Abstract
Objective
Young adulthood is a crucial neurodevelopmental period during which impulsive and compulsive problem behaviours commonly emerge. While traditionally considered diametrically opposed, impulsive and compulsive symptoms tend to co-occur. The objectives of this study were: (i) to identify the optimal trans-diagnostic structural framework for measuring impulsive and compulsive problem behaviours; and (ii) to use this optimal framework to identify common/distinct antecedents of these latent phenotypes.
Methods
654 young adults were recruited as part of the Neuroscience in Psychiatry Network (NSPN), a population-based cohort in the United Kingdom. The optimal trans-diagnostic structural model capturing 33 types of impulsive and compulsive problem behaviours was identified. Baseline predictors of subsequent impulsive and compulsive trans-diagnostic phenotypes were characterised, along with cross-sectional associations, using Partial Least Squares (PLS).
Results
Current problem behaviours were optimally explained by a bi-factor model, which yielded dissociable measures of impulsivity and compulsivity, as well as a general disinhibition factor. Impulsive problem behaviours were significantly explained by prior antisocial and impulsive personality traits, male gender, general distress, perceived dysfunctional parenting, and teasing/arguments within friendships. Compulsive problem behaviours were significantly explained by prior compulsive traits, and female gender.
Conclusions
This study demonstrates that trans-diagnostic phenotypes of 33 impulsive and compulsive problem behaviours are identifiable in young adults, utilizing a bi-factor model based on responses to a single questionnaire. Furthermore, these phenotypes have different antecedents. The findings yield a new framework for fractionating impulsivity and compulsivity; and suggest different early intervention targets to avert emergence of problem behaviours. This framework may be useful for future biological and clinical dissection of impulsivity and compulsivity.
Introduction
Young adults are particularly vulnerable to develop maladaptive, problem, behaviours (Spear, 2000). This vulnerability is thought to stem from neurodevelopmental alterations (Casey et al., 2017) coupled with concomitant changes in the environment (such as lessening parental oversight and increasing exposure to new peer groups). Two key concepts of particular relevance to understanding brain development and problem behaviours in young adulthood are ‘impulsivity’ and ‘compulsivity’ (Hollander et al., 2009). Impulsivity refers to behaviours that are unduly hasty, risky, and that lead to negative outcomes in the long term (Evenden, 1999). Examples of clinical disorders characterised by impulsivity include antisocial personality disorder, gambling disorder, and substance use disorders, e.g. (Krmpotich et al., 2015). Thus an individual may undertake a spontaneous aggressive act (as in antisocial personality disorder), or may crave and consume a substance (or engage in a gambling opportunity), without due regard to potentially damaging consequences. Compulsivity, by contrast, refers to functionally impairing behaviours undertaken repeatedly, often according to rigid rules, manifesting classically in obsessive-compulsive disorder (OCD). Impulsive and compulsive problems are common in young adulthood, have negative effects on long-term outcomes, and frequently co-occur (Fineberg et al., 2013; Cerda et al., 2016; Black et al., 2017).
Mechanistic, diagnostic, and treatment progress in psychiatry has been hindered by an excessive focus on specific mental disorders, typically examined in isolation within clinical settings rather than a continuous or dimensional fashion in the population at large (Cuthbert and Insel, 2013). Intermediate phenotypes (trans-diagnostic markers) hold promise in this regard, and should be measurable along a continuum in the background population, existing in more extreme forms in people with conceptually related mental disorders. Recent reports from population-based studies have suggested that trans-diagnostic phenotypes are indeed likely (St Clair et al., 2017; Stochl et al., 2015). Thus, a crucial next step in impulsivity-compulsivity research and practice is to identify intermediate phenotypes that cut across related problem behaviours, and that are measurable dimensionally both in the general population and in the context of existing categories of mental disorders.
Recent cross-sectional studies have shown that variation in a broad range of impulsive and compulsive behaviours is also present sub-clinically, and that these behaviours can be grouped into latent dimensions of ‘impulsivity’ and ‘compulsivity’ (termed intermediate phenotypes), which are found to be positively correlated (Chamberlain et al., 2017; Guo et al., 2017). This positive correlation could reflect common underpinnings; but also, could theoretically stem from common measurement bias (cross-talk across scale items due to item response bias). It is important to identify an optimal framework within which to conceptualize separable impulsive and compulsive problem behaviours as this could then be used to explore common or distinct antecedents. A recent resurgence of interest in bi-factor models in psychiatry (Reise, 2012b; St Clair et al., 2017), has yet to be adequately deployed and tested in latent phenotyping studies of impulsivity and compulsivity (Chamberlain et al., 2017; Guo et al., 2017). Such bi-factor models incorporate a general factor (capturing common variance across all study measures), as well as specific factors, enabling – theoretically – these constructs to be truly fractionated statistically.
The aims of the current study, were: (i) to identify the optimal trans-diagnostic structural framework for measuring impulsive and compulsive problem behaviours (including consideration of a bi-factor model); and (ii) to use this optimal framework to identify longitudinal antecedents of these latent phenotypes for the first time, with a particular focus on demographic, personality, parenting, and friendship measures. We focused on these measures as they were expected to contribute to subsequent problems, based on prior evidence. The optimal conceptual framework was identified using a competing models approach; and relationships between trans-diagnostic phenotypes and other measures were elicited using the innovative statistical approach of Partial Least Squares, which is well-suited for data likely to be correlated and non-normally distributed (Abdi and Williams, 2013).
Method
Participants
We contacted all individuals from the Neuroscience in Psychiatry Network (NSPN), a longitudinal population-based cohort study examining brain development (Kiddle et al., 2017), via email. Participants completed an online survey implemented in SurveyMonkey in 2018 and had also provided baseline questionnaires via the post (2012-2014). The current data collection (2018) examined a broader range of impulsivity/compulsivity measures, some of which were not available at the time the NSPN cohort was conceived (Chamberlain and Grant, 2018; Guo et al., 2017). The study was approved by Research Ethics Committee and individuals provided informed consent. Participants were given a £15 voucher for taking part.
Measures of interest
Questionnaires collected presently (2018) were designed to capture relevant demographic characteristics (age, gender, ethnic group, level of education), trans-diagnostic measures of problem behaviours, and other relevant measures of impulsivity and compulsivity; plus overall quality of life. The outcome instrument of interest, used to examine underlying latent phenotypes of impulsive and compulsive problem behaviours, was the Impulsive-Compulsive Behaviours Checklist (ICBC) (Guo et al., 2017), which is described in more detail below. Other measures of interest collected in the current data round (2018) and at participant recruitment (2012-2014) are described in Table 1. The latter included measures of impulsive-compulsive tendencies, but also parenting, and friendships, which we expected may impact the ultimate expression of the latent phenotypes on the ICBC. Additionally, the following demographic information was examined, which was completed by the participant’s parent or legal guardian at study baseline: any perinatal complications in proband (yes/no), any history of head trauma in proband (yes/no), family educational level (parent/guardian’s number of years’ education completed), and any current or previous emotional/behavioural/mental health problem in the proband (yes/no).
