Abstract
Objective:
Tobacco harm reduction is one of the most divisive issues in tobacco control. This study analyzed a comprehensive set of articles published in peer-reviewed journals, assessing support for or opposition to the promotion of tobacco product substitution (i.e. substitutional use of smokeless tobacco, potentially reduced exposure products (PREPs), or electronic cigarette products). This study also examined associations between funding sources and stance on tobacco harm reduction.
Methods:
PubMed, Embase, Web of Science, and PsycINFO were searched for articles pertaining to tobacco harm reduction, including all papers, comments, and editorials published in peer-reviewed journals between 1992 and July 26, 2016. According to predefined criteria, investigators double coded article type, funding source, and support or opposition to promotion of smokeless tobacco and/or e-cigarettes as tobacco harm reduction.
Results:
Searches retrieved 826 articles, including non-empirical articles (21%), letters or commentaries (34%), editorials (5%), cross-sectional studies (15%), systematic reviews and meta-analyses (3%), and randomized controlled trials (2%). Overall, 49% of articles endorsed tobacco harm reduction, 42% opposed it, and 9% took neutral/mixed positions. Funding or support from the e-cigarette industry (OR: 20.9. 95%CI: 5.3, 180.7), tobacco industry (OR: 59.4 95%CI: 10.1, +infinity) or pharmaceutical industry (OR: 2.18 95%CI: 1.3, 3.7) was significantly associated with a supportive stance.
Discussion:
Of published articles on tobacco harm reduction, 23.9% disclosed support by industry. Non-industry funded articles were nearly evenly divided in stance; industry funded articles, however, favored tobacco harm reduction. Due to their quantity, letters and comments in peer-review publications may influence perceptions of tobacco harm reduction when empirical studies lack consensus.
Introduction
In 2001, the Institute of Medicine conditionally endorsed reduced harm tobacco products as potentially reducing individual exposure to tobacco toxicants and improving population-level public health outcomes.1 Since then, tobacco harm reduction (THR) has been increasingly interpreted as the complete or partial substitution of cigarettes with purportedly reduced-harm tobacco products (e.g. smokeless tobacco, potentially reduced exposure products (PREPs), or electronic cigarettes).1,2,3 However, this strategy is supported by few empirical studies: the American College of Physicians, the US Preventative Services Task Force, and the National Academy of Sciences, Engineering, and Medicine all concluded that there is insufficient evidence from randomized controlled trials to support the use of e-cigarettes for smoking cessation.4–6 Nonetheless, THR proponents argue that alternative tobacco products should be promoted for cessation or long-term nicotine maintenance if users prefer such products to established cessation aids like nicotine replacement therapies (NRT).3,7,8 Other public health experts argue that alternative tobacco products should not be endorsed, due to a lack of evidence demonstrating these products’ long-term safety and cessation efficacy.9–11
Articles on THR have proliferated since 2001: a search using the keywords “tobacco” and “harm reduction” on PubMed yielded 3 papers in 1999, increasing to 112 in 2016 alone. Published studies, reviews, and opinions exhibit strong differences in their stance on the safety and effectiveness of THR products, and there may be an association between stance and funding or financial conflicts of interest. The tobacco industry has actively promoted new tobacco products including electronic cigarettes, embracing the concept and terminology of tobacco harm reduction.12–15 Given the tobacco, electronic-cigarette, and pharmaceutical industries’ substantial financial interest in tobacco harm reduction, this study quantified industry influence on stance in published articles regarding tobacco harm reduction.
This article presents an analysis of conclusions and stance across a comprehensive set of articles on tobacco harm reduction (THR) including papers of all formats, funding disclosures, and arguments for and against THR published in peer-reviewed journals between 1992 and 2016. Similar to a prior systematic review,16 this review weighed neither the quality of a particular study type, nor evidence for a single clinical outcome. Rather, this review deliberately included all article types (such as non-empirical articles, letters, and comments) so as to systematically evaluate the role of disclosed funding in influencing the academic discourse on tobacco harm reduction. Whereas previous studies have reviewed existing literature on the harm of electronic cigarettes (e-cigarettes),17 smokeless tobacco,18,19 and snus,20 each review acknowledged a paucity of reliable randomized controlled trials in the literature.9 This systematic review included a comprehensive broad review of all published articles from peer-reviewed journals on THR, and examined whether funding, industry affiliation, or other declared support from the tobacco, e-cigarette or pharmaceutical industry was associated with support or opposition to THR.
Methods
A comprehensive review of all papers, letters, and comments on the topic of tobacco harm reduction published in peer-reviewed journals between 1992 and 2016 was conducted. Due to the wide variety of publication types and a non-clinical outcome, the study did not fit the typical format used in systematic review registration; thus a typical review protocol is not available. However, the search strings and complete codebook are provided as supplements to this article.
