy mutations increase myofilament Ca(2+) buffering, alter intracellular Ca(2+) handling, and stimulate Ca(2+)-dependent signaling. J Biol Chem. 2018;293:10487–10499. doi: 10.1074/jbc.RA118.002081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schober T, Huke S, Venkataraman R, Gryshchenko O, Kryshtal D, Hwang HS, Baudenbacher FJ, Knollmann BC. Myofilament Ca sensitization increases cytosolic Ca binding affinity, alters intracellular Ca homeostasis, and causes pause-dependent Ca-triggered arrhythmia. Circ Res. 2012;111:170–9. doi: 10.1161/CIRCRESAHA.112.270041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coppini R, Mazzoni L, Ferrantini C, Gentile F, Pioner JM, Laurino A, Santini L, Bargelli V, Rotellini M, Bartolucci G, Crocini C, et al. Ranolazine Prevents Phenotype Development in a Mouse Model of Hypertrophic Cardiomyopathy. Circ Heart Fail. 2017;10:e003565. doi: 10.1161/CIRCHEARTFAILURE.116.003565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davis J, Davis LC, Correll RN, Makarewich CA, Schwanekamp JA, Moussavi-Harami F, Wang D, York AJ, Wu H, Houser SR, Seidman CE, et al. A Tension-Based Model Distinguishes Hypertrophic versus Dilated Cardiomyopathy. Cell. 2016;165:1147–59. doi: 10.1016/j.cell.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Olivotto I, Cecchi F, Poggesi C, Yacoub MH. Developmental origins of hypertrophic cardiomyopathy phenotypes: a unifying hypothesis. Nat Rev Cardiol. 2009;6:317–21. doi: 10.1038/nrcardio.2009.9. [DOI] [PubMed] [Google Scholar]
- 15.Crilley JG, Boehm EA, Blair E, Rajagopalan B, Blamire AM, Styles P, McKenna WJ, Ostman-Smith I, Clarke K, Watkins H. Hypertrophic cardiomyopathy due to sarcomeric gene mutations is characterized by impaired energy metabolism irrespective of the degree of hypertrophy. J Am Coll Cardiol. 2003;41:1776–82. doi: 10.1016/s0735-1097(02)03009-7. [DOI] [PubMed] [Google Scholar]
- 16.Grynkiewicz G, Poenie M, Tsien RY. A new generation of Ca2+ indicators with greatly improved fluorescence properties. J Biol Chem. 1985;260:3440–50. [PubMed] [Google Scholar]
- 17.Kaestner L, Scholz A, Tian Q, Ruppenthal S, Tabellion W, Wiesen K, Katus HA, Muller OJ, Kotlikoff MI, Lipp P. Genetically encoded Ca2+ indicators in cardiac myocytes. Circ Res. 2014;114:1623–39. doi: 10.1161/CIRCRESAHA.114.303475. [DOI] [PubMed] [Google Scholar]
- 18.Ljubojevic S, Walther S, Asgarzoei M, Sedej S, Pieske B, Kockskamper J. In situ calibration of nucleoplasmic versus cytoplasmic Ca(2)+ concentration in adult cardiomyocytes. Biophys J. 2011;100:2356–66. doi: 10.1016/j.bpj.2011.03.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Broyles CN, Robinson P, Daniels MJ. Fluorescent, Bioluminescent, and Optogenetic Approaches to Study Excitable Physiology in the Single Cardiomyocyte. Cells. 2018;7:51. doi: 10.3390/cells7060051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Trafford AW, Diaz ME, Eisner DA. A novel, rapid and reversible method to measure Ca buffering and time-course of total sarcoplasmic reticulum Ca content in cardiac ventricular myocytes. Pflugers Arch. 1999;437:501–3. doi: 10.1007/s004240050808. [DOI] [PubMed] [Google Scholar]
