Summary
Background
The eastern Mediterranean region is comprised of 22 countries: Afghanistan, Bahrain, Djibouti, Egypt, Iran, Iraq, Jordan, Kuwait, Lebanon, Libya, Morocco, Oman, Pakistan, Palestine, Qatar, Saudi Arabia, Somalia, Sudan, Syria, Tunisia, the United Arab Emirates, and Yemen. Since our Global Burden of Disease Study 2010 (GBD 2010), the region has faced unrest as a result of revolutions, wars, and the so-called Arab uprisings. The objective of this study was to present the burden of diseases, injuries, and risk factors in the eastern Mediterranean region as of 2013.
Methods
GBD 2013 includes an annual assessment covering 188 countries from 1990 to 2013. The study covers 306 diseases and injuries, 1233 sequelae, and 79 risk factors. Our GBD 2013 analyses included the addition of new data through updated systematic reviews and through the contribution of unpublished data sources from collaborators, an updated version of modelling software, and several improvements in our methods. In this systematic analysis, we use data from GBD 2013 to analyse the burden of disease and injuries in the eastern Mediterranean region specifically.
Findings
The leading cause of death in the region in 2013 was ischaemic heart disease (90·3 deaths per 100 000 people), which increased by 17·2% since 1990. However, diarrhoeal diseases were the leading cause of death in Somalia (186·7 deaths per 100 000 people) in 2013, which decreased by 26·9% since 1990. The leading cause of disability-adjusted life-years (DALYs) was ischaemic heart disease for males and lower respiratory infection for females. High blood pressure was the leading risk factor for DALYs in 2013, with an increase of 83·3% since 1990. Risk factors for DALYs varied by country. In low-income countries, childhood wasting was the leading cause of DALYs in Afghanistan, Somalia, and Yemen, whereas unsafe sex was the leading cause in Djibouti. Non-communicable risk factors were the leading cause of DALYs in high-income and middle-income countries in the region. DALY risk factors varied by age, with child and maternal malnutrition affecting the younger age groups (aged 28 days to 4 years), whereas high bodyweight and systolic blood pressure affected older people (aged 60–80 years). The proportion of DALYs attributed to high body-mass index increased from 3·7% to 7·5% between 1990 and 2013. Burden of mental health problems and drug use increased. Most increases in DALYs, especially from non-communicable diseases, were due to population growth. The crises in Egypt, Yemen, Libya, and Syria have resulted in a reduction in life expectancy; life expectancy in Syria would have been 5 years higher than that recorded for females and 6 years higher for males had the crisis not occurred.
Interpretation
Our study shows that the eastern Mediterranean region is going through a crucial health phase. The Arab uprisings and the wars that followed, coupled with ageing and population growth, will have a major impact on the region’s health and resources. The region has historically seen improvements in life expectancy and other health indicators, even under stress. However, the current situation will cause deteriorating health conditions for many countries and for many years and will have an impact on the region and the rest of the world. Based on our findings, we call for increased investment in health in the region in addition to reducing the conflicts.
Funding
Bill & Melinda Gates Foundation.
Introduction
The eastern Mediterranean region is comprised of 22 countries: Afghanistan, Egypt, Bahrain, Djibouti, Iraq, Iran, Jordan, Kuwait, Lebanon, Libya, Morocco, Oman, Pakistan, Palestine, Qatar, Saudi Arabia, Somalia, Sudan, Syria, Tunisia, the United Arab Emirates, and Yemen. The region has a population of about 583 million people.1 Countries in the eastern Mediterranean region vary substantially in their gross domestic product, sociodemographic profiles, health indicators, and health system capacities and coverage.2,3
The political and economic situation in the region since 2010 has suffered from continued unrest and the Arab uprisings. Revolutions and changes in government occurred in Egypt, Libya, Tunisia, and Yemen. A civil war is devastating Syria, and disturbances are common in Afghanistan, Bahrain, Iraq, Palestine, and Somalia. As a result, hundreds of thousands of civilians have been forced to flee and seek refuge.
In this Article, we present the burden of diseases, injuries, and risk factors in the eastern Mediterranean region from 1990 to 2013, with the aim to show the impact of war and unrest on the health of people in the region as of the end of 2013.
Methods
Study overview
The Global Burden of Disease Study 2013 (GBD 2013) includes an annual assessment covering 188 countries from 1990 to 2013. It covers 306 diseases and injuries, 1233 sequelae, and 79 risk factors. Detailed descriptions of the method and approach of GBD 2013 have been published elsewhere.4–7 Key changes in the methods from GBD 2010 are the inclusion of new data through updated systematic reviews and the contribution of unpublished data sources from various collaborators; the use of a counterfactual approach for estimating causes of diarrhoea and pneumonia; elaboration of the sequelae list to include asymptomatic states; use of more detailed nature of injury codes (N-codes); improvements to the Bayesian meta-regression method; increased simulation size for comorbidity; estimation of the prevalence of injuries by cohort; and use of a new method to estimate the distribution of mild, moderate, and severe anaemia by cause. In this systematic analysis, we use data from GBD 2013 to analyse the burden of disease and injuries in the eastern Mediterranean region specifically. We report 95% uncertainty intervals for each value in our analysis.
Mortality estimation
We generated child mortality rates and adult mortality rates under the influence of natural disasters and armed conflicts as previously described.7 Because of ongoing unrest and war, some datapoints needed for our analyses were not available. A list of all datapoints used in this study are available on our Global Health Data Exchange web page. When data were unavailable, we relied on our ensemble modelling techniques to generate the estimates using other available variables and the information for neighbouring countries or countries with a similar health profile in the region. We used six different modelling strategies for the 240 causes of death using our cause-of-death ensemble model for causes with sufficient information. We estimated national time series from 1950 to 2013 for gross domestic product, educational attainment, tobacco prevalence, and obesity. For mortality rates of children younger than 5 years, we analysed all survey, census, sample registration, and vital registration sources. Wherever possible, we analysed microdata from surveys and censuses with updated methods for child mortality. We corrected for bias in different sources in specific countries. For adult mortality, we identified all available vital registration data, sibling history survey data, sample registration data, and household recall of deaths. We assessed vital registration data for completeness and analysed sibling history data to account for survivor bias, zero-surviving sibships, and recall bias. We used spatiotemporal regression and Gaussian process regression to synthesise all measurements of mortality. We used UN population estimates that account for migration in our analyses. Moreover, we applied mortality shocks based on multiple reports to our analyses.
Effects of risk factors on disease burden
We used the comparative risk assessment approach to evaluate how much of the burden of disease observed in a given year can be attributed to past exposure to a risk factor.7 We estimated attributable burden by comparing observed health outcomes with outcomes that would have been observed if an alternative or counterfactual level of exposure had taken place in the past. We used the exposure level that minimises risk for the population, termed the theoretical minimum risk exposure level. We avoided double counting in the presentation of overall results by computing the overlap for joint risk distributions: behavioural risks alone; environmental or occupational risks alone; metabolic risks alone; behavioural and environmental or occupational risks together; behavioural and metabolic risks together; environmental or occupational and metabolic risks together; and behavioural, environmental or occupational, and metabolic risks together.
Disaggregation
We cross-tabulated the quantiles of disability-adjusted life-years (DALYs) by quintiles of annual DALY increase from 1990 to 2013 to show rates of DALY increase by burden. We divided the region into three categories according to the gross national income (GNI) per capita. The first category represents the low-income countries with an average GNI per capita of US$523·3 On the opposite end of the spectrum are oil-rich, high-income countries with an average GNI per capita of $39 688. The nations that lie in between are the middle-income countries with an average GNI per capita of $3251, which can be further subdivided into lower-middle-income and upper-middle-income countries. Low-income countries were Afghanistan, Djibouti, Somalia, and Yemen. Middle-income countries were Egypt, Iran, Iraq, Jordan, Lebanon, Libya, Morocco, Pakistan, Palestine, Sudan, Syria, and Tunisia. High-income countries were Bahrain, Kuwait, Oman, Qatar, Saudi Arabia, and the United Arab Emirates.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility to submit the paper.