Table 1. Summary of instruments included in the study.
| Instrument | Description | Outcome measure(s) |
|---|---|---|
| Measures collected in current data round | ||
| Barratt Impulsiveness Scale (BIS-11 Brief version) (Stanford et al., 2016; Steinberg et al., 2013) | Barratt Impulsiveness Scale (BIS-11 Brief version). The BIS is an extensively used scale used for the classic measurement of impulsivity. We used the 8-item version, which has been previously validated in several studies. The questionnaire asks about impulsive tendencies and behaviours; for each item, the individual indicates the extent to which it applies to them (not at all, a little, quite a lot, or very much; scored 0-4 per item) | Total score |
| Antisocial personality disorder symptoms (American Psychiatric Association, 2013) | Antisocial personality disorder symptoms were quantified using a tick-list of DSM-5 criteria. For each symptom criterion, participants indicated whether the item applied to them or not | Total number of criteria endorsed |
| Padua obsessive-compulsive inventory (Washington State University Revision version) (Sanavio, 1988; Burns, 1995) | This is a 39-item questionnaire measuring obsessive-compulsive symptoms in normative and clinical settings | Symptom domain scores (per Burns et al.) |
| Cambridge-Chicago Trait Compulsivity Scale (CHIT) (Chamberlain and Grant, 2018) | This is a 15-item scale capturing day-to-day aspects of compulsivity. For each item, the individual indicates whether the statement (e.g. “I hate leaving a task unfinished”) applies to them. Response options are: strongly disagree (0), disagree (1), agree (2), or strongly agree (3) | Total score |
| Obsessive Beliefs Questionnaire Short Form (OBQ) (Moulding et al., 2011) | This is a 20-item short version of a widely used questionnaire to assess obsessional beliefs in the context of OCD. For each item, the person indicates how much they agree with a given statement, ranging from disagree very much (scored 1) to agree very much (7). | Summary scores: threat perception, perfection/intolerance of uncertainty, inflated responsibility, and importance/control of thoughts |
| Obsessive-Compulsive Personality Disorder traits (OCPD) (American Psychiatric Association, 2013; Sheehan et al., 1998) | The diagnostic screening questions from the Mini-International Neuropsychiatric Inventory (MINI) were used for OCPD traits. For each item, participants were asked whether the statement applied to them, taking into consideration not only their own view but also what they felt other people (close confidantes) would think | Total number of OCPD traits endorsed |
| General psychopathology (depression/anxiety) from the Mini-International Neuropsychiatric Inventory (MINI) (Sheehan et al., 1998) | General psychopathology (depression/anxiety). The diagnostic screening questions from the Mini-International Neuropsychiatric Inventory (MINI) were used for depressive and anxiety disorders | Presence or depressive and/or anxiety symptoms (total items endorsed) |
| Brunnsviken Brief Quality of life scale (BBQ) (Lindner et al., 2016) | The BBQ is a previously validated self-report quality of life scale, which covers six life areas (leisure time, view of life, creativity, learning, friends/friendship, and view of self) that are important determinants of overall quality of life. This scale has been validated in various normative and clinical population settings | Total quality of life score |
| Measures collected at study baseline (2012-2014) | ||
| Barratt Impulsiveness Scale (BIS 11 full version) (Patton et al., 1995) |
This question asks about impulsive tendencies and behaviours; for each, the individual indicates the extent to which it applies to them (not at all, a little, quite a lot, or very much; scored 0-4 per item) |
Total score |
| The Antisocial Process Screening Device (APSD) (Munoz and Frick, 2007) |
This is a 20-item questionnaire developed to assess psychopathy in young people. For each item, the individual indicates whether a given statement (e.g. “You engage in illegal activities”) is not true at all (0), sometimes true (1), or definitely true (2) |
Total score |
| Padua obsessive-compulsive inventory (Washington State University Revision version) (Sanavio, 1988; Burns, 1995) |
Per current data round |
Per current data round |
| General psychopathology (K10) (Kessler et al., 2002) |
The K10 was developed for assessment of generalised psychological distress, including distress arising from anxiety and depression symptoms. There are ten items each asking about experiences over the preceding 30 days. For each item, responses are: none of the time (0), a little of the time (1), some of the time (2), most of the time (3), or all of the time (4) |
Total score |
| Family Assessment Device (FAD) (Ridenour et al., 1999), Positive Parenting Questionnaire (PPQ), Alabama Parenting questionnaire Child Short Form (APQ) (Elgar et al., 2007) and Measure of Parenting style (MOPs) (Parker et al., 1997) |
Several complementary questionnaires relating to parenting approaches were included. The reader is referred to the cited manuscripts for more detailed descriptions of these instruments, except for the PPQ, which was developed bespoke for the NPSN study. The PPQ asks the extent to which each of 26 positively worded items related to one’s family when living at home (e.g. “We spent quality time together.”; “If I was angry, I was still listened to.”) Each item is responded to with always (scored 0), mostly (1), sometimes (2), or rarely (3). Exploratory Factor Analysis (EFA) was used to identify the optimal data structure across all these questionnaires’ items considered collectively (Supplementary Table 2) |
Factor scores: general parenting, dysfunctional parenting (paternal side), and dysfunctional parenting (maternal side) |
| Friendship questionnaire (Goodyer et al., 1997; van Harmelen et al., 2017) |
This questionnaire assesses the number, availability and adequacy of friendships as well as self-disclosure and difficulties in friendships, and was adapted from previous research work. The individual questions were: are you happy with the number of friends you have? How often do you arrange to see friends other than at school, college or work? Do you feel that your friends understand you? Can you confide in your friends? Do your friends ever laugh at you or tease you in a hurtful way? Do people who aren’t your friends laugh at you or tease you in a hurtful way? Do you have arguments with your friends that upset you? Overall, how happy are you with your friendships? Item response options differed depending on the question but involved 4-6 possible responses (for example, for the question “Do you feel that your friends understand you?”, the response options were most of the time, sometimes, not often, or not at all, which were scored 0, 1, 2, or 3 respectively). Exploratory Factor Analysis (EFA) was used to determine the latent structure of the questionnaire (Supplementary Table 3). |
Factor scores: happiness/number of friends, confiding/understanding, and teasing/arguments |
The ICBC enquires about the presence of 33 types of impulsive and compulsive problem behaviours; for each type of behaviour, the individual endorses whether they and/or others think they have a problem with the behaviour, responding: never, sometimes, often, or always. The behaviours asked about by the ICBC are as follows: washing, smoking, feeling compelled to collect things, being overly cautious with money, re-arranging/ordering, shopping, list making, counting (e.g. money, tiles), grooming, idiosyncratic routines (performing a very personalised sequence of actions), repeating actions (over and over again), exercising, betting/gambling, hair pulling, lying, sexual activities/behaviours, alcohol consumption, planning (e.g. over-organising), illicit drug use, cleaning too much, verbal aggression, violence towards objects/properties, swearing, checking (e.g. locks, light switches), checking (e.g. yourself in the mirror), speed driving, medication use, physical aggression, social networking (e.g. Facebook, twitter, Google+, Myspace), applying rules, purposeful self-injury (i.e. not accidental), re-writing/re-reading, and tattooing. Previous work found the scale to have sound psychometric properties (Guo et al., 2017).
Data analysis
All data analyses were conducted using JMP Pro Version 13.2.0 (SAS Institute Inc.) and Mplus 7.2 (Muthén and Muthén, 1998 - 2012). The latent factor structure of the Impulsive-Compulsive Behaviours Checklist (ICBC, the outcome instrument of interest) was examined using Confirmatory Factor Analysis (CFA) of the covariance matrix using the Weighted Least Squares Means and Variance (WLSMV) adjusted estimator and Theta parameterisation (Muthén et al., 1997; Muthén and Muthén, 1998 - 2012). Based on prior studies and existing conceptual frameworks (Guo et al., 2017; Chamberlain et al., 2017; Reise, 2012a) we evaluated: a correlated two-factor model (two latent factors, i.e. impulsivity and compulsivity, correlated with each other), an orthogonal two-factor model (two latent factors, i.e. impulsivity and compulsivity, not correlated with each other), a one-factor model (one latent factor, corresponding to disinhibition), and a bi-factor model (two latent factors, i.e. impulsivity and compulsivity, plus a general factor). Post hoc model fitting was conducted by freeing theoretically plausible error covariances for estimation one at a time with reference to the highest modification index and these were corrected for significance using the Benjamini-Hochberg False Discovery Rate (.05). Test of exact model fit using the chi square test statistic (χ2) is overly sensitive to minor model misspecification in large sample sizes (Kline, 2016). Model fit was therefore evaluated using a combination of comparative fit indices, including the Root Mean Square Error of Approximation (RMSEA) (ε < .05 close approximate fit; ε = .05 - .08 reasonable approximate fit; ε = > 1.0 not close approximate fit); Comparative Fit Index (CFI) (> .90 reasonable fit; >.95 good fit); and the Weighted Root Mean Residual (WRMR) (<.950 good fit). We used a competing models approach, in which the comparative fit of several alternative models were evaluated to determine which provided the best representation of the covariances in the data.
