Abstract
Serial neurocognitive and perfusion MR imaging findings are described in the perioperative course of a 48-year-old woman with a superficial temporal artery to middle cerebral artery bypass for right hemispheric ischemia due to moyamoya syndrome. Neurocognitive testing reflected both global and focal cerebrovascular dysfunction, which suggests that perfusion augmentation following surgical revascularization may engender cognitive and neurologic improvement beyond focal regions of established ischemia.
Moyamoya syndrome is a rare cerebrovascular disorder characterized by progressive stenosis and occlusion of the internal carotid and the anterior and middle cerebral arteries (MCAs).1 These vascular lesions result in exuberant recruitment of collaterals, typically forming a network of friable vessels in the lenticulostriate distribution. The cloudy angiographic appearance of these diminutive collaterals may suggest a puff of smoke, originally termed “moyamoya” in Japanese.
Moyamoya syndrome is uncommon outside Asia, with only 239 cases reported in the United States before 1996.2 Women are somewhat more vulnerable, with a male:female ratio of 3:2.3 The age of onset is distributed bimodally, with the highest incidence occurring in the first decade of life and another peak occurring in the third or fourth decade.3 The etiology is uncertain with existing theories for both congenital and acquired causes.
Clinical features vary dramatically as patients may be completely asymptomatic, or they may present with intracranial hemorrhage. Neuropsychological effects may be profound, though such impairments go undocumented. Treatment is aimed at ameliorating clinical symptoms, yet definitive therapy and prevention of recurrent ischemia rely on surgical revascularization. One revascularization technique involves dissecting and rerouting a branch of the superficial temporal artery (STA) to a distal branch of the MCA (ie, STA-MCA bypass), thereby providing increased blood flow from the extracranial circulation to potentially ischemic regions beyond the occlusive lesions in the proximal cerebral arteries. Surgical revascularization is favored over medical management in children, but limited data are available regarding the effectiveness of such an arterial bypass in adults.
Postoperative augmentation of perfusion following bypass may diminish cognitive dysfunction associated with ischemia, though there are few published cases reporting neuropsychological status pre- and postrevascularization. Available studies have primarily focused on children for whom the data are limited to intellectual assessments compared with examination of discrete neurocognitive abilities. Developmental variables that affect plasticity, the spontaneous rate of recovery, and cortical reorganization restrict the generalizability of the pediatric literature to adults.
We present the case of a 48-year-old woman with moyamoya syndrome who underwent revascularization following a right hemispheric stroke. The neuropsychological and perfusion MR imaging findings illustrate a temporal relationship between the vascular effects of the bypass procedure and an improvement in neurocognitive status.
Methods
Case Presentation
At the age of 48, a right-handed female attorney presented with acute onset of mild left-sided weakness, left hemineglect, confusion, and slurred speech. Her medical history was significant for hypertension, hypercholesterolemia, and diabetes mellitus. Diffusion-weighted imaging (DWI) revealed infarction in a deep border-zone region of the right hemisphere. Although carotid duplex ultrasonography suggested complete occlusion of the right internal carotid artery, subsequent MR angiography (MRA) revealed trickle flow. Intracranial MRA revealed only minimal flow in the right MCA with collateral preservation of the right anterior cerebral artery. Despite aggressive medical management including anticoagulation, her neurologic status worsened, with severe left hemiparesis and increased confusion. Digital subtraction angiography confirmed the pattern of severe, multifocal occlusive disease on MRA, including severe stenosis of the terminal left internal carotid artery with prominent leptomeningeal collateral filling of the right MCA territory from the anterior and posterior cerebral arteries. The relatively limited extent of border-zone infarction with collateral sparing of most of the right MCA territory prompted consideration of surgical revascularization.
Neuropsychological Assessment
Formal neuropsychological evaluation was conducted 3 months before bypass surgery, which was also 7 months after the right hemispheric stroke. Specific measures administered are listed in the Table. Multiple domains were assessed, including language, visuospatial functions, as well as nonverbal and verbal learning and memory. Assessment was reconducted approximately 6 weeks postneurosurgery, corresponding to 1 year post-stroke, by using alternate test forms when possible.