Data Sources and Searches
With the help of a knowledge synthesis librarian, PubMed, Embase, Web of Science, and PsycINFO were searched for all articles relevant to tobacco harm reduction and associated topics published between January 1, 1992 and July 26, 2016 using a comprehensive search string (Supplement 1). Assessing term frequencies on PubMed, investigators identified 1992 as the first year that the term and concept of “tobacco harm reduction” became popular. This rise in popularity coincided with the introduction of potentially reduced exposure products (PREPs), followed by cigarette branded Swedish snus products in the US, and other smokeless tobacco products. The search string was iteratively refined to ensure it was able to capture a test set of 17 THR papers of different publication types.21,22
Study Selection
All records obtained through database searches were imported into Covidence,23 a web-based software platform. Duplicate citations were eliminated, and 4,816 abstracts were screened independently by two of the authors. Abstracts agreed on by both reviewers as meeting predetermined criteria were included for full text review.
English-language publications addressing the concept of tobacco harm reduction in humans (defined as substituting putatively safer tobacco products) were included in full-text review. Studies on modified cigarettes were excluded (e.g. Marlboro UltraSmooth, hookah/waterpipe, and South Asian smokeless tobacco variants like chuna, gutka, and betel quid), since these products were generally not considered to be reduced harm products in the literature.24–26 Studies discussing alternative product use in pregnant women were excluded as any form of nicotine consumption (including NRT) is generally considered harmful for this population.27 The following study types were also excluded: animal studies; theoretical studies that exclusively discussed concepts in THR debates (e.g. “inveterate smokers”) but did not mention a tobacco or nicotine product; studies addressing long-term use of US Food and Drug Administration-approved NRT; nicotine vaccines; books, theses, reports and other literature not published in peer-reviewed journals; and abstracts from conference proceedings publications without a corresponding published paper.
Studies were excluded only when both independent reviewers agreed on exclusion. Disagreements regarding inclusion/exclusion were discussed, with a third reviewer adjudicating if necessary.
Data Extraction
Data on author names, article titles, date of publication, first author’s country, and journal name were extracted for all articles included in full text review. All articles were double coded for the following: type of article; primary product type (e.g. snus, e-cigarettes); presence of themes for and against THR; the article’s overall stance on THR (five-point Likert scale: strongly pro, weakly pro, mixed/neutral, weakly anti, strongly anti); and concept of tobacco harm reduction present in the article (e.g. long-term product substitution). During this phase of coding, funding information (tobacco, e-cigarette, pharmaceutical industry, or multiple industries) and other affiliation with industry (such as having authors employed by a tobacco company), and each author’s country was determined by a content-blinded research assistant, who reviewed disclosed author affiliations and conflict of interest statements. Two investigators subsequently validated this assessment by independently extracting and verifying industry funding and affiliation coding for the entire data set.
Coding Guideline Development and Definitions
A detailed set of coding guidelines (Supplement 2) was developed to define the different arguments used to support and oppose THR (to aid in consistent assessments of stance on THR) and to classify different publication types.
The coding guidelines were developed iteratively by reading representative THR articles to generate a list of the most frequently used arguments to promote and criticize tobacco product substitution as harm reduction. A sample of 30 articles was coded using the list to determine reliability, consistency, and the need for new codes. The codebook was revised and re-tested with an additional 30 sample articles. Through this iterative analysis, 29 “pro-THR” (supporting) and “anti-THR” (criticizing) arguments were identified and defined. Test sets of articles were coded by all investigators to clarify the definitions and revise the codebook and criteria. Investigators assigned each article a score based on the number of pro-THR and anti-THR arguments, and the strength of position each article endorsed. The five-point score was simplified into three categories for analysis (i.e. pro, anti, neutral). The iterative process of coding test sets continued until the third set of 40 articles where argument saturation and over 70% coding consistency was achieved as measured by Krippendorff’s alpha. All articles in the dataset were double-coded by two investigators and differences in coding were resolved through review and consensus, with adjudication by a third investigator as needed.
Similarly, definitions for coding publication type were developed, using both pre-established definitions of empirical studies like cohort studies, cross-sectional studies, etc., and working definitions of non-empirical published papers to differentiate between commentaries, non-systematic literature reviews and editorials, and other non-empirical opinion pieces. The complete list of pro-THR and anti-THR arguments and publication types with examples for each definition can be found in the codebook (Supplement 2). The final codebook was validated by an external reviewer using the coding guidelines to independently code a stratified random sample of 10 articles from the dataset for comparison.
Data Synthesis and Analysis
A descriptive analysis of extracted data was conducted to determine the frequency with which products were discussed, the number of THR articles by the first author’s country, difference in THR stance by country, and year of publication (relevant to when e-cigarettes entered the market). Stance on THR was also described for each publication type.
To determine association between industry funding/affiliation and stance on THR, we examined only articles classified as pro-THR or anti-THR, excluding neutral articles. First, exact logistic regression models were used with stance on THR as the outcome (pro vs. anti-THR) and source of funding/industry affiliation, which was a categorical variable and indicated whether papers were funded by e-cigarette industry, pharmaceutical industry and tobacco industry, as the predictor. Second, we fit a model with article type as the outcome (non-empirical/ empirical). Due to limited numbers of some types of articles (e.g. randomized controlled trials, quasi-experimental studies), articles classified as letters, commentaries, non-empirical articles, and editorials were grouped as “non-empirical articles.” Other article types were grouped as “empirical articles.” Lastly, a stratified analysis by article type was conducted with separate models for empiric and non-empirical studies with stance on THR as the outcome and funding source as predictor. A sensitivity analysis was also conducted including the neutral articles, using pro-THR vs. neutral/anti-THR as the outcome. All analyses were carried out using STATA 14.