Relationships between explanatory variables of interest and current impulsive-compulsive behaviours (latent scores on the ICBC) were investigated in two separate statistical models: the first examined baseline explanatory variables collected at study entry approximately (on average) 4 years prior; and the second model examined current explanatory variables (the broader range of impulsive and compulsive measures collected via the Internet in 2018). The statistical method of Partial Least Squares (PLS) was used. PLS is a versatile multivariate approach to data modelling that analyses relationships between exploratory (X) variables and outcome (Y) variables by means of fitting one or more latent components (Abdi and Williams, 2013). Unlike standard regression, PLS is robust to violations of normality assumptions and to item cross-correlations. Hence PLS is ideally suited to the current dataset. Candidate explanatory (X) variables in the PLS models were summary scores from the questionnaires, and the outcome variables of interest (Y) were the ICBC latent scores.
For the model exploring baseline predictors of later impulsive and compulsive problem behaviours, the X variables of interest were: age at baseline, gender, ethnic group, family education level (average years’ education for main caregiver), current or past mental health or behavioural problem (parent/guardian report), history of head trauma (parent/guardian report), history of any medical conditions (parent/guardian report), Barratt Impulsiveness Scale scores, antisocial personality total scores, Padua Inventory obsessive-compulsive scores, general psychopathology (K10 scores, including anxiety/depression), parenting scores (general parenting, dysfunctional paternal parenting, and dysfunctional maternal parenting), and friendship scores (happiness/number, confiding/understanding, and teasing/arguments). For the model exploring current measures potentially associated with problem behaviours, X variables of interest were: age, gender, education level, ethnic group, Barratt Impulsivity Scale scores, antisocial personality disorder traits (number of diagnostic criteria met), Padua Inventory obsessive-compulsive scores, OBQ scores, CHIT compulsivity scores, OCPD traits (number of OCPD criteria met), and general psychopathology (presence of depression or anxiety symptoms).
For PLS, missing data points were imputed automatically by JMP software using mean substitution. The PLS models were fitted using leave-one-out cross-validation (non-linear iterative partial least squares, NIPALS algorithm), and the optimal model was identified based on minimizing predictive residual sum of the squares (PRESS). From each initial model, measures with a Variable Importance Parameter (VIP) <0.8 were excluded per convention (Cox and Gaudard, 2013). Explanatory (X) variables significantly contributing to the model (i.e., explaining significant variance in current compulsive and impulsive problem behaviours) were identified on the basis of 95% confidence intervals for bootstrap distribution of the standardised model coefficients not crossing zero (N = 1000 bootstraps; p<0.05).
Results
Six-hundred and fifty-four individuals completed the study. The mean (standard deviation) current age was 23.4 (3.2) years, and 34.7% were males. The current Barratt Impulsiveness Scale (BIS-11 short) mean total score was 16.4 (3.9) and the Padua Inventory mean score was 19.0 (19.1). Participants had returned their baseline data to NSPN on average 4.0 (1.3) years prior to participation in the current study, and were of mean age 19.5 (3.1) years at baseline.
The majority of individuals (354 [53.2%]) endorsed having at least one problem behaviour in the preceding 12 months to some degree, on the ICBC (Supplementary Table 1). A bi-factor model consisting of a general latent ‘Disinhibition’ factor with loadings from all 33 ICBC items and two specific factors capturing residual variance in 14 impulsivity (“Impulsivity”) and 11 compulsivity items (“Compulsivity”) provided the best overall fit to the ICBC data compared to three competing models (Table 2). The loadings of individual behaviours onto the latent factors are shown in Table 3, and the model had had excellent fit (Reise, 2012b). Bi-factor models have a tendency to provide superior fit compared to correlated factors and indirect hierarchical models because they have more parameters (Bonifay et al., 2017). Model diagnostics, including measures of construct replicability, reliability, and unidimensionality were conducted to ensure the general and group factors were capturing meaningful covariances in the data and were not simply a product of overfitting (Rodriguez et al., 2016b). Construct replicability was evaluated by calculating the H index for the Disinhibition (.95), Impulsivity (.83), and Compulsivity (.69) factors, which ranges from 0 – 1 and quantifies the proportion of variance in a factor captured by its indicator variables (Hancock and Mueller, 2001). The results indicate that the strength of the standardised loadings for ICBC items on the latent factors were strong enough to suggest moderate-high replicability across studies using the same measures (Hancock and Mueller, 2001; Rodriguez et al., 2016b).
Table 2. Summary of Fit Statistics for the Different Competing Confirmatory Factor Analysis Models of the Impulsive Compulsive Behaviour Checklist (ICBC) in the NSPN Cohort.
| Model | df | χ2 | p | RMSEA (90%CI) | CFI | WRMR | |
|---|---|---|---|---|---|---|---|
| 1 | Correlated Two-Factor 1 | 484 | 872.282 | <.001 | .035 (.032 - .039) | .960 | 1.146 |
| 2 | Orthogonal Two-Factor 1 | 485 | 3996.889 | <.001 | .106 (.103 - .109) | .643 | 3.507 |
| 3 | One-Factor 1 | 485 | 1187.035 | <.001 | .047 (.044 - .051) | .929 | 1.403 |
| 4 | Bi-Factor 1 | 461 | 647.001 | <.001 | .025 (.020 - .029) | .981 | .886 |
Note.
Model included error covariances, all significant when corrected for multiple post hoc comparisons using the Benjamini-Hochberg False Discovery Rate (FDR) (p =.05); Chi square test statistic (χ2 > .05 exact fit), Root Mean Square Error of Approximation (RMSEA) (ε < .05 close approximate fit; ε = .05 - .08 close approximate fit; ε = .08 – 1.0 reasonable approximate fit); Comparative Fit Index (CFI) (> .90 reasonable fit; >.95 good fit); Weighted Root Mean Residual (WRMR) (<.950 good fit)
Table 3. Standardized Loading Estimates for individual ICBC Items on the Disinhibition, Impulsivity, and Compulsivity Factors. All loading estimates were significant at p < .001, except where indicated. **p < .01, *p < .05.
| ICBC Items | Disinhibition | Impulsivity | Compulsivity |
|---|---|---|---|
| 1. Washing | .677 | ||
| 2. Smoking | .141* | .585 | |
| 3. Collect | .519 | ||
| 4. Money | .295 | .375 | |
| 5. Ordering | .626 | .588 | |
| 6. Shopping | .697 | ||
| 7. List | .586 | .496 | |
| 8. Counting | .705 | .385 | |
| 9. Grooming | .790 | ||
| 10. Routines | .674 | .366 | |
| 11. Repeating | .684 | .234 | |
| 12. Exercising | .629 | ||
| 13. Betting | .312 | .443 | |
| 14. Hair Picking | .427 | ||
| 15. Lying | .602 | .405 | |
| 16. Sexual | .592 | .498 | |
| 17. Alcohol | .379 | .526 | |
| 18. Planning | .608 | .451 | |
| 19. Drug | .168* | .775 | |
| 20. Cleaning | .543 | .422 | |
| 21. Verbal | .625 | .489 | |
| 22. Violence | .605 | .504 | |
| 23. Swearing | .532 | .470 | |
| 24. Checking Locks | .515 | .388 | |
| 25. Checking Mirror | .751 | ||
| 26. Driving | .363 | .201** | |
| 27. Medication | .655 | .214** | |
| 28. Aggression | .637 | .429 | |
| 29. Social | .616 | ||
| 30. Rules | .636 | .257 | |
| 31. Injury | .474 | .310 | |
| 32. Rewriting | .678 | .295 | |
| 33. Tattooing | .595 | .437 |
Calculation of the Explained Common Variance (ECV) revealed that the Impulsivity and Compulsivity group factors collectively accounted for sufficient explained variance (31%) in the ICBC, in addition to the general Disinhibition factor (69%), to justify retaining them over a unidimensional model (Rodriguez et al., 2016a; Reise, 2012b). Information functions generated for the 33 ICBC items loading on the general Disinhibition factor and were relatively distinct for different items (Supplementary Figure 1), suggesting that the general factor was not simply capturing item response bias or other forms of spurious variance (Bonifay et al., 2017). Factor score estimates were generated for the Disinhibition, Impulsivity, and Compulsivity factors for use in subsequent analyses, and exhibited weak bivariate correlations (Disinhibition with Impulsivity r = .115, p =.004 & Compulsivity r = .218, p <.001; Impulsivity with Compulsivity r = -.177, p < .001). These low correlations indicated that the factor score estimates for each latent variable were not heavily contaminated by variance from the other two factors (Grice, 2001).