- 21.Akerboom J, Carreras Calderon N, Tian L, Wabnig S, Prigge M, Tolo J, Gordus A, Orger MB, Severi KE, Macklin JJ, Patel R, et al. Genetically encoded calcium indicators for multi-color neural activity imaging and combination with optogenetics. Front Mol Neurosci. 2013;6:2. doi: 10.3389/fnmol.2013.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spudich JA. Hypertrophic and dilated cardiomyopathy: four decades of basic research on muscle lead to potential therapeutic approaches to these devastating genetic diseases. Biophys J. 2014;106:1236–49. doi: 10.1016/j.bpj.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paul DM, Morris EP, Kensler RW, Squire JM. Structure and orientation of troponin in the thin filament. J Biol Chem. 2009;284:15007–15. doi: 10.1074/jbc.M808615200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Surdo NC, Berrera M, Koschinski A, Brescia M, Machado MR, Carr C, Wright P, Gorelik J, Morotti S, Grandi E, Bers DM, et al. FRET biosensor uncovers cAMP nano-domains at beta-adrenergic targets that dictate precise tuning of cardiac contractility. Nat Commun. 2017;8 doi: 10.1038/ncomms15031. 15031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mank M, Reiff DF, Heim N, Friedrich MW, Borst A, Griesbeck O. A FRET-based calcium biosensor with fast signal kinetics and high fluorescence change. Biophys J. 2006;90:1790–6. doi: 10.1529/biophysj.105.073536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mank M, Santos AF, Direnberger S, Mrsic-Flogel TD, Hofer SB, Stein V, Hendel T, Reiff DF, Levelt C, Borst A, Bonhoeffer T, et al. A genetically encoded calcium indicator for chronic in vivo two-photon imaging. Nat Methods. 2008;5:805–11. doi: 10.1038/nmeth.1243. [DOI] [PubMed] [Google Scholar]
- 27.Henderson MJ, Baldwin HA, Werley CA, Boccardo S, Whitaker LR, Yan X, Holt GT, Schreiter ER, Looger LL, Cohen AE, Kim DS, et al. A Low Affinity GCaMP3 Variant (GCaMPer) for Imaging the Endoplasmic Reticulum Calcium Store. PLoS One. 2015;10:e0139273. doi: 10.1371/journal.pone.0139273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Despa S, Shui B, Bossuyt J, Lang D, Kotlikoff MI, Bers DM. Junctional cleft [Ca(2)(+)]i measurements using novel cleft-targeted Ca(2)(+) sensors. Circ Res. 2014;115:339–47. doi: 10.1161/CIRCRESAHA.115.303582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pollesello P, Papp Z, Papp JG. Calcium sensitizers: What have we learned over the last 25 years? Int J Cardiol. 2016;203:543–8. doi: 10.1016/j.ijcard.2015.10.240. [DOI] [PubMed] [Google Scholar]
- 30.Green EM, Wakimoto H, Anderson RL, Evanchik MJ, Gorham JM, Harrison BC, Henze M, Kawas R, Oslob JD, Rodriguez HM, Song Y, et al. A small-molecule inhibitor of sarcomere contractility suppresses hypertrophic cardiomyopathy in mice. Science. 2016;351:617–21. doi: 10.1126/science.aad3456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Papp Z, Edes I, Fruhwald S, De Hert SG, Salmenpera M, Leppikangas H, Mebazaa A, Landoni G, Grossini E, Caimmi P, Morelli A, et al. Levosimendan: molecular mechanisms and clinical implications: consensus of experts on the mechanisms of action of levosimendan. Int J Cardiol. 2012;159:82–7. doi: 10.1016/j.ijcard.2011.07.022. [DOI] [PubMed] [Google Scholar]
- 32.Watkins H, McKenna WJ, Thierfelder L, Suk HJ, Anan R, O'Donoghue A, Spirito P, Matsumori A, Moravec CS, Seidman JG, et al. Mutations in the genes for cardiac troponin T and alpha-tropomyosin in hypertrophic cardiomyopathy. N Engl J Med. 1995;332:1058–64. doi: 10.1056/NEJM199504203321603. [DOI] [PubMed] [Google Scholar]