Results
In total, 4,816 unique abstracts and 1,041 full-text articles were reviewed to address three key questions. After full-text review, 215 articles were excluded because they did not fit review criteria, resulting in 826 articles for analysis (Figure 1).
Figure 1:
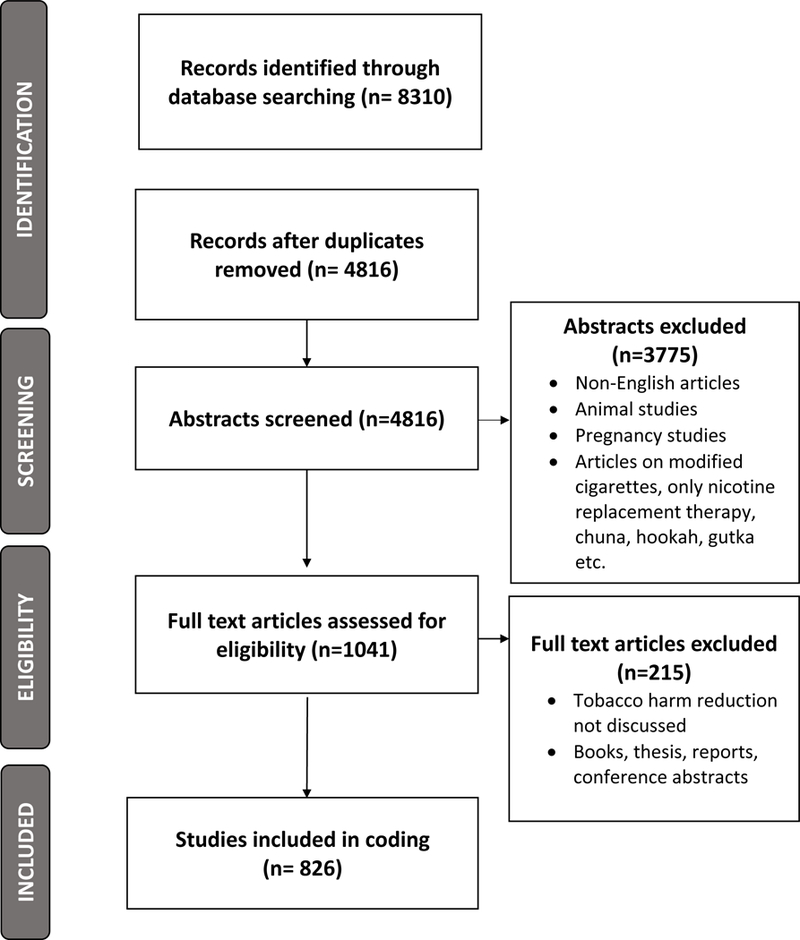
PRISMA Flow Chart
Key Question 1.What types of journal articles on THR were published in peer-reviewed journals?
Most THR articles were published after 2004, with 25% of the sample published between 2004–2010 and 66% published after 2010. Overall, 49.2% of total articles were pro-THR, 9.3% were mixed/neutral and 41.5% were anti-THR. E-cigarettes were the most popular product type discussed (appearing in 48.9% of articles), followed by smokeless tobacco (19.5%), Potential Reduced Exposure Products (PREPs) (11%), snus (17.2%), and other products (3.4%). Based on the affiliation of the first author, 48.6% of articles in the dataset were from the US, followed by the UK (18.3%), Australia (6%), Sweden (5%) and Canada (5%). Among US THR articles, 35% were pro-THR and 54.4% were anti-THR. France and “Other” countries also had a plurality of anti-THR articles. In the U.K., however, this distribution was reversed: 64.9% of articles were pro-THR versus 26.5% anti-THR. The majority of English-language articles from Sweden, Australia, Canada, Italy, New Zealand and Switzerland were also pro-THR (Table 1).
Table 1:
Stance on tobacco harm reduction (THR) of articles by the primary tobacco product type, year of publication, first authors’ country, publication type and funding source.