Results
The leading cause of death in the eastern Mediterranean region in 2013 was ischaemic heart disease (90·3 deaths per 100 000 people).8 It surpassed both diarrhoeal diseases and lower respiratory infections as the leading cause of death in 1990, increasing by 17·2%. There was a shift in main causes of death from communicable to non-communicable diseases in the region. Causes of death and their rates of change varied by country.8 For example, diarrhoeal disease was the leading cause of death in Somalia and accounted for 186·7 deaths per 100 000 people in 2013, a decrease of 26·9% from 1990.9 All countries observed an increase in life expectancy and healthy life expectancy since 1990, although at different rates (appendix pp 7–8). Afghanistan had the lowest life expectancy and healthy life expectancy (56·5 years vs 49·0 years for men, 56·0 years vs 48·8 years for women, respectively), whereas Qatar had the highest (81·2 years vs 69·2 years for men, 83·1 years vs 69·5 years for women, respectively). Lebanon had a higher increase in healthy life expectancy than life expectancy. Global life expectancy for both sexes increased from 65·3 years in 1990, to 71·5 years in 2013.4
There was a change in causes of years of life lost (YLLs) from 1990 to 2013 in all countries (appendix p 9). Overall, regional YLLs decreased from 45 312 years per 100 000 people in 1990 to about 24 160 years per 100 000 people in 2013.8 Cardiovascular diseases, neoplasms, diabetes, chronic kidney disease, and transport injuries increased, especially in high-income and middle-income countries in the region, whereas neonatal disorders, diarrhoeal diseases, and lower respiratory infections decreased. HIV/AIDS and tuberculosis were large contributors to YLLs in 2013 in Djibouti. War was a large contributor to YLLs in Syria in 2013 (38·1% of total YLLs).8
Overall, regional years lived with disability (YLDs) increased from 9526 years per 100 000 people in 1990 to about 10057 years per 100 000 people in 2013.8 Musculoskeletal disorders and mental disorders and substance abuse were major contributors to YLDs in 2013 and had the highest increase (appendix p 10). Nutritional deficiencies (mainly iron-deficiency anaemia) decreased in the region overall, but remained a large burden in low-income countries. For example, nutritional deficiencies remained one of the leading causes of YLDs in Yemen although the YLDs per 100 000 people decreased slightly by 2% from 1990.8
Overall, regional DALYs decreased from 54 838 years per 100 000 people in 1990 to about 34 217 years per 100 000 people in 2013. DALYs vary disproportionately by age and sex. Children younger than 5 years contributed to about 33% of total DALYs with a rate of 94 884 years per 100 000 people, compared with 34 217 years per 100 000 people for the general population.8 Ischaemic heart disease was the leading cause of DALYs in the region in 2013 in males and when data for both sexes were combined, whereas diarrhoeal diseases were the leading cause in 1990 (table 1). Lower respiratory infection was the leading cause of DALYs for females. Causes of DALYs varied by income; lower respiratory infection was the leading cause of DALYs in low-income countries (appendix p 15), ischaemic heart disease in middle-income countries (appendix p 16), and road injuries in high-income countries (appendix p 17). Causes of DALYs and their change from 1990 by country varied widely (appendix p 11). Causes of DALYs varied by age. For example, DALYs for mental health peaked in early adulthood and declined with age, whereas DALYs for cardiovascular diseases and neoplasms increased with age (appendix p 1). Different patterns of DALYs were observed in different income levels (appendix pp 12–14).
Table 1. Top ten causes of disability-adjusted life-years (DALYs) for the eastern Mediterranean region by sex; 1990, 2005, and 2013.
| 1990 | 2005 | 2013 | |
|---|---|---|---|
| Males | |||
| 1 | Diarrhoeal diseases 10·7% (9·1–12·2) | Lower respiratory infections 6·7% (5·6–8) | Ischaemic heart disease 6·7% (5·9–7·6) |
| 2 | Lower respiratory infections 10·3% (8·9–11·6) | Diarrhoeal diseases 5·9% (4·7–7·1) | Lower respiratory infections 5·8% (4·8–6·9) |
| 3 | Preterm birth complications 7·6% (6–9·9) | Preterm birth complications 5·8% (4·6–7·7) | Preterm birth complications 5·2% (3·9–6·8) |
| 4 | Congenital anomalies 4·7% (3·6–6·7) | Ischaemic heart disease 5·6% (5–6·3) | Diarrhoeal diseases 4·5% (3·5–5·7) |
| 5 | Neonatal encephalopathy due to birth asphyxia and trauma 3·9% (2·8–5·1) | Road injuries 4·2% (3·8–4·7) | Road injuries 4·5% (4·0–5·0) |
| 6 | Ischaemic heart disease 3·9% (3·4–4·3) | Congenital anomalies 4·1% (3·2–5·8) | Congenital anomalies 4·0% (3·3–5·1) |
| 7 | Road injuries 3·1% (2·8–4·1) | Neonatal encephalopathy due to birth asphyxia and trauma 4% (2·5–5·5) | Neonatal encephalopathy due to birth asphyxia and trauma 3·7% (2·5–5) |
| 8 | Cerebrovascular disease 2·7% (2·3–3·1) | Cerebrovascular disease 3·1% (2·7–3·7) | Cerebrovascular disease 3·5% (3–4·1) |
| 9 | Other neonatal disorders 2·6% (1·7–4·0) | Low back and neck pain 2·7% (2·0–3·6) | Low back and neck pain 3·4% (2·5–4·4) |
| 10 | Meningitis 2·3% (1·6–3·3) | Chronic obstructive pulmonary disease 2·1% (1·9–2·5) | Diabetes mellitus 2·5% (2·2–2·8) |
| Females | |||
| 1 | Diarrhoeal diseases 12·4% (10·4–14·3) | Lower respiratory infections 7·4% (6–9) | Lower respiratory infections 6·4% (5·2–7·6) |
| 2 | Lower respiratory infections 11·3% (9·7–12·9) | Diarrhoeal diseases 6·7% (5·3–8) | Ischaemic heart disease 5·5% (4·4–6·4) |
| 3 | Preterm birth complications 6·7% (5·4–8·5) | Preterm birth complications 5·2% (4–6·6) | Diarrhoeal diseases 5·1% (3·9–6·5) |
| 4 | Congenital anomalies 5·0% (3·6–6·5) | Ischaemic heart disease 4·8% (3·9–5·4) | Preterm birth complications 4·7% (3·5–5·9) |
| 5 | Ischaemic heart disease 3·4% (2·7–3·9) | Congenital anomalies 4·2% (3·1–5·8) | Congenital anomalies 4·1% (3·2–5·1) |
| 6 | Neonatal encephalopathy due to birth asphyxia and trauma 3·3% (2·3–4·4) | Cerebrovascular disease 3·6% (2·9–4·1) | Cerebrovascular disease 4% (3·2–4·7) |
| 7 | Cerebrovascular disease 2·9% (2·4–3·3) | Neonatal encephalopathy due to birth asphyxia and trauma 3·5% (2·5–4·7 | Low back and neck pain 3·9% (3·0–4·9) |
| 8 | Other neonatal disorders 2·4% (1·6–3·6) | Low back and neck pain 3·1% (2·3–3·9) | Depressive disorders 3·4% (2·4–4·7) |
| 9 | Iron-deficiency anaemia 2·4% (1·8–3·1) | Depressive disorders 2·8% (2·0–3·8) | Neonatal encephalopathy due to birth asphyxia and trauma 3·3% (2·2–4·6) |
| 10 | Tuberculosis 2·2% (1·7–2·6) | Iron-deficiency anaemia 2·6% (2·0–3·5) | Diabetes mellitus 2·9% (2·5–3·2) |
| Total | |||
| 1 | Diarrhoeal diseases 11·5% (10·1–12·9) | Lower respiratory infections 7·1% (5·9–8·3) | Ischaemic heart disease 6·1% (5·4–6·8) |
| 2 | Lower respiratory infections 10·8% (9·6–11·9) | Diarrhoeal diseases 6·2% (5·3–7·3) | Lower respiratory infections 6·1% (5·2–7·0) |
| 3 | Preterm birth complications 7·1% (6·1–8·7) | Preterm birth complications 5·6% (4·7–6·8) | Preterm birth complications 4·9% (4·1–6·0) |
| 4 | Congenital anomalies 4·8% (3·7–6·4) | Ischaemic heart disease 5·2% (4·7–5·8) | Diarrhoeal diseases 4·8% (4·0–5·7) |
| 5 | Ischaemic heart disease 3·6% (3·2–4·0) | Congenital anomalies 4·1% (3·2–5·7) | Congenital anomalies 4·1% (3·4–5) |
| 6 | Neonatal encephalopathy due to birth asphyxia and trauma 3·6% (2·8–4·5) | Neonatal encephalopathy due to birth asphyxia and trauma 3·8% (2·7–4·9) | Cerebrovascular disease 3·7% (3·2–4·2) |
| 7 | Cerebrovascular disease 2·8% (2·4–3·1) | Cerebrovascular disease 3·3% (2·9–3·7) | Low back and neck pain 3·6% (2·7–4·6) |
| 8 | Other neonatal disorders 2·5% (1·9–3·5) | Low back and neck pain 2·9% (2·1–3·7) | Neonatal encephalopathy due to birth asphyxia and trauma 3·5% (2·7–4·4) |
| 9 | Road injuries 2·3% (2·0–2·9) | Road injuries 2·8% (2·6–3·1) | Road injuries 3% (2·7–3·3) |
| 10 | Meningitis 2·2% (1·8–2·8) | Iron-deficiency anaemia 2·2% (1·6–2·9) | Diabetes mellitus 2·6% (2·4–3·0) |
Data are proportion of DALYs out of all DALYs (95% uncertainty interval).
