Abstract
Aims:
To summarise evidence on the frequency and predictors of healthcare utilisation among people who use illicit drugs.
Design:
Systematic search of MEDLINE, EMBASE and PsychINFO for observational studies reporting healthcare utilisation published between 1 January 2000 and 3 December 2018. We conducted narrative synthesis and meta-analysis following a registered protocol (identifier: CRD42017076525).
Setting and participants:
People who use heroin, powder cocaine, crack cocaine, methamphetamine, amphetamine, ecstasy/MDMA, cannabis, hallucinogens, or novel psychoactive substances; have a diagnosis of ‘substance use disorder’; or use drug treatment services.
Measurements:
Primary outcomes were the cumulative incidence (risk) and rate of care episodes in three settings: primary care, hospital admissions (inpatient) and emergency department (ED).
Findings:
92 studies were included, 84% from North America and Australia. Most studies focused on people using heroin, methamphetamine or crack cocaine, or who had a diagnosis of drug dependence. We were able to conduct meta-analysis of rates across 25 studies reporting ED episodes and 25 reporting hospital admissions, finding pooled rates of 151 (95% CI 114–201) and 41 (95% CI 30–57) per 100 person-years respectively; on average 4.8 and 7.1 times more often than the general population. Heterogeneity was very high and was not explained by drugs used, country of study, recruitment setting or demographic characteristics. Predictors of healthcare utilisation were consistent across studies and included unstable housing, drug injection and mental health problems. Opioid substitution therapy was consistently associated with reduced ED presentation and hospital admission. There was minimal research on healthcare utilisation by people using ecstasy/MDMA, powder cocaine, hallucinogens or novel psychoactive substances.
Conclusions:
People who use illicit drugs are admitted to emergency department or hospital several times more often than the general population.
Introduction
Use of illicit drugs is associated with health, social and economic problems. People who are dependent on illicit drugs generally have poor health outcomes, with cohort studies finding mortality rates of up to 15 times the general population, though this varies widely by population and setting [1,2]. As well as overdose, there is excess risk of cancers, cardiovascular, respiratory and liver diseases [3,4]. Excess disease may be due to both the direct effects of illicit drugs and accompanying life circumstances. For instance, people who use illicit drugs are vulnerable to homelessness, imprisonment, and other forms of social exclusion [5], and have high rates of tobacco smoking and harmful alcohol consumption. There are diverse subgroups of people who use drugs, and people who smoke cannabis or use illicit drugs occasionally may have better health outcomes than people who use drugs such as heroin, crack cocaine and methamphetamine [6,7].
Despite the high need for healthcare, qualitative research has identified multiple barriers for people who use illicit drugs. Health professionals may have negative perceptions of patients who use illicit drugs, including poor motivation, seeking prescriptions for non-medical purposes, and violent behaviour; and may feel they lack training and skills to address the needs of this group [8]. Patients report that staff have stigmatising attitudes and that there are barriers to attending appointments, such as transport costs and inflexible timeslots [9]. People who use drugs may delay treatment due to normalisation of pain, fear of stigma in services, and concern about inadequate opioid substitution and pain control when admitted to hospital [10]. These barriers mean that symptoms may not be addressed, leading to presentation late in the course of a disease and use of emergency care. People who use illicit drugs face distinct challenges to healthcare access related to criminalisation and social exclusion. We have therefore chosen to focus on this group rather than include people who use alcohol, tobacco, or other legal drugs.
Studies of patients visiting emergency departments (ED) have found that 10%−20% report recent use of illicit drugs [11–13]; much higher than the general population, and diagnoses of drug dependence are common among frequent ED users [14,15]. Frequent ED users are particularly likely to use drugs [16]. Such observations have led to a perception that people who use drugs are reliant on ED services, but there is limited population-based research into the frequency and patterns of healthcare utilisation in this group. We aimed to (1) describe the frequencies of healthcare utilisation reported in observational studies of people who use illicit drugs and calculate pooled averages; (2) compare the frequency of healthcare utilisation to the general population; and (3) summarise evidence on the predictors and causes of healthcare utilisation.
Methods
Review protocol
We conducted a systematic review following the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines [17]. A protocol for this review has been registered with PROSPERO (identifier: CRD42017076525).
Search strategy
We searched Medline, PsychINFO and EMBASE from 1 January 2000 to 27 September 2017 using keywords and MeSH terms related to substance use, healthcare utilisation and observational study designs (full terms included in the Supplementary Information). We also included studies from a manual search of references. On 3 December 2018 we updated our search using the same databases, search terms and inclusion criteria.
Study inclusion and exclusion criteria
We included English-language cohort and cross-sectional studies where 75% or more of participants recently used illicit drugs. Illicit drugs were defined as heroin, powder cocaine, crack cocaine, methamphetamine, amphetamine, ecstasy/MDMA, cannabis, hallucinogens, or novel psychoactive substances. We also included individuals who had a diagnosis of ‘substance use disorder’ or were recruited from drug treatment services, where we were able to determine that at least 75% used illicit drugs rather than alcohol only. Primary outcomes were the rate or cumulative incidence of ED episodes, hospital admissions and primary care presentation. We excluded studies of participants recruited from acute healthcare services (such as ED), who had acute disease (such as hepatitis A) who were pregnant, or were aged under 18. We also excluded studies with fewer than 30 participants or less than 30 days of observation per participant.
Study quality assessment
Methodological quality was assessed using a modified Newcastle-Ottowa scale [18] that included recruitment bias, non-response, ascertainment of illicit drug use, ascertainment of healthcare utilisation, adequacy of follow-up (for cohort studies), selection of comparison groups (for relative measures), and adjustment (for relative measures). Full details are given in Supplementary Information.
Screening and data extraction
Two authors (DL and JF) independently screened titles and abstracts using Rayyan [19]. There was agreement of 94% (Cohen’s Kappa 0.58) and conflicts were resolved through discussion. We accessed full texts and one author (DL, JF or EK) used a piloted data extraction tool to record details including the study design, year, location of the study, recruitment setting (drug treatment services, community or healthcare), participant demographics, predominant drugs used, and denominator and numerator for primary outcomes. Where relative frequencies (such as rate ratios) were reported, we also recorded the ratio and details of the comparison group. Where predictors of healthcare use and cause-specific healthcare use were reported, we marked the study for narrative synthesis. A second author checked that all data was accurate. Queries that could not be resolved were referred to KIM for a final decision.
Analysis
In a narrative review, we described: (i) the range of values of the primary outcomes; (ii) predictors of healthcare utilisation; and (iii) causes of healthcare utilisation by disease.
In quantitative analysis, we displayed frequency rates of ED and inpatient utilisation using forest plots. To provide informal comparisons with the general population, we used published frequencies of healthcare utilisation in the US, Canada, Australia and the UK [20–22], for the general population group with the most similar age- and sex-profile as the study population. Details of the comparison group used for each study are given in the archived dataset.