| Total N=826 |
% | Pro- THR N=406 |
% | Neutral/ Mixed N=77 |
% | Anti- THR N=343 |
% | |
|---|---|---|---|---|---|---|---|---|
| Primary product Type | ||||||||
| E-cigarettes | 404 | 48.91 | 199 | 49.3 | 38 | 9.4 | 167 | 41.3 |
| Smokeless tobacco | 161 | 19.49 | 75 | 46.6 | 12 | 7.5 | 74 | 45.3 |
| Snus | 142 | 17.19 | 59 | 41.1 | 17 | 12.0 | 66 | 46.5 |
| PREPs | 91 | 11.02 | 58 | 63.7 | 5 | 5.5 | 28 | 30.8 |
| Other | 28 | 3.39 | 15 | 53.6 | 5 | 17.9 | 8 | 28.6 |
| Year of Publication | ||||||||
| Before 2004 | 75 | 9.07 | 39 | 52.0 | 4 | 5.3 | 32 | 42.7 |
| Between 2004–2010 | 205 | 24.83 | 267 | 48.8 | 49 | 11.7 | 230 | 39.5 |
| After 2010 | 546 | 66.10 | 100 | 48.9 | 24 | 9.0 | 81 | 42.1 |
| First author’s country | ||||||||
| United States | 402 | 48.66 | 141 | 35.1 | 43 | 10.7 | 218 | 54.2 |
| United Kingdom | 151 | 18.28 | 98 | 64.9 | 13 | 8.6 | 40 | 26.5 |
| Australia | 51 | 6.17 | 35 | 68.6 | 3 | 5.9 | 13 | 25.5 |
| Sweden | 40 | 4.84 | 24 | 60.0 | 4 | 10.0 | 12 | 30.0 |
| Canada | 40 | 4.84 | 27 | 67.5 | 2 | 5.0 | 11 | 27.5 |
| Italy | 25 | 3.02 | 22 | 88.0 | 1 | 4.0 | 2 | 8.0 |
| France | 14 | 1.69 | 6 | 42.9 | 1 | 7.1 | 7 | 50.0 |
| New Zealand | 17 | 2.05 | 12 | 70.6 | 3 | 17.7 | 2 | 11.8 |
| Switzerland | 13 | 1.57 | 8 | 61.5 | 3 | 23.1 | 2 | 15.4 |
| Other | 73 | 8.83 | 33 | 45.2 | 4 | 5.5 | 36 | 49.3 |
| Publication type | ||||||||
| Non-Empirical studies | 173 | 20.94 | 102 | 59.0 | 17 | 9.8 | 54 | 31.2 |
| Letter/Commentary | 283 | 34.26 | 142 | 50.2 | 16 | 5.7 | 125 | 44.2 |
| Editorial | 44 | 5.32 | 18 | 40.9 | 8 | 18.2 | 18 | 40.9 |
| Qualitative | 31 | 3.75 | 8 | 25.8 | 6 | 19.4 | 17 | 54.8 |
| Literature review | 38 | 4.60 | 15 | 39.5 | 7 | 18.4 | 16 | 42.1 |
| Systematic review/ Meta-analysis | 24 | 2.90 | 10 | 41.7 | 4 | 16.7 | 10 | 41.7 |
| Case studies | 5 | 0.6 | 3 | 60.0 | 0 | 0.0 | 2 | 40.0 |
| Cross-sectional studies | 125 | 15.13 | 51 | 40.8 | 13 | 10.4 | 61 | 48.8 |
| Case-control studies | 8 | 0.97 | 4 | 50.0 | 0 | 0.0 | 4 | 50.0 |
| Cohort studies | 28 | 3.4 | 15 | 53.6 | 1 | 3.6 | 12 | 42.9 |
| Quasi-experimental studies | 49 | 5.93 | 25 | 51.0 | 3 | 6.1 | 21 | 42.9 |
| RCT | 18 | 2.17 | 13 | 72.2 | 2 | 11.1 | 3 | 16.7 |
| Funding* | * | * | ||||||
| E-cigarette industry | 57 | 29.68 | 53 | 92.98 | 2 | 3.51 | 2 | 3.51 |
| Pharmaceutical industry | 124 | 64.58 | 88 | 70.97 | 8 | 6.45 | 28 | 22.58 |
| Tobacco industry | 59 | 30.73 | 54 | 91.53 | 4 | 6.78 | 1 | 1.69 |
Four percent of papers were funded by multiple industries. Thus the total N will add up to more than 192. Total percentage (%) also add up to more than 100%. THR=Tobacco Harm Reduction. PREPs=Potential Reduced Exposure Products. RCT=Randomized Controlled Trial
Only 39.4% (326/826) of the included articles were empirical research articles, while 61% (500/826) were non-empirical letters or commentaries (34% of the entire sample), non-empirical articles (21%), and editorials (5%). The most common types of empirical studies identified were cross-sectional studies (15% of the entire sample), followed by quasi-experimental studies (6%). Randomized controlled trials (RCT’s) made up 2% of the sample.
RCT’s, non-empirical studies, and letters/commentaries were more frequently supportive of THR than not (Table 1). Editorials and systematic reviews were the most evenly divided categories, with roughly equal frequency of pro-THR and anti-THR ratings. Cross-sectional studies, literature reviews and qualitative studies were more frequently anti-THR.
Key Question 2.What proportion of THR articles are funded by the tobacco, pharmaceutical, and e-cigarette industries?
About 23.9% (n=197) of articles were funded by the tobacco, pharmaceutical and e-cigarette industries or some combination thereof. Overall, 14% of articles were funded by the pharmaceutical industry, 7% by the tobacco industry, and 7% by the e-cigarette industry.
Key Question 3.Does the THR-stance of industry-funded THR research differ from non-industry-funded research?
Articles reporting any industry funding were significantly more likely to take a pro-THR position. The odds of taking a pro-THR stance was significantly higher for articles funded/supported by the e-cigarette industry (OR: 20.9 95%CI: 5.3, 180.7), the tobacco industry (OR: 59.4 95%CI: 10.1, +infinity), and the pharmaceutical industry (OR: 2.18 95%CI: 1.3, 3.7). Ninety-five percent of the e-cigarette industry funded articles took a pro-THR stance, as did 88% of the tobacco industry articles and 72% of the pharmaceutical industry funded articles. In contrast, only 41.1% of articles without any industry funding or affiliation took a pro-THR stance (Figure 2).