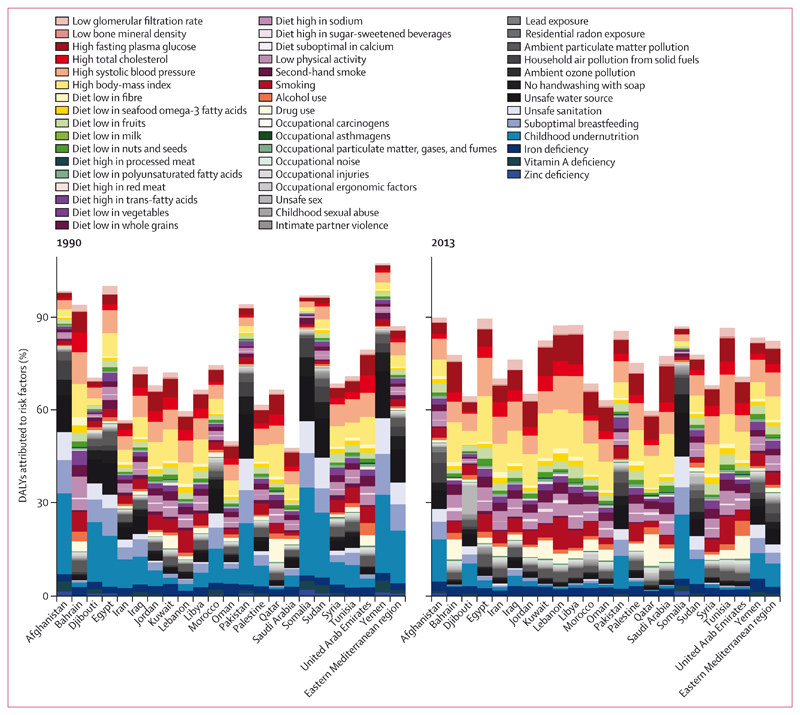
High blood pressure was the leading risk factor for DALYs in 2013, which increased by 83·3% from 1990 (from 8·5 million to 16·1 million DALYs; table 2;8 however, the number of DALYs per 100 000 people increased by only 14%. High blood pressure increased from the fifth highest cause of DALYs in 1990 to first in 2013. Risk factors for DALYs varied by country, with childhood wasting as the leading cause in Somalia, Afghanistan, and Yemen, whereas unsafe sex was the leading cause of DALYs in Djibouti. Conversely, non-communicable disease risk factors were the leading cause of DALYs in high-income countries and middle-income countries (figure 1). DALY risk factors varied by age; child malnutrition and suboptimal breastfeeding affected the younger age groups (aged 7 days to 4 years) and high bodyweight and systolic blood pressure affected the older age groups (aged 60–80 years; appendix p 2).
Table 2. Top ten risk factors contributing to disability-adjusted life-years (DALYs) for the eastern Mediterranean region by sex; 1990, 2005, and 2013.
| 1990 | 2005 | 2013 | |
|---|---|---|---|
| Males | |||
| 1 | Childhood undernutrition 15·8% (14·8–16·6) | Childhood undernutrition 9·3% (8·5–9·9) | High systolic blood pressure 7·9% (7·5–8·2) |
| 2 | Unsafe water source 10·0% (8·4–11·2) | High systolic blood pressure 6·5% (6·2–6·7) | High body-mass index 7·0% (6·6–7·4) |
| 3 | Suboptimal breastfeeding 8·2% (6·2–10·2) | Unsafe water source 6·1% (5·1–6·9) | Childhood undernutrition 7·0% (6·4–7·5) |
| 4 | Unsafe sanitation 6·6% (5·8–7·3) | High body-mass index 5·4% (5·0–5·8) | Smoking 6·1% (5·7–6·5) |
| 5 | high systolic blood pressure4·2% (3·9–4·4 | smoking 5·3% (4·9–5·5) | High fasting plasma glucose 5·0% (4·7–5·3) |
| 6 | No handwashing with soap 3·9% (3·1–4·6) | Suboptimal breastfeeding 4·2% (3·0–5·4) | Unsafe water source 4·9% (4·0–5·6) |
| 7 | Smoking 3·6% (3·3–3·8) | High fasting plasma glucose 4·0% (3·7–4·3) | Suboptimal breastfeeding 3·4% (2·4–4·3) |
| 8 | High body-mass index 3·4% (3·0–3·7) | Unsafe sanitation 3·6% (3·1–4·0) | Ambient particulate matter pollution 3·2% (3·2–3·3) |
| 9 | Household air pollution from solid fuels 2·9% (2·5–3·2) | Ambient particulate matter pollution 2·9% (2·9–2·9) | High total cholesterol 2·9% (2·5–3·3) |
| 10 | Ambient particulate matter pollution 2·8% (2·7–2·8) | Household air pollution from solid fuels 2·7% (2·4–3·1) | Diet high in sodium 2·8% (1·7–4·2) |
| Females | |||
| 1 | Childhood undernutrition 18·3% (17·3–19·3) | Childhood undernutrition 10·9% (10·1–11·5) | Childhood undernutrition 8·2% (7·6–8·6) |
| 2 | Unsafe water source 11·5% (9·6–13·0) | Unsafe water source 6·8% (5·7–7·7) | High body-mass index 8·1% (7·7–8·4) |
| 3 | Suboptimal breastfeeding 8·8% (6·6–11·1) | High body-mass index 6·5% (6·2–6·8) | High systolic blood pressure 7·5% (7·2–7·9) |
| 4 | Unsafe sanitation 7·5% (6·6–8·3) | High systolic blood pressure 6·5% (6·0–6·7) | Unsafe water source 5·5% (4·6–6·3) |
| 5 | No handwashing with soap 4·5% (3·6–5·2) | Suboptimal breastfeeding 4·5% (3·1–5·9) | High fasting plasma glucose 5·0% (4·7–5·2) |
| 6 | High systolic blood pressure 4·2% (3·9–4·4) | High fasting plasma glucose 4·1% (3·8–4·3) | Suboptimal breastfeeding 3·7% (2·5–4·7) |
| 7 | High body-mass index 4·0% (3·7–4·2) | Unsafe sanitation 4·0% (3·5–4·5) | Ambient particulate matter pollution 2·9% (2·9–3·0) |
| 8 | Household air pollution from solid fuels 3·2% (2·8–3·6) | Household air pollution from solid fuels 3·1% (2·8–3·4) | Household air pollution from solid fuels 2·9% (2·6–3·2) |
| 9 | Ambient particulate matter pollution 2·8% (2·6–2·9) | Iron deficiency 2·8% (2·2–3·5) | Iron deficiency 2·9% (2·3–3·6) |
| 10 | Iron deficiency 2·5% (2·0–3·2) | Ambient particulate matter pollution 2·7% (2·7–2·8) | Unsafe sanitation 2·8% (2·4–3·2) |
| Total | |||
| 1 | Childhood undernutrition 17·0% (16·0–17·6) | Childhood undernutrition 10·1% (9·5–10·5) | High systolic blood pressure 7·7% (7·5–7·9) |
| 2 | Unsafe water source 10·7% (9·1–11·9) | High systolic blood pressure 6·5% (6·2–6·6) | Childhood undernutrition 7·5% (7·1–7·8) |
| 3 | Suboptimal breastfeeding 8·5% (6·4–10·6) | Unsafe water source 6·4% (5·5–7·1) | High body-mass index 7·5% (7·2–7·8) |
| 4 | Unsafe sanitation 7·0% (6·2–7·7) | High body-mass index 5·9% (5·6–6·3) | Unsafe water source 5·2% (4·5–5·8) |
| 5 | High systolic blood pressure 4·2% (4·0–4·4) | Suboptimal breastfeeding 4·3% (3·1–5·6) | High fasting plasma glucose 5·0% (4·7–5·2) |
| 6 | No handwashing with soap 4·2% (3·4–4·9) | High fasting plasma glucose 4·0% (3·8–4·2) | Smoking 3·9% (3·8–4·1) |
| 7 | High body-mass index 3·7% (3·3–3·9) | Unsafe sanitation 3·8% (3·4–4·1) | Suboptimal breastfeeding 3·5% (2·5–4·4) |
| 8 | Household air pollution from solid fuels 3·0% (2·7–3·4) | Smoking 3·4% (3·2–3·5) | Ambient particulate matter pollution 3·1% (3·1–3·1) |
| 9 | Ambient particulate matter pollution 2·8% (2·7–2·8) | Household air pollution from solid fuels 2·9% (2·6–3·2) | Household air pollution from solid fuels 2·7% (2·5–3·0) |
| 10 | High fasting plasma glucose 2·4% (2·2–2·6) | Ambient particulate matter pollution 2·8% (2·8–2·8) | Diet high in sodium 2·7% (1·6–3·9) |
Data are proportion of DALYs out of all DALYs (95% uncertainty interval).