We conducted random effects meta-analysis to report the average frequency of healthcare utilisation across study populations, limited to results from high-income countries and excluded studies of subgroups likely to have unusual healthcare utilisation (such as people living with HIV and prisoners). We anticipated that the strongest determinants of heterogeneity would be the predominant drug and the country where the study was conducted and therefore stratified results by these variables. As an exploratory analysis of further sources of heterogeneity (not pre-specified), we included each of the following variables in the meta-analysis equation as a moderator [23]: recruitment setting (healthcare, drug treatment services, community or prison), country, study design, study era (1990–1999, 2000–2009, 2010–2018), risk-of-bias score (low or high), age (average age under or over 30) and sex (greater or less than 60% male), using a threshold of p<0.05 to identify significant moderators.
All analysis was conducted using R version 3.5.1.
Results
Search results
Our search identified 5,528 studies after deduplication, of which 313 were selected for full-text review and 92 were included. Figure 1 shows a flow-chart of studies. Some studies included groups from distinct regions or with distinct drug use patterns, while others duplicated samples from other studies, and we identified 98 unique populations with 204 relevant data points. The full dataset is available in Supplementary Information.
Figure 1:
Flow chart of included studies
Description of study populations
Of the 98 study populations: 53 were in the United States; 16 in Australia; 13 in Canada; 3 in Ireland; 2 each in Taiwan, Italy, New Zealand, UK, Vietnam; and 1 each in Denmark, Finland and Norway.
Although the search strategy included people using any illicit drugs, studies focused on people who used illicit drugs associated with dependence. The largest group was people using opiate substitution (31 populations), mostly recruited from drug treatment services. The next largest was people who inject drugs (29 populations), mostly recruited from community settings. Eight studies focused on cannabis users, seven focused on stimulant users (where injecting was not specified) and five focused on opiate users (where injecting was not specified). Figure 2 shows the number of study populations by predominant drug used and recruitment setting. No studies recruited participants who predominantly used MDMA/ecstasy, powder cocaine, novel psychoactive substances or hallucinogens such as LSD and psilocybin.
Figure 2:
Unique study populations by predominant drug and recruitment source
A mean of 68% (sd. 12%) of participants were male and the mean of average ages (reported in some studies as means and in others as medians) was 36.7 (sd. 6.0).
Study quality
58/204 data points had high risk of bias. The main risk was lack of information on non-response. The overall risk of bias was not associated with frequency of healthcare utilisation in meta-analysis (see below). Table 1 summarises results from the quality assessment.
Table 1:
results of quality assessment
| Data points | High risk | Proportion high risk | |
|---|---|---|---|
| Recruitment bias | 204 | 28 | 14% |
| Non-response | 204 | 121 | 59% |
| Ascertainment of illict drug use | 204 | 43 | 21% |
| Ascertainment of healthcare utilisation | 204 | 44 | 22% |
| Adequacy of follow-up | 82 | 21 | 26% |
| Selection of comparison group | 47 | 4 | 9% |
| Adjustment for confounders | 47 | 4 | 9% |
| Global assessment | 204 | 58 | 28% |
Narrative review
Range of values
Frequencies of all outcomes were high and heterogeneous. ED utilisation ranged from 19 [24] to 1,061 [25] per 100 person-years. The proportion of participants visiting ED in the past 12 months ranged from 10% [26] to 72% [27]. Studies including relative measures showed frequency of ED utilisation of 3–10 times that of comparison groups not using illicit drugs [28–31]. Exceptions were a study in rural Taiwan showing that people who inject heroin had a similar rate of ED presentation as the general population [32], and a study of older people who use cannabis in the United States showing similar odds of ED presentation as those who do not use cannabis [33].
The rate of inpatient episodes ranged from 8 [3] to 852 [28] per 100 person-years. The proportion of participants who were hospitalised in the past 12 months ranged from 8% [34] to 41% [35]. Studies including relative measures showed frequency of hospital admission of 2–8 times that of comparison groups not using illicit drugs [28–30,36–39]. Again, studies of people who inject drugs in rural Taiwan and older people who use cannabis in the United States were exceptions, showing similar frequencies of hospital admission to the general population [32,40].
There were fewer studies primary care utilisation. Ten studies reported rates, ranging from 231 [41] to 2,087 [36] episodes per 100 person-years. The proportion of participants visiting primary care in the past 12 months ranged from 38% [42] to 90% [43]. Three studies found higher frequency than the general population: a study of insurance data in Canada found people with diagnoses of ‘substance abuse’ had 4.2 times more primary care visits than those without this diagnosis [36]; a study of patients at a specialist primary care clinic in Ireland that found that those with methadone prescriptions had 4.2 times the odds of a primary care consultation during 6 months, excluding visits for drug-related problems [44]; and a study of people in drug treatment in Australia that found those primarily in treatment for opioids had a median of 12 primary care visits in the past year, compared to 7 for those in treatment for alcohol [43]. Other studies found low absolute frequency of presentation without providing formal comparisons with the general population. For example, only 58% of people who inject drugs in Baltimore saw a primary care doctor over three years [45]; 53% of people who use methamphetamine in Australia saw a primary care doctor over 12 months [46]; and 32% of people who inject drugs in Montreal saw a primary care provider over six months, which was informally compared to 90% in the general population [47].
Studies investigating the frequency of healthcare utilisation in more than one setting showed that primary care episodes are more frequent than ED or inpatient episodes [48–52].
Predictors of healthcare utilisation
ED presentation was consistently associated with regular or recent injecting [53–56], sex work [53,57], diagnosed Hepatitis C [39], diagnosed HIV [30,35,55,58,59], female sex [35,48,60–63], homelessness or unstable housing [25,54,55,60,64], crack cocaine or stimulant use [55,60,61], alcohol use [62,65,66], polydrug use [46,67], and mental health problems [35,36,62].
Hospital admission was associated with similar factors: regular or recent injecting [54–56,68,69], diagnosed Hepatitis C [70,71], diagnosed HIV [34,55,68,69,72], low CD4 count among HIV positive participants [73], female sex [37,38,48,68,69,71,73], homelessness or unstable housing [54,68] alcohol use [71], polydrug use [46], and mental health problems [30,36].
One study (the Melbourne Injecting Drug User Cohort Study) reported similar associations with primary care utilisation: regular injecting, homelessness, cocaine injection and unstable income [47,74].
Opiate substitution treatment was consistently associated with lower frequency of ED presentation and hospital admission [26,35,41,52,56,70,72,75–80] than comparison groups of untreated opiate users. Among substitution patients, consistent medication was associated with a lower rate of ED utilisation [76,77,81]. Some studies looked at different types of treatment. For example, one study found that take-home methadone was associated with lower risk of hospital admission [82]. No studies looked at the effect of treatment for dependence on drugs other than opiates.