- 33.Thierfelder L, Watkins H, MacRae C, Lamas R, McKenna W, Vosberg HP, Seidman JG, Seidman CE. Alpha-tropomyosin and cardiac troponin T mutations cause familial hypertrophic cardiomyopathy: a disease of the sarcomere. Cell. 1994;77:701–12. doi: 10.1016/0092-8674(94)90054-x. [DOI] [PubMed] [Google Scholar]
- 34.Elliott K, Watkins H, Redwood CS. Altered regulatory properties of human cardiac troponin I mutants that cause hypertrophic cardiomyopathy. J Biol Chem. 2000;275:22069–74. doi: 10.1074/jbc.M002502200. [DOI] [PubMed] [Google Scholar]
- 35.Kimura A, Harada H, Park JE, Nishi H, Satoh M, Takahashi M, Hiroi S, Sasaoka T, Ohbuchi N, Nakamura T, Koyanagi T, et al. Mutations in the cardiac troponin I gene associated with hypertrophic cardiomyopathy. Nat Genet. 1997;16:379–82. doi: 10.1038/ng0897-379. [DOI] [PubMed] [Google Scholar]
- 36.Michele DE, Albayya FP, Metzger JM. Direct, convergent hypersensitivity of calcium-activated force generation produced by hypertrophic cardiomyopathy mutant alpha-tropomyosins in adult cardiac myocytes. Nat Med. 1999;5:1413–7. doi: 10.1038/70990. [DOI] [PubMed] [Google Scholar]
- 37.Ellingsen O, Davidoff AJ, Prasad SK, Berger HJ, Springhorn JP, Marsh JD, Kelly RA, Smith TW. Adult rat ventricular myocytes cultured in defined medium: phenotype and electromechanical function. Am J Physiol. 1993;265:H747–54. doi: 10.1152/ajpheart.1993.265.2.H747. [DOI] [PubMed] [Google Scholar]
- 38.Robinson P, Mirza M, Knott A, Abdulrazzak H, Willott R, Marston S, Watkins H, Redwood C. Alterations in thin filament regulation induced by a human cardiac troponin T mutant that causes dilated cardiomyopathy are distinct from those induced by troponin T mutants that cause hypertrophic cardiomyopathy. J Biol Chem. 2002;277:40710–6. doi: 10.1074/jbc.M203446200. [DOI] [PubMed] [Google Scholar]
- 39.Pardee JD, Spudich JA. Purification of muscle actin. Methods Cell Biol. 1982;24:271–89. doi: 10.1016/s0091-679x(08)60661-5. [DOI] [PubMed] [Google Scholar]
- 40.Weeds AG, Taylor RS. Separation of subfragment-1 isoenzymes from rabbit skeletal muscle myosin. Nature. 1975;257:54–6. doi: 10.1038/257054a0. [DOI] [PubMed] [Google Scholar]
- 41.Zhao Y, Araki S, Wu J, Teramoto T, Chang YF, Nakano M, Abdelfattah AS, Fujiwara M, Ishihara T, Nagai T, Campbell RE. An expanded palette of genetically encoded Ca(2)(+) indicators. Science. 2011;333:1888–91. doi: 10.1126/science.1208592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Simon JN, Chowdhury SA, Warren CM, Sadayappan S, Wieczorek DF, Solaro RJ, Wolska BM. Ceramide-mediated depression in cardiomyocyte contractility through PKC activation and modulation of myofilament protein phosphorylation. Basic Res Cardiol. 2014;109:445. doi: 10.1007/s00395-014-0445-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chang YF, Broyles CN, Brook FA, Davies MJ, Turtle CW, Nagai T, Daniels MJ. Non-invasive phenotyping and drug testing in single cardiomyocytes or beta-cells by calcium imaging and optogenetics. PLoS One. 2017;12:e0174181. doi: 10.1371/journal.pone.0174181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hilliard FA, Steele DS, Laver D, Yang Z, Le Marchand SJ, Chopra N, Piston DW, Huke S, Knollmann BC. Flecainide inhibits arrhythmogenic Ca2+ waves by open state block of ryanodine receptor Ca2+ release channels and reduction of Ca2+ spark mass. J Mol Cell Cardiol. 