Figure 1. DALYs attributed to risk factors in countries of the eastern Mediterranean region, 1990 and 2013.
DALYs=disability-adjusted life-years.
The annualised rates of change for DALY risk factors by burden for the region, low-income, middle-income, and high-income countries are shown in the appendix (pp 3–6). DALYs per 100 000 people attributed to high body-mass index increased by 28% from 1990 to 2013 (from 1961 years per 100 000 people to 2506 years per 100 000 people) and accounted for over 7·3% of total DALYs.8 For high-income countries, high fasting plasma glucose, high body-mass index, alcohol use, and drug use accounted for the highest annual increase with a high DALYs burden.
Decomposition tables for the impact of ageing and population growth on the changes in DALYs from communicable diseases, non-communicable diseases, and injuries for the region are shown in table 3, and in the appendix (pp 18–21) for low-income, middle-income, and high-income countries. DALYs caused by non-communicable diseases and injuries increased (mainly because of population growth), whereas DALYs caused by communicable diseases decreased, although the actual rates of DALYs decreased for all risk factors (table 3).
Table 3. Decomposition of the change of DALYs by cause into contributions from total population growth, population ageing, and changes in age-specific, sex-specific, and cause-specific DALY rates for the eastern Mediterranean region; 1990–2013.
| All causes | Communicable, maternal, neonatal, and nutritional disorders | Non-communicable diseases | Injuries | |
|---|---|---|---|---|
| 1990 DALYs, thousands | 200 590 (190 173 to 211 259) | 109 405 (103 984 to 113 960) | 72 994 (64 276 to 81 552) | 18 191 (16 233 to 21 189) |
| DALYs expected with 2013 population, 1990 population age structure, 1990 DALY rates, thousands | 341 549 (323 445 to 359 991) | 187 154 (177 195 to 195 919) | 123 790 (108 708 to 138 813) | 30 605 (27 404 to 35 345) |
| DALYs expected with 2013 population, 2013 population age structure, 1990 DALY rates, thousands | 300 382 (281 487 to 319 833) | 141 736 (134 031 to 148 771) | 128 693 (113 087 to 144 394) | 29 953 (26 530 to 35 525) |
| 2013 DALYs, thousands | 206 831 (187 375 to 226 886) | 73 251 (67 787 to 79 600) | 112 836 (98 705 to 128 394) | 20 745 (18 617 to 22 910) |
| Median percent change from 1990 due to population growth | 70·3% (69·7 to 70·7) | 71·1% (69·7 to 72·3) | 69·4% (68·2 to 71·4) | 68·3% (65·5 to 70·6) |
| Median percent change from 1990 due to population ageing | –20·6% (–22·3 to –18·8) | –41·5% (–42·5 to –40·5) | 6·9% (3·6 to 9·1) | –3·9% (–8·0 to 1·9) |
| Median percent change from 1990 due to change in DALY rates | –46·6% (–51·4 to –41·9) | –62·6% (–66·7 to –58·2) | –21·8% (–31·1 to –12·5) | –50·3% (–65·1 to –35·1) |
| Median percent change from 1990 to 2013 | 3·1% (–2·9 to 8·7) | –33·1% (–37·3 to –28·5) | 54·5% (44·5 to 64·5) | 14·3% (0·9 to 28·6) |
Data are median (95% CI). DALY=disability-adjusted life-year.
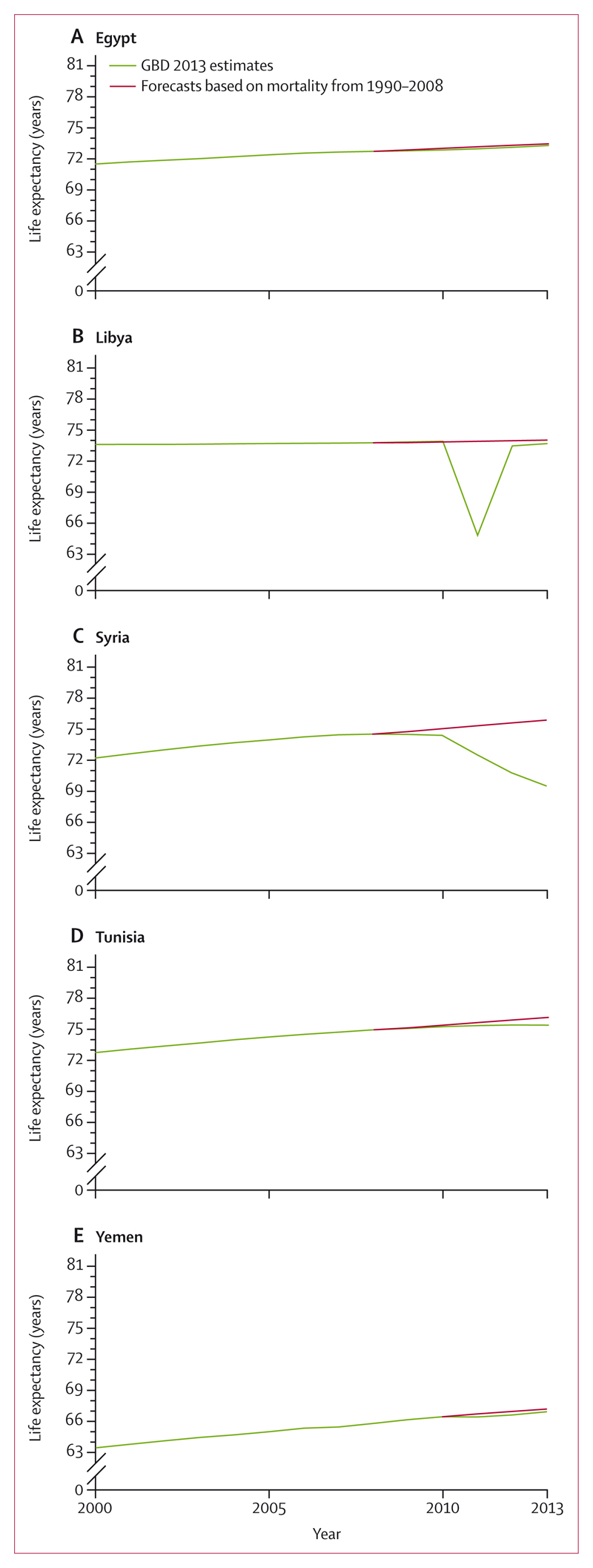
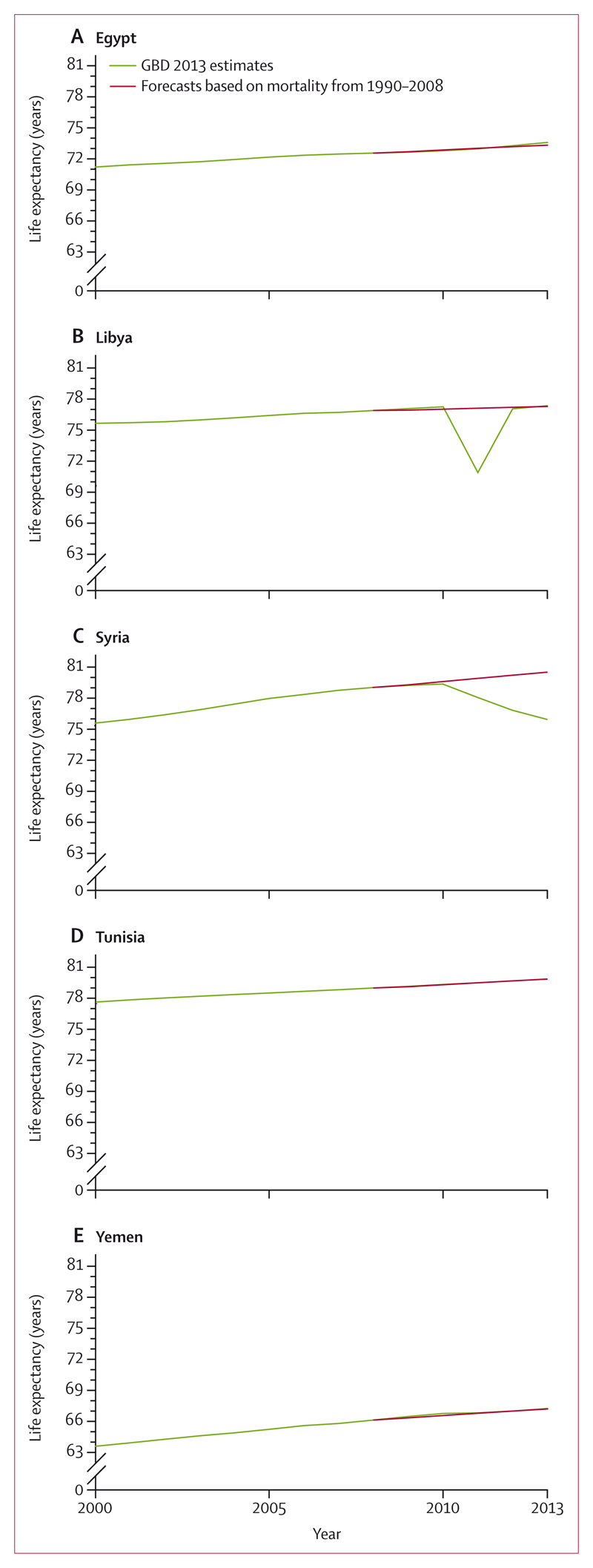
Projected life expectancy using figures from 2009 until 2013, based on the trends observed from 1990 to 2008 compared with observed life expectancy from GBD 2013 are shown in figures 2 and 3. From 1990 to 2010, Egypt, Libya, Syria, and Yemen had a steady increase in life expectancy of about 0·25 years per year, with a slightly higher increase in females (about 0·3 years) than in males. However, Egypt, Tunisia, and Yemen have lost about 0·25 years of life expectancy due to the uprising that began in 2010. When comparing observed life expectancy to expected life expectancy if no crisis had occurred, we found a large decrease in life expectancy in Libya of more than 9 years for males and 6 years for females. Conversely, a steady decrease in life expectancy was observed in Syria because of the continuing war. Therefore, between 1990 and 2013 life expectancy for Syria would have been 6 years higher than observed for males and 5 years higher for females had the crisis not happened. Moreover, our analyses showed that several countries in the region have experienced a slow-down in lowering infant mortality rate. For example, in Syria the annualised rate of reduction in infant mortality between 2010 to 2013 was –9·1%, in sharp contrast with the rate of decrease of 6·0% before 2010.9
Figure 2. Projected versus observed life expectancy at birth of males in Egypt, Libya, Syria, Tunisia, and Yemen, 2000–13.
GBD=Global Burden of Disease.
Figure 3. Projected versus observed life expectancy at birth of females in Egypt, Libya, Syria, Tunisia, and Yemen, 2000–13.
GBD=Global Burden of Disease.
Discussion
The eastern Mediterranean region is facing numerous health challenges as a result of previous wars, recent revolutions, and the wars that followed, and of ageing and population growth. Life expectancy at birth in the region increased from 65 years in 1990 to 71 years in 2013, with an annual increase of about 0·26 years. However, according to our study, the situation has resulted in deteriorating health conditions for many countries that are threatening these gains and will have an impact on the region and worldwide. Hence, on the basis of our results, we call for increased investment in health in the region, and suppression of the conflicts.