Figure 2.
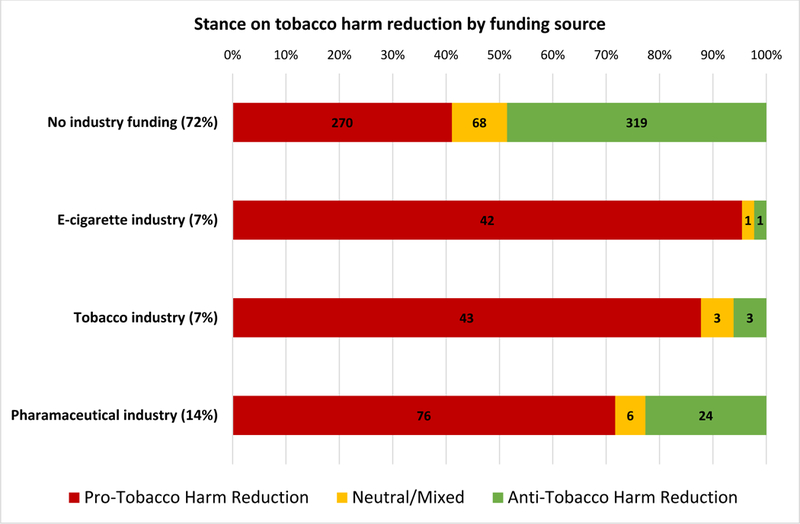
Stance on tobacco harm reduction by funding source (30 articles were funded by multiple sources).
Among empirical studies, tobacco industry funding perfectly predicted a pro-THR stance, so was not included in the model. E-cigarette industry funding was significantly associated with pro-THR stance (OR=16.4 95% CI 2.4, 701.8), as was pharmaceutical funding (OR=2.1 95% CI 1.03, 4.5) for empirical articles. Among non-empirical studies, tobacco industry funding was significantly associated with pro-THR stance (OR=19.1 95% CI 3.0, 799.5), as was e-cigarette industry funding (OR=20.1 95% CI 3.2, 860.2) and pharmaceutical industry funding (OR=2.4 95% CI 1.1, 5.3) (Table 2).
Table 2:
Exact logistic models fit using industry funding/affiliation source as predictors for pro-tobacco harm reduction stance and research article type.
| OR | 95% CI | p-value | Industry funded pro- articles (N) |
|
|---|---|---|---|---|
|
Is presence of industry funding or affiliation associated with pro-tobacco harm reduction stance? (N=749) a | ||||
|
E-cigarette industry Tobacco industry Pharmaceutical industry |
20.9 59.4 2.18 |
5.3,180.7 10.1,+Infinity 1.3,3.7 |
<0.0001 <0.0001 0.002 |
53 54 88 |
|
Is presence of industry funding or affiliation associated with type of research article (empirical) (N=826)? | ||||
|
E-cigarette industry Tobacco industry Pharmaceutical industry |
0.7 2.3 1.3 |
0.4,1.3 1.3,4.2 0.9,2.2 |
0.6 0.002 0.2 |
20 35 56 |
|
Among non-empirical research articles, is industry funding associated with pro- tobacco harm reduction stance? (N=459)b | ||||
|
E-cigarette industry Tobacco industry Pharmaceutical industry |
20.1 19.1 2.4 |
3.2, 860.2 3.0,799.5 1.1, 5.3 |
<0.0001 0.0001 <0.0001 |
34 22 51 |
|
Among empirical research articles, is industry funding associated with pro-tobacco harm reduction stance? (N=258) | ||||
|
E-cigarette industry Tobacco industryc Pharmaceutical industry |
16.4 - 2.1 |
2.46, 701.76 - 1.03, 4.45 |
0.0004 - 0.04 |
19 32 37 |
The articles with tobacco harm reduction stance coded as neutral or mixed (N=77) were excluded from this analysis.
Here, again 77 articles taking a neutral tobacco harm reduction stance were excluded.
In addition to excluding the 77 neutral- tobacco harm reduction articles, all 32 articles funded by/ affiliated with the tobacco industry were dropped from the analysis as they were all pro-tobacco harm reduction (perfect prediction)
Discussion
This systematic review of industry funding in the published literature on tobacco harm reduction found that 23.9% of included articles were funded by industries with a financial interest in promoting nicotine-containing products as tobacco harm reduction. Industry-funded articles were significantly more likely to support THR. Absent these papers, the published literature did not endorse THR, with 41.1% supporting, 10.4% neutral, and 48.6% against THR. In comparison, 80.9% of industry-funded articles endorsed THR. The impact of industry-funded publications may have skewed the overall debate in favor of product substitution.