2010;48:293–301. doi: 10.1016/j.yjmcc.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mosqueira D, Mannhardt I, Bhagwan JR, Lis-Slimak K, Katili P, Scott E, Hassan M, Prondzynski M, Harmer SC, Tinker A, Smith JGW, et al. CRISPR/Cas9 editing in human pluripotent stem cell-cardiomyocytes highlights arrhythmias, hypocontractility, and energy depletion as potential therapeutic targets for hypertrophic cardiomyopathy. Eur Heart J. 2018;39:3879–3892. doi: 10.1093/eurheartj/ehy249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fabiato A, Fabiato F. Effects of pH on the myofilaments and the sarcoplasmic reticulum of skinned cells from cardiace and skeletal muscles. J Physiol. 1978;276:233–55. doi: 10.1113/jphysiol.1978.sp012231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Griffiths EJ. Calcium handling and cell contraction in rat cardiomyocytes depleted of intracellular magnesium. Cardiovasc Res. 2000;47:116–23. doi: 10.1016/s0008-6363(00)00061-4. [DOI] [PubMed] [Google Scholar]
- 48.Malik FI, Hartman JJ, Elias KA, Morgan BP, Rodriguez H, Brejc K, Anderson RL, Sueoka SH, Lee KH, Finer JT, Sakowicz R, et al. Cardiac myosin activation: a potential therapeutic approach for systolic heart failure. Science. 2011;331:1439–43. doi: 10.1126/science.1200113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Orstavik O, Ata SH, Riise J, Dahl CP, Andersen GO, Levy FO, Skomedal T, Osnes JB, Qvigstad E. Inhibition of phosphodiesterase-3 by levosimendan is sufficient to account for its inotropic effect in failing human heart. Br J Pharmacol. 2014;171:5169–81. doi: 10.1111/bph.12647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kopustinskiene DM, Pollesello P, Saris NE. Levosimendan is a mitochondrial K(ATP) channel opener. Eur J Pharmacol. 2001;428:311–4. doi: 10.1016/s0014-2999(01)01350-4. [DOI] [PubMed] [Google Scholar]
- 51.Mosqueira D, Mannhardt I, Bhagwan JR, Lis-Slimak K, Katili P, Scott E, Hassan M, Prondzynski M, Harmer SC, Tinker A, Smith JGW, et al. CRISPR/Cas9 editing in human pluripotent stem cell-cardiomyocytes highlights arrhythmias, hypocontractility, and energy depletion as potential therapeutic targets for hypertrophic cardiomyopathy. Eur Heart J. 2018 doi: 10.1093/eurheartj/ehy249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fatkin D, McConnell BK, Mudd JO, Semsarian C, Moskowitz IG, Schoen FJ, Giewat M, Seidman CE, Seidman JG. An abnormal Ca(2+) response in mutant sarcomere protein-mediated familial hypertrophic cardiomyopathy. J Clin Invest. 2000;106:1351–9. doi: 10.1172/JCI11093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tardiff JC. The Role of Calcium/Calmodulin-Dependent Protein Kinase II Activation in Hypertrophic Cardiomyopathy. Circulation. 2016;134:1749–1751. doi: 10.1161/CIRCULATIONAHA.116.025455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Smith NA, Kress BT, Lu Y, Chandler-Militello D, Benraiss A, Nedergaard M. Fluorescent Ca(2+) indicators directly inhibit the Na,K-ATPase and disrupt cellular functions. Sci Signal. 2018;11:eaal2039. doi: 10.1126/scisignal.aal2039. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.