Our study showed a rapid increase in the burden of mental and drug-use disorders in the region. Unfortunately, the rise in burden of mental health problems has not been met with investment in prevention by most countries in the region, with few exceptions, such as Lebanon and Qatar.10,11 Mental health is not viewed as a major burden by many countries and is not discussed in the agendas of many international agencies and health ministries. We hope that our findings will shed light and lead to more attention by global and regional health agencies to tackle this rising burden.
Similarly, the rapid rise in non-communicable diseases is alarming. Diabetes, for example, is a heavy burden on many countries, with deaths increasing from 12 to 19 per 100 000 people. One study12 showed a high cost of diabetes in Saudi Arabia. These trends, irrespective of their cause, will lead to a strain on finances and human resources in a region where they are already scarce. The prevention and control of risk factors associated with non-communicable diseases should be a priority for the region.
The spread of communicable diseases in the eastern Mediterranean region is of concern. The Hajj annual pilgrimage presents a challenge to health planners. The mass gathering for Hajj has led to several outbreaks of infectious disease such as meningitis and polio in Saudi Arabia and other countries.13 Moreover, the gathering in Iraq for Ashura, a day of mass mourning, has the same potential for the spread of disease.14 In most of these countries, kissing is a normal way of greeting people, and sharing food and social congregations are common. This cultural behaviour has complicated efforts to control Middle East respiratory syndrome (MERS) outbreaks in Saudi Arabia and its spread to other countries.15 Containment and control of emerging diseases and infections in the eastern Mediterranean region is a national interest for all countries.
Our study showed a rise in the burden of disease due to illicit drugs in the region. Several studies have reported that, during stress, individuals might engage in risky behaviours.16 Unfortunately, the response of many countries has been law enforcement measures and strict punishment.17 The region is in need of comprehensive socioculturally appropriate approaches towards education, prevention, and early identification and treatment.
Road-traffic injuries are the leading cause of DALYs in men in high-income countries throughout the region, and rank increasingly higher in low-income and middle-income countries than in previous years. Unfortunately, many countries in the region have yet to fully implement policies and legislation conducive to road safety, and need to strengthen their trauma care systems.18
One of the main challenges and threats for the region is the environment. Most countries in the region are facing water shortages due to population pressure, increasing water demand, and natural climate variability. Moreover, climate change has resulted in increased temperatures in the region, and a major part of the eastern Mediterranean region is projected to be uninhabitable in the next 50–80 years.19 Additionally, most countries in the region are not food sufficient and rely heavily on imports to meet growing demands. Development of a plan to address these issues is crucial for the region and the world, because they will affect the stability and future of the region.
Unrest, civil conflicts, and wars have had a big impact on the burden of disease in the eastern Mediterranean region. However, the long-term impact of the unrest is not yet known. The region is losing its health talents, as many medical doctors and health professionals leave conflict areas in search of a better life elsewhere.20 Moreover, historically high rates of unemployment in the region have caused many other people to seek work elsewhere.
Many countries in the region are facing other health challenges that they are not equipped for. For example, the conflict in Syria has resulted in millions of individuals being displaced internally and millions of others forced to seek refuge in neighbouring countries. Only when an influx of Syrian refugees into Europe occurred did this crisis receive widespread media coverage. There is a need for long-term planning to improve the health of and stabilise the region.
The infrastructure in several of these countries has been destroyed because of war. Water and sanitation will pose major challenges until proper reconstruction is achieved. Unfortunately, these effects will lead to an increased rate of disease spread and outbreaks, which must be properly controlled. Moreover, investment in health information systems in the region is urgently needed. This investment should be a priority for countries and donors once the political situation improves.
Our study showed that many of the health gains achieved by countries in the region are at risk of slowing down. In fact, infant mortality has risen in some countries. It is sad to see that Syria, a country with a good performance in reducing child mortality in the past, saw a rise from 2010 to 2013. Syria is falling behind countries in sub-Saharan Africa when it comes to the rate of change in infant mortality.