Some studies reported non-significant associations with these factors, but none found effects in the opposite direction.
Although some studies show that mental or physical morbidity predicts healthcare utilisation, no studies attempted to show whether increased frequency of healthcare utilisation among people who use illicit drugs was explained by morbidity or other indicators of need for services.
Causes of healthcare utilisation
Studies with cause-specific data showed that a minority of ED and inpatient episodes relate to the direct effects of illicit drugs, such as withdrawal, overdose and intoxication (Figure 3). Infections and particularly skin and soft tissue infections were common causes of ED and inpatient episodes in study populations in Canada [25,30,53,55,58,68], Norway [41] and Taiwan [32]. All infections and particularly pneumonias were important causes of healthcare utilisation in HIV positive opiate users [69,73]. Infections were less important causes of healthcare utilisation in Australia [83,84]. Traumas, injuries and mental health problems were important causes of ED utilisation and hospital admission in all countries [32,53,55,71,83,84].
Figure 3:
Main reason for healthcare utilisation
Quantitative analysis
We conducted meta-analysis of healthcare utilisation rates (25 studies reporting ED episodes and 25 reporting hospital admission) and 12-month cumulative incidence (11 studies reporting ED episodes and 11 reporting hospital admission). 12 months was the most common period examined in the literature. While we collected data from studies of other periods, we did not analyse this data because the periods varied too widely. We were unable to determine the consistency of the definition of primary care visits across studies and therefore did not attempt quantitative analysis. We restricted the analysis to populations who primarily use heroin, crack cocaine or methamphetamine or have a diagnosis of ‘substance abuse disorder’ or drug dependence, since there were few studies of people who use cannabis or have other patterns of use.
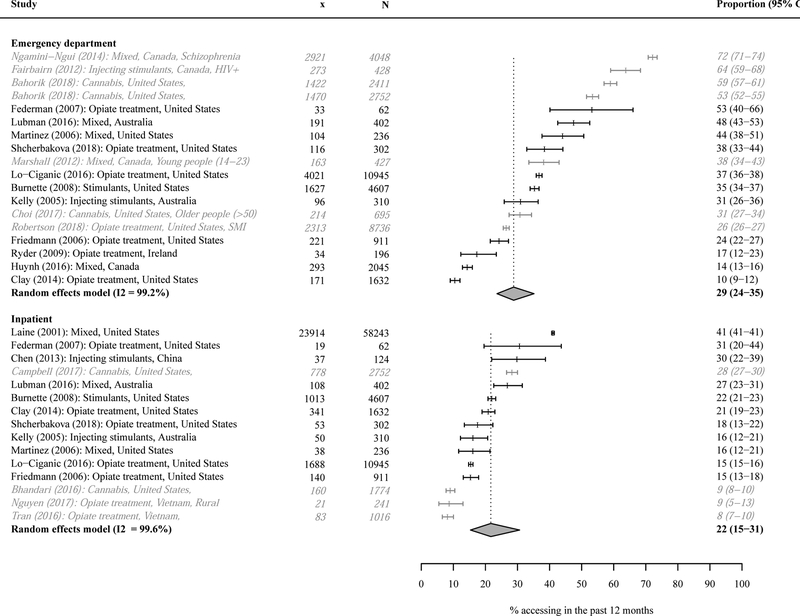
ED frequencies are shown in figures 4 and 5. An average of 29% (95% CI 24%−35%) of participants visited ED over a 12-month period. The pooled rate was 151 visits per 100 person-years (95% CI 114–201). There was high heterogeneity, with I2 approaching 100% for both analyses. 32 study populations were matched with published rates for groups of a similar age and sex in the general population. ED presentation ranged from 0.9 to 24.7 times the general population (mean 4.8). Stratified meta-analysis by predominant drug and country did not show significant differences to the overall pooled estimate (see Supplementary Information), and the exploratory meta-regression found no significant moderators.
Figure 4:
Forest plot of rates of healthcare utilisation. Studies in grey and italics are not included in the pooled estimate
Figure 5:
Forest plot of 12-month cumulative incidence of healthcare utilisation. Studies in grey and italics are not included in the pooled estimate
Hospital admission rates and cumulative incidences are shown in figures 4 and 5. An average of 22% (95% CI 15%−31%) of participants were hospitalised over a 12-month period. The pooled rate was 41 episodes per 100 person-years (95% CI 30–57). There was high heterogeneity, with I2 approaching 100% for both analyses. 27 study populations were matched with published rates for comparable groups in the general population. Hospital admission rates ranged from 1.9 to 35.5 times the general population (mean 7.1). As with the ED results, stratified meta-analysis by predominant drug and country did not show significant differences to the overall pooled estimate, and the exploratory meta-regression found no significant moderators.
Discussion
To our knowledge this is the first systematic review of healthcare utilisation in people who use illicit drugs. The majority of available evidence relates to people who use heroin, methamphetamine and crack cocaine, or have a diagnosis of drug dependence. The results show high but widely varying frequencies of ED presentation and hospital admission in this group.
The pooled frequencies of ED and hospital admissions are substantially higher than the general population. In part, this reflects morbidity and greater need for treatment. However, higher utilisation does not necessarily represent good healthcare access. A systematic review in 2009 [85] identified ten studies showing that people with substance use disorders are less likely to receive definitive treatment for specific conditions, despite higher all-cause attendance. For example, a study of veterans with diagnoses of diabetes in the US found that participants with comorbid substance use were less likely to receive foot or retina examinations [86]. Our finding of high utilisation of acute services may not represent good access, but a pattern where primary and preventative healthcare is poor and unplanned healthcare is common.
The results contrast with studies of healthcare among people who use alcohol, which find that drinkers (including heavy drinkers) have lower rates of healthcare utilisation than abstainers [87]. This is likely to be explained by abstention among people who are unwell, rather than a protective effect of alcohol. In contrast, this review found that people who use illicit drugs present to health services much more frequently than the general population. This may be because studies of people who use illicit drugs tend to focus on people who are dependent or use drugs associated with health harms, while studies of alcohol may include more moderate drinkers.
Predictors of healthcare utilisation were consistent across studies, including unstable housing, drug injection, and mental health problems. These factors reflect previously identified risk factors for poor health in people who use drugs [88], and are likely to be associated with greater need for healthcare.