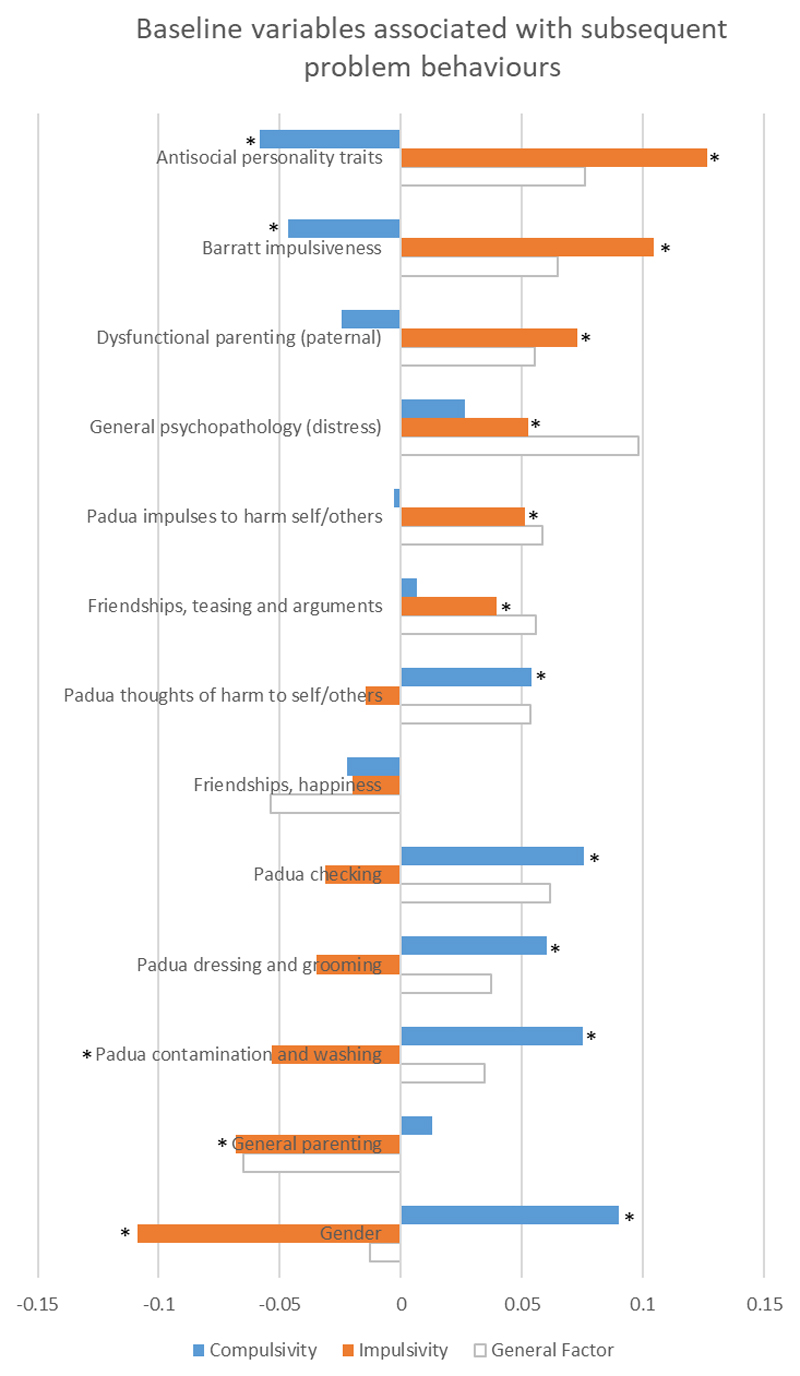
Baseline measures associated with subsequent trans-diagnostic problem behaviours
The optimal PLS model relating baseline variables to current impulsive-compulsive behaviours (ICBC latent scores) accounted for 37.4% of variation in the explanatory (X) measures and 11.6% of variation in later ICBC problem behaviour scores (Y). Variables that were important in the model (passing Variable Importance Parameter [VIP] threshold of 0.8) are shown in Figure 1. The following baseline variables were each significantly associated with higher subsequent impulsive problem behaviours: antisocial personality traits, impulsive traits (Barratt Impulsiveness Scale), dysfunctional perceived parenting scores (both general parenting and paternal parenting scores), general psychopathology/distress (K10), male gender, impulse to harm self/others (Padua Inventory subscore), and teasing/arguments in friendships. Impulsive problem behaviours were also significantly predicted by previous lower contamination obsessions and washing compulsions (Padua Inventory subscore). Baseline variables that were significantly associated with higher subsequent compulsive problem behaviours were: obsessional thoughts of harm to self/others (Padua Inventory subscore), compulsive checking (Padua subscore), dressing/grooming compulsions (Padua Inventory subscore), contamination obsessions and washing compulsions (Padua Inventory subscore), and female gender. Higher levels of compulsive problem behaviours were also significantly predicted by previous lower antisocial personality traits, and lower impulsive traits (Barratt Impulsiveness Scale). The following variables were statistically unimportant in the model and were excluded (VIP < 0.8): age at entry, ethnic group, family education level, current or past mental health or behavioural problem (parent/guardian report), history of head trauma (parent/guardian report), history of perinatal complications (parent/guardian report), and history of any medical conditions (parent/guardian report).
Figure 1.
Standardized model coefficients for variables statistically explaining later problem behaviors (orange: impulsive problems; blue: compulsive problems). * indicates p<0.05 significant by rigorous statistical correction (bootstrap) for impulsive and compulsive problem behaviors. (For reference, model coefficients for the General Factor are shown in light grey outline; these were all significant by bootstrap except for gender [asterisks not shown]).