The political situation in the region continues to be uncertain; since 2013, the wars in Syria and Libya have escalated, and a war has started in Yemen. In some areas, residents are facing starvation and the public health and medical systems are about to collapse. Moreover, wars and unrest in Afghanistan, Iraq, Palestine, and Somalia have continued or re-emerged, and for many people in these countries, survival is the main challenge, not health. The eastern Mediterranean region is facing several health challenges at a time of uncertainty, and the countries in this region are struggling to meet these challenges.
Events in the past 5 years have shown that the wellbeing of people in the eastern Mediterranean region crosses beyond its borders, as exemplified by the spread of MERS to South Korea and the outbreak of infectious diseases in refugee camps in Lebanon and Jordan. A healthy eastern Mediterranean region is a politically stable eastern Mediterranean region, one from which the whole world will benefit. Based on our findings, we call for stepping up efforts at the regional and local levels to improve health, identify barriers to scaling up health promotion and disease prevention services, and to stabilise the region.
Supplementary Material
Research in context.
Evidence before this study
The Global Burden of Disease Study 2010 (GBD 2010) became available in 2012. GBD 2010 reported on disability-adjusted life-years (DALYs), health-adjusted life expectancy, and 67 risks and risk clusters by 21 world regions and 188 countries.
GBD 2010 covered 20 age and sex groups.
Added value of this study
GBD 2013 includes an annual assessment covering 188 countries, from 1990 to 2013. It covers 306 diseases and injuries, 1233 sequelae, and 79 risk factors. GBD 2013 included key methodological differences from GBD 2010, which were inclusion of new data through updated systematic reviews and through the contribution of unpublished data sources from many collaborators; use of a counterfactual approach for estimating diarrhoea and pneumonia causes; elaboration of the sequelae list to include asymptomatic states; use of more detailed nature of injury codes (N-codes); improvements to the Bayesian meta-regression method; increased simulation size for comorbidity; estimation of the prevalence of injuries by cohort; and use of a new method to estimate the distribution of mild, moderate, and severe anaemia by cause. This study provides an overview of the comprehensive burden of diseases and risk factors for the eastern Mediterranean region.
Implications of all the available evidence
The eastern Mediterranean region is facing numerous health challenges, as a result of previous wars, revolutions, the wars that followed, and ageing and population growth. These challenges will have a major impact on health outcomes and available resources. The region has historically seen improvements in life expectancy and other health indicators even under stress. However, according to our study, the current situation has resulted in deteriorating health conditions for many countries that are threatening these gains and will have an impact on the region and the rest of the world. On the basis of our data, we call for increased investment in health in the region and the end of ongoing conflicts.
Acknowledgments
This study was funded by the Bill & Melinda Gates Foundation. LJA-R was supported by Qatar National Research Fund (NPRP 9-040-3-008), who provided the main funding for the generation of data provided by LJA-R to the study. RRAB was supported by funding from The Brien Holden Vision Institute. AKa was supported by funding from Oklahoma Council for Advancement of Science & Technology. GAM is a US government employee. KR was supported by funding from the UK National Institute for Health Research Oxford Biomedical Research Centre, National Institute for Health Research Career Development Fellowship, and Oxford Martin School.
Footnotes
Contributors
AHM and CJLM prepared the first draft. AHM and CJLM finalised the draft based on comments from other authors and reviewer feedback. All other authors provided data, developed models, analysed data, reviewed results, provided guidance on methodology, or reviewed the manuscript.
Declaration of interests
We declare no competing interests.
Contributor Information
Mohamed Magdy Abd El Razek, Aswan University Hospital, Aswan Faculty of Medicine, Aswan, Egypt.
Safa Abdalla, Sudanese Public Health Consultancy Group, Solihull, UK.
Prof Foad Abd-Allah, Department of Neurology, Cairo University, Cairo, Egypt.
Jerry P Abraham, Family Medicine Residency Program at California Hospital, University of Southern California, Los Angeles, CA, USA; Institute for Global Health, Harvard University, Boston, MA, USA.
Laith J Abu-Raddad, Infectious Disease Epidemiology Group, Weill Cornell Medical College in Qatar, Doha, Qatar.
Niveen M E Abu-Rmeileh, Institute of Community and Public Health, Birzeit University, Ramallah, Palestine.
Abdulwahab A Al-Nehmi, Ministry of Health, Sana’a, Yemen.
Ali S Akanda, University of Rhode Island, Kingston, RI, USA.
Hanan Al Ahmadi, Majlis Al Shura, Riyadh, Saudi Arabia.
Mazin J Al Khabouri, Ministry of Health, Muscat, Oman.
Faris H Al Lami, College of Medicine, University of Baghdad, Baghdad, Iraq.
Zulfa A Al Rayess, The Saudi Center for Evidence Based Healthcare, Riyadh, Saudi Arabia.
Deena Alasfoor, Ministry of Health, Muscat, Oman.
Fadia S AlBuhairan, King Abdullah Specialized Children’s Hospital, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia; King Abdullah International Medical Research Center, Riyadh, Saudi Arabia.
Saleh F Aldhahri, King Saud University, Riyadh, Saudi Arabia; King Fahad Medical City, Riyadh, Saudi Arabia.
Suliman Alghnam, King Abdullah International Medical Research Center, Riyadh, Saudi Arabia; Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA.
Samia Alhabib, King Abdullah Bin Abdulaziz University Hospital, Riyadh, Saudi Arabia.
Nawal Al-Hamad, Public Authority for Food and Nutrition, Kuwait.
Raghib Ali, University of Oxford, Oxford, UK.
Syed Danish Ali, University of London, London, UK; Institute and Faculty of Actuaries, Oxford, UK.
Mohammad Alkhateeb, Pediatric Department, King Khalid University Hospital, Riyadh, Saudi Arabia.
Mohammad A AlMazroa, Kingdom of Saudi Arabia Ministry of Health, Riyadh, Saudi Arabia.
Mahmoud A Alomari, Division of Physical Therapy, Department of Rehabilitation Sciences, Irbid, Jordan.
Rajaa Al-Raddadi, Kingdom of Saudi Arabia Ministry of Health, Riyadh, Saudi Arabia.
Ubai Alsharif, Charité Universitätsmedizin, Berlin, Germany.
Nihaya Al-Sheyab, Maternal and Child Health Department, Irbid, Jordan.
Shirina Alsowaidi, Department of Internal Medicine, College of Medicine and Health Sciences, United Arab Emirates University, Al-Ain, United Arab Emirates.
Mohamed Al-Thani, Supreme Council of Health, Doha, Qatar.
Khalid A Altirkawi, King Saud University, Riyadh, Saudi Arabia.
Azmeraw T Amare, Discipline of Psychiatry, School of Medicine, University of Adelaide, Adelaide, SA, Australia; College of Medicine and Health Sciences, Bahir Dar, Ethiopia.
Heresh Amini, Environmental Health Research Center, Kurdistan University of Medical Sciences, Sanandaj, Iran; Department of Epidemiology and Public Health, Swiss Tropical and Public Health Institute, Basel, Switzerland; University of Basel, Basel, Switzerland.
Walid Ammar, Ministry of Public Health, Beirut, Lebanon.
Palwasha Anwari, Kabul, Afghanistan.
Hamid Asayesh, Department of Medical Emergency, School of Paramedic, Qom University of Medical Sciences, Qom, Iran.
Rana Asghar, South Asian Public Health Forum, Islamabad, Pakistan.
Prof Ali M Assabri, Faculty of Medicine and Health Sciences, Sana’a University, Sana’a, Yemen.
Reza Assadi, Mashhad University of Medical Sciences, Mashhad, Iran.
Umar Bacha, School of Health Sciences, University of Management and Technology, Lahore, Pakistan.
Alaa Badawi, Public Health Agency of Canada, Toronto, ON, Canada.
Talal Bakfalouni, Ministry of Health, Damascus, Syria.
Mohammed O Basulaiman, Kingdom of Saudi Arabia Ministry of Health, Riyadh, Saudi Arabia.
Shahrzad Bazargan-Hejazi, Charles R Drew University of Medicine and Science, Los Angeles, CA, USA.
Neeraj Bedi, College of Public Health and Tropical Medicine, Jazan, Saudi Arabia.