These findings are consistent with the scientific literature showing tobacco industry-funded research favors conclusions supportive to the tobacco industry.28–32 This includes industry research supporting nicotine’s benefits for Alzheimer’s disease,33 neuroenhancement,34 and ulcerative colitis.35 Other studies also documented the influence of pharmaceutical industry funding on multiple types of bias in scientific studies.36 This study suggests that major debates in public health such as tobacco harm reduction may be shaped by industry-interested non-empirical articles, letters and commentaries in the scholarly literature.
The pharmaceutical industry was the most common industry funder of THR articles. This may be because pharmaceutical companies have the most active interest in this area; or because there is less stigma associated with disclosure of pharmaceutical funding compared to disclosure of tobacco or electronic cigarette funding sources. The tobacco industry’s history of funding scientific research to undermine the evidence of harms from tobacco is well documented.37–40 The higher frequency of disclosed pharmaceutical funding may be the result of undisclosed tobacco and e-cigarette industry funding. Future studies should address undisclosed funding sources, which may be uncovered from internal industry documents,41,42 or by tracing disclosed funding from authors’ past publications.43,44
In addition, most published articles were non-empirical research, editorials, letter and comments. Funding disclosure policies for these types of publications may be more lax than for empirical studies, so the presence of industry funding reported in this study was likely underestimated. Non-empirical studies and reviews can substantially impact scientific debate, particularly when little empiric evidence exists, as has been the case with e-cigarettes. For example, one paper, which summarized the result of expert opinion in a Delphi process,45 concluded that e-cigarettes were 95% safer than cigarettes, and it was widely cited8,46 as a definitive scientific consensus, despite its tobacco and e-cigarette funding source47 and lack of any specific empirical evidence supporting the estimate of relative safety.48 Medical practitioners and researchers need to be aware of the presence and influence of industry funding in THR when reviewing this evidence base.
Disclosure of industry funding is necessary but not sufficient to minimize the bias introduced by commercial interests in science.43 Some scientific journals and conferences have adopted policies rejecting articles or abstracts submitted by industry funded scientists,44,49,50 on the grounds that the industry’s financial interests bias their research. This systematic review suggests the wisdom of such a strategy to avoid further industry-induced bias that may perpetuate an industry-induced health epidemic that continues to be the leading preventable cause of death worldwide.
Limitations
This study was limited to disclosed funding sources – undisclosed funding may have had a significant effect on THR position. The study relied on a novel coding instrument to measure position on THR, which was nevertheless subjective. To address this inherent limitation, detailed criteria to enumerate the most common THR arguments were established, investigators double-coded all articles to minimize individual variance in assessment of stance on THR, and an outside coder validated a subset of articles. In addition, while an independent research assistant blinded to the article content extracted all funding disclosures, knowledge of authors’ conflicts of interest might have biased the coders’ assessment of stance. The inclusion of many non-empirical articles and the heterogeneity in the dataset precluded the use of meta-analysis or formal analysis of bias other than funding bias. However, the data reflect most of the published literature on THR as of 2016, highlighting how non-empirical papers may influence perceptions of scholarly consensus.
Despite these limitations, this study demonstrates the importance of industry conflict of interest in the tobacco harm reduction debate. It also points out several deficiencies in the current body of literature on this topic, chief among which is the lack of empirical studies compared to opinion pieces, letters and editorials. Future studies may build on this work by analyzing new research with clinical outcomes conducted since 2016; evaluating the risk of bias within different article types; and assessing the role of undisclosed industry funding on investigators’ conclusions.
Conclusion
Industry funding strongly influenced the acceptance of tobacco harm reduction as product substitution. The tobacco harm reduction scientific literature was dominated by non-empirical articles, which were much more likely to support THR if they received industry funding. Industry funding of scientific research has likely influenced perceptions of consensus on tobacco harm reduction as endorsing product substitution as a viable health intervention, when in fact the non-industry-funded scientific literature remained divided on this issue.