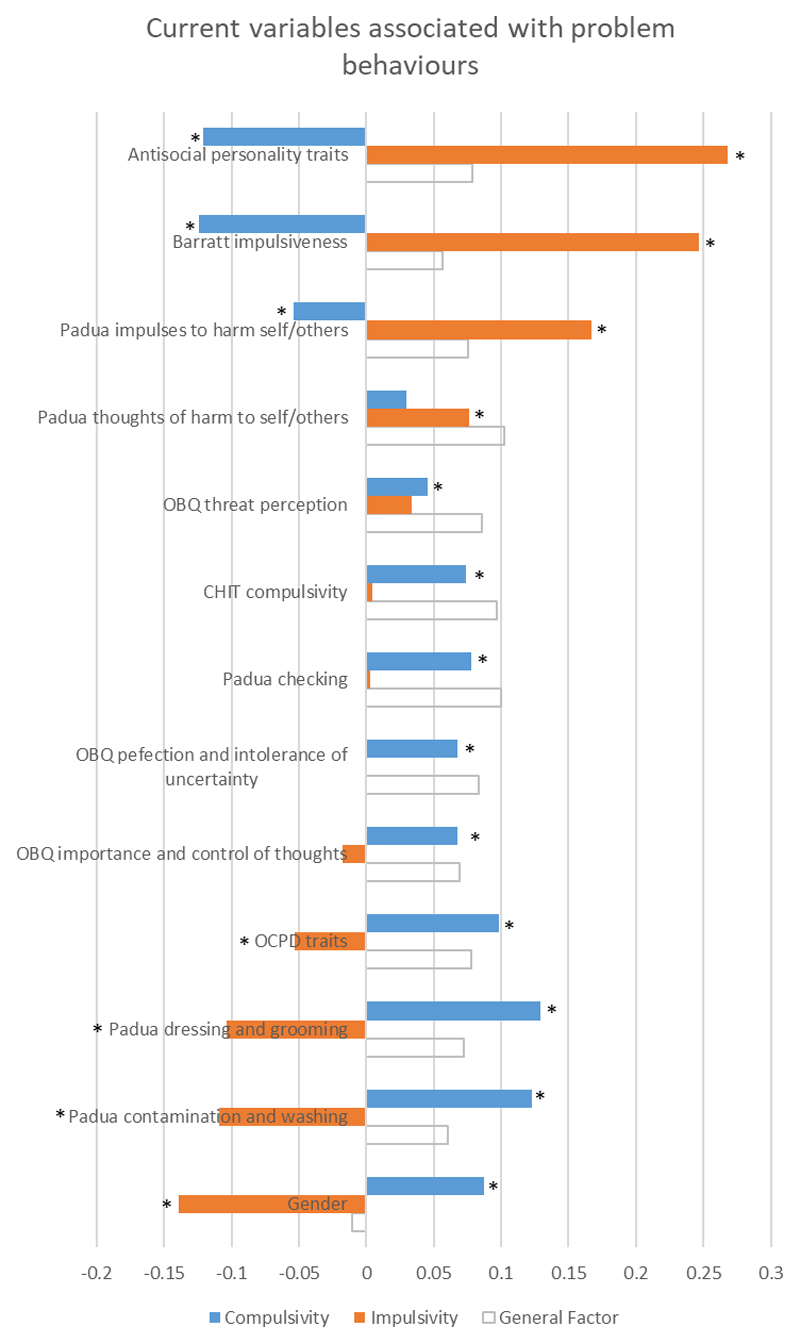
Current measures associated with trans-diagnostic problem behaviours
The optimal PLS model relating current variables to current impulsive-compulsive behaviours (ICBC latent scores) accounted for 48.0% of variation in the explanatory measures (X) and 32.7% of variation in ICBC problem behaviour scores (Y). Variables that were important in the model (passing Variable Importance Parameter [VIP] threshold of 0.8) are shown in Figure 2. The following measures were each significantly associated with higher impulsive problem behaviours: antisocial personality traits, impulsive traits (Barratt Impulsiveness Scale), impulses to harm self/others (Padua Inventory subscore), and male gender. Higher impulsive problem behaviours were also significantly associated with fewer OCPD traits, lower dressing/grooming compulsions (Padua Inventory subscore), and lower contamination obsessions and washing compulsions (Padua Inventory subscore). The following measures were each significantly associated with higher compulsive problem behaviours: checking compulsions (Padua Inventory subscore), thoughts of harm to self/others (Padua Inventory subscore), dressing/grooming compulsions (Padua Inventory subscore), contamination obsessions and washing compulsions (Padua Inventory subscore), threat perception (OBQ), compulsive traits (CHIT), perfection and intolerance of uncertainty (OBQ), importance and control of thoughts (OBQ), OCPD traits, and female gender. Lower impulses to harm self/others (Padua Inventory subscore) was significantly associated with higher compulsive problem behaviours. The following variables were statistically unimportant in the model and were excluded (VIP < 0.8): age, ethnic group, education levels, and general psychopathology (distress).
Figure 2.
Standardized model coefficients for variables statistically explaining current problem behaviors (orange: impulsive problems; blue: compulsive problems). * indicates p<0.05 significant by rigorous statistical correction (bootstrap) for impulsive and compulsive problem behaviors. (For reference, model coefficients for the General Factor are shown in light grey outline; these were all significant by bootstrap except for gender [asterisks not shown]).
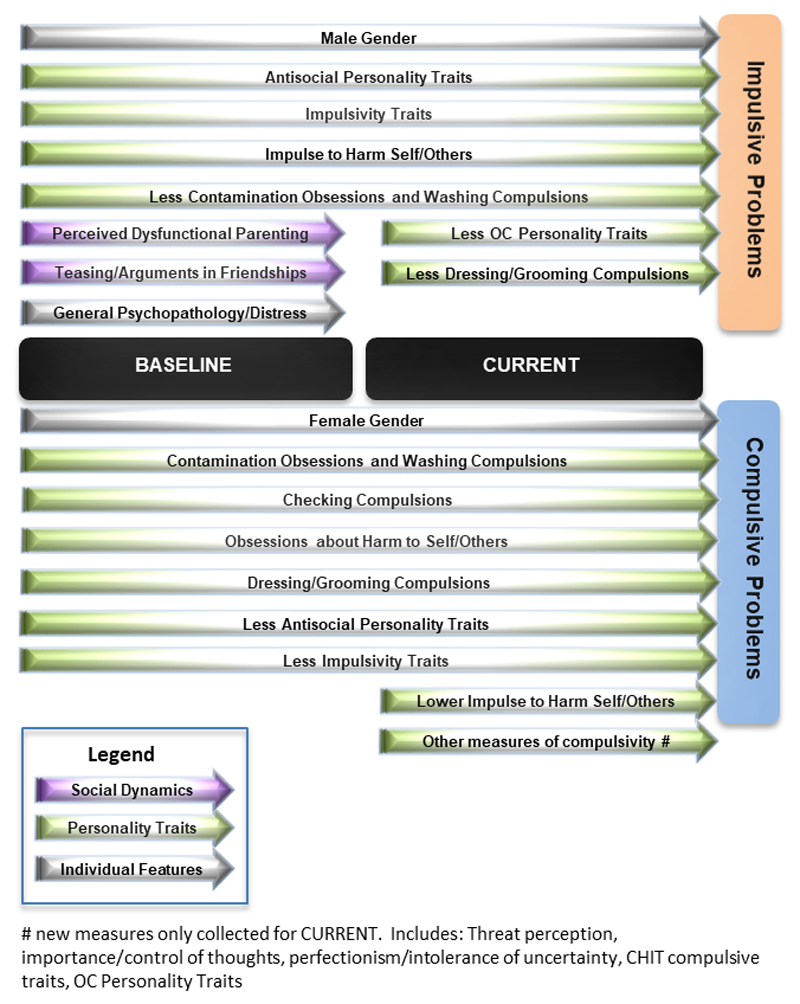
A conceptual schematic of the relationships between variables of interest and latent phenotype scores is provided in Figure 3.
Figure 3.
Variables significantly (p<0.05 bootstrap in PLS models) mapping onto trans-diagnostic phenotypes of impulsive and compulsive problem behaviors. OC = obsessive-compulsive.
Discussion
This study examined latent phenotypes of impulsive and compulsive problem behaviours in young adults. We demonstrated that these behaviours were best conceptualised within a bi-factor model, which included two underlying latent phenotypes corresponding to impulsive and compulsive problems respectively (Guo et al., 2017) as well as a general disinhibition factor. By modelling this additional general factor, we could quantify trans-diagnostic phenotypes that were separable and not due (for example) to common measurement variance (Reise, 2012a). Predictors of the later emergence of these phenotypes were identified (Figure 3), incorporating relevant measures of personality, parenting, and friendship experiences. The statistical approach used (Partial Least Squares) allowed intrinsic control for co-relationships between the important explanatory variables of interest. We did not identify any significant effects of age or education levels on occurrence of problem impulsive or compulsive behaviours.