Effectively all of the variation across studies was due to differences between populations rather than within-study error. Despite consistent predictors of healthcare utilisation within studies, we were not able to explain the variation between studies by the predominant drugs used by study participants, the country of the study or any other study-level variables that we collected. Results varied widely even within countries and populations with apparently similar drug use. For example, in the United States, the rate of hospital admission of people in opiate substitution therapy ranged from 51 to 592 per 100 person-years [52,75–77,89–91]. Other research has conceptualised access to health services as a product of individual factors, social contexts and healthcare systems [92,93]. The extent of the heterogeneity in our results is unlikely to be fully explained by individual-level factors that we did not capture. This suggests that social and healthcare contexts can substantially affect healthcare utilisation. The heterogeneity also highlights the difficulty of generalising results from single studies of healthcare utilisation.
The review identified three main gaps in the evidence. First, 84% of study populations were from the United States, Canada or Australia. We did not identify any studies from low income countries. Second, there were few studies with primary care data, even though existing studies suggest people who use illicit drugs visit primary care more often than acute healthcare settings [48–52], contrary to the stereotype of reliance on ED. Third, almost all studies were of people who use heroin, crack cocaine or methamphetamine, or have a diagnosis of drug dependence. There were only eight studies of people who use cannabis and none of people using MDMA/ecstasy, powder cocaine, hallucinogens, novel psychoactive substances or other drugs.
The results highlight the need for interventions that improve general health outcomes among people who use drugs. Despite a body of research into the effectiveness of opiate substitutes to reduce use of street heroin [94], community-distributed naloxone to prevent overdose deaths [95], strategies to reduce transmission of hepatitis C and improve access to hepatitis C treatment [96], and some strategies to improve treatment of soft tissue infections among people who inject drugs [97], there is limited research into interventions that can improve treatment of health problems that are not specifically associated with drug use. Some studies have shown that Housing First can reduce all-cause ED utilisation, though study outcomes tend to focus on substance use rather than broader health [98]. Case management (where a single case manager is assigned to each patient) can improve drug treatment outcomes, but again evidence of the effect on broader health outcomes is limited [99].
Limitations of the evidence
Most studies in the past have described patients in healthcare services to show the proportion that use drugs, rather than using population-based approaches. This has led in particular to a focus on ED and ‘frequent fliers’. To broaden this focus, we synthesised observational studies that often report healthcare utilisation as a secondary outcome. The strength of this approach is that it has shown the wide variation in utilisation of acute hospital services, and in some settings primary care may be attended more frequently. The limitation is that many studies provide limited insight into predictors and patterns of utilisation.
Half the studies in the review (43/92) rely on linked electronic healthcare records, which may have inaccuracies in diagnostic coding. For example, there is evidence that drug-related events such as overdoses are under-recorded in ED data and may be given other diagnostic codes [100,101]. This could contribute to the small proportion of healthcare episodes that are ‘drug-related’ in our results. In addition, few studies include data from the recent period when synthetic opioids such as fentanyl became more common in North American illicit drug markets. Opioid-related overdoses in the US have increased during this period [102], and the proportion of healthcare episodes that are drug-related may have increased.
The quality assessment identified non-response as the most common problem. This usually resulted from recruitment relying on volunteers or convenience samples rather than a systematic or random approach. These methods are often necessary, since it can be difficult to construct sample frames of people who use drugs. Difficulties in constructing sample frames may also account for the relative lack of studies of people using some illicit drugs, such as powder cocaine, though this may also be due to less severe health outcomes in these groups.
None of the studies included in this review looked at whether higher morbidity explained higher rates of healthcare use, so we were not able to discuss the appropriateness of health service use.
Limitations of the review and meta-analysis
First, we only included English-language studies, which may partially explain the large proportion of studies from English speaking countries – though the English-language restriction only removed 179/5,528 search results. Second, given the heterogeneity of results, meta-analysis is only intended to provide an average across studies rather than a meaningful estimate of healthcare utilisation for any specific population. Third, we defined healthcare utilisation with simple rates or proportions. While this enabled us to perform a traditional systematic review, it meant that the results provide limited insight into the appropriateness or equity of the high rates of healthcare utilisation that we observed. Finally, our review focused on three mainstream healthcare settings (primary care, ED and inpatient hospital care), and did not consider other potential sources of healthcare such as community drug treatment services, which sometimes provide a wider set of interventions. Future research should consider the full range of healthcare provision for people who use drugs, including opportunities for integration between drug treatment and mainstream health services.
Conclusion
People who use illicit drugs present to acute health services several times more often than comparison groups, across primary care, ED and inpatient settings, reflecting high morbidity. Utilisation rates are highest in those who inject drugs, homeless people and those with mental health problems. Research is needed into the quality of healthcare for people who use illicit drugs, provision of healthcare in non-acute settings, and development of health services that are considered safe and acceptable to this group.
Supplementary Material
Funding
DL and MH are funded by the National Institute for Health Research (NIHR) [DRF-2018-11-ST2-016, CDF-2016-09-014]. This paper presents independent research. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. LD and SL are supported by NHMRC Research Fellowships [GNT1041742, GNT1135991, GNT1091878, GNT1140938] and NIDA R01DA1104470. The National Drug and Alcohol Research Centre at UNSW Australia is supported by funding from the Australian Government Department of Health under the Drug and Alcohol Program. EJT is funded by the Medical Research Council [MC_UU_12017/13 & MC_UU_12017/15] and Chief Scientist Office [SPHSU13 & SPHSU15], and by a Chief Scientist Office Clinical Academic Fellowship [CAF/17/11]. AH is an NIHR Senior Investigator and is funded by the Central and North West London NHS Trust. DC is supported by the US National Institutes of Health, National Institute of Drug Abuse Grant DA037820. KIM is funded by the Wellcome Trust [109823/Z/15/Z].
Footnotes
Declarations of competing interests
TM has been a member of the organising committee for, and chaired, conferences supported by unrestricted educational grants from Reckitt Benckiser, Lundbeck, Martindale Pharma, and Britannia Pharmaceuticals Ltd (unpaid). He collaborates (unpaid) with and has received research funding from the substance misuse treatment provider Change Grow Live. He has received speaker honoraria from a commercial healthcare consultancy firm (Applied Strategic). DC reports personal fees from Mallinckrodt Pharmaceuticals and personal fees from Nektar Therapeutics, outside the submitted work.