Supplementary Material
References
- 1.Committee to Assess the Science Base for Tobacco Harm Reduction, Board on Health Promotion and Disease Prevention, Institute of Medicine Clearing the Smoke: Assessing the Science Base for Tobacco Harm Reduction. (Stratton K, Shetty P, Wallace R, Bondurant S, eds.). Washington, D.C.: National Academies Press; 2001. [PubMed] [Google Scholar]
- 2.Terry M, Cummings KM, Erickson A, Shopland D. Ending Cigarette Use By Adults In A Generation Is Possible: The Views Of 120 Leaders In Tobacco Control. Core Team on Tobacco Control; 2017. http://www.tobaccoreform.org/wp-content/uploads/2017/03/Executive-Summary-Report-Ending-Cigarette-Use-by-Adults.pdf. Accessed May 10, 2017. [Google Scholar]
- 3.Meier BM, Shelley D. The fourth pillar of the Framework Convention on Tobacco Control: harm reduction and the international human right to health. Public Health Rep. 2006;121(5):494–500. doi: 10.1177/003335490612100503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patnode CD, Henderson JT, Thompson JH, Senger CA, Fortmann SP, Whitlock EP. Behavioral Counseling and Pharmacotherapy Interventions for Tobacco Cessation in Adults, Including Pregnant Women: A Review of Reviews for the U.S. Preventive Services Task Force. Rockville (MD): Agency for Healthcare Research and Quality; (US: ); 2015. http://www.ncbi.nlm.nih.gov/books/NBK321744/. Accessed November 18, 2018. [PubMed] [Google Scholar]
- 5.Committee on the Review of the Health Effects of Electronic Nicotine Delivery Systems, Board on Population Health and Public Health Practice, Health and Medicine Division, National Academies of Sciences, Engineering, and Medicine Public Health Consequences of E-Cigarettes. (Stratton K, Kwan LY, Eaton DL, eds.). Washington, D.C.: National Academies Press; 2018. doi: 10.17226/24952. [DOI] [PubMed] [Google Scholar]
- 6.Crowley RA. Electronic Nicotine Delivery Systems: Executive Summary of a Policy Position Paper From the American College of Physicians. Annals of Internal Medicine. 2015;162(8):583. doi: 10.7326/M14-2481. [DOI] [PubMed] [Google Scholar]
- 7.Britton J, Arnott D, McNeill A, Hopkinson N, Physicians TAG of the RC of. Nicotine without smoke—putting electronic cigarettes in context. BMJ. 2016;353:i1745. doi: 10.1136/bmj.i1745. [DOI] [PubMed] [Google Scholar]
- 8.Public Health England, McNeill A, Brose LS, et al. E-Cigarettes: An Evidence Update. London: Public Health England; 2015. [Google Scholar]
- 9.Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2016;9:CD010216. doi: 10.1002/14651858.CD010216.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respir Med. 2016;4(2):116–128. doi: 10.1016/S2213-2600(15)00521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berry KM, Reynolds LM, Collins JM, et al. E-cigarette initiation and associated changes in smoking cessation and reduction: the Population Assessment of Tobacco and Health Study, 2013–2015. Tobacco Control. March 2018:tobaccocontrol-2017–054108. doi: 10.1136/tobaccocontrol-2017-054108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yach D Foundation for a smoke-free world. The Lancet. 2017;390(10104):1807–1810. doi: 10.1016/S0140-6736(17)32602-8. [DOI] [PubMed] [Google Scholar]
- 13.Peeters S, Gilmore AB. Understanding the emergence of the tobacco industry’s use of the term tobacco harm reduction in order to inform public health policy. Tob Control. 2015;24(2):182–189. doi: 10.1136/tobaccocontrol-2013-051502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tan CE, Kyriss T, Glantz SA. Tobacco company efforts to influence the Food and Drug Administration-commissioned Institute of Medicine report clearing the smoke: an analysis of documents released through litigation. PLoS Med. 2013;10(5):e1001450. doi: 10.1371/journal.pmed.1001450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.British American Tobacco. Sustainability Report 2016. 2017. www.bat.com/sustainability. Accessed March 21, 2017.
- 16.Wang AT, McCoy CP, Murad MH, Montori VM. Association between industry affiliation and position on cardiovascular risk with rosiglitazone: cross sectional systematic review. BMJ. 2010;340(mar18 1):c1344-c1344. doi: 10.1136/bmj.c1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pisinger C, Døssing M. A systematic review of health effects of electronic cigarettes. Preventive Medicine. 2014;69:248–260. doi: 10.1016/j.ypmed.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 18.Critchley JA, Unal B. Is smokeless tobacco a risk factor for coronary heart disease? A systematic review of epidemiological studies. Eur J Cardiovasc Prev Rehabil. 2004;11(2):101–112. [DOI] [PubMed] [Google Scholar]
- 19.Tam J, Day HR, Rostron BL, Apelberg BJ. A systematic review of transitions between cigarette and smokeless tobacco product use in the United States. BMC Public Health. 2015;15:258. doi: 10.1186/s12889-015-1594-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Evans WD, Horn KA, Gray T. Systematic Review to Inform Dual Tobacco Use Prevention. Pediatr Clin North Am. 2015;62(5):1159–1172. doi: 10.1016/j.pcl.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 21.Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0; 2011. Available from http://handbook.cochrane.org.
- 22.Deyner D, Tranfield D. Producing a systematic review. In: Buchanan D, Bryman A, eds. The SAGE Handbook of Organizational Research Methods. London: SAGE Publications Ltd; 2009:671–689. [Google Scholar]
- 23.Veritas Health Innovation. Covidence systematic review software. 2018. Available at www.covidence.org.