Amit R Bhakta, National Institute of Mental Health, Montgomery Village, MD, USA.
Zulfiqar A Bhutta, Centre of Excellence in Women and Child Health, Karachi, Pakistan; Centre for Global Child Health, The Hospital for Sick Children, Toronto, ON, Canada.
Aref A Bin Abdulhak, University of Iowa Hospitals and Clinics, Iowa City, IA, USA.
Soufiane Boufous, Transport and Road Safety (TARS) Research, University of New South Wales, Sydney, NSW, Australia.
Rupert R A Bourne, Vision & Eye Research Unit, Anglia Ruskin University, Cambridge, UK.
Hadi Danawi, Walden University, Minneapolis, MN, USA.
Jai Das, Department of Paediatrics and Child Health, Karachi, Pakistan.
Amare Deribew, Nuffield Department of Medicine, Oxford, UK; KEMRI-Wellcome Trust Research Programme, Kilifi, Kenya.
Eric L Ding, Harvard T H Chan School of Public Health, Harvard University, Boston, MA, USA.
Adnan M Durrani, National Institutes of Health, Montgomery Village, MD, USA.
Yousef Elshrek, Food Science Department, Faculty of Agriculture, University of Tripoli, Tripoli, Libya.
Mohamed E Ibrahim, Cardiovascular Diseases Control and Prevention Program, The Saudi Center for Evidence Based Healthcare, Riyadh, Saudi Arabia.
Babak Eshrati, Ministry of Health and Medical Education, Tehran, Iran; Arak University of Medical Sciences, Arak, Iran.
Alireza Esteghamati, Endocrinology and Metabolism Research Center, Tehran University of Medical Sciences, Tehran, Iran.
Imad A D Faghmous, London School of Hygiene & Tropical Medicine, London, UK.
Farshad Farzadfar, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Research Center, Tehran University of Medical Sciences, Tehran, Iran.
Andrea B Feigl, Department of Global Health and Population, Harvard University, Boston, MA, USA.
Seyed-Mohammad Fereshtehnejad, Department of Neurobiology, Care Sciences and Society, Karolinska Institute, Stockholm, Sweden.
Irina Filip, Kaiser Permanente Psychiatry Residency Program, Fontana, CA, USA.
Florian Fischer, Bielefeld University, Bielefeld, Germany.
Fortuné G Gankpé, Leras Afrique, Cotonou, Benin; CHU Hassan II, Fez, Morocco.
Ibrahim Ginawi, College of Medicine, University of Hail, Hail, Saudi Arabia.
Melkamu Dedefo Gishu, Haramaya University, Dira Dawa, Ethiopia; Kersa Health and Demographic Surveillance System, Harar, Ethiopia.
Rahul Gupta, West Virginia Bureau for Public Health, Charleston, WV, USA.
Rami M Habash, Kingdom of Saudi Arabia Ministry of Health, Riyadh, Saudi Arabia.
Nima Hafezi-Nejad, Endocrinology and Metabolism Research Center, Tehran University of Medical Sciences, Tehran, Iran.
Prof Randah R Hamadeh, Arabian Gulf University, Manama, Bahrain.
Hayet Hamdouni, Direction des Soins de Santé de Base, Ministry of Health, Tunis, Tunisia.
Samer Hamidi, Hamdan Bin Mohammed Smart University, Dubai, United Arab Emirates.
Hilda L Harb, Ministry of Public Health, Beirut, Lebanon.
Mohammad Sadegh Hassanvand, Center for Air Pollution Research, Institute for Environmental Research, Tehran University of Medical Sciences, Tehran, Iran.
Prof Mohammad T Hedayati, Department of Medical Mycology and Parasitology, School of Medicine, Mazndaran University of Medical Sciences, Sari, Iran.
Pouria Heydarpour, Multiple Sclerosis Research Center, Neuroscience Institute, Tehran University of Medical Sciences, Tehran, Iran.
Prof Mohamed Hsairi, Salah Azaiz Institute, Tunis, Tunisia.
Abdullatif Husseini, Qatar University, Doha, Qatar.
Nader Jahanmehr, School of Public Health, Shahid Beheshti University of Medical Sciences, Tehran University of Medical Sciences, Tehran, Iran.
Prof Vivekanand Jha, The George Institute for Global Health India, University of Oxford, New Delhi, India.
Jost B Jonas, Ruprecht-Karls-University Heidelberg, Department of Ophthalmology, Medical Faculty Mannheim, Mannheim, Germany.
Nadim E Karam, University of Balamand, Beirut, Lebanon.
Amir Kasaeian, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Research Center, Tehran University of Medical Sciences, Tehran, Iran; Hematology–Oncology and Stem Cell Transplantation Research Center, Tehran University of Medical Sciences, Tehran, Iran.
Nega Assefa Kassa, Haramaya University, Harari, Ethiopia.
Anil Kaul, Oklahoma State University Center for Health Sciences, Tulsa, OK, USA.
Prof Yousef Khader, Jordan University of Science and Technology, Irbid, Jordan.
Shams Eldin A Khalifa, Supreme Council of Health, Doha, Qatar.
Ejaz A Khan, Health Services Academy, Islamabad, Pakistan.
Gulfaraz Khan, Department of Microbiology and Immunology, College of Medicine and Health Sciences, United Arab Emirates University, Al-Ain, United Arab Emirates.
Tawfik Khoja, Health Ministers’ Council for Cooperation Council States, Riyadh, Saudi Arabia.
Ardeshir Khosravi, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Research Center, Tehran University of Medical Sciences, Tehran, Iran; Iranian Ministry of Health and Medical Education, Tehran, Iran.
Yohannes Kinfu, Centre for Research & Action in Public Health, Faculty of Health, University of Canberra, Canberra, ACT, Australia.
Barthelemy Kuate Defo, Department of Demography and Public Health Research Institute, University of Montreal, Montreal, QC, Canada and Department of Social and Preventive Medicine, School of Public Health, University of Montreal, Montreal, QC, Canada.
Arjun Lakshmana Balaji, Indegene, Bangalore, India.
Raimundas Lunevicius, Aintree University Hospital National Health Service Foundation Trust, Liverpool, UK; School of Medicine, University of Liverpool, Liverpool, UK.
Prof Carla Makhlouf Obermeyer, Center for Research on Population and Health, Faculty of Health Sciences, American University of Beirut, Beirut, Lebanon.
Reza Malekzadeh, Digestive Diseases Research Institute, Tehran University of Medical Sciences, Tehran, Iran.
Morteza Mansourian, Department of Health Education and Promotion, School of Health, Iran University of Medical Sciences, Tehran, Iran.
Prof Wagner Marcenes, Queen Mary University of London, London, UK.
Habibolah Masoudi Farid, State Welfare Organisation, Tehran, Iran.
Alem Mehari, Howard University College of Medicine, Washington, DC, USA.
Abla Mehio-Sibai, Department of Epidemiology & Population Health, Faculty of Health Sciences, American University of Beirut, Beirut, Lebanon.
Prof Ziad A Memish, Kingdom of Saudi Arabia Ministry of Health, Riyadh, Saudi Arabia; College of Medicine, Alfaisal University, Riyadh, Saudi Arabia.
George A Mensah, Center for Translation Research and Implementation Science, National Heart, Lung, and Blood Institute, Montgomery Village, MD, USA.
Karzan A Mohammad, University of Salahaddin, Erbil, Iraq.
Prof Ziad Nahas, Medical Center, American, University of Beirut, Beirut, Lebanon.
Jamal T Nasher, Ministry of Public Health and Population, Sana’a, Yemen.
Haseeb Nawaz, Southern Illinois University, Springfield, IL, USA.
Prof Chakib Nejjari, Faculty of Medicine, Fez, Morocco.
Muhammad Imran Nisar, Aga Khan University, Karachi, Pakistan.
Saad B Omer, Emory University, Atlanta, GA, USA.
Mahboubeh Parsaeian, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Research Center, Tehran University of Medical Sciences, Tehran, Iran; Department of Epidemiology and Biostatistics, School of Public Health, Tehran, University of Medical Sciences, Tehran, Iran.
Emmanuel K Peprah, National Heart, Lung, and Blood Institute, Bethesda, MD, USA.
Aslam Pervaiz, Postgraduate Medical Institute, Lahore, Pakistan.
Farshad Pourmalek, University of British Columbia, Vancouver, BC, Canada.