References
- 1.Mathers BM, Degenhardt L, Bucello C, et al. Mortality among people who inject drugs: a systematic review and meta-analysis. Bulletin of the World Health Organization 2013;91:102–23. doi: 10.2471/BLT.12.108282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aldridge RW, Story A, Hwang SW, et al. Morbidity and mortality in homeless individuals, prisoners, sex workers, and individuals with substance use disorders in high-income countries: a systematic review and meta-analysis. The Lancet 2018;391:241–50. doi: 10.1016/S0140-6736(17)31869-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Degenhardt L, Larney S, Randall D, et al. Causes of death in a cohort treated for opioid dependence between 1985 and 2005: Mortality among opioid-dependent people. Addiction 2014;109:90–9. doi: 10.1111/add.12337 [DOI] [PubMed] [Google Scholar]
- 4.Degenhardt L, Bucello C, Mathers B, et al. Mortality among regular or dependent users of heroin and other opioids: a systematic review and meta-analysis of cohort studies: Mortality among opioid users. Addiction 2011;106:32–51. doi: 10.1111/j.1360-0443.2010.03140.x [DOI] [PubMed] [Google Scholar]
- 5.Fitzpatrick S, Johnsen S, White M. Multiple Exclusion Homelessness in the UK: Key Patterns and Intersections. Social Policy and Society 2011;10:501–12. doi: 10.1017/S147474641100025X [DOI] [Google Scholar]
- 6.Rogers G, Elston J, Garside R, et al. The harmful health effects of recreational ecstasy: a systematic review of observational evidence. Health Technology Assessment 2009;13. doi: 10.3310/hta13060 [DOI] [PubMed] [Google Scholar]
- 7.Volkow ND, Baler RD, Compton WM, et al. Adverse Health Effects of Marijuana Use. New England Journal of Medicine 2014;370:2219–27. doi: 10.1056/NEJMra1402309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Boekel LC, Brouwers EPM, van Weeghel J, et al. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug and Alcohol Dependence 2013;131:23–35. doi: 10.1016/j.drugalcdep.2013.02.018 [DOI] [PubMed] [Google Scholar]
- 9.Neale J, Tompkins C, Sheard L. Barriers to accessing generic health and social care services: a qualitative study of injecting drug users: Drug injectors and barriers to service use. Health & Social Care in the Community 2007;16:147–54. doi: 10.1111/j.1365-2524.2007.00739.x [DOI] [PubMed] [Google Scholar]
- 10.Summers PJ, Hellman JL, MacLean MR, et al. Negative experiences of pain and withdrawal create barriers to abscess care for people who inject heroin. A mixed methods analysis. Drug and Alcohol Dependence 2018;190:200–8. doi: 10.1016/j.drugalcdep.2018.06.010 [DOI] [PubMed] [Google Scholar]
- 11.Sanjuan PM, Rice SL, Witkiewitz K, et al. Alcohol, tobacco, and drug use among emergency department patients. Drug and Alcohol Dependence 2014;138:32–8. doi: 10.1016/j.drugalcdep.2014.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Macias Konstantopoulos WL, Dreifuss JA, McDermott KA, et al. Identifying Patients With Problematic Drug Use in the Emergency Department: Results of a Multisite Study. Annals of Emergency Medicine 2014;64:516–25. doi: 10.1016/j.annemergmed.2014.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prevalence Binks S. and healthcare burden of illegal drug use among emergency department patients. Emergency Medicine Journal 2005;22:872–3. doi: 10.1136/emj.2004.022665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Urbanoski K, Cheng J, Rehm J, et al. Frequent use of emergency departments for mental and substance use disorders. Emergency Medicine Journal 2018;35:220–5. doi: 10.1136/emermed-2015-205554 [DOI] [PubMed] [Google Scholar]
- 15.Byrne M, Murphy AW, Plunkett PK, et al. Frequent attenders to an emergency department: A study of primary health care use, medical profile, and psychosocial characteristics. Annals of Emergency Medicine 2003;41:309–18. doi: 10.1067/mem.2003.68 [DOI] [PubMed] [Google Scholar]
- 16.Dent A, Hunter G, Webster AP. The impact of frequent attenders on a UK emergency department. European Journal of Emergency Medicine 2010;17:332–6. doi: 10.1097/MEJ.0b013e328335623d [DOI] [PubMed] [Google Scholar]
- 17.Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;349:g7647–g7647. doi: 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 18.Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. https://web.archive.org/web/20190609041323/http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed 18 Jan 2018).
- 19.Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan—a web and mobile app for systematic reviews. Systematic Reviews 2016;5. doi: 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. National Hospital Ambulatory Medical Care Survey: 2015 Emergency Department Summary Tables. 2015https://web.archive.org/web/20190422173149/https://www.cdc.gov/nchs/data/nhamcs/web_tables/2015_ed_web_tables.pdf (accessed 12 Dec 2018).
- 21.Australian Institute of Health and Welfare. Emergency department care 2016–17: Australian hospital statistics. 2017https://web.archive.org/web/20190329121754/https://www.aihw.gov.au/reports/hospitals/ahs-2016-17-emergency-department-care/data (accessed 12 Dec 2018).
- 22.NHS Digital. Hospital Accident and Emergency Activity, 2017–18. 2018https://web.archive.org/web/20190426044531/https://digital.nhs.uk/data-and-information/publications/statistical/hospital-accident--emergency-activity/2017-18 (accessed 12 Dec 2018).