Personality-related questionnaires provide rich dimensional measures, and are typically developed for use in normative settings, as well as in patient populations (Stanford et al., 2016; Sanavio, 1988). Personality measures here showed the clearest differentiation in statistically predicting later trans-diagnostic occurrence of impulsive and compulsive problem behaviours (Figure 3). Higher baseline scores on the Barratt Impulsivity Scale (Stanford et al., 2016), and the Antisocial Process Screening Device (Vitacco et al., 2003), each significantly predicted higher subsequent impulsivity scores derived from the ICBC (an independent instrument); and contrariwise, each of these two baseline personality scores significantly predicted lower subsequent compulsive problem behaviours.
As anticipated, most of the Padua obsessive-compulsive Inventory subscores (Sanavio, 1988) were associated with later emergence of compulsive but not impulsive problem behaviours, especially so for archetypal contamination obsessions and washing compulsions (for further discussion of Padua Inventory results see Supplement). We view scores on the Padua Inventory as personality traits in that they are measurable in the general population along a continuum. In fact the instrument was originally developed for community use (Sanavio, 1988); this is in contrast to clinical measures of OCD, such as the Yale-Brown Obsessive Compulsive Scale (Y-BOCS), which are unsuitable for phenotyping research due to a high likelihood of zero score in those without formal OCD (Goodman et al., 1989).
While the above associations are largely expected, in view of the conceptual domains they encompass, the results also indicate important, differential contribution of earlier personality traits known to be partly heritable (Niv et al., 2012; Tuvblad et al., 2014; Jonnal et al., 2000) to the ultimate manifestation of an extensive array of 33 adult problem behaviours. This pattern of association for impulsive, antisocial, and OC traits was also replicated cross-sectionally, but extending to a broader range of compulsivity instruments not originally included at baseline in the NSPN cohort (Figure 3).
It is well established that among environmental factors relevant to later risk of mental health problems, parenting and friendship networks are particularly important in young people, along with general distress. For example, family and friendship support during early adolescence negatively predicted risk of later adolescent depressive symptoms arising as a function of childhood adversity (van Harmelen et al., 2016). Here we show that worse perceived general parenting, higher levels of perceived dysfunctional parenting (reported by the study participant in relation to their father), and higher levels of general distress (K10 instrument) were specifically associated with later emergence of impulsive but not compulsive problems (Figure 3). Furthermore, participants’ earlier experiences of teasing and arguments within their friendship network, and not other aspects of friendship (as measured), were also significantly associated with later impulsive but not compulsive problem behaviours. Family functioning is an important determinant of specific types of impulsive problems (such as non-suicidal self-injury) (Cassels et al., 2018). Positive relationships between dysfunctional parenting (especially harshness and psychological control) and externalising symptoms have been shown in prior meta-analysis, in young people (Pinquart, 2017). In a longitudinal population-based study of adopted and non-adopted adolescents, parent-child conflict was associated with subsequent impulsive (‘acting-out’) behaviours (Klahr et al., 2011a; Klahr et al., 2011b).
We found a dissociation in the influence of gender on impulsive and compulsive trans-diagnostic phenotypes: male gender was significantly associated with impulsive problem behaviours (viewed trans-diagnostically) whereas female gender was significantly associated with compulsive problem behaviours. Impulsive problems (such as aggression and criminality) are more common in males in much of the literature (Chamorro et al., 2012), findings which may be due to males having higher sensation seeking and risk-taking (Cross et al., 2011). Several previous cross-sectional studies found that female gender is associated with higher obsessive-compulsive traits on the Padua Inventory (Chamberlain et al., 2016; Sanavio, 1988). These results hint at sexually divergent processes in the development of impulsive versus compulsive problems, which are not due (for example) to confounding gender differences in personality traits, parenting, or friendships, which were controlled for in the statistical modelling. Our data also accord well with findings from literature in other areas, particularly internalizing-externalizing studies in young people into adulthood, which commonly report a similar gender discrepancy (Wilhelm, 2014).
The bi-factor modelling approach is increasingly adopted in psychiatry research (Castellanos-Ryan et al., 2016; Hankin et al., 2016; Caspi et al., 2014; Patalay et al., 2015; Stochl et al., 2015). Here, we demonstrate that a bi-factor model yielded superior fit across all metrics for the fractionation of trans-diagnostic phenotypes of impulsive and compulsive problem behaviours. To measure the phenotypes of interest, we used responses from the ICBC, which examined a broad range of 33 behaviours in a single, convenient questionnaire. The nature of the general latent factor, within the bi-factor model, itself is open to interpretation, as in other studies. The general factor was associated with all study measures excepting gender, suggesting that it may relate to general disinhibition (general tendencies towards failure to suppress behaviours). We believe it unlikely that this general factor reflects only common response bias because its relationship with individual ICBC items was variable. It is intended to examine biological substrates of this general disinhibition factor in future work.
There are several limitations in relation to this study. Rigorous demonstration of causality has multiple scientific requirements and cannot be shown definitively within a study design as deployed here. Nonetheless, impulsive, dissocial, and compulsive traits bore strong relationships with their respective expected problem behaviours (measured using a separate questionnaire) both longitudinally and cross-sectionally, showing a sustained and meaningful association. The original recruitment methodology for NSPN was designed to be epidemiologically representative (i.e. stratified based on census statistics) (Kiddle et al., 2017). However, the current study participants provided data in 2018 and thus may not be fully representative of the original NSPN cohort. Our current sample had mean impulsive and compulsive scores (Barratt Impulsivity Scale and Padua Inventory) similar to those reported in previous normative studies (Burns et al., 1996; Steinberg et al., 2013). We measured relatively ‘high level’ trans-diagnostic phenotypes closely allied to overt problems, but the phenotypic approach should ultimately be applied to a range of measures incorporating also cognitive and biological (genetic, imaging) parameters. Lastly, the best fit statistical model for data is contingent on the particular nature and range of measures used; because a given model offers a superior fit, it does not follow that other models have no utility.
In summary, impulsive and compulsive problem behaviours were fractionated trans-diagnostically using a bi-factor model, which yielded the best fit versus other alternative models suggested by the extant literature. Significant baseline predictors of later problem impulsive and compulsive trans-diagnostic phenotypes were identified, using a powerful statistical technique well-suited to large datasets where items are likely to be correlated. Personality-traits were important determinants of impulsive and compulsive problem behaviours, whereas parenting and friendship experiences significantly predicted impulsive problems specifically, and gender specific effects were found (male gender, higher impulsive problems; female gender, higher compulsive problems). This study highlights the potential utility of the trans-diagnostic approach in psychiatry, as applied to impulsivity and compulsivity. The heritability and biological substrates of latent impulsivity, compulsivity, and general model factors merits exploration. For example, if the trans-diagnostic phenotype of compulsivity has higher heritability than impulsivity, this may account for the relatively lower impact of the earlier social milieu on the former. The finding that aspects of parenting and friendships differentially relate to impulsive as opposed to compulsive problems may have implications for tailoring early interventions and targeting vulnerable individuals to avert the development of later problematic behaviours. In particular, such trans-diagnostic approaches can be used to identify candidate risk factors for a broad range of psychiatric symptoms. These risk factors (such as elements of personality, friendship support, and parenting) could in future be targeted for modification in people at risk of impulsive and compulsive problems, in order to avert the development of these impairing pathologies. This would potentially shift the emphasis in psychiatry more towards prevention (Furber et al., 2017), as well as treatment; a shift that has been deployed with success in other areas of healthcare, and in other areas of psychiatry outside the impulsive-compulsive sphere.
Supplementary Material
Acknowledgement
The authors would like to thank the NSPN study team, particularly Gita Prabhu and Laura Villis, for invaluable assistance in setting up the study; and would like to thank the study participants. This research was supported by the NIHR Cambridge Biomedical Research Centre (BRC).