Presurgical and postsurgical neurophysiological data*
| Neuropsychological Measure* | Presurgical Performance | Postsurgical Performance |
|---|---|---|
| Language | ||
| Boston Naming Test (z) | 0.78 | 1.00 |
| Controlled Oral Word Association (percentile) | 25th–75th | 25th–75th |
| WASI: vocabulary subtest (ss) | 14 | NR |
| WASI: similarities subtest (ss) | 13 | NR |
| Visuospatial functions | ||
| WMS-III Spatial Span (ss) | 10 | 12 |
| JOLO (percentile) | <1st | 40th |
| Benton Facial Recognition (percentile) | 33rd–59th | 33rd–59th |
| HVOT (T) | 53 | 58 |
| WASI: block design subtest (ss) | 7 | 8 |
| WASI: matrix reasoning subest (ss) | 11 | 10 |
| Nonverbal learning and memory | ||
| BFLT Total Learning (z) | −3.46 | −2.1 |
| BFLT Delayed Recall (z) | −2.59 | −2.5 |
| BFLT Recognition Discriminability Index | 89% | 89% |
| GFMT Immediate Recognition (percentile) | 10th–20th | 50th |
| GFMT Delayed Recognition (percentile) | <1st | <5th |
| Verbal learning and memory | ||
| CVLT Total Learning (T) | 38 | 64 |
| CVLT Delayed Recall (z) | 0 | 1.5 |
| CVLT Recognition Disriminability Index | 98% | 98% |
| PMT Immediate Recognition (z) | 0.3 | 0.3 |
| PMT Delayed Recognition (z) | 0.4 | 0.4 |
Note:—WASI indicates Wechsler Abbreviated Scales of Intelligence; NR, task not repeated on follow-up evaluation; WMS-III, Wechsler Memory Scale-III; BFLT, Biber Figure Learning Test; GFM, Graduate Facial Memory Test; CVLT, California Verbal Learning Test; PMT, Pseudoword Memory Test; HVOT, Hooper Visual Organization Test; JOLO, Judgement of Line Orientation.
Perfusion MR Imaging
Continuous arterial spin-labeled perfusion MR imaging was acquired 3 months before and 5 days after surgical revascularization. This noninvasive technique uses magnetically labeled arterial blood as a diffusible flow tracer to provide quantitative measures of cerebral perfusion.4,5 Normal perfusion values are approximately 50 mL/100 g/min. Perfusion values diminish with increasing severity of ischemia, leading to cellular dysfunction <20 mL/100 g/min and infarction <10 mL/100 g/min.
Revascularization Procedure
Extracranial-intracranial arterial bypass was performed to augment perfusion in the right cerebral hemisphere. STA-MCA bypass was initiated by performing a craniotomy and opening the dura anterior to the right ear. A branch of the STA was dissected for anastomosis to the MCA. A temporal branch of the distal MCA was selected, and the arachnoid overlying the MCA was dissected off to isolate an appropriate length of vessel. An end-to-side anastomosis was then performed, connecting the mobilized STA to the distal MCA branch. Intraoperative and postoperative angiography confirmed patency of the bypass.
Results
Preoperative neuropsychological assessment revealed findings consistent with the patient's educational and occupational background. Strong language and verbal reasoning abilities were noted, including intact naming, verbal fluency, abstract verbal reasoning, and expressive word knowledge. In light of the right hemispheric stroke, performances on tasks involving visuospatial perception, organization, and construction were generally impaired with respect to estimated premorbid abilities. Particular impairment was noted in appreciation of spatial relationships (JOLO). Consistent with those visuoperceptual difficulties, she demonstrated profound impairment in nonverbal visuospatial memory. Surprisingly, however, she also demonstrated slight compromise of verbal memory abilities (Table).
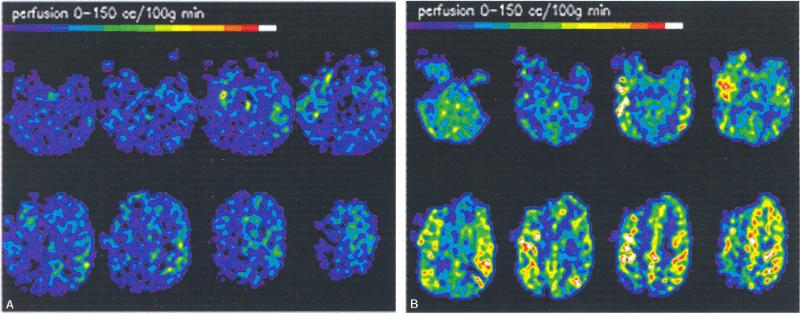
Preoperative perfusion MR imaging suggested hypoperfusion in both cerebral hemispheres (Fig 1). Cerebral blood flow averaged 20 mL/100 g/min in the right hemisphere and 27 mL/100 g/min in the left.
Fig 1.
Quantitative continuous arterial spin-labeling perfusion MR imaging (left, preoperative; right, postoperative).
Postoperative neuropsychological assessment was conducted 5 weeks after the bypass procedure. In light of the right-sided revascularization technique, we anticipated that functions mediated by the right hemisphere would improve. Indeed, visuospatial performance improved to the normal range (JOLO). Although nonverbal visuospatial memory performances did not reach premorbid levels, they did improve considerably on 2 of 4 indexes. In addition, improvements were noted in cognitive domains, presumably mediated by the left hemisphere, unaffected by the original right hemispheric stroke and right-sided bypass procedure. Specifically, verbal learning and delayed recall performances improved dramatically (Table).