- 23.Viechtbauer W Conducting Meta-Analyses in R with the metafor Package. Journal of Statistical Software 2010;36. doi: 10.18637/jss.v036.i03 [DOI] [Google Scholar]
- 24.Chen Y-C, Chen C-K, Lin S-K, et al. Health care service utilization and associated factors among heroin users in northern Taiwan. Addictive Behaviors 2013;38:2635–8. doi: 10.1016/j.addbeh.2013.06.023 [DOI] [PubMed] [Google Scholar]
- 25.Fairbairn N, Milloy M-J, Zhang R, et al. Emergency Department Utilization among a Cohort of HIV-positive Injecting Drug Users in a Canadian Setting. The Journal of Emergency Medicine 2012;43:236–43. doi: 10.1016/j.jemermed.2011.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clay E, Khemiri A, Zah V, et al. Persistence and healthcare utilization associated with the use of buprenorphine/naloxone film and tablet formulation therapy in adults with opioid dependence. Journal of Medical Economics 2014;17:626–36. doi: 10.3111/13696998.2014.925463 [DOI] [PubMed] [Google Scholar]
- 27.Ngamini-Ngui A, Fleury M-J, Moisan J, et al. High Users of Emergency Departments in Quebec Among Patients With Both Schizophrenia and a Substance Use Disorder. Psychiatric Services 2014;65:1389–91. doi: 10.1176/appi.ps.201300474 [DOI] [PubMed] [Google Scholar]
- 28.Schmidt LM, Hesse M, Lykke J. The impact of substance use disorders on the course of schizophrenia—A 15-year follow-up study. Schizophrenia Research 2011;130:228–33. doi: 10.1016/j.schres.2011.04.011 [DOI] [PubMed] [Google Scholar]
- 29.Campbell CI, Bahorik AL, Kline-Simon AH, et al. The role of marijuana use disorder in predicting emergency department and inpatient encounters: A retrospective cohort study. Drug and Alcohol Dependence 2017;178:170–5. doi: 10.1016/j.drugalcdep.2017.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kendall CE, Boucher LM, Mark AE, et al. A cohort study examining emergency department visits and hospital admissions among people who use drugs in Ottawa, Canada: Harm Reduction Journal; 2017;14. doi: 10.1186/s12954-017-0143-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bahorik AL, Satre DD, Kline-Simon AH, et al. Alcohol, marijuana, and opioid use disorders: 5-Year patterns and characteristics of emergency department encounters. Substance Abuse 2018;39:59–68. doi: 10.1080/08897077.2017.1356789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen I-M, Huang CL-C, Yeh B-J, et al. Health service utilization of heroin abusers: A retrospective cohort study. Addictive Behaviors 2015;45:281–6. doi: 10.1016/j.addbeh.2015.01.042 [DOI] [PubMed] [Google Scholar]
- 33.Choi NG, Marti CN, DiNitto DM, et al. Older adults’ marijuana use, injuries, and emergency department visits. The American Journal of Drug and Alcohol Abuse 2018;44:215–23. doi: 10.1080/00952990.2017.1318891 [DOI] [PubMed] [Google Scholar]
- 34.Tran BX, Phan HTT, Nguyen LH, et al. Economic vulnerability of methadone maintenance patients: Implications for policies on co-payment services. International Journal of Drug Policy 2016;31:131–7. doi: 10.1016/j.drugpo.2016.01.017 [DOI] [PubMed] [Google Scholar]
- 35.Turner BJ, Laine C, Yang CP, et al. Effects of Long‐Term, Medically Supervised, Drug‐Free Treatment and Methadone Maintenance Treatment on Drug Users’ Emergency Department Use and Hospitalization. Clinical Infectious Diseases 2003;37:S457–63. doi: 10.1086/377558 [DOI] [PubMed] [Google Scholar]
- 36.Graham K, Cheng J, Bernards S, et al. How Much Do Mental Health and Substance Use/Addiction Affect Use of General Medical Services? Extent of Use, Reason for Use, and Associated Costs. The Canadian Journal of Psychiatry 2017;62:48–56. doi: 10.1177/0706743716664884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Onyeka IN, Beynon CM, Ronkainen K, et al. Hospitalization in a Cohort Seeking Treatment for Illicit Drug Use in Finland. Journal of Substance Abuse Treatment 2015;53:64–70. doi: 10.1016/j.jsat.2014.12.009 [DOI] [PubMed] [Google Scholar]
- 38.Pavarin RM, Gambini D. Health status of users of the Bologna local health authority drug addiction treatment services: a study of hospital admissions in the period 2004–2013. Infez Med 2015;23:5–11. [PubMed] [Google Scholar]
- 39.Tarricone I, Boydell J, Panigada S, et al. The impact of substance use at psychosis onset on First Episode Psychosis course: Results from a 1 year follow-up study in Bologna. Schizophrenia Research 2014;153:60–3. doi: 10.1016/j.schres.2014.01.014 [DOI] [PubMed] [Google Scholar]
- 40.Bhandari S, Hillard CJ, Venkatesan T. Marijuana users do not have increased healthcare utilization: A National Health and Nutrition Examination Survey (NHANES) study. European Journal of Internal Medicine 2016;34:e9–10. doi: 10.1016/j.ejim.2016.07.023 [DOI] [PubMed] [Google Scholar]
- 41.Skeie I, Brekke M, Lindbæk M, et al. Somatic health among heroin addicts before and during opioid maintenance treatment: a retrospective cohort study. BMC Public Health 2008;8. doi: 10.1186/1471-2458-8-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cucciare MA, Han X, Timko C, et al. Longitudinal associations between outpatient medical care use and substance use among rural stimulant users. The American Journal of Drug and Alcohol Abuse 2018;44:235–43. doi: 10.1080/00952990.2017.1339056 [DOI] [PubMed] [Google Scholar]
- 43.Lubman DI, Garfield JBB, Manning V, et al. Characteristics of individuals presenting to treatment for primary alcohol problems versus other drug problems in the Australian patient pathways study. BMC Psychiatry 2016;16. doi: 10.1186/s12888-016-0956-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cullen W, O’Brien S, O’Carroll A, et al. Chronic illness and multimorbidity among problem drug users: a comparative cross sectional pilot study in primary care. BMC Family Practice 2009;10. doi: 10.1186/1471-2296-10-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Riley ED, Wu AW, Junge B, et al. Health services utilization by injection drug users participating in a needle exchange programme. The American Journal of Drug and Alcohol Abuse 2002;28:497–511. doi: 10.1081/ADA-120006738 [DOI] [PubMed] [Google Scholar]
- 46.Kelly E, McKetin R, McLaren J. Health service utilisation among regular methamphetamine users. Sydney:: NDARC 2005. https://web.archive.org/web/20190410220251/https://ndarc.med.unsw.edu.au/resource/health-service-utilisation-among-regular-methamphetamine-users (accessed 9 Nov 2018).