Sources of Funding: This research was funded by a Clinical Fellowship from the Wellcome Trust to Dr. Chamberlain (reference 110049/Z/15/Z). The study was supported by the Neuroscience in Psychiatry Network, a strategic award from the Wellcome Trust to the University of Cambridge and University College London (095844/Z/11/Z).
Role of the sponsor: The Wellcome Trust funded this research via a grant to Dr Chamberlain. The Wellcome Trust approved the theme of the research as part of the grant process but did not play a direct role in the study design, data collection, write-up, or publication process.
Footnotes
Potential conflicts of interest: Dr. Chamberlain consults for Cambridge Cognition and Shire. Dr. Grant has received research grants from NIDA, National Center for Responsible Gaming, American Foundation for Suicide Prevention, and Forest and Roche Pharmaceuticals Dr. Grant receives yearly compensation from Springer Publishing for acting as Editor-in-Chief of the Journal of Gambling Studies and has received royalties from Oxford University Press, American Psychiatric Publishing, Inc., Norton Press, Johns Hopkins University Press, and McGraw Hill. Jeggan Tiego was supported by National Health and Medical Research Council (NHMRC) project grants 1050504 and 1146292. Dr. Fontenelle is supported by the “Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ) under E-26/010.001411/2015; and “Conselho Nacional de Desenvolvimento Científico e Tecnológico” (CNPq)] under grant 308237/2014-5. Dr. Goodyer consults for Lundbeck; is supported by a Wellcome Trust Strategic Award; and is Chairperson of and scientific advisor to the Peter Cundill Centre for Youth Depression Research, Centre for Addictions and Mental Health, University of Toronto. Dr. Yücel was supported by a National Health and Medical Research Council of Australia Fellowship (#APP1117188) and the David Winston Turner Endowment Fund. Dr Rebecca Segrave was supported by the David Winston Turner Endowment Fund. The other authors report no conflicts of interest or disclosures. Dr Hauser is supported by the Jacobs Foundation. Dr Dolan is supported by a Wellcome Investigator Award and by the Max Planck Society. Dr. Bullmore is employed half-time by GSK and holds stock in GSK.
Clinical trials registration: not applicable.
Previous presentations: none.
References
- Abdi H, Williams LJ. Partial least squares methods: partial least squares correlation and partial least square regression. Methods Mol Biol. 2013;930:549–579. doi: 10.1007/978-1-62703-059-5_23. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. (5th ed.) (DSM-5) Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Black DW, Coryell W, McCormick B, et al. A prospective follow-up study of younger and older subjects with pathological gambling. Psychiatry Res. 2017;256:162–168. doi: 10.1016/j.psychres.2017.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonifay W, Lane SP, Reise SP. Three concerns with applying a bifactor model as a structure of psychopathology. Clinical Psychological Science. 2017;5:184–186. [Google Scholar]
- Burns GL. Padua Inventory-Washington State University Revision. Pullman, WA: 1995. (Available from G. Leonard Burns, Department of Psychology, Washington State University, Pullman, WA 99164-4820) [Google Scholar]
- Burns GL, Keortge SG, Formea GM, et al. Revision of the Padua Inventory of obsessive compulsive disorder symptoms: distinctions between worry, obsessions, and compulsions. Behav Res Ther. 1996;34:163–173. doi: 10.1016/0005-7967(95)00035-6. [DOI] [PubMed] [Google Scholar]
- Casey BJ, Heller AS, Gee DG, et al. Development of the emotional brain. Neurosci Lett. 2017 doi: 10.1016/j.neulet.2017.11.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, et al. The p Factor: One General Psychopathology Factor in the Structure of Psychiatric Disorders? Clin Psychol Sci. 2014;2:119–137. doi: 10.1177/2167702613497473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassels M, van Harmelen AL, Neufeld S, et al. Poor family functioning mediates the link between childhood adversity and adolescent nonsuicidal self-injury. J Child Psychol Psychiatry. 2018 doi: 10.1111/jcpp.12866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellanos-Ryan N, Briere FN, O'Leary-Barrett M, et al. The structure of psychopathology in adolescence and its common personality and cognitive correlates. J Abnorm Psychol. 2016;125:1039–1052. doi: 10.1037/abn0000193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerda M, Moffitt TE, Meier MH, et al. Persistent cannabis dependence and alcohol dependence represent risks for midlife economic and social problems: A longitudinal cohort study. Clin Psychol Sci. 2016;4:1028–1046. doi: 10.1177/2167702616630958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain SR, Grant JE. Initial Validation of a Trans-diagnostic Compulsivity Questionnaire: The Cambridge-Chicago Compulsivity Trait Scale. CNS Spectrums. 2018 doi: 10.1017/S1092852918000810. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain SR, Leppink EW, Redden SA, et al. Are obsessive-compulsive symptoms impulsive, compulsive or both? Compr Psychiatry. 2016;68:111–118. doi: 10.1016/j.comppsych.2016.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain SR, Stochl J, Redden SA, et al. Latent traits of impulsivity and compulsivity: toward dimensional psychiatry. Psychol Med. 2017;48:810–821. doi: 10.1017/S0033291717002185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamorro J, Bernardi S, Potenza MN, et al. Impulsivity in the general population: a national study. J Psychiatr Res. 2012;46:994–1001. doi: 10.1016/j.jpsychires.2012.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox I, Gaudard M. Discovering Partial Least Squares with JMP. Cary, North Carolina, USA: SAS Institute Inc; 2013. [Google Scholar]
- Cross CP, Copping LT, Campbell A. Sex differences in impulsivity: a meta-analysis. Psychol Bull. 2011;137:97–130. doi: 10.1037/a0021591. [DOI] [PubMed] [Google Scholar]
- Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med. 2013;11:126. doi: 10.1186/1741-7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elgar FJ, Waschbusch DA, Dadds MR, et al. Development and Validation of a Short Form of the Alabama Parenting Questionnaire. Journal of Child anf Family Studies. 2007;16:243–259. [Google Scholar]
- Evenden JL. Varieties of impulsivity. Psychopharmacology (Berl) 1999;146:348–361. doi: 10.1007/pl00005481. [DOI] [PubMed] [Google Scholar]
- Fineberg NA, Hengartner MP, Bergbaum CE, et al. A prospective population-based cohort study of the prevalence, incidence and impact of obsessive-compulsive symptomatology. Int J Psychiatry Clin Pract. 2013;17:170–178. doi: 10.3109/13651501.2012.755206. [DOI] [PubMed] [Google Scholar]
- Furber G, Leach M, Guy S, et al. Developing a broad categorisation scheme to describe risk factors for mental illness, for use in prevention policy and planning. Aust N Z J Psychiatry. 2017;51:230–240. doi: 10.1177/0004867416642844. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale. II. Validity. Arch Gen Psychiatry. 1989;46:1012–1016. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- Goodyer IM, Herbert J, Tamplin A, et al. Short-term outcome of major depression: II. Life events, family dysfunction, and friendship difficulties as predictors of persistent disorder. J Am Acad Child Adolesc Psychiatry. 1997;36:474–480. doi: 10.1097/00004583-199704000-00009. [DOI] [PubMed] [Google Scholar]
- Grice JW. Computing and evaluating factor scores. Psychological methods. 2001;6:430–450. [PubMed] [Google Scholar]
- Guo K, Youssef GJ, Dawson A, et al. A psychometric validation study of the Impulsive-Compulsive Behaviours Checklist: A transdiagnostic tool for addictive and compulsive behaviours. Addict Behav. 2017;67:26–33. doi: 10.1016/j.addbeh.2016.11.021. [DOI] [PubMed] [Google Scholar]