Postoperative cerebral blood flow values on perfusion MR imaging increased to normal levels in both hemispheres (Fig 1). Cerebral blood flow increased to an average of 53 mL/100 g/min in the right hemisphere and 56 mL/100 g/min in the left.
Discussion
The neuropsychological and perfusion MR imaging data from the present case demonstrate the relatively subtle, yet important, cognitive deficits that are engendered by hypoperfusion. Diminished cerebral perfusion may lead to regional dysfunction in the absence of overt infarction. Associated neurocognitive dysfunction is considerably disabling in chronic cerebrovascular disorders, including moyamoya syndrome, emphasizing the importance of neuropsychological evaluation. The improvement in cognitive function cannot be wholly attributed to spontaneous recovery of function or practice effects because the presurgical neuropsychological evaluation was conducted 7 months poststroke and alternate test forms were used when possible (eg, CVLT).
Perfusion imaging studies reveal focal regions of diminished cerebral blood flow, though current techniques vary in diagnostic accuracy. Contrast-based perfusion techniques provide relative measures of cerebral blood flow that may fail to identify balanced or multifocal areas of hypoperfusion. Absolute or quantitative measures of cerebral perfusion may be obtained with continuous arterial spin-labeling. This technique may be performed serially to evaluate ongoing changes in perfusion because of chronic cerebrovascular disorders. Revascularization, as in this case, may also be monitored with serial perfusion imaging as has previously been reported in another moyamoya case.6
Focal perfusion abnormalities are commonly identified in acute stroke. Regional hypoperfusion may be clinically manifest, though therapeutic modulation of cerebral perfusion, including induced hypertension, may mask such clinical manifestations. Improvement of cerebral perfusion with surgical revascularization led to reversal of both focal and relatively remote areas of hypoperfusion. Left hemispheric dysfunction and hypoperfusion were eliminated in the postoperative phase. Such changes in remote regions may reflect an exquisite dependence on collateral blood flow, which determines residual perfusion in the presence of proximal vascular compromise. Multifocal vascular lesions may elicit a complex pattern of collateral recruitment. Eliminating the collateral demand of a focal brain region with surgical revascularization may allow for the redistribution of collateral circulation. In this case, STA-MCA blood flow improved right hemispheric perfusion and enabled collateral blood flow to compensate more effectively for perfusion deficits associated with left internal carotid artery stenosis. Surgical revascularization of a given arterial distribution in moyamoya may therefore address multifocal or global dysfunction that is clinically detectable as focal and global cognitive improvement following revascularization.
Moyamoya may be characterized by a pattern of primary vascular lesions including stenoses and occlusions, yet the clinical course is determined by the corresponding collateral circulation. Hypoperfusion and resultant neurologic or cognitive dysfunction become manifest because of collateral failure. Furthermore, the therapy of this unusual condition is directed at improving collateral flow. The complex patterns of collateral blood flow may evade standard diagnostic approaches with structural imaging, though perfusion studies may confirm clinical observations. The neuropsychological and perfusion imaging correlates in this case suggest that regional revascularization, such as STA-MCA bypass, may also improve global cerebral blood flow.
Footnotes
A portion of this work was presented at the 22nd annual meeting of the National Academy of Neuropsychology, Miami, Fla, October 9−12, 2002.
References
- 1.Takeuchi K, Shimizu K. Hypoplasia of the bilateral internal carotid arteries. Brain Nerve. 1957;9:37–43. [in Japanese with English abstract] [Google Scholar]
- 2.Chiu D, Shedden P, Bratina P, et al. Clinical features of Moyamoya disease in the United States. Stroke. 1998;29:1347–51. doi: 10.1161/01.str.29.7.1347. [DOI] [PubMed] [Google Scholar]
- 3.Suzuki J, Kodama N. Moyamoya disease: a review. Stroke. 1983;14:104–109. doi: 10.1161/01.str.14.1.104. [DOI] [PubMed] [Google Scholar]
- 4.Detre J, Alsop D, Vives L, et al. Noninvasive MRI evaluation of cerebral blood flow in cerebrovascular disease. Neurology. 1998;50:633–41. doi: 10.1212/wnl.50.3.633. [DOI] [PubMed] [Google Scholar]
- 5.Alsop D, Detre J. Multisection cerebral blood flow MR imaging with continuous arterial spin labeling. Radiology. 1998;208:410–16. doi: 10.1148/radiology.208.2.9680569. [DOI] [PubMed] [Google Scholar]
- 6.Wityk RJ, Hillis A, Beauchamp N, et al. Perfusion-weighted magnetic resonance imaging in adult moyamoya syndrome: characteristic patterns and change after surgical intervention: case report. Neurosurgery. 2002;51:1499–1505. [PubMed] [Google Scholar]
- 7.Lezak MD. Neuropsychological assessment. 3rd ed. Oxford University Press; New York: 1995. [Google Scholar]
- 8.Spreen O, Strauss E. A compendium of neuropsychological tests. Oxford University Press; New York: 1991. [Google Scholar]