- 47.Artenie AA, Jutras-Aswad D, Roy é., et al. Visits to primary care physicians among persons who inject drugs at high risk of hepatitis C virus infection: room for improvement. Journal of Viral Hepatitis 2015;22:792–9. doi: 10.1111/jvh.12393 [DOI] [PubMed] [Google Scholar]
- 48.Darke S, Ross J, Teesson M, et al. Health service utilization and benzodiazepine use among heroin users: findings from the Australian Treatment Outcome Study (ATOS). Addiction 2003;98:1129–35. doi: 10.1046/j.1360-0443.2003.00430.x [DOI] [PubMed] [Google Scholar]
- 49.Darke S, Marel C, Ross J, et al. Health Service Utilization Among Heroin Users: 11-Year Follow-up of the Australian Treatment Outcome Study Cohort. Addictive Disorders & Their Treatment 2015;14:159–66. doi: 10.1097/ADT.0000000000000069 [DOI] [Google Scholar]
- 50.Horyniak D, Higgs P, Jenkinson R, et al. Establishing the Melbourne injecting drug user cohort study (MIX): rationale, methods, and baseline and twelve-month follow-up results. Harm Reduction Journal 2013;10:11. doi: 10.1186/1477-7517-10-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lintzeris N, Rivas C, Monds LA, et al. Substance use, health status and service utilisation of older clients attending specialist drug and alcohol services: Older drug and alcohol clients. Drug and Alcohol Review 2016;35:223–31. doi: 10.1111/dar.12266 [DOI] [PubMed] [Google Scholar]
- 52.McCarty D, Perrin NA, Green CA, et al. Methadone maintenance and the cost and utilization of health care among individuals dependent on opioids in a commercial health plan. Drug and Alcohol Dependence 2010;111:235–40. doi: 10.1016/j.drugalcdep.2010.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Marshall BDL, Grafstein E, Buxton JA, et al. Frequent methamphetamine injection predicts emergency department utilization among street-involved youth. Public Health 2012;126:47–53. doi: 10.1016/j.puhe.2011.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Juday TR, Wu A, Celentano DD, et al. The role of Medicaid HMO enrollment in the longitudinal utilization of medical care services in a cohort of injecting drug users in Baltimore, Maryland. Substance Abuse 2003;24:27–41. doi: 10.1080/08897070309511531 [DOI] [PubMed] [Google Scholar]
- 55.Palepu A, Tyndall MW, Leon H, et al. Hospital utilization and costs in a cohort of injection drug users. CMAJ 2001;165:415–20. [PMC free article] [PubMed] [Google Scholar]
- 56.Stein M Injection frequency mediates health service use among persons with a history of drug injection. Drug and Alcohol Dependence 2003;70:159–68. doi: 10.1016/S0376-8716(02)00344-7 [DOI] [PubMed] [Google Scholar]
- 57.Burnette ML, Lucas E, Ilgen M, et al. Prevalence and Health Correlates of Prostitution Among Patients Entering Treatment for Substance Use Disorders. Archives of General Psychiatry 2008;65:337. doi: 10.1001/archpsyc.65.3.337 [DOI] [PubMed] [Google Scholar]
- 58.Kerr T, Wood E, Grafstein E, et al. High Rates of Primary Care and Emergency Department Use Among Injection Drug Users in Vancouver. Journal of Public Health 2005;27:62–6. doi: 10.1093/pubmed/fdh189 [DOI] [PubMed] [Google Scholar]
- 59.Reynolds GL, Fisher DG, Wood MM, et al. Use of Emergency Room Services by Out-of-Treatment Drug Users in Long Beach, California: Journal of Addictive Diseases; 2003;22:1–13. doi: 10.1300/J069v22n02_01 [DOI] [PubMed] [Google Scholar]
- 60.Cederbaum JA, Guerrero EG, Mitchell KR, et al. Utilization of emergency and hospital services among individuals in substance abuse treatment. Substance Abuse Treatment, Prevention, and Policy 2014;9:16. doi: 10.1186/1747-597X-9-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nambiar D, Stoové M, Dietze P. Frequent emergency department presentations among people who inject drugs: A record linkage study. International Journal of Drug Policy 2017;44:115–20. doi: 10.1016/j.drugpo.2017.03.010 [DOI] [PubMed] [Google Scholar]
- 62.Knowlton AR, Hoover DR, Chung S, et al. Access to medical care and service utilization among injection drug users with HIV/AIDS. Drug and Alcohol Dependence 2001;64:55–62. doi: 10.1016/S0376-8716(00)00228-3 [DOI] [PubMed] [Google Scholar]
- 63.Siegal HA, Falck RS, Wang J, et al. Emergency Department Utilization by Crack-Cocaine Smokers in Dayton, Ohio. The American Journal of Drug and Alcohol Abuse 2006;32:55–68. doi: 10.1080/00952990500328737 [DOI] [PubMed] [Google Scholar]
- 64.Whittaker E, Swift W, Roxburgh A, et al. Multiply disadvantaged: Health and service utilisation factors faced by homeless injecting drug consumers in Australia: Issues faced by homeless injecting drug users. Drug and Alcohol Review 2015;34:379–87. doi: 10.1111/dar.12257 [DOI] [PubMed] [Google Scholar]
- 65.Dietze P, Jenkinson R, Aitken C, et al. The relationship between alcohol use and injecting drug use: Impacts on health, crime and wellbeing. Drug and Alcohol Dependence 2013;128:111–5. doi: 10.1016/j.drugalcdep.2012.08.013 [DOI] [PubMed] [Google Scholar]
- 66.Ryder N, Cullen W, Barry J, et al. Prevalence of problem alcohol use among patients attending primary care for methadone treatment. BMC Family Practice 2009;10. doi: 10.1186/1471-2296-10-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nguyen LH, Nguyen LHT, Boggiano VL, et al. Quality of life and healthcare service utilization among methadone maintenance patients in a mountainous area of Northern Vietnam. Health and Quality of Life Outcomes 2017;15. doi: 10.1186/s12955-017-0633-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lloyd-Smith E, Wood E, Zhang R, et al. Risk factors for developing a cutaneous injection-related infection among injection drug users: a cohort study. BMC Public Health 2008;8. doi: 10.1186/1471-2458-8-405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shoenbaum EE, Lo Y, Floris-Moore M. Predictors of hospitalization for HIV-positive women and men drug users, 1996–2000. Public Health Rep 2002;117:S60–6. [PMC free article] [PubMed] [Google Scholar]
- 70.Baum MK, Jayaweera DT, Duan R, et al. Quality of Life, Symptomatology and Healthcare Utilization in HIV/HCV Co-Infected Drug Users in Miami. Journal of Addictive Diseases 2008;27:37–48. doi: 10.1300/J069v27n02_05 [DOI] [PubMed] [Google Scholar]
- 71.Merrall E, Bird S, Hutchinson S. A record linkage study of hospital episodes for drug treatment clients in Scotland, 1996–2006. Addiction Research & Theory 2013;21:52–61. doi: 10.3109/16066359.2012.690052 [DOI] [PubMed] [Google Scholar]
- 72.Laine C Regular Outpatient Medical and Drug Abuse Care and Subsequent Hospitalization of Persons Who Use Illicit Drugs. JAMA 2001;285:2355. doi: 10.1001/jama.285.18.2355 [DOI] [PubMed] [Google Scholar]
- 73.Floris-Moore M, Lo Y, Klein RS, et al. Gender and Hospitalization Patterns Among HIV-Infected Drug Users Before and After the Availability of Highly Active Antiretroviral Therapy. J Acquir Immune Defic Syndr 2003;34:331–7. [DOI] [PubMed] [Google Scholar]