- Hancock GR, Mueller RO. Rethinking construct reliability within latent variable systems. In: Cudeck R, du Toit S, Sorbom D, editors. Structural equation modeling: Present and future - A festchrift in honor of Karl Joreskog. Lincolnwood, IL: Scientific Software International; 2001. pp. 195–216. [Google Scholar]
- Hankin BL, Snyder HR, Gulley LD, et al. Understanding comorbidity among internalizing problems: Integrating latent structural models of psychopathology and risk mechanisms. Dev Psychopathol. 2016;28:987–1012. doi: 10.1017/S0954579416000663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollander E, Kim S, Braun A, et al. Cross-cutting issues and future directions for the OCD spectrum. Psychiatry Res. 2009;170:3–6. doi: 10.1016/j.psychres.2008.07.015. [DOI] [PubMed] [Google Scholar]
- Jonnal AH, Gardner CO, Prescott CA, et al. Obsessive and compulsive symptoms in a general population sample of female twins. Am J Med Genet. 2000;96:791–796. doi: 10.1002/1096-8628(20001204)96:6<791::aid-ajmg19>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32:959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kiddle B, Inkster B, Prabhu G, et al. Cohort profile: The NSPN 2400 Cohort: a developmental sample supporting the Wellcome Trust NeuroScience in Psychiatry Network. Int J Epidemiol. 2017 doi: 10.1093/ije/dyx117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klahr AM, McGue M, Iacono WG, et al. The association between parent-child conflict and adolescent conduct problems over time: results from a longitudinal adoption study. J Abnorm Psychol. 2011a;120:46–56. doi: 10.1037/a0021350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klahr AM, Rueter MA, McGue M, et al. The relationship between parent-child conflict and adolescent antisocial behavior: confirming shared environmental mediation. J Abnorm Child Psychol. 2011b;39:683–694. doi: 10.1007/s10802-011-9505-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York: The Guilford Press; 2016. [Google Scholar]
- Krmpotich T, Mikulich-Gilbertson S, Sakai J, et al. Impaired Decision-Making, Higher Impulsivity, and Drug Severity in Substance Dependence and Pathological Gambling. J Addict Med. 2015;9:273–280. doi: 10.1097/ADM.0000000000000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindner P, Frykheden O, Forsstrom D, et al. The Brunnsviken Brief Quality of Life Scale (BBQ): Development and Psychometric Evaluation. Cogn Behav Ther. 2016;45:182–195. doi: 10.1080/16506073.2016.1143526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moulding R, Anglim J, Nedeljkovic M, et al. The Obsessive Beliefs Questionnaire (OBQ): examination in nonclinical samples and development of a short version. Assessment. 2011;18:357–374. doi: 10.1177/1073191110376490. [DOI] [PubMed] [Google Scholar]
- Munoz LC, Frick PJ. The reliability, stability, and predictive utility of the self-report version of the Antisocial Process Screening Device. Scand J Psychol. 2007;48:299–312. doi: 10.1111/j.1467-9450.2007.00560.x. [DOI] [PubMed] [Google Scholar]
- Muthén B, du Toit SHC, Spisic D. Robust inference using weighted least squares and quadratic estimating equations in latent variable modeling with categorical and continuous outcomes. Conditionallly accepted for publication in Psychometrika. 1997 [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. Los Angeles, CA: Muthén & Muthén; 1998 - 2012. [Google Scholar]
- Niv S, Tuvblad C, Raine A, et al. Heritability and longitudinal stability of impulsivity in adolescence. Behav Genet. 2012;42:378–392. doi: 10.1007/s10519-011-9518-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker G, Roussos J, Hadzi-Pavlovic D, et al. The development of a refined measure of dysfunctional parenting and assessment of its relevance in patients with affective disorders. Psychol Med. 1997;27:1193–1203. doi: 10.1017/s003329179700545x. [DOI] [PubMed] [Google Scholar]
- Patalay P, Fonagy P, Deighton J, et al. A general psychopathology factor in early adolescence. Br J Psychiatry. 2015;207:15–22. doi: 10.1192/bjp.bp.114.149591. [DOI] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Pinquart M. Associations of parenting dimensions and styles with externalizing problems of children and adolescents: An updated meta-analysis. Dev Psychol. 2017;53:873–932. doi: 10.1037/dev0000295. [DOI] [PubMed] [Google Scholar]
- Reise SP. Invited Paper: The Rediscovery of Bifactor Measurement Models. Multivariate Behav Res. 2012a;47:667–696. doi: 10.1080/00273171.2012.715555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reise SP. The rediscovery of bifactor measurement models. Multivariate Behavioral Research. 2012b;47:667–696. doi: 10.1080/00273171.2012.715555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridenour TA, Daley JG, Reich W. Factor analyses of the family assessment device. Fam Process. 1999;38:497–510. doi: 10.1111/j.1545-5300.1999.00497.x. [DOI] [PubMed] [Google Scholar]
- Rodriguez A, Reise SP, Haviland MG. Applying bifactor statistical indices in the evaluation of psychological measures. J Pers Assess. 2016a;98:223–237. doi: 10.1080/00223891.2015.1089249. [DOI] [PubMed] [Google Scholar]
- Rodriguez A, Reise SP, Haviland MG. Evaluating bifactor models: Calculating and interpreting statistical indices. Psychol Methods. 2016b;21:137–150. doi: 10.1037/met0000045. [DOI] [PubMed] [Google Scholar]
- Sanavio E. Obsessions and compulsions: the Padua Inventory. Behav Res Ther. 1988;26:169–177. doi: 10.1016/0005-7967(88)90116-7. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 34–57. [PubMed] [Google Scholar]
- Spear LP. The adolescent brain and age-related behavioral manifestations. Neurosci Biobehav Rev. 2000;24:417–463. doi: 10.1016/s0149-7634(00)00014-2. [DOI] [PubMed] [Google Scholar]
- Clair MC, Neufeld S, Jones PB, et al. Characterising the latent structure and organisation of self-reported thoughts, feelings and behaviours in adolescents and young adults. PLoS One. 2017;12:e0175381. doi: 10.1371/journal.pone.0175381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanford MS, Mathias CW, Dougherty DM, et al. Fifty years of the Barratt Impulsiveness Scale: An update and review. Personality and Individual Differences. 2016;47:385–395. [Google Scholar]
- Steinberg L, Sharp C, Stanford MS, et al. New tricks for an old measure: the development of the Barratt Impulsiveness Scale-Brief (BIS-Brief) Psychol Assess. 2013;25:216–226. doi: 10.1037/a0030550. [DOI] [PubMed] [Google Scholar]
- Stochl J, Khandaker GM, Lewis G, et al. Mood, anxiety and psychotic phenomena measure a common psychopathological factor. Psychol Med. 2015;45:1483–1493. doi: 10.1017/S003329171400261X. [DOI] [PubMed] [Google Scholar]
- Tuvblad C, Bezdjian S, Raine A, et al. The heritability of psychopathic personality in 14- to 15-year-old twins: a multirater, multimeasure approach. Psychol Assess. 2014;26:704–716. doi: 10.1037/a0036711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Harmelen AL, Gibson JL, Clair MC, et al. Friendships and Family Support Reduce Subsequent Depressive Symptoms in At-Risk Adolescents. PLoS One. 2016;11:e0153715. doi: 10.1371/journal.pone.0153715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Harmelen AL, Kievit RA, Ioannidis K, et al. Adolescent friendships predict later resilient functioning across psychosocial domains in a healthy community cohort. Psychol Med. 2017;47:2312–2322. doi: 10.1017/S0033291717000836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitacco MJ, Rogers R, Neumann CS. The antisocial process screening device: an examination of its construct and criterion-related validity. Assessment. 2003;10:143–150. doi: 10.1177/1073191103010002005. [DOI] [PubMed] [Google Scholar]
- Wilhelm KA. Gender and mental health. Aust N Z J Psychiatry. 2014;48:603–605. doi: 10.1177/0004867414538678. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.