Prof Dima M Qato, College of Pharmacy, University of Illinois, Chicago, IL, USA.
Mostafa Qorbani, Department of Community Medicine, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran.
Amir Radfar, A T Still University of Health Sciences, Kirksville, MO, USA.
Anwar Rafay, Contech International Health Consultants, Lahore, Pakistan.
Kazem Rahimi, University of Oxford, Oxford, UK.
Vafa Rahimi-Movaghar, Sina Trauma and Surgery Research Center, Tehran University of Medical Sciences, Tehran, Iran.
Sajjad Ur Rahman, Hamad Medical Corporation, Doha, Qatar.
Rajesh K Rai, Society for Health and Demographic Surveillance, Suri, India.
Prof Saleem M Rana, Contech International Health Consultants, Lahore, Pakistan; Contech School of Public Health, Lahore, Pakistan.
Sowmya R Rao, Department of Surgery, Boston University School of Medicine, Boston, MA, USA.
Amany H Refaat, Walden University, Minneapolis, MN, USA; Suez Canal University, Ismailia, Egypt.
Serge Resnikoff, Brien Holden Vision Institute, University of New South Wales, Sydney, NSW, Australia; International Health and Development, Geneva, Switzerland.
Gholamreza Roshandel, Digestive Diseases Research Institute, Tehran University of Medical Sciences, Tehran, Iran; Golestan Research Center of Gastroenterology and Hepatology, Golestan University of Medical Sciences, Gorgan, Iran.
Georges Saade, Lebanese University, Beirut, Lebanon; Bellevue Medical Center, Mansourieh El Metn, Lebanon.
Mohammad Y Saeedi, Kingdom of Saudi Arabia Ministry of Health, Riyadh, Saudi Arabia.
Mohammad Ali Sahraian, Multiple Sclerosis Research Center, Neuroscience Institute, Tehran University of Medical Sciences, Tehran, Iran.
Shadi Saleh, Department of Health Management and Policy, American University of Beirut, Beirut, Lebanon.
Lidia Sanchez-Riera, Institut d’Investigacio Biomedica de Bellvitge (IDIBELL), L’Hospitalet de Llobregat, Barcelona, Spain.
Maheswar Satpathy, All India Institute of Medical Sciences, New Delhi, India.
Sadaf G Sepanlou, Digestive Diseases Research Institute, Tehran University of Medical Sciences, Tehran, Iran.
Tesfaye Setegn, Bahir Dar University, Bahir Dar, Ethiopia.
Amira Shaheen, Department of Public Health, An-Najah University, Nablus, Palestine.
Saeid Shahraz, Tufts Medical Center, Boston, MA, USA.
Sara Sheikhbahaei, Endocrinology and Metabolism Research Center, Tehran University of Medical Sciences, Tehran, Iran.
Kawkab Shishani, Washington State University, Spokane, WA, USA.
Prof Karen Sliwa, Faculty of Health Sciences, Hatter Institute for Cardiovascular Research in Africa, University of Cape Town, Cape Town, South Africa.
Mohammad Tavakkoli, Westchester Medical Center, Valhalla, NY, USA.
Abdullah S Terkawi, Department of Anesthesiology, Riyadh, Saudi Arabia; Department of Anesthesiology, University of Virginia, Charlottesville, VA, USA.
Olalekan A Uthman, Warwick Medical School, University of Warwick, Coventry, UK.
Ronny Westerman, Federal Institute for Population Research, Wiesbaden, Germany; German National Cohort Consortium, Heidelberg, Germany.
Mustafa Z Younis, Jackson State University, Jackson, MS, USA.
Prof Maysaa El Sayed Zaki, Faculty of Medicine, Mansoura University, Mansoura, Egypt.
Faiez Zannad, Clinical Investigation Centre INSERM, Université de Lorraine, Vandoeuvre les Nancy, France; CHU de Nancy, Vandoeuvre les Nancy, France.
Abdullah A Al Rabeeah, Kingdom of Saudi Arabia Ministry of Health, Riyadh, Saudi Arabia.
Prof Alan D Lopez, Institute for Health Metrics and Evaluation, University of Washington, Seattle, WA, USA; Melbourne School of Population and Global Health, University of Melbourne, Melbourne, VIC, Australia.
Prof Christopher J L Murray, Institute for Health Metrics and Evaluation, University of Washington, Seattle, WA, USA.
References
- 1.WHO. WHO Regional Office for the Eastern Mediterranean. [accessed May 22, 2016]; http://www.emro.who.int/entity/about-us/index.html.
- 2.Mandil A, Chaaya M, Saab D. Health status, epidemiological profile and prospects: Eastern Mediterranean region. Int J Epidemiol. 2013;42:616–26. doi: 10.1093/ije/dyt026. [DOI] [PubMed] [Google Scholar]
- 3.Mokdad AH, Jaber S, Aziz MIA, et al. The state of health in the Arab world, 1990–2010: an analysis of the burden of diseases, injuries, and risk factors. Lancet. 2014;383:309–20. doi: 10.1016/S0140-6736(13)62189-3. [DOI] [PubMed] [Google Scholar]
- 4.Naghavi M, Wang H, Lozano R, et al. Global, regional, and national age–sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–71. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murray CJL, Barber RM, Foreman KJ, et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet. 2015;386:2145–91. doi: 10.1016/S0140-6736(15)61340-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vos T, Barber RM, Bell B, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forouzanfar MH, Alexander L, Anderson HR, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2287–323. doi: 10.1016/S0140-6736(15)00128-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Institute for Health Metrics and Evaluation, GBD. GBD Compare: cause of disease or injury, stacked bar chart. [accessed Dec 11, 2014];2013 http://viz.healthmetricsandevaluation.org/gbd-compare/
- 9.Institute for Health Metrics and Evaluation, MDG Viz. Viz Hub: compare annualized rates of decline in each MDG from 1990–2010. [accessed June 3, 2016]; http://vizhub.healthdata.org/mdg.
- 10.El Chammay R, Ammar W. Syrian crisis and mental health system reform in Lebanon. Lancet. 2014;384:494. doi: 10.1016/S0140-6736(14)61329-5. [DOI] [PubMed] [Google Scholar]
- 11.Supreme Council of Health (Qatar) Qatar National Mental Health Strategy. Changing minds, changing lives 2013–2018. Qatar: Supreme Council of Health; 2013. [Google Scholar]
- 12.Mokdad AH, Tuffaha M, Hanlon M. Cost of diabetes in the Kingdom of Saudi Arabia, 2014. J Diabetes Metab. 2015;6:575. [Google Scholar]
- 13.Ahmed QA, Arabi YM, Memish ZA. Health risks at the Hajj. Lancet. 2006;367:1008–15. doi: 10.1016/S0140-6736(06)68429-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al-Lami F, Al-Fatlawi A, Bloland P, et al. Pattern of morbidity and mortality in Karbala hospitals during Ashura mass gathering at Karbala, Iraq, 2010. East Mediterr Health J. 2013;19:S13–18. [PubMed] [Google Scholar]
- 15.Hui DS, Perlman S, Zumla A. Spread of MERS to South Korea and China. Lancet Respir Med. 2015;3:509–10. doi: 10.1016/S2213-2600(15)00238-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Psychological and emotional effects of the September 11 attacks on the World Trade Center—Connecticut, New Jersey, and New York, 2001. MMWR Morb Mortal Wkly Rep. 2002;51:784–86. [PubMed] [Google Scholar]
- 17.Amnesty International. The application of the death penalty for drug-related offences and its serious impact on the enjoyment of human rights. [accessed Dec 10, 2015];2015 Sep 11; https://www.amnesty.org/en/documents/ior40/2437/2015/en/
- 18.WHO. Road safety in the Eastern Mediterranean Region: facts from the global status report on road safety 2013. Egypt: World Health Organization; 2013. [accessed Nov 9, 2015]. http://www.who.int/violence_injury_prevention/road_safety_status/2013/report/factsheet_emro_en.pdf. [Google Scholar]
- 19.Schär G. Climate extremes: the worst heat waves to come. Nat Clim Change. 2016;6:128–29. [Google Scholar]
- 20.Mohammed bin Rashid Al Maktoum Foundation, UNDP Regional Bureau for Arab States. Arab knowledge report 2014. Youth and localisation of knowledge. [accessed May 22, 2016];2014 http://www.undp.org/content/dam/rbas/report/UNDP-GENERAL-REPORT-ENG.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.