- 74.Nambiar D, Stoové M, Dietze P. A cross-sectional study describing factors associated with utilisation of GP services by a cohort of people who inject drugs. BMC Health Services Research 2014;14. doi: 10.1186/1472-6963-14-308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Baser O, Chalk M, Fiellin DA, et al. Cost and Utilization Outcomes of Opioid-Dependence Treatments. American Journal of Managed Care 2011;17. [PubMed] [Google Scholar]
- 76.Lo-Ciganic W-H, Gellad WF, Gordon AJ, et al. Association between trajectories of buprenorphine treatment and emergency department and in-patient utilization: Buprenorphine trajectories and outcomes. Addiction 2016;111:892–902. doi: 10.1111/add.13270 [DOI] [PubMed] [Google Scholar]
- 77.Schwarz R, Zelenev A, Bruce RD, et al. Retention on buprenorphine treatment reduces emergency department utilization, but not hospitalization, among treatment-seeking patients with opioid dependence. Journal of Substance Abuse Treatment 2012;43:451–7. doi: 10.1016/j.jsat.2012.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lynch FL, McCarty D, Mertens J, et al. Costs of care for persons with opioid dependence in commercial integrated health systems. Addiction Science & Clinical Practice 2014;9:16. doi: 10.1186/1940-0640-9-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mohlman MK, Tanzman B, Finison K, et al. Impact of Medication-Assisted Treatment for Opioid Addiction on Medicaid Expenditures and Health Services Utilization Rates in Vermont. Journal of Substance Abuse Treatment 2016;67:9–14. doi: 10.1016/j.jsat.2016.05.002 [DOI] [PubMed] [Google Scholar]
- 80.Robertson AG, Easter MM, Lin H-J, et al. Associations between pharmacotherapy for opioid dependence and clinical and criminal justice outcomes among adults with co-occurring serious mental illness. Journal of Substance Abuse Treatment 2018;86:17–25. doi: 10.1016/j.jsat.2017.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shcherbakova N, Tereso G, Spain J, et al. Treatment Persistence Among Insured Patients Newly Starting Buprenorphine/Naloxone for Opioid Use Disorder. Annals of Pharmacotherapy 2018;52:405–14. doi: 10.1177/1060028017751913 [DOI] [PubMed] [Google Scholar]
- 82.Walley AY, Cheng DM, Pierce CE, et al. Methadone Dose, Take Home Status, and Hospital Admission Among Methadone Maintenance Patients: Journal of Addiction Medicine 2012;6:186–90. doi: 10.1097/ADM.0b013e3182584772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nambiar D, Stoové M, Hickman M, et al. A prospective cohort study of hospital separations among people who inject drugs in Australia: 2008–2013. BMJ Open 2017;7:e014854. doi: 10.1136/bmjopen-2016-014854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Aitken C, Kerr T, Hickman M, et al. A cross-sectional study of emergency department visits by people who inject drugs. Emergency Medicine Journal 2912;30. doi: 10.1136/emermed-2012-201170 [DOI] [PubMed] [Google Scholar]
- 85.Mitchell AJ, Malone D, Doebbeling CC. Quality of medical care for people with and without comorbid mental illness and substance misuse: systematic review of comparative studies. British Journal of Psychiatry 2009;194:491–9. doi: 10.1192/bjp.bp.107.045732 [DOI] [PubMed] [Google Scholar]
- 86.Desai MM, Rosenheck RA, Druss BG, et al. Mental Disorders and Quality of Diabetes Care in the Veterans Health Administration. American Journal of Psychiatry 2002;159:1584–90. doi: 10.1176/appi.ajp.159.9.1584 [DOI] [PubMed] [Google Scholar]
- 87.Zarkin GA, Bray JW, Babor TF, et al. Alcohol Drinking Patterns and Health Care Utilization in a Managed Care Organization. Health Services Research 2004;39:553–70. doi: 10.1111/j.1475-6773.2004.00244.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hope VD, Marongiu A, Parry JV, et al. The extent of injection site infection in injecting drug users: findings from a national surveillance study. Epidemiology and Infection 2010;138:1510–8. doi: 10.1017/S0950268810000324 [DOI] [PubMed] [Google Scholar]
- 89.Shah A, Duncan M, Atreja N, et al. Healthcare utilization and costs associated with treatment for opioid dependence. Journal of Medical Economics 2018;21:406–15. doi: 10.1080/13696998.2018.1427101 [DOI] [PubMed] [Google Scholar]
- 90.Gourevitch MN, Chatterji P, Deb N, et al. On-site medical care in methadone maintenance: Associations with health care use and expenditures. Journal of Substance Abuse Treatment 2007;32:143–51. doi: 10.1016/j.jsat.2006.07.008 [DOI] [PubMed] [Google Scholar]
- 91.Manhapra A, Agbese E, Leslie DL, et al. Three-Year Retention in Buprenorphine Treatment for Opioid Use Disorder Among Privately Insured Adults. Psychiatric Services 2018;69:768–76. doi: 10.1176/appi.ps.201700363 [DOI] [PubMed] [Google Scholar]
- 92.Dixon-Woods M, Cavers D, Agarwal S, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Medical Research Methodology 2006;6. doi: 10.1186/1471-2288-6-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Harris M, Rhodes T. Hepatitis C treatment access and uptake for people who inject drugs: a review mapping the role of social factors. Harm Reduction Journal 2013;10:7. doi: 10.1186/1477-7517-10-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sordo L, Barrio G, Bravo MJ, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ 2017;:j1550. doi: 10.1136/bmj.j1550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Clark AK, Wilder CM, Winstanley EL. A Systematic Review of Community Opioid Overdose Prevention and Naloxone Distribution Programs: Journal of Addiction Medicine 2014;8:153–63. doi: 10.1097/ADM.0000000000000034 [DOI] [PubMed] [Google Scholar]
- 96.Hagan H, Pouget ER, Des Jarlais DC. A Systematic Review and Meta-Analysis of Interventions to Prevent Hepatitis C Virus Infection in People Who Inject Drugs. Journal of Infectious Diseases 2011;204:74–83. doi: 10.1093/infdis/jir196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Harris HW, Young DM. Care of Injection Drug Users With Soft Tissue Infections in San Francisco, California. Archives of Surgery 2002;137:1217. doi: 10.1001/archsurg.137.11.1217 [DOI] [PubMed] [Google Scholar]
- 98.Woodhall-Melnik JR, Dunn JR. A systematic review of outcomes associated with participation in Housing First programs. Housing Studies 2016;31:287–304. doi: 10.1080/02673037.2015.1080816 [DOI] [Google Scholar]
- 99.Hesse M, Rapp R, Broekaert E, et al. Case management for persons with substance use disorders. Cochrane Database of Systematic Reviews 2007;4. doi: 10.1002/14651858.CD006265.pub2 [DOI] [PubMed] [Google Scholar]
- 100.Wood DM, Conran P, Dargan PI. ICD-10 coding: poor identification of recreational drug presentations to a large emergency department. Emergency Medicine Journal 2011;28:387–9. doi: 10.1136/emj.2009.088344 [DOI] [PubMed] [Google Scholar]
- 101.Di Rico R, Nambiar D, Stoové M, et al. Drug overdose in the ED: a record linkage study examining emergency department ICD-10 coding practices in a cohort of people who inject drugs. BMC Health Services Research 2018;18. doi: 10.1186/s12913-018-3756-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Slavova S, Costich JF, Bunn TL, et al. Heroin and fentanyl overdoses in Kentucky: Epidemiology and surveillance. International Journal of Drug Policy 2017;46:120–9. doi: 10.1016/j.drugpo.2017.05.051 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.