- 24.Gupta PC, Ray CS. Epidemiology of betel quid usage. Ann Acad Med Singap. 2004;33(4 Suppl):31–36. [PubMed] [Google Scholar]
- 25.Rees VW, Wayne GF, Connolly GN. Puffing style and human exposure minimally altered by switching to a carbon-filtered cigarette. Cancer Epidemiol Biomarkers Prev. 2008;17(11):2995–3003. doi: 10.1158/1055-9965.EPI-07-2533. [DOI] [PubMed] [Google Scholar]
- 26.Maziak W The global epidemic of waterpipe smoking. Addict Behav. 2011;36(1–2):1–5. doi: 10.1016/j.addbeh.2010.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wickström R Effects of Nicotine During Pregnancy: Human and Experimental Evidence. Current Neuropharmacology. 2007;5(3):213–222. doi: 10.2174/157015907781695955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Landman A, Glantz SA. Tobacco Industry Efforts to Undermine Policy-Relevant Research. Am J Public Health. 2009;99(1):45–58. doi: 10.2105/AJPH.2007.130740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith EA, Malone RE. Philip Morris’s Health Information Web Site Appears Responsible but Undermines Public Health: Philip Morris’s Health Information Web site. Public Health Nursing. 2008;25(6):554–564. doi: 10.1111/j.1525-1446.2008.00743.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McDaniel PA, Malone RE. British American Tobacco’s partnership with Earthwatch Europe and its implications for public health. Glob Public Health. 2012;7(1):14–28. doi: 10.1080/17441692.2010.549832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith J, Thompson S, Lee K. The atlas network: a “strategic ally” of the tobacco industry. Int J Health Plann Manage. 2017;32(4):433–448. doi: 10.1002/hpm.2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martínez C, Fu M, Galán I, et al. Conflicts of interest in research on electronic cigarettes. Tobacco Induced Diseases. 2018;16(June). doi: 10.18332/tid/90668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cataldo JK, Prochaska JJ, Glantz SA. Cigarette smoking is a risk factor for Alzheimer’s disease: An analysis controlling for tobacco industry affiliation. J Alzheimers Dis. 2010;19(2):465–480. doi: 10.3233/JAD-2010-1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Turner C, Spilich GJ. Research into smoking or nicotine and human cognitive performance: does the source of funding make a difference? Addiction. 1997;92(11):1423–1426. [PubMed] [Google Scholar]
- 35.Reynolds RJ. Targacept: Key Messages.; 1999. https://www.industrydocumentslibrary.ucsf.edu/tobacco/docs/szbm0008. Accessed April 13, 2018.
- 36.Sismondo S How pharmaceutical industry funding affects trial outcomes: Causal structures and responses. Social Science & Medicine. 2008;66(9):1909–1914. doi: 10.1016/j.socscimed.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 37.Hirshbein L Scientific Research and Corporate Influence: Smoking, Mental Illness, and the Tobacco Industry. J Hist Med Allied Sci. 2012;67(3):374–397. doi: 10.1093/jhmas/jrr019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Muggli ME, Hurt RD, Blanke DD. Science for hire: a tobacco industry strategy to influence public opinion on secondhand smoke. Nicotine Tob Res. 2003;5(3):303–314. [DOI] [PubMed] [Google Scholar]
- 39.Barnes DE, Bero LA. Why review articles on the health effects of passive smoking reach different conclusions. JAMA. 1998;279(19):1566–1570. [DOI] [PubMed] [Google Scholar]
- 40.Mandrioli D, Kearns CE, Bero LA. Relationship between Research Outcomes and Risk of Bias, Study Sponsorship, and Author Financial Conflicts of Interest in Reviews of the Effects of Artificially Sweetened Beverages on Weight Outcomes: A Systematic Review of Reviews. PLOS ONE. 2016;11(9):e0162198. doi: 10.1371/journal.pone.0162198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Glantz SA, Slade J, Bero LA, Hanauer P, Barnes DE, eds. The Cigarette Papers. Berkeley, Calif.: University of California Press; 1998. [Google Scholar]
- 42.Bero L Implications of the tobacco industry documents for public health and policy. Annu Rev Public Health. 2003;24:267–288. doi: 10.1146/annurev.publhealth.24.100901.140813. [DOI] [PubMed] [Google Scholar]
- 43.Bero LA, Glantz S, Hong M-K. The limits of competing interest disclosures. Tob Control. 2005;14(2):118–126. [PMC free article] [PubMed] [Google Scholar]
- 44.Grundy Q, Dunn AG, Bourgeois FT, Coiera E, Bero L. Prevalence of Disclosed Conflicts of Interest in Biomedical Research and Associations With Journal Impact Factors and Altmetric Scores. JAMA. 2018;319(4):408–409. doi: 10.1001/jama.2017.20738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nutt DJ, Phillips LD, Balfour D, et al. Estimating the harms of nicotine-containing products using the MCDA approach. Eur Addict Res. 2014;20(5):218–225. doi: 10.1159/000360220. [DOI] [PubMed] [Google Scholar]
- 46.Royal College of Physicians, Tobacco Advisory Group. Nicotine without Smoke: Tobacco Harm Reduction : A Report. London: Royal College of Physicians; 2016. [Google Scholar]
- 47.Gornall J Public Health England’s troubled trail. BMJ. 2015;351:h5826. [DOI] [PubMed] [Google Scholar]
- 48.Lancet The. E-cigarettes: Public Health England’s evidence-based confusion. The Lancet. 2015;386(9996):829. doi: 10.1016/S0140-6736(15)00042-2. [DOI] [PubMed] [Google Scholar]
- 49.Godlee F, Malone R, Timmis A, et al. Journal policy on research funded by the tobacco industry. Thorax. 2013;68(12):1090–1091. doi: 10.1136/thoraxjnl-2013-204531. [DOI] [PubMed] [Google Scholar]
- 50.The PLoS Medicine Editors. A New Policy on Tobacco Papers. PLoS Medicine. 2010;7(2):e1000237. doi: 10.1371/journal.pmed.1000237. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


